Abstract
Background
Insomnia is the most commonly reported sleep disorder, characterized by trouble falling asleep, staying asleep, or waking up too early. Previous epidemiological data reveal that women are more likely than men to suffer from insomnia symptoms. We investigate the role that mental health history plays in explaining the gender disparity in insomnia symptoms.
Methods
Using logistic regression, we analyze National Health and Nutritional Examination Survey (NHANES) III interview and laboratory data, merged with data on sociodemographic characteristics of the residential census tract of respondents. Our sample includes 5,469 young adults (ages 20 to 39) from 1429 census tracts.
Results
Consistent with previous research, we find that women are more likely to report insomnia symptoms compared to men (16.7% vs. 9.2%). However, in contrast to previous work, we show that the difference between women’s and men’s odds of insomnia becomes statistically insignificant after adjusting for history of mental health conditions (OR=1.08, p>.05).
Conclusions
The gender disparity in insomnia symptoms may be driven by higher prevalence of affective disorders among women. This finding has implications for clinical treatment of both insomnia and depression, especially among women.
Keywords: Insomnia, Gender, Mental Health, Epidemiology, NHANES III
Introduction
National polls reveal that over half of the U.S. population reports having one or more symptom of insomnia (difficulty falling asleep, awake a lot during the night, woke too early and couldn’t get back to sleep, and woke up feeling unrefreshed) at least a few times a week (1, 2). Researchers estimate that chronic insomnia affects between 9 and 24 percent of the general population (3-7). Chronic sleep loss is linked to increased risk of developing chronic conditions such as hypertension, obesity, and cardiovascular disease (8-13). Further, sleep deprivation has been linked to cognitive impairment and depression, which have implications for job productivity and social functioning (14-20). Thus, the total economic, social, and public health burden of insomnia is large.
The burden of insomnia is disproportionately shouldered by women (6, 21-31). A meta-analysis of 31 studies with over 1.2 million participants indicates that women suffer from insomnia more than men by around 40% (OR=1.41 with a 95% confidence interval from 1.28-1.55) (32).
There are three common explanations for this gender difference in the prevalence of insomnia: physiological, sociological, and psychiatric illness (33).
Physiological explanations use animal models and point to hormonal variation to account for sex differences in terms of sleep initiation, maintenance, and quality (34-39). Progesterone, estrogen, and testosterone have all been implicated in explaining differences in men’s and women’s sleep patterns (40-44).
Sociological explanations focus on gender inequality in the balancing of competing obligations between work and family (45). For example, women typically have a greater share of the household responsibilities, especially related to time consuming activities such as child-rearing, food preparation, and cleaning, which may lead to increased trouble falling or staying asleep (46, 47). Despite multiple studies of the impact of gender differences in work and family obligations on health (47-49), researchers have rarely applied this perspective to explain differences in insomnia or insomnia symptoms (50). One study conducted in Taiwan found that the social role hypothesis only accounts for a small portion of the gender difference in insomnia (33).
Psychiatric explanations focus on the differences in prevalence of mental health disorders between men and women and that the gender disparity varies by type of disorder (51, 52). In particular, women are more likely to suffer from affective and neurotic disorders such as depression, whereas men are more likely to suffer from personality disorders (52). Because affective disorders are closely linked to insomnia (13, 15, 19, 20), differences in type and prevalence of psychiatric illness may be a likely candidate to explain the higher prevalence of insomnia symptoms among women. Yet, few studies have empirically explored this hypothesis (30, 31, 53). These studies show that adjusting for mental health conditions does not fully account for the gender discrepancy in insomnia, each in their own sample: Hong Kong Chinese adults (30), adults in Central Pennsylvania (31), and young adults in Uppsala, Sweden (53).
There are several limitations to the studies on the contribution of mental health to the higher prevalence of insomnia among women. First, these studies have relied largely on small, regional samples that lack generalizability. Second, they lack a wide range of sociodemographic, behavioral, and mental health history variables. Third, they do not consider both individual and neighborhood-level factors.
While we know of no prior study of neighborhood effects on insomnia symptoms per se, previous research has found evidence that links neighborhood type with sleep duration (54). We hypothesize that neighborhood characteristics such as noisiness, high population density, and household crowding may affect insomnia symptoms. These characteristics are typically more prevalent in socio-economically disadvantaged neighborhoods. Since women are more likely than men to live in disadvantaged neighborhoods (see Table 1), a neighborhood effect on insomnia symptoms may help explain the gender disparity in insomnia symptoms. Previous research has already shown that there are gender differences in neighborhood effects on health (55-57). Thus it is important to account for the contextual environment captured by neighborhood characteristics when examining gender differences.
Table 1.
