Abstract
BACKGROUND
In general, ischemic colitis has a very good prognosis, but there is concern that when ischemia affects the right side of the colon in an isolated fashion, the prognosis may not be so favorable.
OBJECTIVE
The aim of this study was to compare the clinical features and outcomes of ischemia isolated to the right side of the colon with those of ischemia involving other areas of the colon.
METHODS
A retrospective study was undertaken of patients with colon ischemia hospitalized at the Moses and Weiler Divisions of the Montefiore Medical Center during the interval 1998–2005. Patients were identified using computerized searches of ICD-9 codes for colon ischemia and were divided into two groups: those with isolated right colon ischemia (IRCI) and those with colon ischemia not involving the right colon in an isolated fashion (non-IRCI). Only patients with biopsy-proven ischemic colitis were entered into our study.
RESULTS
A total of 273 cases of biopsy-proven ischemic colitis were identified, of which 71 (26.0%) were isolated to the right side. Of these IRCI cases, 59.2% had an unfavorable outcome compared with 17.3% of cases of non-ICRI: 54.9% of IRCI patients required surgery compared with 10.9% of non-IRCI patients; mortality in patients with IRCI was 22.5% compared with 11.9% in patients with non-IRCI.
CONCLUSIONS
A total of 273 cases of biopsy-proven ischemic colitis were identified of which 71 (26.0%) involved only the right side. Patients with IRCI had a worse outcome than those with colon ischemia involving other colon regions, including a fivefold need for surgery and a twofold mortality.
INTRODUCTION
Colon ischemia accounts for more than half of all cases of gastrointestinal ischemia and at our tertiary care center it is the primary diagnosis in approximately 3 per 1,000 hospital admissions. Colon ischemia has many causes, and occurs most often in the absence of major vessel occlusion (1); its presentations are highly variable, making diagnosis and management clinically challenging (2). Because the presentation of colon ischemia is nonspecific and patients with colon ischemia usually are not severely ill, the disease often is not diagnosed, or misdiagnosed as another occurrence such as Crohn’s disease, diverticulitis, or infectious colitis. Usual symptoms include bloody diarrhea and mild-to-moderate abdominal pain. It can affect young patients, although more frequently it is seen in the elderly with a peak incidence in the 7th decade. Women are affected more than men. Clinically, the disease process varies from self-limiting and transient to fulminant and life-threatening (1). In the more common and milder form of the disease, only the mucosa and submucosa are affected and most of these occurrences resolve spontaneously or with just conservative measures. In contrast, the severe forms of colon ischemia are marked by transmural necrosis of the bowel, often requiring surgery and frequently leading to death (3).
Any part of the colon may be affected by ischemia, and isolated right colon ischemia (IRCI) has been reported to occur in about 10% of cases (4). IRCI, however, also may be the heralding event of otherwise clinically silent focal obstruction or vasoconstriction of the superior mesenteric artery (SMA), because the SMA constitutes the blood supply of both the small intestine and much of the colon, including the right side. Over many years, we have observed that several of our patients with IRCI have developed acute mesenteric ischemia within weeks of their presentation with colon ischemia; acute mesenteric ischemia has a high mortality and requires different management than does colon ischemia (5). In contrast to colon ischemia for which mesenteric angiography generally is not helpful and which responds to conservative medical treatment in most cases, acute mesenteric ischemia benefits from an aggressive diagnostic and therapeutic approach utilizing mesenteric angiography and intrarterial infusion of vasodilators in combination with surgery. The mortality rate of acute mesenteric ischemia is 70–90% when managed by surgery alone and approximately 50% when an aggressive management plan is utilized (5, 6). Thus, it can be questioned whether IRCI should be considered an emergency situation with a potentially grave prognosis just as is acute mesenteric ischemia. To date, only a few studies have documented IRCI to be among the more severe forms of colon ischemia: one showed it to be associated with hemodialysis and chronic renal failure, while the others showed it to occur with increased frequency in patients with shock (7–9); situations precipitating IRCI usually are associated with reductions in circulating blood volume, marked fluid shifts, and hypotension, thereby potentially causing SMA vasoconstriction. The purpose of this study was to compare the clinical features and outcomes of IRCI with ischemia involving other segments of the colon.
