Abstract
Objectives. We examined the effects of community socioeconomic conditions, air pollution, and the physical environment on elderly health and survival in China.
Methods. We analyzed data from a nationally representative sample of 15 973 elderly residents of 866 counties and cities with multilevel logistic regression models in which individuals were nested within each county or city.
Results. After control for individual-level factors, communities' gross domestic product per capita, adult labor force participation rate, and illiteracy rate were significantly associated with physical, mental, and overall health and mortality among the elderly in China. We also found that air pollution increased the odds of disability in activities of daily living (ADLs), cognitive impairment, and health deficits; more rainfall was protective, reducing the odds of ADL disability and cognitive impairment; low seasonal temperatures increased the odds of ADL disability and mortality; high seasonal temperatures increased the odds of cognitive impairment and deficits; and living in hilly areas decreased the odds of ADL disability and health deficits.
Conclusions. Efforts to reduce pollution and improve socioeconomic conditions could significantly improve elderly health and survival.
China's continued rapid economic growth1 has been coupled with significant environmental degradation. For example, approximately 40% of China's land is affected by soil erosion and deforestation.2,3 Rapid economic growth and significant environmental degradation are also occurring in many other developing countries.4,5 Hence, although socioeconomic development may improve population health and survival, related environmental degradation may have an opposite effect in China and elsewhere.
The population of China, as in all developed and many other developing countries, is aging because of substantial declines in both fertility and mortality. The number of persons aged 65 years and older in China is forecast to increase dramatically from 87 million in 2000 (6.7% of the population), to 243–252 million in 2030 (16.5%–17.0%), and then to 352–398 million in 2050 (24.1%–26.4%), with the ranges reflecting uncertainty about changes in mortality in the next few decades.6 Population aging is occurring 3.3 to 4.4 times as quickly in China and other developing countries as it is in Europe.7
Previous studies identified significant associations of community socioeconomic conditions and physical environment (such as degree of air pollution, average temperature, yearly rainfall, and geographic topography) with health and mortality.8,9 Elderly persons are especially sensitive to their physical and social surroundings and may be more vulnerable than younger adults to the negative effects of environmental degradation on health and survival.10–12 Consequently, the concurrent rapid population aging and environmental degradation in China and other developing countries are likely to impair the quality of life of elderly people and their families. Furthermore, developing countries lag behind developed countries in both socioeconomic welfare and environmental protection; with little preparation, the challenges of coping with an aging society that China faces are more serious than those in developed countries. Estimates of the associations of environmental factors with elderly health and survival are therefore vital for the formulation of policies for sustainable development and public health in developing countries. The elderly are among the groups most susceptible to the adverse effects of community socioeconomic problems and environmental pollution; research is needed in this population to identify the most crucial issues as targets of policy remedies.12
The current literature concerning the associations of community conditions with elderly health and mortality has major limitations. First, few longitudinal studies at the nationwide and population level have measured the actual environmental exposures of individual older persons.12 Most previous research collected and analyzed community and individual data from 1 or a few municipalities10,13 or used aggregated data only.14,15 Second, almost all of the published studies focused on elderly persons younger than age 85 years because they lacked a sufficiently large subsample to adequately represent the oldest old, a subpopulation that is growing twice as fast as the overall elderly population (aged 65 years or older).16 Third, previous work mostly focused on the developed countries; published analyses of data from developing countries, including China, are rare.17 In developed countries, the socioeconomic conditions may differ less between different communities than they do in developing countries; this lack of variability may limit the statistical power of analyses of the associations of community environment with elderly health and mortality.
Elderly health outcomes are generally believed to be affected by social and behavioral factors at the individual level, socioeconomic and physical environmental factors at the community level, and genetic factors at the molecular level, as well as the complex interactions among all of these.18 We assessed the impact of community socioeconomic and physical environmental factors on health and survival among the elderly, adjusting for individual social and behavior factors such as age, gender, childhood conditions, and adulthood socioeconomic status (SES). We also conducted statistical analyses of the potential interactions between community- and individual-level factors. Genotype data were not available, but we used random-effects modeling to account for unobserved heterogeneity.
We analyzed data from a large, prospective, nationally representative cohort of the Chinese elderly, including a large subsample of the oldest old and a compatible subsample of the younger old, to test the hypothesis that community socioeconomic conditions, air pollution, and the physical environment in China are associated with elderly health and survival. Community conditions varied tremendously in the 866 counties and cities in our sample, providing a good opportunity to investigate the impact of environmental factors on health and mortality among the elderly.
METHODS
Our data were from the third and fourth waves of the Chinese Longitudinal Healthy Longevity Survey (CLHLS), conducted in 2002 and 2005, with a total sample size of 15 973, including 9017 oldest-old (aged 85 years or older) and 6956 younger-old (aged 65–84 years) respondents. For its sample, the CLHLS randomly selects half of the counties and cities in 22 of China's 31 provinces, representing 85% of the total population of the country. The 1998 baseline and 2000 follow-up surveys included approximately 10 000 interviewees, all in the oldest-old group. Beginning in 2002, the CLHLS also interviewed younger-old persons.
