Abstract
Antisocial personality disorder (APD) is a serious public and mental health concern. Understanding how well conduct disorder (CD) and other mental disorders predict the development of APD among youth involved in the juvenile justice system is critical for prevention. This study used a stratified random sample of 1112 detained youth to examine the development of APD at a three-year follow-up interview. Nearly one fifth of male juvenile detainees later developed APD; approximately one quarter of male juvenile detainees with CD at baseline later developed APD. Significantly more males than females developed APD; no differences were found by race/ethnicity. Having five or more symptoms of CD, dysthymia, alcohol use disorder, or generalized anxiety disorder was significantly associated with developing modified APD (M-APD; APD without the CD requirement). Some disorders were strong predictors of APD; however, none were adequate screeners for identifying which detainees would later develop M-APD. The findings of this study have implications for interventions and further research in developmental psychopathology.
Keywords: conduct disorder, antisocial personality disorder, mental disorder, detained youth, longitudinal
Persistent antisocial behavior places a heavy burden on the community, the justice system, and the public health system (Miller, Cohen, & Wiersema, 1996). Adults with antisocial personality disorder (APD) are likely to experience a range of problematic behaviors and outcomes: criminal and violent behavior, substance use, early death, divorce, unemployment, and homelessness (Black, Baumgard, Bell, & Kao, 1996; Hodgins & Cote, 1993; Jainchill, Hawke, & Yagelka, 2000; Robins, Tipp, & Przybeck, 1991; Westermeyer & Thuras, 2005). Considering the high social and financial costs associated with APD, identifying youth at risk for this disorder is critical for prevention (Loeber, Green, & Lahey, 2003; Offord, 2000).
Among many of the factors hypothesized to affect the development of APD are mental disorders in childhood and adolescence. Conduct disorder (CD) in childhood and adolescence is the factor most often associated with the development of APD (Abramowitz, Kosson, & Seidenberg, 2004; Lahey & Loeber, 1997; Moffitt, Caspi, Rutter, & Silva, 2001). Using meta-analytic techniques to combine results of five retrospective and prospective studies, Loeber et al. (2003) revealed that youth with CD are 17 times more likely to develop APD than youth without CD.
The association between CD and APD may not be as straightforward as suggested by prior research. Evidence indicates that the number of symptoms of CD, and not just the diagnosis of CD, increases risk for APD (Robins, 1966). For example, a recent study found that among youth receiving mental health treatment, the odds of developing APD in emerging adulthood increased by 37% with each additional CD symptom for up to 5 symptoms (Lahey, Loeber, Burke, & Applegate, 2005). These findings argue for a continuous rather than a taxonomic model of how accurately CD predicts APD.
Other research suggests that not all symptoms of CD are equally predictive of APD. A hierarchical development model proposes that among youth with CD, only youth with early-onset, persistent, or “advanced” symptoms of CD (e.g., robbery, rape, assault with a weapon) will progress to having APD (Loeber et al., 2003). Furthermore, findings from two studies indicate that the number of covert CD symptoms (e.g., property crimes and status offenses) but not the number of overt CD symptoms (e.g., physical aggression) is associated with increased risk of APD (Lahey et al., 2005; Satterfield & Schell, 1997). Covert symptoms may be a necessary component in the progression from aggressive behavior early in childhood to persistent antisocial behavior in adulthood (Patterson & Yoerger, 1999). In summary, while most research supports the association between CD and APD, the association is complex.
Reliance on CD alone to predict the development of APD may result in a substantial number of false-positive diagnoses (Lahey et al., 2005). Other disruptive behavior disorders, such as oppositional defiant disorder (ODD) and attention-deficit/hyperactivity disorder (ADHD), may predispose youth to developing APD (Fischer, Barkley, Smallish, & Fletcher, 2002; Lynam, 1996; Moffitt, Caspi, Harrington, & Milne, 2002). The hierarchical developmental model (Loeber et al., 2003) proposes that ODD and ADHD increase risk for APD indirectly by increasing risk for early-onset and persistent CD. Lynam (1996) proposed that the comorbidity of ADHD and CD increase risk for severe APD in adulthood beyond what either disorder contributes independently. In a sample of youth in treatment, ADHD was highly comorbid with CD, but ADHD did not predict APD independent of CD (Lahey et al., 2005).
Mental disorders other than disruptive behavioral disorders may also contribute to the development of APD (Loeber et al., 2003). Substance abuse may increase risk for APD because it increases exposure to deviant peers, increases the need to obtain money for substance use, and can impair decision making (Loeber, Burke, & Lahey, 2002; Loeber et al., 2003). Among adolescents attending outpatient mental health clinics, Loeber et al. (2002) found that the association between marijuana use and the development of APD was stronger than the association between CD and the development of APD.
Internalizing disorders have also been proposed to influence the development of APD. Several studies suggest that depression increases risk for developing APD (Bardone, Moffitt, Caspi, & Dickson, 1996; Loeber et al., 2002; Sourander et al., 2005). Symptoms of depression, such as irritability or hopelessness, may lead to increased risk for APD by reducing concern for the consequences of antisocial behavior and fueling interpersonal conflict (Kasen et al., 2001).
Although depressive disorders may increase risk for APD, anxiety disorders among youth may protect against the development of APD (Loeber et al., 2003). The presence of anxiety may inhibit youth from committing or repeating dangerous or risky behaviors. In contrast, lack of anxiety, as manifested by fearlessness and behavior disinhibition, may predispose youth to serious antisocial behavior in adulthood (Frick, Lilienfeld, Ellis, Loney, & Silverthorn, 1999).
It is important to understand the development of APD among youth most at risk, such as those involved in the juvenile justice system. Detained youth have many risk factors for APD, including a high prevalence of CD and other mental disorders. Recent epidemiologic studies estimate that between half to two thirds of juvenile detainees have at least one mental disorder, and more than one third have CD (Teplin, Abram, McClelland, Dulcan, & Mericle, 2002; Wasserman, McReynolds, Lucas, Fisher, & Santos, 2002). Improving our understanding of what predicts the development of APD among detained youth is especially important because more than 95,000 youth are detained in the United States on any given day (Sickmund, Sladky, & Kang, 2005).
It is also important to understand if the association between mental disorders and APD varies by gender and race/ethnicity. African American males are over-represented in the juvenile justice system, and the proportion of females is increasing (Snyder & Sickmund, 2006). Furthermore, the distribution of mental disorders across gender and racial/ethnic groups of detainees (Teplin et al., 2002) differs from that of the general population (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Rushton, Forcier, & Schectman, 2002). Differences in risk factors for APD by gender and race/ethnicity among youth in the justice system may influence the developmental course of APD. For example, the prevalence of mental and substance use disorders is generally higher among non-Hispanic white and female youth than among males, African Americans, and Hispanics, suggesting varying risk for developing APD.
To our knowledge, no prospective study has examined the development of APD among youth involved in the juvenile justice system. Prior studies of youth at high risk for developing APD have focused on youth attending mental health clinics (Fischer et al., 2002; Fombonne, Wostear, Cooper, Harrington, & Rutter, 2001; Harrington, Fudge, Rutter, Pickles, & Hill, 1991; Krueger, 1999; Loeber et al., 2002; Mannuzza, Klein, Bessler, Malloy, & LaPadula, 1998; Myers, Stewart, & Brown, 1998; Rasmussen & Gillberg, 2000; Rey, Singh, Andrews, & Stewart, 1995; Robins, 1966; 1978; Zoccolillo, Pickles, Quinton, & Rutter, 1992). Clinic samples, however, may not generalize to juvenile justice youth because most detained youth, even those with major affective or psychotic disorders, do not receive mental health services (Teplin, Abram, McClelland, Washburn, & Pikus, 2005). Clinic samples also do not represent the racial/ethnic diversity of the juvenile justice system (Sickmund et al., 2005).
