A descriptive study using a Web-based questionnaire was undertaken to understand the deployment of physician assistants in oncology, as we face a significant shortage of oncology providers by 2020.
Abstract
Purpose:
To understand the deployment of physician assistants (PAs) in oncology. A recent analysis of the oncology workforce in the United States commissioned by ASCO predicted a significant shortage of providers by 2020.
Methods:
A descriptive study was undertaken using a Web-based questionnaire survey. Invited participants, including all PAs listed in the national PA database (n = 855) and all PAs at The University of Texas M. D. Anderson Cancer Center (Houston, TX; n = 159), were mailed letters directing them to the Web-based survey.
Results:
The study produced a 30% response rate. A total of 186 PAs worked in medical oncology (the population of interest). Of the respondents, 80% were women, mean age was 36 years, average time employed as a PA was 9.5 years (6.5 years in oncology), 55% had obtained a master's degree, four had completed a postgraduate oncology program, 91% reported that direct mentorship by a supervising physician was very important in obtaining oncology-based knowledge, and 61% reported that becoming fully competent in the practice of oncology required 1 to 2 years. The majority of PAs (78.5%) worked 33 to 50 hours per week, and 56% of those reported working 41 to 50 hours per week. Three fourths (77%) wrote chemotherapy orders, most requiring physician co-signature, and 69% prescribed schedule III to V controlled substances. Additional data were gathered regarding clinical duties, research, and teaching.
Conclusion:
Oncology PAs are used in multiple medical settings, and many assume high-level responsibilities. Future research addressing function and factors that limit use of PAs may allow for improved organizational efficiency and enhancement in the delivery of health care.
Introduction
A recent analysis of the oncology workforce in the United States commissioned by ASCO predicted a significant shortage of providers by 2020.1 An increase in overall demand of 48% was believed to be driven by the aging population and increasing number of cancer survivors. One proposed option to ease this burden was increased use of nonphysician health care providers. In this workforce survey, oncologists using physician assistants (PAs) and nurse practitioners (NPs) reported higher weekly visit rates and improved efficiency, patient care, and professional satisfaction. Productivity was highest when PAs/NPs were used for advanced activities. The authors concluded that use of PAs/NPs would not suffice to meet the demand predicted for 2020, likely because of the lack of available PAs/NPs recruited to the field of oncology and sustained growth of the profession.
Of 75,000 PAs in the United States, only 2.4% practice in oncology, and little information has been reported about their roles.2 A small study (n = 54) conducted by Ross3 in 2005 regarding the role of PAs in oncology focused on a population at one site: The University of Texas M. D. Anderson Cancer Center (MDACC; Houston, TX). The study yielded information that began to shape the description of PAs working in oncology and provided a basis for a new survey instrument to be developed. However, more information was needed regarding education, training, clinical duties, prescribing authority, research, and educational interests, and a more detailed look at how PAs function in an advanced role was necessary.1 The current study was developed to assess a larger sample, answer more questions, and truly understand the role of PAs in oncology.
Methods
A descriptive study was conducted using a Web-based survey from November 7, 2007, to December 14, 2007. Invited participants included all PAs in the American Academy of Physician Assistants (AAPA) national database (n = 855) who listed practice in medical oncology, hematology/oncology, radiation oncology, surgical oncology, pediatric medical oncology, or pediatric hematology/oncology and all PAs at MDACC (n = 159). A letter or e-mail was sent to the identified PAs explaining the study objectives and directing them to the online survey. A follow-up postcard or e-mail was sent to encourage participation. MDACC PAs who were also listed in the national database were identified and only sent one request to fill out the survey. The survey included a variety of questions (Data Supplement, online only). Ten letters were undeliverable, resulting in a total of 1,004 PAs contacted. The returned anonymous data were processed using SPSS, Version 16 (SPSS, Chicago, IL). The data were additionally stratified by subspecialty of oncology to yield information more specific to each group, allowing for comparisons among groups. Descriptive statistics were used to analyze the data, as was McNemar's test to interpret statistically significant results. No participant numbers, names, or other personal identifiers were included in the reportable data.
