Abstract
Maternal psychological functioning during pregnancy affects both maternal and fetal well-being. The hypothalamic-pituitary-adrenal (HPA) axis provides one mechanism through which maternal psychosocial factors may be transduced to the fetus. However, few studies have examined maternal psychological factors or birth outcomes in relation to the diurnal pattern of cortisol across the day. The current study examined maternal psychological well-being, parity status, and birth weight in relation to the maternal cortisol diurnal rhythm in a group of 98 low-risk pregnant women (51 primiparae). At 36 weeks gestation, participants completed both pregnancy-specific and general self-report measures of psychological functioning and provided saliva samples at 800, 1200, and 1600h on 2 consecutive working days for the assay of cortisol. The expected diurnal decline in salivary cortisol was observed. Higher trait anxiety was associated with a flatter afternoon decline for all mothers. For primiparae, steeper morning cortisol declines were associated with lower infant birth weight. The findings suggest that regulation of the HPA axis may differ by parity status with downstream implications for fetal growth and development.
Keywords: cortisol diurnal rhythm, pregnancy, parity, fetus, anxiety, birth weight
There is much interest in the role of maternal psychological functioning during pregnancy with respect to maternal and fetal well-being. The hypothalamic-pituitary-adrenal (HPA) axis may be a key mechanism whereby maternal psychosocial factors might mediate their effects on the fetus. In general, the release of corticotrophin-releasing hormone (CRH) and arginine-vasopressin (AVP) from the hypothalamus stimulates the secretion of adrenocorticotrophic hormone (ACTH) from the anterior pituitary and the subsequent release of cortisol from the adrenal cortex. During pregnancy, peripheral CRH of placental origin rises dramatically over non-pregnant levels. This increase in CRH is paralleled by elevations in both ACTH and total cortisol levels (for reviews, see Levine, Zagoory-Sharon, Feldman, Lewis, & Weller, 2007; Mastorakos & Ilias, 2003). Free (bioavailable) cortisol remains at non-pregnant levels until around the 25th week of gestation and rises thereafter (Allolio et al., 1990; Demey-Ponsart, Foidart, Sulon, & Sodoyez, 1982). The elevated free cortisol levels of late pregnancy may be due to a resetting of the sensitivity of the HPA axis (Scott, McGarrigle, & Lachelin, 1990). Despite these functional alterations during pregnancy, the diurnal rhythm of cortisol is largely maintained with peak levels at approximately 30-minutes post-waking and a gradual decrease across the day to an early evening nadir (Allolio et al., 1990; de Weerth & Buitelaar, 2005).
While cortisol is often suggested as a mediator of maternal psychological well-being on fetal development (Wadhwa, 2005; Weinstock, 2005), evidence that maternal experience of stress is associated with cortisol levels during pregnancy is inconsistent. In general, self-reported measures of maternal stress, including reports of life events, daily hassles, and perceived stress, are often unrelated to maternal cortisol during pregnancy (Petraglia et al., 2001; Urizar et al., 2004; Wadhwa, Dunkel-Schetter, Chicz-DeMet, Porto, & Sandman, 1996), but small positive associations with cortisol levels have been reported (Buitelaar, Huizink, Mulder, Robles de Medina, & Visser, 2003; Diego et al., 2006). In contrast, one study incorporating measures of both waking and late evening cortisol during the third trimester observed 27% higher evening cortisol levels among women who experienced a stressful life event or were concerned about pregnancy complications during the second trimester. Morning cortisol levels were unaffected suggesting a shallower decline in cortisol across the day in stressed women (Obel et al., 2005). Therefore, the pattern of the daily diurnal decline may be an important indicator of the influence of maternal psychology on the function of the HPA axis.
A focus on general, rather than pregnancy-specific measures of stress may also contribute to the sparse associations observed between maternal psychological stress and cortisol during pregnancy. Pregnant women are confronted with changes in their physical condition (e.g., weight gain, sleep quality), anxiety about fetal well-being, impending labor, and new challenges related to balancing work and family (Affonso, Mayberry, Lovett, & Paul, 1994; Arizmendi & Affonso, 1987; DiPietro, Millet, Costigan, Gurewitsch, & Caulfield, 2003; Norbeck & Anderson, 1989; Yali & Lobel, 1999). Previous experience with pregnancy (i.e. parity) may heighten or attenuate the intensity of pregnancy, possibly influencing both psychological and physiological responses to this context (Condon & Esuvaranathan, 1990; DiPietro, Costigan, & Gurewitsch, 2005). In support of this, there is evidence that HPA axis activity differs by parity status. Higher mid-day total cortisol levels have been observed in primiparae as opposed to multiparous women throughout pregnancy (Rasheed, 1993; Vleugels, Eling, Rolland, & de Graaf, 1986). In contrast, lower waking cortisol levels have been observed among primiparae as compared to multiparous women (Jones, Holzman, Zanella, Leece, & Rahbar, 2006). During the postpartum period, primiparae display greater total cortisol output across the day, while the diurnal rhythm of multiparae is influenced by feeding choice (bottle vs. breastfeeding; Tu, Lupien, & Walker, 2006). Among mothers of 2-year-olds, having multiple children has been associated with lower morning cortisol levels and a flatter decline in cortisol across the day (Adam & Gunnar, 2001). Therefore, parity might exert an influence on the cortisol diurnal rhythm that extends beyond pregnancy.
Alterations in the function of the HPA axis due to parity or pregnancy-specific experiences could result in differential fetal exposure to maternal glucocorticoids with implications for fetal development. The fetus is largely protected from elevated maternal cortisol levels through the catabolic activity of placental 11β-hydroxysteroid-dehydrogenase (11β-HSD; Benediktsson, Calder, Edwards, & Seckl, 1997). However, the work of Gitau and colleagues has demonstrated that maternal cortisol may still account for 33–40% of the variance in fetal cortisol concentrations (Gitau, Cameron, Fisk, & Glover, 1998; Gitau, Fisk, Teixeira, Cameron, & Glover, 2001). Consequently, maternal free cortisol has the capacity to directly influence fetal growth and development (for review, see Seckl & Meaney, 2004). While there appears to be sensitive period in the early second trimester for maternal cortisol to influence the timing of labor (Sandman et al., 2006), late pregnancy, a period of accelerated fetal somatic growth, is a critical period for the determination of size at birth. The peak velocity of adipose tissue deposition occurs after 28 weeks gestation (Tanner, 1989) and environmental influences during this period have the capacity to affect birth weight (Paige & Villar, 1982; Ulijaszek, Johnston, & Preece, 1998). Placental 11β-HSD deficiency, resulting in fetal overexposure to maternal glucocorticoids, has been linked to lower birth weight (McTernan et al., 2001; Murphy et al., 2002; Shams et al., 1998; Stewart, Whorwood, & Mason, 1995). In contrast, low maternal, amniotic, and umbilical cord cortisol levels have been observed in cases of intrauterine growth retardation (IUGR; Nieto-Diaz, Villar, Matorras-Weinig, & Valenzuela-Ruiz, 1996; Strinic, Roje, Marusic, & Capkun, 2007). Taken together, these findings suggest that levels of bioavailable cortisol levels in late pregnancy may be associated with somatic size at birth. However, little is known about the role of cortisol in regulating fetal growth in normative populations.
In summary, interest in the role of maternal psychological functioning on fetal development during pregnancy has prompted a great deal of research, but many questions remain. Basal cortisol levels have been examined as a mediator of these effects, but few studies have examined the cortisol diurnal rhythm as a potential indicator of maternal regulation of the HPA axis during pregnancy. In particular, parity may be an important determinant of maternal perception of the “ups and downs” of pregnancy and this may be translated to the fetus via changes in physiological regulation with implications for both maternal and fetal well-being. The purpose of the current study is 1) to determine if maternal psychological functioning and neonatal birth outcomes are associated with the diurnal rhythm of late pregnancy in a group of low-risk pregnant women; 2) to determine if the maternal cortisol diurnal rhythm differs by parity status; and 3) to determine if maternal parity status moderates associations between salivary cortisol, psychological functioning, and birth outcomes.
