Abstract
Objectives. We assessed change in fruit and vegetable intake in a population-based sample, comparing an online untailored program (arm 1) with a tailored behavioral intervention (arm 2) and with a tailored behavioral intervention plus motivational interviewing–based counseling via e-mail (arm 3).
Methods. We conducted a randomized controlled intervention trial, enrolling members aged 21 to 65 years from 5 health plans in Seattle, Washington; Denver, Colorado; Minneapolis, Minnesota; Detroit, Michigan; and Atlanta, Georgia. Participants reported fruit and vegetable intake at baseline and at 3, 6, and 12 months. We assessed mean change in fruit and vegetable servings per day at 12 months after baseline, using a validated self-report fruit and vegetable food frequency questionnaire.
Results. Of 2540 trial participants, 80% were followed up at 12 months. Overall baseline mean fruit and vegetable intake was 4.4 servings per day. Average servings increased by more than 2 servings across all study arms (P < .001), with the greatest increase (+2.8 servings) among participants of arm 3 (P = .05, compared with control). Overall program satisfaction was high.
Conclusions. This online nutritional intervention was well received, convenient, easy to disseminate, and associated with sustained dietary change. Such programs have promise as population-based dietary interventions.
Accumulating evidence has linked diet to a number of chronic diseases, prompting calls for innovative dietary interventions aimed at increasing intake of fruits and vegetables.1–3 Fewer than 25% of US adults eat 5 servings of fruits and vegetables per day, as recommended by the National Cancer Institute (NCI)4; far fewer meet current guidelines of 5 to 9 servings per day.5,6 Further, intake is disproportionately lower within some sociodemographic groups, such as African Americans, Hispanics, and those with lower education.5,7–9 Reasons for inadequate intake of fruits and vegetables include lack of awareness of recommendations,10 not recognizing the connection between diet and health,11 and perceived difficulty of increasing servings.12
Evidence since the 1990s suggests that computer-tailored interventions can promote healthy eating habits.13–16 The advantages of Internet programs are convenience, relatively low cost of dissemination, and options to incorporate a range of multimedia components (e.g., audio, video) to increase self-paced engagement and appeal to a range of learning styles. Further, content can be individually tailored to personal needs, preferences, and psychological characteristics. Tailored behavior change programs are generally more effective than those with untailored content, in part because they are perceived as more personally relevant and salient.14,16–18
Providing supplemental support through counseling, in addition to online didactic intervention, can augment an intervention's effectiveness,19 especially if counseling includes guided problem-solving and support for participant-generated solutions. This is consistent with the core principles of motivational interviewing,20 a counseling approach that encourages and supports the client's choices. According to recent meta-analyses, motivational interviewing is effective at promoting change across a range of health behaviors,21 including fruit and vegetable consumption.22,23
We designed the present study, Making Effective Nutritional Choices (MENU), to compare the efficacy of (1) a tailored, online dietary intervention program to increase fruit and vegetable intake, (2) this same intervention supplemented with motivational interviewing counseling via e-mail, and (3) an untailored online program. To our knowledge, principles of motivational interviewing have never been applied to counseling delivered via e-mail.
METHODS
This trial was conducted through the Cancer Research Network, a consortium of 14 research organizations affiliated with nonprofit integrated health care delivery systems and the NCI.24 The 5 participating sites were Group Health Cooperative in Washington State, Kaiser Permanente Colorado, HealthPartners in Minnesota, Henry Ford Health System/Health Alliance Plan in Michigan, and Kaiser Permanente Georgia. The Web intervention was developed and maintained in collaboration with the Center for Health Communications Research at the University of Michigan.
Study Population
Using administrative data, each site identified current members aged 21 to 65 years with no evidence of a health condition contraindicating an increase in fruit and vegetable intake. From this list, with oversampling for African Americans in 2 sites and Hispanics in a third site, a random sample of approximately 3000 men and 3000 women was selected from each plan. Over a 7-month period, each site sent an invitation letter to individuals in their subject pool. The letter included eligibility criteria and study details, Web site information, and an incentive $2 bill, along with the promise of $20 for completing each of 3 follow-up online surveys.25 Respondents completed the online eligibility screening, gave informed consent, enrolled, and finished the baseline survey between September 2005 and March 2006. Additional information on the recruitment process has been detailed by Stopponi et al.26
Intervention
The Web-based MENU program content was based on principles from Social Cognitive Theory, the Transtheoretical Model, and the Health Belief Model.27–29 Constructs were incorporated into the tailoring, including motivation to change, specific motives for changing (e.g., health improvement, weight loss, role modeling), barriers to changing (e.g., expense of produce, inadequate cooking skills, disliking the taste), and cues to action (e.g., participants were told to keep produce in sight, program provided recipes).
