Abstract
Objectives. We assessed the effects of prior military service in Iraq or Afghanistan on the health of New Jersey Army National Guard members preparing for deployment to Iraq.
Methods. We analyzed anonymous, self-administered predeployment surveys from 2543 National Guard members deployed to Iraq in 2008. We used bivariate and multivariate analyses to measure the effects of prior service in Afghanistan (Operation Enduring Freedom [OEF]) or Iraq (Operation Iraqi Freedom [OIF]) on mental and physical health.
Results. Nearly 25% of respondents reported at least 1 previous OEF or OIF deployment. Previously deployed soldiers were more than 3 times as likely as soldiers with no previous deployments to screen positive for posttraumatic stress disorder (adjusted odds ratio [AOR] = 3.69; 95% confidence interval [CI] = 2.59, 5.24) and major depression (AOR = 3.07; 95% CI = 1.81, 5.19), more than twice as likely to report chronic pain (AOR = 2.20; 95% CI = 1.78, 2.72) and more than 90% more likely to score below the general population norm on physical functioning (AOR = 1.94; 95% CI = 1.51, 2.48).
Conclusions. Repeated OEF and OIF deployments may adversely affect the military readiness of New Jersey National Guard combat soldiers.
The mental and physical health consequences of service in Afghanistan (Operation Enduring Freedom [OEF]) and Iraq (Operation Iraqi Freedom [OIF]) have been well documented. Studies report rates of posttraumatic stress disorder (PTSD) among returning soldiers ranging from 4%1 to 31%2 and rates of depression ranging from 3%3 to 25%,4 with rates varying by diagnostic criteria, military population, deployment location, and time since deployment. Traumatic brain injury has been identified in 19% of returning troops.5 Those experiencing multiple deployments are most at risk, with the Office of the US Army Surgeon General6 reporting mental health problems in 11.9% of those with 1 deployment, 18.5% with 2 deployments, and 27.2% with 3 or 4 deployments. National Guard and Reserve troops are more vulnerable than active-duty troops, with 35.5% of Guard and Reserve troops at mental health risk 6 months after deployment compared with 27.1% of active-duty soldiers.7 With respect to physical health, the OEF and OIF conflicts have produced the highest ratio of wounded to killed of any previous military operation (approximately 7:1), with over 33 170 wounded in action as of October 2008.8 Orthopedic injuries are the most common class of injury9 and pain one of the most frequently reported symptoms.10,11
Although the adverse health consequences of service in OEF and OIF have focused public attention on the medical needs of returning veterans, concern has also centered on the military readiness of our fighting force, given the unprecedented pattern of repeat deployments unique to this particular conflict. Of all soldiers deployed to Iraq since 2003, approximately 38% have been deployed more than once and 10% have been deployed 3 times or more.12 The Department of Defense and state National Guard authorities conduct extensive pre- and postdeployment screenings to ensure that only “healthy and medically prepared”13 soldiers are deployed to combat. However, because most studies of veterans of OEF and OIF to date have focused on postdeployment populations, we have little information about the effectiveness of military programs in screening seriously impaired soldiers out of the eligibility pool for future deployment. Postdeployment studies, moreover, are likely to include many medically compromised soldiers who were subsequently disqualified from, or voluntarily left, active military service before being recalled to duty. In the absence of large-scale predeployment health studies, we have no information on the effect of multiple deployments on the fitness of soldiers returning to combat. The 1 published study identified by the authors to date that examined predeployment health status7 included a small sample of combat veterans (n = 173) with mixed histories of previous service: some had served in Afghanistan, some in conflicts other than OEF and OIF, but none in Iraq, even though, until recently, Iraq war veterans experienced substantially greater combat stress than veterans from Afghanistan.14
We explored the effects of multiple deployments on the mental and physical health of New Jersey Army National Guard troops preparing for deployment to Iraq. Specifically, we (1) compared the health status of soldiers with previous OEF and OIF deployments with that of soldiers experiencing their first deployment, (2) examined associations between deployment status and health after controlling for possible confounding factors, and (3) compared the present survey with New Jersey's predeployment health assessment on identification rates of key mental health problems.
METHODS
Our survey sampled 2665 of the 2995 New Jersey National Guard members undergoing predeployment medical assessments in preparation for deployment to Iraq in the summer of 2008. Delays in study startup resulted in 128 individuals being omitted from the survey; however, we have no reason to believe they differed in any systematic way from those surveyed. A total of 202 National Guard members who were medically assessed on the days of our survey did not complete the survey and 122 surveys were excluded from the analysis because of poor data quality (inconsistent responses on key variables) as determined by 3 independent raters, leaving a total of 2543 respondents in the final sample.
