Abstract
The role of maternal stress during pregnancy remains a focus of academic and clinical inquiry, yet there are few instruments available that measure pregnancy-specific contributors to maternal psychological state. This report examines the psychometric properties of an abbreviated version of the Pregnancy Experience Scale (PES) designed to evaluate maternal appraisal of positive and negative stressors during pregnancy. The PES-Brief consists of the top 10 items endorsed as pregnancy hassles and 10 pregnancy uplifts from the original scale. The PES-Brief was administered to 112 women with low risk, singleton pregnancies five times between 24 and 38 weeks gestation. Scoring includes frequency and intensity measures for hassles and uplifts, as well as composite measures for the relation between the two. Internal reliability, test-retest reliability, and convergent validity were comparable to the original version. The PES-Brief provides an economical source of information on stress appraisal and emotional valence towards pregnancy.
Keywords: Pregnancy stress, anxiety, Uplifts, Hassles, Questionnaire
Research on potential effects of maternal psychological distress on the developing fetus, pregnancy, and resultant offspring remains a topic of great academic, clinical and public interest [1-3]. Of particular challenge is to gear research towards measurement that captures the full experience of the pregnant woman [4]. Pregnancy is a unique life experience that generates a wide range of concerns that are not measured in general instruments designed to assess generalized distress [5-10]. In addition, the focus on elements of psychological distress during pregnancy, centering on stress and anxiety, obscures the role of positive emotions generated by pregnancy and provides little information on their potential role in fostering good pregnancy outcomes. This shift in orientation coincides with the increasing academic interest in delineating the role of positive psychology on health [11].
Several years ago, in response to these issues, we introduced the Pregnancy Experience Scale (PES) [12]. The scale was developed to measure maternal appraisal of exposures to daily, ongoing hassles and uplifts that are specific to pregnancy and included 41 items, each rated for both hassles and uplifts. Since publication of that scale, a number of investigators have requested a shorter version that could be administered in less time. In addition, the basic task demand of the PES requiring each item to be rated along both negative and positive dimensions was determined to be difficult to implement in some populations, particularly those involving lower levels of literacy. To this end, the PES-Brief was developed, consisting of the top 10 endorsed hassles and uplifts generated by the full scale. The purpose of this report is to examine the psychometric integrity of this abbreviated version, and to compare that to the original scale.
Methods
Participants
Participants were 112 volunteer healthy women with low risk pregnancies who responded to flyers or were referred by word of mouth. Eligibility was restricted to non-smoking women with normally progressing pregnancies carrying singleton fetuses. The sample represents a relatively mature population (M age = 31.2 years, sd = 4.6, range 21 to 45) of well-educated women (M years education = 17.2 years, sd = 2.1; 4.5% high school diploma; 7.2% some college; 32.1% graduates of 4-year college; 36.6% masters coursework or degrees; 19.6% medical or academic doctoral degree). Most were non-Hispanic white (79.5%); the remainder was African-American (13.4%), Hispanic or Asian (7.1%). Most participants were married (91.1%) and nulliparous (72.3%). Sociodemographic characteristics of this sample are comparable to the cohorts that comprised the full PES report (averaged across both cohorts: M age = 30.6; M years education = 16.5, 80% non-Hispanic white; 94% married; 60% nulliparous).
Study Design
The data reported here were part of a larger study designed to evaluate effects of maternal emotion on fetal development commencing mid-way through pregnancy. Women participated in 5 visits across the 3rd trimester with staggered enrollment commencing at 24, 25, or 26 weeks gestation. Subsequent visits occurred every 3 weeks, with the final visit occurring at 36, 37, or 38 weeks, respectively. Four self-administered psychosocial questionnaires were completed at the start of each visit. The study was approved by the local Institutional Review Board and all participants provided informed consent.