Results
Of the 1,004 PAs contacted, 301 responded, yielding a 30% response rate. Of those 301 PAs, 186 (61.8%) reported working in medical oncology (medical oncology, hematology/oncology, mixed medical/surgical oncology, or mixed medical/radiation oncology). Pediatric subspecialties were not included. In addition to the medical oncology subspecialty, the data collected from the 301 PA respondents were used to provide information on the role of radiation oncology PAs, oncology training of PAs and the educational duties they assume, and the ability of PAs to communicate with patients with cancer.4–6
Of the 186 medical oncology PAs, 80% were women. Average age was 36 years, with a range of 23 to 63 years, and 60% were younger than 40 years. PAs from Texas (n = 39), North Carolina (n = 17), and New York (n = 16) were most represented in the survey. The length of time practicing as a PA ranged from less than 1 year to 32 years of experience, with 65% (n = 186) practicing fewer than 10 years. PAs reported working 1 to 25 years in the field of oncology, with 63% (n = 185) working 5 years or fewer and a total of 76.8% working fewer than 10 years.
Education
As their initial PA credential, 55% of respondents (n = 185) received a master's degree. Four PAs had completed a postgraduate training oncology program. Some PAs had completed oncology clinical rotations (27% in hematology/oncology, 7% in surgical oncology, and 4% in pediatric oncology). In addition, PAs rotating through internal medicine, geriatrics, general surgery, pediatrics, and gynecology reported seeing patients currently undergoing cancer treatment (67.6%, 20%, 63.7%, 9.7%, and 44.8%, respectively). Although internal medicine and general surgery yielded the most encounters with patients with cancer, almost half of respondents (47.5%) reported not having completed a geriatrics rotation.
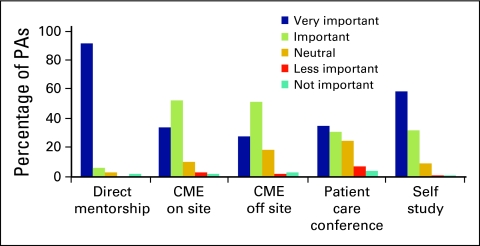
When PAs were asked how important certain factors were in obtaining their knowledge base in the field of oncology, 91.4% (n = 186) rated direct mentorship by physician very important, and 58.5% (n = 183) rated self study very important. Attending continuing medical education (CME) lectures inside and outside of places of employment and attending patient care conferences were also reported by most PAs to be important or very important (85.4% [n = 184], 78% [n = 182], and 65.4% [n = 185], respectively; Fig 1).
Figure 1.
Importance of factors in obtaining a knowledge base in oncology. PA, physician assistant; CME, continuing medical education.
For 86% of PAs (n = 154), becoming “fully competent in the practice of oncology within a setting and discipline” took 6 months to 2 years, with the majority (61%) of these PAs reporting 1 to 2 years. An additional 31 PAs indicated they had not yet met the level of full competence. Of these 31 PAs, 58% had worked in oncology for 1 year or less. Only 37.3% of PAs reported receiving formal training in communication skills.
Current Position
Of 186 PAs, 120 reported working in hematology/oncology, 59 in medical oncology, and seven in medical/surgical oncology combination practice. The number of supervising physicians ranged from one to 30, with 62.8% of PAs (n = 180) working with three or fewer. Forty-eight percent (n = 185) worked in an academic setting (cancer center or university), whereas 42% (n = 185) worked in community practice (single or multispecialty groups or sole physician practice). Other settings included hospice, Veterans Affairs facilities, and community hospitals. PAs working in an academic setting had more supervising physicians on average than those working in community practice (mean, 5.33; range, one to 30 v mean, 3.18; range, one to nine).
The majority of PAs (78.5%; n = 182) worked 33 to 50 hours per week, and of those PAs, 56% reported working 41 to 50 hours per week. Only 22% of PAs (n = 186) took call. Total work time focused on direct patient care, with 91.2% of PAs (n = 181) reporting spending 50% to 100% of their time providing direct patient care. In addition, 54% (n = 179) reported that 10% to 20% of their time was devoted to indirect patient care, defined as returning telephone calls/e-mails from patients and reviewing medical records; 87% (n = 137) reported that 10% or less of their time was spent performing administrative duties; and 76% (n = 137) and 81% (n = 134) reported spending 5% or less of their time on education and research, respectively.
