Abstract
Objective
Meniscal tears and osteoarthritis (OA) frequently coexist, but to our knowledge, no data exist to identify who will benefit from arthroscopic partial meniscectomy (APM) versus nonoperative management. Our objective was to evaluate the capability of preoperative information to predict APM outcomes in OA.
Methods
Using a mathematical model and published data, we combined 2 clinical (mechanical symptoms and pain pattern) and 2 magnetic resonance imaging (tear type and bone marrow lesions) indicators into 36 possible combinations and ranked each combination according to the likelihood of having primarily tear- versus OA-related pain in individuals ages 45–65 years with knee pain, OA, and meniscal tears. By considering alternative thresholds for performing APM, we identified the cutoff rank that maximized the overall population International Knee Documentation Committee (IKDC) score (0–100 scale).
Results
Rank 1 (e.g., displaced tear, locking, increased pain, no bone marrow lesions) represented the highest likelihood of APM benefit; rank 36 (e.g., oblique tear, no mechanical symptoms, static pain, severe bone marrow lesions) represented the lowest likelihood of APM benefit. Indeterminate middle ranks included individuals with mixed findings (i.e., 2 findings consistent with high and 2 with low likelihood of APM benefit). APM thresholds between ranks 17 and 23 resulted in >82% of the population receiving treatment producing the greatest possible IKDC improvement, with mean incremental gains in IKDC score of >24 points. Findings were robust across a broad range of indicator assumptions, but were sensitive to outcome assumptions.
Conclusion
Among individuals with degenerative meniscal tears and OA, easily obtainable clinical information can differentiate those who are more likely to benefit from APM.
INTRODUCTION
One in 2 Americans will likely develop symptomatic knee osteoarthritis (OA) (1). More than 60% of these will use magnetic resonance imaging (MRI) to evaluate their knee pain (2), and up to 80% of those MRIs will identify the presence of meniscal tears (3). Arthroscopic partial meniscectomy (APM) is standard treatment for presumed symptomatic meniscal tears. This translates into approximately 500,000 APMs in individuals with OA each year, representing more than half of all APMs (4).
Every day, thousands of rheumatologists and arthritis specialists must decide whether or not to recommend APM for their patients with OA and MRI evidence of meniscal tears. To our knowledge, there are no large-scale published trials designed to examine the efficacy of APM in these patients. In a small study, Herrlin et al randomized individuals age ≥45 years with nontraumatic meniscal tears, some with OA, to APM or supervised exercise and found indistinguishable improvements in pain, function, and quality of life at 6 months (5). They did not report the impact of OA.
It is difficult to perform blinded randomized controlled trials of APM because sham controls are controversial (6), and both patients and surgeons are reluctant to accept randomization, threatening generalizability (7). Because it will be years before we have robust efficacy data for APM, other approaches should be explored to determine whether easily obtainable clinical data can facilitate decision making for this common condition. Our objective was to evaluate the capability of readily available information to predict APM outcomes in individuals with knee pain, meniscal tear, and OA.
SUBJECTS AND METHODS
Overview
We assumed that the primary etiology of an individual’s knee pain is a strong predictor of their response to APM: individuals with pain primarily due to meniscal tear will benefit from APM, while those with pain primarily due to OA will not. We combined clinical indicators of probable response to APM (tear type, presence of mechanical symptoms, pain pattern, and bone marrow lesions) in individuals with both meniscal tear and OA to create a ranking system to differentiate those with primarily tear-related versus OA-related pain. We then estimated the average improvement in the International Knee Documentation Committee (IKDC) Subjective Knee Form score using each successive rank as the cutoff for performing APM in the population. We selected clinical indicator estimates less predictive than data support and used assumptions favoring APM over nonoperative management, likely overestimating APM benefit, such that our results would represent a highly conservative perspective.
Study population
We considered a hypothetical population of individuals ages 45–65 years with knee pain, in the presence of both knee OA (Kellgren/Lawrence grades 2 to 3) and nontraumatic meniscal tear on MRI (Stoller grade 3) severe enough to warrant consideration of APM (8 –11). Kellgren/Lawrence grade 4 OA is typically amenable to total joint arthroplasty and not APM, and was not considered.
Development of indicator ranking to discriminate between tear- and OA-related pain
This approach is based on work by Neutra (12). We developed our indicator ranking based on 1) whether an individual’s pain was primarily due to meniscal tear versus OA (i.e., base prevalence or pretest likelihood of tear-related pain) and 2) 4 indicators selected for their ability to discriminate between the likely source of pain (meniscal tear versus OA), and thus improve our pretest estimate of tear-related pain and describe the spectrum of APM decision making without overlap. Details on the ranking system development are shown in Supplementary Appendix A (available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home).
Base prevalence
In the absence of data regarding the true base prevalence of tear-related pain, we used recent data supporting the fact that OA is a greater predictor of knee pain than meniscal tear (13). We therefore assumed that the pretest likelihood that an individual’s knee pain was primarily due to their meniscal tear (i.e., the proportion expected to have optimal APM outcomes) was 20%; the remaining 80% had primarily OA-related pain. We varied the base prevalence of pain due to tear from 0% to 90% in the sensitivity analyses.