Weighted Descriptive Statistics of Insomnia Symptoms and Selected Key Variables
| Percentage | Males | Females | |
|---|---|---|---|
|
Report ever having experienced 2 weeks or more of insomnia symptoms |
24.5 | 21.6 | 27.4 |
| Key Var 1: Mental Health History | |||
| Any mental health condition* | 12.9 | 9.2 | 16.7 |
| Key Var 2: NSES Quartiles | |||
| Q1 (NSES less than −0.47) | 25.1 | 47.5 | 52.5 |
| Q2 (NSES between −0.47 and 0.22) | 24.9 | 52.1 | 47.9 |
| Q3 (NSES between 0.22 and 0.67) | 25.2 | 52.8 | 47.2 |
| Q4 (NSES greater than 0.67) | 24.8 | 49.1 | 50.9 |
Ever having had major depressive episode, manic episode, single episode of major depression, recurrent major depression, dysthymic disorder, bipolar disorder, or atypical bipolar disorder
Our study seeks to better understand the role of mental health in contributing to the gender disparity in insomnia by 1) assessing insomnia prevalence in the U.S. using a large nationally-representative sample, 2) systematically exploring the relative contribution of sociodemographic factors, chronic conditions, and mental health history to the gender disparity in insomnia symptoms and 3) using a multi-level perspective by including both individual and neighborhood-level factors as possible contributing factors.
Methods
Data
A specially created geo-coded version of the National Health and Nutrition Examination Survey (NHANES) III, merged with information about neighborhood SES from the US Census, forms the basis for this study. The NHANES III includes interview data on a representative sample of US residents, collected between 1988 and 1994, with an over-sample of Blacks and Mexican Americans. Respondent addresses were geocoded to the census tract, using either address or street intersection. Fourteen-percent of the sample could not be geocoded to this level and are thus excluded. Our analyses included data on 5,469 adults aged 20 to 39, from 83 counties and 1,429 census tracts, who had completed surveys, and were not missing on any of the outcome or covariate measures. The focus on young adults helps to avoid confounding factors related to aging.
Data on neighborhood characteristics were derived from 1990 and 2000 Census data and linked to individual respondents in the NHANES III sample via 1990 census tract identifiers. Neighborhood attributes for years between censuses were estimated by linearly interpolating across decennial tract measures, assuming a constant rate of change in neighborhood conditions. Neighborhood characteristics were linked to individual responses according to the year in which the individual was surveyed.
Measures
Dependent Variable: Symptoms of Insomnia
We assessed insomnia symptoms using the following question from the NHANES III depression and mania module of the Diagnostic Interview Schedule: “Have you ever had a period of two weeks or more when you had trouble falling asleep, staying asleep, or with waking up too early?” We created a dichotomous indicator for insomnia symptoms, such that those who report having any of these symptoms are coded as 1 (24.5% prevalence) and those who do not are coded as 0.
Independent Variables
The social and demographic characteristics used as covariates include: gender; age; race/ethnicity, categorized as non-Hispanic White, non-Hispanic Black, Mexican-American, or other; educational attainment (grade school only, some high school, high school graduate, or post high school); nativity, categorized as US or foreign born; marital status (married or living as married, never married/not living as married, and other not living as married states [widowed, divorced, or separated]); the ratio of family income relative to the federal poverty line (FPL) (6 categories ranging from <1 to more than 5 times the FPL); number of people in the household; and employment status (employed, unemployed, and not in the labor force).
Physical health and health behaviors may confound the relationship between insomnia symptoms and mental health. Body mass index (58-60), smoking (61, 62), alcohol consumption (60, 63), self-rated health (64-66), and chronic conditions (60, 67, 68) are all correlated with both increased sleep disturbance and mental health conditions. Thus, we controlled for body mass index, smoking (current smoker vs. not), binge drinking (a binary variable indicating whether or not the individual had ever consumed 5 or more drinks in one day in the past year), self-rated health (excellent, very good, good, fair, poor), and number of chronic conditions (ranging from zero to three).
The first key independent covariate that we include as a possible mediator is lifetime diagnosis of any of a set of mental health diagnoses. We assessed mental health using a binary indicator of whether the respondent had ever had any of the following DSM-III diagnoses: major depressive episode, manic episode, single episode of major depression, recurrent major depression, dysthymic disorder, bipolar disorder, or atypical bipolar disorder (69).
Our second key variable of interest is neighborhood context. To investigate the relationship of neighborhood factors with insomnia and the extent to which neighborhood factors explain gender differences in insomnia symptoms, we constructed an index of neighborhood socioeconomic status (SES) at the level of census tracts using six variables obtained from the census. These variables were 1) percent of adults older than 25 with less than a high school education; 2) percent of male unemployment; 3) percent of households with income below the poverty line; 4) percent of households receiving public assistance; 5) percent of households with children that are headed only by a female; and 6) median household income. We transformed the variables so that higher values corresponded to higher SES (e.g., we calculated 100 minus the percent male unemployment to obtain the percent male employment). We then standardized each variable to a mean of zero and standard deviation of one. Finally, we added the six standardized variables and standardized the sum. The resulting index of neighborhood SES had a zero mean and standard deviation of one. Thus, an index value greater than zero denotes a tract with a SES-level above the sample average, whereas a score less than zero indicates the converse. For ease of interpretation, the index score was categorized into quartiles.
