Abstract
In recognition of the important role that fathers play in the lives of young children in Haiti, a public health organization instituted fathers’ clubs in 1994 as a strategy to improve the health outcomes of children. Fathers’ clubs focus on child and family health education. To evaluate the effectiveness of fathers’ clubs, we examined the health of children born in Haitian villages with and without active fathers’ clubs and compared results for the two groups. The presence of a fathers’ club in a child's birth village had a positive effect on vaccination status, growth monitoring, and vitamin A supplementation after we controlled for socioeconomic status, time, and the quality of the village health agent. Child weights and mortality were not affected by the fathers’ clubs.
IN MANY LOW-RESOURCE countries, child health is unacceptably poor. Children in such countries suffer from high morbidity and mortality that are often caused by preventable diseases.1 Fortunately, affordable, locally designed programs with a broad, integrated approach can improve child health and survival in these circumstances.2–4 One such program is run by the Haitian Health Foundation (HHF), a nongovernmental organization in rural southwestern Haiti. HHF was founded in 1985 as a single clinic in the town of Jérémie, and the organization has since grown to provide outreach in 104 villages. HHF instituted village-level fathers’ clubs as part of its Primary Care Program in 1994, in response to the discovery that in southwestern Haiti, fathers provided a much larger share of child care than was expected.5 The clubs, unique in Haiti, were founded to enhance child health and welfare.
KEY FINDINGS
▪ Enlisting the strengths and abilities of fathers in the improvement of their children's lives is a worthy goal of public health programs worldwide.
▪ The rural fathers’ clubs of the Haitian Health Foundation are a unique public health intervention that shows promise for improving the health of young children and families.
▪ Adapting this program of father involvement for different communities may augment public health efforts in other parts of Haiti and the world.
▪ Public health improvements rely on continued political and economic change that supports local health efforts.
Fathers’ club participants meet regularly to learn about child and family health. They discuss how to best support their wives and mutually care for their children. Fathers’ clubs are run by the men themselves and are open to all men in the village. Health education sessions occur with input from the nurse or village health agent. Education formats include discussion, songs, and skits.
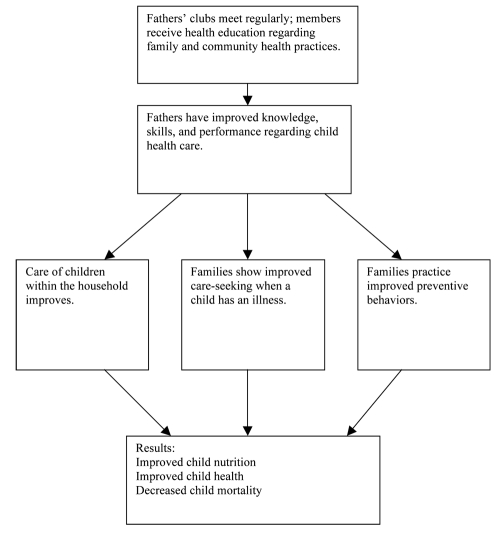
The ultimate goal of the fathers’ clubs is to improve child health through education. The health education provided in the fathers’ clubs is based on the Twelve Key Family Practices identified by the World Health Organization and UNICEF.6 These practices are taught and reinforced in the hope that fathers will institute these practices in their families. The practices include exclusive breastfeeding for 6 months, immunizing children, and providing adequate fluids and seeking appropriate health care when the child is sick. Fathers’ improved knowledge, skills, and performance are expected to improve child health along 3 pathways, as depicted in the intervention impact model shown in Figure 1. HHF developed this model to measure how child health improves over time.
FIGURE 1.
Intervention impact model of how fathers’ clubs lead to improved health for children born in Haiti, 1994–2005.
The specific aims of our study were to document how selected child health indicators have changed for children in particular villages served by HHF since 1988 and to test the hypothesis that child health indicators in a village improve after a fathers’ club is established in that village.
METHODS
HHF maintains centralized computerized data that include information for all Primary Care Program villages and every household in those villages, which allowed us to explore the impact of the fathers’ clubs in the villages. The database is revised and updated regularly and contains individual and household health information. For our study we analyzed data on HHF's original 23 villages, which have had uninterrupted HHF programming since 1988.
