Abstract
Combination therapy of angiotensin-converting enzyme (ACE) inhibition and AT1 receptor blockade has been shown to provide greater renoprotection than ACE inhibitor alone in human diabetic nephropathy, suggesting that ACE-independent pathways for ANG II formation are of major significance in disease progression. Studies were performed to determine the magnitude of intrarenal ACE-independent formation of ANG II in type II diabetes. Although renal cortical ACE protein activity [2.1 ± 0.8 vs. 9.2 ± 2.1 arbitrary fluorescence units (AFU)·mg−1·min−1] and intensity of immunohistochemical staining were significantly reduced and ACE2 protein activity (16.7 ± 3.2 vs. 7.2 ± 2.4 AFU·mg−1·min−1) and intensity elevated, kidney ANG I (113 ± 24 vs. 110 ± 45 fmol/g) and ANG II (1,017 ± 165 vs. 788 ± 99 fmol/g) levels were not different between diabetic and control mice. Afferent arteriole vasoconstriction due to conversion of ANG I to ANG II was similar in magnitude in kidneys of diabetic (−28 ± 3% at 1 μM) and control (−23 ± 3% at 1 μM) mice; a response completely inhibited by AT1 receptor blockade. In control kidneys, afferent arteriole vasoconstriction produced by ANG I was significantly attenuated by ACE inhibition, but not by serine protease inhibition. In contrast, afferent arteriole vasoconstriction produced by intrarenal conversion of ANG I to ANG II was significantly attenuated by serine protease inhibition, but not by ACE inhibition in diabetic kidneys. In conclusion, there is a switch from ACE-dependent to serine protease-dependent ANG II formation in the type II diabetic kidney. Pharmacological targeting of these serine protease-dependent pathways may provide further protection from diabetic renal vascular disease.
Keywords: afferent arteriole, juxtamedullary nephron, db/db mouse, angiotensin-converting enzyme, serine protease, angiotensinogen, angiotensin-converting enzyme 2
diabetic nephropathy is a microvascular complication of type II diabetes mellitus which causes progressive chronic kidney disease, often leading to end-stage renal disease. Pharmacological agents that inhibit the actions of ACE and AT1 receptors delay the onset and slow the progression of diabetic nephropathy in humans, indicating the importance of the renin-angiotensin system (RAS) in diabetic renal disease. However, ACE inhibitors and AT1 receptor blockers do not arrest disease progression to end-stage renal failure. Additionally, the demonstration that combined ACE inhibitor plus AT1 receptor blocker lowers blood pressure (2, 25) and provides greater protection in diabetic nephropathy (13, 27) than ACE inhibitor alone suggests that suppression of the RAS is incomplete. It has been suggested that dual blockade of RAS with inhibition of ACE and AT1 receptor blockade results in an additional reduction in proteinuria in patients with chronic kidney disease (5). Thus ACE inhibitor monotherapy may allow for the continued generation of ANG II via ACE-independent pathways.
Recently, there has been growing interest in the role of ACE-independent ANG II production in various physiological and pathophysiological states. ACE-independent enzymatic pathways include serine proteases, tonin, cathepsin G, trypsin, and kallikrein (38). Vascular chymase is a major serine protease (EC 3.4.21.39) implicated in the ACE-independent production of ANG II in human arteries (23, 31). Chymase, which cleaves ANG I at the same site as ACE, is completely inhibited by serine protease inhibitors; ACE inhibitors do not influence chymase activity (40). Markedly increased chymase expression in mesangial and vascular smooth muscle cells in human diabetic nephropathy (12), IgA nephropathy (33), and hypertensive nephropathy (44) has been reported. The involvement of renal mast cell chymase activity in ANG II generation has also been reported in patients with autosomal dominant polycystic kidney disease (24). Therefore, ACE-independent formation of ANG II may contribute significantly to progression of many forms of renal disease.