Clinical Duties
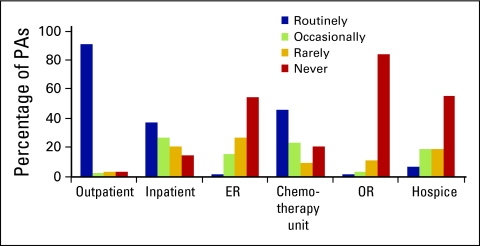
PAs provided direct patient care in a variety of clinical settings, with virtually all PAs seeing patients in the outpatient setting (91.2%; n = 182). In addition, many PAs routinely or occasionally saw patients in the inpatient, emergency center, chemotherapy unit, operating room, and hospice settings (64.3% [n = 182], 17% [n = 177], 69.6% [n = 181], 4.5% [n = 178], and 25.2% [n = 178], respectively; Fig 2).
Figure 2.
Percentage of physician assistants (PAs) providing direct patient care. ER, emergency room; OR, operating room.
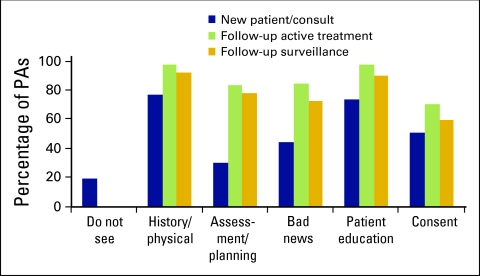
PAs were asked to indicate any function (history and physical, assessment and planning, breaking bad news, patient education, and obtaining patient consent) they performed and assumed primary responsibility for when seeing new patients/consults, follow-up patients receiving active treatment, and follow-up patients undergoing clinical surveillance. All PAs (n = 179) reported seeing follow-up patients, but 20% reported not seeing new patients/consults (P < .0001). When evaluating follow-up patients receiving active treatment or undergoing clinical surveillance, most PAs performed all five functions, respectively: history and physical (97.8% and 92.8%), assessment and planning (83.9% and 78.9%), breaking bad news (85% and 72.8%), patient education (97.8% and 90.6%), and obtaining patient consent (71.1% and 60.6%). However, when evaluating new patients/consults, PAs still performed history and physical (77.1%), patient education (74.3%), and obtaining patient consent (51.4%) functions routinely, but they performed assessment and planning (30.7%) and breaking bad news (44.7%) functions less frequently than during follow-up patient visits (Fig 3). A statistically significant difference (P < .0001) was appreciated between the new patient/consult and follow-up patient visits for each specific function performed. Some PAs independently performed bone marrow aspiration/biopsy (54.8%), paracentesis (14%), central line placement (1.6%), and intrathecal chemotherapy administration (33.3%). No PAs reported administering intravenous chemotherapy.
Figure 3.
Services performed by physician assistants (PAs).
Prescribing Authority
Seventy-seven percent of PAs (n = 182) wrote chemotherapy orders. Of these 140 PAs, 77.9% reported requirement of physician signature/co-signature before order submission. Half of PAs (n = 182) reported that their state allowed PAs to order chemotherapy, whereas 26.9% said their state did not; the remaining 22.5% did not know. Of the 92 PAs reporting state authorization for PAs to order chemotherapy, 13 (14.1%) indicated that their employer did not allow this, despite state policy, and five PAs did not know what their employer allowed. One third (35%; n = 180) reported that 26% to 50% of their patients were receiving narcotics, and an additional 33% reported that more than 51% of their patients were receiving narcotics. Ninety-one percent of PAs (n = 140) had prescriptive delegation by their state for controlled substances, schedule III to V, whereas only 39.8% (n = 108) had delegation for schedule II. Only 5% of those with prescriptive authority for schedule III to V did not have that privilege activated, compared with 25% for schedule II.
Research and Education
Medical oncology PAs were active in research and educational activities as well. Eighty-four percent identified and monitored patients participating in clinical trials, and 29.8% (n = 181) served as principal or co-investigators. An additional 22.5% (n = 178) participated in other research activities, such as retrospective medical record reviews, protocol writing, data collection, and original research. Almost half of PAs (44.8%) precepted PA students, 19.3% provided CME, and 33.1% provided cancer-related community education (n = 181). Moreover, some PAs held faculty positions inside and outside of their institution of employment (7.2% and 8.3%, respectively).
