Abstract
The epidemiologic transition describes changing patterns of population age distributions, mortality, fertility, life expectancy, and causes of death. A number of critiques of the theory have revealed limitations, including an insufficient account of the role of poverty in determining disease risk and mortality, a failure to distinguish adequately the risk of dying from a given cause or set of causes from the relative contributions of various causes of death to overall mortality, and oversimplification of the transition patterns, which do not fit neatly into either historical periods or geographic locations. Recent developments in epidemiologic methods reveal other limitations. A life course perspective prompts examination of changes in causal pathways across the life span when considering shifts in the age distribution of a population as described by the epidemiologic transition theory. The ecological model assumes multiple levels of determinants acting in complex and interrelated ways, with higher level determinants exhibiting emergent properties. Development, testing, and implementation of innovative approaches to reduce the risks associated with the sedentary lifestyle and hyper nutrition in developed countries should not overshadow the continuing threat from infectious diseases, especially resistant strains or newly encountered agents. Interventions must fit populations and the threats to health they experience, while anticipating changes that will emerge with success in some areas. This will require new ways of thinking that go beyond the epidemiologic transition theory.
Keywords: epidemiologic transition, epidemiologic methods, mortality rates, life expectancy, causal models
Introduction
The epidemiologic transition describes changing patterns of population distributions in relation to changing patterns of mortality, fertility, life expectancy, and leading causes of death. The perspective has its origins in demography, but finds a compatible conceptual home in public health and epidemiology in particular. This paper is intended to provide a general overview of the concept, with historical and recent data from the United States and other countries to illustrate key ideas. The paper then proposes a few reasons to consider as revisions to the theory, and finally suggests some implications for epidemiologic methods and public health interventions.
The very term “epidemiologic transition” raises the question of transition from what to what? There are two major components of the transition: (1) changes in population growth trajectories and composition, especially in the age distribution from younger to older, and (2) changes in patterns of mortality, including increasing life expectancy and reordering of the relative importance of different causes of death.
Though the ideas where not original to him, A. R. Omran is typically credited with formulating the theory of the epidemiologic transition in the form that came to be frequently cited. In his 1971 article1 he wrote: “Conceptually, the theory of epidemiologic transition focuses on the complex change in patterns of health and disease and on the interactions between these patterns and their demographic, economic and sociologic determinants and consequences.” Since the 1971 publication the theory has been adopted and adapted, revised and criticized, demonstrating both its influence and limitations. The perspective taken in this paper is that the theory is most relevant as a way of looking at and understanding the relation among disease, mortality patterns, and population dynamics rather than as a definitive explanation or prediction.
The original formulation: Omran’s Five Propositions
The first proposition
Omran’s formulation of the theory consisted of five propositions. Proposition one was: “The theory of epidemiologic transition begins with the major premise that mortality is a fundamental factor in population dynamics. 1” At first glance this seems self-evident and of little heuristic value; however, this proposition is grounded in the insight that declining mortality is typically followed by declining fertility, and it is the combination of lower birth rates as well as lower death rates and higher life expectancy that produce the altered population age distribution. If birth rates remained stable, the process of change in the shape of the population distribution would follow a different pattern.
The second proposition
The second proposition was: “During the transition, a long-term shift occurs in mortality and disease patterns whereby pandemics of infection are gradually displaced by degenerative and man-made [sic] diseases as the chief form of morbidity and primary cause of death. 1” Because this proposition is really at the heart of the theory and includes changes in patterns of mortality and morbidity as well as in the age distribution, it is more complex and requires more extended elaboration.
The first transition
Omran posits three typical phases of transition. The first transition phase, called the “Age of Pestilence and Famine”, is characterized by high and fluctuating mortality rates, variable life expectancy with low average life span, and periods of population growth that are not sustained. Armelagos et al., 2 propose that the earliest transition dates to pre-history (Neolithic period, approximately 10,000 years ago) across geographically widely separated cultures. According to their reading of the evidence, the transitions were a result of the transformation from hunter-gatherer societies to agrarian societies, with more settled life required in order to tend cultivated crops and domesticated animals. The change in patterns of livelihood and living conditions also meant changes in population size and density and daily life in closer proximity to animals. The reduction in human and animal migration created a new kind of ecological imbalance. There was an increase in infectious diseases as a result of exposure to human and animal waste and contaminated water and the reciprocal transmission of organisms between human and animal hosts. The disease patterns that emerged were determined by increasing microbial exposures, dietary deficiencies because the food supply, though perhaps more reliable in good years, was less diverse, illnesses due to inadequate food storage, increased transmission rates and endemic disease as a result of increased population density, eventual development of global trade with a concomitant increase in potential for disease spread over wide geographic regions, and increased mortality which, in keeping with the epidemiologic transition model, would lead to increased birth rate.
