Abstract
Purpose: Caregivers feeling stress and experiencing mental health problems can be at risk for engaging in abusive acts against elderly care recipients. Potentially harmful behavior (PHB) was used as a measure of caregivers’ engagement in, or fear of engagement in, behavior that places dependent care recipients at risk of physical and/or psychological maltreatment and may be seen as an antecedent of, or a proxy for, identifiably abusive behavior. The study examined the ability of anger to mediate and moderate the relations of depression, resentment, and anxiety with PBH. Design and Methods: Data are from the first wave of the second Family Relationships in Late Life study of caregivers of community-dwelling elderly care recipients with whom they coreside. Caregivers (N = 417) completed face-to-face interviews. Results: Anger was found to mediate the relation between anxiety and PHB. Anger both mediates and moderates the relations of both depression and resentment with PHB in a dynamic way such that the mediating effect of anger increases substantially with increased scores on both depression and resentment. Implications: Identifying anger levels among caregivers who report symptoms of depression is warranted. Reducing depression in caregivers who report high levels of anger may result in reductions of PHB. Screening for resentment is warranted, as the relation between resentment and anger is similar to that between depression and anger.
Keywords: Informal caregiving, Risk factors, Caregiving dyads, Depression, Resentment, Anxiety, Potentially harmful behavior
Family members represent the “front line” of care provision for the growing number of ill, disabled, and demented older adults residing in the community. Unfortunately, many of these informal caregivers experience considerable stress and are at higher risk for poorer mental and physical well-being than noncaregivers (Bookwala, Yee, & Schulz, 2000). This article reports on an investigation of the mental health challenges to caregivers that can result in compromised care provision to others.
Several studies have linked caregiver depressive symptomatology with the quality of elderly care (Beach, Schulz, Williamson, Miller, & Weiner, 2005; Williamson, Shaffer, & The Family Relationships in Later Life Project [FRILL], 2001). Depressed caregivers are more likely than nondepressed caregivers to be subjects of investigation by social service agencies for possible elderly mistreatment (Bonnie & Wallace, 2003; Wolf, 1996). More depressive symptoms and feelings of resentment among informal caregivers are associated with caregiver self-reports of potentially harmful behavior (PHB), a precursor to elderly mistreatment (Beach et al.; Williamson et al., 2001, 2005). The association between depression and quality of care holds even after controlling for background characteristics and previous mental health status (Williamson et al., 2001). Conversely, care described as high in quality by caregivers and/or their care recipients is more common among caregivers who express fewer depressive symptoms (Dooley, Shaffer, Lance, & Williamson, 2007). Although the effects of depression are well documented in the caregiving literature, not all informal caregivers experience serious or debilitating symptoms of depression, and other negative affective reactions are possible.
Another frequent reaction to the burdens of care provision is the harboring of resentment. For example, caregivers may resent care recipient dependency or the responsibility associated with ensuring the daily welfare of another adult (Williamson, Shaffer, & Schulz, 1998; Williamson et al., 2001). Caregivers also may resent care recipient behavior that makes helping more difficult. In turn, more resentment is associated with lower quality of informal care (Williamson, Shaffer, & FRILL, 2000). Resentful caregivers may be more likely to harbor ill feelings toward their care recipients, leading to tension and conflict in the relationship (Schofield, Murphy, Herrman, Bloch, & Singh, 1997). These circumstances may lead to intense feelings of anger.
The emotional problem of anxiety has not been as extensively examined in caregiving relations as has depression, despite the fact that anxiety disorders may be more prevalent in caregivers than depression among caregivers (Mahoney, Regan, Katona, & Livingston, 2005). In examining the prevalence and covariates of anxiety in dementia caregivers, Cooper, Balamurali, and Livingston (2007) note that about a quarter of these caregivers demonstrate clinically significant symptoms of anxiety. In reviewing 33 caregiver studies, the authors found that along with physical health and caregiver burden, coping strategies of confrontation or avoidance were indicators of increased anxiety. They noted that although burden and physical health covariates were similar to those of caregiver depression, coping styles were more likely to be associated with anxiety than with depression. Others have found that although most depressed caregivers are also anxious, the inverse is not the case (Mahoney et al.). Neither care recipient cognitive status, degree of activities of daily living impairment, caregiver age, nor duration of caring were associated with caregiver anxiety (Cooper et al.). Given that predictors of depression may not be the same as those of anxiety, there is a need to consider anxiety as a separate outcome measure.
Pinquart and Sorensen’s (2003) systematic review of interventions for caregivers failed to include attention to anxiety, whereas Schulz and colleagues (2002) included a few studies with anxiety as a characteristic of interest. Mehta and colleagues (2003) noted that interventions that reduce depression may have little effect on reducing anxiety and concluded that it is useful to consider anxiety as a separate outcome.
Although efforts have been made to examine the relations among depression, resentment, and care provision, the consequences of anger on the delivery of informal elderly care have received relatively little research consideration. Caregivers may be less likely to acknowledge their anger in research or social service interviews because of shame at having these feelings or fear of social or legal scrutiny (Gallagher-Thompson, Lovett, & Rose, 1991). Yet, some caregivers do report becoming angry or frustrated in certain caregiving circumstances (Williamson et al., 1998; Zarit, Stephens, Townsend, & Green, 1998), such as when a care recipient exhibits behavioral problems (e.g., Kramer, Gibson, & Teri, 1992).