The present study examines how well CD and other mental and substance use disorders predict the development of APD among juvenile detainees. This study has a large, stratified random sample of detained youth; has adequate numbers of key demographic subgroups (e.g., females, Hispanics) to allow examination of differences by gender and race/ethnicity; uses standardized diagnostic instruments; and provides assessments during adolescence (mean age = 15.7) and emerging adulthood (mean age = 19.0). Based on prior research and theory, we examine the following 3 hypotheses:
CD and APD. Having CD will be significantly associated with the development of APD. The odds of developing APD will increase as the number of symptoms of CD increase, even after accounting for the contribution of the CD diagnosis. The number of covert, but not overt, symptoms of CD will be significantly associated with the development of APD.
Disruptive Behavioral Disorders Other than CD. Disruptive behavioral disorders other than CD will be significantly associated with APD; however, having CD will mediate these associations. Further, although ADHD will be common among youth with CD, ADHD will not increase risk for APD independent of CD.
Other Mental Disorders. Mental disorders other than disruptive behavioral disorders will be associated with the development of APD. Depressive disorders and substance use disorder will increase the odds of developing APD, whereas anxiety disorders will decrease the odds of developing APD.
Methods
Participants and Sampling
Data are from the Northwestern Juvenile Project, a longitudinal study of 1829 randomly selected youth arrested and detained at the Cook County Juvenile Temporary Detention Center (CCJTDC) in Chicago, IL. The CCJTDC is used for pretrial detention and for offenders sentenced for fewer than 30 days. Consistent with juvenile detainees nationwide (Sickmund et al., 2005), nearly 90% of detainees at CCJTDC were male and most were racial/ethnic minorities (77.9% African Americans, 5.6% non-Hispanic Whites, 16.0% Hispanics, and 0.5% of other racial/ethnic groups).
No single site can represent the entire country due to differences in diversion practices by region; however, a national probability or multi-city sample would be impractical because of the extensive cooperation required from a complicated network of state and county systems. We selected the CCJTDC because: (1) most juveniles detainees nationwide live in or are detained in urban areas; (2) Cook County is racially/ethically diverse; (3) the juvenile justice system in Illinois is typical of most other states (Illinois Criminal Justice Information Authority, 1997); (4) the size of the CCJTDC (daily census of approximately 650 youth) was large enough to ensure an adequate sample size; and (5) the gender, age, and offense distributions in the CCJTDC are similar to those of detained juveniles nationwide (Sickmund et al., 2005).
Baseline data were collected between November 20, 1995, and June 14, 1998. Participants signed either an assent form (if they were <18 years) or a consent form (if they were ≥18 years). The Northwestern University Institutional Review Board, the Centers for Disease Control and Prevention Institutional Review Board, and the US Office of Protection from Research Risks waived parental consent, consistent with federal regulations regarding research with minimal risk. We nevertheless tried to contact parents or guardians to provide them information and offer them an opportunity to decline participation. Despite repeated attempts to contact a parent or guardian, for 43.8% of the participants, none could be found. In lieu of parental consent, youth assent was overseen by an independent participant advocate representing the interests of the participants. Federal regulations allow for a participant advocate if parental consent is not feasible.
The follow-up interview took place a mean (SD) of 3.28 (0.55) years after the baseline interview, at which time the majority of participants had reached emerging adulthood. For the current analyses, we excluded participants younger than 18 years at the follow-up assessment because they were too young to meet criteria for APD. Among the remaining 1243 participants, 5 (0.4%) were not administered the conduct disorder module at baseline, 26 (2.1%) died before their follow-up interview, 8 (0.6%) declined further participation, 68 (5.5%) did not receive the APD module at the follow-up (48 of whom received an abbreviated telephone interview in which the APD module was not administered), and 24 (1.9%) could not be located for their follow-up interview.
To examine the influence of attrition on the generalizability of our findings, we compared the demographic characteristics (gender, race/ethnicity, age) and baseline diagnoses of those participants who were missing data due to attrition to those participants with complete data. No significant differences were found, except for three groups of participants with missing data: (1) participants who could not be located for their follow-up interview were less likely to have had a diagnosis of oppositional defiant disorder at baseline (Fisher’s exact test, p = .04); (2) a greater proportion of non-Hispanic Whites than African Americans or Hispanics did not receive the APD module because they were interviewed by telephone (Fisher’s exact test, p < .01); and (3) a lower proportion of African Americans than non-Hispanic Whites and Hispanics could not be located for the follow-up interview (Fisher’s exact test, p = .04). We adjusted for potential bias due to different rates of attrition by racial/ethnic groups by weighting the statistical analyses by sampling strata (see Statistical Analysis).
The final sample size is 1112 and includes 431 females and 681 males; 605 African Americans, 319 Hispanics, 186 non-Hispanic Whites, and 2 youth who self-identified as a race/ethnicity other than those indicated. At the follow-up interview, 335 youth were aged 18 years, 499 were aged 19 years, and 278 were aged 20 to 25 years. Approximately 90% of adult participants earned annual incomes below the poverty level (median = $1,700; 25th percentile $250, 75th percentile $6,125) at the follow-up interview.
At baseline, face-to-face, structured interviews were conducted in a private area, most within 2 days of intake to the CCJTDC. Follow-up interviews were conducted in the community (70.2%), prisons or jails (29.2%), or psychosocial treatment facilities (0.5%), wherever participants were currently living. Whenever possible, follow-up interviews were face-to-face; when this was not possible, participants were interviewed by telephone (0.1%). We maintained interviewer consistency throughout the study by monitoring scripted interviews with mock participants.
Measures
To determine the diagnosis of CD and other mental disorders at baseline, we used version 2.3 of the Diagnostic Interview Schedule for Children (DISC) (Schwab-Stone et al., 1996), the most recent English and Spanish versions then available. The DISC 2.3 assesses the presence of DSM-III-R disorders in the past 6 months. We include the following disorders: disruptive behavior (CD, ADHD, ODD), depressive (major depression and dysthymia), anxiety (panic, generalized anxiety disorder [GAD], separation anxiety, obsessive-compulsive, and over-anxious), and substance use (alcohol, marijuana, and other drug).
Diagnosing ADHD required special management. ADHD is difficult to assess via self-report with the DISC 2.3 (Jensen et al., 1999), especially among youth ages 9–11 years (Schwab-Stone et al., 1996). Concordance between self-report of ADHD on the DISC 2.3 and clinical symptom ratings is only fair (Kappa = .27; Schwab-Stone et al., 1996). In addition, caretakers are the best reporters of the DSM-III-R requirement for evidence of symptoms of ADHD prior to the age of seven years. Most of our participants could not remember when their ADHD symptoms began. To avoid gross underestimates of ADHD, we present data counting the disorder as present regardless of the reported age at onset, as long as the duration criterion was met.
Specific symptoms of CD were used to develop counts of overt and covert CD symptoms. Overt symptoms of CD included physical cruelty to animals, forced sexual activity, use of a weapon in a fight, initiation of physical fights, stealing with confrontation, and physical cruelty to people. Covert symptoms included stealing without confrontation, running away overnight, lying, fire-setting, truancy, breaking and entering, and destruction of property. Kuder-Richardson’s coefficient of reliability was .59 for the covert symptom count variable and .55 for the overt symptom count variable.
To determine the diagnosis of APD at follow-up, we used the Diagnostic Interview Schedule, Version IV (DIS-IV) (Robins, Cottler, Bucholz, & Compton, 1995), which assesses DSM-IV disorders in the past year. We altered the APD diagnosis to exclude the requirement of evidence of CD prior to age 15 years. This definition of APD, referred to as modified APD (M-APD) avoids tautological predictions (i.e., CD is associated with APD because APD requires the presence of CD).
Both the DISC 2.3 and the DIS-IV are highly structured, contain detailed symptom probes, have acceptable reliability and validity (Robins, Helzer, Ratcliff, & Seyfried, 1982; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000), and require relatively brief training. Table 1 presents descriptive statistics for the variables used in the analyses.
Table 1.