Pregnancy Experiences Scale- Brief Version (PES-Brief)
This scale is a shortened version of the Pregnancy Experiences Scale (PES), a measure of maternal exposures to daily, ongoing uplifts and hassles specific to pregnancy, modeled on the general Hassles and Uplifts Scale [13]. The full PES consists of a list of 41 items each rated on a 4-point Likert scale for both uplifts (how much the item makes the participant feel “happy, positive, or uplifted”) and hassles (how much item makes the participant feel “unhappy, negative, or upset”). A prior report details the internal reliability, stability, and convergent and discriminant validity of the original [12]. The PES-brief (see Appendix) includes the ten most frequently endorsed uplifts and ten most frequently endorsed hassles, as detailed in that report, each rated from 0 (not at all) to 3 (a great deal). Unlike in the original PES, each item in the PES-Brief is rated along only one dimension (i.e., as either a hassle or an uplift). Scoring yields six scores. These are: the frequency of hassles and the frequency of uplifts, calculated by counting the number of items that are endorsed with values greater than 0; the intensity of hassles and the intensity of uplifts, calculated as the sum of scale scores (1 to 3) divided by hassles or uplifts frequency; and two hassles:uplifts ratio scores computed by dividing hassles frequency scores by uplifts frequency scores and dividing hassles intensity scores by uplifts intensity scores. These ratio scores were implemented to measure the affective valence towards the pregnancy.
State-Trait Anxiety Inventory (STAI-Y2)
The Spielberger Anxiety Scales [14] are among the most commonly used and extensively validated self-administered measures of anxiety. The Y-2 scale used in this study is trait-based with items that describe more persistent attributes (e.g., “I have disturbing thoughts”). Twenty 4-point items are included, reversed as necessary, and summed such that higher scores indicate greater trait anxiety.
Center for Epidemiologic Studies Depression Scale (CES-D)
Depressive symptomatology was assessed using the Center for Epidemiological Studies Depression Scale (CES-D) [15]. The CES-D includes 20 depressive symptoms evaluated along 4-point (0-3) scales (e.g, “I felt depressed”, “I had crying spells”) reported for the period of the prior week. It has been widely applied during pregnancy and has an extensive validity and reliability history.
World Health Organization Well-being Index (WHO-5)
The WHO-5 is a 5-item scale, shortened from a longer version, developed to assess general psychological well-being and quality of life [16]. Items (e.g., I have felt cheerful and in good spirits) are rated on 6-point scales ranging from “all of the time” to “none of the time”; higher scores indicate greater well-being. A number of reports have established high levels of reliability and validity [17,18].
Data analysis
Data were grouped by participant visit as follows: visit 1, 24-26 weeks gestation; visit 2, 27-28 weeks; visit 3, 29 to 31 weeks; visit 4, 32 to 35 weeks; and visit 5, 36 to 38 weeks. Internal reliability was evaluated using Cronbach's alpha. The internal reliability of the PES-Brief was then compared to a criterion value calculated using the Spearman-Brown prophecy formula. This formula incorporates the alpha value from the original full PES and adjusts it by the expected alpha based solely on the exclusion of items in the short-form. The criterion value is the minimum internal reliability required for the short form to be considered an acceptable substitute to the full scale. Repeated measures analysis of variance was used to assess change in PES-Brief scores over time. Test-retest stability and associations between hassles and uplifts were evaluated using Pearson correlations. Convergent validity was evaluated using Pearson correlations between PES-Brief scores and other concurrently administered psychosocial scales.
Results
Item analysis and internal reliability
Table 1 lists the item descriptive statistics at visit 3 (gestational age 30-32 weeks). This gestational period was selected to provide comparability to the original report of the full sample [12]. Two items were designated as uplifts by 100% of participants; the most frequently nominated hassle was less consistently endorsed (88%). In general, uplifts were more consistently endorsed than hassles (84 to 100% vs 47 to 88%), and with greater intensity (item means: 2.12 to 2.76 vs 0.68 to 1.21).
Table 1.
