Abstract
Type 2 diabetes occurs in special groups of children. One of the highest rates of type 2 diabetes in the world occurs in First Nation people. Screening of First Nation children has been recommended. To diagnose diabetes earlier and prevent complications in adulthood, a program of screening and primary prevention of First Nation people must begin with children. One hundred fifteen school-aged First Nation children were approached to participate in the present study, and 93% of the children completed the study. Eight (7%) of the study participants had abnormal capillary blood glucose levels, but no cases of type 2 diabetes were confirmed. Risk factors related to exercise, diet, blood pressure and body mass index were identified. The present paper describes a collaborative program with a small Paediatric Diabetic Education Center and the Beausoleil First Nation people.
Keywords: Children, Disease prevention, First Nation people, Type 2 diabetes
RÉSUMÉ :
Le diabète de type II se produit dans des groupes particuliers d’enfants. L’un des taux les plus élevés de ce type de diabète dans le monde s’observe dans les Premières nations. Le dépistage des enfants des Premières nations a été recommandé. Pour diagnostiquer le diabète plus rapidement et prévenir les complications à l’âge adulte, un programme de dépistage et de prévention primaire des communautés des Premières nations doit commencer par les enfants. Cent quinze enfants d’âge scolaire des Premières nations ont été invités à participer à la présente étude, et 93 % l’ont terminée. Huit (7 %) des participants à l’étude présentaient un taux de glucose capillaire anormal, mais aucun cas de diabète de type II n’a été confirmé. Les facteurs de risque reliés à l’exercice, au régime alimentaire, à la tension artérielle et à l’indice de poids corporel ont été repérés. Le présent article décrit un programme coopératif entre un petit centre d’éducation sur le diabète pédiatrique et la communauté des Premières nations de Beausoleil.
Significant data suggest that type 2 diabetes is a major health problem among First Nation people. The age-adjusted prevalence rate is among the highest in the world (1). To date, no effective treatment has been identified, with the exception of a program of diet and exercise, which yielded a 25% risk reduction in the incidence of diabetes over six years in one study (2). Type 2 diabetes occurs in special groups of children. Currently, it occurs in 1% to 2% of children of First Nation origin (1). Considering the drastic consequences of early-onset disease, it is considered prudent to screen these children. It is suggested that culturally appropriate, community-based intervention strategies should be developed, and that the programs should be aimed at school children and their parents. Furthermore, this approach is believed to be critical to the prevention of diabetes in future generations (1). Previous studies have indicated that programs that involve shared responsibility between medical caretakers and communities stand the best chance of success (3).
Obesity is the most important risk factor for the development of type 2 diabetes mellitus (DM), and physical inactivity is a strong predictor of both obesity and type 2 diabetes.
The rationales for youth-centred programs are many. Most life styles associated with chronic diseases, such as type 2 diabetes, are learned early in life and are well ingrained by adulthood. Many risk factors for diabetes track from childhood into adulthood, and changes in lifestyles among children can lead to improvements in their risk factor levels (2). School aged children represent captive audiences who are eager to learn new ideas and who are in the process of integrating societal norms.
OBJECTIVES
The objectives of the present study were: to initiate a collaborative effort between the medical (paediatric) community that cared for children and the community of Beausoleil First Nation, Christian Island, Ontario; to assess the prevalence of type 2 diabetes in First Nation children; and to begin an educational program on diet and exercise, with a strong community focus led by a community advisory board, the Beausoleil Diabetes School Screening Program (BDSSP).
DESIGN
Initial meetings at the Paediatric Diabetic Education Clinic, Orillia, Ontario regarding the needs of First Nation children were prompted by a review of the literature (1–19). As a paediatric team that served a large geographic area, the authors recognized that there were a number of First Nation communities in the catchment area that may be interested in the authors’ initiatives aimed at both screening for type 2 diabetes and long term prevention. The authors contacted Health Services of the Beausoleil First Nation of Christian Island, and by the fall of 1999, received a response that was very positive. The authors were fortunate to meet with the chief and band council by November 1999 to present their literature review.
The council and chief of Beausoleil First Nation gave enthusiastic support to both screening the children of Christian Island and supporting a long term plan to battle type 2 diabetes in their community. The community advisory committee, the BDSSP (which included members of council, elders, health care and educational personnel, and community representatives), was established.