METHODS
A retrospective study was undertaken of the records of patients hospitalized with colon ischemia at the Moses and Weiler Divisions of the Montefiore Medical Center during the years 1998–2005. After appropriate IRB approval, computerized records were searched and 1,132 patients were identified with diagnoses of mesenteric ischemia or infarction, bowel ischemia or infarction, or ischemic colitis (ICD-9 codes 557.0, 557.1, and 557.9). Patients were excluded if they were younger than 20 yr of age or if they had: prior colonic resection; bowel obstruction including incarcerated hernia, volvulus, and abdominal adhesion; recent or concurrent colonic or pelvic cancer; Crohn’s disease or ulcerative colitis; or only mesenteric ischemia without colon involvement. Only biopsy-proven (colonoscopic, or at surgery or autopsy) cases of ischemic colitis were included in this study. Operations that were performed for colon ischemia included partial, hemi-, and subtotal colectomies. Patients were followed from admission until discharge, a period that ranged from 3 days to 5 months. Data on the following variables were collected for all subjects: age, sex, ethnicity, and coexisting medical conditions including cardiovascular disease, diabetes, and chronic renal failure with or without hemodialysis; presenting symptoms; radiologic and colonoscopic findings; surgical and colonoscopic biopsies; and the hospital course, especially the need for surgery and ultimate outcome. Thirty-day mortality was defined as the primary end point; surgery and the composite of surgery or death were secondary end points. Thirty-day mortality was defined as mortality occurring 30 days after the initial biopsy (either colonoscopic or surgical) that proved colon ischemia. Mortality was taken from the social security death registry using social security number matching. Data were not analyzed further to determine if there was a relationship between mortality and the extent of colon resection. Individual biopsy specimens were not re-reviewed, but rather the official pathology report was utilized for diagnostic purposes. Patients were divided into two groups based on the anatomic segment of the colon affected by ischemia: isolated right colon ischemia (IRCI) and colon ischemia not involving the right colon in an isolated fashion (non-IRCI). Multisegmental colon involvement, even when part or the entire right colon was involved, was not considered as IRCI.
First, the two groups of IRCI and non-IRCI were compared with respect to their demographic and clinical characteristics. The continuous variable, age, was compared using a t-test with equal variances. Categorical variables were compared using χ2 tests. For the zero-sum categorical variables (race and source of referral), an overall χ2 test was used. Second, the groups were compared with respect to the dichotomous outcomes: 30-day mortality, surgery, and “unfavorable” (combination of mortality or surgery). The dichotomous outcomes were tested using χ2 analysis and multivariate logistic regression was used to compare the dichotomous outcomes (mortality, surgery, and unfavorable) between the groups after adjusting for clinical characteristics. Independent variables chosen for the multivariate models included those that appeared to measure a difference between the groups on univariate analysis. Finally, survival curves were constructed for the groups using the method of Kaplan–Meier. The significance of the difference of the survival curves was tested using the log-rank test. STATA software, version 9.0 (StataCorp, College Station, TX) was used for all statistical analyses and data manipulation.
RESULTS
Patient and Group Characteristics
A total of 273 patients with colon ischemia were identified; mean age was 71.8 yr, with a range of 41–95 yr, and most were women (66.3%, P = 0.04) (Table 1). The most common reason for admission was bright red blood per rectum (BRBPR) (57.5%), although only 25.4% of patients with IRCI presented with this complaint, in comparison with 68.8% of patients with non-IRCI (P < 0.001). A total of 27.1% of patients presented with abdominal pain, a symptom that was much more characteristic of IRCI (46.5%) than non-IRCI (20.3%, P < 0.001). Nonbloody diarrhea was uncommon and seen in one patient with IRCI (1.4%) and only 5.9% of patients with non-IRCI. Most patients were admitted from home (73.1%), with smaller percentages from nursing homes or rehabilitation facilities (16.0% and 3.4%, respectively). The most common coexisting medical conditions were hypertension (72.5%), diabetes mellitus (32.2%), coronary artery disease (36.3%), and congestive heart failure (13.2%). A total of 15.4% of patients had chronic kidney disease, and 11.0% of all patients were on hemodialysis. Of all these conditions, only coronary artery disease was statistically more commonly seen in IRCI patients than in non-IRCI patients (49.3% vs 31.7%, P = 0.008). Seasonal occurrences were as follows: spring (March–April–May) 24.6%, summer (June– July–August) 24.3%, fall (September–October–November) 27.6%, and winter (December–January–February) 23.5%; none were significant (P = 0.75).