The second transition
The second transition phase is characterized as the “Age of Receding Pandemics”, and is marked by declining mortality rates that become steeper as epidemics occur less frequently, an increase in average life expectancy from about 30 years to about 50 years of age, and more sustained population growth that eventually becomes exponential. This transition occurs in the early modern period and is characterized by a shift in patterns of disease and mortality from primarily infectious diseases to what have come to be called “chronic” diseases. The theory proposes that this shift is accompanied by a shift in the population age distribution as early infectious disease deaths decline and deaths from chronic and degenerative disease increase, the latter a result not only of the receding competing risk from infectious diseases, but also of the new environmental hazards that came with industrial development and increasing urban living.
Explanations for these changes are multi-faceted and complex and include changes in the relationships in the classic matrix of agent, host, and environment; socioeconomic, political, and cultural changes; improved living conditions and standard of living, including the contributions of the sanitary movement to water and sanitary services, improved nutrition, better personal hygiene, and less overcrowding; medical and public health advances and interventions; better understanding of infectious diseases with acceptance of the germ theory and adoption of antiseptics and pasteurization; lower fertility and longer birth intervals with better infant and child survival; and increasing lifespan resulting in an older population.
The third transition
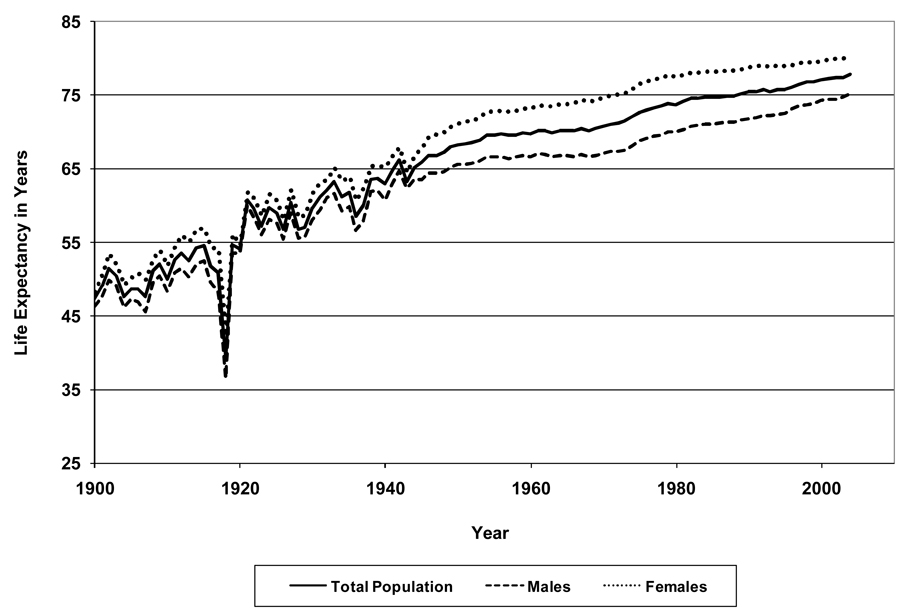
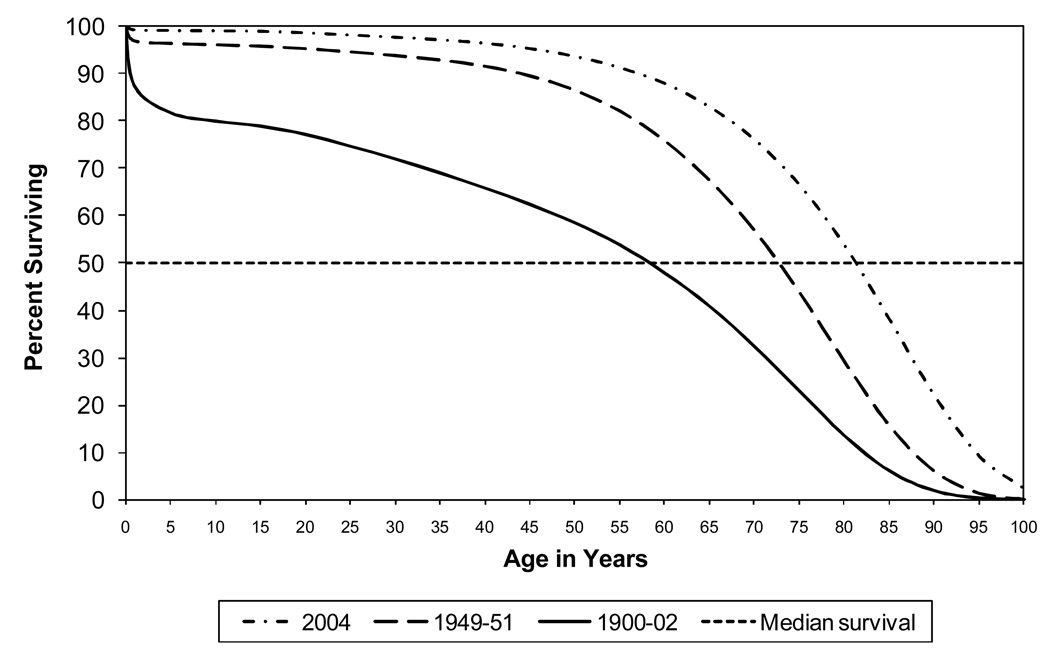
The third transition phase is termed the “Age of Degenerative and Man-Made [sic] Diseases”. In this phase it is theorized that infectious disease pandemics are replaced as major causes of death by degenerative diseases, and infectious agents as the major contributor to morbidity and mortality are overtaken by anthropogenic causes. With declines in mortality rates, average life expectancy increases to > 50 years, fertility becomes more important to population growth, and the anthropogenic and biologic determinants of disease also change. This transition is typically associated with the late 19th and 20th centuries in developed countries. Figure 1 depicts average life expectancy at birth in the United States from 1900 to 2004, overall and by sex. Note life expectancy increases from less than 50 years of age at the beginning of the 20th century to over 75 years at the beginning of the 21st century. Note also the sharp, but transient drop in life expectancy as a result of the influenza pandemic of 1918. This illustrates the impact that a pandemic can have on life expectancy and population distribution. Figure 2 presents survival curves for the US population for the years 1900–02 (death registration states only), 1949–51, and 2004. Note the dramatic increase in median survival time, indicated by the horizontal dotted line. Note also the sharp drop at the beginning of the 1900–02 curve, indicating very high infant mortality.