Participants, who were stratified by health plan, gender, and baseline stage of change (a measure of reported readiness to change, ranging from no intention to change [precontemplative] to already making changes [action]28), were randomly assigned to 1 of 3 experimental arms: an untailored control Web site (arm 1), a tailored Web site (arm 2), or the tailored Web site plus motivational interviewing counseling delivered via e-mail (arm 3). Across all arms, the Web program had the same layout and design and had similar content, which was written at the sixth- to seventh-grade level. On the basis of focus group discussions at the 5 sites,30 functions to make the Web site easy to navigate and practical ways to increase fruit and vegetable intake were integrated into the design and content. The tailored Web site's content matched needs, dietary preferences, and interests expressed in the baseline and 3-month surveys. The control arm provided general fruit and vegetable nutrition information without any tailoring.
For each arm, the Web program was divided into 4 intervention “sessions” offered 1, 3, 13, and 15 weeks after enrollment; automated e-mails notified participants when a new Web site session was available. Each session included 4 to 5 pages of core content, illustrations, optional links to more detailed explanations, and special features designed to supplement session content. For example, special features illustrated serving sizes and nutritional similarities of fresh versus frozen versus canned foods. Another optional feature presented 300 fruit and vegetable–based recipes. Optional short video and audio files were offered to reinforce text on behavioral strategies; audio-only files were available for people unable to access the video clips through their Internet connections. Once available, all program components were accessible throughout the 12-month study period.
Behavioral sessions in arms 2 and 3 were tailored to the participant's stage of change and designed to increase motivation and self-efficacy for eating fruits and vegetables. The welcome page displayed current intake compared with the expanded “goal” intake of 5 to 9 daily servings, and a goal-setting tool was available to aid in planning for change.31
An optional feature offered menus individually tailored by nutrition experts and generated on the basis of participants' fruit and vegetable preferences and dietary restrictions. Additionally, 60-second video clips of recipe preparation by a well-known health-conscious chef, Graham Kerr, were produced by NCI and the Center for Health Communications Research at the University of Michigan, and were available as optional support. Participants in the tailored intervention could also create their own menus from the recipe library.
Participants of arm 3 were assigned to e-mail counseling sessions based on motivational interviewing, which were initiated by a study counselor within a week following a new Web session visit. Counseling was linked to the most current session. Counselors, who were research assistants who had completed a 2-day training session with one of the authors (K. R.) followed by guided practice, used therapeutic principles outlined in motivational interviewing (e.g., allowing ambivalence, expressing empathy, listening reflectively, supporting autonomy).32 Initial exchanges included feedback on current levels of intake and reflection on the participant's plan. Counselors responded to requests for information by referring the participant to the MENU Web site. A maximum of 4 sets of e-mail discussions were offered, coinciding with each of the 4 Web sessions. If a participant failed to respond to an initial e-mail contact, 1 follow-up e-mail was sent; if this produced no response, no further contact was made until (or unless) the participant visited this or the subsequent Web session.
Measures
Two measures of fruit and vegetable intake were used. The primary measure, administered at baseline and 12 months, was a 16-item fruit and vegetable food frequency questionnaire developed by the NCI, which queried frequency and portion size over the past month.33–35 A second short assessment, which appeared first in the survey, was a 2-item measure that included 1 question each asking about total servings of fruits and of vegetables consumed on a typical day.34 This measure was included at baseline and at all follow-up surveys. Guidelines for estimating 1 serving size were included in the 2-item questions (e.g., 1 piece of fruit, 3/4 cup of 100% juice, 1/2 cup canned fruit, or 1/4 cup dried fruit) to improve validity.36 At 12 months, response options were expanded to 0 to 8 or more servings for both single items, but for analyses these were truncated at 4 servings (fruit) and 5 servings (vegetable) to match the categories of 0, 1, 2, 3, 4, or more servings of fruits and 0, 1, 2, 3, 4, 5, or more servings of vegetables offered on preceding surveys. The validity of these scales has been previously reported.33,34 The 16-item measure tends to overestimate true values, and the 2-item measure slightly underestimates them.37 Participants provided self-reported data on demographics, medical history, and psychosocial constructs relevant to dietary behavior.
Follow-up assessments were completed online 3, 6, and 12 months after enrollment. A presurvey mailed letter and automated e-mail reminders alerted participants of the upcoming survey and offered an incentive for completion. A 38-day window was allowed for completing the 3- and 6-month surveys, and 60 days was allowed for the 12-month survey.
Statistical Methods
We assessed baseline equality of study groups with a two-tailed t test, a Wilcoxon rank sum test, and a χ2 test. Reported serving totals greater than 10 for either fruits or vegetables, assessed by the 16-item measure, were considered implausible and classified as missing data. Participants were included in the analysis using the 16-item measure if they answered at least 1 question per category.
Formal tests for study arm effects were based on the log transformation of the 16-item responses, and their sums were used as primary outcome measures. For ease of interpretation, means and standard deviations on the original assessment scale are presented.38 The secondary outcome was the 2-item measure, and its sums were analyzed on the original scale. Baseline correlation between the 16-item and the 2-item measures was 0.60 (P < .001). Cohen's d was computed to assess meaningful differences within and between arms.39 Cohen suggests that values of 0.2, 0.5, and 0.8 can be regarded as small, medium, and large effect sizes, respectively.