Table 1.
Characteristics of Patients With Colon Ischemia
| IRCI (N = 71) |
Non-IRCI (N = 202) |
Total CI (N = 273) |
P Value* | |
|---|---|---|---|---|
| Age (mean ± SD) | 72.1 ± 11.4 | 71.7 ± 12.6 | 71.8 ± 12.3 | 0.83† |
| Male, N (%) | 31 (43.7) | 61 (30.2) | 92 (33.7) | 0.04 |
| Race, N (%) | 0.22 | |||
| White | 21 (29.6) | 80 (39.6) | 101 (37.0) | |
| African-American | 16 (22.5) | 36 (17.8) | 52 (19.1) | |
| Hispanic | 27 (38.0) | 74 (36.6) | 101 (37.0) | |
| Asian | 0 (0.0) | 3 (1.5) | 3 (1.1) | |
| Other/Unknown | 7 (9.9) | 9 (4.5) | 16 (5.9) | |
| Site of referral, N (%) | 0.94 | |||
| Home | 52 (74.3) | 144 (72.7) | 196 (73.1) | |
| Nursing home | 10 (14.3) | 33 (16.7) | 43 (16.0) | |
| Rehabilitation facility | 2 (2.9) | 7 (3.5) | 9 (3.4) | |
| Unknown | 6 (8.6) | 14 (7.1) | 20 (7.5) | |
| Coexisting conditions, N (%) | ||||
| Hypertension | 54 (76.1) | 144 (71.3) | 198 (72.5) | 0.44 |
| Diabetes mellitus | 25 (35.2) | 63 (31.2) | 88 (32.2) | 0.53 |
| Coronary artery disease | 35 (49.3) | 64 (31.7) | 99 (36.3) | 0.008 |
| Congestive heart failure | 14 (19.7) | 22 (10.9) | 36 (13.2) | 0.06 |
| Chronic kidney disease | 15 (21.1) | 27 (13.4) | 42 (15.4) | 0.12 |
| Hemodialysis | 12 (16.9) | 18 (8.9) | 30 (11.0) | 0.06 |
| Presenting symptoms, N (%) | ||||
| Bright red blood per rectum | 18 (25.4) | 139 (68.8) | 157 (57.5) | <0.001 |
| Abdominal pain without BRBPR | 33 (46.5) | 41 (20.3) | 74 (27.1) | <0.001 |
| Diarrhea | 1 (1.4) | 12 (5.9) | 13 (4.8) | 0.12 |
IRCI = isolated right-sided colon ischemia; CI = colon ischemia.
Tested with χ2 unless otherwise noted.
t-test with equal variances.
Outcomes
Of the 273 patients, 71 (26.0%) had colon ischemia isolated to the right side. A favorable outcome was defined as one responding to medical management with resolution of symptoms. An unfavorable outcome was defined as one in which: (a) surgery was performed, (b) surgery was performed and death followed, or (c) death occurred in the absence of surgery (Table 2). Of all 273 cases of biopsy-proven ischemic colitis, 196 (71.8%) had a favorable outcome, of which 85.2% was accounted for by patients with non-IRCI and 14.8% by patients with IRCI (P < 0.001).
Table 2.
Outcomes of Patients With IRCI Compared With Non-IRCI
| IRCI | Non-IRCI | Total CI | P Value* | |
|---|---|---|---|---|
| 30-day mortality, N (%) |
16 (22.5) | 24 (11.9) | 40 (14.7) | 0.03 |
| Surgery, N (%) | 39 (54.9) | 22 (10.9) | 61 (22.3) | <0.001 |
| Unfavorable,† N (%) |
42 (59.2) | 35 (17.3) | 77 (28.2) | <0.001 |
IRCI = isolated right-sided colon ischemia; CI = colon ischemia.