The CLHLS data include demographic characteristics, physical and mental health, chronic disease, socioeconomic status, family and social support and connections, and health practices for individuals and socioeconomic and environmental information for counties and cities. Information about the date of death and health status before dying for deceased respondents was collected through interviews with a close family member. Systematic assessments have documented the quality of the CLHLS data.19,20
Elderly Health Outcomes
We used the activities of daily living (ADL) score for our measure of physical health. Persons who needed help to perform any of the 6 daily tasks of bathing, dressing, moving around indoors, going to the toilet and cleaning themselves afterward, eating, and continence were considered to be ADL disabled; otherwise, respondents were regarded as ADL active.
The internationally accepted Mini-Mental State Examination questionnaire was culturally adapted and translated into Chinese.21 For our mental health measure, we defined respondents who scored under 18 out of a total possible score of 30 as cognitively impaired.
We used the cumulative deficits index (DI) score for our overall health measure. The DI, which has been widely applied in healthy aging studies, is a summation of deficits in variables reflecting different dimensions of health conditions.22,23 Following the general practice in constructing this measure (previously called the frailty index),22,23 we estimated the DI for each respondent from 30 variables, including cognitive function, ADLs, instrumental activities of daily living (IADLs), physical performance, self-rated health, interviewer-reported health, hearing and vision loss, heart rhythm, psychological distress, serious illness in the past 2 years, and specific chronic diseases. We dichotomized DI scores with a cutpoint of 0.45; 10.3% of respondents scored below this cutpoint (DI score mean = 0.26; variance = 0.026). We also monitored mortality during the interwave period of 2002 to 2005.
Community Environmental Variables
Primary county or city variables included air pollution index (API), per capita gross domestic product (GDP), labor force participation rate, and illiteracy rate. We controlled for physical environmental factors (average temperature in January and July, yearly rainfall, and geographic topography) as confounding variables at the community level. The CLHLS measured these community variables in 866 randomly selected community units (counties or cities) in the 22 provinces surveyed (for more detail, see the Appendix available as a supplement to the online version of this article at http://www.ajph.org).
We obtained data on community socioeconomic indicators from the National Bureau of Statistics of China24 and data on the physical environment from the Chinese Natural Resources Database25 and the China Environmental Statistics Yearbook.26 The labor force participation rate was the percentage of the total number of persons aged 15 to 64 years in the community who were currently working for pay.
We used the widely accepted API for 1995 to reflect the possibly delayed effects of air pollution on elderly health in 2002 and mortality in 2002 to 2005. API was graded from 1 = least pollution to 7 = most. The temperatures in January and July and yearly rainfalls were the average for 1950 to 1995.
We obtained geographic topography information from the community questionnaire of the CLHLS in 2002. Our mortality data was derived from the CLHLS longitudinal follow-up of respondents from the 2002 to 2005 waves.
Individual-Level Covariates
We reviewed the existing literature27–29 to select 24 potential confounding factors measured in the 2002 CLHLS and controlled for them in our models.
Demographic characteristics.
Basic demographic data were age, gender, and ethnicity (Han Chinese versus minorities).
Childhood socioeconomic status.
Childhood SES was determined by birth in a rural or urban area, father's occupation, whether both parents were alive when the respondent was aged 10 years, whether the respondent received adequate medication for childhood illnesses, whether the respondent frequently went to bed hungry in childhood, whether the respondent was a first-born child, and arm length (measured at the interview).
Adult socioeconomic status.
Adult SES was determined by current residence (rural versus urban), education level, economic independence (having retirement earnings versus no income), primary lifetime occupation (white collar versus other), family household economic condition, and resources for medical expenses (primarily covered by public funds or insurance versus out of pocket).
Family and social support.
Social network factors were marital status (currently married versus unmarried), number of surviving children, proximity to children (living with children or having at least 1 child close by versus having no children in home or close by), participating in religious activities (yes versus no), and a social and leisure activities index (constructed from available data for 7 activities: personal outdoor activities, gardening, reading newspapers and books, raising domestic poultry or pets, playing cards or mah-jong, watching TV or listening to the radio, and participating in organized social activities other than religion).
Health practices.
Respondents answered 3 dichotomous (yes versus no, for the past 5 years) health practice questions: whether they smoked, heavily consumed alcohol, and exercised regularly.
With the exception of several continuous variables (API, age, and the social and leisure activities index), we dichotomized most of our large number of variables to simplify the analysis. To group the dichotomized variables, we conducted alternative sensitivity modeling, applied our experience with coding in this data set, and consulted other published studies that dichotomized most of the same variables.30–32 The frequency distributions of the 8 socioeconomic and physical environmental factors for the 866 counties and cities, the 3 major indicators of the health outcomes, and the 24 individual-level covariates are presented in Table 1.
TABLE 1.
