In vitro fertilization (IVF) is a well-documented risk factor for thromboembolic complications [1]. Suspected complications have included jugular venous thrombosis [2], carotid thrombosis [3], and fatal cerebral infarction [4]. Possible plasma factor compositional reasons for the link between IVF and thrombotic events include activated protein C resistance [5,6], decreased protein S [5] and antithrombin (AT) [5,7], and increased fibrinogen [5,7,8] and factor (F) VIII [9]. These factors could potentiate increased thrombin generation.
Generation of thrombin, a key enzyme in blood coagulation, has been suggested as a potential marker of risk evaluation [10–12]. Previous studies on citrated plasma using calibrated automated thrombography showed that women using oral contraceptives have shorter thrombin generation lag times and higher peak height [13]. In a computational and empirical study, women on oral contraceptives also had an increased rate and maximum level of thrombin generation in response to a 5 pM tissue factor (TF) stimulus than women not using oral contraceptives [14]. In addition, Harnett et al. noticed a significant decrease in clot time in women undergoing IVF using thrombelastography [15].
In this pilot study, we investigated the effect of high levels of endogenous estrogen on plasma compositional influence on thrombin generation in seven women receiving follicle stimulating hormone in preparation for IVF. Blood was drawn on two separate occasions. Baseline studies were obtained on menstrual cycle day 2 or 3, one month prior to the start of an IVF cycle. A second blood draw took place on the final day of stimulation when estradiol levels would be at their peak. Estradiol rose during treatment (29 pg/mL (SD 12) to 2773 pg/mL (SD 2076) and successful pregnancy occurred in five of seven cases. Factor levels were measured on each of the individuals before and after stimulation for the coagulation proteins FII, FV, FVII, FVIII, FIX, FX, AT and total tissue factor pathway inhibitor (TFPI). FII, FV, FVII, FVIII, FIX and FX were measured by using a Stago STA-R, in which the subjects plasma is added to plasma deficient in the factor to be measured and the degree of correction of clotting time is determined. The degree of the correction is compared with that obtained by adding a normal plasma to the same system. AT is measured using a STA-Stachrom AT Colorimetric assay and total TFPI was measured by ELISA (Diagnostica Stago, France). Factor levels expressed as a percent of normal were translated into molar (M) concentrations using literature values for the mean plasma concentrations [16]. The Wilcoxon signed rank test was utilized for all comparisons, where a p-value ≤0.05 was considered significant. All data are presented as the mean (SD).
Studying patients in IVF cycles permits the observation of thrombin generation over a wide range of estradiol levels. As estradiol rose, protein concentrations were within the normal range. Significant differences after stimulation in coagulation factor concentrations included decreases in FV (25 nM (SD 2) to 21 nM (SD 3); p=0.02) and AT (3.6 μM (SD 0.4) to 3.2 μM (SD 0.3); p=0.05). Other non-significant changes were: a decrease in FII (1.5 μM (SD 0.18) to 1.4 μM (SD 0.18); p=0.12) and TFPI (1.8 nM (SD 0.5) to 1.5 nM (SD 0.3); p=0.08) and an increase in FVIII (1.0 nM (SD 0.2) to 1.2 nM (SD 0.4); p=0.30). Similar levels were observed in FVII (from 9.2 nM (SD 0.9) to 9.2 nM (SD 1.5); p=1.00), FIX (89 nM (SD 14) to 92 nM (SD 14); p=0.61) and FX (181 nM (SD 22) to 185 nM (SD 22); p=0.59).
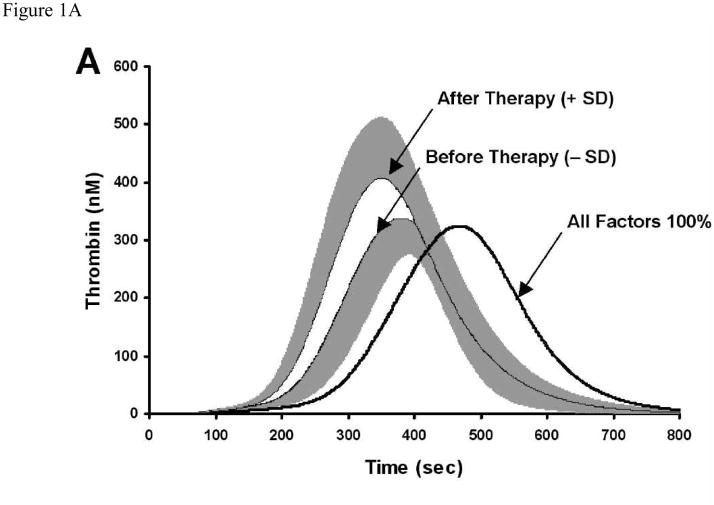
We modeled hypothetical TF-induced thrombin generation utilizing a deterministic simulation system for blood coagulation dynamics [17–19]. Thrombin generation was evaluated by parameters that reflect the global qualities of the thrombin profile [14] which includes: time to 10 nM thrombin (clot time, CT), maximum level (MaxL) and rate (MaxR) of thrombin generation and the times at which they are reached, TMaxL and TMaxR, respectively. Before treatment, the mean simulated thrombin generation profile for the group was shifted in the hypercoagulable direction relative to a mean profile where all factors are at 100% of the mean physiologic concentration (Figure 1A). In six of the seven women, the increased hormone levels coincided with a shift towards a faster and more prominent thrombin generation profile after IVF.