χ2.
Combined end point of surgery or death within 30 days.
A total of 167 of the 202 non-IRCI patients (82.7%) had a favorable outcome, whereas 35 patients (17.3%) had an unfavorable outcome (Table 2). Of the 71 patients with IRCI, 42 (59.5%) had unfavorable outcomes. Of all patients with colon ischemia, 61 (22.3%) underwent surgery (Table 2). Proportionally more patients with IRCI underwent surgery than did those with non-IRCI (54.9% compared with 10.9%, respectively), although postsurgical mortality was similar in IRCI and non-IRCI (37.5% compared with 42.9%, P = 0.78). Overall 30-day mortality was 14.7%, including patients who died after surgery and those who died before surgery could be performed (Table 2). The mortality of patients with IRCI was 22.5% compared with a mortality of 11.9% in patients with non-IRCI (P = 0.03, Table 2).
DISCUSSION
In our medical center, the incidence of colon ischemia is about 3 per 1,000 hospital admissions, a number that has remained relatively constant over the years of this study period. The 26.0% frequency of IRCI, however, was much higher than the 10% previously reported and accounted for one quarter of all cases of colon ischemia (Table 1). It is possible, however, that this greater frequency is inflated because a referral bias existed to increase the proportion of sicker patients with IRCI admitted to the hospital. In view of the severity of comorbid diseases in these hospitalized patients, it is equally conceivable that the frequency of IRCI in an outpatient or outpatient and inpatient study cohort might be less than the 26.0% we documented.
There was no difference in presenting ages or sites of referral in patients with IRCI compared with those who had non-IRCI (Table 1). Curiously, there were approximately twice as many women than men presenting with colon ischemia without regard to the segment of affected colon (66.3% compared with 33.7%, P = 0.04). Patients with IRCI presented in a different manner than did patients with non-IRCI. IRCI more commonly presented with abdominal pain without BRBPR, whereas non-IRCI presented with BRBPR and mild-to-moderate abdominal pain (Table 1). These findings were statistically (P < 0.001) and clinically significant. Severe abdominal pain is a classic feature of the presentation of acute mesenteric ischemia, but in colon ischemia usually is only mild-to-moderate in severity and overshadowed by rectal bleeding. BRBPR, long considered a hallmark of colon ischemia, is uncommon when the ischemic process is confined to the right side of the colon.
IRCI has been reported to complicate low flow states such as hypotension and sepsis, chronic kidney disease, and hemodialysis, presumably secondary to intravascular fluid shifts. Our findings support this teaching. Whereas the incidences of hypertension and diabetes mellitus were not significantly different between IRCI and non-IRCI patient groups (76.1% vs 71.3%, 35.2% vs 31.2%, respectively), coronary artery disease was more prevalent in patients with IRCI compared with patients having non-IRCI (P = 0.008, Table 2). The incidence of chronic kidney disease and hemodialysis was not statistically different among patients with IRCI compared with non-IRCI when both hospital sites were considered in the aggregate. Subgroup analysis, however, revealed that at the Moses Division of Montefiore Medical Center, the incidence of chronic kidney disease was significantly different in patients with IRCI compared with those with non-IRCI; more than twice as many patients with IRCI had chronic kidney disease (25.9% compared with 12.0%, P = 0.01; data not shown). Moreover, approximately threefold more patients with IRCI were on hemodialysis compared with patients with non-IRCI (20.4% vs 8.4%, P = 0.02; data not shown). Because hemodialysis involves potentially large intravascular fluid shifts, thus predisposing to low flow states, it is reasonable to expect IRCI more frequently in these patients than non-IRCI. The differences in prevalence of hemodialysis and IRCI between the two sites can perhaps simply be explained by the fact that there are more patients on hemodialysis and a greater severity of disease at the Moses campus than at the Weiler campus.