Additionally, we obtained de-identified health data from the New Jersey Department of Military and Veterans Affairs (DMAVA) for all 2995 soldiers undergoing New Jersey's predeployment medical assessment. These data listed all relevant medical conditions identified for each soldier during the assessment.
Data Collection
We distributed anonymous, self-administered surveys to all National Guard members undergoing mandatory, predeployment medical assessments between November 2007 and May 2008. The survey, which was administered by Rutgers University researchers to groups of approximately 25 to 75 Guard members, took approximately 30 to 60 minutes to complete. Participation was not mandatory, and Guard leadership was not aware of who completed or failed to complete the survey. No monetary incentives were offered for survey participation.
Variables and Measures
Respondents were separated into 2 groups: (1) no prior OEF or OIF deployments and (2) 1 or more prior OEF or OIF deployments. Participants were classified as having a prior deployment if they reported at least 1 deployment to Iraq or Afghanistan since September 11, 2001.
We employed 2 measures of PTSD on the basis of responses to the 17-item National Center for PTSD Checklist.15 The more restrictive measure required a total summed score of 50 or more across all items16 and the less restrictive measure used the symptom-cluster method based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).17 We used published algorithms from the 9-item depression scale of the Patient Health Questionnaire18 to measure major depression and depression not otherwise specified and created a third measure of general depression defined as either major depression or depression not otherwise specified. We measured somatic symptom severity by summing scores across all items on the 15-item Patient Health Questionnaire nonspecific physical symptom scale.19
We defined 3 measures of alcohol use by using questions and algorithms from the DSM-IV-based National Household Survey of Drug Use and Health20 on (1) heavy drinking during the last 30 days, (2) alcohol dependence during the last 12 months, and (3) binge drinking during the last 6 months. We also asked participants whether they had used heroin, cocaine, marijuana, nonprescribed pain medication, tranquilizers, stimulants, sedatives, or “other” drugs in the past 12 months (yes or no).
Other past-12-month measures of mental health included 2 items that asked respondents if they needed help for emotional or sleeping problems (yes or no); 5 items that probed prescribed use of tranquilizers, antidepressants, sleeping pills, mood stabilizers, or stimulants (yes or no); and 2 items that asked the number of visits to a mental health professional for an emotional or nervous complaint or a substance use problem.
In terms of physical health, we presented respondents with a body diagram (front and back) and asked them to place an “X” on each body part affected by pain in the preceding 2 weeks. We measured pain extensity by summing the number of affected body areas.21 We measured pain intensity with a Borg category-ratio scale22 (score = 0–20) and pain duration with a 3-category fixed-response item (acute, subacute, or chronic). We measured physical functioning with the physical functioning subscale from the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36)23 and calculated normed subscale scores according to published SF-36 algorithms.24 In addition, we recoded each of the physical functioning subscale items to reflect some versus no reported physical limitations. Additionally, we asked respondents about number of visits to a medical professional for a physical health problem in the last year.
We also asked deployed respondents about reporting of mental health symptoms following their most recent OEF or OIF deployment, employing a series of true-or-false items to probe whether they had been screened, felt uncomfortable reporting symptoms, failed to report symptoms to avoid being retained on “medical hold” for further evaluation, and were encouraged by superiors to report symptoms and seek mental health treatment if needed. In addition, we gathered data on demographic characteristics and military service history, including service in conflicts prior to 2001.
With respect to DMAVA health data, we identified 3 key mental health diagnostic categories for analysis because of their comparability with conditions assessed in our survey: PTSD, depression, and substance abuse. These diagnoses were arrived at following a comprehensive assessment by a DMAVA medical professional.
Statistical Analysis
We used χ2 analysis for categorical variables and t tests for continuous variables to compare the 2 groups (deployed versus nondeployed) on our variables of interest. To examine the independent effects of previous OEF or OIF service on mental and physical health, we conducted logistic regression analyses on all health measures, controlling for age, race, sex, education, income, marital status, and previous service in conflicts other than OEF or OIF.
We compared the survey and DMAVA assessments on rates of identification of mental health problems using simple tabulations of numbers and proportions of soldiers diagnosed with each condition. To better understand the factors affecting the reporting of mental health problems during military screening, we used χ2 analysis to compare deployed soldiers with and without PTSD on their experiences with reporting mental health symptoms following their last deployment. All analyses were conducted with SPSS version 16 (SPSS Inc, Chicago, IL).