Predictive indicators
The 4 indicators used in the ranking were tear type, presence of mechanical symptoms, pain pattern, and bone marrow lesions. Tear type and bone marrow lesions represent MRI indicators; mechanical symptoms and pain pattern are clinical indicators. The base estimates are listed in Table 1 and the derivations of all of the estimates are provided in Supplementary Appendix A (available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home): 1) tear type on MRI (dichotomized into Low likelihood of causing pain or symptoms [radial, horizontal, or oblique partial-thickness tears] versus High likelihood [displaced, vertical, complex full-thickness tears]); 2) the presence of mechanical symptoms (categorized as None, Possible [buckling or giving way], and Probable [intermittent locking or catching] mechanical symptoms); 3) pain pattern (dichotomized as Increased [in the last 3 months] versus Static pain); and 4) MRI-based evidence of bone marrow lesions (categorized as None, Mild, or Severe, based on the Whole-Organ MRI Score [14,15], where None was defined as a score of 0, Mild as any area with a maximum score of 1, and Severe as any area with a maximum score of 2 or 3).
Table 1.
Base estimates*
| Tear-related pain | OA-related pain | ||||
|---|---|---|---|---|---|
| Base case |
Plausible range |
Base case |
Plausible range |
Ref. | |
| Base prevalence | 0.20 | 0.00–0.90 | 0.80 | 0.10–1.00 | 13 |
| Tear type | 33 | ||||
| Low likelihood of tear-related pain | 0.30 | 0.05–0.50 | 0.70 | 0.50–0.95 | |
| High likelihood of tear-related pain | 0.70 | 0.50–0.95 | 0.30 | 0.05–0.50 | |
| Mechanical symptoms | |||||
| None | 0.10 | 0.01–0.33 | 0.60 | 0.35–0.90 | |
| Possible (e.g., giving way) | 0.60 | 0.19–0.89 | 0.35 | 0.09–0.40 | 34 |
| Probable (e.g., locking) | 0.30 | 0.10–0.80 | 0.05 | 0.01–0.25 | 21 |
| Pain pattern | 35 | ||||
| Increased | 0.70 | 0.50–0.95 | 0.30 | 0.05–0.50 | |
| Static | 0.30 | 0.05–0.50 | 0.70 | 0.50–0.95 | |
| MRI bone marrow lesions | 15, 36–38 | ||||
| None | 0.45 | 0.33–0.90 | 0.10 | 0.01–0.33 | |
| Mild | 0.35 | 0.09–0.40 | 0.30 | 0.19–0.50 | |
| Severe | 0.20 | 0.01–0.27 | 0.60 | 0.17–0.80 | |
| IKDC change score at 2 years† | 5, 39–43 | ||||
| APM | 50 | 25–70 | 0 | −25 to 25 | |
| No APM | −25 | −40 to 0 | 25 | 0–50 | |
OA = osteoarthritis; MRI = magnetic resonance imaging; IKDC = International Knee Documentation Committee; APM = arthroscopic partial meniscectomy.
IKDC scores range from 0 to 100, with 100 representing no pain or disability and higher changes in scores indicating greater clinical improvement.
Bayesian theory enables us to improve the estimation of the likelihood of tear-related pain (base prevalence) using these indicators (16). Instead of assuming that every patient has the same likelihood of tear-related pain, we used the 36 (2 × 3 × 2 × 3) possible combinations of the above 4 clinical indicators that an individual might experience to estimate the likelihood that a patient’s pain is tear related.
Outcome measures
We chose the improvement (from pretreatment to 2 years posttreatment) in IKDC score (0–100 scale), a validated disease-specific health-related quality of life measure for knee disorders, as our primary clinical outcome measure (17). We selected a 2-year time-frame because this should represent stable values (compared with the immediate postoperative period) (18), but does not require that long-term consequences (i.e., OA progression) be considered. We identified the rank cutoffs for performing APM that produced maximal improvement in population IKDC scores and maximal proportion of the population receiving optimal treatment.
Theoretical constructs and assumptions
We used the following assumptions generated from expert opinion: 1) APM will produce benefit only among individuals with tear-related pain (true-positives), 2) APM will provide no benefit to individuals with OA-related pain (false-positives), 3) individuals with tear-related pain who do not undergo APM (false-negatives) will have worse outcomes compared with those with tear-related pain who undergo APM, and 4) individuals with OA-related pain who do not undergo APM (true-negatives) will have outcomes commensurate to current OA treatment modalities.
Although this analysis is not a classic decision analysis, these assumptions can be considered in this framework (e.g., an individual with knee pain, meniscal tear, and OA presents with a given combination of the 4 clinical indicators listed above and either undergoes APM or receives nonoperative treatment). That individual could have either pain primarily due to tear or OA, the likelihood of which depends on their indicator combination. Their response to the treatment they receive will be dictated by their underlying primary source of pain (tear versus OA). A decision tree representing this hypothetical scenario and details of the evidence supporting the outcome assumptions above and in Table 1 are shown in Supplementary Appendix A (available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home).
Base-case analysis
There are 36 clinical indicator combinations representing all of the possible scenarios among the 4 clinical factors (tear type, presence of mechanical symptoms, pain pattern, and bone marrow lesions). We are aware of no data that describe the prevalence of these combinations. For our base-case analysis, we assumed that the indicators were independent (i.e., the likelihood of observing one indicator is independent of observing any other). This permitted us to estimate the probability of observing a given indicator combination by multiplying the probability of finding each individual indicator in an individual with tear-related or OA-related pain. Although there are published (19) and unpublished (Losina E: personal communication) data documenting that bone marrow lesions and tear size are independent, we recognized the uncertainty regarding the independence assumption and conducted sensitivity analyses to address the likelihood that indicators are not independent of each other.
