Abstract
The US Centers for Disease Control and Prevention established the Environmental Public Health Tracking (EPHT) program to support state and local projects that characterize the impact of the environment on health. The projects involve compiling, linking, analyzing, and disseminating environmental and health surveillance information, thereby engaging stakeholders and guiding actions to improve public health. One of the EPHT objectives is to track the public health impact of ambient air pollution with analyses that are timely and relevant to state and local stakeholders. To address methodological issues relevant to this objective, in January 2008, government officials and researchers from the USA, Canada, and Europe gathered in Baltimore, Maryland for a 2-day workshop. Using commissioned papers and presentations on key methodological issues as well as examples of previous air pollution impact assessments, work group discussions produced a set of consensus recommendations for the EPHT program. These recommendations noted the need for data that will encourage local stakeholders to support continued progress in air pollution control. The limitations of using only local data for analyses were also noted. To improve local estimates of air pollution health impacts, methods were recommended that “borrow strength” from other evidence. An incremental approach to implementing such methods was recommended. The importance and difficulty of communicating uncertainties in local health impact assessments was emphasized, as was the need for coordination among different agencies conducting health impact assessments.
Keywords: Environmental exposure, Population surveillance, Public health, Air pollution
Introduction
The mission of Centers for Disease Control and Prevention (CDC)’s Environmental Public Health Tracking (EPHT) program is “…to provide information from a nationwide network of integrated health and environmental data that drives actions to improve the health of communities,…” (CDC 2006). Consistent with this mission, a key objective of the EPHT program is tracking the public health burden of ambient air pollution with analyses that are timely and relevant to local stakeholders. To address methodological issues relevant to this objective, in January 2008 a 2-day workshop in Baltimore, Maryland, jointly organized and sponsored by Health Effects Institute, CDC, and US EPA, brought together representatives of state and national public health and environmental agencies and academic researchers from the USA, Canada, and Europe. Among the workshop participants were persons with expertise and experience in the development and application of statistical and epidemiologic tools for air pollution health impact assessment in both academic and policy settings in North America and in Europe (see Appendix 1).
Workshop participants were charged with producing recommendations for use at the state and local levels for communicating the results of the analyses to stakeholders. These recommendations would suggest ways to analyze linked air quality and health data and to estimate and track over time health impact indicators for two pollutants: fine particulate matter (PM2.5) and ozone.
Specifically, the participants were asked to recommend:
Approaches for using analyses of state data to generate state and sub-state impact estimates for acute effects of air pollution;
Approaches for using current quantitative estimates—and to develop further estimates—of the relationship between air pollution exposure and health outcomes from the scientific literature, as well as ways to generate estimates of acute and chronic health impacts in local areas; and
Approaches for communicating to stakeholders the estimates and the limitations of those estimates.
In working papers commissioned before the workshop (Bachmann 2008; Fuentes 2009; Hubbell et al. 2009; Medina et al. 2009; Shin et al. 2009; Talbot et al. 2009; Wartenberg 2009; White 2009) and in workshop presentations, relevant work of the EPHT program was reviewed, previous health impact assessments were described, and methodological topics were discussed. The workshop participants then discussed key methodological issues and made recommendations regarding further development and application of indicators of the health effects of air pollution—specifically, indicators that would be suitable for public health tracking of air pollution impacts at the state and local level.
This paper summarizes the workshop discussions and recommendations for developing ongoing and consistent implementation of air pollution health impact assessments by state and local agencies.
The need for timely and locally relevant information on the health effects related to air pollution
Over the past 50 years, the USA has made considerable progress in reducing levels of health-damaging ambient air pollution, progress that has resulted in substantial public health benefits (US EPA 1997, 1999). Nevertheless, in some areas of the country, PM2.5 and ozone levels currently exceed National Ambient Air Quality Standards (US EPA 2008). In terms of increased mortality and morbidity, especially cardiovascular and respiratory disease, exposure to air pollution continues to affect the health of the US population (US EPA 2004a, b, 2005a, b, 2006, 2007).
While air quality improvements are projected to continue, increasing urban sprawl, traffic volume, and congestion may be slowing progress and threatening future gains, especially in some regions (Frumkin et al. 2004). At the same time, growing evidence points to the importance of health impacts associated with intra-urban gradients in ambient air pollution, particularly those related to traffic (Miller et al. 2007; Jerrett et al. 2005). Thus, future advances in public health protection will likely require improved understanding of those local pollution sources and potential control measures that impinge on state and local land use and transportation policy. The more such measures affect local stakeholders, the greater the need for local engagement in the process. Providing local stakeholders timely, understandable and locally relevant data on air pollution health impacts will be a necessary part of such engagement.