RESULTS
The sample had a mean age of 33.2 years (range = 17–60 years) and was predominantly male (88.1%) and non-Hispanic White (47.4%), although it included a relatively large proportion of Hispanics (29.5%) and a smaller proportion of non-Hispanic Blacks (17.2%). National Guard members were well-educated, with 68.4% having completed some college or better, and most (73.1%) had full-time employment. More than half (51.1%) had never been married and 38.6% were currently married. Nearly 25% reported at least 1 previous OEF or OIF deployment and 2.9% reported 2 or more. Of those previously deployed, 92.1% had served in Iraq only, 5.0% in Afghanistan only, and 2.8% in both conflicts. Approximately 14.5% had served in conflicts other than OEF or OIF, including 6% in the first Gulf War and 8.6% in other conflicts.
Deployed and nondeployed soldiers had significantly different demographic and military profiles (Table 1). The deployed group was older, included a higher proportion of women and racial/ethnic minorities, and was better educated and more likely to have full-time employment. Deployed soldiers had served in the National Guard nearly twice as long as nondeployed soldiers, were less likely to serve in combat arms than in service support roles, and were more likely to have served in a previous conflict other than OEF or OIF.
TABLE 1.
Sociodemographic and Military Characteristics of Members of New Jersey National Guard Prior to Deployment to Iraq in 2008
| Sample Characteristics | No Previous OEF or OIF Deployments (n = 1910) | One or More Previous OEF or OIF Deployments (n = 625) | χ2 or t |
| Sociodemographic | |||
| Age, y, mean (SD) | 29.0 (9.3) | 33.2 (8.9) | −9.8*** |
| Female, no. (%) | 210 (11.0) | 90 (14.5) | 5.3* |
| Race, no. (%) | |||
| Non-Hispanic White | 941 (49.3) | 263 (42.1) | 12.9** |
| Non-Hispanic Black | 301 (15.8) | 130 (20.8) | |
| Hispanic | 551 (28.8) | 194 (31.0) | |
| Other | 117 (6.1) | 38 (6.1) | |
| Marital status, no. (%) | |||
| Married | 690 (36.6) | 277 (44.7) | 60.1*** |
| Never married | 1038 (55.1) | 242 (39.1) | |
| Widowed, separated, or divorced | 155 (8.2) | 100 (16.2) | |
| Education,a no. (%) | 19.8*** | ||
| High school or less | 643 (33.8) | 152 (24.4) | |
| Some college | 896 (47.1) | 344 (55.3) | |
| College graduate or higher | 364 (19.1) | 126 (20.3) | |
| Employed full-time, no. (%) | 1325 (70.3) | 502 (81.4) | 28.8*** |
| Military | |||
| Years in National Guard, mean (SD) | 5.4 (5.7) | 10.5 (6.9) | −5.0*** |
| Military occupational specialty,b no. (%) | |||
| Combat arms | 847 (46.7) | 209 (35.2) | 28.7*** |
| Combat support | 611 (33.7) | 221 (37.2) | |
| Combat service support | 354 (19.5) | 164 (27.6) | |
| Served in previous conflict prior to September 11, 2001, no. (%) | 169 (8.8) | 189 (30.2) | 1.8*** |
Note. OEF = Operation Enduring Freedom (war in Afghanistan); OIF = Operation Iraqi Freedom (war in Iraq).
Fewer than 1% of each group had less than a high school education.
Military occupational specialties are as follows: combat arms are soldiers on the front line of battle; combat support are soldiers who directly support the combat service needs of fighting soldiers (e.g., transportation, supply, logistics); combat service support are soldiers who provide less direct forms of support to the fighting force (e.g., personnel, food service).
*P ≤ .05; **P ≤ .01; ***P ≤ .001.
Mental and Physical Health
Deployed soldiers scored significantly lower than nondeployed soldiers on almost every measure of mental and physical health (Table 2). With respect to mental health, deployed soldiers had higher somatic symptom severity scores than did nondeployed soldiers (4.53 versus 2.91; P < .001), were more than 3 times as likely to screen positive for PTSD and major depression, were nearly twice as likely to meet DSM-IV criteria for alcohol dependence, and were more than twice as likely to report binge drinking. Deployed soldiers were also 2.5 times more likely than were nondeployed soldiers to report needing help with emotional problems and nearly 4 times more likely to report needing help with sleeping problems. Higher mental health need was reflected in higher past-12-month treatment rates, with deployed soldiers being nearly 3 times as likely as were nondeployed soldiers to have visited a mental health professional, more than 6 times as likely to have received substance abuse treatment, and 3.5 times as likely to have been prescribed an antidepressant. There was no group difference in illicit drug use.
TABLE 2.