The db/db mouse (BKS.Cg-Dock7m +/+ Leprdb/J) is an animal model of type II diabetes which has a point mutation in the leptin receptor gene (22) that leads to hyperphagia, obesity, progressive hyperglycemia, hyperinsulinemia, and insulin resistance. Diabetic db/db mice exhibit progressive diabetic renal disease characterized by renal and glomerular hypertrophy, albuminuria, glomerulosclerosis, and mesangial matrix expansion, which are features of human diabetic nephropathy (3, 19, 47). Ye et al. (46) have demonstrated that renal cortical ACE protein expression is reduced, while ACE2 protein expression is elevated in diabetic db/db compared with control db/m mice. Elevated ACE2 protein expression is thought to provide a renoprotective effect on diabetic renal injury due to the ability of ACE2 to degrade ANG II and generate ANG1-7. ANG1-7 is a peptide with vasodilator and antiproliferative properties (21). The impact of altered ACE and ACE2 protein expression on intrarenal ANG II formation has not been determined in this model. We recently reported that the renal afferent arteriole vasoconstrictor responses to ANG II remain intact in db/db mice (28). However, the functional consequence of reductions in ACE enzyme activity on the intrarenal formation of ANG II from ANG I on the renal microvasculature of type II diabetes has not been previously investigated.
In the current study, we tested the hypothesis that there is a switch from renal ACE-dependent to ACE-independent ANG II formation in the progression of diabetic vascular disease. The leptin receptor deficient db/db animal model was utilized to study the renal complications of diabetes with an emphasis on afferent arteriole vascular function. Plasma ANG II and kidney and heart ANG I and ANG II levels were determined in control and diabetic mice. Also, kidney and heart ACE and ACE2 activity and protein expression, and urinary excretion of angiotensinogen, were measured. Studies on renal resistance vessel reactivity were carried out using the mouse in vitro blood-perfused juxtamedullary technique, which allows for direct videomicroscopic visualization of afferent arteriolar diameters studied in situ in kidneys obtained from control and diabetic mice. Renal afferent arteriolar vascular responses to the intrarenal conversion of ANG I to ANG II in the absence or presence of enzymatic inhibitors provided a mechanism for investigating the physiological responses to ACE-dependent and ACE-independent pathways for the formation of ANG II in the diabetic mouse kidney.
METHODS
Animals
The procedures used in this study were approved by the Institutional Animal Care and Use Committee of Louisiana State University Health Sciences and conducted according to the National Institutes of Health Guide for the Care and Use of Laboratory Animals. Experiments were performed in a total of 71 male (18 wk old) control db/m (Dock7m +/+ Leprdb) and 69 diabetic db/db (BKS.Cg-Dock7m +/+ Leprdb/J) mouse littermates (stock no. 000642, The Jackson Laboratory, Bar Harbor, ME). Adult male Sprague-Dawley rats (502 ± 8 g body wt, n = 83; Charles River Laboratories, Raleigh, NC) were used as blood donors for the study of the mouse renal microvasculature. All animals were provided ad libitum access to food and water during the study except when food was removed during the time preceding fasted blood glucose measurements. Fasting blood glucose levels were measured in conscious diabetic (n = 27) and control (n = 24) mice housed in the home cage following 18 h of food removal (3 P.M.-9 A.M., Onetouch Ultra 2 Blood Glucose Meter, Lifescan, Milpitas, CA). Measurements were taken ∼1 wk before performance of the renal microcirculation experiments. Fed blood glucose measurements were also obtained in conscious diabetic (n = 20) and control (n = 20) mice on the morning of the preparation for renal microcirculation experiments. Mice were housed individually in metabolic cages specially designed for obese mice for a 3-day equilibration period. The 24-h urine samples were obtained for measurements of urinary angiotensinogen levels by ELISA (16) in diabetic (n = 8) and control (n = 10) mice.
