Abstract
Objective
To characterize the knowledge, attitudes, and beliefs (KAB) regarding childhood obesity among parents of Latino preschoolers.
Methods
Three hundred sixty-nine Mexican immigrant parents of children ages 2–5 were interviewed. Children were weighed and measured.
Results
Parents underestimated their own child’s weight status and had high levels of perceived control over their children’s eating and activity behaviors. Parents of overweight (≥95%ile-for-age-and-sex BMI) versus nonoverweight (<95%ile BMI) children did not differ in their beliefs about ideal child body size.
Conclusion
Latino parents of overweight children did not differ from parents of nonoverweight children with respect to their KAB about childhood obesity.
Keywords: childhood obesity, health beliefs, Mexican Americans
Childhood obesity continues to be a growing epidemic1 even in the very young. Children of ethnic minorities, including children of Mexican American origin, are much more likely to be overweight than the general population,1–5 with 21% of Mexican American children ages 2–19 classified as overweight (≥95%ile age- and sex-specific BMI), compared to 16% of the general population.1 Among children ages 2–5, 17% of Mexican American children are overweight, compared to 12% of the general population.1 Childhood obesity is also an increasing problem in Mexico, where the prevalence of childhood obesity is beginning to approach that of the Mexican American population in the United States.6,7 Rates of overweight among subpopulations of Mexican American children may be even higher: in a school-based sample of kindergarteners from primarily Mexican immigrant families in Chicago (n=250), the prevalence of overweight was 23%.8 The high prevalence of obesity among preschool children is particularly disturbing, as it heralds an accelerating risk of obesity-related health problems as these young people grow to adulthood. Obesity in childhood tracks closely into adult obesity, as even young children who are obese generally remain obese as adults.9–11 Another recent study demonstrated that childhood obesity may be even more highly correlated with adolescent obesity (with a correlation coefficient greater than 0.90 for a 4-year follow-up period) among low-income Mexican American children than in the general population.12
If current trends continue based on projections from National Health and Nutrition Examination Surveys (NHANES) from 1971 to 2004, the entire adult population of the United States of America will be overweight or obese by the year 2048.13 Using the same projections and conservative health care cost estimations, the health care costs directly attributable to obesity are estimated to reach approximately $900 billion US/year by the year 2030.13 Thus, urgent measures are needed to prevent childhood obesity and to derail this impending public health crisis, both in the United States and abroad.
Any program to address the problem of childhood obesity must start with the parents, as parents’ health beliefs strongly influence children’s diet14 and physical activity.15 Several studies have shown that parents tend to underestimate their children’s weight status.8,16–20 For example, an analysis of NHANES III (1988–1994) found that one third of parents of over-weight children underestimated their children’s weight status.16 Studies of several groups of African American parents have consistently found that they underestimate their children’s weight status and their children’s health risks when compared with national estimates from NHANES.17–20
Few studies have explicitly focused on Latino parents’ health beliefs about their children’s weight status.7,21 One study conducted in Mexico found that the majority of parents of overweight children did not perceive their children to be at any health risk,7 whereas another survey of predominantly Latino parents of preschoolers in the United States also found that many parents underestimated their children’s weight status.21 Two studies conducted in ethnically diverse Latino populations found that mothers of all countries of origin generally underestimated child weight status when asked to rate drawings of children of different body sizes.22,23 However, no known published studies have focused specifically on Latinos of Mexican origin, who are the largest group of Latinos in the United States and whose health beliefs may differ significantly from those of Caribbean immigrants. Indeed, experts in Latino child health emphasize that any research conducted among Latino immigrants to the United State measure and report results by country or area of origin, as different subgroups have very disparate health risks and profiles.24
Thus, the present study had 2 objectives:
Characterize parental knowledge, attitudes, and health beliefs about childhood obesity in a sample of primarily Mexican-origin Latino parents in Chicago.
Determine whether the knowledge, attitudes, and beliefs of parents with overweight children differ from those of parents with nonoverweight children.