Health Characteristics of Members of New Jersey National Guard Prior to Deployment to Iraq in 2008
| Sample Characteristics | No Previous OEF or OIF Deployments (n = 1910), No. (%) | One or More Previous OEF or OIF Deployments (n = 625), No. (%) | χ2 | AOR (95% CI)a |
| Mental health | ||||
| Needed help for emotional problems in last 12 mo | 90 (4.7) | 80 (12.8) | 49.2*** | 2.67 (2.11, 3.37) |
| Needed help for sleeping problems in last 12 mo | 92 (4.8) | 98 (15.7) | 80.2*** | 3.97 (2.85, 5.54) |
| PTSD (PCL-17 3 50) | 78 (4.2) | 87 (14.0) | 70.4*** | 3.69 (2.59, 5.24) |
| PTSD (DSM-IV) | 165 (9.0) | 131 (21.1) | 64.0*** | 2.70 (2.05, 3.55) |
| Major depression | 38 (2.0) | 32 (5.1) | 17.2*** | 3.07 (1.81, 5.19) |
| Any depression (major or not otherwise specified) | 44 (2.3) | 41 (6.6) | 26.3*** | 2.94 (2.09, 4.13) |
| Prescribed tranquilizers in last 12 mo | 48 (2.6) | 29 (4.7) | 7.2** | 1.74 (1.05, 2.90) |
| Prescribed antidepressants in last 12 mo | 53 (2.8) | 60 (9.8) | 51.3*** | 3.54 (2.35, 5.33) |
| Prescribed sleeping pills or sedatives in last 12 mo | 68 (3.6) | 55 (9.0) | 27.9*** | 2.41 (1.63, 3.57) |
| Prescribed at least 1 psychotropic medication in last 12 mo | 104 (5.4) | 86 (13.8) | 46.9*** | 2.52 (1.83, 3.49) |
| Heavy drinking last 12 mo | 388 (20.3) | 122 (19.5) | 0.185 | 1.25 (0.97, 1.62) |
| Binge drinking last 6 mo | 90 (4.7) | 44 (7.0) | 5.1* | 2.29 (1.51, 3.48) |
| Alcohol dependence last 12 mo | 127 (6.6) | 56 (9.0) | 3.8 | 1.88 (1.31, 2.69) |
| Illicit drug use last 12 mo | 219 (11.6) | 62 (10.0) | 1.2 | 0.91 (0.66, 1.26) |
| Physical health | ||||
| Reports any pain | 876 (45.9) | 353 (56.5) | 21.3*** | 1.56 (1.28, 1.90) |
| Back pain | 586 (30.7) | 258 (41.3) | 23.8*** | 1.69 (1.37, 2.07) |
| Joint pain | 425 (22.3) | 201 (32.2) | 24.9*** | 1.68 (1.35, 2.08) |
| Moderate to intense pain | 251 (13.4) | 134 (22.0) | 26.1*** | 1.67 (1.28, 2.16) |
| Pain duration | ||||
| Acute (< 3 mo) | 313 (16.7) | 57 (9.3) | 20.2*** | 0.58 (0.42, 0.79) |
| Chronic (≥ 6 mo) | 425 (22.6) | 261 (42.4) | 90.6*** | 2.2 (1.78, 2.72) |
| SF-36 physical function score below population mean for age and gender | 287 (15.5) | 144 (24.4) | 24.1*** | 1.94 (1.51, 2.48) |
| Treatment historyb | ||||
| Mental health treatment in last 12 mo (whole sample) | 149 (7.8) | 135 (21.6) | 90.1*** | 2.96 (2.26, 3.89) |
| Mental health treatment in last 12 mo (among those with PTSD)c | 37 (22.4) | 68 (51.9) | 27.7*** | 3.39 (1.93, 5.99) |
| Substance abuse treatment last 12 mo (whole sample) | 13 (0.7) | 23 (3.7) | 30.3*** | 6.36 (2.98, 13.53) |
| Substance abuse treatment last 12 mo (among those with alcohol dependence) | 4 (3.3) | 7 (13.0) | 5.9* | 2.29 (0.43, 12.17) |
| Medical care in last 12 mo (whole sample) | 671 (35.1) | 326 (52.2) | 57.2*** | 1.81 (1.48, 2.21) |
| Medical care in last 12 mo (among those with chronic and moderate or intense pain) | 91 (63.6) | 72 (72.0) | 1.86 | 1.15 (0.63, 2.13) |
Note. AOR = adjusted odds ratio; CI = confidence interval; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; OEF = Operation Enduring Freedom (war in Afghanistan); OIF = Operation Iraqi Freedom (war in Iraq); PCL-17 = 17-item National Center for PTSD Checklist; PTSD = posttraumatic stress disorder; SF-36 = Medical Outcomes Study 36-Item Short Form Health Survey.
AORs (adjusted for age, sex, race/ethnicity, education, income, marital status, and military deployment other than in OEF or OIF) with 95% CIs reflect risk of each health outcome measure among National Guard members with previous OEF or OIF deployment relative to a nondeployed reference group.