ACE and ACE2 Activities
Kidney cortex, heart, and lung tissues were harvested from diabetic (n = 8) and control (n = 9) mice under pentobarbital sodium anesthesia (90 mg/kg ip). Tissues were homogenized briefly with a glass homogenizer in reaction buffer (30∼50 mg of tissue in 300∼400 μl of reaction buffer; 1 mM NaCl, 75 mM Tris, 0.5 mM ZnCl2, pH 7.5) and centrifuged at 14,000 g for 10 min. Protein concentrations were determined using a commercially available BCA kit (Pierce, Rockford, IL), and samples were stored at −20°C until assayed. Lung tissues from control mice were used for a positive control for ACE and negative control for ACE2 enzymatic activity. ACE and ACE2 activities were assessed using Fluorogenic Peptide Substrate VI [FPSVI; 7Mca-Y-V-A-D-A-PK (Dnp)-OH; R&D Systems, Minneapolis, MN] as we have previously described (7). Samples containing 100 μg of renal cortical, heart, or lung protein extract were incubated with 100 μM of FPSVI, 20 μM captopril (to inhibit ACE activity) or 1 μM DX600 (to inhibit ACE2 activity) in a final volume of 100 μl of reaction buffer to measure total ACE or ACE2 activity. Nonspecific enzyme activity was measured by including the ACE inhibitor (10 μM captopril) and ACE2 inhibitor (1 μM DX600) in the reaction mixture. Fluorescence emission was monitored using a SpectraMax M2 Fluorescence Reader (Molecular Devices) at 10-min intervals for 2 h. Specific ACE activity was calculated by subtracting the activity in the presence of both 10 μM captopril and 1 μM DX600 from the total activity in the presence of 1 μM DX600. ACE2 activity was calculated by subtracting the activity in the presence of both 10 μM captopril and 1 μM DX600 from the total activity in the presence of 10 μM captopril. Data (arbitrary fluorescence units; AFU) were presented as amounts of substrate FPSVI converted to product per minute and were normalized for total protein (AFU·mg−1·min−1).
Blood was also collected from these anesthetized, open-chest mice via cardiac puncture using a 25-G needle and 1-ml syringe containing EDTA (200 mM) and centrifuged at 1,000 g for 10 min, and the plasma was stored at −20°C until assayed. Plasma leptin and insulin levels were measured using commercially available ELISA kits according to the manufacturer's instructions (Mouse Leptin ELISA Kit EZML-82K, Linco Research; Mercodia Ultrasensitive Mouse Insulin ELISA 10-1150-01), respectively.
Renal ACE and ACE2 Immunohistochemistry
In vivo retrograde perfusion fixation (3% paraformaldehyde) was performed in anesthetized diabetic (n = 6) and control (n = 6) mice as we have previously described (11, 29). After fixation, the kidneys were routinely processed to paraffin and sectioned at 5 μm. Immunohistochemistry was performed on kidney sections incubated with the primary Ab or nonimmune serum, washed, and developed using the Vectastain ABC immunoperoxidase system as we have previously described (11, 29). Kidney sections from each animal were incubated with the following antibodies: 1) mouse ACE-specific goat IgG (1:1,000 and 1:2,000, AF1513; R&D Systems), and 2) mouse ACE2-specific rabbit IgG (9) (1:8,000 and 1:10,000). For densitometric analysis of the immunoreactivity for ACE (1:2,000) and ACE2 (1:8,000) protein expression, 6–11 microscopic fields of renal cortex/tissue section/animal were obtained using a ×40 objective and identical image exposure camera settings for all tissue sections with the microscopist blinded to the animal groups as we have previously described (29, 30). Combined tubular and endothelial ACE protein expression was quantified for intensity of immunostaining. Representative color micrographs were obtained from kidney sections immunostained for ACE (1:1,000) and ACE2 (1:10,000) using ×40 and ×100 objectives from control and diabetic kidneys.
Plasma ANG II and Tissue ANG I and ANG II Levels
Blood, kidneys, and hearts were harvested from conscious control (n = 11) and diabetic (n = 11) mice following decapitation. Trunk blood was collected into chilled tubes containing EDTA (5 mM), enalaprilat (20 μM), pepstatin A (10 μM), and 1,10-phenanthroline (1.25 mM) as we have previously described (14). Plasma was separated and stored at −20°C until assayed. Immediately after removal, kidneys and hearts were weighed and then homogenized in ice-cold methanol. ANG I and ANG II levels were quantitated by RIA as previously reported (14).