METHODS
Study Design and Study Population
Interviewers administered questionnaires among a convenience sample of parents of children ages 2–5 in an outpatient clinic waiting room. The survey was conducted at an inner-city community health center that serves a predominantly Mexican immigrant population in Chicago, a city that has the largest concentration of Mexican immigrants in the United States after California and the Southwest.25
Instrument Development
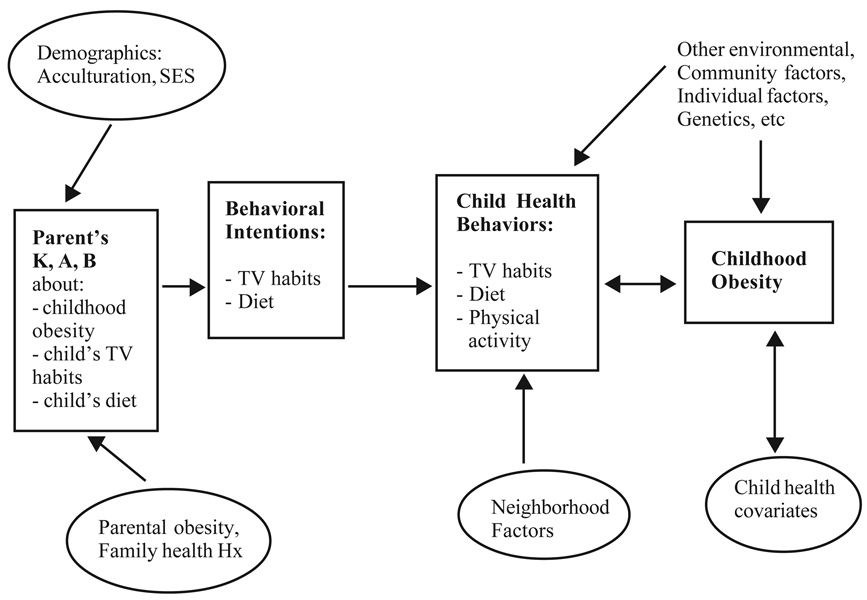
We developed an instrument to determine Latino parents’ health knowledge, attitudes, and beliefs about their own child’s diet (particularly fast food consumption), activities, weight status, and childhood obesity in general. We adapted and revised some questions from existing instruments14,17,18,26 and developed further questions to address parents’ knowledge, attitudes, and health beliefs about children’s diet, activity, and weight status. Questionnaire development was guided by a conceptual model for behavior change27 that contains elements of social learning theory,28 the theory of planned behavior,29 the health belief model,30 and the ecological model.31 The model is reproduced in Figure 1. Application of the model assumes that parents are more likely to change their behavior if they understand the health consequences of obesity, feel empowered to make changes in their lives, and live in a community in which such changes are accepted or encouraged.
Figure 1.
Conceptual Model for Behaviors Leading to Childhood Obesity
Survey questions were designed to target the different domains and behavioral constructs of the conceptual model. For example, parental health beliefs about childhood obesity in general were determined by asking, “What do you think is the earliest age that obesity starts in babies or children?” with an open-ended response format. Health knowledge about obesity was measured with the following open-ended question: “If you knew a child that was very overweight, what health problems would you worry about?”
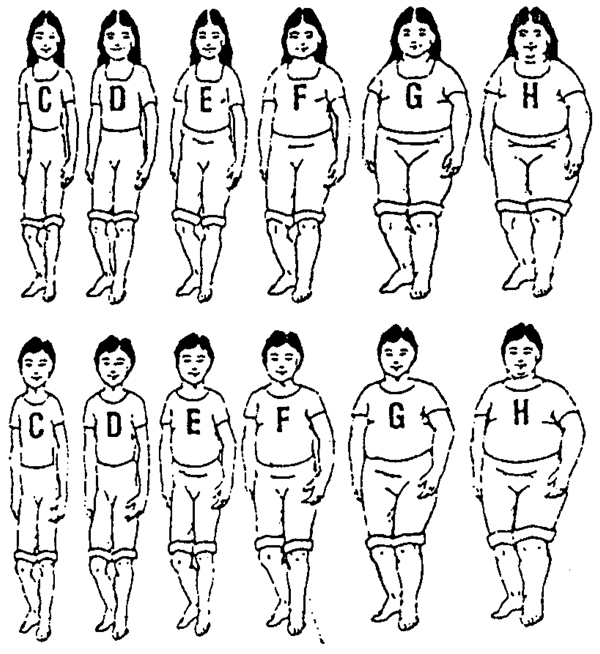
Parental self-efficacy about childhood obesity was measured by the following question: “How much control do parents have over how much their child weighs?” with Likert-type response options of “a lot,” “a little,” “none,” and “don’t know.” Line drawings of boys and girls were adapted from a previous instrument32 and used to further elucidate parental health beliefs. As shown in Figure 2, the 6 line drawings depict children whose appearance range from relatively thin (C) to markedly obese (H). Parents were asked to view the set of line drawings and to select the child they thought most closely resembled their child, which they “most wished their child looked like” (ideal body size) and which looked the “least healthy” from among those depicted. The 2 drawings depicting the thinnest children in the original series were discarded because they might actually be considered the least healthy looking, and the purpose of using the drawings was to force parents to choose between a very overweight versus a relatively thin child as looking the “least healthy” (Figure 1).