We calculated the likelihood ratio (LR) for tear-related pain (i.e., the likelihood of finding a given indicator combination among individuals with tear-related pain versus OA-related pain) for each of the possible 36 indicator combinations by dividing the probability of a given combination of indicators among individuals with tear-related pain by the probability of that same combination among individuals with OA-related pain. The LRs and the associated indicator combinations are provided in Supplementary Appendix A (available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home). For example, individuals in rank 1 (indicator combination High likelihood tear type, Probable mechanical symptoms, Increased pain pattern, and None bone marrow lesions) are 147 times more likely to have tear-related pain than OA-related pain.
This information was then used to refine the original estimate of the prevalence of tear- and OA-related pain using Bayes’ theorem (16). Calculations are shown in Supplementary Appendix A (available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home). Having refined the estimation of the underlying likelihood of tear-related pain, we then applied this ranking to estimate population outcomes if a given indicator combination was used as the cutoff for performing APM (e.g., using rank 10 as the cutoff meant that all of the individuals in ranks 1–10 underwent APM, and the remaining individuals in ranks 11–36 were treated nonoperatively). The improvement in the population IKDC score at this cutoff is a weighted average of the outcomes achieved by: 1) appropriately performing APM on the population in ranks 1–10 who have tear-related pain, 2) inappropriately performing APM on those in ranks 1–10 with OA-related pain, 3) appropriately withholding APM from those in ranks 11–36 with OA-related pain, and 4) inappropriately failing to perform APM on those in ranks 11–36 with tear-related pain. We repeated this estimation using every possible indicator combination as the cutoff. As the cutoff rank increases (i.e., one performs APM in those with a lower likelihood of tear-related pain), more individuals undergo APM and fewer are treated nonoperatively. Therefore, more individuals with tear-related pain are getting APM, but more individuals with OA-related pain are undergoing unnecessary surgery. After assessing each possible cutoff for performing APM (including the situation where everyone receives APM), we identified the cutoff rank that maximized the overall IKDC score for the population and labeled that our optimal threshold.
Sensitivity analyses
One-way sensitivity analyses of all of the data were performed using the ranges in Table 1. Further description is provided in Supplementary Appendix A (available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home). Given the uncertainty surrounding the base prevalence of tear-related pain, we explored the effect of ranging the prevalence from 0% to 90% in one-way sensitivity analyses and also reran all (base, one-way, and multi-way sensitivity) analyses assuming 50% base prevalence. We explored multi-way sensitivity analyses to determine the simultaneous impact of: 1) varying the base prevalence of tear-related pain, 2) decreasing the penalty of failing to perform APM among those with tear-related pain, 3) assuming that APM was harmful to individuals with OA-related pain (i.e., penalizing false-positives), and 4) decreasing the efficacy of appropriately performing APM in individuals with tear-related pain.
We also simultaneously varied both the indicator probabilities among individuals with tear- and OA-related pain and the predictive capability of all 4 indicators. Therefore, we tested various worse-case scenarios for APM in contrast to our base-case analysis, which favored APM.
To address possible dependence among indicators, we repeated the analysis using a highly conservative alternative (i.e., assuming complete dependence between any 2 indicators) by removing the indicators from the ranking one at a time (as would occur if one finding were completely dependent on another). We created receiver operating characteristic (ROC) curves by plotting the proportion of the population with tear-related pain undergoing APM (i.e., true-positive fraction) versus the proportion with OA-related pain undergoing APM (i.e., false-positive fraction) for each of the 36 cutoff ranks, and reported area under the curve (AUC) values for each analysis.
RESULTS
Here we describe 1) the ability of the analysis to discriminate between tear- and OA-related pain, 2) the improvement in the population IKDC scores obtained using different rank thresholds for performing APM, and 3) the threshold rank producing the maximal improvement in the population IKDC score for both the base-case and sensitivity analyses.