Treatment of all conditions was defined as making 1 or more visits in the last 12 months.
Mental health treatment rate for PTSD was assessed for those meeting DSM-IV criteria for PTSD.
*P ≤ .05; **P ≤ .01; ***P ≤ .001.
Deployed soldiers showed similar deficits with respect to physical health. They reported pain in more body areas (mean = 4.2 versus 3.6; P < .05), especially the back and joints, and experienced pain that was more intense and chronic. Deployed soldiers had physical functioning scores that were significantly lower than were those of nondeployed soldiers (54.4 versus 55.7; P < .001) and more likely to be below the general population norm. Deployed soldiers also made significantly more medical care visits in the past year than did nondeployed soldiers.
Among those screening positive for PTSD, deployed soldiers were more than 3 times as likely as were nondeployed soldiers to have received mental health treatment in the previous year. Although rates of substance abuse treatment among those screening positive for alcohol dependence were universally low, deployed soldiers showed a nonsignificant trend toward higher treatment utilization. Among those with chronic pain, deployed soldiers were also somewhat more likely to access medical treatment.
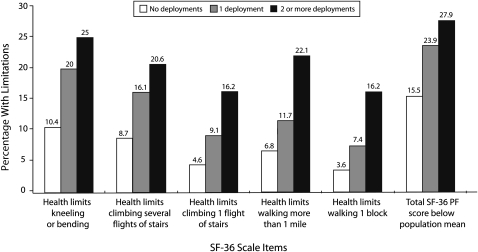
In examining mental and physical health characteristics by numbers of previous deployments (zero, 1, or more than 1), we found little difference between those deployed once versus those deployed more than once on most measures of mental health (not shown). However, there was a tendency for the previously deployed to exhibit progressively worse physical functioning with increasing numbers of deployments. As illustrated in Figure 1, those with more than 1 previous deployment were consistently more likely than were those with 1 or no previous deployments to report limitations in performing ordinary daily activities and to score below the population norm in physical functioning.
FIGURE 1.
Percentage of New Jersey National Guard members reporting health limitations, by number of previous deployments in Afghanistan or Iraq, 2008.
Note. Physical functioning was determined from the Medical Outcomes Study 36-Item Short Form (SF-36) Health Survey Physical Functioning (PF) subscale.23
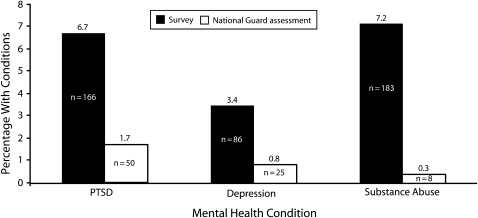
Survey Versus Department of Military and Veterans Affairs
Figure 2 shows that New Jersey's medical assessment identified substantially fewer individuals with the mental health conditions in question than the anonymous survey. DMAVA identified PTSD in 1.7% (n = 50) of the 2995 assessed individuals, whereas the survey identified PTSD in 6.7% (n = 166) of the 2543 survey participants. Similarly, DMAVA identified depression in 0.8% (n = 25) of assessed individuals and the survey identified depression in 3.4% (n = 86). Finally, DMAVA identified substance problems in 0.3% (n = 8) and the survey identified substance problems in at least 7.2% (n = 183).
FIGURE 2.
Percentage of New Jersey National Guard members with mental health conditions prior to deployment in Iraq or Afghanistan, as identified by study survey versus National Guard health assessment, 2008.
Note. For study survey, n = 2543; for National Guard health assessment, n = 2995.
Symptom Reporting
A comparison of deployed soldiers with and without positive screens for PTSD revealed a significant underreporting of symptoms among those with positive PTSD screens. Thus, soldiers screening positive for PTSD were less likely than were others to report being screened for mental health problems after deployment (35.0% versus 57.1%; χ2 = 18.7; P < .001) and to feel that their superiors had encouraged symptom reporting (43.7% versus 72.6%; χ2 = 35.6; P < .001) or treatment seeking (60.0% versus 79.5%; χ2 = 19.5; P < .001). They were more likely to experience discomfort reporting symptoms (63.3% versus 38.4%; χ2 = 24.1; P < .001) and to fail to report symptoms to avoid “medical hold” (59.3% versus 34.1%; χ2 = 25.0; P < .001).