Study Variables and Covariates: Chinese Longitudinal Healthy Longevity Survey, 2002–2005
| Variables | No. or % |
| No. of counties/cities | 866 |
| No. of respondents | 15 973 |
| Community-level variables | |
| Labor force participation rate ≥ 70%a | 79.9 |
| Per capita GDP ≥ $2000 | 87.4 |
| Illiteracy rate < 5% | 14.9 |
| Air pollution index, mean | 3.52 |
| Average temperature in January < −10°C | 11.2 |
| Average temperature in July ≥ 29°C | 13.9 |
| Yearly rainfall ≥ 800 mm | 56.6 |
| Hills or mountains covering ≥ 70% of local area | 52.6 |
| Individual-level variables | |
| Health outcomes | |
| Health deficits index > 0.45 in 2002 | 10.3 |
| ADL disabled in 2002 | 30.8 |
| Cognitively impaired in 2002 | 40.9 |
| Deaths between 2002 and 2005 | 41.8 |
| Demographic characteristics | |
| Age, y, mean | 86.3 |
| Male | 42.7 |
| Ethnic group other than Han | 5.7 |
| Childhood SES | |
| Born in urban area | 15.6 |
| Father had white-collar occupation | 4.0 |
| Both parents alive when respondent was aged 10 y | 63.1 |
| Received adequate medication for illness | 51.0 |
| Frequently went to bed hungry | 65.4 |
| First birth in family | 37.0 |
| Arm length,b mean cm | 49.6 |
| Adult SES | |
| Currently lives in urban area | 46.0 |
| Primary lifetime occupation white collar | 8.6 |
| Family household economic condition good | 17.3 |
| Financially independent | 26.0 |
| Education ≥ 1 y | 38.0 |
| Medical expenses covered primarily by public funds or insurance | 13.0 |
| Family/social connection and support | |
| Currently married | 31.3 |
| Living children, mean | 3.2 |
| Children living nearby or with respondent | 73.7 |
| Social and leisure activity index,c mean | 2.15 |
| Participation in religious activities | 17.5 |
| Health practices | |
| Smoked in past 5 y | 22.8 |
| Consumed alcohol in past 5 y | 24.5 |
| Regularly exercised in past 5 y | 34.0 |
Note. ADL = activities of daily living; GDP = gross domestic product; SES = socioeconomic status.
Percentage of persons aged 15 to 64 years currently working for pay.
Arm measured from processus styloideus ulnae to acromion.
Social and leisure activity index score derived from 7 dichotomized variables: gardening, personal outdoor activities (excluding exercise), raising poultry or pets, reading, playing cards or mah-jong, listening to the radio or watching TV, and participating in some organized social activities (excluding religious participation).
Statistical Analyses
In our multilevel, multivariate logistic regression models, individuals were nested within geographic areas of counties and cities to detect associations of community environmental factors with elderly ADL disability, cognitive impairment, and health deficits. The mathematical equations of the models, sampling weights, and the other technical issues are described in the Appendix (available as an online supplement). We used HLM version 6.0 for all analyses.32
We evaluated various interaction terms (including interactions between community variables and individual SES) in our analyses, but almost none of the results were statistically significant, thus are not presented here (data available upon request).
RESULTS
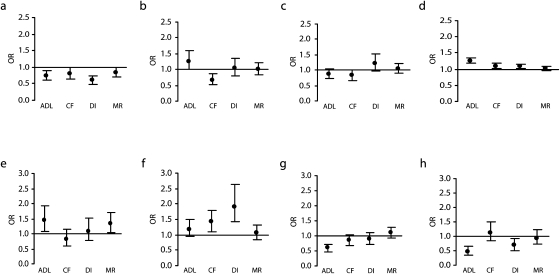
Table 2 presents detailed estimates of the odds ratios for associations of community-level factors with elderly health and mortality risk, after control for confounding individual-level factors, including age. Figure 1 depicts the main results. Although associations of individual-level factors are also presented in Table 2, we focus here on community-level factors. Detailed discussions of associations between health and childhood and adult SES and between SES and mortality among elderly Chinese are available elsewhere.33,34
TABLE 2.
