Abstract
When using community-based participatory methods to develop health promotion programs for specific communities, it is important to determine if participation differs based on sociodemographics and the extent to which program participants are demographically representative of the target community, especially when non-random recruitment methods are used. We evaluated rates of participating in a health promotion program among African American residents in an urban community and determined if program participants were representative of community residents in terms of sociodemographic factors. While participation in the program was modest, participation did not differ based on psychological factors or body mass index. However, individuals who were unemployed were significantly more likely to participate in the program compared with those who were employed. Our sample included a greater proportion of individuals who only had a high school education compared with community residents but was similar to community residents in terms of gender, marital status and employment.
Introduction
Each year, thousands of African Americans experience morbidity and mortality from several chronic diseases. National studies continue to demonstrate that African Americans are at greater risk than non-Hispanic Whites for developing most forms of cancer [1] and cardiovascular diseases [2]. Health promotion programs developed to address the specific needs of this population include community-based programs that provide education and training on strategies for eating a healthy diet and being more physically active [3, 4]. In addition to evaluating the effects of these programs on health behaviors and other outcomes, it is important to determine the extent to which programs reach the intended audiences and whether or not participation differs based on sociodemographic factors and other variables. When programs are offered in specific settings such as churches or in partnership with other types of sponsoring organizations, the population reached can be estimated by knowing the membership and characteristics of the organization or clientele [5]. However, when programs are developed and offered to African Americans using non-random community-based approaches, it may be more difficult to estimate their reach because exposure to recruitment initiatives (e.g. health fairs, newspaper advertisements) is unknown. In these instances, it is useful to determine the extent to which program participants are demographically representative of the target community and to evaluate rates of program participation.
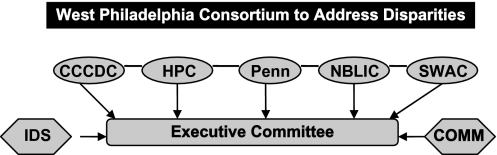
In 2007, we conducted an exploratory study to evaluate the feasibility of offering an integrated risk counseling program for cancer and cardiovascular disease to African American men and women who were residents of an urban community in a large metropolitan city. This research was conducted as part of the West Philadelphia Consortium to Address Disparities, which is an academic-community partnership consisting of four community-based organizations in Philadelphia, PA (the Christ of Calvary Community Development Corporation, the Health Promotion Council of Southeastern Pennsylvania, the Philadelphia Chapter of the National Black Leadership Initiative on Cancer and the Southwest Action Coalition) and academic researchers and staff from the University of Pennsylvania. Consistent with the principles of community-based participatory research (CBPR) [6, 7], the partnership was developed to facilitate collaboration between community and academic members on research efforts to address the health priorities and concerns of community residents. As such, community and academic members (e.g. E.D., V.B., C.H.H., B.W.) of the partnership shared responsibility for developing the intervention and monitoring accrual to the study. Collaboration on these issues, and strategic direction for the partnership, was achieved through regular meetings of the Executive Committee, which consisted of academic and community representatives (Fig. 1).
Fig. 1.
Organizations in the West Philadelphia Consortium to Address Disparities.
The intervention was developed to increase motivation for eating a healthier diet and increasing physical activity among African American residents in West and Southwest Philadelphia. We focused on this community for several reasons. First, focusing on a specific geographic community is in line with the principles of CBPR [7]. Also, since the University of Pennsylvania is located in West Philadelphia, we believed that it was important to implement our research and develop programs in a setting that would build on the activities at an important resource for health care in the West and Southwest Philadelphia community. Finally, several of the census tracts in West and Southwest Philadelphia have been designated as Health Professional Shortage Areas. According to the 2000 census, of the more than 200 000 residents in West and Southwest Philadelphia, more than 70% are African American and/or Black, and within this population, 41% are men and 59% are women. In addition, 40% are in the labor force and 27% live below poverty [8].