Figure 2.
Line Drawings of Children
Although obesity prevention efforts for older children are ideally targeted to both child and parents, the best available evidence suggests that during the preschool years, parents (and mothers in particular) are the overwhelming decision makers regarding their children’s diet and activities rather than the children themselves.33, 34 Therefore, because prevention efforts in this age-group are best targeted primarily to parents, they alone were the focus of the current study.
Questions were written in English, translated into Spanish by native bilingual speakers, and then, to assure accuracy, back-translated into English by a bilingual speaker who had not seen the original English version. The items were then iteratively pretested in the field to assure good comprehension for a relatively low literacy population. A Mexican-origin bilingual, bicultural dietitian (M.S.-R.) experienced in working with the study population of interest participated in survey conception, development, and pretesting. The survey consisted of 65 items and generally took between 10 and 15 minutes to administer including the child weight and height measurements.
Subject Recruitment
Research assistants approached parents with young children in the clinic waiting room and told them of an ongoing study “about child health and nutrition.” Parents who met all eligibility criteria (mother or father of a child ages 2 to 5, lived in the same household with their child, and considered themselves Latino) were then asked to participate. Verbal informed consent was obtained. Bilingual, bicultural research assistants conducted face-to-face interviews in English or Spanish according to parental preference. Interviews were conducted Monday through Friday during regular clinic hours between September 2003 and March 2004. Parents were given a small toy for their child for participating in the study. We maintained anonymity by not collecting participant names or any other protected health information. The study was approved by the institutional review boards at the University of Chicago and Alivio Medical Center.
Participants
Of the 505 potential subjects who met the criteria for eligibility, 416 (82%) agreed to participate. Of those, 371 (89%) interviews contained enough data to be included in the analysis, whereas the remaining 45 (11%) were not used due to poor quality or missing height or weight data. Two children with identified chronic medical conditions likely to affect growth were excluded from the analysis. The final sample consisted of 369 subjects.
Anthropometric Measures
No universally accepted definition of obesity or overweight among young children exists, nor is there a universally accepted gold standard of measurement.35 Although imperfect, BMI has been proposed as a reasonable measure of body fatness for young children by the International Obesity Task Force.35 Child weight status was therefore determined by weighing and measuring each child on the clinic scale and stadiometer, and age-and sex-specific BMI percentile was determined for each child using 2000 CDC reference values.36 Children at or above the 95th percentile age- and sex-specific BMI percentile were considered overweight, children between the 5th and 94th percentiles were considered normal weight (including those between the 85th and 94th percentiles, who are more correctly classified as “at risk of overweight”), and children less than the 5th percentile were considered underweight per US Department of Health and Human Services (HHS) recommendations.37 Maternal and paternal height and weight were determined by self-report.
Statistical Analysis
The primary outcome measure was child BMI status (overweight versus nonoverweight). Bivariate associations were determined using chi-square tests for categorical data and t-tests for continuous variables with normal distributions.
RESULTS
Patient Demographics
Selected patient demographics and child health covariates are shown in Table 1. Ninety percent of respondents were mothers and 10% were fathers. Most of the mothers (335, or 91%) were born in Mexico; 24 (7%) were born in the United States, with the remainder born in South America (2%), Central American (1%), and Puerto Rico (0.5%). The median level of maternal education was 9 years, and only 31% of mothers had completed high school. Maternal English proficiency was also low, as 18% of mothers reported speaking English either well or very well whereas 81% reported speaking English not very well or not at all. Paternal education was also low, with a median educational level of 9 years for fathers, although a higher proportion of fathers spoke English either well or very well (40%) than did mothers. Nearly all of the surveys (99%) were conducted in Spanish. Median household income was $1100 per month, although only 205 respondents (56%) answered this question.