We planned 2 tests for intervention effects using the main outcome 16-item measure: (1) untailored versus tailored only and (2) untailored versus tailored plus motivational interviewing via e-mail, with a Hochberg multiple comparisons adjustment.40 The Hochberg adjustment requires that if P < .05 for only 1 comparison, it must be equal to or less than .025 for significance. Secondary analyses did not include multiple comparison adjustments. Although the original analysis plan called for Wilcoxon rank sum tests for the 2 primary comparisons, analysis of covariance was used instead to adjust for a baseline imbalance by arm in the 16-item fruit and vegetable outcome. For dichotomous goal attainment outcomes, logistic regression was used with baseline status as a covariate.
Sample size estimates assumed an overall intervention effect of 0.6 servings at 12 months, with one third of the increment (0.2 servings) seen between arms 2 and 3 and an increase of 0.4 servings between arms 1 and 2. Power calculations were based on t tests and a standard deviation of 1.2 for change in servings. To detect a 0.2-serving difference with 80% power and α = 0.05 (i.e., assuming the first comparison was significant in the Hochberg analysis), a net sample size of 567 per group was required. Assuming 25% loss to follow-up, at least 2127 enrolled subjects would be required. To ensure power at greater attrition levels, 2500 enrollees was the target enrollment.
RESULTS
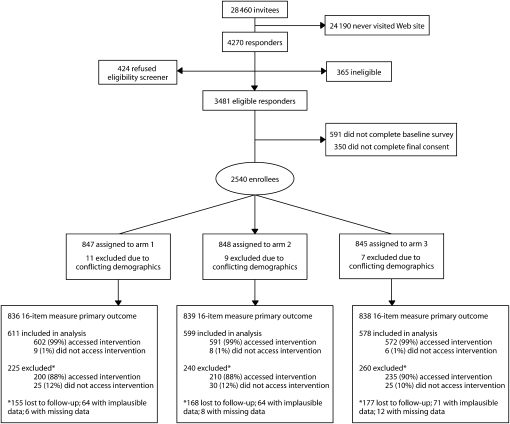
Of 28 460 people invited, 4270 (15%) signed on to the study Web site and 2540 (8.9%) participated (Figure 1). Data were dropped for 27 participants whose baseline and follow-up responses were inconsistent on key factors (e.g., gender, birth date), yielding 2513 participants. Women and minority members made up 69% and 32% of enrollees, respectively (Table 1). Mean age (46.3 years; SD = 10.8) and distribution by gender, race/ethnicity, and living status (married or living with a partner) were virtually identical across arms. Half (50%) reported education as high school or less than a college degree and half had a college or postcollege degree. Half (50%) were in the “contemplation” stage of change, 20% were in “preparation,” 21% were in “maintenance,” and 7% had recently become “active” in reaching minimum fruit goal intake.28
FIGURE 1.
Flow chart of recruitment and retention: Making Effective Nutritional Choices (MENU) study, 2005–2006.
TABLE 1.
Baseline Description of Participants Enrolled in an Online Intervention to Improve Fruit and Vegetable Consumption, by Study Arm: Making Effective Nutritional Choices (MENU) Study, 2005–2006
| Variable | Total (n = 2513) | Arm 1 (n = 836) | Arm 2 (n = 839) | Arm 3 (n = 838) |
| Age, y, mean (SD); median | 46.3 (10.8); 48.0 | 46.1 (10.6); 47.0 | 46.5 (10.8); 48.0 | 46.4 (10.9); 47.0 |
| Female, no. (%) | 1729 (69) | 576 (69) | 577 (69) | 576 (69) |
| African American, no. (%) | 585 (24) | 192 (23) | 196 (24) | 197 (24) |
| Hispanic, no. (%) | 192 (8) | 69 (8) | 66 (8) | 57 (7) |
| Married or with partner, no. (%) | 1805 (72) | 595 (72) | 602 (72) | 609 (73) |
| Education, no. (%) | ||||
| High school education or less | 217 (9) | 76 (9) | 70 (8) | 71 (9) |
| Associate degree or some college | 1023 (41) | 334 (40) | 352 (42) | 337 (40) |
| College degree | 659 (26) | 219 (26) | 232 (28) | 208 (25) |
| Postbachelor education | 607 (24) | 205 (25) | 183 (22) | 219 (26) |
| Stage of change | ||||
| Fruit, no. (%) | ||||
| Precontemplation | 49 (2) | 17 (2) | 14 (2) | 18 (2) |
| Contemplation | 1247 (50) | 412 (49) | 421 (50) | 414 (49) |
| Preparation | 511 (20) | 164 (20) | 175 (21) | 172 (21) |
| Action | 170 (7) | 54 (6) | 61 (7) | 55 (7) |
| Maintenance | 533 (21) | 189 (23) | 166 (20) | 178 (21) |
| Vegetable, no. (%) | ||||
| Precontemplation | 40 (2) | 11 (1) | 17 (2) | 12 (1) |
| Contemplation | 1547 (62) | 519 (62) | 523 (62) | 505 (60) |
| Preparation | 389 (15) | 128 (15) | 124 (15) | 137 (16) |
| Action | 104 (4) | 35 (4) | 35 (4) | 34 (4) |
| Maintenance | 430 (17) | 143 (17) | 138 (16) | 149 (18) |
| Fruit and vegetable servings/day,a16-item measure,b mean (SD); median | 4.4 (2.8); 3.8 | 4.6 (3.0); 3.9 | 4.2 (2.7); 3.6 | 4.5 (2.7); 4.0 |
| Fruits and vegetables servings/day,2-item measure,c mean (SD); median | 3.3 (1.6); 3.0 | 3.3 (1.6); 3.0 | 3.2 (1.6); 3.0 | 3.4 (1.6); 3.0 |
Note. Arm 1 was the control, arm 2 was a tailored behavioral intervention, and arm 3 was a tailored behavioral intervention plus motivational interviewing via e-mail.
