Summary
Anthrax lethal toxin triggers death in some cell types, such as macrophages, and causes a variety of cellular dysfunctions in others. Collectively, these effects dampen the innate and adaptive immune systems to allow Bacillus anthracis to survive and proliferate in the mammalian host. The diverse effects caused by the toxin have in part been attributed to its interference with signaling pathways in target cells. Lethal factor (LF) is the proteolytic component of the toxin, which cleaves six members of the mitogen activated protein kinase kinase (MAPKK) family after being delivered to the cytosol by the cell-binding component of the toxin, protective antigen. The effect of cleaving these MAPKKs is to interfere with ERK, p38 and JNK signaling. Here we characterize an LF mutant, LF-K518E/E682G, that is defective at causing pyroptosis in RAW 264.7 cells and at activating the Nlrp1b inflammasome in a heterologous expression system. LF-K518E/E682G does not exhibit an overall impairment of function, however, because it is able to downregulate the ERK pathway, but not the p38 or JNK pathways. Furthermore, LF-K518E/E682G efficiently killed melanoma cells, which were shown previously to undergo apoptosis in response to lethal toxin or to pharmacological inhibition of the ERK pathway. Our results suggest that LF-K518E/E682G is defective at cleaving a substrate involved in the activation of the Nlrp1b inflammasome.
Keywords: lethal toxin, anthrax, MAPKK, Nlrp1b
Introduction
Bacillus anthracis lethal toxin (LeTx) is a binary toxin that is released by the bacterium during an infection. It consists of a proteolytic component, lethal factor (LF), and a cell-binding component, protective antigen (PA), which delivers LF to the mammalian cell cytosol [1, 2]. Injection of purified LeTx into animals causes death, possibly by inducing vascular leakage that leads to shock and multi-organ failure [3-6]. The role of LeTx in anthrax pathogenesis is complex, however, and likely involves the impairment of the innate and adaptive immune responses in a number of ways that aid bacterial survival. In particular, LeTx kills a subset of immune cell types and reduces function in others [7-9].
LeTx kills only certain cell types even though the known substrates of LF, mitogen activated protein kinase kinases (MAPKKs) 1-4, 6 and 7, are ubiquitously expressed and toxin receptors have been found on all cell types that have been tested [10, 11]. Receptor expression level influences the degree of toxin-sensitivity, but it does not determine whether a cell is inherently susceptible or resistant to killing [12, 13]. Cells that require ERK activity to proliferate tend to undergo apoptosis upon LeTx treatment, whereas intoxicated macrophages from certain strains of mice are rapidly killed by pyroptosis. Pyroptosis differs from apoptosis in that it is a pro-inflammatory form of cell death that depends on caspase-1 activity.
A highly polymorphic gene, Nlrp1b (Nalp1b), encodes a protein required for the pyroptotic response to LeTx observed in macrophages derived from some mouse strains (e.g. BALB/cJ, C3H/HeJ) [14]. Nlrp1b detects the activity of LF and assembles into an inflammasome complex that activates caspase-1, which mediates LeTx-induced pyroptosis [14-17]. Other mouse strains (e.g. A/J, C57BL/6J) express an allele of Nlrp1b that appears to encode a protein that is non-responsive to LeTx. Macrophages from these strains of mice undergo apoptosis after LeTx-treatment, but only if they have been activated by bacterial components. One group has suggested that concomitant activation of the cells and downregulation of the p38 MAPK pathway is sufficient to cause apoptosis [18], although pharmacological inhibition of p38 did not mimic LeTx activity in another study [19]. The involvement of MAPK pathway inhibition in the pyroptotic response to LeTx has not been established.
Some tumor cell lines are susceptible to killing by LeTx. In many tumor cells, including melanoma cells, the ERK pathway is constitutively activated, which promotes proliferation and survival. Downregulation of this pathway by LeTx or U0126, a MAPKK1/2 inhibitor, caused apoptosis in melanoma cells [20]. Furthermore, treatment of human melanoma tumors in nude mice with sublethal doses of LeTx led to tumor regression without any obvious side effects [20], suggesting that LeTx could potentially be used as a cancer therapeutic [21].