Figure 1. US Life Expectancy at Birth Overall and by Sex, 1900 – 2004.
Data from National Center for Health Statistics
Figure 2. US Population Survival Curves, 1900–02, 1949–51, 2004.
Note: Median line represents half of the population has died and half remain alive, so point at which median line crosses each survival curve is the median survival time for that cohort. Data for 1900–02 from death registration states only. Data from National Center for Health Statistics.
The third proposition
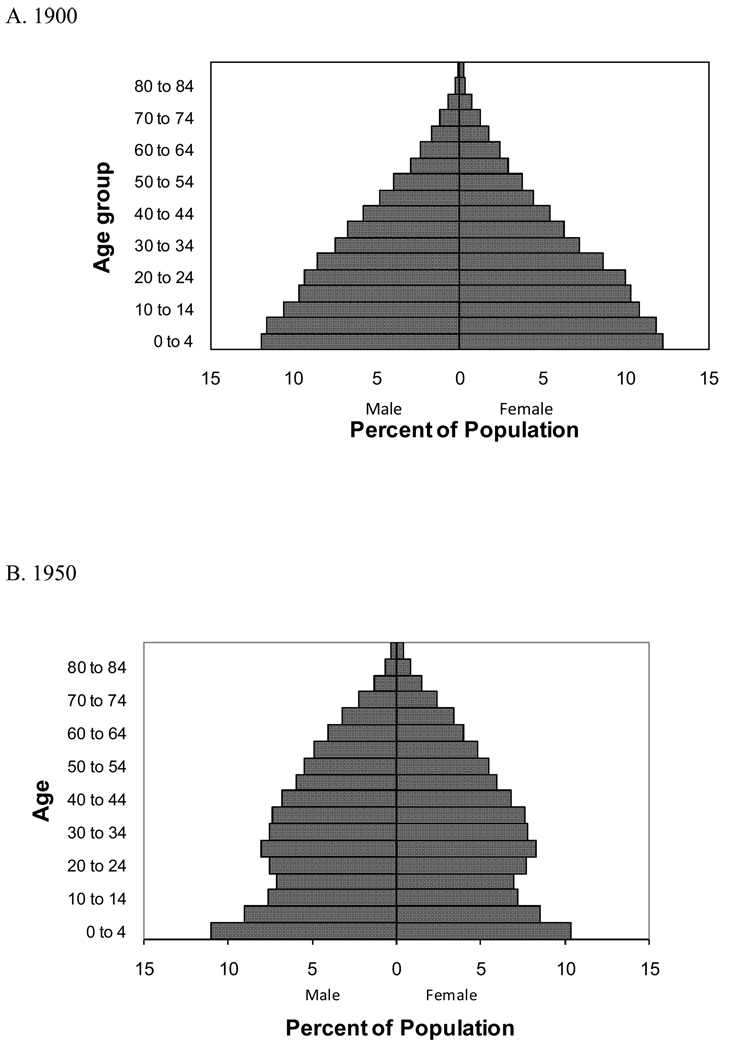
Proposition three states that “During the epidemiologic transition the most profound changes in health and disease patterns obtain among children and young women.”1 This phenomenon is largely a result of declining infant and maternal mortality and a consequent drop in fertility. Note in Figure 1 that the difference in life expectancy between women and men is greater in the last half of the 20th century than in the first half, no doubt reflecting reduced rates of perinatal maternal mortality. Similarly, Figure 3 shows population pyramids for the US in 1900, 1950, and 2000. The reduction in fertility over time is clear, as is the increasing proportion of older people in the population. Note the impact of the depression on births evident in the 1950 diagram as well as the leading edge of the post-war “baby boom”. The baby boom bulge is evident in the 2000 diagram.
Figure 3. US Population Distribution by Age and Sex, 1900, 1950, 2000.
Data from National Center for Health Statistics
The fourth proposition
The fourth proposition holds that “The shifts in health and disease patterns that characterize the epidemiologic transition are closely associated with the demographic and socioeconomic transitions that constitute the modernization complex. 1” This proposition in some ways bridges the other propositions in that, consistent with the third, it is characterized by lower fertility and longer birth intervals, and in keeping with the second and fifth it is posited that improved socioeconomic status leads to better nutrition and sanitation, which in turn improve health and reduce morbidity and mortality.
The fifth proposition
The final proposition outlines three basic models of the epidemiologic transition that are a function of “peculiar variations in the pattern, the pace, the determinants and the consequences of population change. 1” These three models are “the classical or western model, the accelerated model and the contemporary or delayed model.” They roughly correspond respectively to (1) the experience of developed countries that evidence slow declines in death rates followed by lower fertility that accompanies modernization; (2) the experience of countries, such as Japan, where the course of the transition was much more rapid and the amount of time required to reach the milestone mortality rate of 10 deaths per 1000 population is much shorter; and (3) the experience of developing countries where there have been more recent declines in mortality, but not in fertility rates because infant and maternal mortality rates still remain high.