DISCUSSION
The present findings suggest that despite comprehensive health screenings by state and federal military authorities, the repeated OEF and OIF deployment of New Jersey National Guard troops may result in a substantial number of medically impaired soldiers being returned to combat. After control for potentially confounding psychosocial and military factors, those with previous OEF or OIF service were more than 3 times as likely as others to screen positive for major depression and PTSD, twice as likely to screen positive for alcohol dependence and chronic pain, and twice as likely to have physical functioning scores below the general population mean. Despite a comprehensive assessment by the New Jersey National Guard, military authorities identified substantially fewer soldiers with mental health impairment than were identified in the anonymous survey. Only 2.5% (n = 76) of the 2995 assessed National Guard members were excluded from deployment by New Jersey for mental health reasons (New Jersey National Guard, unpublished data, 2008). Follow-up data on mobilization training rejection rates by the US Department of Defense indicate that approximately 40 additional soldiers were subsequently returned from active duty for any reason, representing only about 1% of the total New Jersey National Guard force.
There is no clear standard for what constitutes a medically fit fighting force (having PTSD, for example, does not disqualify someone from military service), and symptom reporting on screening instruments does not substitute for a diagnostic assessment by a medical professional. In addition, functional status, which directly relates to performance, may be more important than symptoms in determining who remains in the military. However, the Pentagon's own data indicate that, between 2003 and 2008, 43 000 troops deemed medically unfit for active duty by their physicians were deployed to Iraq.25 Similarly, findings of the Office of the US Army Surgeon General6 suggest that multiple deployments have adverse effects on work performance during deployment, with multiply deployed soldiers being more likely than are others to report limitations in their ability to work effectively (16.6% versus 9.7%), supervisory concern about their job performance (14.1% versus 7.9%), and alcohol use during deployment (6.6% versus 4.3%).
The primary military screening mechanisms for identifying medically impaired soldiers are the Department of Defense's Post-Deployment Health Assessment (PDHA) and the Post-Deployment Health Assessment and Re-Assessment (PDHRA). The prevalence of health problems presently observed among previously deployed Guard members, however, raises questions about the effectiveness of the PDHA–PDHRA in screening out soldiers with compromised health. A recent study of OEF and OIF postdeployment assessments found that 74% of veterans who subsequently sought mental health treatment were not identified by the PHDRA as needing treatment, although there was an association between treatment seeking and the reporting of some mental health concern.7 Studies suggest that 1 factor in the underidentification of health problems by the PDHA–PDHRA is the underreporting of symptoms by soldiers seeking to avoid the perceived stigmatizing or other potentially adverse consequences of acknowledging mental health problems.26 In the present study, previously deployed soldiers screening positive for PTSD reported significant concern about mental health stigma, citing discomfort reporting symptoms and a belief that their superiors would not encourage mental health treatment. Similarly, release from active duty after deployment may be delayed among soldiers reporting health problems.5 In the present study, 59% of previously deployed soldiers with positive PTSD screens said they did not report symptoms after deployment to avoid “medical hold.”
In addition to symptom underreporting, there may be limitations in the universality of the PDHA–PDHRA administration process. Many OEF and OIF troops may not have received a PDHRA if they were previously deployed prior to 2005, the year the reassessment was instituted. In the present study, a substantial proportion of previously deployed soldiers, including nearly 58% of those screening positive for PTSD, reported not receiving a postdeployment mental health screen. Although this finding may reflect poor recall, especially among psychologically distressed soldiers returning from combat, other studies, including a recent Government Accountability Office report, have raised questions about the universality of PDHA–PDHRA screening.27–29 Since research indicates that higher rates of PTSD emerge in the months following return from combat,14 the postdeployment reassessment is critical to identifying the potentially large group of soldiers who may have been asymptomatic or failed to report symptoms immediately after deployment.
Despite the limitations of military screens, in the present study, previously deployed soldiers accessed treatment at higher rates than did other soldiers, corroborating previous findings that although the PDHA–PDHRA may lack sensitivity in identifying which veterans need treatment, the screening process itself may have a positive effect on treatment seeking.7 However, overall treatment rates remained low. Nearly half of previously deployed soldiers screening positive for PTSD and close to 90% of those screening positive for alcohol dependence reported no treatment in the past 12 months. The particularly low rate of alcohol treatment has been noted in other studies, where it was related in part to the military's lack of confidentiality surrounding substance abuse treatment.7 Lack of health care coverage may also represent a barrier.7 In the present study, 57% of those screening positive for PTSD who had either military, Department of Veterans Affairs (VA), or private health insurance received treatment, compared with only 39% without this insurance (not shown).