There is considerable interindividual variability in the frequency of anger and the manner in which anger is managed and expressed. For example, individuals prone to experiencing shame are more likely to feel resentment and/or anger, blame others for negative events, or act aggressively toward others in the face of interpersonal conflict. Individuals prone to experiencing guilt are more likely to adopt more constructive and prosocial conflict resolution strategies (Tangney, Wagner, Fletcher, & Gramzow, 1992; Tangney, Wagner, HillBarlow, Marschall, & Gramzow, 1996). There also is evidence of congruity of anger in close relationships such that when one partner expresses negative emotions and the other partner also experiences negative emotions in the same or different domains (Lane & Hobfoll, 1992). Spouses of depressed individuals commonly report depression, dissatisfaction, or anger (Bookwala & Schulz, 1996; Druley, Stephens, Martire, Ennis, & Wojno, 2003). Averill (1982) has identified several behavioral reactions to anger, including direct aggression, indirect aggression, displaced aggression, and nonaggressive responses.
Some caregiving literature gives attention to adverse consequences of caregiving stress on the quality of care given to older persons as well as to the coping strategies of caregivers. Coping strategies refer to specific behavioral and psychological efforts to master, tolerate, or minimize stressful events (Lazarus & Folkman, 1984). The use of one type rather than another is determined by one’s personal style as well as the nature of the stressful event (Folkman & Lazarus, 1988). When caregiving is long term, the predominant methods for dealing with stress appear to be emotion-focused coping strategies (Pruchno & Resch, 1989). Kramer (1993) found emotion-focused coping to be a significant predictor of depression for wives caring for husbands with dementia. Carver and Scheier (1994) identified coping mechanisms that they believe to be dysfunctional: denial, mental disengagement, behavioral disengagement, and the use of alcohol. Thus, coping styles may affect caregiver mental health outcomes.
In a study identifying predictors of elderly abuse and neglect, caregivers who reported physical abuse displayed higher depression scores, whereas those who reported neglect reported higher anxiety scores (Reay & Browne, 2001). A study by Gallagher, Rose, Rivera, Lovett, and Thompson (1989) reported that approximately two thirds of the elderly caregivers reported feeling angry or engaging in angry behavior toward their care recipient; many reported sufficient concern that their anger led them to seek formal services.
A National Research Council Report (Bonnie & Wallace, 2003) on elderly mistreatment concluded that depression is highly characteristic of perpetrators of elderly abuse. Williamson, Shaffer, & FRILL (2001) found that higher depression scores were predictive of more frequent occurrences of PHB, regardless of demographics, interpersonal relationships, and care recipient illness severity. Further analyses of the relationship between depression, resentment, and proactively aggressive caregiving strategies indicates that resentment mediated the impact of depression, suggesting that care recipients are at increased risk for PHB particularly when their depressed caregivers are resentful about their caregiving responsibilities (Shaffer, Dooley, & Williamson, 2007)
Thus, there is evidence that the quality of care given to an older person is affected by the existence of caregiver depression, anxiety, and resentment. What is not clearly understood, however, is the specific relationship between caregiver anger and anxiety, depression, and resentment. Given the important effect resentment has on depression in caregivers, examining the relationship between anger and depression, resentment, and anxiety is warranted.
Focus of the Study
The present study examines associations among caregiver mental health and quality of elderly care; specifically, we examine care that places older adults at risk for physical or psychological maltreatment. We tested a model in which the relations between the frequency of possible adverse behavior toward care recipients (PHB) and the caregiver anxiety, depression, and resentment are moderated and mediated by the anger experienced by the caregiver. The proposed hypotheses are found in Table 1.
Table 1.
Predicted Hypotheses
| Hypothesis 1 | Anger mediates the relations of anxiety (Hypothesis 1a), depression (Hypothesis 1b), and resentment (Hypothesis 1c) with PHB |
| Hypothesis 2 | Anger moderates the relations of anxiety, depression, and resentment with PHB such that the strength of the relation between anxiety (Hypothesis 2a), depression (Hypothesis 2b), and resentment (Hypothesis 2c) with PHB will vary across different levels of caregiver anger |
| Hypothesis 3 | The degree to which anger mediates the relations between anxiety (Hypothesis 3a), depression (Hypothesis 3b), and resentment (Hypothesis 3c) will depend on the levels of these variables such that the mediation will be stronger under high anxiety, depression, and resentment than under low anxiety, depression, and resentment. This is a prediction of moderated mediation (Preacher, Rucker, & Hayes, 2007) |
Note: PHB = potentially harmful behavior.
Method
Procedure
The analyses presented in this article are based on the first wave of interviews from the second FRILL2 Project, a multisite longitudinal study of informal care provided by caregivers of community-dwelling elderly care recipients with whom they coresided. The voluntary sample was recruited from Athens, GA, Pittsburgh, PA, Tuscaloosa, AL, and surrounding areas. To be eligible for the study, caregivers had to be primarily responsible for the care of a cognitively or physically impaired care recipient more than 60 years of age with whom they coresided and they had to provide unpaid help with at least one basic activity of daily living or two instrumental activities of daily living.