Prevalence and Means of Mental Disorders and Symptom Counts of Youth in Detentiona
| Males (n=681) | Females (n=431) | |||||||
|---|---|---|---|---|---|---|---|---|
| Mental Disorder | N | % | CI | SE | N | % | CI | SE |
| CD | 291 | 36.0 | (30.3 – 41.7) | 2.9 | 170 | 39.1 | (33.8 – 44.4) | 2.7 |
| ≥5 CD symptoms | 145 | 18.1 | (13.6 – 22.7) | 2.3 | 77 | 16.0 | (12.7 – 19.4) | 1.7 |
| ADHD | 120 | 17.1 | (12.5 – 21.7) | 2.3 | 87 | 19.1 | (15.3 – 22.8) | 1.9 |
| Oppositional defiant | 107 | 15.0 | (10.7 – 19.2) | 2.2 | 69 | 14.9 | (11.5 – 18.2) | 1.7 |
| Major depression | 91 | 12.9 | (8.9 – 16.9) | 2.1 | 97 | 24.0 | (18.7 – 29.4) | 2.7 |
| Dysthymia | 76 | 11.7 | (7.8 – 15.7) | 2.0 | 71 | 15.8 | (12.3 – 19.3) | 1.8 |
| Alcohol | 204 | 28.2 | (22.8 – 33.6) | 2.8 | 121 | 28.8 | (23.5 – 34.2) | 2.7 |
| Marijuana | 336 | 44.8 | (38.8 – 50.8) | 3.1 | 184 | 43.1 | (38.3 – 47.9) | 2.4 |
| Other drug | 51 | 2.9 | (1.7 – 4.1) | 0.6 | 33 | 8.4 | (3.5 – 13.2) | 2.5 |
| Generalized anxiety | 44 | 7.5 | (4.3 – 10.8) | 1.7 | 35 | 7.7 | (5.2 – 10.2) | 1.3 |
| Separation anxiety | 87 | 14.2 | (9.9 – 18.5) | 2.2 | 84 | 18.9 | (15.1 – 22.7) | 1.9 |
| Overanxious | 46 | 8.5 | (5.0 – 12.0) | 1.8 | 52 | 11.8 | (8.7 – 14.9) | 1.6 |
| Panic | 3 | 0.2 | (0.0 – 0.4) | 0.1 | 8 | 1.6 | (0.5 – 2.7) | 0.6 |
| Obsessive compulsive | 68 | 8.5 | (5.3 – 11.7) | 1.6 | 45 | 10.3 | (7.4 – 13.2) | 1.5 |
| APDb | 134 | 17.8 | (13.3 – 22.3) | 2.3 | 50 | 10.9 | (8.0 – 13.9) | 1.5 |
| Modified-APDb | 193 | 28.3 | (22.9 – 33.7) | 2.8 | 79 | 17.9 | (14.2 – 21.6) | 1.9 |
| CD Symptom Counts | Mean | Range | CI | SE | Mean | Range | CI | SE |
| Overt Symptoms | 0.8 | (0–6) | (0.6 – 0.9) | 0.1 | 0.6 | (0–4) | (0.5 – 0.7) | 0.1 |
| Covert Symptoms | 1.5 | (0–7) | (1.4 – 1.7) | 0.1 | 1.8 | (0–6) | (1.6 – 2.0) | 0.1 |
| All CD Symptoms | 2.3 | (0–11) | (2.1 – 2.6) | 0.1 | 2.4 | (0–12) | (2.1 – 2.6) | 0.1 |
Data are weighted to reflect the population of the Cook County Juvenile Temporary Detention Center
Assessed at the follow-up interview
Note: CI = 95% confidence interval; SE = standard error; CD = conduct disorder; ADHD = attention-deficit/hyperactivity disorder; APD = antisocial personality disorder
Statistical Analysis
As part of the study design, selected strata were oversampled to obtain data on key subgroups (e.g., Hispanic females). The sample was stratified on the following variables: age (10–13 years or ≥14 years), gender, race/ethnicity (African American, non-Hispanic White, and Hispanic), and legal status (processed as a juvenile or an adult). We used sample weights to estimate descriptive statistics and model parameters that reflect CCJTDC’s population. Taylor series linearization was used to estimate standard errors (Cochran, 1977; Levy & Lemeshow, 1999).
We used logistic regression to examine how mental disorders and demographic characteristics (gender, race/ethnicity) are associated with M-APD. To examine if demographic factors moderate the associations between mental disorders and M-APD, we added interaction terms for demographic variables that had a main effect on M-APD. Finally, we examined if the results differed when we excluded the 185 participants (16.6%) whose follow-up interview occurred more than 3.5 years after the baseline interview.
Results
CD and APD
Prevalence of APD
Three years after the baseline interview, 17.3% of detained youth had developed APD, and 27.6% had developed M-APD. Significantly more males than females developed APD (17.8% vs. 10.9%, odds ratio [OR] = 1.77, 95% confidence interval [CI] = 1.15 –2.71, p = .009) and M-APD (28.3% vs. 17.9%, OR = 1.81, 95% CI = 1.26 – 2.61, p = .001). There were no significant differences in the development of APD or M-APD by race/ethnicity for males or females. Because males were more likely than females to develop M-APD, we included gender as a covariate in regression analyses of mental disorders and M-APD. We report ORs adjusted for gender in the analyses that follow.
Association of CD and M-APD
Among those with M-APD, 77.5% met criteria for CD at least once in their lifetime by the time of the follow-up interview. Among youth with CD at baseline, 25.2% of males and 18.5% of females developed APD, and 34.9% of males and 26.2% of females developed M-APD. Having CD at baseline significantly increased the odds of developing M-APD at the follow-up interview (adjusted OR [AOR]= 1.68, 95% CI = 1.01 – 2.81, p = .046).
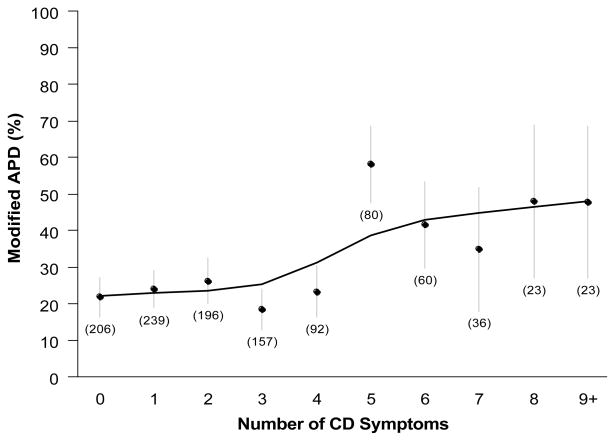
Figure 1 presents the weighted proportions and associated standard errors for the fraction of participants who developed M-APD according to the number of CD symptoms. As hypothesized, there was a significant linear association between the number of CD symptoms and having M-APD (AOR = 1.17, 95% CI = 1.05 – 1.31, p = .005). Figure 1, however, suggests a discontinuity in the linear relationship. The proportion of participants who developed M-APD increased in participants who had 5 or more CD symptoms.
Figure 1.
The percentage of detained youth that met criteria for modified antisocial personality disorder (APD; excludes the criteria for conduct disorder [CD] symptoms prior to age 15 years) at their 3-year follow-up interview by the number of self-reported symptoms of CD at the baseline interview. The numbers in parenthesis represent unweighted numbers of subjects with the corresponding symptom count. Bars represent one standard error above and one standard error below point estimates.
Based on Figure 1, we reasoned that the linear association may mask a threshold effect in which additional symptoms prior to or beyond 5 CD symptoms would not change the odds of developing M-APD. Post hoc analysis also suggested a threshold effect: participants with 5 or more CD symptoms were significantly more likely to develop M-APD than participants with fewer than 5 symptoms (AOR = 3.06, 95% CI = 1.68 – 5.57, p < .001). To examine the location of the threshold at 5 or more symptoms, we estimated a model predicting M-APD with indicator (dummy) variables for exactly 1 CD symptom, exactly 2 CD symptoms, etc., through exactly 5 CD symptoms, as well as an indicator for 6 or more CD symptoms. Only the coefficients for exactly 5 CD symptoms (AOR = 5.03, 95% CI = 1.74 – 14.53, p = 0.003) and 6 or more symptoms (AOR = 2.60, 95% CI = 1.04 – 6.50, p = 0.042) were statistically significant.