Methods
Participants
Eligibility was restricted to normotensive, non-smoking adult women (18 years or older) with uncomplicated pregnancies at the time of enrollment. Women with serious medical conditions known to complicate pregnancy (e.g., Type I or II diabetes) were ineligible to participate. Accurate dating of the pregnancy was required and based on early first trimester pregnancy testing or examination and confirmed by ultrasound. A total of 98 self-referred pregnant women from the local community were enrolled in the 36-week protocol. Participants continued to have generally healthy pregnancies and subsequent pregnancy complications were uncommon and mild in nature. All infants were born healthy at full term with the exception of one fetal death in utero prior to term. This case was excluded from analysis. Three additional participants were excluded due to use of steroid-based mediations during pregnancy. The sample represents a population of mature, relatively well-educated women (M age = 31.1, SD = 4.8, range 21 to 43; M years education = 16.8 years, SD = 2.3, range 12 to 20), with fairly high occupational status (Hollingshead, 1975; M = 7.23, SD = 1.41, range 2 to 9). Most (87%) women were non-Hispanic white and the remainder was of African-American (6%), Hispanic or Asian (6%) decent. The majority were married (94%) and expecting their first child (52%). Thirty-two percent had one previous child and 15% had two or more. Fifty-one percent of the fetuses were female.
Design and Procedure
Women included in the current analysis constituted a subset of a larger study of prenatal development including maternal-fetal assessments at 32 and 36 weeks gestation. Advertisements in hospital publications, flyers, and word-of-mouth were the primary recruitment vehicles. Written informed consent was obtained during a laboratory visit at 32 weeks gestation or later for women who did not participate at 32 weeks (n = 10). Participants were provided a packet of study collection materials to be completed during the 36th week of gestation. This packet included three self-report questionnaires to assess both pregnancy-specific and general maternal psychological well-being. Participants were also provided with materials and instructions to complete at home saliva collection.
Salivary Cortisol
Saliva Collection
Participants were instructed to collect saliva at 800, 1200 and 1600 hours on two consecutive work days and to refrain from eating, drinking coffee, or brushing their teeth for 30 minutes prior to each sample. Saliva collection times, time of waking, daily hours worked, sleep quality and the presence of blood in the oral cavity that day were recorded. The use of filter strips for saliva collection and their validation have been described in detail previously (Neu, Goldstein, Gao, & Laudenslager, 2007). Saliva was collected by placing a small, specially cut filter paper (2.5 × 9.0 cm, Whatman Grade 42) in the subject’s mouth and having them wet the filter thoroughly. The strip was removed from the subject’s mouth while carefully wiping excess saliva from the surface with their lips. Filters were allowed to air dry. A recent validation study revealed that cortisol remains stable in this dried format for more than 6 months and demonstrated 92% recovery of cortisol from filters as compared to whole saliva (Neu et al., 2007).
Cortisol Assay
The dried filters were extracted by cutting a fixed area from the filter that varies with each filter lot. Each lot must be calibrated using a known volume of radiolabeled tracer in a saliva pool. Cut filter papers were placed in a 1.4 ml microcentrifuge tube to which assay buffer was added. These tubes were shaken for 24 hrs after which the extraction buffer was added in duplicate to the appropriate wells of the assay plate. Extraction dilutes the saliva approximately 1:5. Salivary cortisol concentration in the extraction buffer was determined using a commercial expanded range high sensitivity EIA kit (No. 1-3002/1-3012, Salimetrics) that detects cortisol levels in the range of .003 – 3.0 µg/dl (0.083 – 82.77 nmol/L). Standard curves were fit by a weighted regression analysis using commercial software (Revelation 3.2) for the ELISA plate reader (Dynex MRX). After taking the dilution into consideration, the detection limit is 0.018 µg/dl (0.50 nmol/L) for cortisol. This kit shows minimal cross reactivity (4% or less) with other steroids present in the saliva. Controls run on every plate for determination of inter-assay coefficients of variation were less than 7.5% for high and low laboratory controls in the present study. Intra-assay coefficients of variation for duplicate determinations were less than 3% in the present study.
Maternal Psychological Well-Being
Maternal psychological well-being during pregnancy was assessed with one pregnancy-specific instrument and two extensively validated measures of general psychological distress. In addition, upon enrollment, women were asked to rate their level of anxiety specific to this pregnancy on a 5-point scale ranging from low to high.
Pregnancy Experience Scale
The Pregnancy Experience Scale (PES; DiPietro, Ghera, Costigan, & Hawkins, 2004) was developed to assess maternal appraisal of daily, pregnancy-specific hassles and uplifts. This scale consists of 41 items listing pregnancy-specific experiences such as “comments from others about your pregnancy/appearance” or “discussions with spouse about baby names”. Participants were asked to rate the degree to which each experience constituted both a hassle and an uplift on 5-point scales ranging from “not at all” to “a great deal”. Scoring was based on the ratio of hassles to uplifts (intensity of hassles divided by intensity of uplifts) where higher values indicate greater negative emotional valence towards pregnancy.
State-Trait Anxiety Inventory
The Spielberger State-Trait Anxiety Inventory (STAI) distinguishes between state anxiety, as an unpleasant negative emotion experienced in response to a threatening stimulus and trait anxiety, which is defined as a stable tendency to respond with anxiety to perceived threats (Spielberger, 1983). In particular, the Trait Form (Y2) was administered at 36 weeks and consists of 20 items that ask respondents to rate how they feel in general on a 4-point scale ranging from “almost never” to “almost always”. Items were reversed as necessary and summed, such that higher total scores reflect greater trait anxiety.
Perceived Stress Scale
The 14-item Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) was designed to measure the degree to which situations in one’s life are perceived as stressful. Women were asked to rate their thoughts and feelings about stressful situations since their pregnancy began. Items such as “How often have you felt nervous or ‘stressed’?” and “How often have you found you could not cope with all the things that you had to do?” were scored on 5-point scales from “never” to “very often”. Items were reversed as necessary and summed, such that a higher score indicates a higher level of perceived stress.
Neonatal Birth Outcomes
Women were provided with a labor and delivery form and asked to present these to their labor and delivery nurse immediately after delivery. Attendant hospital personnel extracted the information from the medical record and returned these by mail. Extracted infant data included infant birth weight, gestational age at birth, and Apgar scores at 1- and 5-minutes.
Data Management and Analysis
Variables were examined for outliers and skewness. Preliminary analyses, including independent sample t-tests, bivariate correlations, and one-way analysis of variance (ANOVA) were used to identify potential confounds. To test hypotheses, linear mixed models were estimated using SPSS MIXED in order to examine the overall pattern of individual differences in the maternal cortisol diurnal rhythm. These models incorporate two levels; Level 1 models the change in the dependent variable over time for each individual in the sample, while the Level 2 relates individual growth parameters to predictors of interest (Bryk & Raudenbush, 1987; Singer & Willett, 2003). Two important advantages emerge from the use of these models. First, individuals are not directly compared based on their cortisol levels, but on the parameters describing their diurnal decline across the day. Therefore, sample collection times are allowed to vary across participants and are accounted for in the Level 1 model. Second, the number of data points per subject can also vary, as long as there is sufficient information to describe the diurnal decline for that individual. Therefore, unbalanced data sets (missing data) are acceptable in these models (Singer & Willett, 2003).