We performed random mutagenesis on the catalytic domain of LF and screened the resulting mutants for ones that were defective at killing the murine macrophage cell line, RAW 264.7. We report here the characterization of a double mutant obtained from the screen, LF-K518E/E682G. In combination with PA, LF-K518E/E682G was defective at killing RAW 264.7 cells and at activating the Nlrp1b inflammasome in a reconstituted expression system. LF-K518E/E682G exhibited wild-type levels of activity towards some, but not all, of its MAPKK substrates and consequently the mutant reduced phosphorylation of ERK, but not of JNK or p38. LF-K518E/E682G also reduced ERK phosphorylation in a melanoma cell line, but in contrast to what was observed in RAW 264.7 cells, the mutant was able to efficiently kill these cells. These data are consistent with the notion that induction of pyroptosis and apoptosis by LF occurs through the cleavage of distinct substrates.
Results and Discussion
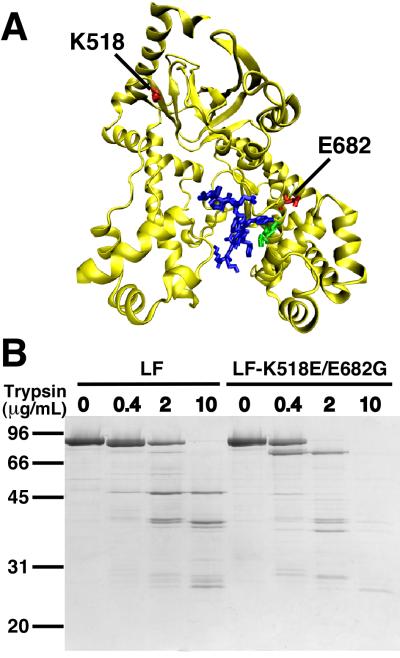
We screened a collection of LF mutants, which were generated by error-prone PCR, for a mutant that was defective at killing RAW 264.7 cells (data not shown). One of the identified mutants contained two substitution mutations, K518E and E682G (Fig. 1A). Amino acid K518 is within a patch of amino acids that was previously implicated in binding MAPKKs [22]. Amino acid E682 is within an α-helix that also contains the amino acids that form the 686HExxH690 metalloprotease motif (Fig. 1A) [23]. We performed a limited tryptic digest to assess whether the mutations altered the tertiary structure of LF. Purified wild-type LF or LF-K518E/E682G was incubated with various concentrations of trypsin and the mixtures were then subjected to SDS-PAGE. Differences between the patterns of tryptic fragments were observed for LF-K518E/E682G and wild-type LF and the mutant appeared to be somewhat more sensitive to trypsin (Fig. 1B). This suggested that while the mutations altered the tertiary structure of the protein, they did not cause it to become grossly misfolded and destabilized. Since we were interested in characterizing a mutant with altered catalytic properties, rather than identifying amino acids that might bind substrates directly, we decided to study this mutant further.
Figure 1.
An LF double mutant, LF-K518E/E682G. (A) Structure of the catalytic domain of LF. Amino acids 518 and 682 are shown in red. Residues of the HExxH motif are depicted in green. An optimized peptide substrate is shown in blue. The model was created using coordinates from PDB 1PWW [23] and the computer programs VMD 1.8.3 [26] and POV-Ray 3.6. (B) Limited tryptic digest of wild-type and mutant LF. LF or LF-K518E/E682G was incubated with indicated concentrations of trypsin for 1 h. Protein samples were subjected to SDS-PAGE and stained with Coomassie blue.
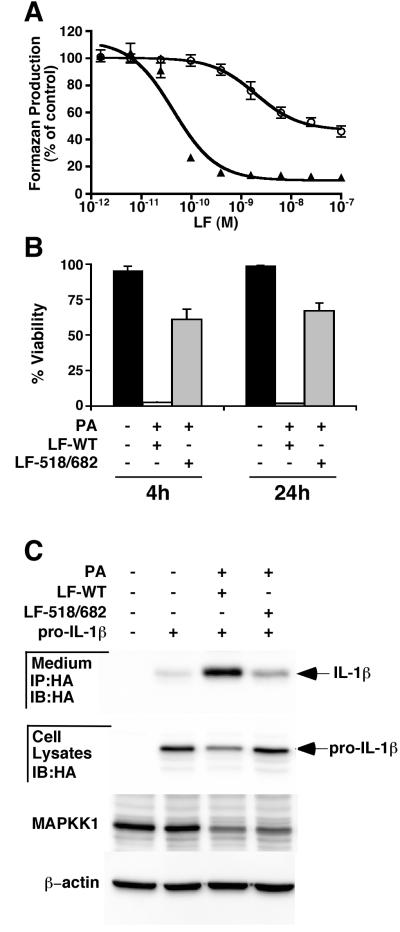
We first assessed the severity of the cytotoxicity defect caused by the mutations. PA and various concentrations of either wild-type LF or LF-K518E/E682G were incubated with RAW 264.7 cells for 4 h and cell viability was estimated using the MTS assay, which measures mitochondrial function. Whereas the concentration of LF required to kill 50% of the cells (EC50) was estimated to be 4 × 10−11 M, LF-K518E/E682G did not cause enough cell death under these conditions for an accurate EC50 to be determined (Fig. 2A). Increasing the time of toxin exposure from 4 h to 24 h did not markedly decrease the EC50 for wild-type LF or decrease the viability of cells exposed to the mutant (data not shown). The reduced ability of the LF mutant to kill RAW 264.7 cells was tested further using a trypan blue exclusion assay (Fig. 2B). Cells were left untreated (black bars) or were exposed to a mixture of 10−8 M PA and 10−8 M wild-type LF (white bars) or mutant LF (grey bars) for either 4 h or 24 h and the fraction of cells that excluded trypan blue under each condition was determined. Similar to what was observed using the MTS assay, this assay indicated that LF-K518E/E682G was less cytotoxic than wild-type LF; increasing the time of toxin incubation from 4 h to 24 h did not lead to an increased level of cell death (Fig. 2B).