Transitions in epidemiology and public health
It is instructive to consider historical transitions in epidemiology and public health that in some ways mirror the transitions described above. The modern public health movement had its origins in the Sanitary Movement of the 18th and early 19th centuries, with its focus on community characteristics, economic conditions, and environmental influences. Improvement of living conditions was seen as a means of improving health. This formative period in the history of public health continues to be relevant, reflecting a rudimentary version of the current understanding of the determinants of health as multifactorial and contextual. 3
By the end of the 19th century, the germ theory of disease had matured and largely displaced the miasma theory on the basis of scientific advances in bacteriology, chemistry, and medicine as well as epidemiology. The recognition of infectious diseases as major contributors to morbidity and mortality, the rapid development of new knowledge and tools, and the effectiveness of public health efforts in reducing the incidence of and mortality from some infectious diseases led to increasing dominance of this theory, which dramatically shaped public health programs and practice, and contributed to steep declines in mortality from infectious diseases in the U.S. and other developed countries. The other side of this development was that public health came to be viewed largely through the lens of infectious disease prevention and control.
Consistent with the transition theory, by mid-20th century, public health attention shifted to chronic disease prevention and control, with emphasis on risk factor epidemiology and interventions directed toward individual behavior and lifestyle. The earlier dominance of germ theory and microbiology may have narrowed the view of the mission of public health, putting the population focus and developing quantitative approaches in competition with the microscope, but new developments in understanding genetic and cellular processes (a potential new “germ theory”) have been accompanied by renewed interest in both psychosocial characteristics and broader contextual and environmental influences. This broader perspective on the determinants of health and disease encompasses but goes beyond traditional risk factor epidemiology. It includes explicit attention to the complexity of systems and the challenges of integrating multiple levels from the genetic to the personal to social, political, and economic contexts across the life span.