Environmental public health tracking has been defined as the “ongoing collection, integration, analysis and dissemination of data from environmental hazard monitoring, human exposure tracking, and health effects surveillance” (Meyer et al. 2006; Environmental Health Tracking Project Team 2000). Consistent with CDC’s model of public health surveillance, the communication of findings to those with a “need to know” (Thacker and Berkelman 1988) is a key component. The tracking model broadly defines stakeholders who are targets of dissemination efforts to include policy makers, government and nongovernmental agencies, businesses, researchers, the media, and members of the public. Because the health effects of PM2.5 and ozone are well established, the EPHT program identifies ambient air pollution as a priority for tracking indicators of exposure and for health impact assessment. As a result of a collaboration between CDC, US EPA, and state EPHT programs, an infrastructure within the Environmental Public Health Tracking Network (EPHTN) is under development (Talbot et al. 2009; Boothe et al. 2005). This infrastructure will enable ongoing, periodic, and timely analyses of the health impacts of air pollution at the state and local levels and will address such questions as:
What is the public health burden attributable to ambient PM2.5 and ozone levels?
How does the burden vary within and between states?
Is the burden changing over time, for example, in response to efforts to reduce air pollution levels and population exposure?
Methodological challenges
Estimating the health impacts of air pollutants is more complex than estimating some health impacts of certain environmental exposures. For example, acute carbon monoxide poisonings (which generally result from indoor, not ambient, exposures) can be diagnosed with specificity when compatible signs and symptoms occur in the presence of an elevated level of carboxyhemoglobin. The number and rate of such events can be tracked using hospital inpatient and emergency department administrative data. For the EPA’s criteria air pollutants, generally, there is, unfortunately, no similarly straightforward way to track public health impacts. The most serious known health effects of exposure to air pollutants such as PM2.5 and ozone, both indicators of complex mixtures with no well-accepted or easily measured specific biomarkers, involve morbidity and mortality from diseases of the cardiovascular and respiratory systems that have multiple other complex causes. Therefore, although the contribution of the diseases themselves to the overall burden of disease in a population can be estimated categorically by identifying individuals who meet pre-specified clinical criteria, the burden attributable to PM2.5 or ozone cannot be unambiguously identified and can only be estimated from statistical models.
While an extensive body of research has established causal links between exposure to these pollutants and human health, concentration–response (CR) relationships quantifying these links have, for a variety of reasons, been shown to vary among geographic areas and over time (Samet et al. 2000; Samet 2008; Katsouyanni et al. 2001; Hubbell et al. 2009). PM2.5 and ozone may serve in part as indicators of complex pollutant mixtures (White 2009), and variation in composition by space and time may alter the concentration/health impact relationship. Additional modifying factors include population susceptibility and local health care utilization, services, and recording practices. In addition to these relatively stable local differences, exceptional local weather events or emission sources, including forest or structural fires or construction demolition, may introduce within a local area different pollutant species or extreme pollutant levels. In addition, local interventions, including enhanced air quality alerts, land use and transportation changes, and control of local point sources may alter local air quality and affect human exposure and its relationship to health.
Although estimates from purely local analyses should in theory best reflect local modifiers of a CR function, “true” CR relationships at prevalent ambient air pollution levels are small relative to random error and potential bias affecting a single local study. Thus, estimates based on local data only may not accurately reflect the underlying CR relationship and may even give indications of either anomalous “protective” effects or implausibly large effect risk estimates. The methodological challenges stemming from use of local data are even greater for estimating time trends at the state and sub-state levels for air pollution’s impact on health.
Communicating with stakeholders in a meaningful and complete way concerning the information gained from the EPHT analysis poses additional challenges, especially when attempting to set out clearly any uncertainties and their implications (IPCC 2005).
Previous health impact assessments of air pollution conducted in Europe, the USA, and Canada have grappled with these issues (Cohen et al. 2004; Le Tertre et al., 2005; USEPA 2005b; Burnett et al. 2005; Medina et al. 2009). Considering the lessons learned from these efforts, other relevant methodological work, and the context of EPHT programs based in state and local health departments, workshop participants developed the conclusions and recommendations summarized below. A full version of the workshop report and recommendations is available at http://www.cdc.gov/nceh/tracking/default.htm.