Restricted maximum likelihood (REML) is used in reporting model parameters when assessing the significance of the random effects; degrees of freedom were estimated using the Satterthwaite method. The 95% confidence interval (CI) for random variation around each fixed effect was calculated as ± 2 standard deviations of its accompanying random variance term. A piecewise model with time of sample collection as the variable time structure was selected to model maternal cortisol decline across the day. Time of day was centered at 800h, such that the intercept represented cortisol level at the time of the initial assessment. Piecewise models included a morning slope to represent diurnal decline from 800h to noon, and an afternoon slope to represent the degree of cortisol declivity from 1200h onwards. Day of sample collection was also examined as a potential source of variation. Models were initially specified with random intercepts and the effects of including random slopes, morning and afternoon, on model fit were subsequently evaluated. Covariates identified during preliminary analyses were next inspected as potential predictors. The fixed effects of each predictor (measures of psychological well-being, neonatal birth outcome, parity status) on the intercept, morning, and afternoon declines were tested sequentially in the whole group. Next, an interaction term with parity was included to determine if these associations operated differently in first time vs. experienced mothers. All significant predictors were retained in the final model. Model fit was assessed with likelihood deviance difference tests for nested models.
Results
Several circumstances resulted in missing cortisol values at one or more collection points. These included failure to collect, failure to collect as directed, and cortisol values beyond detectable limits. Failure to collect was associated with the following missing values encompassing 16 participants: Day 1 morning (6), noon (5), late afternoon (3); Day 2 morning (3), noon (5), late afternoon (5). Two participants were excluded both days for failure to collect as directed. An additional participant’s Day 2 data was excluded due to night shift work. Eleven participants generated one or more cortisol values beyond assay limits (Day 1: morning [3], noon [2], late afternoon [4]; Day 2: morning [2], noon [2], late afternoon [3]). Of the 94 participants, 91 provided valid samples for modeling on at least one day and 67 (71%) had usable data available for all 6 samples. Samples were log-transformed to correct for positive skew. Table 1 presents descriptive statistics and final sample sizes for use in linear mixed models for each collection period. Although transformed values were used in all analyses, untransformed values are presented in tables and figures to facilitate interpretation. To convert µg/dl to nmol/L, multiply by 27.59.
Table 1.
Descriptive Statistics for Maternal Diurnal Salivary Cortisol Levels (µg/dl)
| Morning |
Noon |
Late Afternoon |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Cortisol | N | Mean | SD | N | Mean | SD | N | Mean | SD |
| Day 1 Levels | 84 | .49 | .22 | 85 | .31 | .15 | 86 | .24 | .12 |
| Day 2 Levels | 87 | .47 | .20 | 85 | .30 | .14 | 84 | .26 | .16 |
| Mean Levels | 91 | .48 | .18 | 90 | .31 | .13 | 91 | .25 | .14 |
Note – To convert µg/dl to nmol/L, multiply by 27.59.
Preliminary Analyses
For use in preliminary analyses only, cortisol values were “binned” by sample collection time to represent levels in the morning (range: 700 to 1100), midday (range: 1100 to 1500), and late afternoon (range: 1500 to 2300) for each day. For precision in these analyses, additional observations were excluded if they fell outside the time ranges specified above. Twelve participants collected at least one sample outside of these time windows (Day 1: morning [2], noon [2]; Day 2: morning [4], noon [4], afternoon [2]). Day 1 and Day 2 mean cortisol values were highly correlated, r (86) = .58, p < .001, and correlations between values collected at the same time of day were highly significant and ranged from .38 to .60. Therefore, mean values for binned cortisol variables were used in subsequent preliminary analyses. Controlling for sample collection time, gain scores were calculated from these variables by regressing midday on morning cortisol levels to reflect the morning decline and late afternoon on midday cortisol levels to reflect afternoon declines. Since typical diurnal patterns involve cortisol declines across the day, more negative gain scores indicate steeper declines.
Wake time, time elapsed between waking and morning sample collection, daily hours of work, sleep quality, and the presence or absence of blood in the oral cavity on the day of collection were all examined as potential confounds. Preliminary analyses revealed that a steeper morning cortisol decline (gain score) was found to be associated with earlier wake times, rs (83 & 82) = .27 and .26, ps < .05, greater elapsed time between waking and morning sample collection, rs (78) = −.30 and −.23, ps < .05, and more hours worked, rs (84 & 83) = −.23 and −.27, ps < .05, on both days. Thus, these variables were examined as covariates in subsequent analyses.
Maternal Cortisol Diurnal Rhythm
As described above, linear mixed models were fit to produce estimates of morning cortisol levels at 800h (intercept) and the slopes for both the morning and afternoon declines. Model parameters are given in Table 2. Model coefficients are generated from transformed values and can be interpreted with the use of inverse transforms. Intercept values in the original scale of measurement can be obtained by applying the exponential function. Coefficients for independent variables (IV; i.e, time structure, covariates, predictors) can be interpreted as the percentage change in outcome per unit change in the IV through application of the following transform: β%change = [exp (βln)] − 1. Maternal salivary cortisol showed the expected pattern of diurnal decline. Both morning and afternoon slopes were highly significant (p < .001). The addition of a random morning slope term (as well as the covariance between the random intercepts and morning slopes) resulted in a significant improvement to the model, REML deviance difference (2) = 25.80, p < .001. Day of sample collection, wake time, and hours worked were not significantly associated with morning cortisol levels or decline. However, controlling for the interval between waking and morning sample collection enhanced model fit, ML deviance difference (2) = 23.62, p < .001. At 800h, cortisol levels (M = .51 µg/dl) were estimated with 95% confidence intervals of .45 to .56 µg/dl. Between 800 and 1200h, maternal cortisol levels decreased by 10.5% or .053 µg/dl per hour (95% CI: −8.0% to −13.0%) with a decline in rate after 1200h to 8.5% or .025 µg/dl per hour (95% CI: −6.2% to −10.8%). Morning cortisol levels at 800h were 7.5% or .038 µg/dl lower for every additional hour between waking and sample collection, and afternoon cortisol decline was 1.3% flatter. This covariate was maintained in all subsequent models.
Table 2.
Preliminary Covariate Model for the Maternal Cortisol Diurnal Rhythm During Late Pregnancy
| Fixed Effects: | Coefficient | SE | t | Interpretation |
|---|---|---|---|---|
| Predicting 8AM cortisol: | ||||
| Intercept | −.682*** | .054 | −12.72 | .506 µg/dl |
| Wake Interval | −.078** | .026 | −2.96 | −7.5% lower per hour |
| Predicting Diurnal Decline: | ||||
| Morning Slope | −.111*** | .014 | −7.93 | −10.5% decline per hour |
| Afternoon Slope | −.089*** | .013 | −6.94 | −8.5% decline per hour |
| Wake Interval*Afternoon Slope | .013* | .006 | 2.36 | +1.3% flatter per hour |
| Random Effects: | Coefficient | SE | z | |
| Within-Person Residual | .133*** | .011 | 12.57 | |
| Intercept Variance | .080** | .026 | 3.11 | |
| Morning Slope Variance | .006** | .002 | 2.81 | |
| Intercept – Morning Slope Covariance | −.005 | .006 | −0.87 | |
p < .05
p < .01
p < .001
Associations of Maternal Psychological Well-Being and Neonatal Birth Outcomes
Descriptive statistics for each psychological measure and neonatal birth outcome are presented in Table 3. A single case each for the PES uplifts scale and the Trait Anxiety Inventory was missing due to subject non-completion. There were also missing Apgar scores on provider-completed delivery forms in 12 cases. Fixed effects of maternal psychological well-being and neonatal birth outcomes on the intercept, morning, and afternoon declines were tested sequentially in the whole group. Significant predictors were retained in the model. To aid interpretation, pregnancy anxiety and the PES hassles to uplifts intensity ratio were centered at 1, while trait anxiety, perceived stress, and birth weight were centered at the mean. Gestational length was centered at 40 weeks and Apgar scores at the optimal score of 10. Model parameters are presented in Table 4. Inclusion of trait anxiety and birth weight as predictors significantly improved the fit of the model, ML deviance difference (4) = 14.98, p < .01. While neither morning cortisol levels nor morning cortisol decline were associated with psychological factors, a flatter afternoon cortisol decline was associated with higher trait anxiety (1.74% per +1 SD increase; 95% CI: 0% to 3.3%). Infant birth weight was associated with both maternal cortisol levels at 800h and the morning cortisol decline. For mothers of infants weighing 1 kg above the mean at birth (4449 g or 9.8 lbs), maternal morning cortisol levels were 18.0% or .091 µg/dl lower (95% CI: 0.7% to 32.2%) and the maternal morning cortisol decline was 5.7% flatter (95% CI: 0.1% to 10.4%). As a corollary, mothers with infants 1 kg below the mean (2449 g or 5.41 lbs), would have morning cortisol levels 18.0% higher than the intercept, and a 5.7% steeper morning decline.