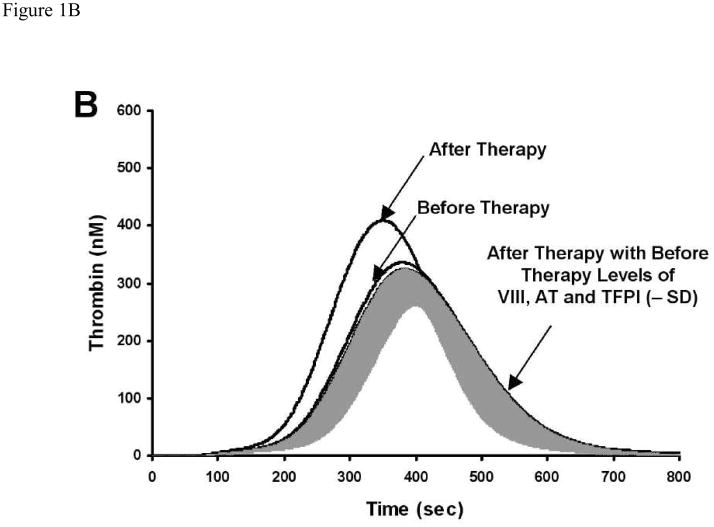
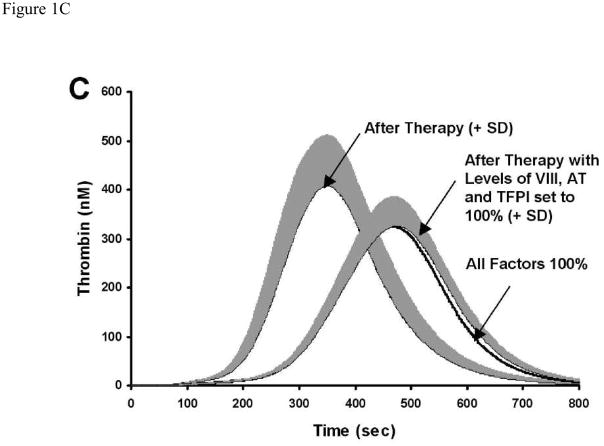
Figure 1. The influence of 100-fold rise in estradiol on simulated thrombin generation.
A) IVF subjects (n=7) before and after gonadotropin stimulation and a theoretical control (physiologic mean). The data are shown as mean and SD in gray (+SD for after therapy and −SD for before stimulation) B) IVF subjects at basal, after stimulation and after stimulation levels of FVIII, AT and TFPI set back to basal levels (shown as the mean and −SD in gray). C) IVF subjects after stimulation (mean +SD), a theoretical control (physiologic mean), and after stimulation levels of FVIII, AT and TFPI set back to theoretical control levels (mean −SD in gray).
At high levels of endogenous estradiol, the CT decreased (151 s (SD 26) to 129 s (SD 12); p=0.03) and the MaxL increased (382 nM (SD 5) to 444 nM (SD 89); p=0.05) with a shortened TMaxL (394 s (SD 46) to 355 s (SD 34); p=0.02). Likewise, the MaxR increased (2.90 nM/s (SD 0.66) to 3.76 nM/s (SD 1.03); p=0.03) and the TMaxR decreased (312 s (SD 36) to 281 s (SD 26); p=0.02). In addition, the concentration of estradiol after treatment was positively correlated (r2 = 0.86) with the MaxL. Although this is a limited study, the two individuals who were not successful in becoming pregnant had the highest MaxL and the fastest CT. These findings are in agreement with Rogolino et al. who observed significantly higher thrombin-antithrombin levels in ovarian hyperstimulation syndrome patients who did not become pregnant [20].