By the Kruskal–Wallis test, the intake levels by arm were statistically significantly different (P = .049).
A 16-item fruit and vegetable food frequency questionnaire developed by the National Cancer Institute that queried frequency and portion size over the past month.
A short, 2-item measure that included 1 question each asking about total servings of fruits and of vegetables consumed on a typical day.
Overall, the baseline daily mean fruit and vegetable intake was 4.4 servings (SD = 2.8) by the 16-item measure and 3.3 (SD = 1.6) by the 2-item measure (Table 1). Despite randomization, statistically significant differences were found in reported fruit and vegetable intake at baseline by study arm when the 16-item measure was used, with fewer servings in arm 2.
Follow-up participation rates were 86% at 3 months, 80% at 6 months, and 80% at 12 months. Of the 2513 enrollees, 99.9% provided complete 2-item baseline responses and 97% provided complete 16-item baseline responses. For analysis, 80% provided usable 2-item survey data at both baseline and 12 months, and 71% provided usable 16-item survey data at both assesments. Of the 725 participants missing the 16-item assessments, 10% at baseline and 20% at 12 months were excluded because of implausibly high reported fruit and vegetable servings and 70% did not complete both the baseline and the 12-month assessments.
Response rates for participants with complete 16-item data were 73% for arm 1, 71% for arm 2, and 69% for arm 3 (P = .18). Proportions of those completing both assessments differed significantly (P < .05) from the baseline-only participants by location (ranging from 60%–79% by site), age (for < 30 years, 68%; for ≥ 60 years, 75%), gender (74% for women; 66% for men), race (77% for Whites versus 59% for African Americans, and 58% for Hispanics versus 72% for non-Hispanics), education (78% for postcollege versus 61% for high school or vocational school), and baseline fruit and vegetable servings as assessed by the 2-item measure (3.4 servings versus 3.2 servings). Stage of change for eating recommended servings of vegetables varied (P < .05): of baseline participants, 80% of those in the precontemplation stage were in the final analytic data set, compared with 73% of contemplators, 70% of maintainers, 66% of preparers, and 62% in the “action” stage; no statistical difference in response was seen by baseline stage of change for fruit (P = .13).
The number of responses per person to counselor-initiated e-mails ranged from 0 to 17 (mean = 6). Participation rate in e-mail support exchanges in arm 3 varied, with 22% having no exchanges, 29% having 1 to 3, 17% having 4 to 8, and 33% having 9 or more. Counselors limited their e-mail messages to 2 short paragraphs; the length of participant-sent messages ranged from a single sentence to several paragraphs.
At 12 months, average fruit and vegetable servings increased by more than 2 servings across each arm, as assessed by the 16-item measure (Table 2). The adjusted mean change was statistically greater for arm 3 participants (+2.80 servings) than for control participants (+2.34 servings) (P = .025, or P = .050 after the Hochberg adjustment). There was no statistical difference between arms 1 and 2 (P = .177) or arms 2 and 3 (P = .37). Cohen's effect sizes (0.6–0.8) indicate medium to large within-arm changes relative to small effect sizes (0.04–0.10) for between-arm differences.
TABLE 2.
Mean Fruit and Vegetable Servings Per Day at 12 Months Versus Baseline, by Outcome Measure and Study Arm: Making Effective Nutritional Choices (MENU) Study, 2005–2006
| 16-Item Measurea |
2-Item Measureb |
|||||||||||||||||
| Servings at Baseline, No. (SD) | Servings at 12 Months, No. (SD) | Adjusted No. at 12 Monthsc | Cohen d |
Servings at Baseline No. (SD) | Servings at 12 Months, No. (SD) | Adjusted No. at 12 Monthsc | Adjusted Mean Changed | Cohen d |
||||||||||
| Study Arm | No. at baseline | No. at 12 Months | Adjusted Mean Changed | P e | Within Arm | Compared With Arm 1 | No. at baseline | No. at 12 Months | P e | Within Arm | Compared With Arm 1 | |||||||
| Arm 1 | 818 | 4.57 (2.9) | 619 | 6.83 (3.5) | 611 | 2.34 | … | 0.6 | … | 836 | 3.28 (1.6) | 681 | 5.71 (1.8) | 681 | 2.38 | … | 1.3 | … |
| Arm 2 | 812 | 4.23 (2.7) | 613 | 6.98 (3.7) | 599 | 2.68 | .177 | 0.8 | 0.04 | 837 | 3.24 (1.6) | 671 | 5.85 (1.8) | 669 | 2.55 | .05 | 1.5 | 0.08 |
| Arm 3 | 811 | 4.46 (2.7) | 588 | 7.18 (3.4) | 578 | 2.80 | .050f | 0.8 | 0.10 | 837 | 3.35 (1.6) | 661 | 5.93 (1.8) | 661 | 2.55 | .042 | 1.4 | 0.13 |
| Total | 2411 | 1820 | 1788 | 2510 | 2013 | 2011 | ||||||||||||
Note. Arm 1 was the control, arm 2 was a tailored behavioral intervention, and arm 3 was a tailored behavioral intervention plus motivational interviewing via e-mail. At 12 months, all within-arm changes in fruit and vegetable servings from baseline are statistically significant (P < .001).