PES-Brief item description (n = 94).
| % | M | SD | |
|---|---|---|---|
| Uplifts | |||
| “How much have each of the following made you feel happy, positive, or uplifted?” | |||
| How much the baby is moving | 100 | 2.76 | 0.50 |
| Thinking about the baby's appearance | 100 | 2.61 | 0.64 |
| Feelings about being pregnant at this time | 99 | 2.45 | 0.65 |
| Courtesy/assistance from others because you are pregnant | 97 | 2.27 | 0.89 |
| Comments from others about your pregnancy/appearance | 97 | 2.23 | 0.87 |
| Visits to obstetrician/midwife | 96 | 2.27 | 0.86 |
| Making or thinking about nursery arrangements | 96 | 2.24 | 0.89 |
| Discussions with spouse about pregnancy/childbirth issues | 95 | 2.27 | 0.89 |
| Spiritual feelings about being pregnant | 93 | 2.28 | 0.95 |
| Discussions with spouse about baby names | 84 | 2.12 | 1.13 |
| Hassles | |||
| “How much have each of the following made you feel unhappy, negative, or upset?” | |||
| Normal discomforts of pregnancy (heartburn, incontinence) | 88 | 1.21 | 0.75 |
| Getting enough sleep | 83 | 1.20 | 0.80 |
| Ability to do physical tasks/chores | 79 | 1.19 | 0.87 |
| Thinking about your labor and delivery | 77 | 1.20 | 0.91 |
| Your weight | 69 | 1.03 | 0.92 |
| Body changes due to pregnancy | 69 | 0.95 | 0.86 |
| Thoughts about whether the baby is normal | 67 | 1.05 | 0.94 |
| Clothes/shoes don't fit | 63 | 0.95 | 0.93 |
| Physical intimacy | 53 | 0.70 | 0.80 |
| Concerns about physical symptoms (pain, spotting, etc.) | 47 | 0.68 | 0.87 |
Internal reliability was high for both the uplifts (α= 0.82) and the hassles (α= 0.83) subscales. The Spearman-Brown prophecy formula generated a minimum required alpha coefficient of 0.71 for uplifts (full PES α= 0.91) and 0.82 for hassles (full PES α= 0.95), based on a reduction from 41 to 10 items for each scale. Both of the observed internal reliability values exceed these criterion values, indicating the internal reliability of the PES-Brief is psychometrically comparable to the full PES scale.
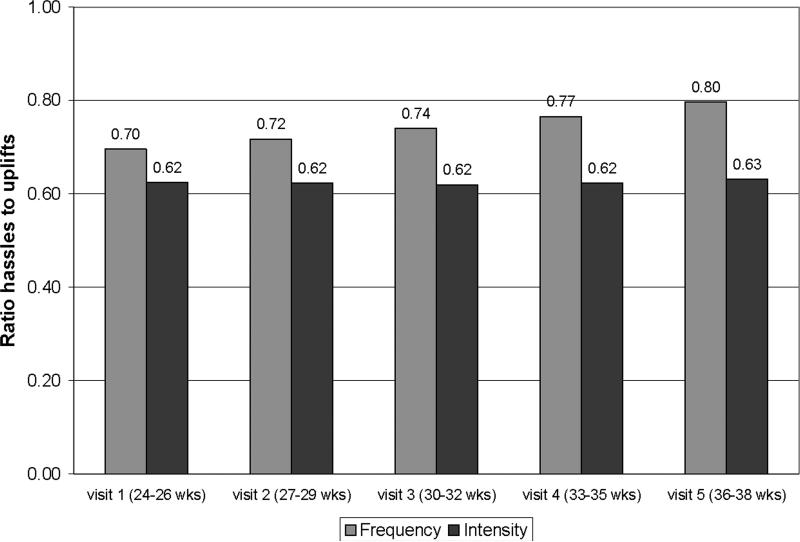
PES descriptive values
Table 2 shows the mean frequency and intensity scores for hassles and uplifts. Paired t-tests indicated significantly greater uplift frequency and intensity relative to hassle frequency and intensity at each gestational period (all ts, p < .001). This is confirmed by the values for the ratio scores of hassles to uplifts presented in Figure 1; values less than 1.0 indicate greater uplifts relative to hassles for each measure. There was no change in either the frequency of uplifts or the intensity of hassles over time. However, uplifts intensity increased (F (4,216) = 3.33, p < .01) as did hassles frequency (F (4,208) = 3.68, p < .01). Neither ratio score changed over gestation. There were no main effects for maternal parity; however there was a significant interaction for uplifts intensity, with nulliparous women reporting modestly increasing uplift intensity as compared to diminishing intensity for primiparous women (F (4,212) = 2.82, p < .05).