The purpose of the present study was to evaluate rates of participation in an integrated risk counseling program that was developed through the partnership. Because recent reports suggest that among African Americans, decisions to participate in health promotion programs offered in research settings might be influenced by factors such as the amount of community support for participation (e.g. endorsement of community leaders), sociodemographic factors (e.g. education), psychological variables (e.g. perceived risk) and risk factors for disease [9, 10], we evaluated the relationship between participation in the program and sociodemographic factors, health beliefs and intentions to make behavioral changes. We also assessed the representativeness of our sample in comparison to the demographic composition of our target community because we used non-random methods to recruit individuals to participate in the intervention.
Materials and methods
Study population
This study was conducted at the University of Pennsylvania and was approved by the Institutional Review Board. Participants were adult African American men and women who were residents in an urban community in Philadelphia. To be eligible for participation, individuals had to be at least 18 years of age and be a current resident in West or Southwest Philadelphia. Individuals who had a personal history of cancer and those who had ever had a heart attack, stroke or heart disease were not eligible for participation in the study because our interest was in assessing motivation for behavior change for the primary prevention of these conditions.
Procedures
Participant recruitment and eligibility
Participants were recruited into the study through self-referrals from newspaper advertisements, flyers and health fairs from July 2007 through November 2007. Advertisements were placed in free regional and community newspapers. These advertisements described the study as a research program that would provide information about risk factors for cancer and cardiovascular disease and strategies for improving one's health. Participants were also told about the study by community members of the partnership and also by individuals who had completed the risk counseling program. Regardless of how people learned about the study, those who were interested in participating were instructed to call the study line for additional information. Following self-referral, a screening interview was completed to determine eligibility; those who were eligible to participate in risk counseling completed a baseline telephone interview. The interview was a 30-minute structured questionnaire that obtained information on sociodemographics, height and weight, perceived risk of developing cancer and cardiovascular disease, self-efficacy for diet and physical activity and motivation to eat healthier and exercise more. Prior receipt of advice to lose weight was also assessed during the baseline. These interviews were conducted by research assistants at the University of Pennsylvania following provision of verbal consent; at the end of the interview, individuals were invited to participate in risk counseling.
Intervention
Risk counseling consisted of participating in a group session during which individuals received information about the occurrence of cancer and cardiovascular disease in African Americans, risk factors for these diseases and strategies for reducing their risk using a multimedia format. The program was developed by members of the partnership to address the health priorities and concerns of African American residents that were identified through a multiphase needs assessment that included focus groups, key informant interviews and community health survey and used the health belief model as the conceptual framework [11]. To facilitate the process of developing the intervention, we formed an Intervention Development Subcommittee (IDS) that consisted of academic and community members of the partnership (e.g. E.D., V.B., C.H.H., B.W.). The IDS met regularly to develop the objectives for the intervention, develop its content and strategies to increase behavioral motivations and develop methods for evaluating the effects of the intervention. As part of risk counseling, participants completed activities that were designed to highlight the connection between risk factors for cancer and cardiovascular disease (e.g. obesity, diet, physical activity). For instance, following a video presentation about risk factors for cardiovascular disease [12], the facilitator led a discussion about risk factors for cancer during which individuals were asked to describe risk factors for this disease. Participants then completed a group exercise in which they identified risk factors that were common to both cancer and cardiovascular disease. Elements from motivational interviewing [13] were also included in the protocol to increase motivation to make behavioral change. Specifically, participants completed a values clarification exercise and were asked to indicate how motivated and confident they were to make changes in their diet and physical activity practices. An experienced health educator facilitated the risk counseling sessions and each session lasted about 2–3 hours. All the counseling sessions were held during a weekday evening at the University of Pennsylvania using a group format. Eight sessions were held during the study period and the average number of participants in each session was 13. Written informed consent was obtained prior to the provision of counseling, those who completed counseling received an incentive of $20 and $15 was also provided to compensate individuals for travel-related expenses.