A primary goal of FRILL2 was to oversample African American caregiving dyads in order to obtain data sufficient to address issues conspicuously missing in previous research on the quality of informal elderly care (e.g., longitudinal comparisons between White and African American caregivers). Within these constraints, we attempted to obtain as representative a sample as possible. These efforts began with random-digit dialing (RDD) in the data collection sites. We then narrowed our search to age-targeted RDD (e.g., individuals aged 60 years and older according to U.S. Census data). To increase the number of African American participants, we used community-based snowball referral methods at the Georgia site in which enrolled African American dyads were recontacted and asked to provide the names and telephone numbers of other potentially eligible dyads. In initial screening, RDD methods identified 877 potential dyads; snowballing methods produced 95 potential dyads. Our recruitment efforts produced 765 eligible dyads, 321 (42%) of whom declined participation, resulting in a sample of 444 caregivers (58% participation rate). Of these, 27 caregivers had enough missing data to be excluded from the current analyses, resulting in a sample size of 417. These methods resulted in a sample that was 55% White and 43% African American.
Face-to-face structured interviews, lasting between 1.5 and 2 hr, were conducted in respondents’ homes by pairs of carefully trained interviewers. Each participant was paid $25 for a completed interview. To prevent data contamination, caregivers and care recipients were interviewed separately and simultaneously by two interviewers. The consent form for the study contained a sentence advising participants that suspected cases of abuse would be reported to the proper authorities. No reportable cases were observed, and no participants refused to be interviewed after receiving information informing them of our obligation to report suspected cases of abuse.
Sample
Similar to national estimates (e.g., National Alliance for Caregiving & the American Association of Retired Persons, 1997; Select Committee on Aging, U.S. House of Representatives, 1987), 69% of caregivers and 52% of care recipients in the study were women. Mean caregiver age was 60 years (SD = 15, range 18–98), and care recipients were, on average, 75 years (SD = 7.8, range 60–102). Slightly more than half of the caregivers (52%) were spouses of their care recipients. African Americans were oversampled in order to obtain a sample with roughly equivalent numbers of Whites and African Americans. The ethnic background of our final sample was 55% White, 43% African American, and 2% other ethnic heritage. Twenty-seven percent of care recipients had a medical diagnosis of dementia or another disorder that causes memory problems (e.g., Alzheimer’s disease, Parkinson’s disease). Duration of care provision at the time of the interviews ranged from less than 1 year to more than 50 years (M = 6.9 years, SD = 7.8, range <1–58). Median household income for these families was $20,000–$29,000 (range <$5,000–>$100,000).
Measures
Caregiver Depressed Affect.—
Caregiver depression was assessed using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D) (Radloff, 1977), which asks about the frequency with which respondents have experienced depressive symptoms within the last week (e.g., “I was bothered by things that usually don’t bother me,” “I felt that everything I did was an effort”). Total scores range from 0 to 60, with higher scores indicating elevated levels of depressive symptoms. The mean CES-D score was 11.9 (SD = 9.9, range 0–47). Individuals with scores of 16 or above are considered to be at risk for clinical depression; 27% of our caregivers were in this category. Cronbach’s α for our sample was .89.
Caregiver Anger.—
A short form of the Spielberger’s State-Trait Anger Scale (Spielberger, 1983) was used to assess how often respondents “generally” (trait) and “in the past week” (state) have felt mad, furious, etc. Higher scores on the scale indicate greater anger. This instrument has been used extensively in other studies, demonstrating good internal consistency (Spielberger, Jacobs, Russell, & Crane, 1983). It has shown concurrent validity with measures of hostility, neuroticism, and anxiety (Spielberger et al.) and has been used successfully to identify anger and hostility among elderly caregivers (Vitaliano, Young, Russo, Romano, & Magana-Amato, 1993). Cronbach’s α for our sample was .89.
Caregiver Resentment.—
We operationalized caregiver resentment as the sum of responses to a 17-item instrument adapted from previous research. Prior analyses have shown that combining 10 items from a resentment scale devised by Thompson, Medvene, and Freedman (1995) with 7 items from the Caregiver Burden Scale (Zarit, Reever, & Bach-Peterson, 1980) results in a measure of caregiver resentment that is psychometrically sound (Williamson et al., 2000, 2005). Caregivers indicated how often (1 = never, 5 = almost always) they felt resentful about such circumstances as not having enough time for themselves, having to give up plans for the future, or that their care recipients were overly dependent or made unreasonable demands. As in previous studies, Cronbach’s α in this sample was more than .90 (Martin-Cook, Remakel-Davis, Svetlik, Hynan, & Weiner, 2003; Williamson et al., 2000, 2005).
Caregiver Anxiety.—
Anxiety was measured using the Spielberger’s State-Trait Anxiety Inventory (STAI; Spielberger, Gorsuch, & Lushene, 1970). The measure consists of two subscales, one measuring enduring (trait) and the other transient (state) aspects of anxiety. We used the global score in our analyses. The STAI has high internal consistency and predictive validity in adult samples (Spielberger et al.) and is both reliable and valid in elderly populations (Nagatomo, Nomaguchi, & Takigawa, 1995). Cronbach’s α for our sample was .89.
