A survey in response to Washington oncology practices' workforce shortage on employment patterns for advanced nurse practitioners and physician assistants found that practices have embraced these roles.
Abstract
Purpose:
In response to the looming oncology manpower shortage, the Washington State Medical Oncology Society (Vancouver, WA) surveyed medical oncology practices in Washington regarding employment patterns for advanced nurse practitioners (ANPs) and physician assistants (PAs) in oncology.
Methods:
Funded by a 2008 ASCO State Affiliate Grant and using Surveymonkey.com as a platform, practices were queried regarding practice demographics, employment patterns, and functions of ANPs and PAs.
Results:
Of the total queried, 25 practices (50%) responded, representing the spectrum of single-specialty (n = 8), multispecialty (n = 7), hospital-based (n = 6), and academic practices (n = 4). Sixty-eight percent of practices employed ANPs and/or PAs. Compared with PAs, ANPs were more likely to work independent of supervision (64% v 0%), perform follow-up in the outpatient setting (93% v 77%), evaluate patients in infusion centers (71% v 62%), and provide genetic counseling (42% v 0%). PAs were more likely to see hospitalized patients (62% v 42%) and supervise infusion centers (15% v 7%). New patient consultations were performed with similar frequency (PAs, 29% and ANPs, 31%). ANPs were more likely to review research eligibility (25% v 15%), obtain informed consent (33% v 15%), and monitor compliance (13% v 8%).
Conclusion:
Washington practices have embraced advanced practitioners. Given the diversity of practice patterns, practices can learn from one another how to maximize ANP/NP roles. Practices need to promote practice-based educational opportunities to attract ANPs/PAs to medical oncology.
Introduction
The ASCO Workforce Study of 2007 predicted a 48% increase in demand for medical oncology services by 2020.1,2 Efforts to expand fellowship positions for medical oncology have begun but are constrained by funding issues and will likely yield only a 14% increase over the next 10 years.3 This suggests that adoption of other models of care will be necessary. One option is the increased employment of advanced nurse practitioners (ANPs) and physician assistants (PAs) in medical oncology practices.
PAs and ANPs have been trained in the United States since the 1960s.4,5 and were predominantly employed in primary care until the 1990s. There are approximately 71,000 PAs currently practicing in the United States. The number of ANPs nationally is projected to increase from 58,000 in 1995 to 170,000 in 2015. Specialization has lagged behind, with only 23 ANP programs and one PA oncology training program. The Oncology Nursing Society documented an increase in ANPs from 35 in 1994 to 663 in 1998.6 In 2005, the American Academy of Nurse Practitioners estimated that there were only 2,400 oncology-trained ANPs nationally.7
Studies of ANP roles in clinical practice have surveyed ANPs and appear mainly in nursing journals, which are read infrequently by physicians. In an effort to delineate the roles of nonphysician practitioners in medical oncology as seen from the perspective of medical oncology practices, the Washington State Medical Oncology Society (WSMOS; Vancouver, WA) applied for and was awarded a 2008 ASCO State Affiliate Grant to evaluate how ANPs and PAs function in medical oncology practices and develop a directory of Washington medical practices and educational institutions to stimulate increased training and recruitment of medical personnel in the field of medical oncology. This report presents the results of the medical practice/midlevel provider portion of this project.
Methods
Using Surveymonkey.com as a platform, the survey collected data on practice demographics, number of employed physicians, employment patterns, functions of ANPs and PAs at each practice, roles of medical personnel in research activities, and practices' experience with providing training opportunities for medical personnel. No data were requested about procedures performed by ANPs or PAs. Medical oncology practices were self-categorized as single specialty, part of a multispecialty group practice, hospital based, or academic (ie, university based). Human resources directors, nurse managers, WSMOS physician members, and all ASCO physician members from Washington were e-mailed a request to respond to the survey. In addition to a Web link in the e-mail request, the survey link was posted on the WSMOS Web site (http://www.wsmos.org).
Results
Of the 49 identified Washington medical oncology practices, 25 completed the survey, a response rate of 50%. The respondents were evenly divided with eight single-specialty, seven multispecialty, and six hospital-based practices responding. Four separate units in the University of Washington, Seattle Children's Hospital, Fred Hutchinson Cancer Center Consortium (Seattle Cancer Care Alliance) comprised the academic respondents. These practices represented 38 physicians in single-specialty groups, 61 in multispecialty groups, 36 in hospital-based practices, and 78 in the academic setting.
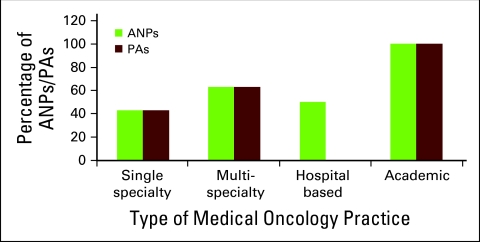
Of the 25 practices, 17 (68%) employed ANPs or PAs. ANPs were employed by 43% of single-specialty, 63% of multispecialty, 50% of hospital-based, and 100% of academic practices. PAs were employed by 43% of single-specialty, 63% of multispecialty, 0% of hospital-based, and 100% of academic practices. Because of differences in employment patterns, five of eight single-specialty and six of seven multispecialty practices used some type of physician extender. Figure 1 presents the employment of NPs and PAs by practice type.