Measures
Sociodemographics
Gender, age, marital status, education level, employment status and income were obtained by self-report during the baseline telephone interview. We recoded marital status, education, employment and income into dichotomous variables based on the distribution of responses.
Body mass index
We obtained height and weight by self-report during the baseline telephone interview and calculated body mass index (BMI in kilograms per square meter) using the formula: weight (lb)/(height (in))2 × 703.
Risk perceptions
We used items from previous research to evaluate perceived risk of developing cancer and cardiovascular disease [14]. Specifically, participants were asked to indicate how likely it was that they would develop specific forms of these diseases compared with other individuals of their age (1 = much lower, 2 = a little lower, 3 = the same, 4 = a little higher and 5 = much higher). In this report, we focused on perceived risks of developing colon cancer and having a heart attack.
Self-efficacy
We used instruments from previous research to evaluate perceptions of confidence to eat a healthy diet and to be more physically active. Specifically, dietary self-efficacy was assessed in terms of perceived confidence to eat fruit and vegetables under a variety of circumstances (e.g. have extra vegetables at dinner, have fruits and vegetables when they were tired) [15]. Similarly, the self-efficacy for physical activity scale [16] asked participants to indicate how confident they were that they could be physically active under various conditions (e.g. if tired, during inclement weather, when they were busy). Both instruments had good internal consistency (Cronbach's alpha for diet and physical activity self-efficacy was 0.86 and 0.79, respectively).
Behavioral motivations
We developed items to evaluate motivations for behavioral change. Specifically, participants were asked to indicate how likely it was that they would try to eat healthier and exercise more (1 = not at all likely, 2 = a little likely, 3 = somewhat likely and 4 = very likely) during the next month as a part of the baseline telephone interview.
Participation and representativeness variables
As in prior reports [10], we assessed participation in the program in terms of the proportion of individuals found to be eligible who completed a risk counseling session. Participation in the program involved completing one risk counseling session. Individuals who completed counseling were categorized as program acceptors and those who declined to participate in the program or did not complete the session after accepting the invitation were categorized as non-participants. The representativeness of the program participants was determined based on the extent to which our program participants were similar to African American residents in West and Southwest Philadelphia in terms of sociodemographic characteristics (e.g. gender, marital status, education level, employment status).
Data analysis
First, we generated descriptive statistics to characterize participants in terms of sociodemographic factors and participation in risk counseling. In order to determine whether participants in our sample were representative of the target community (e.g. African American residents in West and Southwest Philadelphia), we conducted exact one-sample hypothesis tests. Specifically, we compared the prevalence of key sociodemographic variables (e.g. gender, marital status, education, employment status) from our study sample with those for these characteristics among African American residents in the seven Zip codes for West and Southwest Philadelphia using exact binomial methods. Information on sociodemographic characteristics was computed from data in the 2000 census [8]. Specifically, we extracted data for gender, education and employment from the total population of African American and/or Black residents who were at least 18 years of age and created dichotomous variables for these characteristics that were conceptually similar to those that were obtained during the baseline telephone interview. Information on marital status was not available specifically for African Americans; therefore, we used the percent married for all residents in West and Southwest Philadelphia. We then conducted chi square tests of association to evaluate the relationship between participation in risk counseling and sociodemographic characteristics, perceived risk variables, self-efficacy and behavioral motivations. All statistical tests were performed at the alpha = 0.05 level and were two sided.
Results
A total of 285 individuals self-referred for participation in the study. Of the individuals who self-referred for participation, 218 (76%) completed the screening interview and 156 were eligible to participate. The enrollment rate equaled the number of eligible individuals who enrolled in the study divided by the total number of eligible individuals. Of the 156 eligible individuals, 137 (88%) enrolled in the study, completed the baseline telephone interview and were invited to participate in risk counseling. Since eligible individuals who did not complete the baseline telephone interview (n = 20) did not enroll in the study and were not invited to participate in risk counseling, the rate for participating in risk counseling (74%) equaled the number of program acceptors (n = 101) divided by the total number of individuals who enrolled in the study (n = 137) [A more conservative estimate of program participation (65%) can be calculated from the total number of eligible individuals (n = 156) divided by the number of program acceptors (101).]. Most of the individuals who participated in risk counseling were recruited from newspaper advertisements (60%) that were placed in a free regional circular.