The influence of each coagulation protein (or set of proteins) on thrombin generation was analyzed by systematically running independent thrombin generation simulations [21]. Each simulation had one (or more) of the proteins set to the level it was prior to gonadotropin stimulation, while leaving all others at post-stimulation levels. In four of the six women who had their profile shift in a prothrombotic direction, adjusting the after stimulation levels of FVIII, AT and TFPI to the levels they were at before stimulation, resulted in near identical thrombin generation curves to those generated when all proteins were at before stimulation (Figure 1B). Despite the fact that pre- to post-gonadotropin stimulation differences in FV, FVII, FIX and FX existed, adjustments of these factors did not affect the thrombin generation curve. Additionally, adjusting the after gonadotropin stimulation levels of FVIII, TFPI and AT to their mean physiologic concentrations (while leaving other factors at their after stimulation level) produces a thrombin generation curve similar to a theoretical control curve where values are set at mean physiologic concentrations (Figure 1C).
These studies generate hypothetical thrombin generation profiles which do not include the contribution of the anticoagulant protein C pathway, the contact pathway and the vasculature. The numerical model that was used for these studies includes key plasma pro- and anti- coagulants of the TF pathway to thrombin generation that are evaluated in clinical laboratories. This model correlates well to empirical models describing the TF pathway [18,22–24].
In conclusion, women receiving IVF treatment in this pilot study who have normal but slightly prothrombotic thrombin generation profiles responded to high levels of hormones by becoming more prothrombotic. A systematic analysis of the plasma coagulation factors has isolated FVIII, AT and TFPI as the components most responsible for the additional procoagulant shift. This pattern of small concerted changes in the triad of FVIII, AT and TFPI levels may contribute to the prothrombotic state in some women undergoing IVF.
Acknowledgments
This work was supported by an NIH P01 HL46703 grant.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chan WS, Dixon ME. The “ART” of thromboembolism: A review of assisted reproductive technology and thromboembolic complications. Thromb Res. 2008;121:713–726. doi: 10.1016/j.thromres.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 2.Leibman Y, Ayalon M, Steiner IP. Internal Jugular Venous Thrombosis after In Vitro Fertilization. J Emerg Med. 2009 Jul;37(1):29–31. doi: 10.1016/j.jemermed.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 3.Martí E, Santamaria A, Mateo J, Tolosa A, Querol L, Viscasillas P, Fontcuberta J. Carotid thrombosis after in vitro fertilization: a relatively new thrombotic complication in women. Br J Haematol. 2008;141:897–899. doi: 10.1111/j.1365-2141.2008.07120.x. [DOI] [PubMed] [Google Scholar]
- 4.Cluroe AD, Synek BJ. A fatal case of ovarian hyperstimulation syndrome with cerebral infarction. Pathology. 1995;27:344–346. doi: 10.1080/00313029500169273. [DOI] [PubMed] [Google Scholar]
- 5.Biron C, Galtier-Dereure F, Rabesandratana H, Bernard I, Aguilar-Martinez P, Schved JF, Hedon B. Hemostasis parameters during ovarian stimulation for in vitro fertilization: results of a prospective study. Fertil Steril. 1997;67:104–109. doi: 10.1016/s0015-0282(97)81864-x. [DOI] [PubMed] [Google Scholar]
- 6.Curvers J, Nap AW, Thomassen MC, Nienhuis SJ, Hamulyak K, Evers JL, Tans G, Rosing J. Effect of in vitro fertilization treatment and subsequent pregnancy on the protein C pathway. Br J Haematol. 2001;115:400–407. doi: 10.1046/j.1365-2141.2001.03118.x. [DOI] [PubMed] [Google Scholar]
- 7.Aune B, Hoie KE, Oian P, Holst N, Østerud B. Does ovarian stimulation for in-vitro fertilization induce a hypercoagulable state? Hum Reprod. 1991;6:925–927. doi: 10.1093/oxfordjournals.humrep.a137461. [DOI] [PubMed] [Google Scholar]
- 8.Michelon J, Petracco A, Bruxel DM, Moretto M, Badalotti M. [Analysis of coagulation parameters in patients undergoing controlled ovarian hyperstimulation for in vitro fertilization] Rev Assoc Med Bras. 2002;48:345–347. doi: 10.1590/s0104-42302002000400042. [DOI] [PubMed] [Google Scholar]