Potentially Harmful Behavior.—
Due to the voluntary nature of our sample, we did not expect to identify dyads in which caregivers were guilty of severe forms of abuse and neglect. Rather, we assessed PHB (e.g., Beach et al., 2005; Dooley et al., 2007; Miller et al., 2006; Shaffer et al., 2007; Williamson et al., 2001) defined as adverse care that is not so severe that social or legal intervention is required. PHB was measured using a 10-item instrument developed from the Conflict Tactics Scale (Straus, 1979), work by Steinmetz (1988) and Pillemer and Suitor (1992), and our own analyses of the elderly abuse and neglect literature. The resulting instrument has adequate psychometric properties (e.g., Williamson et al.) and comprises five indicators of psychological mistreatment (e.g., caregiver screams and yells at care recipient) and five indicators of physical mistreatment (e.g., caregiver hits, slaps, or handles care recipient roughly). These questions were placed near the end of the structured interview with instructions carefully worded to decrease respondent reactance. Specifically, caregivers were asked to rate how often (0 = never and 4 = all of the time) they employed “methods that caregivers use when care recipients won’t follow a doctor’s orders or do what caregivers feel they should do.” Responses were summed to create a measure of PHB, with higher scores representing more frequent PHB, and an acceptable Cronbach’s α of .62.
As has been found in samples representing the general population (Cooper et al., 2009; Laumann, Leitsch, & Waite, 2008), PHB was, on average, infrequent in this sample (M = 1.1), but there was adequate variability (SD = 1.9, range 0–15). Most frequently cited indicators of PHB were psychological in nature; that is, caregivers reported at least occasionally screaming and yelling (34.9%); swearing at, insulting, or calling the care recipient names (19.9%); and threatening to abandon the care recipient (5.9%) or to send him or her to a nursing home (8.5%). However, 58% of our caregivers admitted to at least one of the following: shaking, hitting, slapping, handling the care recipient roughly, and/or to feeling afraid that they might hit or try to hurt the care recipient.
Analysis Plan
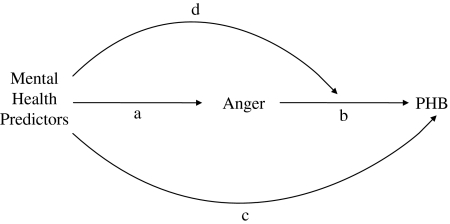
The model examined by our analyses is presented in Figure 1. We think that mental health predictors influence caregiver anger (Path A), which in turn influences the occurrence of PHB (Path B). This suggests that anger mediates the relation between mental health predictors and PHB (Hypothesis 1). In addition, mental health predictors directly influence PHB above and beyond the effect of anger (Path C). Finally, we think that the strength of the relation between anger and PHB is influenced by the mental health predictors (Path D). This suggests that mental health predictors moderate the relation between anger and PHB (Hypothesis 2).
Figure 1.
Model tested.
The strength of the mediated effect of a mental health behavior going through anger can be determined by multiplying together the coefficient for Path A and the coefficient for Path B (Sobel, 1982). If a variable changes the value of this product then it means that it is moderating the strength of the mediation effect (Preacher, Rucker, & Hayes, 2007). Our proposal that mental health predictors moderate the relation between anger and PHB (Path D) suggests that the value of B will depend on the values of the mental health predictors. Mathematically, we know that when B changes, the value of A × B also changes. This means that the presence of Path D suggests that the strength of the mediated effect will depend on the values of the mental health predictors. Thus, it is reasoned that the values of the mental health predictors will moderate the strength of the mediating path going through anger (Hypothesis 3).
To assess the hypothesized paths by which mental health variables might influence PHB, we undertook correlational, mediational, and moderational analyses, leading us to develop moderated mediation tests of our model. The addition of the moderated mediation analyses enables us to explain both how and when a given effect occurs. Preacher and colleagues (2007) propose that moderated mediation effects may occur in multiple ways. In this study, we specifically propose that the independent variables also function as a moderator of the path from the mediator variable to the dependent variable (see Figure 1, Path B).
Results
Correlational Analyses
Table 2 presents the correlations among anger, anxiety, depression, resentment, and PHB. All the predictor variables were positively correlated with one another, indicating the expected relationships between these emotional states. As anticipated, all predictor variables were significantly related to PHB.
Table 2.
Correlations Among Study Variables
| Anger | Anxiety | Depression | Resentment | |
| PHB | .44 | .27 | .32 | .46 |
| Anger | .51 | .55 | .42 | |
| Anxiety | .80 | .50 | ||
| Depression | .53 |
Notes: All correlations were significant at p < .001. PHB = potentially harmful behavior.
Hypothesis 1: Mediation Analyses.—
Using the guidelines specified by Baron and Kenny (1986), we tested whether the significant relations of anxiety, depression, and resentment with PHB were mediated by feelings of anger. Mediation can be tested by determining whether the relation between a predictor and the outcome is significantly reduced after controlling for the mediator. Sobel (1982) provides a test of whether the relation between the predictor and the outcome is significantly reduced after controlling for the mediator. If the relation between the predictor and the outcome is not significant after controlling for the mediator, it is referred to as full mediation. If there is still a relation between the predictor and the outcome after controlling for the mediator but the relation is significantly reduced, it is referred to as partial mediation. As seen in Table 3, anger fully mediated the relation between anxiety and PHB (Hypothesis 1a), partially mediated the relation between depression and PHB (Hypothesis 1b) and partially mediated the relation between resentment and PHB (Hypothesis 1c).
Table 3.
Tests of the Mediating Effects of Anger
| Anxiety | Depression | Resentment | |
| Relation between IV and PHB | b = 0.05, t(428) = 5.82, p < .001 | b = 0.06, t(431) = 7.03, p < .001 | b = 0.06, t(426) = 10.50, p < .001 |
| Relation between IV and PHB after controlling for the mediator | b = 0.01, t(427) = 1.26, p = .21 | b = 0.02, t(430) = 2.21, p = .03 | b = 0.04, t(425) = 7.16, p < .001 |
| Sobel test of mediation | Mediated effect = 0.04, Z = 6.66, p < .001 | Mediated effect = 0.04, Z = 6.42, p < .001 | Mediated effect = 0.02, Z = 5.50, p < .001 |
Note: IV = independent variable; PHB = potentially harmful behavior.