Table 1.
Patient Demographics and Health History by Child’s Overweight Status
| Overweight Children (>=95%ile BMI)* |
Nonoverweight Children (<95%ile BMI)* |
Total Sample |
|
|---|---|---|---|
| n, (%) | 78 (21%) | 291 (79%) | 369 (100%) |
| % male | 56 | 49 | 51 |
| Age in months, mean (s.d.) | 42 (11) | 40 (11) | 41 |
| % of mothers Mexican-born | 94 | 90 | 91 |
|
Maternal years in United States if foreign-born, mean (s.d.) |
8.6 (6.3) | 8.6 (5.9) | 8.6 |
| Years maternal education, mean (s.d.) | 9.0 (2.9) | 9.5 (3.1) | 9.4 |
| % born premature (<37 weeks gestation) | 8 | 8 | 8 |
| % born with birth weight >4000 grams | 11 | 12 | 12 |
| % born with birth weight <2500 grams | 4 | 7 | 7 |
Note.
Differences between overweight and nonoverweight children were nonsignificant (P>0.05) for every variable.
Child weight status
Seventy-eight of 369 children (21%) were overweight (at or above the 95th percentile age- and sex-adjusted BMI). Only 9/369 children (2%) were less than the 5th percentile or underweight, limiting comparisons to this group. Therefore, these underweight children were included in the “nonoverweight” group.
Parental weight status
Maternal height and weight were reported by only 204 of 369 respondents (55%). Even fewer paternal heights and weights were reported (169/369, or 46%). Therefore, we were unable to adequately assess the influence of parental weight status on respondents’ knowledge, attitudes, and beliefs about childhood obesity.
Parental Health Knowledge About Childhood Obesity
Parents demonstrated reasonably good knowledge about the health consequences of obesity. When asked to name specific health problems parents would worry about in an overweight child, 77% of all respondents named at least one of the following: heart problems (mentioned by 44%), diabetes (31%), asthma (27%), elevated cholesterol (15%), and hypertension (7%). Parents of overweight children did not differ from parents of nonoverweight children with respect to their health knowledge about obesity-related medical conditions: 72% of parents of overweight children mentioned at least one of these complications, compared to 78% of parents of nonoverweight children.
Perceived Parental Control Over Child Weight
Parents reported high levels of perceived control about their children’s weight. When asked, “How much control do parents have over how much their child weighs?” parents answered as follows: a lot: 52%; a little: 37%; none: 5%; don’t know: 7%. There were no differences between parents of overweight versus nonoverweight children.
Parental Ratings of Their Children’s Weight Status
The majority of parents of overweight children did not believe that their child was overweight (Table 2). Among parents of overweight children, 3% considered them to be “much too overweight” and 29% believed them to be “a little overweight” whereas 65% considered them “about the right weight.” Very few parents reported their overweight children to be “a little underweight” (1%) or “much too underweight” (1%). When asked to choose which line drawings most closely resembled their child, parents of overweight children most frequently chose Child E, followed by Child D. Parents of nonoverweight children most frequently rated their children as Child D, followed by Child C.
Table 2.
Parents’ Ratings of Their Child’s Weight Status, by Child’s Overweight Status
| Parents of overweight (n=72) n, (%age) |
Parents of nonoverweight (n=280) (%age) |
|
|---|---|---|
| Much too underweight | 1, (1) | 3, (1) |
| A little underweight | 1, (1) | 49, (18) |
| About the right weight | 47, (65) | 221, (79) |
| A little overweight | 21, (29) | 7, (3) |
| Much too overweight | 2, (3) | 0, (0) |
Health Attitudes and Beliefs About Childhood Obesity
When shown line drawings of children and asked to rate “which child do you most wish your child looked like” (ideal body image), parents of overweight children did not differ from parents of nonoverweight children in their answers, as both groups chose Child D in greater than 50% of cases. When asked which boy and girl looked the “least healthy,” parents of overweight and nonoverweight children did not differ in their answers and overwhelmingly chose Child H, the most overweight child. As mentioned above, the drawings were chosen to force a choice between a relatively thin but normal-weight child and an overweight child.
Parents of both overweight and nonoverweight children believed that the process of obesity starts very early in childhood. When asked “What age do you think that obesity starts in babies or children?” parents overall reported a median age of just 1.5 years.