Mouse In Vitro Blood-Perfused Juxtamedullary Nephron Technique
Experiments were conducted using the mouse in vitro blood-perfused juxtamedullary nephron technique as we have previously reported in detail (10, 28). Briefly, mice were anesthetized with pentobarbital sodium (90 mg/kg ip), the right renal artery was cannulated, the upper third of the cortex was removed, the distal arteries were tied, and the pelvic mucosa and connective tissues were removed, revealing the juxtamedullary nephrons. The kidney was placed on the stage of a microscope, and the afferent arteriole was visualized using a video camera, image enhancer, and recorded on a DVD. Kidneys were studied under euglycemic (5 mM = 110 mg/dl glucose) and hyperglycemic (30 mM = 540 mg/dl glucose) incubation conditions (5% BSA perfusion solution, 1% BSA superfusion solution, rat plasma) for control and diabetic mice, respectively (28). Donor blood was collected from anesthetized rats subjected to bilateral nephrectomy and exsanguinated via a carotid arterial cannula. Rat plasma was spiked with glucose (4 mg of glucose/ml of plasma) to achieve a final concentration of 30 mM (526 ± 14 mg/dl, n = 18) for the perfusion of kidneys obtained from diabetic mice. The kidney was bathed with warmed Tyrode buffer containing 1% BSA and perfused with blood pressurized to 95 mmHg with 95% O2-5% CO2. Peptides and drugs were added to the 5% BSA perfusion solution and/or 1% BSA superfusion and/or rat plasma. A minimum of 15 min was allowed for equilibration of the renal vasculature upon initiation of the blood perfusion. Baseline afferent arteriole diameters were measured during control conditions (1% BSA solution superfusion, 5 min). Each protocol was followed by a 15-min recovery period. Afferent arteriole diameters were measured during the following protocols.
Protocol 1: ANG I.
Afferent arteriole diameters were measured during superfusion with ANG I to determine the vascular effects of intrarenal conversion of ANG I to ANG II in kidneys of diabetic (n = 10) and control (n = 12) mice. Kidneys were exposed to 1, 10, 100, and 1,000 nM human ANG I (catalog no. 002-01, Phoenix Pharmaceuticals) applied in the superfusion solution for 5-min periods each. Only one ANG I dose-response was performed in each kidney. ANG I substrate availability was not limiting in this experimental method since the rate of delivery of ANG I via the superfusion is ∼10–20 ml/min. In one diabetic kidney, two afferent arterioles were visualized during exposure to ANG I, and both vessel diameters were analyzed.
Protocol 2: ANG I in the presence of AT1 receptor blockade.
Kidneys were superfused with the AT1 receptor antagonist (100 μM candesartan; kindly provided by AstraZeneca) for 10 min followed by 1, 10, and 100 nM ANG I for 5-min periods each in diabetic (n = 7) and control (n = 6) mice. Since it was expected that the AT1 receptor antagonist would block the vasoconstriction resulting from conversion of ANG I to ANG II, the vasoconstrictor response to 1 μM norepinephrine (3 min) was examined in the same vessels at the conclusion of the experiment.
Protocol 3: ANG I in the presence of ACE inhibition.
Captopril (catalog no. C4042, Sigma) was used for ACE inhibition in control and diabetic mice. Mice were pretreated using an injection of captopril (100 mg/kg ip) 30 min before kidney harvesting (4). Captopril (1 mM final concentration) was also added to the perfusion and superfusion solutions to ensure continuous ACE blockade throughout the entire experiment. The effects of ANG I (1, 10, 100 nM, 5-min period each) in the presence of ACE inhibition on afferent arteriolar diameter were measured in diabetic (n = 6) and control (n = 6) mice. The response to 100 nM ANG II was examined in the same vessels at the conclusion of the experiment.
Protocol 4: ANG I in the presence of serine protease inhibition.