Figure 2.
LF-K518E/E682G is defective at killing RAW 264.7 cells and inducing the Nlrp1b inflammasome. (A) PA and various concentrations of wild-type LF (σ) or LF-K518E/E682G (○) were incubated with RAW 264.7 cells and viability was assessed after 4 h using the MTS assay. Values represent the mean ± standard error of the mean for three independent experiments. (B) RAW 264.7 cells were left untreated (black bars) or treated with PA and wild-type LF (white bars) or PA and LF-K518E/E682G (grey bars) for 4 h or 24 h. Viability was assessed as the fraction of cells that excluded trypan blue. Values represent the mean ± standard error of the mean for three independent experiments. (C) HT1080 cells were mock transfected or were transfected with plasmids encoding Nlrp1b, pro-caspase-1 and pro-IL-1b. After 24 h, cells were treated with PA and either wild-type LF or LF-K518E/E682G. IL-1β, MAPKK1, and β-actin were detected by immunoblotting. The results shown represent three independent experiments.
To confirm that LF-K518E/E682G is defective at activating Nlrp1b, we used an independent approach that takes advantage of a recently developed heterologous expression system [24]. HT1080 human fibroblasts were transfected with plasmids encoding murine Nlrp1b, pro-caspase-1 and pro-IL-1β and after ~24 h the cells were treated with combinations of PA, LF and LF-K518E/E682G. PA and LF activated the inflammasome as determined by the loss of pro-IL-1β in the cytosol and the appearance of IL-1β in the cell supernatants (Fig 2C). A lower level of IL-1β was found in the supernatants of cells treated with LF-K518E/E682G, suggesting that the mutant was defective at activating the inflammasome. LF-K518E/E682G entered cells and was catalytically active, however, since it cleaved MAPKK1 (Fig. 2C).
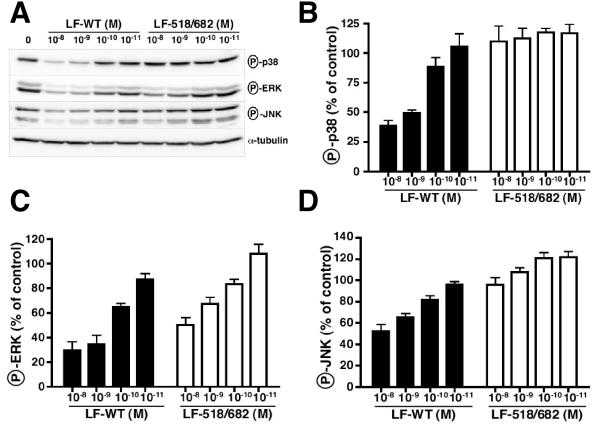
Since it is unclear whether cleavage of MAPKKs by LF causes pyroptosis of RAW 264.7 cells, we attempted to correlate cyotoxicity with downregulation of the MAPK pathways. RAW 264.7 cells were treated with PA and either wild-type LF or LF-K518E/E682G and then the cells were stimulated with lipopolysaccharide to activate the signaling pathways. Cellular lysates were prepared and probed for phosphorylated ERK, p38, and JNK by Western blotting (Fig. 3). Exposure of cells to PA and increasing concentrations of wild-type LF for 1 h resulted in decreased phosphorylation of the three MAPKs. Interestingly, increasing the LF concentration from 10−11 M to 10−10 M had a considerable effect on cell viability, but relatively minor effects on the phosphorylation of the MAPKs (compare Figs. 2A and 3). LF-K518E/E682G decreased phosphorylation of ERK almost as effectively as wild-type LF, but did not decrease phosphorylation of p38 or JNK below the level observed in cells treated with lipopolysaccharide alone. Thus, while wild-type LF interfered with signaling in all three MAPK pathways, LF-K518E/E682G selectively downregulated the ERK pathway.