Associations of Community-Level Factors With Elderly Health Indicators and Mortality Risk After Adjustment for Individual-Level Confounding Factors: Chinese Longitudinal Healthy Longevity Survey, 2002–2005
| Health indicators |
||||
| Variables (Refa) | ADL Disability, OR (95% CI) or % | Cognitive Impairment, OR (95% CI) or % | Deficits Index > 0.45, OR (95% CI) or % | Mortality, OR (95% CI) or % |
| Community-level variables | ||||
| Labor force participation rate ≥ 70%b (< 70%) | 0.74*** (0.62, 0.89) | 0.80** (0.65, 0.99) | 0.60† (0.49, 0.75) | 0.84** (0.72, 0.99) |
| Per capita GDP ≥ $2000 (< $2000) | 1.26** (1.00, 1.58) | 0.67*** (0.53, 0.87) | 1.04 (0.79, 1.36) | 1.01 (0.84, 1.21) |
| Illiteracy rate < 5% (≥ 5%) | 0.87 (0.72, 1.05) | 0.82* (0.67, 1.00) | 1.20 (0.96, 1.52) | 1.04 (0.89, 1.20) |
| Average temperature in January < −10°C (≥ −10°C) | 1.44** (1.06, 1.94) | 0.83 (0.61, 1.14) | 1.08 (0.77, 1.53) | 1.32* (1.03, 1.70) |
| Average temperature in July ≥ 29°C (< 29°C) | 1.18 (0.94, 1.49) | 1.41*** (1.09, 1.81) | 1.92† (1.41, 2.63) | 1.06 (0.85, 1.32) |
| Yearly rainfall ≥ 800 mm (< 800 mm) | 0.59† (0.48, 0.73) | 0.84* (0.68, 1.03) | 0.91 (0.73, 1.12) | 1.09 (0.92, 1.28) |
| Hills or mountains covering ≥ 70% of local area (< 70%) | 0.48† (0.35, 0.67) | 1.12 (0.83, 1.51) | 0.68** (0.49, 0.94) | 0.94 (0.73, 1.22) |
| Air pollution index | 1.25† (1.18, 1.34) | 1.09** (1.01, 1.18) | 1.08** (1.01, 1.16) | 1.02 (0.97, 1.07) |
| Individual-level variables | ||||
| Demographic characteristics | ||||
| Age, y | 1.07† (1.06, 1.07) | 1.08† (1.08, 1.09) | 1.03† (1.02, 1.03) | 1.08† (1.07, 1.08) |
| Male (female) | 0.77† (0.69, 0.86) | 0.74† (0.67, 0.81) | 0.95 (0.82, 1.10) | 1.50† (1.35, 1.66) |
| Ethnic group other than Han (Han) | 0.88 (0.69, 1.12) | 0.98 (0.75, 1.27) | 0.94 (0.68, 1.29) | 0.91 (0.71, 1.16) |
| Childhood SES | ||||
| Born in urban area (rural) | 1.20*** (1.06, 1.37) | 0.92 (0.82, 1.04) | 1.25** (1.05, 1.50) | 1.14* (0.99, 1.29) |
| Father had white-collar occupation (no) | 0.94 (0.76, 1.15) | 0.92 (0.75, 1.14) | 0.94 (0.69, 1.30) | 1.04 (0.83, 1.31) |
| Both parents alive when respondent was aged 10 y (no) | 0.93 (0.86, 1.02) | 0.75† (0.69, 0.81) | 0.85*** (0.76, 0.95) | 0.88*** (0.81, 0.97) |
| Received adequate medication for illness (no) | 1.03 (0.94, 1.14) | 1.04 (0.96, 1.13) | 0.93 (0.83, 1.04) | 0.98 (0.90, 1.07) |
| Frequently went to bed hungry (no) | 0.92* (0.84, 1.00) | 1.16*** (1.07, 1.27) | 1.05 (0.92, 1.21) | 1.00 (0.92, 1.09) |
| First birth in family (no) | 0.95 (0.88, 1.03) | 1.06 (0.98, 1.14) | 1.00 (0.90, 1.12) | 0.96* (0.89, 1.04) |
| Arm length in highest 20% (lowest 80%) | 0.94 (0.83, 1.06) | 0.83*** (0.73, 0.93) | 0.91 (0.78, 1.06) | 0.90 (0.80, 1.00) |
| Adult SES | ||||
| Urban resident (rural) | 1.23† (1.11, 1.36) | 0.90** (0.81, 1.00) | 1.09 (0.95, 1.24) | 0.94 (0.85, 1.04) |
| Primary lifetime occupation white collar (no) | 1.46† (1.22, 1.76) | 0.91 (0.76, 1.08) | 1.22 (0.93, 1.61) | 1.02 (0.86, 1.21) |
| Family economic condition good (no) | 1.06 (0.95, 1.18) | 0.71† (0.65, 0.79) | 0.86* (0.73, 1.01) | 1.07 (0.96, 1.19) |
| Financially independent (no) | 0.94 (0.83, 1.08) | 0.73† (0.65, 0.83) | 0.97 (0.82, 1.15) | 0.76† (0.67, 0.86) |
| Education ≥ 1 y (no) | 1.13** (1.02, 1.25) | 0.72† (0.65, 0.79) | 1.16** (1.01, 1.33) | 1.11** (1.00, 1.23) |
| Medical expenses covered primarily by public funds or insurance (no) | 1.22** (1.04, 1.43) | 1.06 (0.90, 1.24) | 1.51† (1.23, 1.89) | 1.08 (0.93, 1.27) |
| Family/social connection and support | ||||
| Currently married (no) | 1.03 (0.93, 1.15) | 0.91** (0.83, 1.00) | 1.36† (1.16, 1.57) | 0.81† (0730.90) |
| Living children (no) | 1.03** (1.01, 1.05) | 0.98** (0.96, 1.00) | 1.00 (0.97, 1.03) | 0.98* (0.96, 1.00) |
| Children living nearby or with respondent (no) | 1.13** (1.03, 1.25) | 1.03 (0.93, 1.13) | 0.89* (0.78, 1.01) | 1.08 (0.97, 1.20) |
| Social and leisure activity index | 0.49† (0.47, 0.51) | 0.66† (0.64, 0.68) | 0.34† (0.33, 0.37) | 0.78† (0.75, 0.81) |
| Participation in religious activities (no) | 0.83*** (0.74, 0.94) | 0.72† (0.63, 0.82) | 0.57† (0.48, 0.67) | 9.86*** (0.76, 0.96) |
| Health practices | ||||