This methodological transition has been particularly evident in the remarkable evolution of epidemiology as a discipline since World War II.4 These changes have resulted from developments on several interrelated fronts both within and outside the field. Theories of health and disease have received greater attention, with broader concepts of health as encompassing more than the absence of disease. A renewed focus on population health, as well as development of more complex causal models reflecting new discoveries focused greater attention on more thoughtful considerations of causal inference and explanation of causal associations, not just identification of risk factors. The continuing threat from infectious diseases and increasing attention to health disparities have challenged traditional risk factor approaches. Some of the more recent discoveries in infectious disease have arisen from an approach and conceptual framework and methodology rather distinct from that of the golden age of late 19th and early 20th century microbiology. Awareness of the importance of a life span perspective has also been accompanied by increased attention to etiologic investigations of degenerative diseases of aging formerly thought to be unavoidable. Alongside explorations of genetic causes has been renewed interest in research on environmental factors, both as external causal agents and as potential modifiers of genetic causes, with the goal of understanding processes in order to develop more effective preventive interventions. While retaining intervention and prevention as goals, epidemiologists now seek to incorporate systems perspectives within an ecological model with its multi-leveled approach and life span considerations.
In sum, the eco-epidemiologic5,6 approach is characterized by a life course perspective, recognition of multiple, interrelated levels of causation, and an emphasis on models that are more integrated rather than fragmented.7 The implications for our research methods parallel those three components. First, the life course perspective requires us to think in terms of changes in causal pathways across the life span when considering shifts in the age distribution of a population as described by the epidemiologic transition theory. Second, the causal models on which we rely must allow for multiple levels of determinants acting in complex and interrelated ways, often synergistically or with feed-back loops or reciprocal lines of causality. Further, we have to consider that higher level or “upstream” determinants may have emergent properties that are more than the aggregate of their constituent parts, so that we must consider them along with the lower level elements in our models and analysis. Finally, when considering the multiple levels of the ecological model, we rely on the understanding that disease occurs in individuals, but interventions can occur at any level, including communities.
The 2002 Institute of Medicine follow-up report8 emphasized the “public” aspect of public health, that is, “healthy people in healthy communities.” This in some ways is a recapitulation of the Sanitary Movement’s emphasis on living conditions, but goes beyond that earlier perspective. There has been a rich discussion in the public health literature on the definition and nature of healthy communities. For purposes of this paper, the critical development is that public health professionals increasingly recognize an organic notion of community, emphasizing that individual health is achieved or threatened by larger scale contextual factors, including social networks, environment, education, economic opportunity, and other characteristics of communities, many of which evidence emergent properties as described above.8
This emerging perspective sees the whole range of determinants as integral to personal and community health and well-being.3,5–6 The modern ecological model of public health practice stresses the multiple dimensions that constitute our lives, relationships and environments, and, therefore, contribute to health and wellness or disease and disability.8 Further, the threat of emerging infectious diseases continues to have global significance in an era of resurgent multidrug resistant tuberculosis, pandemic AIDS, and widespread distribution of vector borne diseases. These demonstrate that the transitions cannot be neatly categorized into either historical periods or geographic locations. The multilevel view of the ecological model also reminds us that the various and shifting foci observed in the historical stages of public health must be incorporated into a more encompassing view with more complex models, systems, and processes rather than the simple identification of isolated risk factors.
Critiques of the theory
The epidemiologic transition theory appears to have some confirmation in recent trends that were characterized by increased life expectancy and a shift in the population age distribution to older ages as well as the concomitant increase in the numbers of people living with chronic degenerative disease. These changes have profound impact on public health planning, health care resources and workforce development, and a range of social, political, and financial policies. While such changes consistent with the theory have been evident, the theory has not been without its critics and a number of issues remain controversial. Caldwell writes that the original theory “fails to grasp the global nature and historical sequence of the mortality transition as it spread.9” Criticisms of the original theory reflect continuing development in theories of health and disease, disagreement about the role of advances in medicine relative to public health interventions, and debate about the relative importance of various contributors to the unquestioned changes in mortality and disease patterns, especially with regard to nutrition, poverty, and income inequalities.