It is possible that there is a linear relationship as well as a threshold effect (e.g. the odds of developing M-APD may significantly increase with a jump from 4 to 5 symptoms in addition to the odds increasing with every CD symptom). To examine this possibility, we estimated a model with an indicator for 5 or more CD symptoms and with the number of CD symptoms as predictors. The linear term was not significant (AOR = 0.97, 95% CI = 0.80 – 1.18, p = 0.77) when 5 or more CD symptoms was included (AOR = 3.50, 95% CI = 1.22 – 10.06, p = 0.02) in the model.
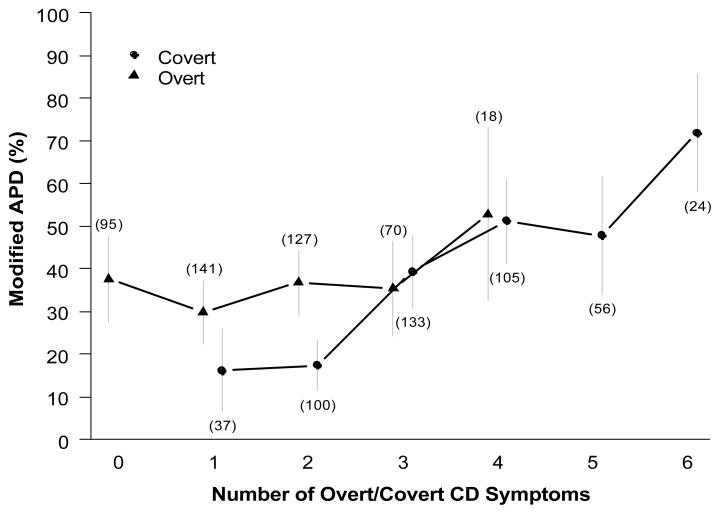
Association of Overt and Covert CD Symptoms and M-APD
We next examined the associations between the number of overt and covert CD symptoms and M-APD. As illustrated in Figure 2, the number of covert symptoms (AOR = 1.38, 95% CI = 1.13 – 1.69, p = .002), but not overt symptoms, increased the odds of developing M-APD. Based on our preceding findings, we conducted a post hoc analysis of the association between the number of covert symptoms and M-APD, adjusting for 5 or more symptoms of CD. This analysis was conducted to determine if the odds of developing M-APD increased with 5 or more CD symptoms in addition to the odds increasing with every covert symptom. The number of covert symptoms was not significantly associated with M-APD (AOR = 1.14, 95% CI = 0.89 – 1.46, p = .31) when 5 or more CD symptoms was included in the model (AOR = 4.59, 95% CI = 1.63 – 12.94, p = .004). Following the procedures of Lahey et al (2005), we repeated these analyses only among those with CD and we found the same results.
Figure 2.
The percentage of detained youth that met criteria for modified antisocial personality disorder (APD; excludes the criteria for conduct disorder [CD] symptoms prior to age 15 years) at their 3-year follow-up interview by the number of self-reported overt and covert symptoms of CD at the baseline interview. The numbers in parenthesis represent unweighted numbers of subjects with the corresponding symptom count.
Gender did not significantly moderate the associations between M-APD and CD, between M-APD and number of CD symptoms, or between M-APD and 5 or more CD symptoms.
Disruptive Behavioral Disorders Other than CD
ADHD (AOR = 2.35, 95% CI = 1.11 – 4.97, p = .03), but not ODD significantly increased the odds of developing M-APD. Although ADHD was significantly associated (concurrently) with CD (AOR = 8.72, 95% CI = 4.34 – 17.54, p < .001), CD did not account for the association between ADHD and M-APD when CD was included in the model. Post hoc analyses, however, showed that 5 or more symptoms of CD, which was also concurrently associated with ADHD (AOR = 5.93, 95% CI = 3.07 – 11.46, p < .001), mediated the association between ADHD and M-APD (Z[Sobel] = 2.18, p = .03).
Among youth with CD, 36.7% had comorbid ADHD at baseline compared with 6.2% of youth without CD. Although ADHD was significantly associated with CD, ADHD did not increase the odds of developing M-APD. Further, neither the interaction of ADHD and CD, nor the interaction of ADHD and 5 or more CD symptoms significantly increased the odds of developing M-APD after accounting for either CD or 5 or more CD symptoms.
Gender did not moderate the associations of ADHD and ODD with M-APD.
Other Mental Disorders
We examined depressive, anxiety, and substance use disorders as independent variables in a logistic regression model with M-APD as the outcome variable. Dysthymia (AOR = 3.09, 95% CI = 1.24 – 7.72, p = .02) and alcohol use disorder (AOR = 2.07, 95% CI = 1.12 – 3.81, p = .02) significantly increased the odds of developing APD, whereas GAD significantly decreased the odds of developing APD (AOR = 0.20, 95% CI = 0.05 – 0.77, p = .02). Adding CD to the model did not alter the significance or direction of the existing findings; however, CD was not significantly associated with M-APD. In contrast, a post hoc analysis found that 5 or more symptoms of CD was significantly associated with M-APD (AOR = 2.92, 95% CI = 1.41 – 6.04, p = .004); dysthymia (AOR = 3.28, 95% CI = 1.35 – 7.98, p = .009), GAD (AOR = 0.23, 95% CI = 0.55 – 0.96, p = .044), and alcohol use disorder (AOR = 1.88, 95% CI = 1.00 – 3.53, p = .048) remained significant in the model.
Gender moderated the associations of dysthymia and GAD with M-APD. For males, dysthymia significantly increased the odds (OR = 3.56, 95% CI = 1.54 – 8.24, p = 0.003) and GAD significantly decreased the odds of developing M-APD (OR = 0.15, 95% CI = 0.04 – 0.52, p = 0.003). In contrast, neither dysthymia (OR = 1.13, 95% CI = 0.58 – 2.20, p = 0.715) nor GAD (OR = 1.27, 95% CI = 0.53 – 3.03, p = 0.594) significantly changed the odds of developing M-APD for females.
Sensitivity, Specificity, and Positive and Negative Predictive Values
To examine how well mental disorders and CD symptoms at baseline predicted the development of M-APD at follow-up, we computed weighted estimates of the following: (1) sensitivity or the true-positive fraction (i.e., among youth that developed M-APD, the proportion that had a specific predictor at baseline); (2) specificity or 1 – the false-positive fraction (i.e., among youth who did not develop M-APD, the proportion of youth that did not have a specific predictor at baseline); (3) positive predictive value (i.e., among youth with a specific predictor at baseline, the proportion that developed M-APD); and (4) negative predictive value (i.e., among youth without a specific predictor at baseline, the proportion that did not develop M-APD) (Gordis, 2004). These tests were originally developed to evaluate the validity of new or alternative diagnostic tests (Gordis, 2004; Pepe, 2003); however, they are useful in evaluating the value of mental disorders in predicting the development of APD.
The findings from these analyses, conducted separately for females and males, are presented in Table 2. Because positive and negative predictive values depend on the base rates of the predictor and the association between the predictor and M-APD, Table 2 also lists the prevalence of the predictors at baseline. As shown in Table 2, none of the predictors proved to be sensitive at identifying males or females who developed M-APD. Among all the variables, CD was the most sensitive predictor (i.e., among those with M-APD, 57% of females and 44% of males had CD at baseline). Yet, reliance on these markers would fail to identify approximately half of the participants who developed M-APD. Moreover, CD showed the lowest specificity, suggesting that approximately one third of participants who had CD would be incorrectly categorized as at risk for developing APD. Among males, the comorbidity of 5 or more symptoms of CD and dysthymia had the highest positive predictive value (i.e., 61% of males with 5 or more symptoms of CD and dysthymia at baseline developed M-APD); however, only 15% of males who developed M-APD had 5 or more symptoms of CD and dysthymia at baseline. Among females, all of the predictors had low positive predictive values.