A 16-item fruit and vegetable food frequency questionnaire developed by the National Cancer Institute that queried frequency and portion size over the past month.
A short, 2-item measure that included 1 question each asking about total servings of fruits and of vegetables consumed on a typical day.
Adjusted numbers indicate participants who completed both baseline and 12-month data.
Adjusted for baseline serving intake.
P values are comparisons of arm 1 with arm 2 or of arm 1 with arm 3.
Adjusted change: 16-item measure comparison P values based on log scale comparisons, using Hochberg multiple comparisons adjustment as well as adjusting for baseline servings; original P value was .025 for arm 3 versus arm 1.
When the 2-item measure was used, with more complete follow-up data and adjusting for baseline servings, fruit and vegetable intake increased in the tailored arm (arm 2; P = .05) and in the tailored plus e-mail counseling arm (arm 3; P = .04); both of these arms increased by an average 2.55 servings compared with 2.38 servings for the control group (Table 2). When the 2-item measure was used, the proportion of participants within study arms eating 5 or more fruit and vegetable servings daily ranged from 20% to 22% at baseline to 67% to 75% at the 3-month assessment (P < .001; Table 3). These gains were sustained at 6 and 12 months. At follow-up, 85% to 92% of participants reached minimum fruit intake goals and 59% to 73% met minimum vegetable intake goals; differences between arms were most pronounced at 3 and 6 months. For fruits alone, statistically significant differences between the arms remained at 12 months. The intervention effect was smaller but similar for vegetables, but results were imprecise at final follow-up, presumably because of lower statistical power.
TABLE 3.
Comparison of Fruit and Vegetable Consumption Levels Over Time Using the 2-Item Measure, by Study Arm: Making Effective Nutritional Choices (MENU), 2005–2006
| Baseline |
3 Months |
6 Months |
12 Months |
Average of 3, 6, and 12 Months |
12 Months Only |
|||||||||||
| Serving Intake | Arm 1, No. (%) | Arm 2, No. (%) | Arm 3, No. (%) | Arm 1, No. (%) | Arm 2, No. (%) | Arm 3, No. (%) | Arm 1, No. (%) | Arm 2, No. (%) | Arm 3, No. (%) | Arm 1, No. (%) | Arm 2, No. (%) | Arm 3, No. (%) | Arm 1 vs Arm 2, Pa | Arm 1 vs Arm 3, Pa | Arm 1 vs Arm 2, Pa | Arm 1 vs Arm 3, Pa |
| ≥ 5 fruits and vegetables | 173 (21) | 165 (20) | 181 (22) | 491 (67) | 509 (70) | 533 (75) | 496 (72) | 508 (77) | 528 (80) | 509 (75) | 524 (78) | 516 (78) | .028 | .001 | .103 | .0193 |
| ≥ 2 fruits | 354 (42) | 349 (42) | 344 (41) | 628 (85) | 634 (87) | 625 (88) | 611 (89) | 591 (90) | 605 (92) | 592 (87) | 602 (90) | 596 (90) | .130 | .017 | .071 | .046 |
| ≥ 3 vegetables | 185 (22) | 185 (22) | 207 (25) | 431 (59) | 453 (62) | 470 (66) | 435 (63) | 459 (70) | 479 (73) | 472 (70) | 485 (72) | 475 (72) | .008 | .003 | .205 | .445 |
Note. Arm 1 was the control, arm 2 was a tailored behavioral intervention, and arm 3 was a tailored behavioral intervention plus motivational interviewing via e-mail. All within-arm changes from baseline are significant (P < .001). Total number of participants was n = 2011. The 2-item questionnaire included 1 question each asking about total servings of fruits and of vegetables consumed on a typical day.
P values are from generalized estimating equation logistic regression models adjusting for baseline status.
Assessment of frequency of Web site visits across the duration of the study demonstrated that increases in fruit and vegetable servings corresponded with more visits, regardless of arm; mean daily intake increased by 2.2, 2.4, and 3.0 servings for participants who visited infrequently (< 7 Web site visits), moderately often (7–13 visits), and very often (> 13 visits), respectively (P < .001) (data not shown). Program satisfaction assessments at 6 and 12 months, regardless of arm, revealed that 95% of respondents rated the program as “very good” to “excellent”; in addition, 90% reported that they would recommend the program to others and that involvement of family and others had increased over time.