Major workshop conclusions and recommendations
Future progress in public health protection will likely require improved understanding of local air pollution sources and control measures that require the engagement of local stakeholders. By providing timely and locally relevant data on air pollution health impacts, the EPHTN can become a motivating factor in such engagement while making an important contribution to public health protection.
Analyses of PM2.5 and ozone health impacts that use only air pollution and health data from a single geographic area are unlikely to provide robust estimates of the relation between air pollution and acute and chronic health effects, although such analyses may be appropriate for other research or for surveillance applications (Talbot et al. 2009). Therefore, when making such estimates, various methods of “borrowing strength” from other evidence are essential, especially when quantifying local public health impacts (Fuentes 2009).
The EPHT program should incrementally develop tracking of air quality health impacts (Fig. 1).
An initial goal should be the development, testing, and application of a methodology for local health impact assessment at selected locations and that methodology should use quantitative estimates of the concentration–response relationships between air pollution exposure and health outcomes from the scientific literature (Hubbell et al. 2009). Clear operational guidance for applying the method and communicating results should be provided.
In the longer term, a network of EPHT programs should develop analyses that draw strength from pooled evidence across locations to produce cross-sectional estimates of local CR functions (Fuentes 2009). Once established, this type of network would enable longitudinal analyses that track impact over time, which may identify changes in CR functions attributable, for example, to changes in PM2.5 composition. Such analyses could support “accountability” measures (Shin et al. 2009; HEI Accountability Working Group 2003) of the effectiveness of local, regional, and national air quality management initiatives.
Developing local CR function estimates that describe, at the state and sub-state levels, the relationship between air pollution exposure and health will initially require considerably more methodological groundwork, as discussed by Fuentes (2009), than will health impact assessments using published CR function estimates. In addition, this approach requires a process that ensures standard methods for data preparation and analysis across states while addressing the confidentiality requirements of data stewards in each state.
The EPHT should review the current experience with regard to choice of air pollution health impact metrics (e.g., counts of attributable deaths and other adverse health outcomes vs. attributable impact on life expectancy or healthy life expectancy) and the way in which they are communicated, with the goals of (1) achieving consensus on the best approaches for the EPHTN and (2) identifying critical knowledge gaps that could be addressed with additional research or methods development. Currently, the scientific community has yet to resolve which metric(s) best quantify the impacts of air pollution and which are most meaningful to diverse stakeholders, including the public (McMichael et al. 1998; Rabl 2005; Brunekreef et al. 2007; Wartenberg 2009).
A critical but challenging goal for EPHTN will be to provide a complete and straightforward account of the uncertainties in local air pollution health impact estimates. The CDC Environmental Public Health Tracking Program should review the current experience with regard to efforts to communicate uncertainty in estimates of health effects and health impact assessments of environmental hazards (e.g., IPCC 2005), with the goals of (1) achieving consensus on the best approaches for the EPHTN; (2) identifying critical knowledge gaps that could be addressed with additional research; and (3) supporting the overall transparency and credibility of the tracking network’s results.
Communication among different agencies conducting health impact assessments is also needed. Currently, in the USA, health impact assessments of exposure to air pollution are carried out by agencies at different levels, including US EPA, states, and municipalities. The tracking program should work with involved agencies to avoid, if possible, methodologic inconsistencies that could produce artifactual differences in impact estimates. A well-developed communication strategy regarding health effects and impacts of air pollution, coordinated with other relevant agencies such as US EPA, should be an integral part of the EPHT.
Fig. 1.