Parental Knowledge, Attitudes, and Beliefs About Fast Food Consumption
Parents were also asked about their health beliefs and reasons for taking their children to “American-style fast food restaurants, such as McDonald’s, Burger King, and Taco-Bell.” Interviewers listed several possible reasons that parents may give for taking their children to eat at fast food restaurants and asked parents to rate each reason as “not at all important,” “somewhat important,” or “very important” to their family. Parents were also asked to name any other important reasons not listed. The 5 most frequently endorsed responses are listed in Table 3.
Table 3.
Parents’ Stated Reasons for Fast Food Consumption, by Child’s Overweight Statusa
| Parents of overweight (n=73) |
Parents of nonoverweight (n=280) |
|
|---|---|---|
| Because fast food is | ||
| convenient | 15 | 19 |
| affordable | 28 | 35 |
| healthy | 15 | 16 |
|
For the playground equipment |
81 | 83 |
|
For the toy that comes with the meal |
62 | 50 |
Note.
Reported as percentage responding affirmatively; respondents could choose more than one answer.
Differences between overweight and nonoverweight children were nonsignificant (P>0.05) for every variable
The most commonly reported reason that parents gave for taking their child to fast food restaurants was “to play on the playground equipment” (83% of parents overall reported it was “somewhat” or “very important”). Another commonly reported reason was “for the toy that comes with the kid’s meal” (52%). Few parents thought that fast food was affordable (33%), convenient (18%), or healthy (15%). There were no differences between parents of overweight versus nonoverweight children (Table 3).
DISCUSSION
In this population of low-income primarily Mexican-origin immigrant families, parental health knowledge, attitudes, and beliefs did not generally differ between parents of overweight versus nonoverweight children. Parents had reasonably good health knowledge about the consequences of childhood obesity, believed that childhood obesity started very early in childhood, had appropriate perceptions of ideal body size for their children, and high levels of perceived control about their children’s weight status.
However, the parents in this study displayed a marked disconnect between their knowledge, attitudes, and beliefs about childhood obesity in general and those referring to their own children’s weight status. None of the measures used in this study were adequate predictors of parental knowledge, attitudes, and behaviors regarding their young children’s weight status. This suggests that health messages that explicitly target obesity prevention or treatment for overweight children are unlikely to change the behaviors of these parents. After all, they understood the health risks of childhood obesity. They just did not think that those risks applied to their own children. In the future it will be important to explore the underlying reasons for this apparent disconnect between parents’ knowledge, attitudes, and beliefs about child obesity in general versus those regarding their own children.
Another focus for research area in coming years could be the further development and validation of our (or another) instrument to encompass the complex interactions between knowledge, attitudes, beliefs, and the social-cognitive and environmental factors that ultimately result in unhealthy behavior and childhood overweight. Future studies of this subject would also be well served to measure actual parental height and weight rather than rely on self-report, particularly as so many parents refused to answer the question.
Finally, we were surprised to find that parents’ most frequently reported reason for taking their children to fast food restaurants was “to play on the playground equipment.” Although at least one study demonstrated a positive correlation between proximity to parks and increased energy expenditure for older children,38 another found no significant relationship between distance lived from a playground and risk of overweight among low-income preschoolers.39 We cannot exclude the possibility that the parents in our sample listed this reason to our interviewers due in part to a social desirability bias. However, the use of fast food playgrounds may truly reflect the lack of safe, accessible public recreational space, particularly during the harsh Chicago winters.
This research demonstrated a prevalence of overweight among preschool children that was far higher than national estimates, although limited conclusions about prevalence and generalizability can be drawn as it was a clinic-based convenience sample. Furthermore, because we had no information about whether each child’s clinic visit that day was related to his or her weight status, we cannot exclude a selection bias. On the other hand, we had a relatively large sample size and a high study participation rate.