Table I shows the bivariate analysis of participation in risk counseling. There were no differences in participation in terms of gender, marital status, education, income, perceived risk or motivation variables. There were also no differences between participants and non-participants in BMI or self-efficacy (Table II). However, individuals who were unemployed were significantly more likely to participate in risk counseling compared with those who were employed.
Table I.
Participation in risk counseling by sociodemographic characteristics, risk perception and behavioral motivation among survey respondents (n = 137)a
| Variable | Level | % Participate | Chi square | P value |
| Sociodemographic characteristics | ||||
| Gender | Male | 73 | 0.12 | 0.72 |
| Female | 76 | |||
| Marital status | Married | 80 | 0.86 | 0.35 |
| Not married | 73 | |||
| Education level | ≥Some college | 75 | 0.05 | 0.82 |
| ≤High school | 73 | |||
| Employment status | Employed | 63 | 5.66b | 0.02 |
| Not employed | 81 | |||
| Income level | <$20 000 | 74 | 0.006 | 0.94 |
| ≥$20 000 | 73 | |||
| Perceived risk and motivation variables | ||||
| Colon cancer | Higher or much higher | 82 | 0.90 | 0.34 |
| Same/lower | 72 | |||
| Heart attack | Higher or much higher | 79 | 0.63 | 0.43 |
| Same/lower | 72 | |||
| Advice to lose weight | Yes | 73 | 0.06 | 0.81 |
| No | 75 | |||
| Exercise more | Very likely | 79 | 1.36 | 0.24 |
| Less likelyb | 70 | |||
| Eat healthier | Very likely | 77 | 1.02 | 0.31 |
| Less likelyb | 69 | |||
Sample sizes for some comparison do not equal 137 because of missing data. The n represents the number of eligible individuals who enrolled in the study and completed the baseline telephone interview.
Less likely represents respondents who reported not likely, a little likely or somewhat likely.
Table II.
Participation in risk counseling by BMI and self-efficacy (n = 137)a
| Variable | Participants | Non-participants | t Value | P value |
| Mean (SD) | Mean (SD) | |||
| BMI (kg/m2) (range 19.4–50 kg/m2) | 29.9 (6.7) | 30.6 (6.9) | 0.54 | 0.59 |
| Dietary self-efficacy score (range 9–45) | 33.4 (6.4) | 32.4 (7.6) | 0.77 | 0.44 |
| Physical activity self-efficacy score (range 13–35) | 22.6 (4.8) | 22.3 (4.4) | 0.29 | 0.77 |
N represents the number of eligible individuals who enrolled in the study and completed the baseline telephone interview.
Table III shows the characteristics of our study sample compared with African American residents in West and Southwest Philadelphia. Consistent with the characteristics of community residents, our sample included more females than males and the proportion of men and women who participated in risk counseling was consistent with the percentage of male and female residents. In addition, a comparable proportion of risk counseling participants were not married relative to community residents. However, our sample included a greater proportion of individuals who only had a high school education relative to community residents.
Table III.
Representativeness of risk counseling participants compared with community residents
| Variable | Level | Risk counseling participants (%) | Community residents based on 2000 US census (%) | P value*** |
| Gendera | Male | 37 | 41 | 0.4187 |
| Female | 63 | 59 | ||
| Marital statusb | Not married | 71 | 66 | 0.2941 |
| Education levelc | High school graduate | 34 | 21 | 0.0031 |
| Employment status | Employed | 32 | 40 | 0.1037 |
Data for community residents are based on those who are 18 years and older.
Data for community residents are based on those who are 25 years and older.