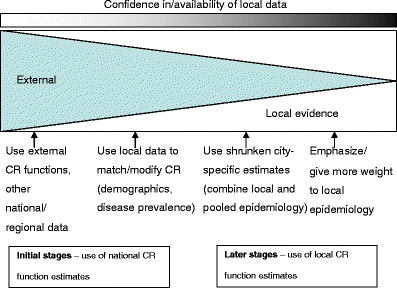
Conceptual model for staged development of air pollution health impact assessment for environmental public health tracking
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Appendix 1
Workshop participants
Workshop on Methodologies for Environmental Public Health Tracking of Air Pollution Effects
January 15–16, 2008
Admiral Fell Inn
Baltimore, Maryland
Participant list
Robert Altenburg
Pennsylvania Department of Environmental Protection
Policy Office
Harrisburg, PA
H Ross Anderson
Professor of Epidemiology and Public Health
Community Health Sciences
St. George’s University of London
London, UK
Steve Anderson
Research Scientist
New Jersey Department of Environmental Protection
Trenton, NJ
John Bachmann (Work group chair)
Principal
Vision Air Consulting, LLC
Chapel Hill, NC
John Balmes (Work group chair)
Professor
University of California, Berkeley
and University of California, San Francisco
San Francisco, CA
Richard Burnett
Senior Research Scientist
Environmental Health Directorate Health Canada
Ottawa, Canada
Aaron Cohen (Steering committee member)
Principal Scientist
Health Effects Institute
Boston, MA
Fred Dimmick (Steering committee member)
Branch Chief
US Environmental Protection Agency
National Exposure Research Laboratory
Research Triangle Park, NC
Francesca Dominici
Professor
Department of Biostatistics
Johns Hopkins Bloomberg School of Public Health
Baltimore, MD
Jerald Fagliano
Program Manager
New Jersey Department of Health and Senior Services
Trenton, NJ
Faye Floyd
Public Health Advisor/Project Officer
US Centers for Disease Control and Prevention
National Center for Environmental Health
Environmental Health Tracking Branch
Atlanta, GA
Montserrat Fuentes
Associate Professor
Department of Statistics
North Carolina State University
Raleigh, NC
Paul Garbe
Branch Chief, Air Pollution and Respiratory Health
Centers for Disease Control and Prevention
National Center for Environmental Health
Atlanta, GA
Valerie Haley
Research Scientist
New York State Department of Health
Troy, NY
Lisa Hines
Senior Health Communications Specialist
Environmental Health Tracking Branch
Centers for Disease Control and Prevention
Atlanta, GA
Bryan Hubbell
Senior Advisor for Science and Policy Analysis
Health and Environmental Impacts Division
US Environmental Protection Agency
Research Triangle Park, NC
Nicholas Jones (Steering committee member; Work group rapporteur)
Team Lead Scientific Development
Environmental Health Tracking Branch
US Centers for Disease Control and Prevention
Atlanta, GA
Michal Krzyzanowski
Regional Advisor
World Health Organization
Bonn, Germany
Thomas Lambert
Environmental Health Data Analyst
New Hampshire Department of Health and Human Services
Concord, NH
Sam LeFevre
Program Manager
Environmental Epidemiology Program, Utah Department of Health
Salt Lake City, UT
Jonathan Levy
Associate Professor of Environmental Health and Risk Assessment
Harvard School of Public Health Department of Environmental Health
Boston, MA
Thomas Louis (Work group chair)
Professor
Department of Biostatistics
Johns Hopkins Bloomberg School of Public Health
Baltimore, MD
Helene Margolis
Epidemiologist
California Department of Public Health
Sacramento, CA
Thomas Matte (Steering committee member)
Medical Epidemiologist
US Centers for Disease Control and Prevention
Sylvia Medina
Coordinator of European Projects
Institut de Veille Sanitaire (InVS) Department of Environmental Health
Saint Maurice, France
Orrin Myers
Department of Internal Medicine
University of New Mexico
Albuquerque, NM
Clifford S. Mitchell
Director of Environmental Health Coordination Program
Maryland Department of Health and Mental Hygiene
Baltimore, MD
Lucas Neas
Acting Chief, Epidemiology and Biomarkers Branch
US Environmental Protection Agency
Chapel Hill, NC
Robert O’Keefe
Vice President
Health Effects Institute
Boston, MA
Chris Paulu
Epidemiologist
State of Maine
Augusta, ME
Judy Rager
Research Specialist
University of Pittsburgh
Graduate School of Public Health
Pittsburgh, PA
Eric Roberts
Director Health Surveillance
California Environmental Health Tracking Program
Richmond, CA
Margaret Round
Environmental Analyst
Massachusetts Department of Public Health
Bureau of Environmental Health
Boston, MA
Jonathan Samet (Steering committee member; Steering committee chair)
Professor and Chair
Department of Epidemiology
Johns Hopkins Bloomberg School of Public Health
Baltimore, MD
Jeremy Sarnat (Steering committee member; Work group rapporteur)
Assistant Professor of Environmental and Occupational Health
Emory University School of Public Health
and US Centers for Disease Control and Prevention
Atlanta GA
Susan Stone
Environmental Health Scientist
US Environmental Protection Agency
Research Triangle Park, NC
Thomas Talbot
Chief
Environmental Health Surveillance Section
New York State Department of Health
Troy, NY
Evelyn Talbott
Professor
University of Pittsburgh
Graduate School of Public Health Department of Epidemiology
Pittsburgh, PA
Annemoon van Erp
Senior Scientist
Health Effects Institute
Boston, MA
Daniel Wartenberg
Professor
Department of Environmental and Occupational Medicine
University of Medicine and Dentistry of New Jersey
Piscataway, NJ
Warren White
Atmospheric Mathematician
Crocker Nuclear Laboratory
University of California
Davis, CA
Fuyuen Yip (Steering committee member; Work group rapporteur)
Epidemiologist
Centers for Disease Control and Prevention
National Center for Environmental Health Air Pollution and Respiratory Health Branch
Atlanta, GA
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect the views of the Health Effects Institute (HEI) or its sponsors.