Analysis
We estimated a series of logistic generalized estimating equation (GEE) regression models to account for the clustering of observations within census tracts. The dependent variable was an indicator for the presence of insomnia symptoms for two or more weeks. Each successive model included all variables in the previous model as well as additional variables, specified below. In particular, we assessed the roles of individual-level social and demographic characteristics, neighborhood characteristics, health behaviors, and health status variables as confounding variables or as mediating factors.
The sequence of the models is based on an a priori causal ordering, in an attempt to understand which factors may explain gender differences in insomnia symptoms. In Model 1, we focus on the associations between gender and race/ethnicity adjusting only for age and age squared. In Model 2, we adjust for neighborhood SES. We include neighborhood context before other control variables because we view contextual influences as upstream determinants. Consequently, the potential relationship of neighborhood SES may be explained by more proximal compositional or mediating factors included in subsequent models. As such, in Model 3, we add adjustments for individual-level education, nativity, marital status, FPL, number of household members, and employment status. Models 4-6 include potential confounders and mediating variables that are hypothesized to explain the relationships observed in the earlier models. Model 4 adjusts for smoking status, body mass index, and binge drinking. Model 5 adjusts for self-rated health and chronic conditions, and Model 6 includes history of mental health conditions.
Analyses were performed at the secure Research Data Center at the National Center for Health Statistics in Hyattsville, Maryland, and were conducted using SAS Version 9.1. All analyses were weighted using the NHANES MEC weights and used empirical variance estimation to compute robust standard errors.
Results
Table 1 shows weighted descriptive statistics for the sample, including insomnia prevalence and demographic, social, and health characteristics. Almost a quarter of the sample reported having insomnia symptoms, and women had higher prevalence (27.4%) than men (21.6%). The distributions of the two key variables and how they vary by gender are also shown in Table 1.
Table 2 presents odds ratios for Models 1, 2, and 6, as previously described. As illustrated in Figure 1, in Model 1 (with age and race/ethnicity controls) women are 36% more likely to report insomnia symptoms than men. The size of the gender disparity does not change in Model 2 with the additional control for neighborhood SES. With the addition of other variables in the intervening models (results not shown), there is a slight reduction in the gender disparity, but it remains statistically significant. It disappears only in Model 6 when an indicator of mental health is added (OR=1.08, p>.05). Thus, having a history of a diagnosed mental health problem fully explains the remaining difference in insomnia between men and women. This can be explained primarily by the fact that women are more likely than men to ever have reported a mental health diagnoses (16.7% vs. 9.2%), as shown in Table 1. Note that in Model 6 the odds of having insomnia symptoms if the individual has ever reported having a mental health condition is 10.8 (p<.001). This finding strongly affirms the high co-morbidity of mental health conditions with insomnia symptoms.
Table 2.
Odds Ratios of Logistic Regressions Predicting Insomnia Symptoms (Models 3-5 not shown)
| Model 1 | 95% Confidence Interval |
Model 2 | 95% Confidence Interval |
Model 6 | 95% Confidence Interval |
||||
|---|---|---|---|---|---|---|---|---|---|
| Gender | |||||||||
| Female | 1.36** | [1.11- | 1.66] | 1.36** | [1.11- | 1.67] | 1.08 | [1.39- | 1.86] |
| Male | 1.00 | - | - | 1.00 | - | - | |||
| Key Var 1: Mental Health History | 10.81*** | [8.21- | 14.23] | ||||||
| Key Var 2: NSES | |||||||||
| Lowest Quartile | 1.23 | [0.90- | 1.70] | 0.91 | [0.61- | 1.37] | |||