This committee met at least three times before the actual day of screening. Each BDSSP committee member was responsible for a specific area (obtaining supplies, consent forms, etc). Consent forms were distributed to each student through the school on two different occasions. To ensure as many participants as possible, two volunteers were sought to go door to door to reinforce the need for consent from parents in the community.
The testing day was April 12, 2000, with a start time of 09:00. All children enrolled in Christian Island Elementary School were offered the testing. A main station was set up as a central area to organize charts, record results and reorganize charts for the next step in the process. Teams were positioned in classrooms. First, the fasting capillary blood glucose value was obtained by using the Precision QID (Abbott Laboratories, USA) glucose meter. The meters were initially sent to the laboratory at Orillia Soldiers Memorial Hospital to ensure glucose control calibration. Only registered nurses with Certified Diabetes Educator training performed the glucose testing. Disposable unistix (Lifescan, Canada) were used.
Immediately after the glucose testing, each child’s height, weight and blood pressure were measured at three separate stations. Height was measured using tape that was carefully placed on a wall. Blood pressure was measured on the right arm, with the child sitting on a chair. The children moved through the three stations in groups. They were assisted by second-year nursing students who ensured that each child completed all stations. Stickers were given to the children as they completed each station. A 75 g glucose snack (granola bar, milk and banana) was given, and the children were supervised by the nursing students to ensure that the entire snack was consumed. The time when each child completed the snack was recorded. The team returned to the first group and performed an exact 2 h PC capillary blood glucose (using glucose meters). Team members then moved to the next group to complete the 2 h PC capillary blood glucose. Impaired fasting glucose (IFG) was defined as 6.1 to 6.9 mmol/L. Impaired glucose tolerance was defined as fasting less than 7.0 mmol/L and 2 h PC 7.8 to 11.0 mmol/L. DM was defined as fasting more than 7.0 mmol/L and 2 h PC less than 11.1 mmol/L (1).
In the afternoon at 13:00, a one-quarter mile route was mapped out. Each child was encouraged to run the entire course and was timed.
Before the testing day, children filled out questionnaires regarding lifestyle and nutrition, which were subsequently analyzed (unpublished data).
SETTING
Beausoleil First Nation Community is an Ojibway community situated on Christian Island in Georgian Bay. On the island, there is only one school, a public elementary school for children from junior kindergarten to grade 8. The island is relatively remote. It is accessed in the winter by snowmobile and in the summer by boat. The Paediatric Diabetic Education Centre in Orillia is located approximately 1 h away from Christian Island. The Paediatric Diabetic Education Centre functions in the context of a regional neonatal and paediatric program that serves children in regions of Simcoe, Muskoka and Parry Sound counties.
It is estimated that 30% of the adult community on Christian Island has type 2 diabetes.
POPULATION STUDIED
All 115 students who attended Christian Island Elementary School were entered into the study’s population group. Children’s ages ranged from four to 14 years. In total, 91.3% of the study group obtained parental consents and completed the entire procedure. In only 0.9% of the study group, children who obtained parental consents subsequently refused to participate. The refusals were for no specific reason. On the testing day, 3.5% of the study group was absent and did not complete the assessment. The authors do not know why these children were absent from school on that day. In this study group (ie, children who attended school on the testing day), 2.6% of the children refused to consent to participate in the study. With regard to the screening procedures, 100% of the children who partcipated undertook the anthropometric screening, 100% completed blood pressure testing, 93.3% completed the exercise testing, 100% provided fasting capillary blood glucose samples and 95.2% undertook 2-h post 75 g glucose load capillary blood testing. Refusals to participate in the screening procedures were generally nonspecific (Table 1).