Figure 3.
LF-K518E/E682G inhibits the phosphorylation of ERK, but not of p38 or JNK. RAW 264.7 cells were treated with 10−8 M PA and the indicated concentrations of either wild-type LF or LF-K518E/E682G for 1 h and then treated with lipopolysaccharide for 15 min. Cellular lysates were made and probed for phosphorylated MAPKs or α-tubulin control by Western blotting. Representative blots are shown in (A). Panels B-D show the results of quantifying the levels of phosphorylated proteins in toxin-treated cells compared to cells that were not treated with toxin. Values represent the mean ± standard error of the mean for three independent experiments.
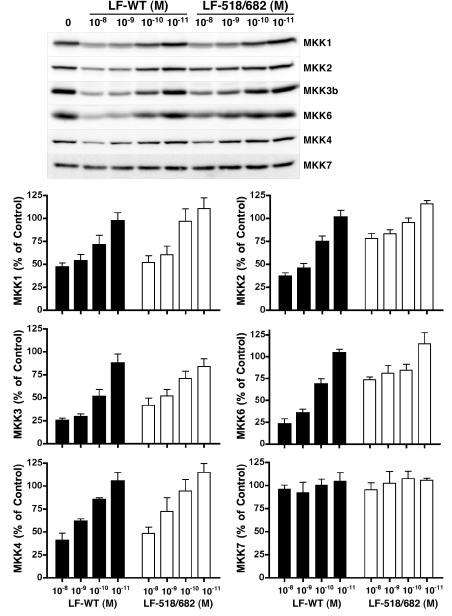
To examine why the mutant demonstrated increased specificity towards downregulating the ERK pathway, we next compared the abilities of wild-type LF and LF-K518E/E682G to cleave MAPKKs (Fig. 4). MAPKK1 and MAPKK2, which phosphorylate ERK, were both cleaved by wild-type LF as assessed by Western blotting. At the highest concentration of LF tested (10−8 M), ~50% of MAPKK1 and ~60% of MAPKK2 was cleaved after 1 h. Treatment of cells with PA and 10−8 M LF-K518E/E682G resulted in ~50% of MAPKK1 and ~20% of MAPKK2 being cleaved. Since the mutant was able to downregulate the ERK pathway almost as efficiently as wild-type LF, these results suggest that MAPKK1 is primarily responsible for ERK activation under these conditions.
Figure 4.
LF-K518E/E682G has a reduced ability to cleave some MAPKKs. RAW 264.7 cells were treated with 10−8 M PA and the indicated concentrations of either wild-type LF or LF-K518E/E682G for 1 h. Cellular lysates were prepared and probed for phosphorylated MAPKKs by Western blotting. The amount of full-length MAPKK remaining after 1 h was quantified. Values represent the mean ± standard error of the mean for three independent experiments.
We next sought to determine the cause of the mutant’s deficiency at downregulating p38 by examining the cleavage of MAPKK3 and MAPKK6. LF-K518E/E682G was modestly defective at cleaving MAPKK3 compared to wild-type LF, but was considerably more defective at cleaving MAPKK6. The inability of the mutant to prevent phosphorylation of p38 (Fig. 3) indicates that the level of MAPPK3/6 that remained in the cell was sufficient to support maximal p38 phosphorylation.
We next probed cellular lysates for MAPKK4 and MAPKK7, which phosphorylate JNK. LF-K518E/E682G cleaved similar amounts of MAPKK4 as did wild-type LF. Neither wild-type LF nor the mutant cleaved appreciable amounts of MAPKK7 after 1 h of toxin treatment. Thus, wild-type LF and LF-K518E/E682G exhibited similar activities towards MAPKK4 and 7, but only wild-type LF reduced the level of phosphorylation of JNK to ~50% as compared to the control. There is no evident explanation for these results; the difference in JNK phosphorylation observed might be due to an indirect effect of intoxication.