Census data reflect information on the percent married for all residents in West and Southwest Philadelphia. We determined the percent not married based on this information. According to census data, 34% of residents in West and Southwest Philadelphia are married. Using this information, we determined that 66% were not married.
P value for the exact binomial test is the probability that observed risk counseling prevalence is equal to the prevalence in community residents, the target population (versus the two-sided alternative that they are not equal).
Discussion
The purpose of this study was to evaluate whether participation in a health promotion program that was offered as part of an academic-community partnership for cancer and cardiovascular disease differed based on sociodemographic factors and psychological variables in a community-based sample of African American men and women. We also evaluated the extent to which our sample was demographically representative of our target community. Although a benefit of CBPR is that it may increase the relevancy of studies and overcome barriers to participation such as mistrust [6, 7], the rate for participating in the risk counseling intervention offered in the present study was modest. However, our participation rates were greater than those reported in other research that did not use a CBPR framework. For instance, only about 50% of African American women participated in a cancer risk counseling program that was offered as part of a genetic counseling research protocol [10] and attendance at a breast health and weight loss intervention ranged from 41 to 55% among African American women [17]. We did not find differences between participants and non-participants based on BMI or psychological factors and participation in the program did not differ based on gender, martial status, education or income. However, individuals who were unemployed were significantly more likely to participate in risk counseling compared with those who were employed. This could be because individuals who are not working have greater availability. The counseling sessions were offered during a weekday evening; thus, it may be important to offer health promotion programs at other times such as on weekends and at other locations in the community in order to provide greater opportunities for participation among individuals who are employed. Alternatively, individuals who were unemployed may have been more receptive to the financial incentive that was provided following completion of risk counseling. Previous reports have shown that financial incentives are effective at increasing response rates among female residents in minority Zip codes [18]. Similarly, giving potential participants a prepaid incentive along with promising an additional amount for retention led to equal enrollment rates among gender and racial groups in a study that evaluated enrollment in an online program for heath behavior [19]. It is important to note that differences in participation based on employment status did not affect the representativeness of the sample for this variable. This suggests that differences in participation based on sociodemographic factors may not necessarily affect the representativeness of the sample.
With a few exceptions, our sample was comparable to community residents in terms of sociodemographic factors. We found that a greater proportion of our sample only had a high school education compared with the proportion of community residents who only had this amount of formal education. This finding could be the result of using non-random methods to recruit participants and may be a reflection of the characteristics of individuals who read free circulars, attend health fairs or are responsive to flyers posted in community locations. Although we did not compare participation in the program based on recruitment source, our findings suggest that it is important to use recruitment strategies and sources that are likely to reach potential participants who are diverse in terms of sociodemographic characteristics and comparing the effects of these approaches in future research [20].
In considering the results of this study, some limitations should be noted. First, our participation rates may not be comparable to those in health promotion programs that involve multiple visits and have more complex study procedures. In addition, we provided a financial incentive for participating in risk counseling. Nevertheless, our study provides novel insight on the outcomes of using non-random community-based approaches to recruit African Americans in a specific community context. Because of the challenges associated with recruiting African Americans to participate in health promotion research, investigators are likely to use a number of different strategies to reach accrual goals. These approaches are likely to have some benefits as well as limitations. Our findings demonstrate that non-random methods are likely to yield a sample that is mostly representative of the larger community from which it was drawn. Furthermore, there is not likely to be systematic participation bias based on most sociodemographic or psychological factors. Future studies should identify strategies that are most effective in terms of recruiting representative samples and those that yield a high participation rate.
Funding
National Center on Minority Health and Health Disparities (R24MD001594 to C.H.H.).
Conflict of interest statement
None declared.
Acknowledgments
We are very appreciative to all the individuals who participated in this research. We would like to thank Amy Hillier, PhD, Latifah Griffin, BA, Aliya Collier, BA, and George Moody for assistance with data collection and management.