PMSF (catalog no. P7626, Sigma) was used for inhibition of serine proteases in kidneys of diabetic and control mice. Mice were pretreated with an injection of PMSF (3 mg ip) 30 min before kidney harvesting, and PMSF (1 mM final concentration) was added to the perfusion and superfusion solutions to ensure continuous enzymatic blockade (40). The effects of ANG I (1, 10, 100 nM, 5-min period each) in the presence of serine protease inhibition on afferent arteriole diameter were measured in diabetic (n = 6) and control (n = 6) mice. The response to 100 nM ANG II was determined in the same vessels at the conclusion of the experiment. The stock solution of PMSF was diluted in 100% anhydrous ethanol (final concentration in perfusion and superfusion solutions 0.33% ethanol). Diluent control experiments were performed to determine the effect of 0.33% ethanol on renal vascular reactivity to ANG I in diabetic (n = 8) and control mice (n = 8).
Protocol 5: ANG I in the presence of both ACE and serine protease inhibition.
The effects of ANG I (1, 10, 100 nM, 5-min period each) in the presence of the combination of ACE and serine protease inhibition on afferent arteriole diameter were measured in diabetic (n = 6) and control (n = 7) mice. The response to 100 nM ANG II was determined in the same vessels at the conclusion of the experiment.
Data Analyses and Statistics
Renal arterial perfusion pressure and vessel diameters were sampled at 1 Hz and converted to a digital form using analog-to-digital data-acquisition and -analysis software as we have previously described (28, 42). Afferent arteriolar luminal diameters were measured manually and continuously throughout the protocol at a single site along the length of the afferent arteriole using a digital image-shearing monitor. Afferent arterioles were studied at a site from the glomerulus of 25–50% along the length of the vessel. The average diameter (μm) during the control (5 min), ANG I or ANG II (5 min), AT1 receptor antagonist (final 5 min), norepinephrine (3 min), and recovery (final 5 min) periods was used for statistical analysis. The peak diameter (μm) responses during the 5-min application of ANG I were also determined. The EC50 was determined for afferent arteriole dose-responses to ANG I and ANG II (ANG II data obtained from Ref. 28) by measuring the concentration of the peptide that produced a half-maximal effect. Statistical analyses were performed on the raw data by one-way repeated-measures or two-way ANOVA followed by Dunnett's or Bonferroni's test. Because of the significant difference in baseline afferent arteriole diameters between control and diabetic mice, two-way ANOVA was conducted on the percent change from the baseline diameter for the afferent arteriole responses to all peptides and drugs. A paired or unpaired t-test was used as appropriate. Statistical analyses were performed using a statistical software program (SigmaStat 3.5, Systat Software). P ≤ 0.05 was considered statistically significant. Values are presented as means ± SE (n = no. of arterioles, no. of tissues, or no. of mice as appropriate).
RESULTS
Metabolic Parameters
Experiments were performed in 18-wk-old adult male control db/m (Dock7m ++ Leprdb) and diabetic db/db (BKS.Cg-Dock7m +/+ Leprdb/J) mouse littermates. Body weight and fed and fasting blood glucose levels were significantly elevated in diabetic compared with control mice at 18 wk of age (Table 1). Fed blood glucose levels were significantly higher than fasting blood glucose levels in both groups. As there was no negative feedback on plasma leptin levels due to loss of leptin receptor signaling, plasma leptin levels were significantly higher in diabetic compared with control mice. Plasma insulin levels were significantly higher in diabetic compared with control mice. There were no differences in kidney weight or tibia length between control and diabetic mice. Right kidney weight was significantly greater than left kidney weight in each group. Heart weight was significantly reduced in diabetic compared with control mice. These diabetic mice exhibited significant albuminuria (822 ± 365 vs. 28 ± 8 μg/day, n = 11–12) as we have published previously (28).
Table 1.