DISCUSSION
The MENU online program was designed to provide a large, geographically and demographically diverse sample of generally healthy adults with practical health promotion strategies for a single eating behavior, using an accessible, convenient, and engaging medium. The main outcomes were assessed at 12 months to ensure that observed dietary changes persisted over time and were not caused by seasonal fluctuations in diet.
A significant increase in fruit and vegetable servings was seen in all 3 intervention groups, as observed by other investigators of online interventions.41 A greater effect was found for the tailored plus e-mail counseling arm when the 16-item measure was used and was suggested for both tailored intervention arms when the 2-item measure was used. Additionally, the percentage reaching the traditional goal of “5-a-day”4 nearly tripled at the first follow-up and was maintained over the duration of the study, regardless of arm. The control arm was an attractive, well-designed Web site that, although not tailored, was obviously also appealing and effective.
This trial was initiated when more ambitious dietary intake goals for fruits and vegetables were being publicized nationally (7 servings daily for women, 9 for men, and 6 for those older than 50 years).1 Although the investigators were concerned that the more ambitious recommendations would threaten efforts to reach higher guidelines, they may have actually inspired participants to enroll and take advantage of this program. A number of elements proven effective by other Internet interventions were used, including goal setting and display of current behavior along with the intake goal.15,31
With the majority of enrollees being “contemplators” or “preparers”28 and fewer than 25% of enrollees reporting that they met the traditional 5-a-day minimum intake, the program attracted people who had room to improve, approximating the dietary pattern of the general population.4 As in other dietary Internet-based interventions, women enrolled at a rate twice that of men,15 possibly because women have a greater role in shopping and preparing food and pay greater attention to nutrition.30
An advantage of online interventions is the ability to observe how often participants connect to the materials. Like other online trials,14,41,42 increasing the amount of time spent with the sessions enhanced behavior change, further supporting findings that dose matters with Web-based interventions.
Participants' overall rate of returning to the Web site at 12 months was 80%, similar to that of other Web-based interventions.42 As with other reports,15,43 those enrolling and staying with the program were more likely to be women, to be older than 50 years, to be from a nonminority ethnic group, and to have a higher level of education. Although the connection between food and health or disease may have appealed to older adults as they faced more health challenges, the fact that they enrolled and remained in this online program was something of a surprise. Younger adults may be more familiar with software and computer programs; however, they may also be less motivated.
Satisfaction with the program remained high, and participants reported sharing the information with others in their household, regardless of study arm, suggesting that the intervention had appeal and was useful. Family members reportedly became more involved from midyear to end of year, which may have contributed to the durability of increased fruit and vegetable servings over time. This sustained behavior pattern is in contrast to other behavior change outcomes in which attrition of behavior is reported.19
The strengths of this study were its randomized design, long-term follow-up, high retention rates throughout the 12-month study period, participant diversity, and appeal to individuals with suboptimal fruit and vegetable intake. Limitations included eligibility being restricted to those with Internet access and weekly e-mail use and loss to follow-up through dropping out and implausible data. We acknowledge a probable volunteer bias caused by the self-initiated, voluntary enrollment of people motivated to participate, which varied by gender, race/ethnicity, and other characteristics, limiting generalizability to other large US minority groups such as Hispanics; however, because of randomization and high follow-up, internal validity was optimized. Just as focus groups were used prior to our intervention to identify factors appealing to generally healthy adults,30 more formative work is needed to guide recruitment, retention, and interventions that specifically target and are adapted to population subgroups, including minority populations,44 young adults,45 men,46 and those with lower educational attainment.
All intake measures were self-reported and contained no clinical or biological markers to verify intake47; however, recent analyses have shown acceptable reliability of self-report measures of fruit and vegetable intake.37 An improvement in the reliability of self-reported fruit and vegetable intake is noted when serving sizes are clarified, as was done for the 2-item measure survey.36 The possibility that participants might have become acquainted with cup-size servings and intake goals through the program may have affected responses over time,48 but this would not bias comparisons between study arms.
It was not possible to determine which specific optional components of the online intervention sessions had the most effect. Measurement and analysis of component use on outcomes may prove useful in future projects.49 Finally, because the study did not include a fourth intervention arm providing motivational interviewing e-mail alone without the tailored Web site, we are unable to definitively discriminate between the potential overlapping effects of the 2 interventions compared with a control arm that was more efficacious than was expected.
The results of this study contribute to the growing body of literature on the extent to which health behavior changes may be initiated and sustained with the assistance of an online program. If patients, health plan members, or any of the more than 73% of US adults who are using the Internet50 are interested in improving their fruit and vegetable intake, dramatic, rapid, and prolonged improvement can be attained through the use of a well-designed, contemporary, and appealing Web-based program. Once developed, such a program can be delivered to an unlimited number of individuals for relatively little cost.
Acknowledgments
This study was supported by the Cancer Research Network (grant U19 CA079689) with funding from the National Cancer Institute.