Table 2.
Classification of Modified APD by Mental Disorders of Youth in Detention
| Predictors | Base Rate of Predictors | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | |
| Conduct disorder | 39% | 36% | 0.57 | 0.44 | 0.65 | 0.67 | 0.26 | 0.35 | 0.87 | 0.75 |
| 5 or more CD symptoms | 16% | 18% | 0.25 | 0.32 | 0.86 | 0.87 | 0.28 | 0.49 | 0.84 | 0.76 |
| Dysthymia | 16% | 12% | 0.17 | 0.20 | 0.85 | 0.91 | 0.20 | 0.48 | 0.82 | 0.74 |
| Generalized anxiety disorder | 8% | 8% | 0.09 | 0.03 | 0.93 | 0.91 | 0.21 | 0.13 | 0.83 | 0.71 |
| Alcohol use disorder | 29% | 28% | 0.30 | 0.41 | 0.71 | 0.77 | 0.19 | 0.40 | 0.82 | 0.77 |
| 5 or more CD symptoms & dysthymia | 7% | 7% | 0.11 | 0.15 | 0.93 | 0.96 | 0.25 | 0.61 | 0.83 | 0.74 |
Note: APD = antisocial personality disorder; CD = conduct disorder
For all of the predictors, the negative predictive values were between 71% and 77% for males and between 82% and 87% for females, in large part because 72% of males and 82% of females did not develop M-APD, and none of the mental disorders are adequate classifiers (Pepe, 2003). In other words, the probability of not developing APD is similar regardless of diagnosis.
Analyses of the Follow-up Interval
When we repeated analyses without the 185 participants whose follow-up interview occurred 3.5 years after the baseline interview, the direction and statistical significance of nearly all the findings remained unchanged. The exceptions were as follows: (1) The gender test of APD was no longer significant, although the AOR was similar to the full sample (AOR = 1.58, 95% CI = 0.98 – 2.55, p = .06); (2) in the “Other Mental Disorders Model,” the diagnosis of dysthymia was no longer significantly associated with M-APD (AOR = 1.92, 95% CI = 0.69 – 5.38, p = .21); however, major depressive disorder was significant (AOR = 3.04, 95% CI = 1.08 – 8.56, p = .04); and (3) in the “Other Mental Disorders Model,” the diagnosis of dysthymia was not significantly associated with M-APD when 5 or more symptoms of CD was added to the model (AOR = 2.65, 95% CI = 0.80 – 6.92, p = .12), although the direction of the association did not change.
Discussion
Detained adolescents are at high risk for developing APD as they enter emerging adulthood. Nearly one-fifth developed APD, rates substantially higher than those in the general population (1%–4%) (Grant et al., 2004; Lyons & Jerskey, 2002; Robins et al., 1991). Detained youth, similar to youth receiving mental health treatment (Loeber et al., 2002; Robins, 1966), demonstrate continuity of behavioral disorder from CD in adolescence to APD in emerging adulthood. CD was significantly associated with M-APD, and more than three quarters of the participants who developed M-APD reported a history of CD prior to age 15.
The hierarchical development model of APD proposes that youth with the most advanced and diversified symptoms of CD (e.g., rape, assault with a weapon, robbery) are at the greatest risk for developing APD (Loeber et al., 2003). Findings from this and others studies (Lahey et al., 2005; Satterfield & Schell, 1997), however, suggest the accumulation of covert symptoms increase the odds of developing APD. These findings are consistent with social interaction and coercive theories of delinquency, which propose that growth in covert antisocial behavior may mediate the progression from early overt antisocial behaviors to chronic adult antisocial behavior (Patterson & Yoerger, 1999). Early overt antisocial behavior may lead to increased association with deviant peers and subsequent training and reinforcement in covert antisocial behavior (Patterson & Yoerger, 1999). In addition, as children age into early adolescence, overt antisocial behavior is increasingly unacceptable to adults and peers, and either extinguishes or becomes more covert (Snyder, Reid, & Patterson, 2003).
Post-hoc analyses found that the odds of developing M-APD significantly increased among youth with 5 or more symptoms of CD, regardless of the type of symptom. Taken together, these findings suggest that among detained youth, growth in covert CD symptoms may increase risk for APD, but only up to a specific number of symptoms. Once detained youth reach this threshold, the type of CD symptom may matter less than the sheer number of symptoms.
Despite the significant associations between CD or number of CD symptoms and M-APD, the utility of CD or number of CD symptoms for identifying which detained youth will develop M-APD is limited. Although Lahey et al. (2005) found that 65% of low-income, clinic-referred youth with CD developed M-APD by age 18 or 19 years, only one third of detained youth with CD developed M-APD. Similar to general population youth, most detained youth appear to be characterized by Moffitt’s adolescent-limited antisocial pathway (Moffitt, 1993), which proposes that youth engage in antisocial behavior for social and affiliative reasons during adolescence and desist from antisocial behavior in emerging adulthood. Our findings should not be interpreted, however, as suggesting that most detained youth desist from unlawful behavior. Even in the general population, youth characterized by adolescent limited antisocial behavior may continue to engage in unlawful behavior into young adulthood (Moffitt et al., 2002). Our findings suggest instead that only a subset of detained youth with CD develop personality characteristics that facilitates the persistent violation of societal rules and norms (Loeber et al., 2003).
In contrast to prior findings (Lahey et al., 2005), the diagnosis of CD did not account for the association between ADHD and M-APD. This finding may reflect problems with the self-report measurement of ADHD in this study; however, it also may reflect how poorly CD predicts M-APD among juvenile detainees. Indeed, post hoc analyses showed that 5 or more symptoms of CD, a more robust predictor of M-APD in this sample, accounted for the association between ADHD and M-APD. This finding provides partial support for the theory that ADHD indirectly contributes to the development of APD through the development of CD symptoms in adolescence (Lahey et al., 2005; Loeber et al., 2003).
Comorbid ADHD and CD did not significantly increase the odds of developing M-APD after accounting for CD. Lahey et al. (2005) explained similar findings in a sample of youth in treatment by noting that nearly all youth with CD had ADHD; however, fewer than half of detained youth with CD had comorbid ADHD. In contrast to Lynam (1996), these findings indicate that ADHD fails to contribute to the development of APD among detained youth.
The hierarchical developmental model proposes that a subset of children demonstrate continuity of antisocial behavior from ODD in childhood, to CD in adolescence, and to APD in young adulthood. The finding that ODD was not significantly associated with APD, even after excluding the contribution of CD, was unexpected, but not necessarily contradictory to the hierarchical developmental model. In contrast to prior research, ODD in this sample was assessed during adolescence rather than in childhood (Lahey et al., 2005). ODD in childhood may contribute to later antisocial behavior in detained youth; however, these findings suggest covert antisocial symptoms in adolescence appear to contribute far more to the persistence of antisocial behavior than angry, aggressive, or oppositional behavior in adolescence (Loeber, Green, Lahey, Frick, & McBurnett, 2000; Snyder et al., 2003).
Heterotypic continuity of disorder was also found across categories of mental disorder. Even after accounting for CD symptoms or diagnosis, dysthymia, alcohol use disorder, and GAD were significantly associated with M-APD. Findings suggest that the relationship between these mental disorders and M-APD is complex; depression and alcohol use disorder increase the risk of developing M-APD, while anxiety decreases this risk.
Depressive symptoms in adolescence may manifest externally through antisocial behavior in emerging adulthood (Puig-Antich0, 1982). Chronic symptoms of hopelessness, irritability, low self-esteem, and pessimism may contribute to a pattern of argumentativeness and interpersonal conflict (Kasen et al., 2001). Impaired prosocial decision-making and coping skills associated with chronic depressive symptoms may further increase the risk for engaging in irresponsible behavior (Kasen et al., 2001). In contrast to the greater level of impairment associated with acute depression, youth with more chronic depression may continue to associate with delinquent peers. They may be more willing than youth without depression to take risks and engage in self-destructive or reckless behavior than their peers, similar to the phenomenon of victim-precipitated suicide, or “suicide-by-cop” (Lindsay & Lester, 2004).