| Q2 | 1.50* | [1.10- | 2.04] | 1.30 | [0.89- | 1.91] | |||
| Q3 | 1.21 | [0.88- | 1.68] | 1.15 | [0.80- | 1.68] | |||
| Highest Quartile | 1.00 | - | - | 1.00 | - | - | |||
| Age | 1.01 | [0.99- | 1.03] | 1.01 | [0.99- | 1.03] | 1.01 | [0.98- | 1.03] |
| Age Squared | 1.00 | - | 1.00] | 1.00 | [1.00- | 1.00] | 1.00 | [1.00- | 1.00] |
| Race | |||||||||
| White | 1.00 | - | - | 1.00 | - | - | 1.00 | - | - |
| Black | 0.81* | [0.68- | 0.98] | 0.79* | [0.64- | 0.98] | 0.76* | [0.59- | 0.97] |
| Mexican-American | 0.69*** | [0.57- | 0.83] | 0.67*** | [0.54- | 0.82] | 0.76 | [0.55- | 1.05] |
| Other | 0.66 | [0.41- | 1.06] | 0.63 | [0.40- | 1.01] | 0.73 | [1.22- | 0.31] |
| Educational Attainment | |||||||||
| Grade school | 0.51 | [0.27- | 0.96] | ||||||
| Some high school | 1.08 | [0.68- | 1.71] | ||||||
| High school | 0.92 | [0.64- | 1.31] | ||||||
| Some college | 1.02 | [0.71- | 1.47] | ||||||
| College and more | 1.00 | - | - | ||||||
| US born (1/0) | 1.08 | [0.72- | 1.61] | ||||||
| Marital Status | |||||||||
| Married or living as married | 1.00 | - | - | ||||||
| Single—never married | 1.17 | [0.86- | 1.58] | ||||||
| Other— (widowed, div. or sep.) | 1.48* | [1.05- | 2.09] | ||||||
| Income/Poverty Ratio | |||||||||
| Less than 1 | 1.11 | [0.64- | 1.90] | ||||||
| Between 1 and 2 | 0.89 | [0.53- | 1.50] | ||||||
| Between 2 and 3 | 0.91 | [0.57- | 1.45] | ||||||
| Between 3 and 4 | 0.80 | [0.49- | 1.29] | ||||||
| Between 4 and 5 | 0.80 | [0.46- | 1.39] | ||||||
| Greater than 5 | 1.00 | - | - | ||||||
| No. of Household Members | 0.96 | [0.89- | 1.04] | ||||||
| Employment Status | |||||||||
| Employed | 1.19 | [0.79- | 1.81] | ||||||
| Unemployed | 1.00 | [1.00- | 1.00] | ||||||
| Not in Labor Force | 1.23 | [0.76- | 1.97] | ||||||
| BMI | 1.01 | [0.99- | 1.03] | ||||||
| Current smoker (1/0) | 1.17 | [0.90- | 1.51] | ||||||
| Binge Drinking (1/0) | 1.00 | [1.00- | 1.00] | ||||||
| Self-Rated Health | |||||||||
| Excellent | 1.00 | - | - | ||||||
| Very good | 1.63 | [0.54- | 4.89] | ||||||
| Good | 1.10 | [0.37- | 3.25] | ||||||
| Fair | 0.87 | [0.29- | 2.60] | ||||||
| Poor | 0.84 | [0.28- | 2.55] | ||||||
| No. of Chronic Conditions | 1.18 | [0.91- | 1.53] | ||||||
p<.05
p<.01
p<.001
Model 1: Demographic variables
Model 2: Demographic and Neighborhood SES variables
Model 6: Demographic, Neighborhood SES, Social (education levels, US born, marital status, family income/poverty line ratio, employment status and number of people in the household), Health Behavior (smoking, binge drinking, and
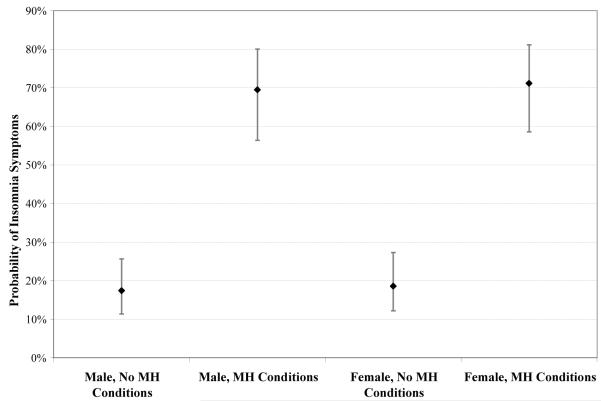
Figure 1.
Predicted Probabilities of Reporting Insomnia Symptoms of Four Idealized Persons (based on Model 6)
Predicted probabilities for above individuals assume the following characteristics: age=30 (sample mean), white, US-born, some college, PIR between 3 and 4, employed, married, avg. household size=3.5 (sample mean), non-smoker, binge drinking episodes=21 (sample mean), BMI=25.6 (sample mean), SRH=good, number of chronic conditions=0.21 (sample mean).
An additional interest of this analysis is the association of neighborhood SES with insomnia. We find in Model 2 that quartile 2 is the only one that has significantly higher reporting of insomnia symptoms relative to quartile 4 (with the highest SES) (1.50, p<.05). This association is explained by individual-level sociodemographic and health characteristics (Models 3-6); it is no longer statistically significant in Model 6 (1.30, p>.05).
Figure 1 shows predicted probabilities of having insomnia symptoms from Model 6 for four idealized individuals: a man and a woman with and without a history of mental health problems. The four individuals shown in Figure 1 are all set to the sample means or most common categories (see figure for details). As shown, using the predicted probabilities, there are no statistically significant differences between men and women who have had a history of mental health disorders (69.5% [95%CI 56.4%-80.0%] vs. 71.1% [95%CI 58.5%-81.1%]) and men and women who have not had a history of mental health disorders (17.4% [95%CI 11.4%-25.6%] vs. 18.5% [95%CI 12.1%-27.3%]).