Results of the base-case analysis: discrimination
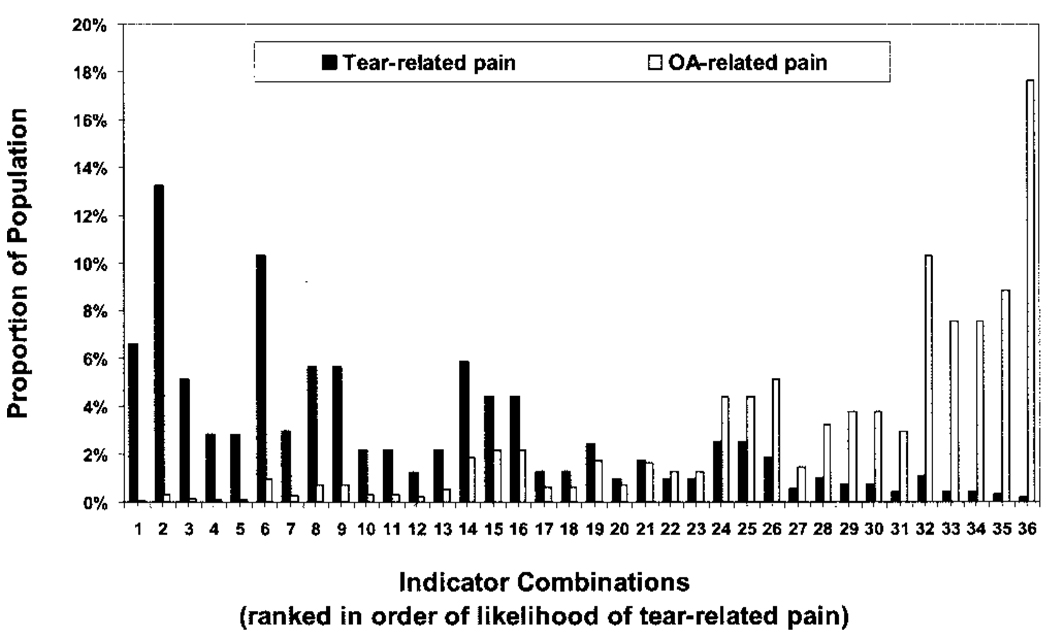
Figure 1 shows the proportion of individuals with tear- and OA-related pain in each of the 36 indicator combinations. Rank 1 refers to the combination with the highest LR of tear-related pain (High, Probable, Increased, None), and rank 36 refers to the combination with the lowest LR of tear-related pain (Low, None, Static, Severe). There is good discrimination between ranks where individuals with tear-related pain predominate (77.8% of those with tear-related pain are in ranks 1–16) and ranks where individuals with OA-related pain predominate (81.0% with OA-related pain are in ranks 24–36). The middle ranks 17–23, where individuals with tear- and OA-related pain are located in relatively equal proportion, are sparsely populated, containing <8% of the total population.
Figure 1.
Proportions of individuals with tear- and osteoarthritis (OA)–related pain in each of 36 possible indicator combinations. Rank 1 refers to the indicator combination of High likelihood tear type, Probable mechanical symptoms, Increased pain pattern, and None bone marrow lesions (highest likelihood ratio [LR] of tear-related pain), and rank 36 refers to the indicator combination of Low likelihood tear type, No mechanical symptoms, Static pain pattern, and Severe bone marrow lesions (lowest LR of tear-related pain).
Results of the base-case analysis: IKDC score improvements
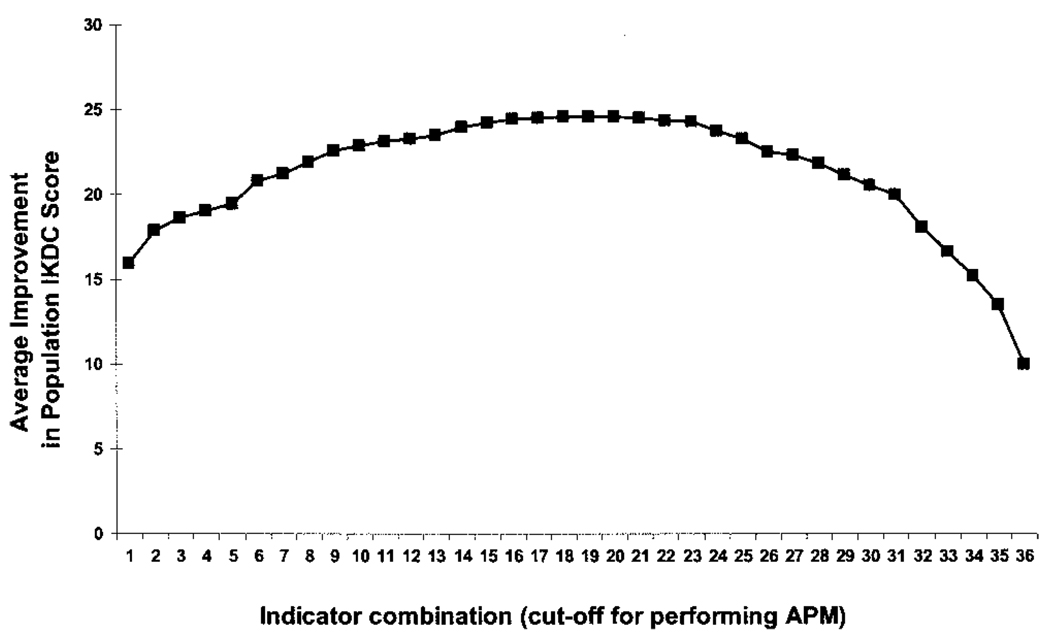
Figure 2 shows the expected 2-year improvement in the population IKDC score at each possible APM cutoff. The horizontal axis lists the 36 possible indicator combinations and the vertical axis shows the average incremental improvement in the population IKDC score over 2 years. Each data point represents the average improvement in IKDC score for the population if one were to use that combination as the APM cutoff. Starting at the left side of the figure, the majority of patients have tear-related pain. Moving to the right, initially (e.g., through rank 16), most patients have tear-related pain and surgical success rates are high. However, continuing to the right, a much smaller proportion of individuals have tear-related pain. Accordingly, the success rate of surgery diminishes and the population outcomes worsen.
Figure 2.
Total 2-year population outcomes according to the indicator combination rank used as the cutoff for performing arthroscopic partial meniscectomy (APM). Rank 1 refers to the indicator combination of High likelihood tear type, Probable mechanical symptoms, Increased pain pattern, and None bone marrow lesions (highest likelihood ratio [LR] of tear-related pain), and rank 36 refers to the indicator combination of Low likelihood tear type, No mechanical symptoms, Static pain pattern, and Severe bone marrow lesions (lowest LR of tear-related pain). IKDC = International Knee Documentation Committee.