Table 2.
PES-Brief frequency and intensity scale*
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | |
|---|---|---|---|---|---|
| 24-26 wks | 27-29 wks | 30-32 wks | 33-35 wks | 36-38 wks | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Frequency Hassles | 6.54 (2.32) | 6.62 (2.29) | 7.02 (2.30) | 7.18 (2.56) | 7.56 (2.24) |
| Frequency Uplifts | 9.48 (1.00) | 9.48 (1.13) | 9.55 (0.81) | 9.45 (1.07) | 9.62 (0.89) |
| Intensity Hassles | 1.37 (0.43) | 1.37 (0.43) | 1.42 (0.48) | 1.40 (0.46) | 1.43 (0.43) |
| Intensity Uplifts | 2.31 (0.47) | 2.34 (0.46) | 2.44 (0.45) | 2.38 (0.48) | 2.40 (0.46) |
ns vary per visit as follows: visit 1 = 107; visit 2 = 100; visit 3 = 94; visit 4 = 101; visit 5 = 87.
Figure 1.
Combined hassles/uplifts intensity and frequency scores reflecting overall emotional valence to pregnancy. Scores below 1.00 indicate greater uplifts relative to hassles.
Test-retest stability
Test-retest correlations for frequency and intensity scores are presented in Tables 3a and 3b. Average associations for each measure were similar: uplifts frequency, r = 0.63; uplifts intensity, r = 0.73; hassles frequency, r = 0.66; hassles intensity, r = 0.63. Paired associations among ratio scores (not shown) were of similar consistency and magnitude (e.g., rs range from 0.46 to 0.67, ps < .001, for frequency ratio and from 0.56 to 0.82 for intensity ratio, ps < .001); average correlations were rs = .59 and .71, respectively.
Table 3a.
Test-retest stability of PES-Brief uplifts correlations over time
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | |
|---|---|---|---|---|---|
| Visit 1 | . | 0.64 | 0.53 | 0.44 | 0.39 |
| Visit 2 | 0.71 | . | 0.79 | 0.71 | 0.59 |
| Visit 3 | 0.69 | 0.74 | . | 0.71 | 0.76 |
| Visit 4 | 0.69 | 0.69 | 0.76 | . | 0.73 |
| Visit 5 | 0.68 | 0.70 | 0.79 | 0.88 | . |
Note. Correlations for uplifts frequency are presented above the diagonal; correlations for uplifts intensity are presented below the diagonal. All ps < .0001.
Table 3b.
Test-retest stability of PES-Brief hassles correlations over time
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | |
|---|---|---|---|---|---|
| Visit 1 | . | 0.70 | 0.53 | 0.67 | 0.60 |
| Visit 2 | 0.56 | . | 0.65 | 0.73 | 0.66 |
| Visit 3 | 0.56 | 0.77 | . | 0.70 | 0.61 |
| Visit 4 | 0.50 | 0.67 | 0.73 | . | 0.74 |
| Visit 5 | 0.45 | 0.68 | 0.68 | 0.73 | . |
Note. Correlations for hassles frequency presented above the diagonal; correlations for hassles intensity are presented below the diagonal. All ps < .0001.
Test-retest stability of the full PES instrument was measured in cohorts with 6 week intervals between tests. To compare stability of the two scales, correlations of PES-brief tests with 6 week intervals were examined. Average correlations were comparable between the PES-brief and full PES (e.g., uplifts frequency, r = 0.67 vs r = 0.71; uplifts intensity, r = 0.72 vs r = 0.75; hassles frequency, r = 0.62 vs r = 0.77; hassles intensity, r = 0.64 vs r = 0.69, between the brief and full versions, respectively).