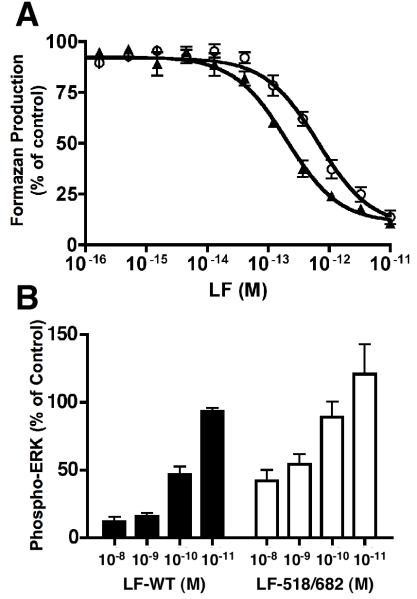
Since downregulation of the ERK pathway has been shown to be sufficient to cause apoptosis in MALME-3M cells [20], we next compared the activities of wild-type LF and LF-K518E/E682G in a cytotoxicity assay using this melanoma cell line. PA and either wild-type or mutant LF were incubated with MALME-3M cells for 72 h and viability was estimated using the MTS assay (Fig. 5A) [20]. The EC50 for wild-type LF was determined to be 2 × 10−13 M and the EC50 for LF-K518E/E682G was only ~3-fold higher at 7 × 10−13 M. These results indicate that LF-K518E/E682G is markedly more defective compared to wild-type LF at killing the murine macrophage cells than the melanoma cells. We next assessed the phosphorylation of ERK in MALME-3M cells treated with either wild-type or mutant LF and found that LF-K518E/E682G downregulated the ERK pathway almost as effectively as wild-type LF did (Fig. 5B). This is consistent with previous work that indicated the requirement of ERK signaling for survival of these cells and suggests that different types of cells are killed by LF as a result of the cleavage of distinct substrates.
Figure 5.
LF-K518E/E682G causes death of melanoma cells. (A) PA and various concentrations of wild-type LF (σ) or LF-K518E/E682G (○) were incubated with MALME-3M cells and viability was assessed after 72 h using the MTS assay. Values represent the mean ± standard error of the mean for three independent experiments. (B) MALME-3M cells were treated with 10−8 M PA and the indicated concentrations of either wild-type LF or LF-K518E/E682G for 2 h and then treated with 2.5 μg/mL anisomycin for 15 min. Cellular lysates were prepared and probed for phosphorylated MAPKs. Values indicate the level of phosphorylated MAPK in toxin-treated cells as a fraction of the level in cells that were not treated with toxin. The results shown represent the mean ± standard error of the mean for three independent experiments.
To summarize, we have isolated an LF mutant that is impaired in its ability to activate the Nlrp1b inflammasome, but remains able to cause apoptosis in a melanoma cell line. LF-K518E/E682G activity prevented phosphorylation of ERK, but did not prevent phosphorylation of JNK or p38. This observation serves to explain why the mutant retains its ability to kill the melanoma cells, as it has been shown previously that inhibition of the ERK pathway is sufficient to induce apoptosis. It is unclear why the mutant is defective at causing pyroptosis, but it is presumably because LF-K518E/E682G has a diminished capacity to cleave a substrate that is involved in the activation of Nlrp1b.
Materials and Methods
Reagents
Antibodies raised against the amino-terminus of MAPKK1 (catalog# 07-641) or full-length MAPKK6 (catalog# 07-417) were obtained from Upstate. Antibody raised against the amino-terminus of MAPKK2 (catalog# 610235) was obtained from BD Biosciences. Antibodies raised against the amino-termini of MAPKK3b (catalog# 9238), MAPKK4 (catalog# 9152), and MAPKK7 (catalog# 4172) were obtained from Cell Signaling Technologies. Antibodies that detect phospho-p38 (catalog# 9215) and phospho-ERK (catalog# 9101) were obtained from Cell Signaling Technologies; and anti-phospho-JNK was obtained from Biosource (catalog# 44-682). A control antibody, anti-α-tublin (T9026), was obtained from Sigma.
Tryptic Digestion of LF
Various amounts of trypsin were incubated with 2 μg of LF or LF-K518E/E682G for 1 h at 23°C in a total volume of 10 μL of 20 mM Tris-HCl pH 8.0, 150 mM NaCl. Digested proteins were subjected to SDS-PAGE and stained with Coomassie blue.
Cell lines
Murine macrophage RAW 264.7 cells (ATCC) were cultured in RPMI-1640 medium supplemented with 5% fetal bovine serum (HyClone) and 1% penicillin/streptomycin (Sigma) at 37°C in a humidified atmosphere of 5% CO2. MALME-3M cells (ATCC) were cultured in RPMI-1640 supplemented with 10% Nu-Serum (BD Biosciences) and 1% penicillin/streptomycin.