Discussion
Consistent with previous literature, we find that women are more likely to report insomnia symptoms than men. Only a few studies have previously investigated why this disparity exists (33, 53). We enhance this research by analyzing the role that various individual-level and neighborhood-level factors play in explaining the gender difference in insomnia. We find that neighborhood SES did not explain any of the gender difference. Individual-level sociodemographic factors, health behaviors and health status explain only a small portion of the disparity. Rather, we find that most of the gender disparity in insomnia can be explained by accounting for lifetime history of a mental health condition. While the identification of the co-morbidity between insomnia and mental health conditions is not new (6, 70-72), the finding about its relationship with gender differences sheds light on the possible causes and treatments of insomnia among women.
Identifying the direction of causality between co-morbid conditions of mental health and insomnia symptoms presents a difficult challenge. Our cross-sectional analysis could not explore whether mental health was truly explaining why women have more insomnia or that insomnia was causing women to have more mental health conditions. As such, we were unable to investigate the question of causality.
Future work using longitudinal data and experimental designs is needed to further disentangle the co-morbid relationships between insomnia and mental health. Longitudinal studies that have information on timing of both mental health condition and insomnia symptoms can help tease out the ordering of these conditions. If depression or mental health conditions precede or cause insomnia symptoms, the clinical implication may suggest that depression is the underlying cause of the insomnia. On the other hand, insomnia itself may create episodes of depression. For example, insomnia may increase risks of depression and suicidality (71, 73). Because sleep disturbances and sleep restriction are associated with altered stress responsivity (74), treating insomnia directly with evidence-based therapies (75, 76) may also lead to improvements in mental health outcomes. This research indicates a need to better understand the linkages between physical and mental health. Mental health diagnoses should also be considered as possible co-morbidities in patients, especially women, who report symptoms of insomnia.
A limitation of our study is that the NHANES III question about insomnia symptoms is a single question, rather than a list of individual symptoms. This does not allow a distinction between chronic insomnia and occasional, transient insomnia because it does not precisely measure duration or intensity of episodes. Nor is it possible to distinguish between those who suffer from a sleep disorder and those who suffer from insomnia as a symptom of a mental disorder, a concern others have raised regarding epidemiological studies of insomnia (77). In addition, the NHANES measure does not assess the timing of insomnia, and instead asks if the respondent has ever experienced these symptoms. This may bias the results because older respondents have had more years over which to have experienced insomnia symptoms. To address this issue we adjusted for age and limited the age range of our sample (ages 20-39).
Our analyses also have a number of strengths. We control for a host of socio-demographic, health, and neighborhood characteristics in a large nationally-representative sample. Consistent with prior studies, we find statistically significant gender differences in insomnia symptoms across the population. Then, we identify one of the primary reasons for this gender difference – women have more mental health conditions associated with increased insomnia. Awareness of the gendered nature of this co-morbidity between insomnia and prior mental health condition may help clinicians treat patients, especially women, who suffer from both insomnia and mental health conditions. In doing so, the clinicians may improve the sleep and wellbeing of the population, in addition to minimizing the gender disparity in the overall prevalence of insomnia symptoms.
Footnotes
Disclaimer: The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.NSF . Sleep in America Poll. 2005. [Google Scholar]
- 2.NSF . Sleep In America Poll. 2008. [Google Scholar]
- 3.Buscemi N, Vandermeer B, Friesen C, Bialy L, Tubman M, Ospina M, et al. Manifestations and management of chronic insomnia in adults. Evid Rep Technol Assess (Summ) 2005;(125):1–10. doi: 10.1037/e439752005-001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chesson AL, Jr., Anderson WM, Littner M, Davila D, Hartse K, Johnson S, et al. Practice parameters for the nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep. 1999;22(8):1128–33. doi: 10.1093/sleep/22.8.1128. [DOI] [PubMed] [Google Scholar]