Hypothesis 2: Moderation Analyses.—
We next sought to determine whether anger moderated the relations of anxiety, depression, or resentment with PHB. We were interested in the extent to which the strength of the relation of anxiety, depression, and resentment with PHB vary across different levels of caregiver anger. To test for moderation, we used multiple regression to examine whether interactions between each mental health predictor variable and anger explained a significant proportion of variance in PHB scores. In order to avoid multicollinearity, we zero-centered anger and all predictor variables before computing interaction terms. More importantly for our interests, zero centering the predictor variables also changes the interpretation of the tests so that the noninteraction coefficients represent the main effects of the independent variables.
The results of moderation analyses are presented in Table 4. Anger moderated the relation of depression (Hypothesis 2b) and resentment (Hypothesis 2c) with PHB. Our results indicate that anger did not moderate the relation of anxiety with PHB; thus, Hypothesis 2a was not supported. Our results indicate that anger did not moderate the relation of anxiety with PHB. The presence of anger intensifies the likelihood that caregivers with either high levels of depression or high levels of resentment will exhibit PHB. There was also a main effect of anger such that caregivers reporting more anger scored higher on PHB.
Table 4.
Tests of the Moderating Effects of Anger
| Anxiety | Depression | Resentment | |
| Intercept | b = 1.12, t(426) = 12.70, p < .001 | b = 1.03, t(429) = 12.02, p < .001 | b = 1.01, t(424) = 12.76, p < .001 |
| IV | b = 0.01, t(426) = 1.26, p = .21 | b = 0.02, t(429) = 1.76, p = .08 | b = 0.04, t(424) = 6.63, p < .001 |
| Moderator (anger) | b = 0.17, t(426) = 6.65, p < .001 | b = 0.13, t(429) = 5.41, p < .001 | b = 0.10, t(424) = 5.13, p < .001 |
| IV × Moderator | b = −0.00, t(426) = −0.08, p = .933 | b = 0.00, t(429) = 2.38, p = .02 | b = 0.00, t(424) = 3.80, p < .001 |
| Test of full model | R2 = .19, F(3, 426) = 33.76, p < .001 | R2 = .21, F(3, 429) = 38.46, p < .001 | R2 = .31, F(3, 424) = 62.37, p < .001 |
Note: IV = independent variable.
Hypothesis 3: Moderated Mediation Analysis.—
The prior analyses demonstrated that anger mediates the relations of anxiety, depression, and resentment with PHB and that the relation between anger and PHB is moderated by depression and resentment. These findings indicate the presence of moderated mediation of anger by both depression and resentment (Preacher et al., 2007). As a reminder, moderated mediation means that the ability of a mediator to explain the relation between predictor and outcome depends on the level of the predictor (i.e., the moderator). There is no need for additional overall tests to determine the presence of moderated mediation because it is always present when the relation between a significant mediator and the outcome is moderated by another variable. Our focus therefore turns to understanding how the strength of the mediated effect changes. Preacher and colleagues provide a formula to assess the strength of a mediated effect across different levels of a moderating variable. We used this formula to explore how the ability of anger to mediate the relations between mental health predictors and PHB depends on the levels of those mental health predictors.
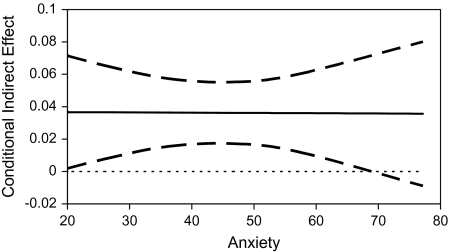
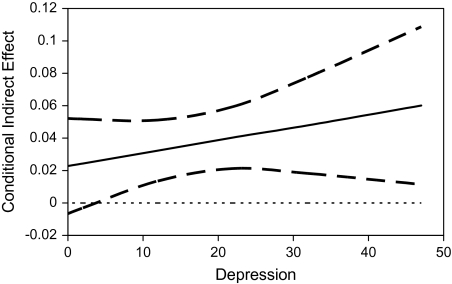
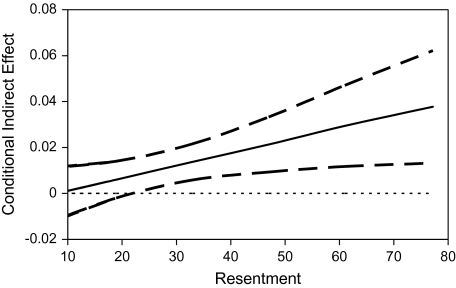
Figure 2 illustrates the conditional mediated effect of anger on PHB for different levels of anxiety. Although anxiety did not moderate the relation between anger and PHB, we wanted to illustrate the absence of conditional mediated effects for anxiety to act as a contrast for the results obtained for depression and resentment. Figure 2 shows that anger has a similar mediating effect across all values of anxiety, as noted by the horizontal nature of “anxiety”; thus, Hypothesis 3a was not supported. Figure 3 illustrates the conditional mediated effect of depression through anger for different levels of depression; Figure 4 illustrates the conditional mediated effect of resentment through anger for different levels of resentment. As shown in these figures, the mediating effect of anger substantially increases with higher scores on depression and resentment, respectively, thus supporting Hypotheses 3b and 3c.