Protein purification
PA was purified from E. coli as described previously [25].
The plasmids pWH1520-LF-K518E/E682G and pWH1520-LF were transformed into B. megaterium protoplasts according to manufacturer’s instructions (MoBiTec). An overnight culture of B. megaterium expressing either wild-type LF or LF-K518E/E682G was used to inoculate 500 mL of TB containing 10 μg/ml tetracycline. The culture was grown at 37°C until an OD600~0.8 was reached. At this time, the expression of LF was induced into the supernatant by the addition of 20% xylose (Sigma) to a final concentration of 0.5%. The culture was grown for another 4 to 4.5 hours and then centrifuged at 7000 g for 30 min in a Sorvall Evolution RC centrifuge. The supernatant was decanted into 500 mL of autoclaved 40% PEG8000 (Sigma) and the resulting solution was rotated overnight at 4°C. The solution was centrifuged at 9500 g for 30 min and the supernatant was decanted. The pellet was resuspended in 10 mL of supernatant and then centrifuged at 20 000 g for 30 min. The supernatant was decanted and 10 mL of 20 mM Tris-HCl pH 8.0 was used to dissolve the pellet. The sample was then centrifuged at 20 000 g for 10 min to remove undissolved material. The resulting supernatant was filtered using a 0.2 μm syringe filter (Pall Sciences) and loaded onto a column containing ~1 mL of Q-sepharose (Amersham Pharmacia Biotech). The column was washed first with 10 mL of 20 mM Tris-HCl pH 8.0 and then with 20 mM Tris-HCl pH 8.0, 0.15 M NaCl. LF was eluted in 20 mM Tris-HCl pH 8.0, 0.25 M NaCl.
Cytotoxicity Assays
For the MTS assay, RAW 264.7 cells were seeded in 96-well plates at a density of 1 × 105 cells/100 μl of media for 24 h and MALME-3M cells were seeded in 96-well plates at a density of 3 × 104 cells/100 μl of media for 24 h. Cells were washed once with PBS and then incubated in medium with 1 × 10−8 M PA and various concentrations of LF. Viability of RAW 264.7 cells was assessed after 4 h and 24 h and MALME-3M cells after 72 h using the MTS assay according to the manufacturer’s instructions (Promega). The EC50 values were determined using the graphical program GraphPad Prism 4.
For the trypan blue exclusion assay, 3 × 106 RAW 264.7 cells/well were seeded in 6-well plates. Cells were washed once with PBS and then incubated in medium with 1 × 10−8 M PA and 1 × 10−8 M LF for 4 h or 24 h. The cells were resuspended in medium, stained with trypan blue, and counted using a haemocytometer.
Nlrp1b reconstitution assay
The Nlrp1b reconstitution assay was performed as described previously [24]. Briefly, HT1080 cells were transfected with 1μg each of pNTAP-Nlrp1b, pcDNA3-pro-caspase-1-T7, and pcDNA3-pro-IL-1β-HA using 9 μL of 1 mg/mL polyethyleneimine pH 7.2. Cells were treated with 10−8 M LF and 10−8 M PA for 3 h. The culture supernatant was incubated overnight with 1 μL of α-HA antibody (Sigma-Aldrich H9658), followed by a 2 h incubation with 100 μL of protein A sepharose (GE Healthcare). Proteins were eluted with SDS loading dye and subjected to immunoblotting using a polyclonal HA antibody (Santa Cruz sc805).
Cell pellets were harvested and then lysed with 300 μL of EBC buffer (0.5% NP-40, 20 mM Tris pH 8, 150 mM NaCl, 1 mM PMSF) for 60 min. Equivalent amounts of cell lysate protein (~ 30 μg) were subjected to SDS-PAGE and immunoblotted with α-HA (Santa Cruz sc805) and α-β-actin (Sigma-Aldrich A5441) antibodies.