Results of the base-case analysis: maximizing IKDC scores
Using indicator combination 19 (Low, Possible, Static, Mild) as the cutoff, operating on all of the subjects in symptom combination ranks 1–19 and not operating on those in ranks 20–36, maximizes 2-year improvements in population IKDC scores, producing an average benefit of 24.6 points by performing APM on 27.8% of the population (and 14.1% of individuals with primarily OA-related pain). Selecting a cutoff from any rank between ranks 17 and 23 yields equivalent incremental benefit (improvements of 24.2–24.5 IKDC points) and ensures that at least 82% of individuals would receive the favored treatment for their knee pain.
Results of sensitivity analyses: discrimination
Varying the base prevalence of tear-related pain and/or the outcome assumptions (i.e., improvements in IKDC scores) does not alter how well the indicator ranking discriminates between individuals with tear- versus OA-related pain. The relative scarcity of individuals in the middle ranks means that shifting the threshold for performing APM among those indeterminate ranks has little effect on the overall population outcomes. Therefore, although decreasing the predictive capacity of any given individual indicator also decreased the overall discriminatory power of the model, this only flattened the outcome curves further (i.e., lowered the maximum improvements in the population IKDC scores shown in Figure 2). This resulted in somewhat greater ambivalence regarding the optimal rank, but had minimal clinical impact regardless of the threshold rank selected (see below).
Results of sensitivity analyses: improvements in IKDC scores
Varying input assumptions regarding the base prevalence of tear-related pain, the predictive ability of the indicators, and clinical outcomes (across the ranges in Table 1) had little impact on the overall population outcomes. Differences between the population IKDC score improvements were less than 7.5 points for all of the variables except base prevalence and the assumed improvement in IKDC score for individuals with OA-related pain receiving nonoperative treatment. Improvements in IKDC scores ranged from 23.7 to 45.3 points when we varied the base prevalence of tear-related pain from 0% to 90%, because more tear-related pain increases the population benefit of APM. Ranging the base prevalence between 0% and 30% produced maximal improvements in IKDC scores of 23.7–26.3 points, with the nadir at a base prevalence of 9% tear-related pain. In addition, ranging the improvement in IKDC score for nonoperative treatment from 0 to 50 points in individuals with OA-related pain resulted in average population improvements of 10.0–42.7 IKDC points. This influence was attenuated by assuming a greater base prevalence of tear-related pain. Performing a similar sensitivity analysis with a 50% base prevalence of tear-related pain reduced the variation in average population improvements from 25.0 to 40.5 points. (For additional results obtained assuming 50% base prevalence of tear-related pain, see Supplementary Appendix B, available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home).
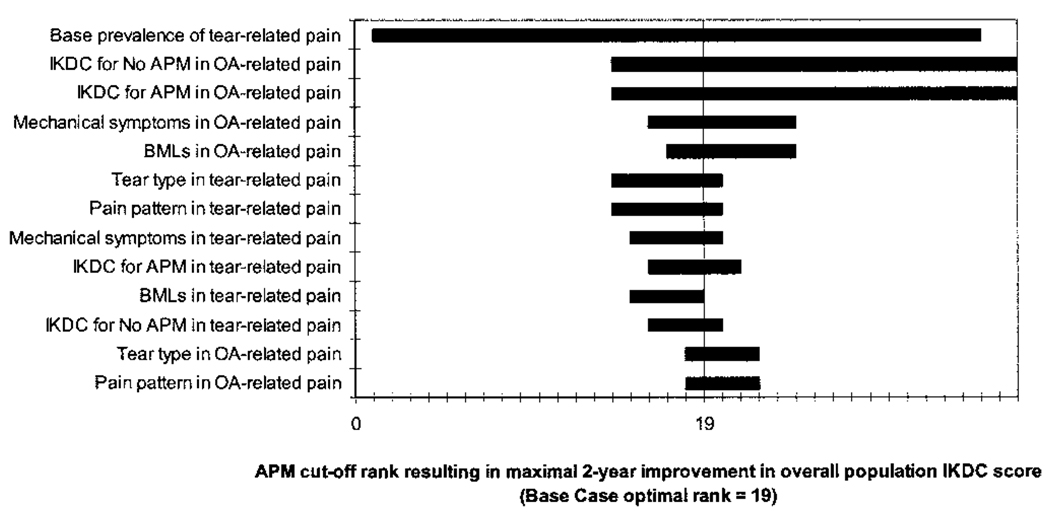
Results of sensitivity analyses: maximizing 2-year IKDC scores
Varying input assumptions (as above) similarly had little impact on the APM cutoff rank that yielded the greatest improvement in the overall population IKDC score. The results of the one-way sensitivity analyses are shown in a tornado diagram (Figure 3). Each horizontal bar represents an uncertain input data parameter. A given horizontal bar denotes how much the optimal cutoff rank (i.e., the cutoff that produces a maximal 2-year improvement in IKDC score for the entire population) fluctuates when the parameter of interest is varied over its plausible range. Therefore, wider bars represent instances where the optimal cutoff result is sensitive to the uncertainty in the input data; narrower bars represent instances where the optimal cutoff result is robust in the face of input data uncertainty. The vertical axis is located at the base-case optimal rank (optimal rank of 19). For example, varying the improvement in the IKDC score for performing APM in individuals with tear-related pain from 25 to 70 points changed the optimal cutoff rank for performing APM from rank 16 to 21.