Metabolic parameters of control and diabetic mice
| Control | n | Diabetic | n | |
|---|---|---|---|---|
| BW g | 29.7±0.3 | 71 | 53.7±0.7* | 69 |
| Fed blood glucose, mg/dl | 154±6 | 20 | 534±18* | 20 |
| Fasting blood glucose, mg/dl | 137±6† | 24 | 400±16*† | 27 |
| Plasma leptin, ng/ml | 5.1±0.8 | 9 | 106±20* | 9 |
| Plasma insulin, μg/l | 1.9±0.7 | 9 | 20±6* | 8 |
| Total kidney wt, mg | 384±7 | 20 | 392±9 | 20 |
| Right kidney wt, mg | 201±4‡ | 20 | 203±5‡ | 20 |
| Left kidney wt, mg | 183±3 | 20 | 190±5 | 20 |
| Heart wt, mg | 131±4 | 20 | 114±2* | 20 |
| Left tibia length, mm | 18.0±0.2 | 9 | 17.6±0.3 | 9 |
Values are means ± SE. BW, body wt.
P < 0.05 vs. control.
P < 0.05 vs. fed.
P < 0.05 vs. left kidney.
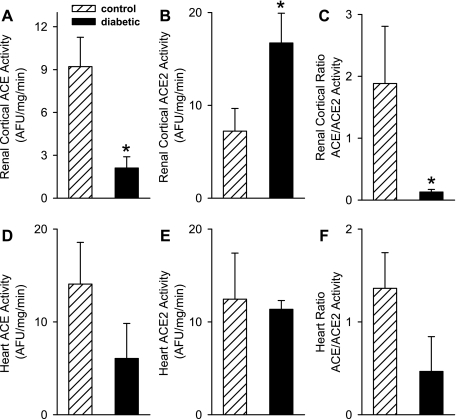
ACE and ACE2 Activities in Renal Cortex, Heart, and Lung
Renal cortical ACE activity was significantly decreased (Fig. 1A, 2.1 ± 0.8 vs. 9.2 ± 2.1 AFU·mg−1·min−1, n = 8, 8), while ACE2 activity was significantly increased (Fig. 1B, 16.7 ± 3.2 vs. 7.2 ± 2.4 AFU·mg−1·min−1, n = 8, 8) in diabetic compared with control mice. The ACE/ACE2 ratio in kidneys was significantly lower in diabetic compared with control mice (Fig. 1C, 0.13 ± 0.04 vs. 1.88 ± 0.92). However, ACE and ACE2 activities, and ACE/ACE2 ratios were similar in the hearts of diabetic and control mice (Fig. 1D, 6.1 ± 3.8 vs. 14.1 ± 4.5 AFU·mg−1·min−1, P = 0.20, n = 5; Fig. 1E, 11.4 ± 0.9 vs. 12.4 ± 5.0 AFU·mg−1·min−1: n = 4–5; Fig. 1F, 0.47 ± 0.37 vs. 1.36 ± 0.38). Lung ACE (29.9 ± 5.6 AFU·mg−1·min−1: n = 4) and ACE2 (4.1 ± 1.0 AFU·mg−1·min−1: n = 4) activities were measured in control mice. In tissues of control mice, the lung ACE/ACE2 ratio (9.8 ± 4.3) was significantly greater than the renal cortical ACE/ACE2 ratio.
Fig. 1.
Angiotensin-converting enzyme (ACE; A and D) and ACE2 (B and E) enzymatic activities and ACE/ACE2 ratios (C and F) in renal cortex (A; n = 8: B; n = 8: C; n = 7, 8) and heart (D; n = 5: E; n = 4–5: F; n = 4, 5) of control (hatched bars) and diabetic (filled bars) mice. Renal cortical ACE activity was significantly lower (P = 0.003) and ACE2 activity was significantly higher (P = 0.02) in diabetic compared with control mice. There were no differences in ACE (P = 0.1) and ACE2 (P = 0.4) activities in the heart of control and diabetic mice. Ratios of ACE/ACE2 activities were significantly reduced in the renal cortex (P = 0.03) of diabetic compared with control mice; however, there were no significant differences in the heart (P = 0.07). *P ≤ 0.05 control vs. diabetic.