For our study, we employed a quasi-intervention design. Because of logistic limitations at HHF, it was not feasible to get a full listing of each of the children born in all 23 villages, so we used a 2-stage sampling strategy to select participants. In the first stage, we randomly selected individual villages and specific years from 1988 through 2005; in the second stage, we randomly selected children born in those villages during the selected years (n = 559 children). All 23 villages had fathers’ clubs, so this sampling method meant that none of the villages were exclusively control villages or intervention villages; instead, we used children from before and after the intervention in each village. Thus, all children who were born before the intervention began in their village served as the control group, and all children born after the intervention began in their village served as the intervention group.
The outcomes we measured were vaccine status, growth monitoring, child weight, vitamin A supplementation, and infant mortality. All outcomes except for mortality were measured at 1 and 2 years of age. Vaccine status was a binary outcome, with children considered fully vaccinated at 1 year of age if they had received 8 specific vaccines (3 diphtheria, pertussis, and tetanus [DPT]; 3 polio; 1 measles; and 1 Bacillus Calmette-Guérin [BCG]); at 2 years of age, full vaccination was 10 vaccines (the previous 8 vaccines plus another DPT and another polio). Vitamin A supplementation was a binary outcome, with children considered fully supplemented if they had received 1 dose by 1 year of age; at 2 years of age, full supplementation was 3 doses. Growth monitoring measured the number of times a child was weighed. Child weights were calculated as weight-for-age z scores.
For analyses, we controlled for 2 factors: the quality of the village health agent, measured using a semisubjective rating,7 and socioeconomic status, measured as a composite score based on the family home's type of roof, type of floor, and number of rooms (scored on the basis of available data). We also accounted for the year of child's birth, which anchored the time of the observed outcomes; this was necessary because fathers’ club start times varied from village to village.
We used logistic regression and multiple linear regression for analysis, with robust standard errors to account for the clustering of children in villages. For each of the outcome variables, we conducted 2 separate regressions: an unadjusted regression and the full model that adjusted for socioeconomic status and the quality of the village health agent.
RESULTS
After adjusting for socioeconomic status and the quality of the village health agent, we found that being born in a village with a fathers’ club had statistically significant positive effects on vaccination status at 1 and 2 years of age, vitamin A supplementation at 1 year of age, and growth monitoring at 1 and 2 years of age (Table 1). Two-year-olds born in villages with fathers’ clubs were 2.6 times more likely to be fully vaccinated than were 2-year-olds born in villages without fathers’ club (odds ratio [OR] = 2.55; 95% confidence interval [CI] = 1.75, 3.71), and children were 3.75 times more likely to receive vitamin A supplementation by 1 year of age when born in a village with a fathers’ club (OR 3.75; 95% CI = 2.07, 6.78). Children had significantly more episodes of growth monitoring in villages with fathers’ clubs. By contrast, being born in a village with a fathers’ club did not improve actual child weights (Table 2) or infant mortality.
TABLE 1.
Effects of Fathers’ Clubs on Vaccination, Vitamin A Supplementation, and Mortality on Children Born in Haiti (n = 559) From 1988–2005
| Unadjusted Regression, OR (95% CI) | Adjusted Regression,a OR (95% CI) | |
| Full vaccination at 1 y of age | 2.25* (1.45, 3.50) | 2.20* (1.40, 3.41) |
| Full vaccination at 2 y of age | 3.69* (2.35, 5.80) | 2.55* (1.75, 3.71) |
| Vitamin A supplementation at 1 y of age | 3.62* (2.01, 6.51) | 3.75* (2.07, 6.78) |
| Vitamin A supplementation at 2 y of age | 0.94 (0.65, 1.37) | 1.03 (0.66, 1.61) |
| Death before 1 y of age | 0.82 (0.34, 1.96) | 0.82 (0.34, 1.97) |
Note. OR = odds ratio; CI = confidence interval.
Adjusted for socioeconomic status and quality of the village health agent.
P < .001.
TABLE 2.