Convergent and discriminant validity: Associations with other psychosocial measures
Correlations between PES scores and the other psychosocial measures are displayed in Table 4. All scale scores, with the exception of frequency uplifts, showed statistically significant associations in the expected directions with the STAI, CES-D, and WHO at each study visit.
Table 4.
Concurrent validity: Correlations between PES, STAI, CES-D, and WHO scores
| Visit 1 | Visit 2 | Visit 3 | Visit 4 | Visit 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STAI |
CES-D |
WHO |
STAI |
CES-D |
WHO |
STAI |
CES-D |
WHO |
STAI |
CES-D |
WHO |
STAI |
CES-D |
WHO |
|
| Frequency Hassles | 0.27** | 0.36 | −0.34 | 0.40 | 0.38 | −0.38 | 0.40 | 0.35 | −0.35 | 0.38 | 0.40 | −0.39 | 0.34 | 0.39 | −0.39 |
| Frequency Uplifts | 0.03† | −0.06† | 0.09† | −0.16† | −0.19† | 0.16† | −0.25* | −0.23* | 0.27** | −0.34 | −0.32 | 0.26** | −0.13† | −0.11† | 0.03† |
| Intensity Hassles | 0.40 | 0.44 | −0.36 | 0.54 | 0.47 | −0.51 | 0.56 | 0.57 | −0.53 | 0.59 | 0.66 | −0.59 | 0.44 | 0.55 | −0.58 |
| Intensity Uplifts | −0.20* | −0.33** | 0.29** | −0.24* | −0.21* | 0.27** | −0.45 | −0.35 | 0.42 | −0.37 | −0.29** | 0.33 | −0.46 | −0.30** | 0.30** |
| Frequency Ratio | 0.27** | 0.37 | −0.38 | 0.53 | 0.49 | −0.48 | 0.47 | 0.41 | −0.41 | 0.51 | 0.49 | −0.46 | 0.39 | 0.40 | −0.37 |
| Intensity Ratio | 0.44 | 0.55 | −0.47 | 0.59 | 0.54 | −0.57 | 0.65 | 0.62 | −0.59 | 0.66 | 0.67 | −0.61 | 0.56 | 0.54 | −0.55 |
ns
p < .05
p < .01
all others p < .001.
Discussion
These findings support the psychometric reliability and validity of a shortened form of the Pregnancy Experience Scale. Internal reliability alphas were modestly lower in the shortened version than in the original (i.e., low .80's here versus low .90's in the original), despite the reduction of items constituting each score by over 75%. Test-retest reliability remained high and comparable to the original scale. Like the original, the PES-Brief revealed that pregnant women rate the intensity and frequency of pregnancy-specific uplifts higher than their experience of pregnancy-specific hassles. The average ratio of hassles to uplift frequency was identical to the original report (M = .75), while that for intensity was slightly more positive (M = .62).
The current results extend convergent validity information from the original report to include a measure of well-being, the WHO-5, as well as provide replication of associations with the STAI and CES-D which were previously collected at only a single time point. Results indicate significant, positive associations between PES-Brief hassles (frequency and intensity) and emotional valence (i.e., ratio scores) with both anxiety and depressive symptoms at each of the 5 gestational age periods of comparable or higher correlation magnitude than in the report of the original scale. When significant associations between the STAI or CES-D and uplift scores were detected, these were negative in direction. Finally, WHO-5 scores were negatively associated with PES-Brief hassles and ratio scores at each visit and positively associated with uplifts scores at with both uplift scores at most visits.
As in the original report, most PES measures showed little change over the second half of gestation. While the results indicate an increase in hassle frequency as well as uplifts intensity, these findings must be tempered by constraints of repeated measures analysis of variance, which excludes cases with any missing data points from the analysis. However, application of hierarchical linear modeling to these data, using each gestational age data point between 24 and 38 weeks gestation, confirmed the increase in uplift intensity but not hassle frequency [19].
There are a number of on-going studies employing the PES-Brief in a variety of populations. Comorbidity of depressive and anxiety disorders was uniquely associated with significantly more negative emotional valence towards pregnancy (i.e., intensity ratio scores) [20] and emotional valence as indexed through PES-Brief ratio scores has also been reported to be negatively associated with attachment security [21]. There has also been confirmation that an association between higher ratio scores are associated with higher levels of fetal motor activity, originally reported using the original, full scale [22], has recently been confirmed using the PES-Brief [19].