Discussion
Role of the Oncology PA
The results of this study prove that medical oncology PAs are performing advanced activities, defined by Erikson et al1 as “assisting with NP/CO [new patients/consults], ordering routine chemotherapy, and performing invasive procedures.” Therefore, this should result in improved efficiency and patient care as well as professional satisfaction for physicians.
In addition to these advanced activities, PAs assumed other responsibilities. For example, 74% reported working more hours per week (41 to > 50 hours) than the national average in all education and health services (33.3 hours) reported by the Bureau of Labor Statistics for 2007.7 PAs worked in multiple clinical settings and routinely used independent judgment when evaluating both new patients/consults and follow-up patients. Many PAs also helped to manage and prescribe narcotics for a large patient population requiring pain management.
Furthermore, PAs played an important role in educating and communicating with patients and their families. Direct patient care accounted for most of PAs' time, but time was also allocated for reviewing medical records and returning telephone calls/e-mails to patients, families, and collaborating physicians. Use of PAs may possibly result in a higher level of patient and family contentment, but PAs may also provide additional time for physicians to engage in other projects, resulting in professional satisfaction, as reported by Erikson et al.1 Although most PAs reported that only a small portion of their time was devoted to research and education, many still found time to precept PA students, hold faculty positions, and provide CME and community education.
Exposing PAs to Oncology
With only 2.4% of PAs practicing in oncology, there is work to be done regarding exposing and recruiting PAs to the field.2 According to the data collected, internal medicine and general surgery rotations most commonly exposed PA students to patients undergoing cancer treatment. Completion of a geriatrics rotation may have seemed the obvious answer to exposing PA students to patients with cancer, but only 38% came into contact with such patients in this way. An even smaller number of PAs reported completing an oncology-based rotation. Overall, limited time is devoted to oncology in PA programs. In addition to informing PA students about a subspecialty of medicine that may be of interest to them, it is important that PAs receive a broad education in medicine.8 Because cancer is the number-two leading cause of death in the United States, it is safe to say that most clinically practicing PAs will diagnose cancer, provide medical care to patients undergoing cancer treatment, or discuss cancer prevention with a patient at some point in their careers.9 As the population ages, this may become even more common. Therefore, working with PA programs and encouraging a stronger emphasis in oncology in the curriculum is essential.
On-the-Job Training
With an average age of 36 years, 65% having worked fewer than 10 years, and 63% reporting practicing in oncology 5 years or fewer, many PAs may be entering the field of oncology directly after graduating from PA school. If there is little emphasis on oncology in PA programs, how are PAs trained in this specialty? What is the knowledge base required to begin a job in an oncology setting? Is it worth the time of an oncology practice to invest in a new PA graduate? Although a significant component of medical oncology is based on internal medicine training, additional specialty training and understanding are required to become competent in an oncology practice. Only four PAs reported completing the postgraduate oncology program at MDACC. How did the other PAs learn oncology? Ninety-one percent of PAs reported that direct mentorship by their supervising physician was very important, and more than half reported self study to be very important. Most PAs reported feeling fully competent after 6 months to 2 years. Despite the lack of formal oncology training for PAs, it seems taking on a PA may prove to be a greater advantage than burden for an oncology practice. However, physicians must understand that the most important factor in obtaining this knowledge base is direct mentorship, and therefore, their involvement is indispensable.
Study Limitations
Surveys are one of the most popular tools for collecting descriptive data. An excellent return rate for a mailed questionnaire is defined as 60% to 80%, with a realistic return rate ranging from 30% to 60%.10 Of 1,004 PAs, 301 PAs responded, resulting in a 30% response rate. The AAPA database archives all registered PAs indefinitely, and the specialty is updated only if the PA makes the necessary changes. Therefore, some PAs no longer working in oncology may have received the survey and elected not to participate. In addition, not all MDACC PAs work in an oncology-based specialty, such as cardiology. Therefore, they may have also elected not to participate. If any of these PAs elected not to participate and did not answer a key question—“Do you currently work in oncology?”—this may have resulted in an incorrect total number of PAs surveyed and therefore translated into a lower response rate.