Effects of Fathers’ Clubs on Weight Monitoring and Weight-for-Age z Score on Children Born in Haiti (n = 559) From 1988–2005
| Unadjusted Regression, OR (95% CI) | Adjusted Regression,a OR (95% CI) | |
| No. times weighed by 1 y of age | 2.45* (1.19, 3.71) | 2.43* (1.22, 3.65) |
| No. times weighed by 2 y of age | 3.77* (1.71, 5.83) | 3.81* (1.84, 5.78) |
| Weight-for-age z score at 1 y of age | –0.12 (–0.39, 0.14) | –0.16 (–0.40, 0.08) |
| Weight-for-age z score at 2 y of age | –0.15 (–0.44, 0.15) | –0.17 (–0.49, 0.15) |
Note. OR = odds ratio; CI = confidence interval.
Adjusted for socioeconomic status and quality of the village health agent.
P < .001.
A fathers’ club meets in rural Haiti. Photograph by Elizabeth Sloand.
DISCUSSION
When comparing child health indicators before and after the initiation of fathers’ clubs, we found that children born in villages with fathers’ clubs were significantly more likely to be fully vaccinated at ages 1 and 2 years of age, more likely to have received vitamin A supplementation at 1 year of age, and had closer growth monitoring at 1 and 2 years of age. These results show the potential power of fathers’ clubs to improve the health of children in Haiti. Notably, 61% of children in the HHF villages were fully vaccinated at 1 year of age, regardless of the presence of fathers’ clubs, and 62% of children were fully vaccinated at 2 years of age. These figures are much higher than the 19% national immunization rate at 1 year of age, as recorded by the Demographic and Health Survey.8 The high rate of vaccination in HHF villages points to the success of ongoing efforts by the public health program at HHF.
HAITIAN HEALTH FOUNDATION
▪ The main clinic of the Haitian Health Foundation (HHF), located in the town of Jérémie, is equipped with medical examination suites, a medical laboratory, a pharmacy, a clinical laboratory, a dental operatory, medical and dental radiology capabilities, and sonogram equipment. A second campus in Jérémie provides maternal health care, child health care, a residential malnutrition treatment program, and a maternal waiting home for high-risk women.
▪ Village health agents, trained to provide preventive and basic health care and education, are responsible for health care in 104 villages.
▪ HHF strictly maintains a comprehensively participatory community-based approach in which many decisions are made by the community, including such areas as planning, disease prevention education, community development, utilization of services, and monitoring and evaluation.
▪ HHF encourages and supports more than 200 active community-based organizations, including village health committees, mothers’ and fathers’ clubs, and youth groups. These community-based organizations give their members information on family health and community development to enhance communication, transfer skills, promote adoption of new health practices, teach disease prevention, and support community participation in the provision of health services.
The results for growth monitoring are revealing because that measure is unaffected by supply-side factors—such as medicines and supplies being unavailable because of financial resources, weather, or political instability—which can affect some of the other outcomes. Growth monitoring is noteworthy because it is a pure indication of parental attention to child health: families do not typically receive anything concrete when they bring a child to the village health agent to be weighed, nor do village health agents seek out children to weigh, as they might do with vaccinations. It is also important to note that parents receive age-appropriate health education at growth-monitoring sessions.
All study variables did not show positive results. Actual weights of children and infant mortality—measures that are arguably more important than the more proximal outcomes of growth monitoring, vaccinations, and vitamin A supplementation—did not improve with the intervention. Furthermore, child weights remained flat over the years of the study. Malnutrition is still a major problem in Haiti and continues to contribute to high morbidity and mortality in the first years of life. Malnutri-tion appears resistant to HHF efforts and is instead affected by factors well beyond the scope of a public health services program, such as the underlying conditions of economic deprivation in rural Haiti and the political upheaval that has endured in Haiti for many years.
A mother holds her baby as they wait for health services in rural Haiti. Photograph by Elizabeth Sloand.