Figure 3.
Tornado diagram demonstrating the impact of one-way sensitivity analyses of all model assumptions on the operable cutoff rank resulting in maximal improvement in 2-year overall population International Knee Documentation Committee (IKDC) scores. Bars show the variation from the optimal cutoff (identified in the base-case analysis and the point at which maximal outcomes are achieved for the population) that is produced by varying each model assumption, listed along the vertical axis, through the full range of its plausible values. APM = arthroscopic partial meniscectomy; OA = osteoarthritis; BMLs = bone marrow lesions.
For 10 of the 13 variables, the one-way sensitivity analyses reversed the treatment (from APM to nonoperative treatment or vice versa) for <6% of the population. Varying the base prevalence from 0% to 90% changed treatment for 96.9% of the population; 80.9% would experience a change in treatment when the improvements in 2-year IKDC scores for individuals with OA-related pain receiving either nonoperative therapy or APM were varied. Therefore, with the exception of the base prevalence of tear-related pain and clinical outcomes for OA-related pain, the decision to perform APM or treat conservatively is invariant across all of the assumptions in the input data for >90% of the population.
We also examined the effects of varying our base prevalence assumption simultaneously with APM efficacy. Ranging the base prevalence of tear-related pain from 0% to 30% while simultaneously varying assumptions regarding APM efficacy altered the maximal improvement in population IKDC score by ≤6 points, except when APM efficacy in tear-related pain and nonoperative treatment efficacy in OA-related pain were lowered simultaneously and all of the outcomes decreased in parallel. Under our worst-case scenario for APM (i.e., assuming no benefit for tear-related pain treated nonoperatively, maximal harm for OA-related pain undergoing APM, and reduced clinical benefit for tear-related pain undergoing APM), the maximal improvement in IKDC score ranged from 20.6 to 25.0. (Further results of the multi-way sensitivity analyses are shown in Supplementary Appendix B, available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home.)
Omitting each indicator from the analysis in sequence produced a change in treatment for <9% of the population compared with the base-case analysis. ROC curve analysis similarly demonstrated little impact of removing each indicator sequentially on the overall ability to discriminate between individuals with tear- versus OA-related pain. The total AUC for the base-case ROC curve was 92.02; AUC values for these sensitivity analyses were 86.2–90.0 (ROC curves are shown in Supplementary Appendix C, available in the online version of this article at http://www3.interscience.wiley.com/journal/77005015/home).
DISCUSSION
We combined Bayesian theory and decision analysis to create an indicator ranking to examine the effects of different cutoffs for performing APM on a hypothetical population of middle-aged individuals with knee pain, degenerative meniscal tear, and OA. Our analysis demonstrated that readily available information can effectively distinguish between individuals with a high probability of operative success and those unlikely to benefit from APM. Under assumptions favoring APM, to optimize clinical outcomes and the proportion receiving favorable treatment, one should select a cutoff for performing APM from the middle ranks 17–23, which results in less than one-third of the population undergoing APM. Because ranks 17–23 encompass individuals with more indeterminate clinical findings (e.g., rank 18: Probable mechanical symptoms and Increased pain pattern but Low tear type and Severe bone marrow lesions) and contain a small proportion of the population, shifting the cutoff within these ranks had little effect on population outcomes or the proportion receiving favorable treatment. This prediction was invariant for more than 90% of the population across a wide range of assumptions, but was sensitive to the prevalence of tear-related pain and certain outcome assumptions. Assuming either that nonoperative treatment has no clinical benefit for OA-related pain or that APM provides clinical relief for OA-related pain at 2 years did drive the model to favor performing APM on everyone, regardless of rank. Although scarce data are available, neither assumption is likely to be routinely true. The model was also sensitive to reductions in APM efficacy because decreases in efficacy lowered the population outcomes and led to fewer APMs. This assumption may well be clinically accurate and would best be addressed by randomized clinical trials with adequate followup.
There are limitations to our analysis. The assumption of independence among our indicators is likely inaccurate. We addressed this using a highly conservative alternative assumption, complete dependence, and this did not alter our findings. We chose to include a history of mechanical symptoms over physical maneuvers due to their limited reproducibility (20) and sensitivity, particularly in OA (21). Our study also only considered short-term outcomes. Given data supporting APM as a risk factor for OA development and progression (22–25), this may underestimate the negative impact of performing APM in this population. Also, because observational data describe worse outcomes and higher complication rates following APM in individuals with OA and up to 25% of individuals undergo reoperation after APM (9–11,23,26–30), considering cumulative quality of life (e.g., quality-adjusted life years) rather than isolated 2-year outcomes would likely yield even lower population benefits after APM. Although we acknowledge that these indicators are imperfect, we leveraged generally accepted clinical concepts to improve decision making where limited data exist to guide care and are unlikely to be available in the near future.