- 5.Morin CM, LeBlanc M, Daley M, Gregoire JP, Merette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123–30. doi: 10.1016/j.sleep.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 6.NIH State-of-Science Conference Statement: National Institute of Health; 2005. [Google Scholar]
- 7.Ohayon MM, Partinen M. Insomnia and global sleep dissatisfaction in Finland. J Sleep Res. 2002;11(4):339–46. doi: 10.1046/j.1365-2869.2002.00317.x. [DOI] [PubMed] [Google Scholar]
- 8.Newman AB, Nieto FJ, Guidry U, Lind BK, Redline S, Pickering TG, et al. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol. 2001;154(1):50–9. doi: 10.1093/aje/154.1.50. [DOI] [PubMed] [Google Scholar]
- 9.Singh M, Drake CL, Roehrs T, Hudgel DW, Roth T. The association between obesity and short sleep duration: a population-based study. J Clin Sleep Med. 2005;1(4):357–63. [PubMed] [Google Scholar]
- 10.Perceived insufficient rest or sleep--four states, 2006. MMWR Morb Mortal Wkly Rep. 2008;57(8):200–3. [PubMed] [Google Scholar]
- 11.Colten HR, Altevogt BM, Institute of Medicine (U.S.) Committee on Sleep Medicine and Research . Sleep disorders and sleep deprivation: an unmet public health problem. Institute of Medicine: National Academies Press; Washington, D.C.: 2006. [PubMed] [Google Scholar]
- 12.Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med. 2005;6(1):23–7. doi: 10.1016/j.sleep.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 13.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30(2):213–8. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 14.Killgore WD, Kahn-Greene ET, Lipizzi EL, Newman RA, Kamimori GH, Balkin TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. 2008;9(5):517–26. doi: 10.1016/j.sleep.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Riemann D. Insomnia and comorbid psychiatric conditions. Sleep Medicine. 2007;8(Supplement 4):S15–S20. doi: 10.1016/S1389-9457(08)70004-2. [DOI] [PubMed] [Google Scholar]
- 16.Neckelmann D, Mykletun A, Dahl AA. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. 2007;30(7):873–80. doi: 10.1093/sleep/30.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kahn-Greene ET, Killgore DB, Kamimori GH, Balkin TJ, Killgore WD. The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Med. 2007;8(3):215–21. doi: 10.1016/j.sleep.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry. 2003;160(6):1147–56. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 19.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39(6):411–8. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 20.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–80. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hajak G. Epidemiology of severe insomnia and its consequences in Germany. Eur Arch Psychiatry Clin Neurosci. 2001;251(2):49–56. doi: 10.1007/s004060170052. [DOI] [PubMed] [Google Scholar]
- 22.Leger D. Public health and insomnia: economic impact. Sleep. 2000;23(Suppl 3):S69–76. [PubMed] [Google Scholar]
- 23.Philip P, Leger D, Taillard J, Quera-Salva MA, Niedhammer I, Mosqueda JG, et al. Insomniac complaints interfere with quality of life but not with absenteeism: respective role of depressive and organic comorbidity. Sleep Med. 2006;7(7):585–91. doi: 10.1016/j.sleep.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Roth T. Introduction - Advances in our understanding of insomnia and its management. Sleep Med. 2007;8(Suppl 3):25–6. doi: 10.1016/j.sleep.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Walsh JK, Engelhardt CL. The direct economic costs of insomnia in the United States for 1995. Sleep. 1999;22(Suppl 2):S386–93. [PubMed] [Google Scholar]
- 26.Leger D, Massuel MA, Metlaine A. Professional correlates of insomnia. Sleep. 2006;29(2):171–8. [PubMed] [Google Scholar]
- 27.Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30(3):263–73. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- 28.Stoller MK. Economic effects of insomnia. Clin Ther. 1994;16(5):873–97. discussion 854. [PubMed] [Google Scholar]
- 29.Broman JE, Lundh LG, Hetta J. Insufficient sleep in the general population. Neurophysiol Clin. 1996;26(1):30–9. doi: 10.1016/0987-7053(96)81532-2. [DOI] [PubMed] [Google Scholar]
- 30.Li RH, Wing YK, Ho SC, Fong SY. Gender differences in insomnia--a study in the Hong Kong Chinese population. J Psychosom Res. 2002;53(1):601–9. doi: 10.1016/s0022-3999(02)00437-3. [DOI] [PubMed] [Google Scholar]
- 31.Bixler EO, Vgontzas AN, Lin HM, Vela-Bueno A, Kales A. Insomnia in central Pennsylvania. J Psychosom Res. 2002;53(1):589–92. doi: 10.1016/s0022-3999(02)00450-6. [DOI] [PubMed] [Google Scholar]