One of the arguments made today is that the emergence of cities and organized societies that triggered the first transition came with social stratification that is a precursor of the disparities in social position and wealth observed in later stages and prominent still. 2 The argument is that wealth and poverty and their relative distribution play central roles in health and well being in each stage. Pearson 10 has argued that the roles of income and education in the most recent stage are paradoxical in that, compared to those who are poor and less educated, wealthier and more educated persons tended to be earlier adopters of lifestyles that contributed to the increased risk of those diseases that now constitute the major causes of death, but they were also earlier adopters of treatments and lifestyle changes that subsequently reduce the risk of morbidity and mortality. The result, according to Pearson is that poor and poorly educated populations may experience later peaks in the incidence of the diseases that define the third transition phase, but also continue to suffer from elevated rates of those chronic diseases after rates have begun to decline among those better off. Pearson argues that this requires simultaneously working for economic development and improved education to reduce perinatal, infectious, and nutrition-related diseases while implementing proven strategies to discourage adoption of those detrimental behaviors and exposures associated with chronic diseases in more prosperous segments of the population. Note that these differences are most evident in comparisons of developed and underdeveloped countries, but also hold for different segments of the population within the same country.
It can be argued that the publication of Omran’s paper came at a time of naïve optimism concerning mortality patterns, causes of morbidity and mortality, and global progress in life expectancy. In 1969 testimony before congress the US Surgeon General said that it was “time to close the book on infectious disease as a major health threat. 2” Though it might have been impossible at that point to foresee the global emergence of HIV/AIDS and other so-called emerging infectious diseases and the serious challenges of antibiotic resistance, ecological disruption with its consequences for health and environment (including contributing to emerging diseases) was taking place, and the devastating impact of infectious disease on the poor and those living in developing or under-developed countries was evident. More recently, and somewhat ironically, recognition of the continuing impact of infectious diseases and inadequate nutrition, coupled with ecological disruption, has come with an emphasis on the role of poverty in poorer outcomes and wider disparities. Armelagos et al2., write: “While disease and death are inevitable, a major cause of unnecessary, premature, preventable disease and death is simple; it is extreme poverty.”
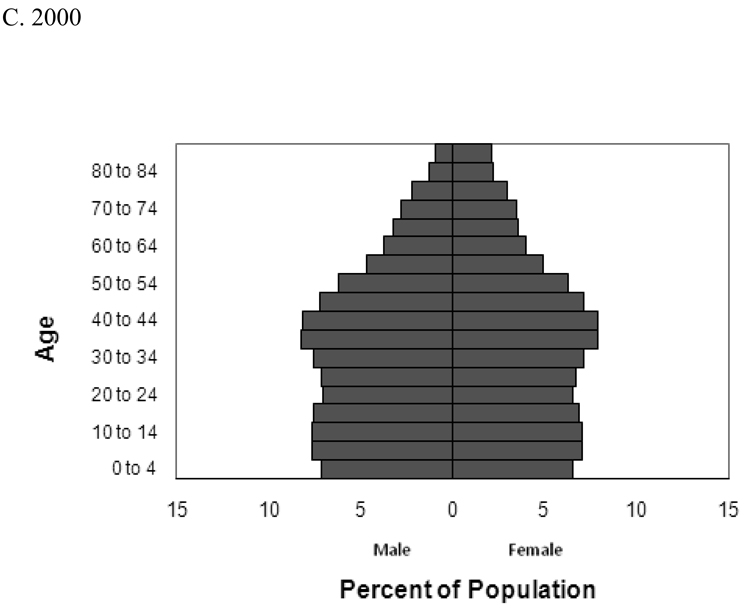
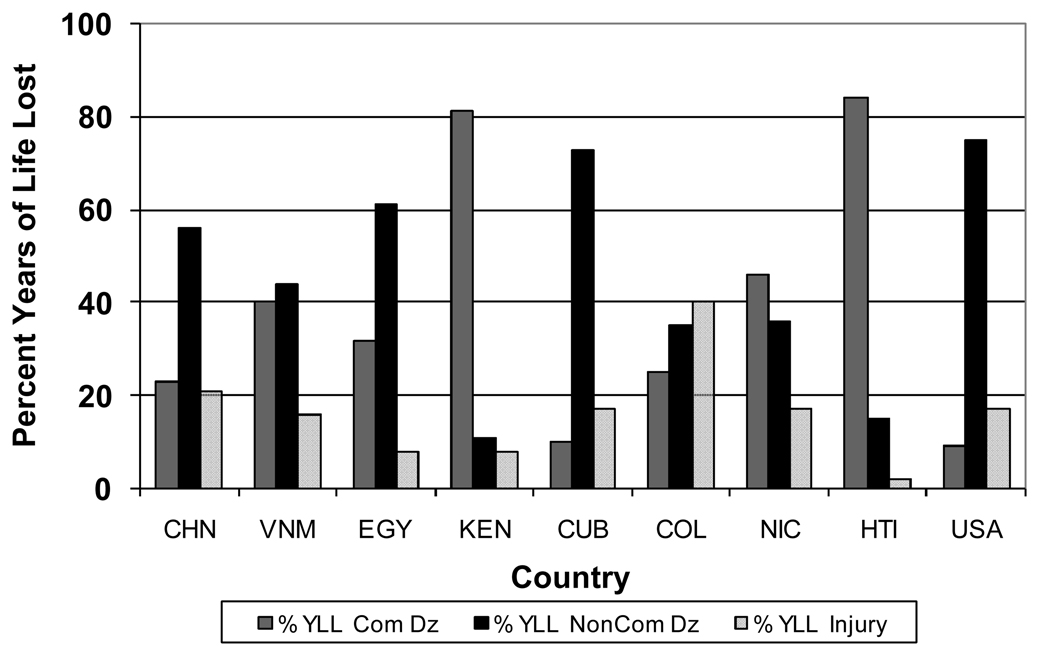
Another criticism of the traditional theory is that it fails to distinguish adequately the risk of dying from any given cause or set of causes from the relative contributions of the various causes of death to overall mortality.11 To take an example comparing age groups in the US rather than historical periods or countries, accidents (unintentional injuries) are the leading cause of death among persons 15 to 24 years old in the US, accounting for 46% of all deaths in that age group in 2004, while among those ages 65 to 74 they accounted for just over 2% of all deaths. However, the cause-specific rate (as an estimate of the risk) of death from accidents in 2004 was 37.4/100,000 in the younger group versus 46.3/100,000 in the older group. As patterns of disease and mortality change, there are changes in the relative contribution of different causes to overall mortality that may not reflect changes