References
- 1.American Cancer Society. Cancer Facts and Figures. Atlanta, GA: American Cancer Society; 2009. [Google Scholar]
- 2.American Heart Association. Heart Disease and Stroke Statistics. Dallas, TX: American Heart Association; 2007. [Google Scholar]
- 3.Resnicow K, Jackson A, Wang T, et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the Eat for Life Trial. Am J Public Health. 2001;91:1686–93. doi: 10.2105/ajph.91.10.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hart A, Jr, Tinker L, Bowen DJ, et al. Correlates of fat intake behaviors in participants in the eating for a healthy life study. J Am Diet Assoc. 2006;106:1605–13. doi: 10.1016/j.jada.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Bopp M, Wilcox S, Laken M, et al. Using the RE-AIM framework to evaluate a physical activity intervention in churches. Prev Chronic Dis. 2007;4:A87. [PMC free article] [PubMed] [Google Scholar]
- 6.Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 7.Israel BA, Schulz AJ, Parker EA, et al. Critical issues in developing and following community based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass; 2003. pp. 53–76. [Google Scholar]
- 8.U.S. Census Bureau. Census 2000 data releases. Available at: http://www.census.gov/main/www/cen2000.html. Accessed: December 2008. [Google Scholar]
- 9.Ashing-Giwa KT. Can a culturally responsive model for research design bring us closer to addressing participation disparities? Lessons learned from cancer survivorship studies. Ethn Dis. 2004;15:130–7. [PubMed] [Google Scholar]
- 10.Halbert CH, Brewster K, Collier A, et al. Recruiting African American women to participate in hereditary breast cancer research. J Clin Oncol. 2005;23:7967–73. doi: 10.1200/JCO.2004.00.4952. [DOI] [PubMed] [Google Scholar]
- 11.Janz NK, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 2002. pp. 45–66. [Google Scholar]
- 12.Association of Black Cardiologists, Inc, The Congress of National Black Churches, Inc, Bristol-Myers Squibb Company. 7 Steps to a Healthy Heart for African Americans [Video] Copyright 2002. [Google Scholar]
- 13.Rollnick S, Butler CC, Stott N. Helping smokers make decisions: the enhancement of brief intervention for general medical practice. Patient Educ Couns. 1997;31:191–203. doi: 10.1016/s0738-3991(97)01004-5. [DOI] [PubMed] [Google Scholar]
- 14.Hughes C, Lerman C, Lustbader E. Ethnic differences in risk perception among women at increased risk for breast cancer. Breast Cancer Res Treat. 1996;40:25–35. doi: 10.1007/BF01806000. [DOI] [PubMed] [Google Scholar]
- 15.Henry H, Reimer K, Smith C, et al. Associations of decisional balance, processes of change, and self-efficacy with stages of change for increased fruit and vegetable intake among low-income, African-American mothers. J Am Diet Assoc. 2006;106:841–9. doi: 10.1016/j.jada.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 16.McNeill LH, Wyrwich KW, Brownson RC, et al. Individual, social environmental, and physical environmental influences on physical activity among black and white adults: a structural equation analysis. Ann Behav Med. 2006;31:36–44. doi: 10.1207/s15324796abm3101_7. [DOI] [PubMed] [Google Scholar]
- 17.Fitzgibbon ML, Stolley MR, Schiffer L, et al. A combined breast health/weight loss intervention for Black women. Prev Med. 2005;40:373–83. doi: 10.1016/j.ypmed.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Whiteman MK, Langenberg P, Kjerulff K, et al. A randomized trial of incentives to improve response rates to a mailed women's health questionnaire. J Womens Health. 2003;12:821–8. doi: 10.1089/154099903322447783. [DOI] [PubMed] [Google Scholar]
- 19.Alexander GL, Divine GW, Couper MP, et al. Effect of incentives and mailing features on online health program enrollment. Am J Prev Med. 2008;34:382–8. doi: 10.1016/j.amepre.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]