Western blot experiments
RAW 264.7 cells were seeded into 6-well plates at 106 cells/well. Following overnight incubation, cells were treated for 1 h with media alone, or with 1 × 10−8 M PA and indicated concentrations of either LF-WT or LF-K518E/E682G. LPS (100 ng/mL) was added to all wells for 15 min. Cells were harvested in 500 μL of 1X Cell Lysis Buffer (Cell Signaling Technologies) containing 1 mM phenylmethylsulfonyl fluoride (Sigma) and sonicated four times for a total of 40 s using the Sonic Dismembrator Model 100 (Fisher Scientific). Cell lysates were then clarified by microcentrifugation at 13 000 rpm (Eppendorf Centrifuge 5415D) for 10 min at 4°C. Equal amounts of lysate were electrophoresed on 10% SDS-polyacrylamide gels. Proteins were transferred to nitrocellulose (Pall Life Science) using a Mini Trans-Blot Electrophoretic Transfer Cell (Bio-Rad). Blots were blocked in 0.1% Tween-20 TBS (100 mM Tris-HCl pH 8.0, 0.9% NaCl) containing 5% powdered skim milk for 1 h. Blots were incubated with primary antibodies diluted according to manufacturer’s instructions. Blots were then rinsed three times in 0.05% Tween-20 TBS and incubated with either Peroxidase-conjugated goat anti-rabbit or goat anti-mouse IgG secondary antibodies (Pierce) in 0.1% Tween-20 TBS containing 5% powdered skim milk. Blots were incubated with SuperSignal West Dura Extended Duration Substrate (Pierce) for 5 min and then visualized using a Kodak Gel-Image Station 2000R.
Acknowledgements
This research was supported by NIH grant RO1 AI067683. J.M. holds the Canada Research Chair in Bacterial Pathogenesis.
References
- 1.Abrami L, Reig N, van der Goot FG. Anthrax toxin: the long and winding road that leads to the kill. Trends Microbiol. 2005;13:72–78. doi: 10.1016/j.tim.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Young JA, Collier RJ. Anthrax toxin: receptor binding, internalization, pore formation, and translocation. Annu Rev Biochem. 2007;76:243–265. doi: 10.1146/annurev.biochem.75.103004.142728. [DOI] [PubMed] [Google Scholar]
- 3.Warfel JM, Steele AD, D’Agnillo F. Anthrax lethal toxin induces endothelial barrier dysfunction. Am J Pathol. 2005;166:1871–1881. doi: 10.1016/S0002-9440(10)62496-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gozes Y, Moayeri M, Wiggins JF, Leppla SH. Anthrax lethal toxin induces ketotifen-sensitive intradermal vascular leakage in certain inbred mice. Infect Immun. 2006;74:1266–1272. doi: 10.1128/IAI.74.2.1266-1272.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moayeri M, Haines D, Young HA, Leppla SH. Bacillus anthracis lethal toxin induces TNF-alpha-independent hypoxia-mediated toxicity in mice. J Clin Invest. 2003;112:670–682. doi: 10.1172/JCI17991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cui X, Moayeri M, Li Y, Li X, Haley M, Fitz Y, Correa-Araujo R, Banks SM, Leppla SH, Eichacker PQ. Lethality during continuous anthrax lethal toxin infusion is associated with circulatory shock but not inflammatory cytokine or nitric oxide release in rats. Am J Physiol Regul Integr Comp Physiol. 2004;286:R699–709. doi: 10.1152/ajpregu.00593.2003. [DOI] [PubMed] [Google Scholar]
- 7.Baldari CT, Tonello F, Paccani SR, Montecucco C. Anthrax toxins: A paradigm of bacterial immune suppression. Trends Immunol. 2006;27:434–440. doi: 10.1016/j.it.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Banks DJ, Ward SC, Bradley KA. New insights into the functions of anthrax toxin. Expert Rev Mol Med. 2006;8:1–18. doi: 10.1017/S1462399406010714. [DOI] [PubMed] [Google Scholar]
- 9.Tournier JN, Rossi Paccani S, Quesnel-Hellmann A, Baldari CT. Anthrax toxins: A weapon to systematically dismantle the host immune defenses. Mol Aspects Med. 2009 doi: 10.1016/j.mam.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Duesbery NS, Webb CP, Leppla SH, Gordon VM, Klimpel KR, Copeland TD, Ahn NG, Oskarsson MK, Fukasawa K, Paull KD, et al. Proteolytic inactivation of MAP-kinase-kinase by anthrax lethal factor. Science. 1998;280:734–737. doi: 10.1126/science.280.5364.734. [DOI] [PubMed] [Google Scholar]