in actual risk. For example, in this country rates of mortality of cardiovascular disease (CVD) have been declining, but CVD remains the leading cause of death overall. If the risk of dying from one causes decreases, the relative proportions of other causes will increase even if the actual risk remains the same. Actual risk for death from a specific cause could even decline while the proportion of deaths attributed to that cause goes up if risk of death from other causes declines more rapidly. Heuveline et al have shown the people in the poorest quintile suffer consistently higher mortality in all three of the major categories of disease used by the World Health Organization than those in the richest quintile, and the most of the excess mortality is primarily due to the higher risk of communicable diseases.12 Both the relative contributions and the actual risk of death from the major cause of death categories vary widely across countries, even between countries in the same region, as well as across population groups within a country. Figure 4 shows the relative contributions of the three major cause of death categories, though not the actual risk associated with each, for nine countries to illustrate this point graphically. The point is that the epidemiologic transition theory oversimplifies the patterns and relations among risk of mortality, mortality causes, and life expectancy. The patterns are clearly more complex than simply declining mortality rates from infectious diseases and increasing rates of death from the so-called chronic diseases and do not fit neatly into either historical periods or geographic locations.
Figure 4. Percent Years of Life Lost to Major Cause of Death Groups for Selected Countries.
Note: YLL=Years of life lost; Com Dz = Communicable Diseases; NonCom Dz=Noncommunicable diseases; CHN=China; VNM=Viet Nam; EGY=Egypt; KEN=Kenya; CUB=Cuba; COL=Colombia; NIC=Nicaragua; HTI=Haiti; USA=United States. Data from World Health Organization
A further complexity now being recognized is that the distinction between infectious and chronic disease is not clearly demarcated. Not only is it the case that some infectious diseases have chronic disease characteristics, but we have come to recognize the importance of infectious agents and related inflammatory processes in the etiology of a number of chronic diseases and adverse outcomes, such as cervical cancer (HPV), gastroduodenal ulcer (H Pylori), and cardiovascular disease (inflammation), and there is more research now on links to outcomes as divergent as diabetes, preterm delivery, and some mental illnesses. The other side of that complex picture is that many of the characteristics and behaviors we have found to be protective for chronic disease may also provide some protection against infectious disease or reduce the severity of sequelae.
Implications for epidemiologic methods and conclusion
The theory of epidemiologic transition has been useful in laying out an overarching perspective on changing demographic patterns. The various criticisms of the theory suggest it is most relevant as a way of looking at and understanding the relation among disease, mortality patterns, and population rather than as a definitive explanation or prediction. Among the major critiques of the theory is that the overemphasis on mortality rather than disease causality and morbidity misses critical pieces of complex phenomena. The focus on mortality and life expectancy gives insufficient attention to disability and quality of life. Further, our understanding of and approach to causal inference have matured in the nearly four decades since Omran’s original article appeared. The importance of the ecological model and what has been called eco-epidemiology have enriched our thinking and our methods and enhanced our understanding of differential patterns of morbidity and mortality within and across populations and different segments of populations.