What This Study Adds
Relatively little was previously known about Mexican American parents’ health beliefs about childhood obesity. This study showed that in a Mexican immigrant population with little formal education, parents had relatively good knowledge and appropriate beliefs about ideal body size for young children in general, but they underestimated their own children’s weight status. These findings suggest that obesity prevention programs that focus primarily on health education are unlikely to be successful, as knowledge alone, although important to motivating change, may not be sufficient to modify parental behavior if it is not correctly identified as relevant to the child’s own health status. Rather, this study adds to the growing body of literature implying that the battle against childhood obesity is likely to be won only by primary prevention, including the creation of community-wide environments for healthier diets and increased opportunities for physical activity for all children, not just those at risk or already overweight.40
Acknowledgments
The authors thank the staff and community of Alivio Medical Center for collaborating in this project, particularly all the families who participated in the study. This research was funded by grants from the Robert Wood Johnson Clinical Scholars Program and the Section of General Pediatrics at the University of Chicago. This manuscript was presented as an oral presentation at the Robert Wood Johnson Clinical Scholars National Meeting, Tucson, Arizona, November 4, 2003, and as a poster at the Pediatric Academic Societies Annual Meeting, San Francisco, California, May 4, 2004.
REFERENCES
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008 May 28;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Alexander MA, Sherman JB, Clark L. Obesity in Mexican-American preschool children—a population group at risk. Public Health Nurs. 1991 Mar;8(1):53–58. doi: 10.1111/j.1525-1446.1991.tb00743.x. [DOI] [PubMed] [Google Scholar]
- 3.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001 Dec 12;286(22):2845–2848. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 4.Trevino RP, Marshall RM, Jr, Hale DE, et al. Diabetes risk factors in low-income Mexican-American children. Diabetes Care. 1999 Feb;22(2):202–207. doi: 10.2337/diacare.22.2.202. [DOI] [PubMed] [Google Scholar]
- 5.Foreyt JP, Cousins JH. Primary prevention of obesity in Mexican-American children. Ann N Y Acad Sci. 1993 Oct 29;699:137–146. doi: 10.1111/j.1749-6632.1993.tb18845.x. [DOI] [PubMed] [Google Scholar]
- 6.Encuesta Nacional de Nutricion. Encuesta Nacional de Nutricion 1999. Cuernavaca, Morelos: Instituto Nacional de Salud Publica; 2000. [Google Scholar]
- 7.Brewis A. Biocultural aspects of obesity in young Mexican schoolchildren. Am J Human Biol. 2003 May–Jun;15(3):446–460. doi: 10.1002/ajhb.10161. [DOI] [PubMed] [Google Scholar]
- 8.Eckstein KC, Mikhail LM, Ariza AJ, et al. Parents’ perceptions of their child’s weight and health. Pediatrics. 2006 Mar;117(3):681–690. doi: 10.1542/peds.2005-0910. [DOI] [PubMed] [Google Scholar]
- 9.Gardner DS, Hosking J, Metcalf BS, et al. Contribution of early weight gain to childhood overweight and metabolic health: a longitudinal study (EarlyBird 36) Pediatrics. 2009 Jan;123(1):e67–e73. doi: 10.1542/peds.2008-1292. [DOI] [PubMed] [Google Scholar]
- 10.Janssen I, Katzmarzyk PT, Srinivasan SR, et al. Utility of childhood BMI in the prediction of adulthood disease: comparison of national and international references. Obes Res. 2005 Jun;13(6):1106–1115. doi: 10.1038/oby.2005.129. [DOI] [PubMed] [Google Scholar]
- 11.Freedman DS, Khan LK, Serdula MK, et al. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005 Jan;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 12.Olvera N, Sharma S, Suminski R, et al. BMI tracking in Mexican American children in relation to maternal BMI. Ethn Dis. 2007 Autumn;17(4):707–713. [PubMed] [Google Scholar]
- 13.Wang YBM, Liand L, Caballero B, Kumanyika SK. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity. 2008 Oct;16(10):2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- 14.Davison KK, Birch LL. Weight status, parent reaction, and self-concept in five-year-old girls. Pediatrics. 2001 Jan;107(1):46–53. doi: 10.1542/peds.107.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore LL, Lombardi DA, White MJ, et al. Influence of parents’ physical activity levels on activity levels of young children. J Pediatr. 1991 Feb;118(2):215–219. doi: 10.1016/s0022-3476(05)80485-8. [DOI] [PubMed] [Google Scholar]