In contrast to depression, anxiety disorders may protect against the development of APD by increasing fearfulness and behavioral inhibition (Frick et al., 1999; Gray, 1982). Although these traits were not examined in this study, the excessive worrying associated with GAD is conceptually inconsistent with the fearlessness and behavioral disinhibition found among the most severely antisocial adolescents and adults (Frick et al., 1999). Anxiety may also increase social isolation and thereby decrease deviant peer association and opportunities for engagement in antisocial behavior (Farrington, Gallagher, Morley, St. Ledger, & West, 1988; Moffitt et al., 2002).
Alcohol use disorder was the only substance use disorder to significantly increase the odds of developing M-APD among detained youth. Loeber et al. (2002) found an association between marijuana use – but not alcohol use – and APD in their sample of youth receiving mental health treatment. In contrast to youth receiving treatment, marijuana use and disorder may not represent an aberrant behavior among juvenile detainees; nearly all juvenile detainees have used marijuana at least once, more then three-quarters currently use marijuana (McClelland, Teplin, & Abram, 2004), and nearly half have a marijuana use disorder (Teplin et al., 2002). In contrast, alcohol use disorder is half as common as marijuana use disorder among juvenile detainees (Teplin et al., 2002), and alcohol intoxication may increase volatility and impulsivity.
Significantly more males developed APD than females, as found in prior studies (Fazel & Danesh, 2002; Kim-Cohen et al., 2003; Lyons & Jerskey, 2002). Gender also moderated some findings; dysthymia and GAD were significantly associated with APD for males but not females, and positive predictive values were substantially lower for females than males. Although the lower prevalence of APD among females may partially account for the weaker prediction of APD by mental disorders, unobserved factors are likely more predictive of APD for females. These findings suggest that future research consider a female-specific pathway in understanding the development of APD (Silverthorn & Frick, 1999).
The lack of racial/ethnic differences in the development of APD is consistent with findings among youth receiving mental health treatment. Although Lahey et al., (2005) found African Americans were more likely to develop APD than non-Hispanic Whites, this difference was accounted for by socioeconomic status (Lahey et al., 2005). Most of our participants, regardless of race/ethnicity, were poor; approximately 10% earned annual incomes above the poverty level. A greater number of non-Hispanic Whites had risk factors for APD at baseline; however, they did not have an increased risk for APD at follow-up. Further research is necessary to understand the mediators of racial/ethnic differences and to specifically understand why greater risk for APD in adolescence among non-Hispanic whites does not result in a greater likelihood of developing APD in emerging adulthood.
It is important to consider these findings in the context of the limitations of this study. Our findings may apply only to youth from large urban areas who are detained. We examined youth only twice, three years apart, limiting the detection of mental disorders and APD. Many youth with CD experience brief periods of subthreshold symptoms and may not meet full criteria for the disorder at a given assessment (Lahey et al., 1995). Consequently, we may have underestimated the true continuity of antisocial behavior. Alternatively, we may have overestimated the prevalence of APD because our assessment of APD occurred during an age at which APD diagnoses in the community are the most prevalent (Robins et al., 1991).
This study is subject to the limitations associated with our use of the self-report versions of the DISC 2.3 and DIS-IV; unfortunately, obtaining collateral informants for most detained youth was not feasible (Teplin et al., 2002). Because reliance on self-report is especially problematic for ADHD (Jensen et al., 1999), our findings on ADHD must be considered preliminary at best. Assessing disorders in a correctional facility may alter the validity or reliability of the DISC 2.3 or DIS-IV. This study also did not examine other variables that may be important markers of APD, such as non-diagnostic psychosocial factors (Farrington, 2000), or callous/unemotional or narcissistic traits (Frick et al., 1999; Loeber et al., 2002). The diagnosis of APD also is not synonymous with engagement in illegal behavior or other outcomes. Finally, the apparent association of 5 or more symptoms of CD with M-APD found in data-derived, post hoc analyses may be specific to this sample and needs to be confirmed by other studies.
Despite the limitations, the findings have clinical implications for the assessment and treatment of antisocial behavior among detained youth and for future research. The prevalence of APD in this population underscores the need for early intervention for youth at high risk for persistent antisocial behavior. Clinicians, researchers, and policy makers must collaborate to identify promising strategies to reduce the likelihood that detained youth will develop APD. Programs to prevent the initial onset of conduct problems are key to preventing persistent antisocial behavior (Loeber et al., 2002); however, it is also important to alter the course of antisocial behavior among those youth already displaying conduct problems. Intervention studies need to examine if the symptoms of mental disorder, such as anxiety, depression, or alcohol use, are useful targets for prevention or intervention with detained youth.
Prevention and intervention programs targeted at the youth most at risk for developing APD make the best use of limited community and correctional resources; however, this requires accurate identification of youth at risk for APD. Unfortunately, while CD may adequately predict APD among youth in the general population (Lewinsohn, Rohde, & Farrington, 2000) and treatment samples (Lahey et al., 2005), findings from this study suggest that CD is a poor screener for identifying risk for APD among detained youth. Furthermore, the specificity of CD as a predictor, even in the general population, is not clear; a recent study found early conduct problems preceded nearly every mental disorder in adulthood (Kim-Cohen et al., 2003).
Exploratory findings suggest that the predictive accuracy of individual prognoses may be improved by examining multiple problem areas (e.g., dysthymia comorbid with 5 or more symptoms of CD). Reliance on combinations of disorders with a low prevalence in the population, however, will fail to identify the majority of detained youth who eventually develop APD. A similar problem arises when specific types of antisocial behavior are used for screening, such as psychopathy. Screeners for psychopathy may only identify a subset of youth at risk for APD, such as those at risk for future violent behavior (Gretton, Hare, & Catchpole, 2004). Furthermore, the use of psychopathy measures as a clinical tool remains controversial (Seagrave & Grisso, 2002). Better screening measures are needed to identify youth at risk for developing APD among youth already identified as delinquent by the juvenile justice system.
Future studies need to disentangle the pathways and mechanisms by which mental disorders and other psychosocial variables (e.g., callous/unemotional traits, parenting practices, peer influences) contribute to the development of APD among detained youth. Mental disorders may not directly influence the development of APD; instead, the associations may be due to correlations with underlying factors (McGue & Iacono, 2005). For example, longitudinal studies have found a high degree of concurrent and prospective comorbidity among CD, depression, and anxiety from childhood to adolescence (Lahey, Loeber, Burke, Rathouz, & McBurnett, 2002; Salekin, Leistico, Neumann, DiCicco, & Duros, 2004), suggesting the possibility of underlying psychological processes, such as negative emotionality (Lahey et al., 2002), or an interaction of neurobehavioral processes (Depue & Lenzenweger, 2006).
It is unlikely that future research will be able to identify mental or other psychosocial factors that will prove to be adequate predictors of APD for all detained youth. Because of the heterogeneity of detained youth and adults with APD (Loeber et al., 2003), aggregated analyses likely obfuscate factors that may predict the development of APD in specific subgroups. Consequently, future studies should assess if and how the development of APD varies for specific subgroups of antisocial youth. Longitudinal studies should take advantage of analytic techniques that examine heterogeneity within samples and identify predictive factors that are specific to developmental trajectories of antisocial behavior.