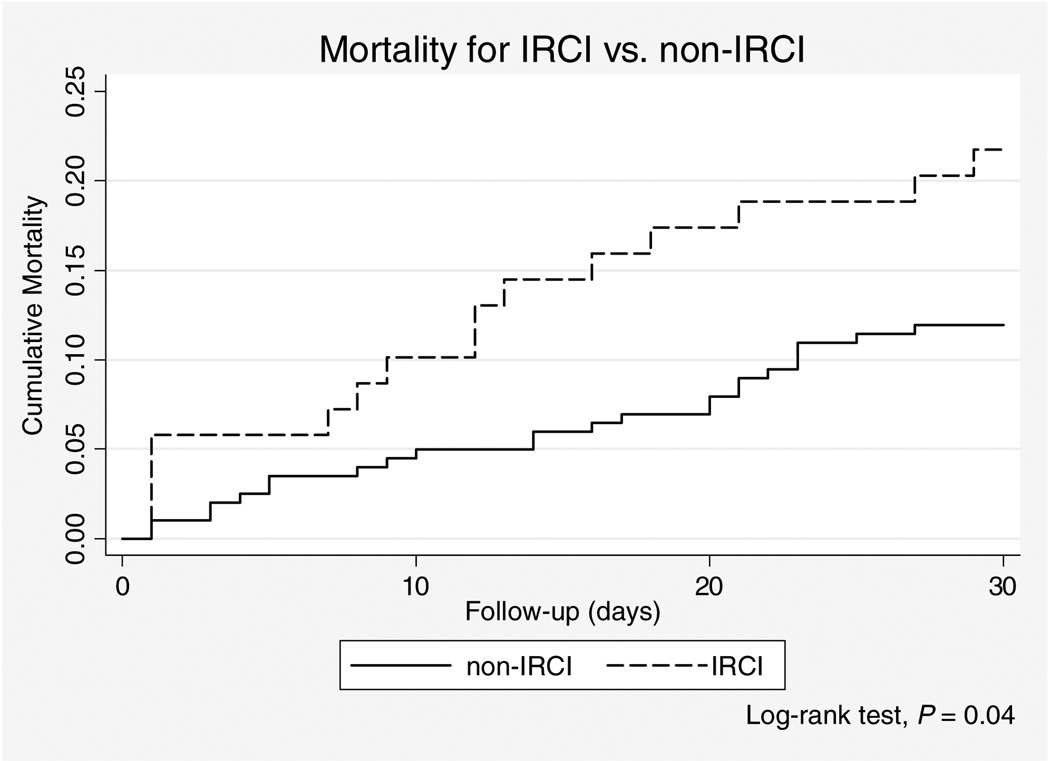
Although some studies have evaluated the severity of the ischemic insult in cases of IRCI and some have suggested there may be differences in outcomes of patients with IRCI compared with patients having with non-IRCI (7, 10–12), ours is the first study that compares the outcomes of these patient groups. Most patients with ischemic colitis had a favorable outcome (71.8%). Patients with IRCI, however, had a significantly worse outcome compared with patients who had non-IRCI (59.2% vs 17.3%, respectively, P < 0.001) (Table 2). These worse outcomes included surgery, death, or the combined end point of surgery or death. Patients with IRCI had a fivefold higher frequency of surgery than did patients with non-IRCI (54.9% vs 10.9%, P < 0.001; Table 2). Patients with IRCI also had a twofold higher mortality than did patients with non-IRCI (22.5% vs 11.9%, P = 0.03; Table 2). The odds ratio (OR) for surgery was 9.97 for patients with IRCI compared with patients having non-IRCI. After adjustment for baseline differences between the populations, the association between IRCI and mortality remained strong (OR 9.83) and significant (Table 3). Although patients with IRCI underwent surgery more frequently than did patients with non-IRCI, postoperative mortality rates were similar in IRCI patients and patients with non-IRCI (37.5% vs 42.9%, P = 0.78), suggesting that the higher mortality rate of IRCI is explained by the nature of the disease itself. The adjusted odds ratio for mortality was 1.61 for patients with IRCI compared with patients having non-IRCI, demonstrating a significant association between IRCI and mortality (Table 3). Furthermore, the adjusted odds ratio for unfavorable outcomes for patients with IRCI compared with patients having non-IRCI is 6.70, supporting our hypothesis that patients with IRCI have a worse prognosis (Table 3). Similarly, the Kaplan–Meier 30-day mortality curves further demonstrate that there is a clinical and statistical difference in outcomes among patients with IRCI compared with those having non-IRCI; patients with IRCI have a higher mortality (Fig. 1).