References
- Bachmann J. Air pollution forecasts and results-oriented tracking. Air Qual Atmos Health. 2008;1(4):203–207. doi: 10.1007/s11869-008-0025-8. [DOI] [Google Scholar]
- Boothe V, Dimmick WF, Talbot TO (2005) Relating air quality and environmental public health tracking data. In: Aral MM, Sinks T (Eds) Environmental exposure and health. Ecol Environ 85:43–52
- Brunekreef B, Miller BG, Hurley JF. The brave new world of lives sacrificed and saved, deaths attributed and avoided. Epidemiol. 2007;18:785–788. doi: 10.1097/EDE.0b013e3181570d88. [DOI] [PubMed] [Google Scholar]
- Burnett RT, Bartlett S, Jessiman B, et al. Measuring progress in the management of ambient air quality: the case for population health. J Toxicol Environ Health, Part A. 2005;68:1289–1300. doi: 10.1080/15287390590936157. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2006) CDC’s National Environmental Public Health Tracking Program: National Network Implementation Plan (NNIP). Available at: http://www.cdc.gov/nceh/tracking/pdfs/nnip.pdf
- Cohen AJ, Anderson HR, Ostro B, Pandey KD, Krzyzanowski M, Kuenzli N, Gutschmidt K, Pope CA, Romieu I, Samet JM, Smith KR. Mortality impacts of urban air pollution. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, editors. Comparative quantification of health risks: global and regional burden of disease due to selected major risk factors, vol 2. Geneva: World Health Organization; 2004. [Google Scholar]
- Environmental Health Tracking Project Team (2000) America’s environmental health gap: why the country needs a nationwide health tracking network. http://healthyamericans.org/reports/files/healthgap.pdf
- Frumkin H, Frank L, Jackson R. Urban sprawl and public health. Washington: Island Press; 2004. [Google Scholar]
- Fuentes M. Statistical issues in health impact assessment at the state and local levels. Air Qual Atmos Health. 2009;2(1):47–55. doi: 10.1007/s11869-009-0033-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HEI Accountability Working Group . Assessing health impact of air quality regulations: concepts and methods for accountability research. communication 11. Boston: Health Effects Institute; 2003. [Google Scholar]
- Hubbell B, Fann N, Levy JI. Methodological considerations in developing local scale health impact assessments: balancing national, regional, and local data. Air Qual Atmos Health. 2009;2(2):99–110. doi: 10.1007/s11869-009-0037-z. [DOI] [Google Scholar]
- Intergovernmental Panel on Climate Change (2005) Guidance notes for lead authors of the IPCC Fourth Assessment Report on Addressing Uncertainties. Available at: http://www.ipcc.ch/pdf/assessment-report/ar4/wg1/ar4-uncertaintyguidancenote.pdf. Accessed 4/1/08
- Jerrett M, Burnett RT, Ma R, Pope CA, 3rd, Krewski D, Newbold KB, Thurston G, Shi Y, Finkelstein N, Calle EE, Thun MJ. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology. 2005;16(6):727–736. doi: 10.1097/01.ede.0000181630.15826.7d. [DOI] [PubMed] [Google Scholar]
- Katsouyanni K, Touloumi G, Samoli E, et al. Confounding and effect modification in the short-term effects of ambient particles on total mortality: results from 29 European cities within the APHEA2 project. Epidemiol. 2001;12(5):521–531. doi: 10.1097/00001648-200109000-00011. [DOI] [PubMed] [Google Scholar]
- Le Tertre A, Schwartz J, Touloumi G. Empirical Bayes and adjusted estimates approach to estimating the relation of mortality to exposure to PM10. Risk Anal. 2005;25:711–718. doi: 10.1111/j.1539-6924.2005.00606.x. [DOI] [PubMed] [Google Scholar]
- McMichael AJ, Anderson HR, Brunekreef B, Cohen AJ. Inappropriate use of daily mortality analyses to estimate longer-term mortality effects of air pollution. Int J Epidemiol. 1998;27:450–453. doi: 10.1093/ije/27.3.450. [DOI] [PubMed] [Google Scholar]
- Medina S, Le Tertre A, Sklad M (2009) The APHEIS Project: air pollution and health—a European information system. Air Qual Atmos Health 2(4) (this issue). doi:10.1007/s11869-009-0050-2 [DOI] [PMC free article] [PubMed]