| Smoked in past 5 y (no) | 0.92 (0.83, 1.02) | 1.00 (0.90, 1.12) | 0.87* (0.75, 1.00) | 1.09 (0.98, 1.20) |
| Consumed alcohol in past 5 y (no) | 0.97 (0.88, 1.07) | 0.91** (0.83, 0.99) | 0.81*** (0.69, 0.94) | 1.01 (0.92, 1.10) |
| Regularly exercised in past 5 y (no) | 0.82† (0.74, 0.90) | 0.74† (0.67, 0.81) | 0.60† (0.52, 0.69) | 0.93 (0.84, 1.03) |
| Health deficits index in 2002 | — | — | — | 2.11† (1.86, 2.38) |
| Variances | ||||
| Individual level, variance (SE) | 0.9435 (0.0108) | 0.8782 (0.0101) | 0.8631 (0.0099) | 0.9454 (0.0116) |
| Community level, variance | 0.7831 (0.0650) | 1.1664 (0.0837) | 0.8224 (0.0860) | 0.3756 (0.0391) |
| Total variance,c % | 45.3 | 57.1 | 49.8 | 28.4 |
Note. ADL = activities of daily living; OR = odds ratio; CI = confidence interval; GDP = gross domestic product; SES = socioeconomic status.
Values in parentheses represent the reference group of environmental factors.
Percentage of persons aged 15 to 64 years currently working for pay.
Variance at community level divided by the summation of variances at individual and community levels, then multiplied by 100.
*P < .1; **P < .05; ***P < .01; †P < .001.
FIGURE 1.
Odds ratios (OR) of association between major health outcomes among the elderly and community-level factors of (a) labor participation rate ≥ 70% vs < 70%, (b) GDP per capita ≥ $2000 vs < $2000, (c) illiteracy rate < 5% vs ≥ 5%, (d) air pollution index continuous mean, (e) mean temperature in January < −10°C vs ≥ −10°C, (f) mean temperature in July > 29°C vs ≤ 29°C, (g) annual rainfall ≥ 800 mm vs < 800 mm, and (h) hilly terrain ≥ 70% vs < 70%: Chinese Longitudinal Healthy Longevity Survey, 2002–2005.
Note. ADL = activities of daily living; CF = cognitive function; DI = deficits index; GDP = gross domestic product; MR = mortality risk. ADL and CF values are for odds of impairment; DI impairment is a score higher than 0.45. All estimates were adjusted for 24 confounding factors pertaining to demographic characteristics, socioeconomic status in both childhood and adulthood, family support, social contacts, and lifestyle at the individual level. To estimate mortality risk, we further controlled for the DI in 2002.
Source. Data were obtained from the 2002 to 2005 Chinese Longitudinal Healthy Longevity Survey follow-up data.19
After controlling for a wide range of potentially confounding individual and community environmental factors, we found statistically significant associations between community-level socioeconomic factors and health outcomes among the elderly in China. Higher labor force participation among persons aged 15 to 64 years in the community reduced older persons' risk of ADL disabilities (26%; P < .01), cognitive impairment (20%; P < .05), health deficits (40%; P < .001), and death over a 3-year follow-up (16%; P < .05).
Higher per capita GDP and lower community rate of illiteracy decreased the odds of cognitive impairment by 33% (P < .01) and 18% (P < .10), respectively. Notably, higher per capita GDP increased the rate of ADL disability by 26% (P < .05).
Community-level physical environmental factors were also associated with health outcomes, after adjustment for individual- and community-level socioeconomic variables. Air pollution increased the odds of developing ADL disability (25%; P < .001), cognitive impairment (9%; P < .05), and health deficits (8%; P < .05). Air pollution increased mortality, but this association was not statistically significant, possibly because the follow-up period was not long enough.
Weather had significant effects on diverse health outcomes. More rainfall was protective, reducing the odds of developing ADL disability (41%; P < .001) and cognitive impairment (16%; P < .10). The effect of temperature was significant as well: very low seasonal temperature increased the odds of ADL disability by 44% (P < .1) and increased mortality by 32% (P < .05); very high seasonal temperature increased the odds of developing cognitive impairment (41%; P < .01) and health deficits (92%; P < .001). Living in hilly areas decreased the odds of developing ADL disability by 52% (P < .001) and decreased DI scores by 32% (P < .05).