In summary, the PES-Brief provides a short but reliable and valid assessment of maternal perception of both the joys and hassles of pregnancy. Its psychometric properties, including internal and test-retest reliability, and convergent validity, are comparable to those of the original scale, which required double scoring of 41 items. In selecting the original PES versus the PES-Brief, we suggest that the PES might be most useful when the research focus is geared at more comprehensively describing maternal pregnancy-specific stress or emotional orientation, but that the PES-Brief is a sufficient measure of pregnancy-specific stress or affect when such measurement is desirable within a battery of psychosocial assessment.
Acknowledgements
This research was supported by a National Institutes of Health/National Institute of Child Health and Human Development (R01 HD27592) award to the first author. We thank the generous and diligent participation of our study families.
Appendix
Pregnancy Experience Scale
Below are 10 items that you may consider to be uplifting aspects of your pregnancy and 10 items that may be less appealing. Please circle the degree to which each item affects you now.
| 0 = Not at all | 1 = Somewhat | 2 = Quite a bit | 3 = A great deal | ||
| How much have each of the following made you feel happy, positive, or uplifted? | |||||
| 1. How much the baby is moving | 0 | 1 | 2 | 3 | |
| 2. Discussions with spouse about baby names | 0 | 1 | 2 | 3 | |
| 3. Comments from others about your pregnancy/appearance | 0 | 1 | 2 | 3 | |
| 4. Making or thinking about nursery arrangements | 0 | 1 | 2 | 3 | |
| 5. Feelings about being pregnant at this time | 0 | 1 | 2 | 3 | |
| 6. Visits to obstetrician/midwife | 0 | 1 | 2 | 3 | |
| 7. Spiritual feelings about being pregnant | 0 | 1 | 2 | 3 | |
| 8. Courtesy/assistance from others because you are pregnant | 0 | 1 | 2 | 3 | |
| 9. Thinking about the baby's appearance | 0 | 1 | 2 | 3 | |
| 10. Discussions with spouse about pregnancy/childbirth issues | 0 | 1 | 2 | 3 | |
| How much have each of the following made you feel unhappy, negative, or upset? | |||||
| 1. Getting enough sleep | 0 | 1 | 2 | 3 | |
| 2. Physical intimacy | 0 | 1 | 2 | 3 | |
| 3. Normal discomforts of pregnancy (heartburn, incontinence) | 0 | 1 | 2 | 3 | |
| 4. Your weight | 0 | 1 | 2 | 3 | |
| 5. Body changes due to pregnancy | 0 | 1 | 2 | 3 | |
| 6. Thoughts about whether the baby is normal | 0 | 1 | 2 | 3 | |
| 7. Thinking about your labor and delivery | 0 | 1 | 2 | 3 | |
| 8. Ability to do physical tasks/chores | 0 | 1 | 2 | 3 | |
| 9. Concerns about physical symptoms (pain, spotting, etc.) | 0 | 1 | 2 | 3 | |
| 10. Clothes/shoes don't fit | 0 | 1 | 2 | 3 | |
References
- 1.Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20:189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- 2.Littleton H, Breitkopf C, Berenson A. Correlates of anxiety symptoms during pregnancy and association with perinatal outcomes: A meta-analysis. Am J Obstet Gynecol. 2007;196:424–432. doi: 10.1016/j.ajog.2007.03.042. [DOI] [PubMed] [Google Scholar]
- 3.Van den Bergh B, Mulder E, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioral development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. 2005;29:237–258. doi: 10.1016/j.neubiorev.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Chandra P, Ranjan S. Psychosomatic obstetrics and gynecology - a neglected field? Curr Opin Psychiatry. 2007;20:168–173. doi: 10.1097/YCO.0b013e32801450a6. [DOI] [PubMed] [Google Scholar]
- 5.Arizmendi T, Affonso D. Stressful events related to pregnancy and postpartum. J Psychosom Res. 1987;31:743–756. doi: 10.1016/0022-3999(87)90023-7. [DOI] [PubMed] [Google Scholar]