We are indebted to the participants in MENU Choices and to the research team for their contributions to this trial, including the following: Linda Shultz, MPH, Julie Richards, MPH, and Roy Pardee, MA, from Group Health; Nikki Carroll, MS, Anna Sukhanova, MA, Candido A. Chacon III, Mary Kershner, RN, BSN, Judy Mouchawar, MD, and Debra P. Ritzwoller, PhD, from Kaiser Permanente Colorado; Mary Kelley and Kristine Fortman, PhD, from HealthPartners; Sarah Claud Zweig, MPH, Margie Day, Richard Krajenta, BS, Nancy Oja-Tebbe, BS, and Noel Maddy from Henry Ford Hospital and Health System; Roslin Nelson from Kaiser Permanente Georgia; Janine Konkel, MPH, Ed Saunders, MS, Mike Nowak, MS, and Carola Carlier, MSW, from the University of Michigan; and Rachel Ballard-Barbash, MD, from the National Cancer Institute.
Human Participant Protection
This study was approved by institutional review boards from the 5 participant research sites and the University of Michigan, the site of the online program development and maintenance.
References
- 1.Dietary Guidelines for Americans Washington, DC: US Dept of Health and Human Services, US Dept of Agriculture; 2005:1–84 [Google Scholar]
- 2.Hung HC, Joshipura KJ, Jiang R, et al. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst 2004;96(21):1577–1584 [DOI] [PubMed] [Google Scholar]
- 3.He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet 2006;367(9507):320–326 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Prevalence of Fruit and Vegetable Consumption. Behavioral Risk Factor Surveillance System Survey Data. 2007. Atlanta, GA, Department of Health and Human Services; Available at: http://www.cdc.gov/brfss. Accessed October 20, 2008 [Google Scholar]
- 5.Casagrande SS, Wang Y, Anderson C, Gary TL. Have Americans increased their fruit and vegetable intake? The trends between 1988 and 2002. Am J Prev Med 2007;32(4):257–263 [DOI] [PubMed] [Google Scholar]
- 6.Reeves MJ, Rafferty AP. Healthy lifestyle characteristics among adults in the United States, 2000. Arch Intern Med 2005;165(8):854–857 [DOI] [PubMed] [Google Scholar]
- 7.Kant AK, Graubard BI, Kumanyika SK. Trends in black–white differentials in dietary intakes of US adults, 1971–2002. Am J Prev Med 2007;32(4):264–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Serdula MK, Gillespie C, Kettel-Khan L, Farris R, Seymour J, Denny C. Trends in fruit and vegetable consumption among adults in the United States: behavioral risk factor surveillance system, 1994–2000. Am J Public Health 2004;94(6):1014–1018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Potter JD. Vegetables, fruit, and cancer. Lancet 2005;366(9485):527–530 [DOI] [PubMed] [Google Scholar]
- 10.Stables GJ, Subar AF, Patterson BH, et al. Changes in vegetable and fruit consumption and awareness among US adults: results of the 1991 and 1997 5 A Day for Better Health Program surveys. J Am Diet Assoc 2002;102(6):809–817 [DOI] [PubMed] [Google Scholar]
- 11.Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Ann Behav Med 2007;34(3):304–312 [DOI] [PubMed] [Google Scholar]
- 12.Campbell MK, Reynolds KD, Havas S, et al. Stages of change for increasing fruit and vegetable consumption among adults and young adults participating in the national 5 A Day for Better Health community studies. Health Educ Behav 1999;26(4):513–534 [DOI] [PubMed] [Google Scholar]
- 13.Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M. Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res 2006;8(2):e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strecher V. Internet methods for delivering behavioral and health-related interventions (eHealth). Annu Rev Clin Psychol 2007;3:53–76 [DOI] [PubMed] [Google Scholar]
- 15.Oenema A, Brug J, Lechner L. Web-based tailored nutrition education: results of a randomized controlled trial. Health Educ Res 2001;16(6):647–660 [DOI] [PubMed] [Google Scholar]
- 16.Brug J, Campbell M, van Assema P. The application and impact of computer-generated personalized nutrition education: a review of the literature. Patient Educ Couns 1999;36(2):145–156 [DOI] [PubMed] [Google Scholar]
- 17.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull 2007;133(4):673–693 [DOI] [PubMed] [Google Scholar]
- 18.Hawkins RP, Kreuter M, Resnicow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res 2008;23(3):454–466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA 2003;289(14):1833–1836 [DOI] [PubMed] [Google Scholar]
- 20.Miller W, Rolnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior New York, NY: Guilford Press; 1991 [Google Scholar]
- 21.Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol 2005;1:91–111 [DOI] [PubMed] [Google Scholar]
- 22.Resnicow K, Jackson A, Wang T, et al. A motivational interviewing intervention to increase fruit and vegetable intake through black churches: results of the Eat for Life trial. Am J Public Health 2001;91(10):1686–1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Resnicow K, Jackson A, Blissett D, et al. Results of the healthy body healthy spirit trial. Health Psychol 2005;24(4):339–348 [DOI] [PubMed] [Google Scholar]