DISCUSSION
To our knowledge, ours was the first study to use a national longitudinal data set to investigate the effects of environmental factors on health and mortality among the elderly in China, the largest developing country. The major contribution of our study is its statistically robust conclusions derived from data from large subsamples of oldest-old and younger-old adults living in 866 highly diverse counties and cities and including information on both community- and individual-level factors. Our results indicated that, at the community level, both socioeconomic and physical environmental factors were strongly predictive of diverse health outcomes among the elderly in China, including cognitive impairment, physical disability, health deficits, and mortality.
The associations of the community-level socioeconomic factors with elderly health and survival should be interpreted in the unique social and familial contexts in China. For example, higher labor force participation rate among younger adults might seem to have little to do with the health of the elderly, who are not included in this measurement. However, in China, most elderly persons are cared for by their own families within the local community. A higher labor force participation rate among persons aged 15 to 64 years in the community results in higher community and family income and improved surroundings, which in turn may improve elderly health and survival.35–37
Our finding that higher per capita GDP was associated with a higher rate of ADL disability is consistent with a study by Zeng and Vaupel that found fewer ADL disabilities among rural than urban elderly Chinese.38 Conditions in communities with low GDP may force older persons to perform daily activities by themselves; that is, the elderly may be required to be active, and therefore they may not admit to disability. It is also possible that frequent exercise may enable them to maintain their ADL abilities longer than do their counterparts in areas with higher GDP. Similarly, the elderly in Indonesia, Malaysia, the Philippines, Singapore, and Thailand have been found to be more active than the elderly in developed countries.39,40 Moreover, persons with ADL disabilities may die earlier in poor areas but survive in richer communities that offer better medical services or other advantages.
The observed relationship between community-level physical environmental factors and health outcomes among the Chinese elderly is generally consistent with what is known about other countries.41–43 Air pollution appears to exacerbate symptoms of chronic obstructive pulmonary disease. If cleaner air promotes outdoor physical activities, it may protect against ADL disability, cognitive impairment, and health deficits. Comfortable temperatures may similarly encourage outdoor exercise, along with reducing the transmission of contagious diseases, which increases when people spend most of their time indoors.41 Fresh air and more rainfall likely signal greater availability of food and fresh water, and may lead to better pulmonary function and nutritional status, thus to better health in the elderly. Understanding the relationship between climate and health outcomes may be useful in light of global warming.44 We found that living in hilly terrain lowered the odds of developing ADL disability, probably because daily activities require more exertion in these surroundings. Studies of physical exercise in the elderly have found protective effects for strength, aerobic capacity, walking, and balance.45
Limitations
The 3-year follow-up period in our data set might not have been long enough to fully capture all the associations between environmental factors and elderly mortality. There is also an unavoidable trade-off between surveying a large nationwide sample with many community units and collecting the level of detail from respondents that would be required for deeper analysis of causal mechanisms. The associations we observed therefore could not be interpreted as determining causality.
Further work will be necessary to clarify the causal mechanisms by which Chinese elderly people's health and survival are influenced by environmental factors, including direct and indirect effects (through mediators or interactions). Possible factors that future studies might examine to help answer these questions include geochemical conditions such as drinking water quality, components of the soil in which the main food crops grow, and microelements in samples of diet and hair collected from respondents residing in carefully selected and diverse areas.
Conclusions
Recent estimates are that 13% to 37% of the worldwide disease burden could be prevented by environmental improvements, resulting in approximately 13 million fewer deaths per year.46 The world's population is aging rapidly, and further understanding of the socioeconomic and physical environmental factors associated with health and mortality in elderly persons is vital from both societal and scientific perspectives.12 Research on the elderly, who are highly susceptible to the adverse effects of environmental degradation, may help identify the environmental factors that present the greatest risk for ill health and to mitigate their effects through policy interventions in China and elsewhere. For example, interventions to counteract the effects of adverse environmental circumstances might include exercise programs designed to compensate for local environmental constraints, such as leg strengthening exercises for people living in locations without hills or aerobic exercises that could be performed indoors where air pollution precludes walking outdoors.
Our findings support an urgent need for further research to inform policies and programs to improve both community environments and socioeconomic circumstances. Benefits to public health and the health of the elderly could also lead to greater social stability in China and elsewhere.
Acknowledgments
This study is part of the CLHLS project funded by the National Institute on Aging (grant R01 AG023627-01), China Natural Science Foundation (grant 70533010), United Nations Population Fund, China Social Sciences Foundation, and Hong Kong Research Grants Council. Jama Purser was also supported by the National Center for Medical Rehabilitation Research, National Institute of Child Health and Human Development (grant 5K01HD049593), National Institute on Aging (grant 1P30AG028716), and Global Health Institute, Duke University.
We thank Ilene C. Siegler for her comments on our draft.