TABLE 1:
Study participants
| Age (in years) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total | % | |
| Participants | |||||||||||||
| Students (number) | 5 | 16 | 11 | 12 | 20 | 12 | 12 | 6 | 10 | 10 | 1 | 115 | 100.0 |
| Consents obtained; study completed | 4 | 15 | 11 | 12 | 18 | 11 | 11 | 5 | 10 | 7 | 1 | 105 | 91.3 |
| Consent obtained by own physician | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1.7 |
| Parental consent obtained but child refused to participate | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0.9 |
| Child absent with consent; study not completed | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 2 | 0 | 4 | 3.5 |
| Parental consent not obtained; therefore, child refused to participate | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 3 | 2.6 |
| Screening procedures | |||||||||||||
| Anthropometric screening competed | 4 | 15 | 11 | 12 | 18 | 11 | 11 | 5 | 10 | 7 | 1 | 105 | 100.0 |
| Blood pressure taken | 4 | 15 | 11 | 12 | 18 | 11 | 11 | 5 | 10 | 7 | 1 | 105 | 100.0 |
| Exercise completed | 2 | 14 | 10 | 11 | 17 | 11 | 11 | 5 | 9 | 7 | 1 | 98 | 93.3 |
| Fasting capillary blood glucose samples provided | 4 | 15 | 11 | 12 | 18 | 11 | 11 | 5 | 10 | 7 | 1 | 105 | 100.0 |
| 2 h PC completed | 3 | 13 | 11 | 10 | 18 | 11 | 11 | 5 | 10 | 7 | 1 | 100 | 95.2 |
INTERVENTIONS
Five separate physical assessments were undertaken. The anthropometric assessments included height, weight and the calculation of body mass index (BMI). Three registered dietitians measured each child’s height and weight. Blood pressure was assessed by a nurse on the team who measured sitting blood pressure on the right arm, with the appropriate sized cuff. The capillary blood tests were peformed by registered nurses with Certified Diabetes Educator training. The 75 g glucose load was monitored by second-year nursing students, and, at the appropriate time, further follow-up capillary blood glucose values were obtained. Exercise testing consisted of a one-quarter mile distance run on laid out track. All children were requested to complete the exercise and their times were recorded. The lifestyle and nutrition questionnaires were analyzed to determine the percentage of time spent watching television during the day, exercise indicators, and the diet of students aged 10 to 13 years (and one 14-year-old student). The age range was selected based on the ability to fill out the questionnaire.
MAIN RESULTS
Seven children aged 5, 5, 6, 10, 10, 10 and 11 years had IFG: two children in the senior kindergarten class; one child in grade 1; three children in grade 5; and one child in grade 6. One child had evidence of DM (fasting plasma glucose greater than or equal to 7.0 mmol/L). All eight children were contacted, and arrangements were made through either the Paediatric Diabetic Education Centre or their family physicians for them to return for a proper venous sampling of both fasting blood glucose levels and 2 h PC (75 g glucose load). All eight children were found to have normal venous fasting blood glucose values and normal 2-h PC glucose levels (75 g glucose load).
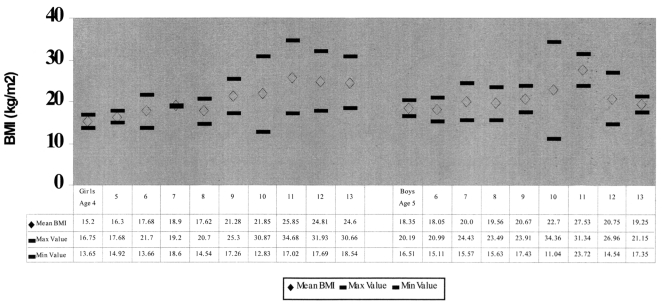
The heights and weights of all the children who participated in the study were recorded, and their BMIs were calculated. The BMIs for boys in this sample who were aged nine, 10 and 11 years (a total of 12 boys) was greater than those expected, based on the standards in Physical Best Health Fitness Standards (20). Girls aged nine to 13 years had a mean BMI above that which is recognized in Physical Best Health Fitness Standards (Figure 1) (20). Individually, girls in the seven to 11 year age range and those who were 13 years of age met the obesity criteria (obesity defined as greater than 95% BMI). Boys in the five to 11 year age group met the obesity criteria. Only the 13-year-old boys fell within acceptable norms for BMI (21).
Figure 1).
Body mass index (BMI) values of study participants. Max Maximum; Min Minimum
Systolic and diastolic blood pressures were analyzed, based on age. The mean systolic and diastolic blood pressures were less than the 90th percentile for all age groups for both boys and girls (16).
Exercise testing was done over a one-quarter mile distance run, with times recorded in minutes and seconds. All groups, except for two, fell within the standards outlined in Physical Best Health Fitness Standards (20). Two groups (boys aged 10 and 11 years) scored above the mean for their age groups.