Figure 2.
Conditional mediated effect for anxiety.
Figure 3.
Conditional mediated effect for depression.
Figure 4.
Conditional mediated effect for resentment.
Discussion
As the demands facing caregivers increase, so too does their risk for providing compromised care (Dooley et al., 2007). It is our opinion that increases in caregiver anger and other negative psychological states over the course of caregiving may lead to increased risks for older care recipients. A better understanding of the influences of caregiver mental health characteristics on PHB enhances our ability to target preventive interventions at the precursors to adversity in the caregiving experience.
This study shows that the influences of anxiety, depression, and resentment on quality of care are largely determined by the degree to which caregivers also experience anger. For instance, we found that caregiver anxiety does not predict PHB in the absence of caregiver anger. This suggests that caregiver anxiety may not directly lead to PHB against care recipients. Rather, the risk of PHB among these “anxious caregivers” may be due to the amount of anger produced by the anxiety. One practice implication of this finding is that efforts should be directed toward reducing anger in anxious caregivers’ efforts rather than toward reducing anxiety itself as a means of lessening the risk of PHB.
Depression and resentment directly influence PHB. Additionally, anger plays a significant role in the relations between depression and PHB and resentment and PHB. As anger increases, both depression and resentment appear to become more highly associated with PHB. Therefore, it is quite possible that managing anger can have positive effects on lessening the likelihood that depressed or resentful caregivers will engage in PHB. Our moderated mediation analyses suggest that as caregivers become more depressed or more resentful, anger is more likely to be associated with PHB. The practice implications of this are that identifying anger levels among caregivers who report symptoms of depression is warranted. Reducing depression in caregivers who report high levels of anger may result in reductions of PHB. Similarly, screening for resentment is warranted, as the relations between resentment and anger are similar to those between depression and anger.
Our findings have important implications for the identification of individuals who are appropriate or, perhaps more importantly, who are inappropriate for undertaking the caregiver role for a frail or dependent older person. In short, persons who are angry about their caregiving responsibilities may not provide adequate care to their elderly family members. When anger is coupled with moderate or high levels of depression or resentment, the levels of PHB increase significantly, suggesting the need for additional assessment of the caregiving experience. Caregivers demonstrating high levels of anger in addition to depression or resentment resulting from caregiving responsibilities cannot be considered good candidates as care providers as their care recipients are more vulnerable to the possibility of poor quality care.
The stress that these caregivers experience may emanate from many sources other than their caregiving responsibilities. Thus, professionals need to be sensitive not only to emotions related to the older care recipient but also to any existing tension, pressure, or resentment among caregivers. It seems that regardless of the causes of these emotions in the caregiver, the vulnerability of the older person to the possibility of harmful behavior may be high. Clearly, pragmatic concerns preclude a person’s exclusion from a caregiving role, even with elevated anger levels, but such circumstances should raise “red flags” for health and social service providers that additional assessment and intervention should be considered.
There is a clear need for supportive resources and interventions for caregivers experiencing anger as well as depression and resentment. In order to ensure the adequacy and quality of care being provided to vulnerable older persons, comprehensive assessments of caregivers for anger, depression, and resentment need to be periodically conducted. Interventions, including respite services, anger management training, cognitive reframing (for resentment), and increasing pleasant events, should be provided to address these conditions.
Limitations and Future Research Efforts
We recognize that in order to confirm the existence of mediation, it is necessary that both the effects of predictors on an outcome are related to the mediator and that evidence exists of a logically expected causal order (Baron & Kenny, 1986). The current study is cross sectional, and we suggest that logical arguments for the causal ordering of these variables have been presented elsewhere (Williamson et al., 2001).
Many studies of elderly abuse use known-group samples of individuals identified as perpetrators of these behaviors or offenses. Much of the literature on caregiving with older populations has focused specific caregiving systems, such as families in which dementia and terminal illnesses prompt caregiving. Our sample, on the other hand, included a wider focus of informal caregivers of older persons with physical, mental, and/or cognitive problems. Although we are confident that our sample is representative of a significant portion of caregivers of older persons in America, the extent to which our findings are generalizable to caregivers of older persons in other locations is seen to be limited. Subsequent studies that include broader samples are needed.
A number of additional research projects are suggested by this study. Although our sample was obtained from multiple sites, larger studies with broader representation of informal caregivers are needed. Studies employing measures that specifically capture caregiving-related depression and anger would be informative. More studies are needed to further our knowledge of how anxiety and resentment relate to caregiving. As our study relied on cross-sectional data, longitudinal data that examines how the relations we found change over time would be enlightening. Finally, the moderated mediation analysis we conducted is new, and further applications may suggest more important nuances and refinements allowing us to better understand and use this statistical test.
There is much more to know about the relations between mental health variables, including anger and PHB. The exploration of this topic is still in its early stages, but the benefits of continuing the search are great: ensuring the quality of care for older and impaired relatives by members of their own families.
Funding
The study was supported by the National Institute on Aging, Grant AG15321.
Acknowledgments
The second FRILL Project was conducted in the Department of Psychology of the University of Georgia (G. M. Williamson, principal investigator; W. K. Dooley, C. E. Lance, L. S. Miller, and D. R. Shaffer, coinvestigators) in collaboration with the University of Alabama (J. I. Kosberg, D. Nelson-Gardell, and F. Scogin, coinvestigators) and the University of Pittsburgh (R. Schulz, coinvestigator).