- 32.Zhang B, Wing YK. Sex differences in insomnia: a meta-analysis. Sleep. 2006;29(1):85–93. doi: 10.1093/sleep/29.1.85. [DOI] [PubMed] [Google Scholar]
- 33.Chen YY, Kawachi I, Subramanian SV, Acevedo-Garcia D, Lee YJ. Can social factors explain sex differences in insomnia? Findings from a national survey in Taiwan. J Epidemiol Community Health. 2005;59(6):488–94. doi: 10.1136/jech.2004.020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Koehl M, Battle S, Meerlo P. Sex differences in sleep: the response to sleep deprivation and restraint stress in mice. Sleep. 2006;29(9):1224–31. doi: 10.1093/sleep/29.9.1224. [DOI] [PubMed] [Google Scholar]
- 35.Paul KN, Dugovic C, Turek FW, Laposky AD. Diurnal sex differences in the sleep-wake cycle of mice are dependent on gonadal function. Sleep. 2006;29(9):1211–23. doi: 10.1093/sleep/29.9.1211. [DOI] [PubMed] [Google Scholar]
- 36.Sinton CM, Valatx JL, Jouvet M. Increased sleep time in the offspring of caffeine-treated dams from two inbred strains of mice. Neurosci Lett. 1981;24(2):169–74. doi: 10.1016/0304-3940(81)90243-3. [DOI] [PubMed] [Google Scholar]
- 37.Fang J, Fishbein W. Sex differences in paradoxical sleep: influences of estrus cycle and ovariectomy. Brain Res. 1996;734(12):275–85. [PubMed] [Google Scholar]
- 38.Manber R, Armitage R. Sex, steroids, and sleep: a review. Sleep. 1999;22(5):540–55. [PubMed] [Google Scholar]
- 39.Bowersox SS, Floyd T, Dement WC. Electroencephalogram during sleep in the cat: age effects on slow-wave activity. Sleep. 1984;7(4):380–4. doi: 10.1093/sleep/7.4.380. [DOI] [PubMed] [Google Scholar]
- 40.Lund BC, Bever-Stille KA, Perry PJ. Testosterone and andropause: the feasibility of testosterone replacement therapy in elderly men. Pharmacotherapy. 1999;19(8):951–6. doi: 10.1592/phco.19.11.951.31574. [DOI] [PubMed] [Google Scholar]
- 41.Vitiello MV, Larsen LH, Moe KE. Age-related sleep change: Gender and estrogen effects on the subjective-objective sleep quality relationships of healthy, noncomplaining older men and women. J Psychosom Res. 2004;56(5):503–10. doi: 10.1016/S0022-3999(04)00023-6. [DOI] [PubMed] [Google Scholar]
- 42.Moline ML, Broch L, Zak R, Gross V. Sleep in women across the life cycle from adulthood through menopause. Sleep Med Rev. 2003;7(2):155–77. doi: 10.1053/smrv.2001.0228. [DOI] [PubMed] [Google Scholar]
- 43.Murphy PJ, Campbell SS. Sex hormones, sleep, and core body temperature in older postmenopausal women. Sleep. 2007;30(12):1788–94. doi: 10.1093/sleep/30.12.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saletu-Zyhlarz G, Anderer P, Gruber G, Mandl M, Gruber D, Metka M, et al. Insomnia related to postmenopausal syndrome and hormone replacement therapy: sleep laboratory studies on baseline differences between patients and controls and double-blind, placebo-controlled investigations on the effects of a novel estrogen-progestogen combination (Climodien, Lafamme) versus estrogen alone. J Sleep Res. 2003;12(3):239–54. doi: 10.1046/j.1365-2869.2003.00356.x. [DOI] [PubMed] [Google Scholar]
- 45.Bird CE, Fremont AM. Gender, time use, and health. J Health Soc Behav. 1991;32(2):114–29. [PubMed] [Google Scholar]
- 46.Bianchi SM, Robinson JP, Milkie MA. Changing rhythms of American family life. Russell Sage Foundation; New York: 2006. [Google Scholar]
- 47.Bird CE, Rieker PP. Gender and health: the effects of constrained choices and social policies. Cambridge University Press; Cambridge; New York: 2008. [Google Scholar]
- 48.Gove WR, Tudor JF. Adult Sex Roles and Mental Illness. American Journal of Sociology. 1973;78(4):812–835. doi: 10.1086/225404. [DOI] [PubMed] [Google Scholar]
- 49.Bird CE, Rieker PP. Gender matters: an integrated model for understanding men’s and women’s health. Social Science & Medicine. 1999;48(6):745–755. doi: 10.1016/s0277-9536(98)00402-x. [DOI] [PubMed] [Google Scholar]
- 50.Williams SJ. Sleep and society: sociological ventures into the (un)known. Routledge; London; New York: 2005. [Google Scholar]
- 51.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 52.Dohrenwend BP. Mental illness in the United States: epidemiological estimates. Praeger Publishers; New York: 1980. [Google Scholar]
- 53.Lindberg E, Janson C, Gislason T, Bjornsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: can gender differences be explained by differences in psychological status? Sleep. 1997;20(6):381–7. doi: 10.1093/sleep/20.6.381. [DOI] [PubMed] [Google Scholar]
- 54.Hale L, Do DP. Racial Differences in Self-Report of Sleep Duration in a Population-Based Study. Sleep. 2007;30(9):1092–99. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stafford M, Cummins S, Macintyre S, Ellaway A, Marmot M. Gender differences in the associations between health and neighbourhood environment. Soc Sci Med. 2005;60(8):1681–92. doi: 10.1016/j.socscimed.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 56.Molinari C, Ahern M, Hendryx M. The relationship of community quality to the health of women and men. Soc Sci Med. 1998;47(8):1113–20. doi: 10.1016/s0277-9536(98)00114-2. [DOI] [PubMed] [Google Scholar]