Next steps at HHF must address actual weights and malnutrition among children, which are critically important, given the role that malnutrition plays in mortality among children. Malnutrition is a particular concern for children in Haiti and other developing countries, where malnutrition has been found to be an underlying cause of death among children in more than 50% of cases.9–11 One potential strategy to address these problems would be to follow the World Health Organization's recommendation to educate parents about the importance of timely, active, and adequate complementary feeding, particularly during the age range from 6 months through 24 months, when children are most vulnerable to undernutrition.12–14 This recommendation, however, may not be fully feasible, given the economic constraints in many households in developing countries. Further research is needed to develop programs that can be successful within these constraints.12
In conclusion, fathers’ clubs appear to be an effective strategy in child health programs. The success of fathers’ clubs in Haiti may encourage other global efforts to include fathers in a wide range of child health programs that use a community-based participatory approach.
Acknowledgments
Funding was generously provided by the Johns Hopkins Bloomberg School of Public Health Department of Population and Family Health Sciences, and by the Ruth Freeman Memorial Award.
The front image shows two girls walking along the road in southwest rural Haiti. Photograph by Tom Bernadzikowski.
The authors are grateful to the fathers, families, and health care staff of the Haitian Health Foundation, Jérémie, Haiti. Appreciation goes to Kelly Wilson-Fowler, who competently assisted with manuscript preparation and reference management.
Human Participant Protection
This study was approved by the human subjects committee at the Johns Hopkins University Bloomberg School of Public Health and by the appropriate authorities at the Haitian Health Foundation.
References
- 1.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet 2003;361(9376):2226–2234 [DOI] [PubMed] [Google Scholar]
- 2.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. How many child deaths can we prevent this year? Lancet 2003;362(9377):65–71 [DOI] [PubMed] [Google Scholar]
- 3.Bryce J, el Arifeen S, Pariyo G, Lanata C, Gwatkin D, Habicht JP. Reducing child mortality: can public health deliver? Lancet 2003;362(9378):159–164 [DOI] [PubMed] [Google Scholar]
- 4.Perry H, Cayemittes M, Philippe F, et al. Reducing under-five mortality through Hôpital Albert Schweitzer's integrated system in Haiti. Health Policy Plan 2006;21(3):217–230 [DOI] [PubMed] [Google Scholar]
- 5.Devin RB, Erickson PI. The influence of male care givers on child health in rural Haiti. Soc Sci Med 1996;43(4):479–488 [DOI] [PubMed] [Google Scholar]
- 6.Pan American Health Organization Key Family Practices for Healthy Growth and Development Washington, DC; Pan American Health Organization, World Health Organization; 2008 [Google Scholar]
- 7.Gebrian B. Community Participation in Primary Health Care in Rural Haiti: An Ecological Approach [dissertation]. Storrs: University of Connecticut; 1993 [Google Scholar]
- 8.Demographic and Health Surveys Haiti: Standard DHS, 2000. Available at: http://www.measuredhs.com/countries/metadata.cfm?surv_id=155&ctry_id=16&SrvyTp=ctry&cn=Haiti. Accessed February 12, 2009
- 9.Caulfield LE, de Onis M, Blossner M, Black RE. Undernutrition as an underlying cause of child deaths associated with diarrhea, pneumonia, malaria, and measles. Am J Clin Nutr 2004;80(1):193–198 [DOI] [PubMed] [Google Scholar]
- 10.Pelletier DL, Frongillo EA, Jr, Schroeder DG, Habicht JP. The effects of malnutrition on child mortality in developing countries. Bull World Health Organ 1995;73(4):443–448 [PMC free article] [PubMed] [Google Scholar]
- 11.Rice AL, Sacco L, Hyder A, Black RE. Malnutrition as an underlying cause of childhood deaths associated with infectious diseases in developing countries. Bull World Health Organ 2000;78(10):1207–1221 [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization Complementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge Geneva, Switzerland: World Health Organization; 1998 [Google Scholar]
- 13.World Health Organization Nutrition, Infant and Young Child: Complementary Feeding Geneva, Switzerland: World Health Organization; 2007 [Google Scholar]
- 14.Heffelfinger J, Davis T, Gebrian B, Bordeau R, Schwartz B, Dowell S. Evaluation of children with recurrent pneumonia diagnosed by World Health Organization criteria. Pediatr Infect Dis J 2002;21(2):108–112 [DOI] [PubMed] [Google Scholar]