References
- Averill JR. Anger and aggression: An essay on emotion. New York: Springer-Verlag; 1982. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beach SR, Schulz R, Williamson GM, Miller LS, Weiner ME. Risk factors for potentially harmful informal caregiver behavior. Journal of the American Geriatrics Society. 2005;53:255–261. doi: 10.1111/j.1532-5415.2005.53111.x. [DOI] [PubMed] [Google Scholar]
- Bonnie RJ, Wallace RB. Elder mistreatment: Abuse, neglect, and exploitation in an aging America. Washington, DC: The National Academic Press; 2003. [PubMed] [Google Scholar]
- Bookwala J, Schulz R. Spousal similarity in subjective well being:The cardiovascular health study. Psychology and Aging. 1996;11:582–590. doi: 10.1037//0882-7974.11.4.582. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Yee JL, Schulz R. Caregiving and detrimental mental and physical health outcomes. In: Williamson GM, Shaffer DR, Parmelee PA, editors. Physical illness and depression in older adults: A handbook of theory, research, and practice. New York: Plenum; 2000. pp. 93–131. [Google Scholar]
- Carver CS, Scheier ME. Situational coping and coping dispositions in a stressful transaction. Journal of Personality and Social Psychology. 1994;66:184–195. doi: 10.1037//0022-3514.66.1.184. [DOI] [PubMed] [Google Scholar]
- Cooper C, Balamurali TBS, Livingston G. A systematic review of the prevalence and covariates of anxiety in caregivers of people with dementia. International Psychogeriatrics. 2007;19:175–195. doi: 10.1017/S1041610206004297. [DOI] [PubMed] [Google Scholar]
- Cooper C, Selwood A, Blanchard M, Walker Z, Blizard R, Livingston G. Abuse of people with dementia by family carers: Representative cross sectional survey. British Medical Journal. 2009;338:155–157. doi: 10.1136/bmj.b155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooley WK, Shaffer DR, Lance CE, Williamson GM. Informal care can be better than adequate: Development and evaluation of the Exemplary Care Scale. Rehabilitation Psychology. 2007;52:359–369. [Google Scholar]
- Druley JA, Stephens MA, Martire LM, Ennis N, Wojno WC. Emotional congruence in older couples coping with wives’ osteoarthritis: Exacerbating effects of pain behavior. Psychology and Aging. 2003;18:406–415. doi: 10.1037/0882-7974.18.3.406. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. The relationship between coping and emotion: Implications for theory and research. Social Science and Medicine. 1988;26:309–317. doi: 10.1016/0277-9536(88)90395-4. [DOI] [PubMed] [Google Scholar]
- Gallagher D, Rose J, Rivera P, Lovett S, Thompson L. Prevalence of depression in family caregivers. The Gerontologist. 1989;29:449–456. doi: 10.1093/geront/29.4.449. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Lovett S, Rose J. Psychotherapeutic interventions for stressed family caregivers. In: Myers WA, editor. New techniques in the psychotherapy of older patients. Washington, DC: American Psychiatric Press; 1991. pp. 61–78. [Google Scholar]
- Kramer B, Gibson J, Teri L. Interpersonal family stress in Alzheimer’s disease: Perceptions of patients and caregivers. Clinical Gerontologist. 1992;12:57–75. [Google Scholar]
- Kramer BJ. Marital history and the prior relationship as predictors of positive and negative outcomes among wife caregivers. Family Relations. 1993;42:367–375. [Google Scholar]
- Lane C, Hobfoll SE. How loss affects anger and alienates potential supporters. Journal of Consulting and Clinical Psychology. 1992;60:935–943. doi: 10.1037//0022-006x.60.6.935. [DOI] [PubMed] [Google Scholar]
- Laumann EO, Leitsch SA, Waite LJ. Elder mistreatment in the United States: Prevalence estimates from a nationally representative study. Journal of Gerontology. 2008;63:248–254. doi: 10.1093/geronb/63.4.s248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing; 1984. [Google Scholar]
- Mahoney R, Regan C, Katona C, Livingston G. Anxiety and depression in family caregivers of people with Alzheimer’s disease—The LASER-AD study. American Journal of Geriatric Psychiatry. 2005;13:795–801. doi: 10.1176/appi.ajgp.13.9.795. [DOI] [PubMed] [Google Scholar]
- Martin-Cook K, Remakel-Davis B, Svetlik D, Hynan LS, Weiner MF. Caregiver attribution and resentment in dementia care. American Journal of Alzheimer’s Disease and Other Dementias. 2003;18:366–374. doi: 10.1177/153331750301800606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta KM, Smonsick EM, Penninix BWJH, Schulz R, Rubin SM, Satterfield S, et al. Prevalence and correlates of anxiety symptoms in well-functioning older adults: Findings from the Healthy Aging and Body Composition Study. Journal of the American Geriatrics Society. 2003;51:499–504. doi: 10.1046/j.1532-5415.2003.51158.x. [DOI] [PubMed] [Google Scholar]
- Miller LS, Lewis MS, Williamson GM, Lance CE, Dooley WK, Schulz R, et al. Caregiver cognitive status and potentially harmful caregiver behavior. Aging and Mental Health. 2006;10:125–133. doi: 10.1080/13607860500310500. [DOI] [PubMed] [Google Scholar]
- Nagatomo I, Nomaguchi M, Takigawa M. Anxiety and quality of life in residents of a special nursing home. International Journal of Geriatric Psychiatry. 1995;10:541–555. [Google Scholar]