Table 3.
Odds Ratios for Outcomes of Patients With IRCI Compared With Non-IRCI
| Unadjusted Odds Ratio* (95% CI) |
Adjusted Odds Ratio*† (95% CI) |
|
|---|---|---|
| 30-Day mortality | 2.15 | 1.61 |
| (1.06–4.32) | (0.76–3.41) | |
| Surgery | 9.97 | 9.83 |
| (5.24–18.98) | (5.03–19.24) | |
| Combined | 6.99 | 6.70 |
| (3.85–12.70) | (3.57–12.58) |
Odds ratio for event in IRCI versus non-IRCI.
Adjusted for presence of coronary artery disease, congestive heart failure, hemodialysis.
Figure 1.
Kaplan–Meier curves for IRCI compared with non-IRCI.
It has been demonstrated that right colon involvement is associated with more severe forms of colon ischemia and occurs more frequently in patients on hemodialysis (8). These findings also were true among patients at one of the campuses of our medical center. In comparison with the unfavorable outcomes seen in 28.2% of all patients with colon ischemia, 17.3% of patients with non-IRCI, and 59.2% of patients with IRCI, the prognosis of patients with colon ischemia who were on hemodialysis was significantly worse (data not shown). Of all 25 patients with colon ischemia on hemodialysis, 13 (52.0%) had an unfavorable outcome; this is more than three times that of patients with colon ischemia not on hemodialysis (52.0% vs 16.8%, P < 0.001; data not shown). Further analysis of this group of patients on hemodialysis and with colon ischemia showed that 28.6% of the patients with non-IRCI and 81.8% of the patients with IRCI had unfavorable outcomes (P = 0.02; data not shown). This study clearly shows that patients on hemodialysis who develop IRCI have a higher morbidity than those who develop non-IRCI. These data support the adage that patients with right-sided colon ischemia have worse outcomes if they are on hemodialysis (8).
It has been shown that patients with IRCI have more severe forms of ischemic injury to the colon, but this is the first time that the outcomes of these patients have been studied. Overall, patients with IRCI had a higher need for surgery and a higher mortality than patients with colon ischemia affecting other segments of the colon or the right colon simultaneously with other segments. This, coupled with our findings that patients with IRCI do not typically present with the classic symptom of bright red blood per rectum, but rather with nonspecific abdominal pain, sets up a challenging clinical scenario. Given the high morbidity and mortality of IRCI and the vague presenting symptoms, early diagnosis and aggressive management is critical. It has been theorized that the reason why patients with IRCI do so poorly is because of insufficient collateralization and blood flow to the right side of the colon. Alternatively, it is possible that IRCI may represent the herald presentation of an acute superior mesenteric artery occlusion and thus its outcome reflects that of acute mesenteric ischemia. We are currently investigating this possibility.
While we report the incidence of IRCI as a quarter of all admissions with ischemic colitis, we only studied patients with biopsy-proven ischemia. Thus, our study population represents only a portion of all cases of ischemic colitis. Further studies that are currently underway broaden our study population and review outcomes in larger numbers of patients with IRCI and non-IRCI diagnosed clinically as well as by pathology. Nevertheless, IRCI remains a disease that presents in association with certain comorbidities (coronary artery disease, chronic kidney disease, and hemodialysis), has a presentation not unlike acute mesenteric ischemia (abdominal pain), and has a previously unrecognized high incidence and mortality, especially in patients on hemodialysis.
STUDY HIGHLIGHTS.
What Is Current Knowledge
Isolated right colon ischemia (IRCI) accounts for 10% of all cases of colon ischemia.