Twenty-seven million Americans have OA, and this number is rising (31). The use of MRI in individuals with nonspecific knee pain is also rising (32). Because up to 80% of individuals with knee OA have meniscal tears on MRI (3), which are commonly addressed using APM, the decision to perform APM in this population constitutes a staggering public health dilemma. Our findings support the urgent need for research defining the efficacy of APM in individuals with OA. Although there are already more than 500,000 APMs performed in individuals with concomitant OA each year in the US, we do not know whether APM is under- or overused in this population. Our findings support the fact that easily obtainable clinical information can effectively distinguish between individuals likely and unlikely to benefit from APM. Given this discrimination, there may be limited value in eliciting more or better clinical predictors. Short-term clinical trials are unlikely to address the relevant questions regarding whether or not to perform APM in individuals with OA. A large randomized clinical trial with an extended followup period to accurately define clinical outcomes and the potential negative downstream effects of APM in these individuals is needed. While physicians await the results of such a trial, the analysis presented in this study may help guide decision making in patients with meniscal tears and concomitant knee OA.
Supplementary Material
Acknowledgments
Dr. Suter’s work was supported by an NIH Mentored Career Development Award (K23-AR054095-01) and an Arthritis Foundation Arthritis Investigator Award. Dr. Fraenkel’s work was supported by the NIH (grant K23-AR048826). Dr. Losina’s work was supported by an Arthritis Foundation Innovative Research Grant and in part by the NIH/National Institute of Arthritis and Musculoskeletal and Skin Diseases (grants R01-AR053112, P60-AR-47782, K24-02123, and R01-AR55557). Dr. Katz’s work was supported in part by the NIH/National Institute of Arthritis and Musculoskeletal and Skin Diseases (grants R01-AR053112, P60-AR-47782, K24-02123, and R01-AR55557).
Footnotes
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Suter had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Suter, Fraenkel, Losina, Katz, Gomoll, Paltiel.
Acquisition of data. Suter, Losina, Paltiel.
Analysis and interpretation of data. Suter, Fraenkel, Losina, Katz, Gomoll, Paltiel.
REFERENCES
- 1.Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. 2008;59:1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gordon AC, Branson J, Simmons C, Berland KA, Willsey DS, Andrews AL, et al. Over-utilization of MRI in the osteoarthritis patient; American Academy of Orthopaedic Surgeons 75th Annual Meeting; San Francisco (CA): AAOS; 2008. p. P145. [Google Scholar]
- 3.Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85A:4–9. doi: 10.2106/00004623-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 4.National Center for Health Statistics. Number of ambulatory surgery procedures by procedure category in the US: 1996. Hyattsville (MD): NCHS; 1998. p. 7. [Google Scholar]
- 5.Herrlin S, Hallander M, Wange P, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthosc. 2007;15:393–401. doi: 10.1007/s00167-006-0243-2. [DOI] [PubMed] [Google Scholar]
- 6.Macklin R. The ethical problems with sham surgery in clinical research. N Engl J Med. 1999;341:992–996. doi: 10.1056/NEJM199909233411312. [DOI] [PubMed] [Google Scholar]
- 7.Creel AH, Losina E, Mandl LA, Marx RJ, Mahomed NN, Martin SD, et al. An assessment of willingness to participate in a randomized trial of arthroscopic knee surgery in patients with osteoarthritis. Contemp Clin Trials. 2005;26:169–178. doi: 10.1016/j.cct.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Stoller DW, Martin C, Crues J, Kaplan L, Mink J. Meniscal tears: pathologic correlation with MR imaging. Radiology. 1987;163:731–738. doi: 10.1148/radiology.163.3.3575724. [DOI] [PubMed] [Google Scholar]
- 9.Schimmer RC, Brulhart KB, Duff C, Glinz W. Arthroscopic partial meniscectomy: a 12-year follow-up and two-step evaluation of the long-term course. Arthroscopy. 1998;14:136–142. doi: 10.1016/s0749-8063(98)70031-3. [DOI] [PubMed] [Google Scholar]
- 10.Katz JN, Harris TM, Larson MG, Krushell RJ, Brown CH, Fossel AH, et al. Predictors of functional outcomes after arthroscopic partial meniscectomy. J Rheumatol. 1992;19:1938–1942. [PubMed] [Google Scholar]
- 11.Meredith DS, Losina E, Mahomed N, Wright J, Katz JN. Factors predicting functional and radiographic outcomes after arthroscopic partial meniscectomy: a review of the literature. Arthroscopy. 2005;21:211–223. doi: 10.1016/j.arthro.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Neutra RR. Indications for the surgical treatment of suspected acute appendicitis: a cost effectiveness approach. In: Bunker JP, Barnes BA, Mosteller F, editors. Costs, risks, and benefits of surgery. New York: Oxford University Press; 1977. pp. 277–307. [Google Scholar]
- 13.Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–1115. doi: 10.1056/NEJMoa0800777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterfy CG, Guermazi A, Zaim S, Tirman PF, Miaux Y, White D, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–190. doi: 10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–2992. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 16.Bayes T. Studies in the history of probability and statistics: IX. Thomas Bayes’ essay towards solving a problem in the doctrine of chances. Biometrika. 1958;45:296–315. [Google Scholar]