- 9.Bremme K, Wramsby H, Andersson O, Wallin M, Blombäck M. Do lowered factor VII levels at extremely high endogenous oestradiol levels protect against thrombin formation? Blood Coagul Fibrinolysis. 1994;5:205–210. doi: 10.1097/00001721-199404000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Hron G, Kollars M, Binder BR, Eichinger S, Kyrle PA. Identification of patients at low risk for recurrent venous thromboembolism by measuring thrombin generation. JAMA. 2006;296:397–402. doi: 10.1001/jama.296.4.397. [DOI] [PubMed] [Google Scholar]
- 11.Brummel-Ziedins K, Vossen CY, Rosendaal FR, Umezaki K, Mann KG. The plasma hemostatic proteome: thrombin generation in healthy individuals. J Thromb Haemost. 2005;3:1472–1481. doi: 10.1111/j.1538-7836.2005.01249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hemker HC, Al Dieri R, DE Smedt E, Béguin S. Thrombin generation, a function test of the haemostatic-thrombotic system. Thromb Haemost. 2006;96:553–561. [PubMed] [Google Scholar]
- 13.Tchaikovski SN, van Vliet HA, Thomassen MC, Bertina RM, Rosendaal FR, Sandset PM, Helmerhorst FM, Tans G, Rosing J. Effect of oral contraceptives on thrombin generation measured via calibrated automated thrombography. Thromb Haemost. 2007;98:1350–1356. [PubMed] [Google Scholar]
- 14.Brummel-Ziedins KE, Vossen CY, Butenas S, Mann KG, Rosendaal FR. Thrombin generation profiles in deep venous thrombosis. Journal of Thrombosis and Haemostasis. 2005;3:2497–2505. doi: 10.1111/j.1538-7836.2005.01584.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harnett MJ, Bhavani-Shankar K, Datta S, Tsen LC. In vitro fertilization-induced alterations in coagulation and fibrinolysis as measured by thromboelastography. Anesth Analg. 2002;95:1063–6. doi: 10.1097/00000539-200210000-00050. table. [DOI] [PubMed] [Google Scholar]
- 16.Brummel-Ziedins K, Orfeo T, Jenny NS, Everse SJ, Mann KG. Blood coagulation and fibrinolysis. In: Greer JP, Foerster J, Lukens J, Rodgers GM, Paraskevas F, Glader B, editors. Wintrobe’s Clinical Hematology. Philidelphia: Lippencott Williams & Wilkins; 2003. pp. 677–774. [Google Scholar]
- 17.Jones KC, Mann KG. A model for the tissue factor pathway to thrombin. II. A mathematical simulation [published erratum appears in J Biol Chem 1995 Apr 14;270(15):9026] J Biol Chem. 1994;269:23367–23373. [PubMed] [Google Scholar]
- 18.Hockin MF, Jones KC, Everse SJ, Mann KG. A model for the stoichiometric regulation of blood coagulation. J Biol Chem. 2002;277:18322–18333. doi: 10.1074/jbc.M201173200. [DOI] [PubMed] [Google Scholar]
- 19.Butenas S, Orfeo T, Gissel MT, Brummel KE, Mann KG. The significance of circulating factor IXa in blood. J Biol Chem. 2004;279:22875–22882. doi: 10.1074/jbc.M400531200. [DOI] [PubMed] [Google Scholar]
- 20.Rogolino A, Coccia ME, Fedi S, Gori AM, Cellai AP, Scarselli GF, Prisco D, Abbate R. Hypercoagulability, high tissue factor and low tissue factor pathway inhibitor levels in severe ovarian hyperstimulation syndrome: possible association with clinical outcome. Blood Coagul Fibrinolysis. 2003;14:277–282. doi: 10.1097/01.mbc.0000061296.28953.d0. [DOI] [PubMed] [Google Scholar]
- 21.Brummel-Ziedins K, Undas A, Orfeo T, Gissel M, Butenas S, Zmudka K, Mann KG. Thrombin generation in acute coronary syndrome and stable coronary artery disease: dependence on plasma factor composition. J Thromb Haemost. 2008;6:104–110. doi: 10.1111/j.1538-7836.2007.02799.x. [DOI] [PubMed] [Google Scholar]
- 22.Brummel-Ziedins K, Rivard GE, Pouliot RL, Butenas S, Gissel M, Parhami-Seren B, Mann KG. Factor VIIa replacement therapy in factor VII deficiency. J Thromb Haemost. 2004;2:1735–1744. doi: 10.1111/j.1538-7836.2004.00922.x. [DOI] [PubMed] [Google Scholar]
- 23.Orfeo T, Brummel-Ziedins KE, Gissel M, Butenas S, Mann KG. The nature of the stable blood clot procoagulant activities. J Biol Chem. 2008;283:9776–9786. doi: 10.1074/jbc.M707435200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Butenas S, Orfeo T, Brummel-Ziedins KE, Mann KG. Influence of bivalirudin on tissue factor-triggered coagulation. Blood Coagul Fibrinolysis. 2007;18:407–414. doi: 10.1097/MBC.0b013e32814fcdb8. [DOI] [PubMed] [Google Scholar]