- National Alliance for Caregiving, & the American Association of Retired Persons. Family caregiving in the U.S.: Findings from a national survey. Washington, DC: Author; 1997. [Google Scholar]
- Pillemer K, Suitor JJ. Violence and violent feelings: What causes them among family caregivers? Journal of Gerontology. 1992;47:165–172. doi: 10.1093/geronj/47.4.s165. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sorensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Pruchno RA, Resch NL. Mental health of caregiving spouses: Coping as a mediator, moderator, or main effect. Psychology and Aging. 1989;4:454–463. doi: 10.1037//0882-7974.4.4.454. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reay AMC, Browne KD. Risk factor characteristics in carers who physically abuse or neglect their elderly dependents. Aging & Mental Health. 2001;5:56–62. doi: 10.1080/13607860020020654. [DOI] [PubMed] [Google Scholar]
- Schofield HL, Murphy B, Herrman HE, Bloch S, Singh B. Family caregiving: Measurement of emotional well-being and various aspects of the caregiving role. Psychological Medicine. 1997;3:647–657. doi: 10.1017/s0033291797004820. [DOI] [PubMed] [Google Scholar]
- Schulz R, O’Brien A, Czaja S, Ory M, Norris R, Martire LM, et al. Dementia caregiver intervention research: In search of clinical significance. The Gerontologist. 2002;42:589–602. doi: 10.1093/geront/42.5.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Select Committee on Aging, U.S. House of Representatives. Exploding the myths: Caregiving in America. Washington, DC: U.S. Government Printing Office; 1987. [Google Scholar]
- Shaffer DR, Dooley WK, Williamson GM. Endorsement of proactively aggressive caregiving strategies moderates the relation between caregiver mental health and potentially harmful caregiver behavior. Psychology and Aging. 2007;22:494–504. doi: 10.1037/0882-7974.22.3.494. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology 1982. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Spielberger C, Jacobs G, Russell S, Crane RS. Assessment of anger: The State-Trait Anger Scale. In: Butcher JN, Spielberger CD, editors. Advances in personality assessment. Vol. 2. Hillsdale, NJ: Erlbaum; 1983. pp. 159–187. [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Spielberger L, Gorsuch R, Lushene R. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Steinmetz SK. Elder abuse by family caregivers: Processes and intervention strategies. Contemporary Family Therapy. 1988;10:256–271. [Google Scholar]
- Straus M. Measuring intrafamily conflict and violence: The Conflict Tactics (CT) scales. Journal of Marriage and Family. 1979;41:75–88. [Google Scholar]
- Tangney JP, Wagner P, Fletcher C, Gramzow R. Shamed into anger? The relation of shame and guilt to anger and self-reported aggression. Journal of Personality and Social Psychology. 1992;62:669–75. doi: 10.1037//0022-3514.62.4.669. [DOI] [PubMed] [Google Scholar]
- Tangney JP, Wagner PE, Hill-Barlow D, Marschall DE, Gramzow RH. Relation of shame and guilt to constructive versus destructive responses to anger across the lifespan. Journal of Personality and Social Psychology. 1996;70:797–809. doi: 10.1037//0022-3514.70.4.797. [DOI] [PubMed] [Google Scholar]
- Thompson SC, Medvene LJ, Freedman D. Caregiving in the close relationships of cardiac patients: Exchange, power, and attributional processes on caregiver resentment. Personal Relationships. 1995;2:125–142. [Google Scholar]
- Vitaliano PP, Young HM, Russo J, Romano J, Magana-Amato A. Does expressed emotion in spouses predict subsequent problems among care recipients with Alzheimer’s disease? Journal of Gerontology. 1993;48:202–209. doi: 10.1093/geronj/48.4.p202. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Martin-Cook K, Weiner MF, Svetlik DA, Saine K, Hynan L, et al. Caregiver resentment: Explaining why care recipients exhibit problem behavior. Rehabilitation Psychology. 2005;50:215–223. [Google Scholar]
- Williamson GM, Shaffer DR, Schulz R. Activity restriction and prior relationship history as contributors to mental health outcomes among middle-aged and older spousal caregivers. Health Psychology. 1998;17:152–162. doi: 10.1037//0278-6133.17.2.152. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Shaffer DR. The Family Relationships In Later Life Project. Caregiver loss and quality of care provided: Pre-illness relationship makes a difference. In: Harvey JH, Miller ED, editors. Loss and trauma: General and close relationship perspectives. Philadelphia: Brunner/Mazel; 2000. pp. 230–237. [Google Scholar]
- Williamson GM, Shaffer DR The Family Relationships In Later Life Project. Relationship quality and potentially harmful behaviors by spousal caregivers: How we were then, how we are now. Psychology and Aging. 2001;16:217–226. [PubMed] [Google Scholar]
- Wolf RS. Understanding elder abuse and neglect. Aging. 1996;367:4–13. [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired aged: Correlates of feelings of burden. The Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Stephens MAP, Townsend A, Greene R. Stress reduction for family caregivers: Effects of day care use. Journal of Gerontology. 1998;53:267–277. doi: 10.1093/geronb/53b.5.s267. [DOI] [PubMed] [Google Scholar]