- 6.DaCosta D, Brender W, Larouche J. A prospective study of the impact of psychosocial and lifestyle variables on pregnancy complications. J Psychosom Obstet Gynecol. 1998;19:28–37. doi: 10.3109/01674829809044218. [DOI] [PubMed] [Google Scholar]
- 7.Huizink A, Mulder E, Robles de Medina P, Visser G, Buitelaar J. Is pregnancy anxiety a distinctive syndrome? Early Hum Dev. 2004;79:81–91. doi: 10.1016/j.earlhumdev.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Kumar R, Robson KM, Smith AMR. Development of a self-administered questionnaire to measure maternal adjustment and maternal attitudes during pregnancy and after delivery. J Psychosom Res. 1984;28:43–51. doi: 10.1016/0022-3999(84)90039-4. [DOI] [PubMed] [Google Scholar]
- 9.Lobel M. Conceptualizations, measurement, and effects of prenatal maternal stress on birth outcomes. J Behav Med. 1994;17:225–272. doi: 10.1007/BF01857952. [DOI] [PubMed] [Google Scholar]
- 10.Yali A, Lobel M. Coping and distress in pregnancy: An investigation of medically high risk women. J Psychosom Obstet Gynecol. 1999;20:39–52. doi: 10.3109/01674829909075575. [DOI] [PubMed] [Google Scholar]
- 11.Seligman M, Steen T, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol. 2005;60:410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- 12.DiPietro JA, Ghera MM, Costigan KA, Hawkins M. Measuring the ups and downs of pregnancy. J Psychosom Obstet Gynecol. 2004;25:189–201. doi: 10.1080/01674820400017830. [DOI] [PubMed] [Google Scholar]
- 13.DeLongis A, Folkman S, Lazarus RS. The impact of daily stress on health and mood: Psychological and social resources as mediators. J Pers Soc Psychol. 1988;54:486–495. doi: 10.1037//0022-3514.54.3.486. [DOI] [PubMed] [Google Scholar]
- 14.Spielberger C. Manual for the State-Trait Anxiety Inventory (Form Y) Mind Garden, Inc; Palo Alto, CA: 1983. [Google Scholar]
- 15.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 16.World Health Organization, Regional Office for Europe . Well-being measures in primary health care: The DepCare Project. Stockholm, Sweden: 2008. [Google Scholar]
- 17.Bech P, Olsen L, Kjoller M, Rasmussen N. Measuring well-being rather than the absence of distress symptoms: a comparison of the SF-36 Mental health subscale and the WHO-Five Well-Being Scale. Int J Methods Psychiatr Res. 2003;12:85–91. doi: 10.1002/mpr.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Henkel V, Moehrenschlager M, Hegerl U, Moeller H, Ring J, Worret W. Screening for depression in adult acne vulgaris patients: tools for the dermatologist. J Cosmet Dermatol. 2002;1:202–207. doi: 10.1111/j.1473-2165.2002.00057.x. [DOI] [PubMed] [Google Scholar]
- 19.DiPietro JA, Kivlighan KT, Costigan KA, Henderson J, Rubin S, Shiffler DE, Pillion JP. Prenatal antecedents of newborn neurological development. Child Dev. doi: 10.1111/j.1467-8624.2009.01384.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evans L, Myers M, Monk C. Pregnant women's cortisol is elevated with anxiety and depression, but only when comorbid. Arch Womens Ment Health. 2008;11:239–248. doi: 10.1007/s00737-008-0019-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monk C, Leight K, Fang Y. Relationship between women's attachment style and perinatal mood disturbance: Implications for screening and treatment. Arch Womens Ment Health. 2008;11:117–129. doi: 10.1007/s00737-008-0005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DiPietro JA, Hilton SC, Hawkins M, Costigan KA, Pressman EK. Maternal stress and affect influence fetal neurobehavioral development. Dev Psychol. 2002;38:659–668. [PubMed] [Google Scholar]