Note. The content of this article is the sole responsibility of the authors and does not necessarily represent the official views of the funding agencies acknowledged here.
Human Participation Protection
The research ethics committees of Duke University and Peking University approved the protocol for each wave of the CLHLS, which is the data source of this study. The survey respondents gave informed consent before participating.
References
- 1.International Monetary Fund World economic and financial surveys. World economic outlook database. 2007. Available at: http://www.imf.org/external/pubs/ft/weo/2007/02/weodata/index.aspx. Accessed June 12, 2008
- 2.Wang Y. Environmental degradation and environmental threats in China. Environ Monit Assess 2004;90(1–3):161–169 [DOI] [PubMed] [Google Scholar]
- 3.Cann CW, Cann MC, Gao S. China's road to sustainable development. : Day KA, China's Environment and the Challenge of Sustainable Development New York, NY: M. E. Sharpe; 2005:3–34 [Google Scholar]
- 4.López R. Environmental degradation and economic openness in LDCs: the poverty linkage. Am J Agric Econ 1992;74(5):1138–1143 [Google Scholar]
- 5.Chousa JP, Tamazian A, Vadlamannati KC. Rapid Economic Growth at the Cost of Environment Degradation? Panel Data Evidence from BRIC Economies Ann Arbor: University of Michigan; 2008. William Davidson Institute working paper 908 [Google Scholar]
- 6.Zeng Y, George LK. Population aging and old-age care in China. : Dannefer D, Phillipson C, Sage Handbook of Social Gerontology Thousand Oaks, CA: Sage; In press [Google Scholar]
- 7.Nizamuddin M. Javed Sajjad Ahmad, Fauzia Maqsood. Demography of aging. : Zeng Y, Encyclopedia of Life Support Systems: Demography Volume Theme 6.147 Oxford, UK: UNESCO Publishing-EOLSS Publisher; 2008 [Google Scholar]
- 8.Filleul L, Rondeau V, Cantagrel A, Dartigues J-F, Tessier J-F. Do subject characteristics modify the effects of particulate air pollution on daily mortality among the elderly? J Occup Environ Med 2004;46(11):1115–1122 [DOI] [PubMed] [Google Scholar]
- 9.Kawachi I, Berkman LF. Neighborhoods and Health New York, NY: Oxford University Press; 2003 [Google Scholar]
- 10.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol 2002;155(6):507–515 [DOI] [PubMed] [Google Scholar]
- 11.Nordstrom CK, Diez Roux AV, Jackson SA, Gardin JM. The association of personal and neighborhood socioeconomic indicators with subclinical cardiovascular disease in an elderly cohort: the Cardiovascular Health Study. Soc Sci Med 2004;59(10):2139–2147 [DOI] [PubMed] [Google Scholar]
- 12.Sandstrom T, Frew AJ, Svartengren M, Viegi G. The need for a focus on air pollution research in the elderly. Eur Respir J 2003;21(Suppl 40):92S–95S [DOI] [PubMed] [Google Scholar]
- 13.Lepeule J, Rondeau V, Filleul L, Dartigues J-F. Survival analysis to estimate association between short-term mortality and air pollution. Environ Health Perspect 2006;114(2):242–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donaldson GC, Kovats RS, Keatinge WR, McMichael R. Heat- and cold-related mortality and morbidity and climate change. : Expert Group on Climate Change and Health in the UK, ed. Health Effects of Climate Change in the UK London, UK: Department of Health; 2001:71–80 [Google Scholar]
- 15.Keatinge WR, Donaldson GC. The impact of global warming on health and mortality. South Med J 2004;97(11):1093–1099 [DOI] [PubMed] [Google Scholar]
- 16.Suzman RM, Manton KG, Willis DP. Introducing the oldest old. : Suzman RM, Willis DP, Manton KG, The Oldest Old New York, NY: Oxford University Press; 1992 [Google Scholar]
- 17.Kan H, Chen B. Air pollution and daily mortality in Shanghai: a time-series study. Arch Environ Health 2003;58(6):360–367 [PubMed] [Google Scholar]
- 18.Hernandez LM, Blazer DG, Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate Washington, DC: National Academies Press; 2006 [PubMed] [Google Scholar]
- 19.Gu D. General data assessment of the Chinese Longitudinal Healthy Longevity Survey in 2002. : Zeng Y, Poston DL, Vlosk DA, Gu D, Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions Dordrecht, Netherlands: Springer; 2008:39–58 [Google Scholar]
- 20.Zeng Y, Gu D. Reliability of age reporting among the Chinese oldest-old in the CLHLS datasets. : Zeng Y, Poston DL, Vlosk DA, Gu D, Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions Dordrecht, Netherlands: Springer; 2008:61–79 [Google Scholar]
- 21.Folstein MF, Folstein SE, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psych Res 1975;12:189–198 [DOI] [PubMed] [Google Scholar]