Though it is true that the burden from infectious diseases has been surpassed in many countries by the burden from chronic disease and mental disorder, it is still the case in many countries and in many populations within countries that morbidity and mortality from infectious disease, poor nutrition, and perinatal complications dominate, with poverty being the most evident shared characteristic. We cannot assume that the evidence of the epidemiologic transition means we can redirect our attention and resources away from those determinants of death and disease that still threaten the lives and well being of a large portion of the world’s population. But we must also recognize that those same populations will be victims of the obesity, CVD, hypertension, and diabetes epidemics that now characterize the US. Even as we continue to develop, test, and implement innovative approaches to reduce the risks associated with the sedentary lifestyle and hyper nutrition in developed countries, we must also recognize the continuing threat from infectious diseases, especially resistant strains or agents that are newly encountered. The relative protection we have enjoyed from many infectious diseases is no longer a foregone conclusion. At the same time we need to address multiple fronts in developing countries: historical threats from infectious agents, malnutrition, and perinatal complications, as well as emerging threats of the same sort we now see from resistant strains of infectious agents and contact with new agents, and the looming emergence and increasing importance of the chronic and degenerative diseases that are likely to follow successful programs to increase education and reduce poverty. One of the lessons of the epidemiologic transition is that interventions must fit the population and the threats to health it currently experiences, while we anticipate the changes that success in one area are likely to bring out and the new challenges that will emerge. This will require new ways of thinking that go beyond the epidemiologic transition theory.
Acknowledgements
Based on paper originally presented at Arizona State University, Mesa, AZ on February 28–29, 2008.
References
- 1.Omran AR. The Epidemiologic Transition. Milbank Mem Fund Q. 1971;49:509–538. [PubMed] [Google Scholar]
- 2.Armelagos GJ, Brown PJ, Turner B. Evolutionary, historical and political economic perspectives on health and disease. Soc Sci Med. 2005;61:755–765. doi: 10.1016/j.socscimed.2004.08.066. [DOI] [PubMed] [Google Scholar]
- 3.The Future of Public Health. Washington, DC: National Academy Press; 1988. Institute of Medicine, Committee for the Study of the Future of Public Health. [Google Scholar]
- 4.Susser M. Epidemiology in the United States after World War II: The Revolution of Technique. Epidemiologic Reviews. 1985;7:147–177. doi: 10.1093/oxfordjournals.epirev.a036280. [DOI] [PubMed] [Google Scholar]
- 5.Susser E, Susser M. Choosing a Future for Epidemiology: I. Eras and Paradigms. American Journal of Public Health. 1996;86:668–673. doi: 10.2105/ajph.86.5.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Susser E, Susser M. Choosing a Future for Epidemiology: II. From Black Box to Chinese Boxes and Eco-epidemiology. American Journal of Public Health. 1996;86:674–677. doi: 10.2105/ajph.86.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krieger N. Epidemiology and the Web of Causation: Has Anyone Seen the Spider? Soc Sci Med. 1994;39:887–903. doi: 10.1016/0277-9536(94)90202-x. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine, Committee on Assuring the Health of the Public in the 21st Century. The Future of the Public's Health in the 21st Century; Washington, DC. National Academy Press; 2003. [Google Scholar]
- 9.Caldwell JC. Population Health in Transition. Bull World Health Organ. 2001;79:159–160. [PMC free article] [PubMed] [Google Scholar]
- 10.Pearson TA. Education and Income: Double-Edged Swords in the Epidemiologic Transition of Cardiovascular Disease. Ethnicity and Disease. 2003;13:S2-158–S2-163. [PubMed] [Google Scholar]
- 11.Gage TB. Are Modern Environments Really Bad for Us?:Revisiting the Demographic and Epidemiologic Transitions. Yrbk Phys Anthropol. 2005;48:96–117. doi: 10.1002/ajpa.20353. [DOI] [PubMed] [Google Scholar]
- 12.Heuveline P, Guillot M, Gwatkin DR. The Uneven Tides of the Health Transition. Soc Sci Med. 2002;55:313–322. doi: 10.1016/s0277-9536(01)00172-1. [DOI] [PMC free article] [PubMed] [Google Scholar]