- 24.Wagner EH, Greene SM, Hart G, et al. Building a research consortium of large health systems: the Cancer Research Network. J Natl Cancer Inst Monogr 2005;(35):3–11 [DOI] [PubMed] [Google Scholar]
- 25.Alexander GL, Divine GW, Couper MP, et al. Effect of incentives and mailing features on online health program enrollment. Am J Prev Med 2008;34(5):382–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stopponi MA, Alexander GL, McClure JB, et al. Recruitment to a Web-based nutrition intervention trial. J Med Internet Res 2009:11(3):e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol 2001;52:1–26 [DOI] [PubMed] [Google Scholar]
- 28.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12(1):38–48 [DOI] [PubMed] [Google Scholar]
- 29.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q 1984;11(1):1–47 [DOI] [PubMed] [Google Scholar]
- 30.Rolnick SJ, Calvi J, Heimendinger J, et al. Focus groups inform a Web-based program to increase fruit and vegetable intake. Patient Educ Couns 2009;77(2):314–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwarzer R, Schuz B, Ziegelmann JP, Lippke S, Luszczynska A, Scholz U. Adoption and maintenance of four health behaviors: theory-guided longitudinal studies on dental flossing, seat belt use, dietary behavior, and physical activity. Ann Behav Med 2007;33(2):156–166 [DOI] [PubMed] [Google Scholar]
- 32.Resnicow K, DiIorio C, Soet JE, Ernst D, Borrelli B, Hecht J. Motivational interviewing in health promotion: it sounds like something is changing. Health Psychol 2002;21(5):444–451 [PubMed] [Google Scholar]
- 33.Thompson FE, Subar AF, Smith AF, et al. Fruit and vegetable assessment: performance of 2 new short instruments and a food frequency questionnaire. J Am Diet Assoc 2002;102(12):1764–1772 [DOI] [PubMed] [Google Scholar]
- 34.Resnicow K, Odom E, Wang T, et al. Validation of three food frequency questionnaires and 24-hour recalls with serum carotenoid levels in a sample of African-American adults. Am J Epidemiol 2000;152(11):1072–1080 [DOI] [PubMed] [Google Scholar]
- 35.Peterson KE, Hebert JR, Hurley TG, et al. Accuracy and precision of two short screeners to assess change in fruit and vegetable consumption among diverse populations participating in health promotion intervention trials. J Nutr 2008;138(1):218S–225S [DOI] [PubMed] [Google Scholar]
- 36.Bensley L, Van EJ, Bruemmer BA. Measuring fruit and vegetable consumption: providing serving size information doubles estimated percent eating five per day. J Am Diet Assoc 2003;103(11):1530–1532 [DOI] [PubMed] [Google Scholar]
- 37.Greene GW, Resnicow K, Thompson FE, et al. Correspondence of the NCI Fruit and Vegetable Screener to repeat 24-H recalls and serum carotenoids in behavioral intervention trials. J Nutr 2008;138(1):200S–204S [DOI] [PubMed] [Google Scholar]
- 38.Vittinghoff E, Shiboski SC, Glidden DV, McCulloch CE. Regression Methods in Biostatistics: Linear, Logistic, Survival, and Repeated Measures Models New York, NY: Springer; 2005 [Google Scholar]
- 39.Cohen JA. Power primer. Psychol Bull 1992;112(1):155–159 [DOI] [PubMed] [Google Scholar]
- 40.Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika 1988;75(4):800–802 [Google Scholar]
- 41.Cook RF, Billings DW, Hersch RK, Back AS, Hendrickson A. A field test of a Web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: randomized controlled trial. J Med Internet Res 2007;9(2):e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of Web-based vs non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res 2004;6(4):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Verheijden MW, Jans MP, Hildebrandt VH, Hopman-Rock M. Rates and determinants of repeated participation in a Web-based behavior change program for healthy body weight and healthy lifestyle. J Med Internet Res 2007;9(1):e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Resnicow K, Davis RE, Strecher VJ, et al. Tailoring a fruit and vegetable intervention on ethnic identity: results of a randomized study. Health Psychol 2009;28(4):394–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Park A, Nitzke S, Kritsch K, et al. Internet-based interventions have potential to affect short-term mediators and indicators of dietary behavior of young adults. J Nutr Educ Behav 2008;40(5):288–297 [DOI] [PubMed] [Google Scholar]
- 46.Dumbrell S, Mathai D. Getting young men to eat more fruit and vegetables: a qualitative investigation. Health Promot J Austr 2008;19(3):216–221 [DOI] [PubMed] [Google Scholar]
- 47.Subar AF, Kipnis V, Troiano RP, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol 2003;158(1):1–13 [DOI] [PubMed] [Google Scholar]
- 48.Hebert JR, Hurley TG, Peterson KE, et al. Social desirability trait influences on self-reported dietary measures among diverse participants in a multicenter multiple risk factor trial. J Nutr 2008;138(1):226S–234S [DOI] [PubMed] [Google Scholar]
- 49.Danaher BG, Boles SM, Akers L, Gordon JS, Severson HH. Defining participant exposure measures in Web-based health behavior change programs. J Med Internet Res 2006;8(3):e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Evers KE. eHealth promotion: the use of the Internet for health promotion. Am J Health Promot 2006;20(4):1–7 [DOI] [PubMed] [Google Scholar]