Figure 1.
Employment of advanced nurse practitioners (ANPs) physician assistants (PAs) by type of medical oncology practice. Graph represents percentage of responding practices that employed ANPs and PAs.
ANPs worked independent of supervision in 64% of these practices. The survey did not ask whether they billed independently or worked off site. ANPs were more likely than PAs to perform outpatient follow-up (93% v 77%), evaluate patients in infusion centers (71% v 62%), and provide genetic counseling (43% v 0%).
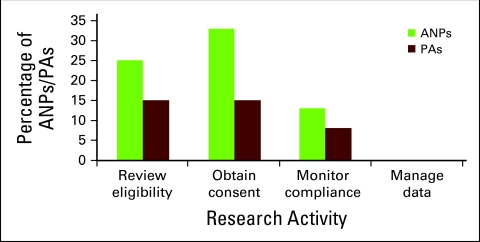
No PAs worked independently. PAs saw hospitalized patients more frequently than ANPs (62% v 42%) and were more likely to supervise infusion areas (15% v 7%). No PAs or NPs routinely administered chemotherapy. PAs and ANPs provided new outpatient consultations with equal frequency (29% v 31%). Figure 2 presents ANP and PA functions, and Figure 3 describes ANP and PA activities in practices performing research. Of practices employing ANPs/PAs, 15 responded to questions related to research activity. NPs were more likely than PAs to review eligibility for research studies (25% v 15%), obtain informed consent (33% v 15%), and monitor compliance (13% v 8%). No ANPs or PAs performed data management.
Figure 2.
Functions of advanced nurse practitioners (ANPs) physician assistants (PAs) in Washington medical oncology practices. Results represent the roles fulfilled by ANPs and PAs as a percentage of all responding medical oncology practices employing ANPs or PAs. Genetic counseling includes evaluating patients with known genetic mutations, providing counseling for possible genetic mutations, and providing appropriate preventive measures. Supervising infusion areas includes management of personnel and drug procurement in inpatient and outpatient chemotherapy infusion areas but not administration of chemotherapy.
Figure 3.
Activity of advanced nurse practitioners (ANPs) physician assistants (PAs) in practices performing research. Results represent ANP/PA research roles in practices reporting employing ANPs or PAs. No ANPs or PAs performed data management.
Discussion
This survey demonstrates the broad acceptance by Washington medical oncology practices of the diverse roles that ANPs and PAs perform. The 2007 ASCO workforce analysis predicted a shortage of 2,550 to 4,040 oncologists by 2020.1,2 Erikson et al1 estimated that these nonphysician practitioners—with an estimated productivity of 85% of that of a physician, and with current PA and ANP oncology programs being few—would increase physician productivity by only 4% to 11%. Recruitment of medical personnel at all levels to medical oncology practices, mentoring programs, and practice support of advanced training for personnel may help medical oncology compete for these valued professionals. The WSMOS initiative to create a directory cross-linking medical oncology practices and educational institutions in Washington and enhance awareness of the professional roles ANPs and PAs perform is our first effort to help alleviate this anticipated workforce shortage.
Acknowledgment
The Washington State Medical Oncology Society gratefully acknowledges ASCO for its support of this project, which was funded by a grant from the ASCO State Affiliate Grant Program in 2008. ASCO State Affiliate Grants are designed to help state affiliate societies in their promotion of quality care for patients with cancer in their states.
Author's Disclosures of Potential Conflicts of Interest
The author indicated no potential conflicts of interest.
References
- 1.Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: Challenges to assuring access to oncology services. J Oncol Pract. 2007;3:79–86. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warren JL, et al. Current and Future Utilization of Services from Medical Oncologists. J Clin Oncol. 2008;26:3242–3247. doi: 10.1200/JCO.2007.14.6357. [DOI] [PubMed] [Google Scholar]
- 3.Erikson C, Schulman S, Kosty M, et al. Oncology workforce: Results of the ASCO 2007 Program Directors Survey. J Oncol Pract. 2009;5:62–65. doi: 10.1200/JOP.0922003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones PE. Physician assistant education in the United States. Acad Med. 2007;82:882–887. doi: 10.1097/ACM.0b013e31812f7c0c. [DOI] [PubMed] [Google Scholar]
- 5.Larson EH, Hart LG. Growth and changes in physician assistant workforce in the United States, 1967-2000. J Allied Health. 2007;36:121–130. [PubMed] [Google Scholar]
- 6.Lynch MP, Cope DG, Murphy-Ende K. Advanced practice issues: Results of the ONS Advanced Practice Nursing survey. Oncol Nurs Forum. 2001;28:1521–1530. [PubMed] [Google Scholar]
- 7.Young T. Utilizing oncology nurse practitioners: A model strategy. Comm Oncol. 2005;2:218–224. [Google Scholar]