Limitations
The study is limited by its reliance on self-report screening instruments, which may not reflect actual disease prevalence rates. However, validation studies of our 2 primary mental health diagnostic instruments, the Patient Health Questionnaire and the 17-item National Center for PTSD Checklist, suggest that these instruments are more likely to underestimate than to overestimate the prevalence of impairment.16,30
The generalizability of the current findings is limited by several factors. First, previous studies suggest that National Guard OEF and OIF veterans have a higher prevalence of mental health problems than regular-military OEF and OIF veterans,7 possibly because of experiences unique to the National Guard. Many, for example, may experience family, employment, and financial stressors that contribute to a more complicated postdeployment adjustment. Similarly, National Guard soldiers lack the centralized military support available to active-duty troops through their connection to military bases. In terms of generalizability to other National Guard populations, comparisons between the current sample and a 2006 national sample of Army National Guard31 showed comparability within 5 percentage points or less with respect to age, sex, education, marital status, and full-time civilian employment status. The New Jersey sample, however, included a higher proportion of Hispanics (29.5% versus 10.1%) and fewer non-Hispanic Whites (47.4% versus 72.6%), although analyses of the present data by race/ethnicity (not shown) showed few racial/ethnic differences in health outcomes. Moreover, the New Jersey sample was similar to the national sample on several key outcomes, including heavy drinking (18.9% versus 20.1%), past-12-month illicit drug use (11.2% versus 14.6%), and PTSD (6.7% versus 10.5%).
Despite these similarities, however, there may be regional differences in physical conditioning, attitudes toward combat, financial stressors, and other characteristics that may limit the generalizability of these findings beyond New Jersey. Similarly, although the current sample represented approximately 50% of the New Jersey National Guard force, it is possible that those called for duty were not representative of all New Jersey National Guard members. Finally, these results may not generalize to past or future wars because of the unique characteristics of the OEF and OIF conflicts.
Conclusions
Our findings suggest that repeated deployments to Iraq and Afghanistan adversely affect the physical and mental functioning of New Jersey National Guard troops. The implications of these findings for the health of all active-duty forces recalled to OEF or OIF combat require further investigation. Screening programs and mobilization trainings remain imperfect mechanisms for identifying and insuring treatment of psychologically impaired soldiers. It is important, therefore, for military and veteran authorities to develop mechanisms for the truly confidential and accessible assessment and treatment of mental and behavioral health problems. These findings also suggest the need to examine existing policies regarding multiple deployments of troops to the OEF and OIF conflicts.
Acknowledgments
This study was funded by the New Jersey Department of Military and Veterans Affairs.
We thank Col Stephen Abel for his generous support of this project and Col Deborah Burr for providing information regarding New Jersey's predeployment medical assessments. We also thank staff from the Bloustein Center for Survey Research, Rutgers University, including Chris Bruzios, director, and Fran Brooks, research associate, for overseeing the data collection and management and Marc Weiner, associate director, for his valuable input on the data analysis.
Human Participant Protection
This study was approved by the institutional review boards of the Veterans Administration New Jersey Health Care System and of Rutgers University. Because the survey was anonymous, no informed consent documents were signed; however, participants were provided with verbal and written information about the study prior to their participation and were informed that participation was not mandatory.
References
- 1.Hotopf M, Hull L, Fear NT, et al. The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet 2006;367(9524):1731–1741 [DOI] [PubMed] [Google Scholar]
- 2.Lapierre CB, Schwegler AF, LaBauve BJ. Posttraumatic stress and depression symptoms in soldiers returning from combat operations in Iraq and Afghanistan. J Trauma Stress 2007;20(6):933–943 [DOI] [PubMed] [Google Scholar]
- 3.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA 2006;295(9):1023–1032 [DOI] [PubMed] [Google Scholar]
- 4.Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF. Neuropsychological outcomes of army personnel following deployment to the Iraq war. JAMA 2006;296(5):519–529 Available at: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=16882958. Accessed August 19, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Rand Corp, Center for Military Health Policy Research Invisible wounds of war: psychological and cognitive injuries, their consequences, and services to assist recovery. 2008. Available at: http://www.rand.org/pubs/monographs/MG720. Accessed August 3, 2008