- 22.Kulminski AM, Ukraintseva SV, Kulminskaya IV, Arbeev KG, Land KC, Yashin AY. Cumulative deficits better characterize susceptibility to death in the elderly than phenotypic frailty: lessons from the Cardiovascular Health Study. J Am Geriatr Soc 2008;56(5):898–903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goggins WB, Woo J, Sham A, Ho SC. Frailty index as a measure of biological age in a Chinese population. J Gerontol A Biol Sci Med Sci 2005;60(8):1046–1051 [DOI] [PubMed] [Google Scholar]
- 24.Socioeconomic Development Data at County Level in China [CD-ROM] Beijing: Nation Bureau of Statistics of China; 2003 [Google Scholar]
- 25.Chinese Natural Resources Database Beijing: Chinese Academy of Sciences Institute of Geographical Sciences and Natural Resources; 2004. Available at: http://www.data.ac.cn/index.asp. Accessed June 12, 2008 [Google Scholar]
- 26.National Bureau of Statistics of China and State Environmental Protection Administration China Statistical Yearbook on Environment Beijing: China Statistics Press; 2004 [Google Scholar]
- 27.Ferraro KF, Farmer MM, Wybraniec JA. Health trajectories: long-term dynamics among Black and White adults. J Health Soc Behav 1997;38(1):38–54 [PubMed] [Google Scholar]
- 28.Kim JM, Stewart R, Shin IS, Yoon JS. Limb length and dementia in an older Korean population. J Neurol Neurosurg Psychiatry 2003;74(4):427–432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med 1999;48(4):445–469 [DOI] [PubMed] [Google Scholar]
- 30.Koening HG, Hays JC, Larson DB, et al. Does religious attendance prolong survival? A six-year follow-up study of 3,968 older adults. J Gerontol A Med Sci 1999;54(7):M370–M376 [DOI] [PubMed] [Google Scholar]
- 31.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. Am J Public Health 1997;87(6):957–961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raudenbush S, Bryk A, Cheong YE, Congdon R, du Toit M. HLM: Hierarchical Linear and Nonlinear Modeling Lincolnwood, IL: Scientific Software International; 2004 [Google Scholar]
- 33.Zeng Y, Gu D, Land KC. The association of childhood socioeconomic conditions with healthy longevity at the oldest-old ages in China. Demography 2007;44(3):497–518 [DOI] [PubMed] [Google Scholar]
- 34.Zeng Y, Poston D, Vlosky DA, Gu D, Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions Dordrecht, Netherlands: Springer; 2008 [Google Scholar]
- 35.Ballester F, Corella D, Perez-Hoyos S, Saez M, Hervas A. Mortality as a function of temperature. A study in Valencia, Spain, 1991–1993. Int J Epidemiol 1997;26(3):551–561 [DOI] [PubMed] [Google Scholar]
- 36.Armstrong D, Barnett E, Casper M, Wing S. Community occupational structure, medical and economic resources, and coronary mortality among U.S. Blacks and Whites, 1980–1988. Ann Epidemiol 1998;8(3):184–191 [DOI] [PubMed] [Google Scholar]
- 37.King WC, Belle SH, Brach JS, Simkin-Silverman LR, Soska T, Kriska AM. Objective measures of neighborhood environment and physical activity in older women. Am J Prev Med 2005;28(5):461–469 [DOI] [PubMed] [Google Scholar]
- 38.Zeng Y, Vaupel JW. Functional capacity and self-evaluation of health and life of the oldest-old in China. J Soc Issues 2002;58:733–748 [Google Scholar]
- 39.Chen AJ, Jones G. Aging in ASEAN: Its Socioeconomic Consequences Singapore: Institute of Southeast Asian Studies; 1989 [Google Scholar]
- 40.Lamb VL. Active Life Expectancy of the Elderly in Selected Asian Countries Tokyo, Japan: Nihon University, Population Research Institute; 1999. Research paper 69 [Google Scholar]
- 41.Bell ML, Dominici F. Effect modification by community characteristics on the short-term effects of ozone exposure and mortality in 98 US communities. Am J Epidemiol 2008;167(8):986–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sint T, Donohue JF, Ghio AJ. Ambient air pollution particles and the acute exacerbation of chronic obstructive pulmonary disease. Inhal Toxicol 2008;20(1):25–29 [DOI] [PubMed] [Google Scholar]
- 43.Stige LC, Stave J, Chan KS, et al. The effect of climate variation on agro-pastoral production in Africa. Proc Natl Acad Sci USA 2006;103(9):3049–3053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lobell DB, Burke MB, Tebaldi C, Mastrandrea MD, Falcon WP, Naylor RL. Prioritizing climate change adaptation needs for food security in 2030. Science 2008;319(5863):607–610 [DOI] [PubMed] [Google Scholar]
- 45.Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med 2003;25(3 Suppl 2):129–136 [DOI] [PubMed] [Google Scholar]
- 46.Prüss-Ustün A, Bonjour S, Corvalán C. The impact of the environment on health by country: a meta-synthesis. Environ Health 2008;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]