Acknowledgments
This work was supported by National Institute of Mental Health grants R01MH54197 and R01MH59463 (Division of Services & Intervention Research and Center for Mental Health Research on AIDS) and grants 1999-JE-FX-1001 and 2005-JL-FX-0288 from the Office of Juvenile Justice and Delinquency Prevention. Major funding was also provided by the National Institute on Drug Abuse, the Substance Abuse and Mental Health Services Administration (Center for Mental Health Services, Center for Substance Abuse Prevention, Center for Substance Abuse Treatment), the NIH Center on Minority Health and Health Disparities, the Centers for Disease Control and Prevention (National Center on Injury Prevention & Control and National Center for HIV, STD & TB Prevention), the National Institute on Alcohol Abuse and Alcoholism, the NIH Office of Research on Women’s Health, the NIH Office on Rare Diseases, Department of Labor, The William T. Grant Foundation, and The Robert Wood Johnson Foundation. Additional funds were provided by The John D. and Catherine T. MacArthur Foundation, The Open Society Institute, and The Chicago Community Trust. We thank all our agencies for their collaborative spirit and steadfast support.
This study could not have been accomplished without the advice of Ann Hohmann, Ph.D., Kimberly Hoagwood, Ph.D., Heather Ringeisen, Ph.D., and Eugene Griffin, Ph.D. Grayson Norquist, M.D., and Delores Parron, Ph.D., provided support and encouragement. Celia Fisher, Ph.D., guided our human subject procedures. We thank all project staff, especially Amy Mericle, Ph.D., for instrumentation development and project leadership and Lynda Carey, M.A, for her superb data management. We also greatly appreciate the cooperation of everyone working in the Cook County and State of Illinois systems. Without their cooperation, this study would not have been possible. We thank the anonymous reviewers for their many helpful comments. Finally, we thank the participants for their time and willingness to participate and our field interviewers for their commitment to excellence.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/ccp.
References
- Abramowitz CS, Kosson DS, Seidenberg M. The relationship between childhood attention deficit hyperactivity disorder and conduct problems and adult psychopathy in male inmates. Personality & Individual Differences. 2004;36:1031–1047. [Google Scholar]
- Bardone AM, Moffitt T, Caspi A, Dickson N. Adult mental health and social outcomes of adolescent girls with depression and conduct disorder. Development & Psychopathology. 1996;8:811–829. [Google Scholar]
- Black DW, Baumgard CH, Bell SE, Kao C. Death rates in 71 men with antisocial personality disorder: a comparison with general population mortality. Psychosomatics: Journal of Consultation Liaison Psychiatry. 1996;37:131–136. doi: 10.1016/S0033-3182(96)71579-7. [DOI] [PubMed] [Google Scholar]
- Cochran WG. Sampling Techniques. 3. New York, NY: Wiley; 1977. [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Depue RA, Lenzenweger MF. Toward a developmental psychopathology of personality disturbance: a neurobehavioral dimensional model. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology: Developmental Neuroscience. 2. Vol. 2. Hoboken, NJ: John Wiley & Sons, Inc; 2006. pp. 762–796. [Google Scholar]
- Farrington DP. Psychosocial predictors of adult antisocial personality and adult convictions. Behavioral Sciences & the Law. 2000;18:605–622. doi: 10.1002/1099-0798(200010)18:5<605::aid-bsl406>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Farrington DP, Gallagher B, Morley L, St Ledger RJ, West DJ. Are there any successful men from criminogenic backgrounds? Psychiatry: Journal for the Study of Interpersonal Processes. 1988;51:116–130. [PubMed] [Google Scholar]
- Fazel S, Danesh J. Serious mental disorder in 23,000 prisoners: a systematic review of 62 surveys. Lancet. 2002;359:545–550. doi: 10.1016/S0140-6736(02)07740-1. [DOI] [PubMed] [Google Scholar]
- Fischer M, Barkley RA, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. Journal of Abnormal Child Psychology. 2002;30:463–475. doi: 10.1023/a:1019864813776. [DOI] [PubMed] [Google Scholar]
- Fombonne E, Wostear G, Cooper V, Harrington R, Rutter M. The Maudsley long-term follow-up of child and adolescent depression: 1. psychiatric outcomes in adulthood. British Journal of Psychiatry. 2001;179:210–217. doi: 10.1192/bjp.179.3.210. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Lilienfeld SO, Ellis M, Loney B, Silverthorn P. The association between anxiety and psychopathy dimensions in children. Journal of Abnormal Child Psychology. 1999;27:383–392. doi: 10.1023/a:1021928018403. [DOI] [PubMed] [Google Scholar]
- Gordis L. Epidemiology. 3. Philadelphia, PA: WB Saunders; 2004. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Gray JA. The Neuropsychology of Anxiety. New York, NY: Oxford University Press; 1982. [Google Scholar]
- Gretton HM, Hare RD, Catchpole REH. Psychopathy and offending from adolescence to adulthood: a 10-year follow-up. Journal of Consulting and Clinical Psychology. 2004;72:636–645. doi: 10.1037/0022-006X.72.4.636. [DOI] [PubMed] [Google Scholar]
- Harrington R, Fudge H, Rutter M, Pickles A, Hill J. Adult outcomes of childhood and adolescent depression: II. links with antisocial disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1991;30:434–439. doi: 10.1097/00004583-199105000-00013. [DOI] [PubMed] [Google Scholar]
- Hodgins S, Cote G. The criminality of mentally disordered offenders. Criminal Justice & Behavior. 1993;20:115–129. [Google Scholar]
- Illinois Criminal Justice Information Authority. Trends and Issues 1997. Chicago: Illinois Criminal Justice Information Authority; 1997. [Google Scholar]
- Jainchill N, Hawke J, Yagelka J. Gender, psychopathology, and patterns of homelessness among clients in shelter-based TCs. American Journal of Drug & Alcohol Abuse. 2000;26:553–567. doi: 10.1081/ada-100101895. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, et al. Parent and child contributions to diagnosis of mental disorder: are both informants always necessary? Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- Kasen S, Cohen P, Skodol AE, Johnson JG, Smailes E, Brook JS. Childhood depression and adult personality disorder: alternative pathways of continuity. Archives of General Psychiatry. 2001;58:231–236. doi: 10.1001/archpsyc.58.3.231. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Krueger RF. Personality traits in late adolescence predict mental disorders in early adulthood: a prospective-epidemiological study. Journal of Personality. 1999;67:39–65. doi: 10.1111/1467-6494.00047. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R. Attention-deficit/hyperactivity disorder, oppositional defiant disorder, conduct disorder, and adult antisocial behavior: a life span perspective. In: Stoff DM, Breiling J, Maser JD, editors. Handbook of Antisocial Behavior. New York, NY: John Wiley & Sons, Inc; 1997. pp. 51–59. [Google Scholar]
- Lahey BB, Loeber R, Burke J, Rathouz PJ, McBurnett K. Waxing and waning in concert: dynamic comorbidity of conduct disorder with other disruptive and emotional problems over 17 years among clinic-referred boys. Journal of Abnormal Psychology. 2002;111:556–567. doi: 10.1037//0021-843x.111.4.556. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Burke JD, Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. Journal of Consulting and Clinical Psychology. 2005;73:389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Loeber R, Hart EL, Frick PJ, Applegate B, Zhang Q, et al. Four-year longitudinal study of conduct disorder in boys: patterns and predictors of persistence. Journal of Abnormal Psychology. 1995;104:83–93. doi: 10.1037/0021-843X.104.1.83. [DOI] [PubMed] [Google Scholar]
- Levy PS, Lemeshow S. Sampling of Populations: Methods and Applications. 3. New York, NY: John Wiley & Sons, Inc; 1999. [Google Scholar]
- Lewinsohn PM, Rohde P, Farrington DP. The OADP-CDS: a brief screener for adolescent conduct disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:888–895. doi: 10.1097/00004583-200007000-00018. [DOI] [PubMed] [Google Scholar]