- 6.Office of the US Army Surgeon General Mental Health Advisory Team V Report. February 14, 2008. Available at: http://www.armymedicine.army.mil/reports/mhat/mhat_v/mhat-v.cfm. Accessed March 4, 2008
- 7.Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve components soldiers returning from the Iraq war. JAMA 2007;298(18):2141–2148 [DOI] [PubMed] [Google Scholar]
- 8.Department of Defense Operation Iraqi Freedom/Operation Enduring Freedom US casualty status. October 21, 2008. Available at: http://www.defenselink.mil/news/casualty.pdf. Accessed October 21, 2008
- 9.Yun HC, Branstetter JG, Murray CK. Osteomyelitis in military personnel wounded in Iraq and Afghanistan. J Trauma 2008;64(2 suppl):S163–S168 [DOI] [PubMed] [Google Scholar]
- 10.Gironda RJ, Clark ME, Massengale JP, Walker RL. Pain among veterans of Operations Enduring Freedom and Iraqi Freedom. Pain Med 2006;7(4):339–343 [DOI] [PubMed] [Google Scholar]
- 11.Clark ME, Bair MJ, Walker RLJ, et al. Pain and combat injuries in soldiers returning from Operations Enduring Freedom and Iraqi Freedom: implications for research and practice. J Rehabil Res Dev 2007;44(2):179–194 [DOI] [PubMed] [Google Scholar]
- 12.Shanker T. Army is worried by rising stress of return tours to Iraq. New York Times April 6, 2008. Available at: http://www.nytimes.com/2008/04/06/washington/06military.html. Accessed September 2, 2008 [Google Scholar]
- 13.US Dept of Defense, Military Health System Military Health System mission. Available at: http://www.health.mil/StrategicPlan/Mission.aspx. Accessed September 20, 2008
- 14.Killgore WDS, Stetz MC, Castro CA, Hoge CW. The effects of prior combat experience on the expression of somatic and affective symptoms in deploying solders. J Psychosom Res 2006;60(4):379–385 [DOI] [PubMed] [Google Scholar]
- 15.Blanchard EB, Jones-Alexander J, Buckley TC, et al. Psychometric properties of the PTSD Checklist (PCL). Behav Res Ther 1996;34(8):669–673 [DOI] [PubMed] [Google Scholar]
- 16.Andrykowski MA, Cordova MJ, Studts JL, et al. Posttraumatic stress disorder after treatment for breast cancer: prevalence of diagnosis and use of the PTSD Checklist–Civilian Version (PCL-C) as a screening instrument. J Consult Clin Psychol 1998;66(3):586–590 [DOI] [PubMed] [Google Scholar]
- 17.Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. J Trauma Stress 2005;18(1):53–62 [DOI] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer R. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002;32(9):509–515 [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 2002;64(2):258–266 [DOI] [PubMed] [Google Scholar]
- 20.US Dept of Health and Human Services, Substance Abuse and Mental Health Services Administration, Office of Applied Studies. National Survey on Drug Use and Health 2006 [computer file] Research Triangle Park, NC: Research Triangle Institute; 2007. DHHS publication SMA 07-4293 [Google Scholar]
- 21.Staud R, Price DD, Robinson ME, et al. Body pain area and pain-related negative affect predict clinical pain intensity in patients with fibromyalgia. J Pain 2004;5(6):338–343 [DOI] [PubMed] [Google Scholar]
- 22.Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health 1990;16:55–58 [DOI] [PubMed] [Google Scholar]
- 23.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36), I: conceptual framework and item selection. Med Care 1992;30(6):473–483 [PubMed] [Google Scholar]
- 24.Ware JE, Kosinski M, Dewey JE. How to Score Version Two of the SF-36 Health Survey Lincoln, RI: QualityMetric Inc; 2000 [Google Scholar]
- 25.Zoroya G. US deploys more than 43,000 unfit for combat. USA Today May 8, 2008. Available at: http://www.usatoday.com/news/military/2008-05-07-nondeploy_N.htm. Accessed May 25, 2008 [Google Scholar]
- 26.Hoge CW, Castro CA, Messer SC, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351(1):13–22 [DOI] [PubMed] [Google Scholar]
- 27.Martin CB. Routine screening and referrals for post-traumatic stress disorder after returning from Operation Iraqi Freedom in 2005, US Armed Forces. MSMR: Medical Surveillance Monthly Report October/September2007;14(6):2–7 Available at: http://www.afhsc.mil/msmr_pdfs/2007/v14_n06.pdf#Post-traumatic_stress_disorder. Accessed 6, 2008 [Google Scholar]
- 28.Karney BR, Ramchand R, Chan K, Calderone-Barnes L, Burns R. Invisible Wounds: Predicting the Immediate and Long-term Consequences of Mental Health Problems in Veterans of Operation Enduring Freedom and Operation Iraqi Freedom Santa Monica CA: Rand Center for Military Health Policy Research; 2007 [Google Scholar]
- 29.US Government Accountability Office Defense health care: oversight of military services' post-deployment health reassessment completion rates is limited. September 4, 2008. Available at: http://www.gao.gov/new.items/d081025r.pdf. Accessed September 6, 2008
- 30.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999;282(18):1737–1744 [DOI] [PubMed] [Google Scholar]
- 31.Hourani LL, Bray RM, Marsden ME, et al. 2006 Department of Defense Survey of health related behaviors among the Guard and Reserve force: a component of the Defense Lifestyle Assessment Program (DLAP). Report prepared for the assistant secretary of defense (health affairs) by RTI International, September 2007. Available at: http://www.tricare.mil/hpae/_docs/RC_2006%20Reserve%20Component_FR_9-07.pdf. Accessed May 15, 2009