Table 3.
Descriptive Statistics for Measures of Psychological Well-Being and Neonatal Birth Outcomes
| N | Mean | SD | Range | |
|---|---|---|---|---|
| Pregnancy-Specific Psychological Well-Being | ||||
| Pregnancy Anxiety | 94 | 2.31 | .98 | 1.00 – 5.00 |
| Pregnancy Experiences Scale | ||||
| Ratio of Hassles/Uplifts | 93 | .77 | .22 | .38 – 1.51 |
| General Psychological Well-Being | ||||
| Trait Anxiety (Y2) | 93 | 38.08 | 8.71 | 8.00 – 70.00 |
| Perceived Stress Scale | 94 | 24.88 | 6.85 | 9.00 – 44.00 |
| Neonatal Birth Outcomes | ||||
| Birth weight (grams) | 94 | 3449 | 457 | 2489 – 5315 |
| Gestational age at birth (weeks) | 94 | 39.41 | 1.08 | 37.00 – 41.71 |
| 1 Minute Apgar scores | 82 | 7.87 | 1.55 | 1 – 10 |
| 5 Minute Apgar scores | 82 | 8.74 | .78 | 5 – 10 |
Table 4.
Preliminary Model Relating Trait Anxiety and Neonatal Birth Weight to the Maternal Cortisol Diurnal Rhythm During Late Pregnancy
| Fixed Effects: | Coefficient | SE | t | Interpretation |
|---|---|---|---|---|
| Predicting 8AM Cortisol: | ||||
| Intercept | −.677*** | .053 | −12.67 | .508 µg/dl |
| Wake Interval | −.079** | .026 | −3.03 | −7.6% per hour |
| Trait Anxiety | −.005 | .004 | −1.12 | |
| Birth Weight | −.198* | .096 | −2.06 | −18.0% per kg |
| Predicting Diurnal Decline: | ||||
| Morning Slope | −.110*** | .014 | −7.95 | −10.4% decline per hour |
| Birth Weight | .055* | .028 | 2.01 | +5.7% flatter per kg |
| Afternoon Slope | −.090*** | .013 | −7.10 | −8.6% decline per hour |
| Wake Interval | .014* | .006 | 2.46 | + 1.4% flatter per hour |
| Trait Anxiety | .002* | .001 | 2.28 | +1.74% flatter per +1 SD |
p < .05
p < .01
p < .001
Association with Parity Status
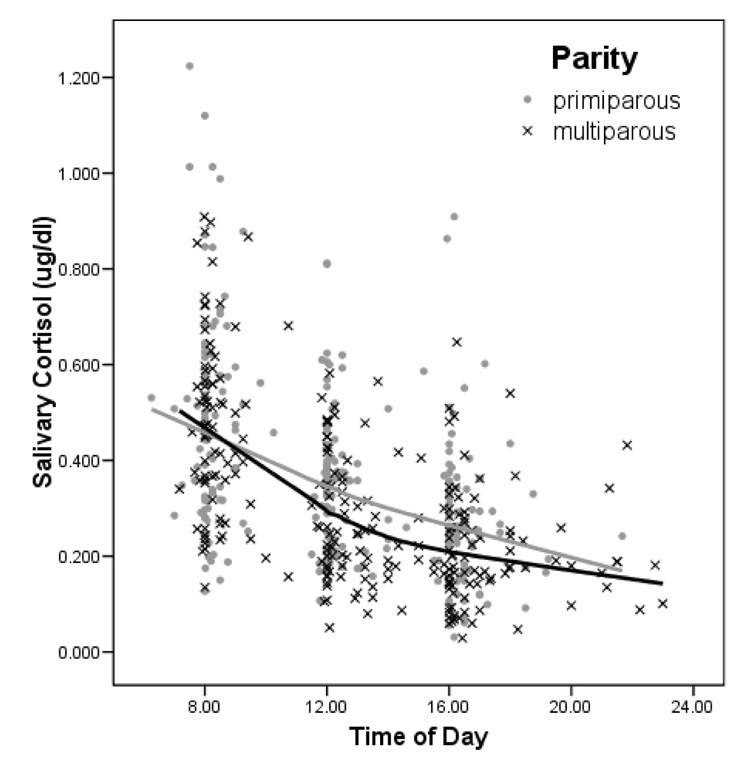
Parity status was next examined as a predictor of the maternal cortisol diurnal rhythm. Prior to examining parity effects, analyses were conducted to determine whether any sociodemographic or predictor variables were associated with parity status. Maternal parity was significantly associated with maternal age, F (1, 91) = 5.29, p < .05, η2p = .06, and occupational status, F (1, 92) = 5.42, p < .05, η2p = .06, such that women with previous children were older and had lower status occupations. Maternal parity status, age, and occupation status were all examined as predictors in the model of the diurnal decline of maternal cortisol. Primiparae were used as the reference group for parity status and maternal age and occupation status were centered at the mean. Inclusion of both maternal age and parity as predictors significantly improved the fit over the covariate model, ML deviance difference (4) = 22.11, p < .001. Parameters describing the intercept and diurnal decline were similar to those reported in previous models. There was a main effect of maternal age such that at 800h, cortisol levels were 2.7% higher per year older. Overall, morning cortisol levels were similar in first time versus experienced mothers, but there was a trend for primiparous mothers to display a 4.4% more gradual decline in cortisol per hour (95% CI: −0.6% to 9.6%) during the morning than multiparae (−12.7% decline per hour), t (86.47) = 1.74, p < .09. See Figure 1.
Figure 1.
Primiparae show a marginally less pronounced morning cortisol decline as compared to multiparae.
Interactions with Parity in the Prediction of the Maternal Cortisol Diurnal Rhythm
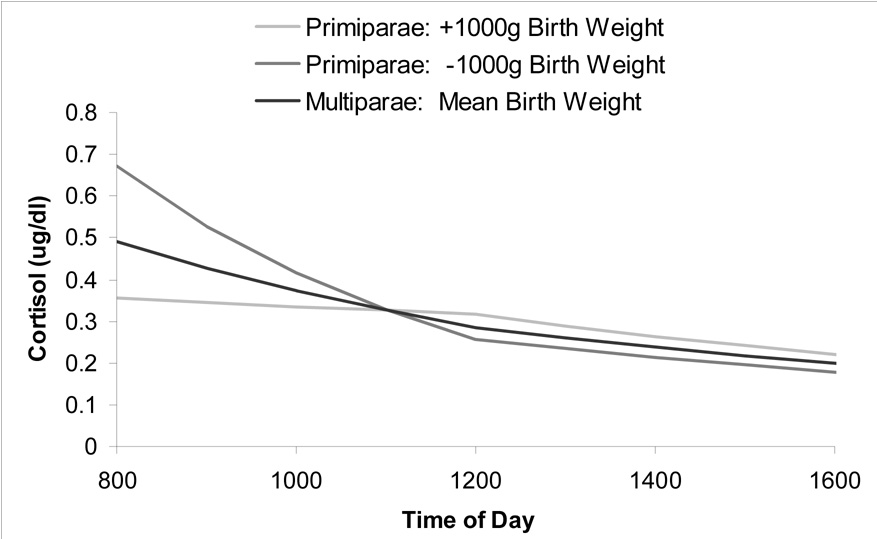
For the final model, all previously significant predictors were included with the addition of interaction terms to determine if parity status acted as a moderator of previously observed associations. Preliminary analyses revealed that neither trait anxiety nor size at birth differed by parity in this sample. Model parameters are presented in Table 5. The fit of the final model was a significant improvement over all prior models, ps < .01. There were no interactions between parity and trait anxiety. There was a significant birth weight by parity interaction in the prediction of the morning cortisol decline, such that there was an 11.0% flatter morning decline per +1 kg increase in birth weight among primiparae (95% CI: 0% to 23.0%). As a corollary to this finding, first time mothers of infants with a birth weight 1 kg below the mean (2449g) displayed an 11.0% steeper morning cortisol decline. See Figure 2.