- 16.Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics. 2003 May;111(5 Part 2):1226–1231. [PubMed] [Google Scholar]
- 17.Baughcum AE, Chamberlin LA, Deeks CM, et al. Maternal perceptions of overweight pre-school children. Pediatrics. 2000 Dec;106(6):1380–1386. doi: 10.1542/peds.106.6.1380. [DOI] [PubMed] [Google Scholar]
- 18.Baughcum AE, Powers SW, Johnson SB, et al. Maternal feeding practices and beliefs and their relationships to overweight in early childhood. J Dev Behav Pediatr. 2001 Dec;22(6):391–408. doi: 10.1097/00004703-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Jain A, Sherman SN, Chamberlin DL, et al. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001 May;107(5):1138–1146. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 20.Young-Hyman D, Herman LJ, Scott DL, Schlundt DG. Care giver perception of children’s obesity-related health risk: a study of African American families. Obes Res. 2000 May;8(3):241–248. doi: 10.1038/oby.2000.28. [DOI] [PubMed] [Google Scholar]
- 21.Myers S, Vargas Z. Parental perceptions of the preschool obese child. Pediatr Nurs. 2000 Jan–Feb;26(1):23–30. [PubMed] [Google Scholar]
- 22.Sherry B, McDivitt J, Birch LL, et al. Attitudes, practices, and concerns about child feeding and child weight status among socio-economically diverse white, Hispanic, and African-American mothers. J Am Diet Assoc. 2004 Feb;104(2):215–221. doi: 10.1016/j.jada.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 23.Contento IR, Basch C, Zybert P. Body image, weight, and food choices of Latina women and their young children. J Nutr Educ Behav. 2003 Sep–Oct;35(5):236–248. doi: 10.1016/s1499-4046(06)60054-7. [DOI] [PubMed] [Google Scholar]
- 24.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA. 2002 Jul 3;288(1):82–90. doi: 10.1001/jama.288.1.82. [DOI] [PubMed] [Google Scholar]
- 25.Portes A, Rumbaut RG. Immigrant America. 3rd ed. Berkeley and Los Angeles: University of California Press; 2006. [Google Scholar]
- 26.Story M, Kaphingst KM, French S. The role of schools in obesity prevention. Future Child. 2006 Spring;16(1):109–142. doi: 10.1353/foc.2006.0007. [DOI] [PubMed] [Google Scholar]
- 27.Burnet DL, Plaut AJ, Ossowski K, et al. Community and family perspectives on addressing overweight in urban, African-American youth. J Gen Intern Med. 2008 Feb;23(2):175–179. doi: 10.1007/s11606-007-0469-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 29.Ajzen I, Madden T. Prediction of goal-directed behavior: Attitudes, intentions and perceived behavioral control. J Exp Soc Psychol. 1986;22:453–474. [Google Scholar]
- 30.Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;2:328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 31.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988 Winter;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 32.Stevens J, Story M, Becenti A, et al. Weight-related attitudes and behaviors in fourth grade American Indian children. Obes Res. 1999 Jan;7(1):34–42. doi: 10.1002/j.1550-8528.1999.tb00388.x. [DOI] [PubMed] [Google Scholar]
- 33.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood over-weight. Pediatr Clin North Am. 2001 Aug;48(4):893–907. doi: 10.1016/s0031-3955(05)70347-3. [DOI] [PubMed] [Google Scholar]
- 34.Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics. 2007 Spring;35(1):22–34. doi: 10.1111/j.1748-720X.2007.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dietz WH, Bellizzi MC. Introduction: the use of body mass index to assess obesity in children. Am J Clin Nutr. 1999 July;70(1 Part 2):123S–125S. doi: 10.1093/ajcn/70.1.123s. [DOI] [PubMed] [Google Scholar]
- 36.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000 Jun 8;(314):1–27. [PubMed] [Google Scholar]
- 37.Barlow SE, Dietz WH. Obesity Evaluation and Treatment: Expert Committee Recommendations. The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human Services. Pediatrics. 1998 Sep;102(3):E29. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 38.Cohen DA, Ashwood JS, Scott MM, et al. Public parks and physical activity among adolescent girls. Pediatrics. 2006 Nov;118(5):e1381–e1389. doi: 10.1542/peds.2006-1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med. 2004 Jan;38(1):57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 40.Koplan JP, Liverman CT, Kraak VI. Preventing childhood obesity: health in the balance: executive summary. J Am Diet Assoc. 2005 Jan;105(1):131–138. doi: 10.1016/j.jada.2004.11.023. [DOI] [PubMed] [Google Scholar]