- 57.Kavanagh AM, Bentley R, Turrell G, Broom DH, Subramanian SV. Does gender modify associations between self rated health and the social and economic characteristics of local environments? J Epidemiol Community Health. 2006;60(6):490–5. doi: 10.1136/jech.2005.043562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158(12):1139–47. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 59.Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hillier TA, et al. The association between sleep duration and obesity in older adults. Int J Obes (Lond) 2008 doi: 10.1038/ijo.2008.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Janson C, Lindberg E, Gislason T, Elmasry A, Boman G. Insomnia in men-a 10-year prospective population based study. Sleep. 2001;24(4):425–30. doi: 10.1093/sleep/24.4.425. [DOI] [PubMed] [Google Scholar]
- 61.Riedel BW, Durrence HH, Lichstein KL, Taylor DJ, Bush AJ. The relation between smoking and sleep: the influence of smoking level, health, and psychological variables. Behav Sleep Med. 2004;2(1):63–78. doi: 10.1207/s15402010bsm0201_6. [DOI] [PubMed] [Google Scholar]
- 62.Patten CA, Gillin JC, Golshan S, Wolter TD, Rapaport M, Kelsoe J. Relationship of mood disturbance to cigarette smoking status among 252 patients with a current mood disorder. J Clin Psychiatry. 2001;62(5):319–24. doi: 10.4088/jcp.v62n0502. [DOI] [PubMed] [Google Scholar]
- 63.Turnbull JE, Gomberg ES. Impact of depressive symptomatology on alcohol problems in women. Alcohol Clin Exp Res. 1988;12(3):374–81. doi: 10.1111/j.1530-0277.1988.tb00211.x. [DOI] [PubMed] [Google Scholar]
- 64.Fleishman JA, Zuvekas SH. Global self-rated mental health: associations with other mental health measures and with role functioning. Med Care. 2007;45(7):602–9. doi: 10.1097/MLR.0b013e31803bb4b0. [DOI] [PubMed] [Google Scholar]
- 65.Molarius A, Janson S. Self-rated health, chronic diseases, and symptoms among middle-aged and elderly men and women. J Clin Epidemiol. 2002;55(4):364–70. doi: 10.1016/s0895-4356(01)00491-7. [DOI] [PubMed] [Google Scholar]
- 66.Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: the role of sleep. Psychosom Med. 2002;64(2):337–44. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 67.Power JD, Perruccio AV, Badley EM. Pain as a mediator of sleep problems in arthritis and other chronic conditions. Arthritis Rheum. 2005;53(6):911–9. doi: 10.1002/art.21584. [DOI] [PubMed] [Google Scholar]
- 68.Mills TL. Comorbid depressive symptomatology: isolating the effects of chronic medical conditions on self-reported depressive symptoms among community-dwelling older adults. Soc Sci Med. 2001;53(5):569–78. doi: 10.1016/s0277-9536(00)00361-0. [DOI] [PubMed] [Google Scholar]
- 69.American Psychiatric Association . Work Group to Revise DSM-III. Diagnostic and statistical manual of mental disorders: DSM-III-R. 3rd ed. American Psychiatric Press; Washington, DC: 1987. American Psychiatric Association. [Google Scholar]
- 70.Riedel BW, Lichstein KL. Insomnia and daytime functioning. Sleep Med Rev. 2000;4(3):277–298. doi: 10.1053/smrv.1999.0074. [DOI] [PubMed] [Google Scholar]
- 71.Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ. Sleep complaints and depression in an aging cohort: A prospective perspective. Am J Psychiatry. 2000;157(1):81–8. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- 72.Weyerer S, Dilling H. Prevalence and treatment of insomnia in the community: results from the Upper Bavarian Field Study. Sleep. 1991;14(5):392–8. [PubMed] [Google Scholar]
- 73.Cukrowicz KC, Otamendi A, Pinto JV, Bernert RA, Krakow B, Joiner TE. The Impact of Insomnia and Sleep Disturbances on Depression and Suicidality. Dreaming. 2006;16(1):1–10. [Google Scholar]
- 74.Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Med Rev. 2008;12(3):197–210. doi: 10.1016/j.smrv.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 75.Perlis ML, Jungquist C, Smith MT, Posner D. Cognitive Behavioral Treatment of Insomnia: A Session-by-Session Guide. Springer; New York: 2005. [Google Scholar]
- 76.Lack L, Wright H, Kemp K, Gibbon S. The treatment of early-morning awakening insomnia with 2 evenings of bright light. Sleep. 2005;28(5):616–23. doi: 10.1093/sleep/28.5.616. [DOI] [PubMed] [Google Scholar]
- 77.Ohayon MM. Prevalence of DSM-IV diagnostic criteria of insomnia: distinguishing insomnia related to mental disorders from sleep disorders. J Psychiatr Res. 1997;31(3):333–46. doi: 10.1016/s0022-3956(97)00002-2. [DOI] [PubMed] [Google Scholar]