Table 5.
Final Model Examining Interactions with Parity in the Prediction of the Maternal Cortisol Diurnal Rhythm During Late Pregnancy
| Fixed Effects: | Coefficient | SE | t | Interpretation |
|---|---|---|---|---|
| Predicting 8AM cortisol: | ||||
| Intercept | −.715*** | .066 | −10.79 | .499 µg/dl |
| Wake to Collection Interval | −.078** | .026 | −3.02 | −7.5% per hour |
| Maternal Age | .025** | .009 | 2.84 | +2.5% per year older |
| Trait Anxiety | −.005 | .004 | −1.27 | |
| Birth Weight | −.028 | .132 | −0.22 | |
| Parity (Primiparae) | .080 | .081 | 0.98 | |
| Birth Weight*Parity | −.315† | .183 | −1.73 | |
| Predicting Diurnal Decline: | ||||
| Morning Slope | −.135*** | .019 | −7.26 | −12.6% decline per hour |
| Maternal Age | −.005 | .003 | −1.86 | |
| Birth Weight | .000 | .038 | 0.01 | |
| Parity (Primiparae) | .039 | .024 | 1.64 | |
| Birth Weight*Parity | .104* | .053 | 1.96 | +11.0% flatter per kg for primps |
| Afternoon Slope | −.091*** | .013 | −7.08 | −8.7% decline per hour |
| Wake Interval | .015** | .006 | 2.68 | +1.5% flatter per hour |
| Trait Anxiety | .002* | .001 | 2.25 | +1.74% flatter per +1 SD |
p = .09
p < .05
p < .01
p < .001
Figure 2.
Parity moderates the predictive relationship between the maternal morning cortisol decline and infant birth weight. An 11% flatter morning slope was associated with a 1000 g increase in birth weight from the mean (3449 g) for primiparae (dark gray). As a corollary to this finding, an 11% steeper morning slope was associated with a 1000 g lower birth weight for this group (light gray). In contrast, the diurnal rhythm of cortisol was not associated with birth weight for multiparae (black). Note – Differences in cortisol levels at 800h are only marginally significant (p = .088) and are included in the figure to aid interpretation.
Discussion
The current findings both confirm and extend previous knowledge regarding the psychobiological regulation of the HPA axis during normative pregnancy with downstream implications for fetal growth and development. Women in the current study displayed the expected pattern of salivary cortisol decline across the day with a steeper decline in the morning and a more gradual slope in the afternoon. In addition, mean salivary cortisol levels (M = .35 µg/dl or 9.66 nmol/L) in this sample were similar to those reported by others for women in their 36th week of pregnancy (Alliolo et al., 1990; Meulenberg & Hofman, 1990), and approximately 1.5 times higher than mean values previously reported for non-pregnant controls (Alliolo et al., 1990; Meulenberg & Hofman, 1990). These observations confirm that women in this sample displayed the moderate elevations in salivary cortisol normal for late pregnancy.
In general, maternal psychological functioning had little impact on the cortisol diurnal rhythm of late pregnancy. This is in line with previous research, which has either failed to identify a link between measures of stress and cortisol during pregnancy (Petraglia et al., 2001; Urizar et al., 2004), or similar to this study, the observed correlations have been relatively small (Buitelaar et al., 2003; Diego et al., 2006). In the current study, greater maternal trait anxiety was associated with a mild flattening of the afternoon cortisol decline. This is consistent with reports of elevated evening cortisol levels among stressed pregnant women in their third trimester (Obel et al., 2005). Other studies of non-pregnant individuals have also reported that afternoon cortisol levels might be the most susceptible to the influence of psychological stress (Grossi, Perski, Lundberg, & Soares, 2001; Powell et al., 2002). Taken together, these findings suggest that the resetting of the HPA axis during pregnancy might overwhelm our ability to detect hormone-behavior associations, but that late afternoon might be the optimal time of day to uncover associations if they exist.
The maternal cortisol diurnal rhythm was also associated with neonatal birth outcomes in this sample. Both morning cortisol levels and the morning decline were linked with infant birth weight, such that higher morning cortisol levels and a steeper morning decline were associated with smaller neonates. Over-exposure to exogenous glucocorticoids has been linked to declines in fetal growth (for review, see Sloboda, Challis, Moss, & Newnham, 2005). Similarly, maternal urinary cortisol levels in the second trimester have been associated with reductions in estimated fetal weight in a low socioeconomic status, but medically low-risk group (Diego et al., 2006). Cortisol levels during the morning peak may have the greatest relevance for influencing fetal development. In mice, the greatest maternal-to-fetal glucocorticoid transfer occurs at the peak of the circadian rhythm due to saturation of the 11β-HSD enzyme (Venihaki, Carrigan, Dikkes, and Majzoub, 2000). If a similar process applies in human pregnancies, the chronobiological regulation of the HPA axis may represent one mechanism for the regulation of fetal growth.
The heaviest neonates were born to women with a relatively flat diurnal rhythm characterized by a blunted morning peak. In a non-pregnant population, similar diurnal patterns have been associated with both compromised health (Sephton, Sapolsky, Kraemer, & Spiegel, 2000; Wirtz et al., 2007) and cognitive functioning (Fiocco, Wan, Weekes, Pim & Lupien, 2006). Blunted awakening responses have also been observed among pregnant women with a history of childhood trauma (Shea et al., 2007). However, regulation of the diurnal rhythm of the HPA axis appears to be functionally altered during pregnancy. While the awakening response and stereotypical pattern of the diurnal decline in cortisol are maintained (de Weerth & Buitelaar, 2005; Magiakou et al. 1996), individual differences in the magnitude of the morning peak do not appear to be conserved into the postpartum period (de Weerth & Buitelaar, 2005). Blunting of the 24 hour rhythm during low-risk pregnancy has been reported (Cousins et al., 1983; Cousins, Yen, Meis, Halberg, & Brink, 1986) and lower morning cortisol levels have been observed in first pregnancies (Jones et al., 2006). Taken together, a flattening of the diurnal rhythm may be a common condition of pregnancy and may protect the fetus from overexposure to glucocorticoids during the morning peak.
The observed associations between cortisol and birth weight could be a proxy for alternative hormonal, immunological, or placental-derived regulatory mechanisms for fetal growth. One possibility is that maternal cortisol influences fetal growth via regulation of placental morphogenesis. There is a well-recognized positive association between placental and fetal growth (for review, see Jansson & Powell, 2007), and in studies of intrauterine growth restriction, decreased placental weight is usually evident prior to disruption of fetal growth (Hafner et al., 2003; Jansson, Thordstein, & Kjellmer, 1986). Animal studies have shown that experimentally-induced, modest elevations in cortisol reduce placental weight and alter placental blood flow and morphology, in addition to impairing fetal growth (Jensen, Gallaher, Breier, & Harding, 2002; Jensen, Wood, & Keller-Wood, 2005). Exposure to elevated morning cortisol levels could have influenced placental growth similarly in the current study. Preliminary findings in a subset of 27 women for whom placental weight was available also support this hypothesis. Placental and birth weight were highly correlated (r = .61) and morning cortisol levels were inversely associated with both placental weight (r = −.31) and birth weight (r = −.27).