The questionnaires that addressed lifestyle were analyzed for time spent watching television and exercising, and for dietary information. The students who filled out the questionnaires were aged 10 to 13 years. The questionnaire was considered to be a subjective measurement of physical activity and a guide to target groups of children about community strategies to improve activity. Seventy-one per cent of 10-year-old children, 80% of 11-year-old children and 49% of 12-year-old children watched more than three television programs/day on school days. The trend seemed to reverse in 13-year-old children, but the major difference for these children was the increased time spent watching videos, which reached 88% on most days. Overall, the children indicated that their mothers exercised less frequently than their fathers. However, they indicated that their mothers asked them to exercise more frequently than did their fathers.
Diet recalls were filled out by children aged 10 to 13 years. It was decided that a weekly trend in dietary choices would be easier for this age to remember; however, the authors recognized that the data were very subjective and could only be used to indicate trends over time. Canada’s Food Guide to Healthy Eating (23) was used as the reference to review the children’s answers. Only 10% to 20% of the children consumed milk or grain products on the majority of days during the week in the 10-year-old age group. The 11-year-old age group consumed very few milk products on most days of the week. In the 12-year-old group, the consumption of milk and grain products was also very low, with only 10% of the children consuming these food groups on most days of the week. The 13-year-old group recalled consuming milk and grain products more frequently than the younger age groups.
CONCLUSIONS
The project described in this paper was successful in screening First Nation children for type 2 diabetes. However, even more importantly, a relationship was forged between the medical group and the people of Beausoleil First Nation through the band council and the community advisory board, the BDSSP.
The assessment (screening) successfully demonstrated that such a project could be carried out with a high compliance rate when an appropriate structure was in place within this First Nation community. The authors consider this project to be a model for further exploration with other First Nation communities both in their catchment area and throughout Canada. As the authors progressed through the process, they realized that the key to success was not the technical expertise of the medical personnel, but rather the determination and foresight of the band council and community advisory committee. The screening results indicated a group of children with risk factors for type 2 diabetes of increased body mass and some exercise intolerance. Areas of concern regarding trends in television watching and diet were found. The community advisory committee team hopes to institute changes that could affect these trends. The entire medical team, band council, community advisory committee and people of Beausoleil First Nation recognized that this endeavour was merely a first step toward changing the face of a devastating disease in the First Nations community.
The authors regard this project to be a 10-year program. The next step includes a structured school education program on diet and exercise that is delivered to the school children of Christian Island Elementary School during the fall season (unpublished data). There will be a major incentive to improve the exercise status of the residents of Christian Island through the community advisory committee; furthermore, interventions into the dietary habits of the residents of Christian Island will be looked at by the community advisory committee and the band council.
The collaborative team hopes to screen this population on a yearly basis, looking at trends involving blood pressure, body mass and exercise over the years.
Acknowledgments
The principal authors thank the following people for their assistance and enthusiasm: Christian Island Health Center staff (Mary Smith), North Simcoe Diabetes Resource Centre, volunteer mothers (especially Sue Vanier, Mary-Lou Crowthers), Dr and Mrs McNamara, Tom Puttycomb, Peggy Monague, Julie Pope and the Georgian College students. Permission to publish the results of this study was given by The Beausoleil First Nation Band Council Resolution No 141-2000-2001:023.