Although surveys can provide anonymity and flexibility, they are vulnerable to misinterpretation of both questions and responses.10 For example, many questions asked for a specific number of events, such as “indicate the number of patients you see per week.” Multiple participants responded with ranges, and therefore, the median number was used when a range was given for any question. Another difficult question to interpret was that including the phrase “indicate any of the following.” This question should have given the respondent the option of answering yes, no, or not applicable. This would have allowed for a better interpretation of whether the answer was no, the response was missed, or the respondent skipped the question. A pilot study using this survey may have helped to eliminate any ambiguous questions.
Conclusion
Working as a PA was ranked one of the best careers of 2008 by US News & World Report.11 Employment of PAs is expected to grow 27% from 2006 to 2016, faster than the average rate for all occupations reported by the Bureau of Labor Statistics.12 This study helps to confirm that PAs are performing advanced activities and can be a positive asset to their health care team when used in the correct way. To help ease the burden of increased demand for oncology health care providers, we need to do a better job of exposing and recruiting PAs to the specialty.
This study was successful in determining many group descriptors of PAs in oncology and in contributing to an understanding of many of the roles medical oncology PAs play. Conducting more focused research should be the first step in enhancing our knowledge about the subject. A more extensive look is needed at how many patients are seen in clinic, how much time is spent per patient, what the primary diagnoses of patients are, and which patient needs arise during each visit. In addition, a comparison between the workload and responsibilities of oncology PAs and those of physicians would be useful. The interest in and knowledge about using PAs in the field of oncology are continuing to grow. Gaining greater understanding of PAs' current role and addressing factors that limit their use may help PAs play a key role in ensuring that quality medical care is available for patients with cancer for future decades.
Supplementary Material
Acknowledgment
The study survey was created to ask physician assistants (PAs) practicing in oncology a variety of questions. The data obtained were vast and could be categorized into separate projects. This is the only report we have written/submitted on the role of PAs in oncology in the subset of medical oncology. We stratified the data for this study to include only those PAs practicing in medical oncology or hematology/oncology, excluding those in pediatric oncology, surgical oncology, and radiation oncology. This study also did not focus on a single aspect, such as clinical duties or role in education; it encompasses all arenas in which medical oncology PAs play a role.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
References
- 1.Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: Challenges to assuring access to oncology services. J Oncol Pract. 2007;3:79–86. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Physician Assistants. 2008 AAPA Physician Assistant Census Report. www.aapa.org/about-pas/data-and-statistics/389–2008-data.
- 3.Ross AC. The role of PAs in oncology. Adv Phys Assist. 2008;16:46–49. [Google Scholar]
- 4.Parker P, Baile W, Ross A, et al. Communicating with cancer patients: What physician assistants report as their most challenging encounters. Presented at the 10th World Congress of Psycho-Oncology; June 9-13, 2008; Madrid, Spain. [Google Scholar]
- 5.Polansky M, Ross AC, Gould MS, et al. The role of physician assistants in radiation oncology. Int J Radiat Oncol Biol Phys. 2008;72(suppl):1. abstr S485. [Google Scholar]
- 6.Polansky M, Ross AC, Parker PA. Oncology training of physician assistants and the educational roles they assume. Presented at the 2008 Physician Assistant Education Association Annual Education Forum; October 29-November 2, 2008; Savannah, GA. [Google Scholar]
- 7.Bureau of Labor Statistics. Current employment statistics—Hours and earnings series. http://www.bls.gov/ces/cesaepp.htm.
- 8.American Academy of Physician Assistants. Education and certification. http://www.aapa.org/education-and-certification/physician-assistant-programs.
- 9.Centers for Disease Control and Prevention. National Center for Health Statistics: Leading causes of death. http://www.cdc.gov/nchs/FASTATS/lcod.htm.
- 10.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. ed 2. Upper Saddle River, NJ: Prentice Hall Health; 2000. [Google Scholar]
- 11.US News & World Report. Best careers 2008. http://www.usnews.com/features/business/best-careers/best-careers-2008.html.
- 12.Bureau of Labor Statistics. Occupational Outlook Handbook, 2008-09 Edition. http://www.bls.gov/oco/ocos081.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.