- Meyer P, Watkins T, Qualters J. Establishing a national environmental public health tracking network. Pittsburgh: Air and Waste Management Association; 2006. pp. 22–24. [Google Scholar]
- Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356(5):447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- Rabl A. Air pollution mortality: harvesting and loss of life expectancy. J Toxicol Environ Health Part A. 2005;68:1175–1180. doi: 10.1080/15287390590936049. [DOI] [PubMed] [Google Scholar]
- Samet JM, Zeger SL, Dominici F, Curriero F, Corsac I, Dockery DM, Schwartz J, Zanobetti A. The national morbidity, mortality, and air pollution study, part II: morbidity and mortality from air pollution in the United States. Research Report 94. Cambridge: Health Effects Institute; 2000. [PubMed] [Google Scholar]
- Samet JM. (2008) Air pollution risk estimates: determinants of heterogeneity. J Toxicol Environ Health A. 2008;71:578–582. doi: 10.1080/15287390801997666. [DOI] [PubMed] [Google Scholar]
- Shin HH, Stieb DM, Jessiman B, Goldberg MS, Brion O, Brook J, Ramsay T, Burnett RT. Measuring public health accountability of air quality management. Air Qual Atmos Health. 2009;2(1):11–20. doi: 10.1007/s11869-009-0029-z. [DOI] [Google Scholar]
- Talbot TO, Strand M, Vedal S, Rodes C, Dutton SJ, Gelfand EW, Rabinovitch N, Haley VB, Dimmick WF, Paulu C, Talbott EO, Rager E (2009) Developing consistent data and methods to measure the public health impacts of ambient air quality for environmental public health tracking: progress to date and future directions. Air Qual Atmos Health 2(4) (this issue). doi:10.1007/s11869-009-0043-1 [DOI] [PMC free article] [PubMed]
- Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Rev. 1988;10:164–190. doi: 10.1093/oxfordjournals.epirev.a036021. [DOI] [PubMed] [Google Scholar]
- US Environmental Protection Agency . The benefits and costs of the Clean Air Act: 1970 to 1990. Washington: Office of Air and Radiation/Office of Policy; 1997. [Google Scholar]
- US Environmental Protection Agency . The benefits and costs of the Clean Air Act: 1990 to 2010. Washington: Office of Air and Radiation/Office of Policy; 1999. [Google Scholar]
- US Environmental Protection Agency (2004a) Air quality criteria for particulate matter (October 2004). Washington, DC, EPA 600/P-99/002aF-bF
- US Environmental Protection Agency (2004b) Final regulatory analysis: control of emissions from nonroad diesel engines. EPA420-R-04-007. Prepared by the Office of Air and Radiation. Available at: http://www.epa.gov/nonroad-diesel/2004fr/420r04007.pdf
- US Environmental Protection Agency (2005a) Regulatory impact analysis for the clean air interstate rule. EPA 452/-03-001. Prepared by the Office of Air and Radiation. Available at: http://www.epa.gov/cair/pdfs/finaltech08.pdf
- US Environmental Protection Agency (2005b) Particulate matter health risk assessment for selected urban areas. December 2005, EPA 452/R-05-007A
- US Environmental Protection Agency (2006) Air quality criteria for ozone and related photochemical oxidants (Final). US Environmental Protection Agency, Washington, DC, EPA/600/R-05/004aF-cF
- US Environmental Protection Agency (2007) Regulatory impact analysis of the proposed revisions to the national ambient air quality standards for ground-level ozone. Office of Air Quality Planning and Standards, EPA-452/R-07-008
- US Environmental Protection Agency (2008) National air quality status and trends through 2007. Office of Air Quality Planning and Standards, Research Triangle Park, North Carolina, EPA-454/R-08-006
- Wartenberg D (2009) Communicating air quality health impact estimates and their limitations to stakeholders. Air Qual Atmos Health 2(4) (this issue). doi:10.1007/s11869-009-0046-y
- White W (2009) Considerations in the use of ozone and PM2.5 data in exposure assessment. Air Qual Atmos Health 2(4) (this issue). doi:10.1007/s11869-009-0056-9 [DOI] [PMC free article] [PubMed]