Parity status was found to moderate the association between cortisol and birth weight, such that the relationship between the morning decline and infant birth weight was observed for first-born infants only. While overall differences in birth weight by parity were not observed in the current study, the link between parity and birth weight is well-recognized. In general, first pregnancies produce smaller neonates (Cogswell & Yip, 1995; Kramer, 1987) and a slower rate of fetal growth has been observed among the offspring of primiparae during the last trimester (de Jong et al., 1998). While physical factors, such as intrauterine space, may contribute to the determination of fetal growth (Cogswell & Yip, 1995), physiological differences may also be at play in first versus subsequent pregnancies (Ulijaszek et al., 1998). In addition to higher cortisol levels, Rasheed (1993) observed an association between cortisol levels in cord blood and birth weight / placental weight ratios in the infants of primiparae only. Regulation of fetal growth is complex and multifactorial and different mechanisms may be at play in first pregnancies (Rasheed, 1993).
A few limitations to the current study should be noted. The study relied on maternal report of saliva sample collection times for modeling the cortisol diurnal rhythm. While the study staff made it clear to participants that accuracy in reporting collection time was important, it is possible that some women may have abandoned accuracy in order to appear more compliant with the protocol. However, this circumstance would have only served to reduce our ability to detect significant associations. In addition, the use of filter paper for saliva collection in the current study may be open to scrutiny. Most studies have used filter discs as opposed to the filter strips applied in the present study. Poor reliability is associated with the diffusion properties of the discs compared to the strips. Filter discs are subject to super saturation whereas the linear shape of the filter strips allows excess saliva to move down a diffusion gradient resulting in more uniform wetting at the distal end. Participants were also instructed to wipe off excess saliva with their lips as the filter was removed which is not feasible with round discs. Finally, validation studies of the filter strip method have indicated that cortisol levels obtained from filter strip collection correlate with those from contemporaneous fluid saliva samples with an r2 > .90 (Neu et al, 2007).
Future work in this area should focus on the mechanisms responsible for the link between HPA axis regulation during late pregnancy and birth weight, with special attention to the multifactorial processes involved in fetal growth. Such work may also have implications for postnatal health and development. A growing body of epidemiological work has demonstrated that influences on fetal growth have the capacity to program postnatal physiology, metabolism, and vulnerability to stress resulting in predisposition for chronic disease (Barker, 2006). Over-exposure to glucocorticoids is hypothesized to play a major role in programming a variety of fetal tissues, including brain, heart, pancreas, and adipose tissues (for review, see Seckl & Meaney, 2004). Of particular interest, prenatal glucocorticoid exposure also sets the feedback sensitivity of the HPA axis, elevating basal cortisol levels in adulthood (Welberg, Seckl, & Holmes, 2001). The inverse association between morning cortisol levels and birth weight in this largely normative sample indicates that subtle glucocorticoid programming may have occurred in other fetal tissues as well. Given the increased potential for cortisol to cross the placental barrier at peak levels (Venihaki et al., 2000), investigation of the maternal cortisol diurnal rhythm as a predictor of fetal programming outcomes may be worthwhile. In particular, the cortisol awakening response could be essential for elucidating the role of HPA axis regulation in fetal growth and development.
In conclusion, the present study has demonstrated that daily chronobiological regulation of the HPA axis is open to influence by both parity status and trait anxiety during late pregnancy, and may be associated with the regulation of fetal growth during first, but not subsequent pregnancies. As maternal psychological functioning appears to have only a minor impact on the afternoon decline in cortisol, the diurnal rhythm does not appear to be a mediator of the effects of maternal self-reported stress on neonatal birth outcomes. Therefore, future work that identifies the factors responsible for the associations between the morning decline in maternal cortisol levels and birth weight will be invaluable to this area of inquiry.
Acknowledgements
This research was supported by awards from the NIH/NICHD (R01 HD27592) to Janet DiPietro; and from the NIAAA (AA013973) and the Developmental Psychobiology Endowment Fund, University of Colorado to Mark Laudenslager.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adam EK, Gunnar MR. Relationship functioning and home and work demands predict individual differences in diurnal cortisol patterns in women. Psychoneuroendocrinology. 2001;26:189–208. doi: 10.1016/s0306-4530(00)00045-7. [DOI] [PubMed] [Google Scholar]
- Affonso DD, Mayberry LJ, Lovett SM, Paul S. Cognitive adaptation to stressful events during pregnancy and postpartum: Development and testing of the case instrument. Nurs. Res. 1994;43:338–343. [PubMed] [Google Scholar]
- Allolio B, Hoffmann J, Linton EA, Winkelmann W, Kusche M, Schulte HM. Diurnal salivary cortisol patterns during pregnancy and after delivery: Relationship to plasma corticotrophin-releasing-hormone. Clin. Endocrinol. (Oxf.) 1990;33:279–289. doi: 10.1111/j.1365-2265.1990.tb00492.x. [DOI] [PubMed] [Google Scholar]
- Arizmendi TG, Affonso DD. Stressful events related to pregnancy and postpartum. J Psychosom. Res. 1987;31:743–756. doi: 10.1016/0022-3999(87)90023-7. [DOI] [PubMed] [Google Scholar]
- Benediktsson R, Calder AA, Edwards CR, Seckl JR. Placental 11 beta-hydroxysteroid dehydrogenase: A key regulator of fetal glucocorticoid exposure. Clin. Endocrinol. (Oxf.) 1997;46:161–166. doi: 10.1046/j.1365-2265.1997.1230939.x. [DOI] [PubMed] [Google Scholar]
- Barker DJ. Adult consequences of fetal growth restriction. Clin. Obstet. Gynecol. 2006;49:270–283. doi: 10.1097/00003081-200606000-00009. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Application of hierarchical linear models to assessing change. Psych. Bulletin. 1987;101:147–158. [Google Scholar]
- Buitelaar J, Huizink A, Mulder E, Robles de Medina P, Visser G. Prenatal stress and cognitive development and temperament in infants. Neurobiol. Aging. 2003;24:S53–S60. doi: 10.1016/s0197-4580(03)00050-2. [DOI] [PubMed] [Google Scholar]