REFERENCES
- 1.Meltzer S, Leiter L, Daneman D, et al. 1998 clinical practice guidelines for the management of diabetes in Canada. Canadian Diabetes Association. CMAJ. 1998;159(Suppl 8):S1–29. [PMC free article] [PubMed] [Google Scholar]
- 2.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–43. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- 3.Macaulay AC, Paradis G, Potvin L, et al. The Kahnawake Schools Diabetes Prevention Project: Intervention, evaluation and baseline results of a diabetes primary prevention program with a native community in Canada. Prev Med. 1997;26:779–90. doi: 10.1006/pmed.1997.0241. [DOI] [PubMed] [Google Scholar]
- 4.Dean H. Treatment of type 2 diabetes in youth: An argument for randomized controlled studies. Paediatr Child Health. 1999;4:265–70. doi: 10.1093/pch/4.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fox C, Harris S, Whalen-Brough E. Diabetes among Native Canadians in Northwestern Ontario: 10 years later. Chronic Dis Can. 1994;15:92–6. [Google Scholar]
- 6.Harris S, Perkins B, Whalen-Brough E. Non-insulin-dependent diabetes mellitus among First Nations children. New entity among First Nations people of north western Ontario. Can Fam Physician. 1996;42:869–76. [PMC free article] [PubMed] [Google Scholar]
- 7.Pinhas-Hamiel O, Zeitler P. Type 2 diabetes in adolescents, no longer rare. Pediatr Rev. 1998;19:434–5. doi: 10.1542/pir.19-12-434. [DOI] [PubMed] [Google Scholar]
- 8.Dean H, Young T, Flett B, Wood-Steiman P. Screening for type-2 diabetes in aboriginal children in northern Canada. Lancet. 1998;352:1523–4. doi: 10.1016/S0140-6736(05)60329-7. [DOI] [PubMed] [Google Scholar]
- 9.Dean H. NIDDM-Y in First Nation children in Canada. Clin Pediatr (Phila) 1998;37:89–96. doi: 10.1177/000992289803700205. [DOI] [PubMed] [Google Scholar]
- 10.Sellers E, Dean H. Type 2 diabetes mellitus in First Nation youth in Canada. Contemp Pediatr. 1998;2:12–4. [Google Scholar]
- 11.Harris S, Gittelsohn J, Hanley A, et al. The Prevalence of NIDDM and associated risk factors in native Canadians. Diabetes Care. 1997;20:185–7. doi: 10.2337/diacare.20.2.185. [DOI] [PubMed] [Google Scholar]
- 12.Dean H, Mundy R, Moffatt M. Non-insulin-dependent diabetes mellitus in Indian children in Manitoba. CMAJ. 1992;147:52–7. [PMC free article] [PubMed] [Google Scholar]
- 13.UKPDS Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complication in-patients with type 2 diabetes. Lancet. 1998;352:837–52. [PubMed] [Google Scholar]
- 14.Hegele RA, Cao H, Harris SB, Hanley AJ, Zinman B. The hepatic nuclear factor-1alpha G319S variant is associated with early-onset type 2 diabetes in Canadian Oji-Cree. J Clin Endocrinol Metab. 1999;84:1077–82. doi: 10.1210/jcem.84.3.5528. [DOI] [PubMed] [Google Scholar]
- 15.Anderson J. Diabetes in Aboriginal populations. CMAJ. 2000;162:11–2. [PMC free article] [PubMed] [Google Scholar]
- 16.Update on the 1987 Task Force Report on High Blood Pressure in Children and Adolescents: A working group report from the National High Blood Pressure Education Program. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Pediatrics. 1996;98:649–58. [PubMed] [Google Scholar]
- 17.Committee on Nutrition, American Academy of Pediatrics Cholesterol in childhood. Pediatrics. 1998;10:141–6. [PubMed] [Google Scholar]
- 18.Fox CS, Esparza J, Nicolson M, et al. Is a low leptin concentration, a low resting metabolic rate, or both the expression of the “thrifty genotype”? Results from Mexican Pima Indians. Am J Clin Nutr. 1998;68:1053–7. doi: 10.1093/ajcn/68.5.1053. [DOI] [PubMed] [Google Scholar]
- 19.Hanson RV, Ehm MG, Pettitt D, et al. An autosomal genomic scan for loci linked to type 2 diabetes mellitus and body-mass index in Pima Indians. Am J Hum Genet. 1998;63:1130–8. doi: 10.1086/302061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reston VA. Physical Best Health Fitness Standards. American Alliance for Health, Physical Education, Recreation and Dance. 1989:138–9. [Google Scholar]
- 21.Hummer L, Kraemer H, Wilson D. Standardized percentile curves of body-mass index for children and adolescents. Am J Dis Child. 1991;145:259–63. doi: 10.1001/archpedi.1991.02160030027015. [DOI] [PubMed] [Google Scholar]
- 22.Canada’s Food Guide to Healthy Eating (For People Four Years and Over) Catalogue number H39-252/1992Ottawa: Minister of Supply and Services Canada; 1992 [Google Scholar]