- 11.Vitale G, Bernardi L, Napolitani G, Mock M, Montecucco C. Susceptibility of mitogen-activated protein kinase kinase family members to proteolysis by anthrax lethal factor. Biochem J. 2000;352(Pt 3):739–745. [PMC free article] [PubMed] [Google Scholar]
- 12.Abi-Habib RJ, Urieto JO, Liu S, Leppla SH, Duesbery NS, Frankel AE. BRAF status and mitogen-activated protein/extracellular signal-regulated kinase kinase 1/2 activity indicate sensitivity of melanoma cells to anthrax lethal toxin. Mol Cancer Ther. 2005;4:1303–1310. doi: 10.1158/1535-7163.MCT-05-0145. [DOI] [PubMed] [Google Scholar]
- 13.Maldonado-Arocho FJ, Fulcher JA, Lee B, Bradley KA. Anthrax oedema toxin induces anthrax toxin receptor expression in monocyte-derived cells. Mol Microbiol. 2006;61:324–337. doi: 10.1111/j.1365-2958.2006.05232.x. [DOI] [PubMed] [Google Scholar]
- 14.Boyden ED, Dietrich WF. Nalp1b controls mouse macrophage susceptibility to anthrax lethal toxin. Nat Genet. 2006;38:240–244. doi: 10.1038/ng1724. [DOI] [PubMed] [Google Scholar]
- 15.Fink SL, Bergsbaken T, Cookson BT. Anthrax lethal toxin and Salmonella elicit the common cell death pathway of caspase-1-dependent pyroptosis via distinct mechanisms. Proc Natl Acad Sci U S A. 2008;105:4312–4317. doi: 10.1073/pnas.0707370105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wickliffe KE, Leppla SH, Moayeri M. Anthrax lethal toxin-induced inflammasome formation and caspase-1 activation are late events dependent on ion fluxes and the proteasome. Cell Microbiol. 2008;10:332–343. doi: 10.1111/j.1462-5822.2007.01044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nour AM, Yeung YG, Santambrogio L, Boyden ED, Stanley ER, Brojatsch J. Anthrax lethal toxin triggers the formation of a membrane-associated inflammasome complex in murine macrophages. Infect Immun. 2009;77:1262–1271. doi: 10.1128/IAI.01032-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park JM, Greten FR, Li ZW, Karin M. Macrophage apoptosis by anthrax lethal factor through p38 MAP kinase inhibition. Science. 2002;297:2048–2051. doi: 10.1126/science.1073163. [DOI] [PubMed] [Google Scholar]
- 19.Kim SO, Jing Q, Hoebe K, Beutler B, Duesbery NS, Han J. Sensitizing anthrax lethal toxin-resistant macrophages to lethal toxin-induced killing by tumor necrosis factor-alpha. J Biol Chem. 2003;278:7413–7421. doi: 10.1074/jbc.M209279200. [DOI] [PubMed] [Google Scholar]
- 20.Koo HM, VanBrocklin M, McWilliams MJ, Leppla SH, Duesbery NS, Woude GF. Apoptosis and melanogenesis in human melanoma cells induced by anthrax lethal factor inactivation of mitogen-activated protein kinase kinase. Proc Natl Acad Sci U S A. 2002;99:3052–3057. doi: 10.1073/pnas.052707699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frankel AE, Koo HM, Leppla SH, Duesbery NS, Vande Woude GF. Novel protein targeted therapy of metastatic melanoma. Curr Pharm Des. 2003;9:2060–2066. doi: 10.2174/1381612033454162. [DOI] [PubMed] [Google Scholar]
- 22.Liang X, Young JJ, Boone SA, Waugh DS, Duesbery NS. Involvement of domain II in toxicity of anthrax lethal factor. J Biol Chem. 2004;279:52473–52478. doi: 10.1074/jbc.M409105200. [DOI] [PubMed] [Google Scholar]
- 23.Turk BE, Wong TY, Schwarzenbacher R, Jarrell ET, Leppla SH, Collier RJ, Liddington RC, Cantley LC. The structural basis for substrate and inhibitor selectivity of the anthrax lethal factor. Nat Struct Mol Biol. 2004;11:60–66. doi: 10.1038/nsmb708. [DOI] [PubMed] [Google Scholar]
- 24.Liao KC, Mogridge J. Expression of Nlrp1b inflammasome components in human fibroblasts confers susceptibility to anthrax lethal toxin. Infect Immun. 2009;77:4455–4462. doi: 10.1128/IAI.00276-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller CJ, Elliott JL, Collier RJ. Anthrax protective antigen: prepore-to-pore conversion. Biochemistry. 1999;38:10432–10441. doi: 10.1021/bi990792d. [DOI] [PubMed] [Google Scholar]
- 26.Humphrey W, Dalke A, Schulten K. VMD: visual molecular dynamics. J Mol Graph. 1996;14:33–38. 27–38. doi: 10.1016/0263-7855(96)00018-5. [DOI] [PubMed] [Google Scholar]