- Cogswell ME, Yip R. The influence of fetal and maternal factors on the distribution of birthweight. Semin. Perinatol. 1995;19:222–240. doi: 10.1016/s0146-0005(05)80028-x. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc. Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Condon JT, Esuvaranathan V. The influence of parity on the experience of pregnancy: A comparison of first- and second- time expectant couples. Br J Med. Psychol. 1990;63:369–377. doi: 10.1111/j.2044-8341.1990.tb01632.x. [DOI] [PubMed] [Google Scholar]
- Cousins L, Rigg L, Hollingsworth D, Meis P, Halberg F, Brink G, et al. Qualitative and quantitative assessment of the circadian rhythm of cortisol in pregnancy. Am. J Obstet. Gynecol. 1983;145:411–416. doi: 10.1016/0002-9378(83)90309-5. [DOI] [PubMed] [Google Scholar]
- Cousins L, Yen SS, Meis P, Halberg F, Brink G. Circadian rhythm and diurnal excursion of plasma cortisol in diabetic pregnant women. Am. J Obstet. Gynecol. 1986;155:1176–1181. doi: 10.1016/0002-9378(86)90140-7. [DOI] [PubMed] [Google Scholar]
- de Jong CL, Gardosi J, Baldwin C, Francis A, Dekker GA, Geijn HPV. Fetal weight gain in a serially scanned high-risk population. Ultrasound Obstet. Gynecol. 1998;11:39–43. doi: 10.1046/j.1469-0705.1998.11010039.x. [DOI] [PubMed] [Google Scholar]
- de Weerth C, Buitelaar JK. Cortisol awakening response in pregnant women. Psychoneuroendocrinology. 2005;30:902–907. doi: 10.1016/j.psyneuen.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Demey-Ponsart E, Foidart JM, Sulon J, Sodoyez JC. Serum CBG, free and total cortisol and circadian patterns of adrenal function in normal pregnancy. J Steroid Biochem. 1982;16:165–169. doi: 10.1016/0022-4731(82)90163-7. [DOI] [PubMed] [Google Scholar]
- Diego MA, Jones NA, Field T, Hernandez-Reif M, Schanberg S, Kuhn C, et al. Maternal psychological distress, prenatal cortisol, and fetal weight. Psychosom. Med. 2006;68:747–753. doi: 10.1097/01.psy.0000238212.21598.7b. [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Costigan KA, Gurewitsch ED. Maternal psychophysiological change during the second half of gestation. Biol. Psychol. 2005;69:23–38. doi: 10.1016/j.biopsycho.2004.11.003. [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Ghera MM, Costigan KA, Hawkins M. Measuring the ups and downs of pregnancy. J Psychosom. Obstet. Gynecol. 2004;25:189–201. doi: 10.1080/01674820400017830. [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Millet S, Costigan KA, Gurewitsch E, Caulfield LE. Psychosocial influences on weight gain attitudes and behaviors during pregnancy. J Am. Diet Assoc. 2003;103:1314–1319. doi: 10.1016/s0002-8223(03)01070-8. [DOI] [PubMed] [Google Scholar]
- Fiocco AJ, Wan N, Weekes N, Pim H, Lupien SJ. Diurnal cycle of salivary cortisol in older adult men and women with subjective complains of memory deficits and/or depressive symptoms: relation to cognitive functioning. Stress. 2006;9:143–152. doi: 10.1080/10253890600965674. [DOI] [PubMed] [Google Scholar]
- Gitau R, Cameron A, Fisk N, Glover V. Fetal exposure to maternal cortisol. Lancet. 1998;352:707–708. doi: 10.1016/S0140-6736(05)60824-0. [DOI] [PubMed] [Google Scholar]
- Gitau R, Fisk NM, Teixeira JM, Cameron A, Glover V. Fetal hypothalamic-pituitary-adrenal stress responses to invasive procedures are independent of maternal responses. J Clin. Endocrinol. Metab. 2001;86:104–109. doi: 10.1210/jcem.86.1.7090. [DOI] [PubMed] [Google Scholar]
- Grossi G, Perski A, Lundberg U, Soares J. Associations between financial strain and the diurnal salivary cortisol secretion of long-term unemployed individuals. Int. Physiol. Behav. Sci. 2001;36:205–219. doi: 10.1007/BF02734094. [DOI] [PubMed] [Google Scholar]
- Hafner E, Metzenbauer M, Höfinger D, Munkel M, Gassner R, Schuchter K, et al. Placental growth from the first to the second trimester of pregnancy in SGA-foetuses and preeclamptic pregnancies compared to normal foetuses. Placenta. 2003;24:336–342. doi: 10.1053/plac.2002.0918. [DOI] [PubMed] [Google Scholar]
- Hollingshead A. Four factor index. New Haven: Yale University; 1975. [Google Scholar]
- Jansson T, Powell TL. Role of the placenta in fetal programming: underlying mechanisms and potential interventional approaches. Clin. Sci. 2007;113:1–13. doi: 10.1042/CS20060339. [DOI] [PubMed] [Google Scholar]
- Jansson T, Thordstein M, Kjellmer I. Placental blood flow and fetal weight following uterine artery ligation. Biol. Neonate. 1986;49:172–180. doi: 10.1159/000242528. [DOI] [PubMed] [Google Scholar]
- Jensen EC, Gallaher BW, Breier BH, Harding JE. The effect of a chronic maternal cortisol infusion on the late-gestation sheep. J Endocrinol. 2002;174:27–36. doi: 10.1677/joe.0.1740027. [DOI] [PubMed] [Google Scholar]
- Jensen EC, Wood E, Keller-Wood M. Chronic alterations in ovine maternal corticosteroid levels influence uterine blood flow and placental and fetal growth. Am. J Physiol. Regul. Integr. Comp. Physiol. 2005;288:R54–R61. doi: 10.1152/ajpregu.00149.2004. [DOI] [PubMed] [Google Scholar]
- Jones NM, Holzman CB, Zanella AJ, Leece CM, Rahbar MH. Assessing mid-trimester salivary cortisol levels across three consecutive days in pregnant women using an at-home collection protocol. Paediatr. Perinat. Epidemiol. 2006;20:425–437. doi: 10.1111/j.1365-3016.2006.00744.x. [DOI] [PubMed] [Google Scholar]
- Kramer MS. Intrauterine growth and gestational duration determinants. Pediatrics. 1987;80:502–511. [PubMed] [Google Scholar]
- Levine A, Zagoory-Sharon O, Feldman R, Lewis JG, Weller A. Measuring cortisol in human psychobiological studies. Physiol. Behav. 2007;90:43–53. doi: 10.1016/j.physbeh.2006.08.025. [DOI] [PubMed] [Google Scholar]
- Magiakou MA, Mastorakos G, Rabin D, Margioris AN, Dubbert B, Calogero AE, et al. The maternal hypothalamic-pituitary-adrenal axis in the third trimester of human pregnancy. Clin. Endocrinol. (Oxf.) 1996;44:419–428. doi: 10.1046/j.1365-2265.1996.683505.x. [DOI] [PubMed] [Google Scholar]
- Mastorakos G, Ilias I. Maternal and fetal hypothalamic-pituitary-adrenal axes during pregnancy and postpartum. Ann. N Y Acad. Sci. 2003;997:136–149. doi: 10.1196/annals.1290.016. [DOI] [PubMed] [Google Scholar]
- McTernan CL, Draper N, Nicholson H, Chalder SM, Driver P, Hewison M, et al. Reduced placental 11 beta-hydroxysteroid dehydrogenase type 2 mRNA levels in human pregnancies complicated by intrauterine growth restriction: An analysis of possible mechanisms. J Clin. Endocrinol. Metab. 2001;86:4979–4983. doi: 10.1210/jcem.86.10.7893. [DOI] [PubMed] [Google Scholar]
- Meulenberg PM, Hofman JA. The effect of oral contraceptive use and pregnancy on the daily rhythm of cortisol and cortisone. Clin. Chem. Acta. 1990;190:211–221. doi: 10.1016/0009-8981(90)90175-r. [DOI] [PubMed] [Google Scholar]
- Murphy VE, Zakar T, Smith R, Giles WB, Gibson PG, Clifton VL. Reduced 11 beta-hydroxysteroid dehydrogenase type 2 activity is associated with decreased birth weight centile in pregnancies complicated by asthma. J Clin. Endocrinol. Metabol. 2002;87:1660–1668. doi: 10.1210/jcem.87.4.8377. [DOI] [PubMed] [Google Scholar]