- 17.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34:1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 18.Roos EM, Roos HP, Ryd L, Lohmander LS. Substantial disability 3 months after arthroscopic partial meniscectomy: a prospective study of patient-relevant outcomes. Arthroscopy. 2000;16:619–626. doi: 10.1053/jars.2000.4818. [DOI] [PubMed] [Google Scholar]
- 19.Vincken PW, Ter Braak BP, van Erkel AR, Coerkamp EG, Mallens WM, Bloem JL. Clinical consequences of bone bruise around the knee. Eur Radiol. 2006;16:97–107. doi: 10.1007/s00330-005-2735-8. [DOI] [PubMed] [Google Scholar]
- 20.Dervin G, Stiell I, Wells G, Rody K, Grabowski J. Physicians’ accuracy and interrater reliability for the diagnosis of unstable meniscal tear in patients having osteoarthritis of the knee. Can J Surg. 2001;44:267–274. [PMC free article] [PubMed] [Google Scholar]
- 21.Lowery D, Farley T, Wing D, Sterett WI, Steadman JR. A clinical composite score accurately detects meniscal pathology. Arthroscopy. 2006;22:1174–1179. doi: 10.1016/j.arthro.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 22.Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE. Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: a prospective cohort study. Am J Sports Med. 2008;36:1717–1725. doi: 10.1177/0363546508316770. [DOI] [PubMed] [Google Scholar]
- 23.Rangger C, Klestil T, Gloetzer W, Kemmler G, Benedetto KP. Osteoarthritis after arthroscopic partial meniscectomy. Am J Sports Med. 1995;23:240–244. doi: 10.1177/036354659502300219. [DOI] [PubMed] [Google Scholar]
- 24.Cicuttini F, Forbes A, Yuanyuan W, Rush G, Stuckey SL. Rate of knee cartilage loss after partial meniscectomy. J Rheumatol. 2002;29:1954–1956. [PubMed] [Google Scholar]
- 25.Covall DJ, Wasilewski SA. Roentgenographic changes after arthroscopic meniscectomy: five-year follow-up in patients more than 45 years old. Arthroscopy. 1992;8:242–246. doi: 10.1016/0749-8063(92)90044-c. [DOI] [PubMed] [Google Scholar]
- 26.Englund M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford) 2001;40:631–639. doi: 10.1093/rheumatology/40.6.631. [DOI] [PubMed] [Google Scholar]
- 27.Benedetto KP, Rangger C. Arthroscopic partial meniscectomy: 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1993;1:235–238. doi: 10.1007/BF01560216. [DOI] [PubMed] [Google Scholar]
- 28.Barrett GR, Treacy SH, Ruff CG. The effect of partial lateral meniscectomy in patients > or = 60 years. Orthopedics. 1998;21:251–257. doi: 10.3928/0147-7447-19980301-06. [DOI] [PubMed] [Google Scholar]
- 29.Rand JA. Arthroscopic management of degenerative meniscus tears in patients with degenerative arthritis. Arthroscopy. 1985;1:253–258. doi: 10.1016/s0749-8063(85)80093-1. [DOI] [PubMed] [Google Scholar]
- 30.Fauno P, Nielsen AB. Arthroscopic partial meniscectomy: a long-term follow-up. Arthroscopy. 1992;8:345–349. doi: 10.1016/0749-8063(92)90066-k. [DOI] [PubMed] [Google Scholar]
- 31.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Solomon DH, Katz JN, Carrino JA, Schaffer JL, Bohn RL, Mogun H, et al. Trends in knee magnetic resonance imaging. Med Care. 2003;41:687–692. doi: 10.1097/01.MLR.0000062705.24024.9F. [DOI] [PubMed] [Google Scholar]
- 33.Zanetti M, Pfirrmann C, Schmid M, Seifert B, Hodler J. Patients with suspected meniscal tears: prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. Am J Roentgenol. 2003;181:635–641. doi: 10.2214/ajr.181.3.1810635. [DOI] [PubMed] [Google Scholar]
- 34.Felson DT, Niu J, McClennan C, Sack B, Aliabadi P, Hunter DJ, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147:534–540. doi: 10.7326/0003-4819-147-8-200710160-00005. [DOI] [PubMed] [Google Scholar]
- 35.Booth RE. Arthroscopy before arthroplasty: a con or a comfort? J Arthroplasty. 2004;19 Suppl 1:2–4. doi: 10.1016/j.arth.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 36.Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med. 2001;134:541–549. doi: 10.7326/0003-4819-134-7-200104030-00007. [DOI] [PubMed] [Google Scholar]
- 37.Sowers MF, Hayes C, Jamadar D, Capul D, Lachance L, Jannausch M, et al. Magnetic resonance-detected subchondral bone marrow and cartilage defect characteristics associated with pain and x-ray-defined knee osteoarthritis. Osteoarthritis Cartilage. 2003;11:387–393. doi: 10.1016/s1063-4584(03)00080-3. [DOI] [PubMed] [Google Scholar]
- 38.Torres L, Dunlop DD, Peterfy C, Guermazi A, Prasad P, Hayes KW, et al. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2006;14:1033–1040. doi: 10.1016/j.joca.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 39.the Société Française d’Arthroscopie. Chatain F, Adeleine P, Chambat P, Neyret P. A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy. 2003;19:842–849. doi: 10.1016/s0749-8063(03)00735-7. [DOI] [PubMed] [Google Scholar]
- 40.Biedert RM. Treatment of intrasubstance meniscal lesions: a randomized prospective study of four different methods. Knee Surg Sports Traumatol Arthrosc. 2000;8:104–108. doi: 10.1007/s001670050195. [DOI] [PubMed] [Google Scholar]
- 41.Rosseland LA, Solheim N, Stubhaug A. Pain and disability 1 year after knee arthroscopic procedures. Acta Anaesthesiol Scand. 2008;52:332–337. doi: 10.1111/j.1399-6576.2007.01541.x. [DOI] [PubMed] [Google Scholar]
- 42.Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 43.Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097–1107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.