- Lindsay M, Lester D. Suicide-by-Cop: Committing Suicide by Provoking Police to Shoot You. Amityville, NY: Baywood Publishing; 2004. [Google Scholar]
- Loeber R, Burke JD, Lahey BB. What are adolescent antecedents to antisocial personality disorder? Criminal Behaviour & Mental Health. 2002;12:24–36. doi: 10.1002/cbm.484. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB. Risk factors for adult antisocial personality. In: Farrington DP, Coid JW, editors. Early Prevention of Adult Antisocial Behaviour. Cambridge, England: Cambridge University Press; 2003. pp. 79–108. [Google Scholar]
- Loeber R, Green SM, Lahey BB, Frick PJ, McBurnett K. Findings on disruptive behavior disorders from the first decade of the Developmental Trends Study. Clinical Child & Family Psychology Review. 2000;3:37–60. doi: 10.1023/a:1009567419190. [DOI] [PubMed] [Google Scholar]
- Lynam DR. Early identification of chronic offenders: who is the fledgling psychopath? Psychological Bulletin. 1996;120:209–234. doi: 10.1037/0033-2909.120.2.209. [DOI] [PubMed] [Google Scholar]
- Lyons MJ, Jerskey BA. Personality disorders: epidemiological findings, methods, and concepts. In: Tsuang MT, Tohen M, editors. Textbook in Psychiatric Epidemiology. 2. New York, NY: Wiley-Liss; 2002. pp. 563–599. [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. American Journal of Psychiatry. 1998;155:493–498. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- McClelland GM, Teplin LA, Abram KM. Detection and Prevalence of Substance Use Among Juvenile Detainees. Washington, DC: Office of Juvenile Justice and Delinquency Prevention; 2004. No. NCJ 203934. [Google Scholar]
- McGue M, Iacono WG. The association of early adolescent problem behavior with adult psychopathology. American Journal of Psychiatry. 2005;162:1118–1124. doi: 10.1176/appi.ajp.162.6.1118. [DOI] [PubMed] [Google Scholar]
- Miller TR, Cohen MA, Wiersema B. Victim costs and consequences: a new look. Washington, DC: National Institute of Justice, US Department of Justice; 1996. No. NCJ 155282. [Google Scholar]
- Moffitt TE. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Development & Psychopathology. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva PA. Sex Differences in Antisocial Behaviour: Conduct Disorder, Delinquency, and Violence in the Dunedin Longitudinal Study. Cambridge, England: Cambridge University Press; 2001. [Google Scholar]
- Myers MG, Stewart DG, Brown SA. Progression from conduct disorder to antisocial personality disorder following treatment for adolescent substance abuse. American Journal of Psychiatry. 1998;155:479–485. doi: 10.1176/ajp.155.4.479. [DOI] [PubMed] [Google Scholar]
- Offord DR. Prevention of antisocial personality disorder. In: Rapoport JL, editor. Childhood Onset of “Adult” Psychopathology: Clinical and Research Advances. Washington, DC: American Psychiatric Publishing, Inc; 2000. pp. 379–398. [Google Scholar]
- Patterson GR, Yoerger K. Intraindividual growth in covert antisocial behaviour: a necessary precursor to chronic juvenile and adult arrests? Criminal Behaviour and Mental Health. 1999;9:24–38. [Google Scholar]
- Pepe MS. The Statistical Evaluation of Medical Tests for Classification and Prediction. Oxford, England: Oxford University Press; 2003. [Google Scholar]
- Puig-Antich J. Major depression and conduct disorder in prepuberty. Journal of the American Academy of Child Psychiatry. 1982;21:118–128. doi: 10.1016/s0002-7138(09)60910-9. [DOI] [PubMed] [Google Scholar]
- Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:1424–1431. doi: 10.1097/00004583-200011000-00017. [DOI] [PubMed] [Google Scholar]
- Rey JM, Singh M, Andrews G, Stewart GW. Continuities between psychiatric disorders in adolescents and personality disorders in young adults. American Journal of Psychiatry. 1995;152:895–900. doi: 10.1176/ajp.152.6.895. [DOI] [PubMed] [Google Scholar]
- Robins LN. Deviant Children Grown Up: A Sociological and Psychiatric Study of Sociopathic Personality. Baltimore, MD: Williams & Wilkins; 1966. [Google Scholar]
- Robins LN. Sturdy childhood predictors of adult antisocial behaviour: replications from longitudinal studies. Psychological Medicine. 1978;8:611–622. doi: 10.1017/s0033291700018821. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler LB, Bucholz K, Compton W. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University; 1995. [Google Scholar]
- Robins LN, Helzer JE, Ratcliff KS, Seyfried W. Validity of the Diagnostic Interview Schedule, Version II: DSM-III diagnoses. Psychological Medicine. 1982;12:855–870. doi: 10.1017/s0033291700049151. [DOI] [PubMed] [Google Scholar]
- Robins LN, Tipp J, Przybeck T. Antisocial personality. In: Robins LN, Regier DA, editors. Psychiatric Disorders in America. New York, NY: Free Press; 1991. pp. 224–271. [Google Scholar]
- Rushton JL, Forcier M, Schectman RM. Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:199–205. doi: 10.1097/00004583-200202000-00014. [DOI] [PubMed] [Google Scholar]
- Salekin RT, Leistico AMR, Neumann CS, DiCicco TM, Duros RL. Psychopathy and comorbidity in a young offender sample: taking a closer look at psychopathy’s potential importance over disruptive behavior disorders. Journal of Abnormal Psychology. 2004;113:416–427. doi: 10.1037/0021-843X.113.3.416. [DOI] [PubMed] [Google Scholar]
- Satterfield JH, Schell A. A prospective study of hyperactive boys with conduct problems and normal boys: adolescent and adult criminality. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1726–1735. doi: 10.1097/00004583-199712000-00021. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Shaffer D, Dulcan MK, Jensen PS, Fisher P, Bird HR, et al. Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3) Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:878–888. doi: 10.1097/00004583-199607000-00013. [DOI] [PubMed] [Google Scholar]
- Seagrave D, Grisso T. Adolescent development and the measurement of juvenile psychopathy. Law and Human Behavior. 2002;26:219–239. doi: 10.1023/a:1014696110850. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sickmund M, Sladky TJ, Kang W. Census of Juveniles in Residential Placement Databook. 2005 Retrieved June 1, 2006, from http://www.ojjdp.ncjrs.org/ojstatbb/cjrp/
- Silverthorn P, Frick PJ. Developmental pathways to antisocial behavior: the delayed-onset pathway in girls. Development and Psychopathology. 1999;11:101–126. doi: 10.1017/s0954579499001972. [DOI] [PubMed] [Google Scholar]
- Snyder HN, Sickmund M. Juvenile Offenders and Victims: 2006 National Report. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention; 2006. [Google Scholar]
- Snyder J, Reid J, Patterson G. A social learning model of child and adolescent antisocial behavior. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of Conduct Disorder and Juvenile Delinquency. New York, NY: Guilford Press; 2003. pp. 27–48. [Google Scholar]
- Sourander AM, Multimaki PM, Nikolakaros GM, Haavisto AM, Ristkari TM, Helenius HM, et al. Childhood predictors of psychiatric disorders among boys: a prospective community-based follow-up study from age 8 years to early adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:756–767. doi: 10.1097/01.chi.0000164878.79986.2f. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2002;59:1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Washburn JJ, Pikus AK. Detecting mental disorder in juvenile detainees: who receives services. American Journal of Public Health. 2005;95:1773–1780. doi: 10.2105/AJPH.2005.067819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman GA, McReynolds LS, Lucas CP, Fisher P, Santos L. The voice DISC-IV with incarcerated male youths: prevalence of disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:314–321. doi: 10.1097/00004583-200203000-00011. [DOI] [PubMed] [Google Scholar]
- Westermeyer J, Thuras P. Association of antisocial personality disorder and substance disorder morbidity in a clinical sample. American Journal of Drug & Alcohol Abuse. 2005;31:93–110. [PubMed] [Google Scholar]
- Zoccolillo M, Pickles A, Quinton D, Rutter M. The outcome of childhood conduct disorder: implications for defining adult personality disorder and conduct disorder. Psychological Medicine. 1992;22:971–986. doi: 10.1017/s003329170003854x. [DOI] [PubMed] [Google Scholar]