- Neu M, Goldstein M, Gao D, Laudenslager ML. Salivary cortisol in preterm infants: Validation of a simple method for collecting saliva for cortisol determination. Early Hum. Dev. 2007;83:47–54. doi: 10.1016/j.earlhumdev.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Nieto-Diaz A, Villar J, Matorras-Weinig R, Valenzuela-Ruíz P. Intrauterine growth retardation at term: association between anthropometric and endocrine parameters. Acta Obstet. Gynecol. Scand. 1996;75:127–131. doi: 10.3109/00016349609033303. [DOI] [PubMed] [Google Scholar]
- Norbeck JS, Anderson NJ. Life stress, social support, and anxiety in mid- and late-pregnancy among low-income women. Res. Nurs. Health. 1989;12:281–287. doi: 10.1002/nur.4770120503. [DOI] [PubMed] [Google Scholar]
- Obel C, Hedegaard M, Henriksen T, Secher N, Olsen J, Levine S. Stress and salivary cortisol during pregnancy. Psychoneuroendocrinology. 2005;30:647–656. doi: 10.1016/j.psyneuen.2004.11.006. [DOI] [PubMed] [Google Scholar]
- Paige DM, Villar J. Fetal and maternal nutrition. In: Lifshitz F, editor. Pediatric Nutrition: Infant feedings – deficiencies – diseases. New York: Marcel Dekker, Inc; 1982. pp. 3–34. [Google Scholar]
- Petraglia F, Hatch M, Lapinski R, Stomati M, Reis F, Cobellis L, et al. Lack of effect of psychosocial stress on maternal corticotropin-releasing factor and catecholamine levels at 28 weeks gestation. J Soc. Gynecol. Invest. 2001;8:83–88. [PubMed] [Google Scholar]
- Powell LH, Lovallo WR, Matthews KA, Meyer P, Midgely AR, Baum A, et al. Physiological markers of chronic stress in premenopausal, middle-aged women. Psychosom. Med. 2002;64:502–509. doi: 10.1097/00006842-200205000-00015. [DOI] [PubMed] [Google Scholar]
- Rasheed F. Parity, birthweight, and cortisol. Lancet. 1993;341:828. doi: 10.1016/0140-6736(93)90602-d. [DOI] [PubMed] [Google Scholar]
- Sandman CA, Glynn L, Schetter CD, Wadhwa P, Garite T, Chicz-DeMet A, et al. Elevated maternal cortisol early in pregnancy predicts third trimester levels of placental corticotropin releasing hormone (CRH): Priming the placental clock. Peptides. 2006;27:1457–1463. doi: 10.1016/j.peptides.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Scott EM, McGarrigle HH, Lachelin GC. The increase in plasma and saliva cortisol levels in pregnancy is not due to the increase in corticosteroid-binding globulin levels. J Clin. Endocrinol. Metab. 1990;71:639–644. doi: 10.1210/jcem-71-3-639. [DOI] [PubMed] [Google Scholar]
- Seckl JR, Meaney MJ. Glucocorticoid programming. Ann. N Y Acad. Sci. 2004;1032:63–84. doi: 10.1196/annals.1314.006. [DOI] [PubMed] [Google Scholar]
- Sephton SE, Sapolsky RM, Kraemer HC, Spiegel D. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl. Cancer Inst. 2000;92:884–1000. doi: 10.1093/jnci/92.12.994. [DOI] [PubMed] [Google Scholar]
- Shams M, Kilby MD, Somerset DA, Howie AJ, Gupta A, Wood PJ, et al. 11 Beta-hydroxysteroid dehydrogenase type 2 in human pregnancy and reduced expression in intrauterine growth restriction. Hum. Reprod. 1998;13:799–804. doi: 10.1093/humrep/13.4.799. [DOI] [PubMed] [Google Scholar]
- Shea AK, Streiner DL, Fleming A, Kamath MV, Broad K, Steiner M. The effect of depression, anxiety, and early life trauma on the cortisol awakening response during pregnancy: preliminary results. Psychoneuroendocrinology. 2007;32:1013–1020. doi: 10.1016/j.psyneuen.2007.07.006. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Sloboda DM, Challis JR, Moss TJ, Newnham JP. Synthetic glucocorticoids: Antenatal administration and long-term implications. Curr. Pharm. Des. 2005;11:1459–1472. doi: 10.2174/1381612053507873. [DOI] [PubMed] [Google Scholar]
- Spielberger C. Manual for the state-trait anxiety inventory (Form Y) Palo Alto, CA: Mind Garden, Inc; 1983. [Google Scholar]
- Stewart PM, Whorwood CB, Mason JI. Type 2 11 beta-hydroxysteroid dehydrogenase in foetal and adult life. J Steroid Biochem. Mol. Biol. 1995;55:465–471. doi: 10.1016/0960-0760(95)00195-6. [DOI] [PubMed] [Google Scholar]
- Strinic T, Roje D, Marusic J, Capkun V. Cord blood cortisol level is lower in growth-restricted newborns. J Obstet. Gynaecol. Res. 2007;33:144–150. doi: 10.1111/j.1447-0756.2007.00493.x. [DOI] [PubMed] [Google Scholar]
- Tanner JM. Foetus into man. Ware: Castlemead Publications; 1989. [Google Scholar]
- Tu MT, Lupien SJ, Walker CD. Diurnal salivary cortisol levels in postpartum mothers as a function of infant feeding choice and parity. Psychoneuroendocrinology. 2006;31:812–824. doi: 10.1016/j.psyneuen.2006.03.006. [DOI] [PubMed] [Google Scholar]
- Ulijaszek SJ, Johnston F, Preece M. The Cambridge encyclopedia of human growth and development. Cambridge: Cambridge University Press; 1998. [Google Scholar]
- Urizar G, Milazzon M, Le H, Delucchi K, Sotelo R, Munoz R. Impact of stress reduction instructions on stress and cortisol levels during pregnancy. Biol. Psychol. 2004;67:275–282. doi: 10.1016/j.biopsycho.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Venihaki M, Carrigan A, Dikkes P, Majzoub JA. Circadian rise in maternal glucocorticoid prevents pulmonary dysplasia in fetal mice with adrenal insufficiency. Proc. Natl. Acad. Sci. USA. 2000;97:7336–7341. doi: 10.1073/pnas.97.13.7336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vleugels M, Eling W, Rolland R, de Graaf R. Cortisol levels in human pregnancy in relation to parity and age. Am. J Obstet. Gynecol. 1986;155:118–121. doi: 10.1016/0002-9378(86)90092-x. [DOI] [PubMed] [Google Scholar]
- Wadhwa P. Psychoneuroendocrine processes in human pregnancy influence fetal development and health. Psychoneuroendocrinology. 2005;30:724–743. doi: 10.1016/j.psyneuen.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Dunkel-Schetter C, Chicz-DeMet A, Porto M, Sandman CA. Prenatal psychosocial factors and the neuroendocrine axis in human pregnancy. Psychosom. Med. 1996;58:432–446. doi: 10.1097/00006842-199609000-00006. [DOI] [PubMed] [Google Scholar]
- Weinstock M. The potential influence of maternal stress hormones on development and mental health of the offspring. Brain Behav. Immun. 2005;19:296–308. doi: 10.1016/j.bbi.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Welberg LAM, Seckl JR, Holmes MC. Prenatal glucocorticoid programming of brain corticosteroid receptors and corticiotrophin-releasing hormone: possible implications for behaviour. Neuroscience. 2001;104:71–79. doi: 10.1016/s0306-4522(01)00065-3. [DOI] [PubMed] [Google Scholar]
- Wirtz PH, von Känel R, Emini L, Ruedisueli K, Groessbauer S, Maercker A, et al. Evidence for altered hypothalamus-pituitary-adrenal axis functioning in systemic hypertension: blunted cortisol response to awakening and lower negative feedback sensitivity. Psychoneuroendocrinology. 2007;32:430–436. doi: 10.1016/j.psyneuen.2007.02.006. [DOI] [PubMed] [Google Scholar]
- Yali A, Lobel M. Coping and distress in pregnancy: An investigation of medically high risk women. J Psychosom. Obstet. Gynecol. 1999;20:39–52. doi: 10.3109/01674829909075575. [DOI] [PubMed] [Google Scholar]