Colon ischemia typically presents with bloody diarrhea.
Right-sided colon involvement is associated with severe colitis.
What Is New Here
IRCI accounts for 26% of biopsy-proven cases of colon ischemia.
Patients with IRCI present with abdominal pain, not bloody diarrhea.
IRCI has 5× morbidity and 2× mortality than non-IRCI.
Patients on hemodialysis who develop IRCI have an especially unfavorable outcome.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Igal Khorshidi for assistance on the data collection.
Footnotes
CONFLICT OF INTEREST
Guarantor of the article: Lawrence J. Brandt, M.D.
Specific author contributions: John Sotiriadis: data acquisition and compilation, drafting and editing of manuscript. Lawrence J. Brandt: study conceptualization, manuscript preparation and editing, general supervisor. Daniel S. Behin: data acquisition. William N. Southern: statistical analyses.
Financial support: None.
Potential competing interests: None.
REFERENCES
- 1.Brandt LJ. Intestinal ischemia. In: Feldman M, Friedman L, Brandt LJ, editors. Sleisenger & Fordtran’s gastrointestinal and liver disease: Pathophysiology, diagnosis, management. Philadelphia: Elsevier; 2006. pp. 2563–2586. [Google Scholar]
- 2.Sreenarasimhaiah J. Diagnosis and management of ischemic colitis. Curr Gastroenterol Rep. 2005;7:421–426. doi: 10.1007/s11894-005-0013-1. [DOI] [PubMed] [Google Scholar]
- 3.Mitsudo S, Brandt LJ. Pathology of intestinal ischemia. Surg Clin North Am. 1992;72:43–63. doi: 10.1016/s0039-6109(16)45627-6. [DOI] [PubMed] [Google Scholar]
- 4.Brandt LJ, Boley SJ. Colonic ischemia. Surg Clin North Am. 1992;72:203–229. doi: 10.1016/s0039-6109(16)45635-5. [DOI] [PubMed] [Google Scholar]
- 5.Robert JH, Mentha G, Rohner A. Ischaemic colitis: Two distinct patterns of severity. Gut. 1993;34:4–6. doi: 10.1136/gut.34.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brandt LJ, Boley SJ. AGA technical review on intestinal ischemia. American Gastrointestinal Association. Gastroenterology. 2000;118:954–968. doi: 10.1016/s0016-5085(00)70183-1. [DOI] [PubMed] [Google Scholar]
- 7.Guttormson NL, Bubrick MP. Mortality from ischemic colitis. Dis Colon Rectum. 1989;32:469–472. doi: 10.1007/BF02554499. [DOI] [PubMed] [Google Scholar]
- 8.Flobert C, Cellier C, Berger A, et al. Right colonic involvement is associated with severe forms of ischemic colitis and occurs frequently in patients with chronic renal failure requiring hemodialysis. Am J Gastroenterol. 2000;95:195–198. doi: 10.1111/j.1572-0241.2000.01644.x. [DOI] [PubMed] [Google Scholar]
- 9.Sakai L, Keltner R, Kaminski D. Spontaneous and shock-associated ischemic colitis. Am J Surg. 1980;140:755–760. doi: 10.1016/0002-9610(80)90111-7. [DOI] [PubMed] [Google Scholar]
- 10.Longo WE, Ballantyne GH, Gusberg RJ. Ischemic colitis: Patterns and prognosis. Dis Colon Rectum. 1992;35:726–730. doi: 10.1007/BF02050319. [DOI] [PubMed] [Google Scholar]
- 11.Longo WE, Ward D, Vernava AM, 3rd, et al. Outcome of patients with total colonic ischemia. Dis Colon Rectum. 1997;40:1448–1454. doi: 10.1007/BF02070711. [DOI] [PubMed] [Google Scholar]
- 12.Landreneau RJ, Fry WJ. The right colon as a target organ of nonocclusive mesenteric ischemia. Case report and review of the literature. Arch Surg. 1990;125:591–594. doi: 10.1001/archsurg.1990.01410170037007. [DOI] [PubMed] [Google Scholar]