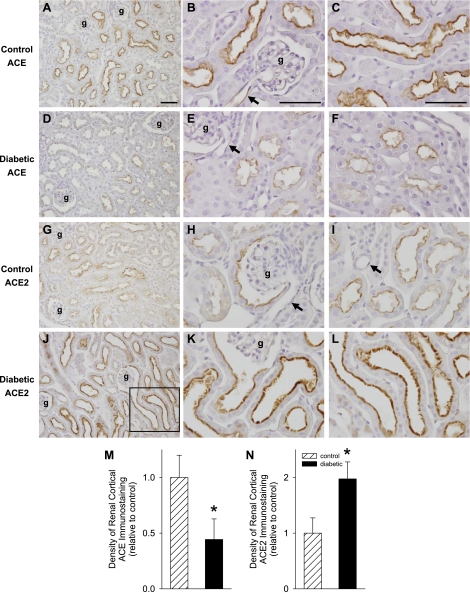
ACE and ACE2 Protein Immunohistochemical Localization and Quantitative Analysis
ACE protein immunohistochemical localization was determined in kidney sections of control (Fig. 2, A–C, n = 6) and diabetic (Fig. 2, D–F, n = 5) mice. ACE protein expression is localized to the proximal tubule brush border and endothelial cells of both renal vasculature and glomerular capillaries of mouse kidneys (Fig. 2, A–F). Quantitative analysis of the density of ACE protein immunostaining (Fig. 2M) indicated that ACE protein expression (arbitrary units relative to control) is significantly reduced in the diabetic (0.4 ± 0.2) compared with control (1.0 ± 0.2) kidneys. ACE2 protein immunohistochemical localization was determined in kidney sections of control (Fig. 2, G–I, n = 6) and diabetic (Fig. 2, J–L, n = 6) mice. ACE2 protein expression is localized to the proximal tubule brush border (Fig. 2, G–L). Endothelial cells do not stain for ACE2 protein (Fig. 2, H and I). The number and intensity of ACE2 positively stained proximal tubules were qualitatively greater in diabetic compared with control kidneys. High-power magnification of the inset in Fig. 2J is illustrated in Fig. 2L. Note the intense ACE2 immunostaining in the proximal tubule brush border of the diabetic kidney. ACE2 immunostaining density (Fig. 2N) is significantly greater in diabetic compared with control kidneys (2.0 ± 0.3 vs. 1.0 ± 0.3).
Fig. 2.
ACE (A–F) and ACE2 (G–L) immunohistochemical localization and quantitative analysis (M; n = 6, 5: N; n = 6, 6) of renal cortex of control (A–C, G–I, hatched bars) and diabetic (D–F, J–L, filled bars) mice. ACE and ACE2 proteins are localized to the proximal tubule brush border of control and diabetic kidneys. ACE is also expressed in endothelial cells of the renal vasculature and glomerular capillaries. The density (M) of renal cortical ACE protein immunostaining is significantly reduced in diabetic compared with control kidneys. However, ACE2 immunostaining density (N) is significantly greater in diabetic compared with control kidneys. Antibody dilutions for ACE and ACE2 antibodies were 1:1,000 and 1:10,000, respectively. Images were obtained from the midcortical region of the kidney using a ×40 (A, D, G, J) or ×100 oil-immersion lens (B and C, E and F, H and I, K and L). g, Glomerulus; arrows, endothelial cells; inset in J indicates higher magnification in L. Bar = 50 μm. *P < 0.05 control vs. diabetic.
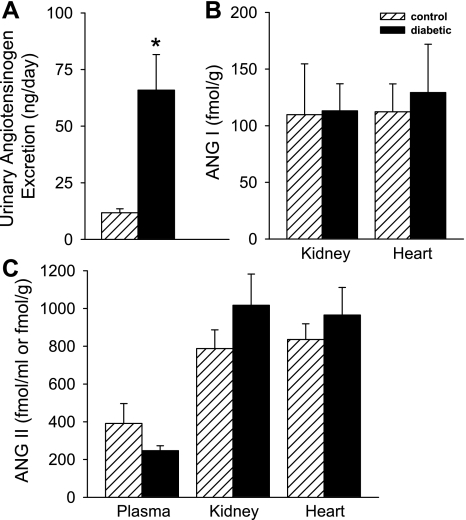
Urinary Angiotensinogen Excretion, ANG I, and ANG II Peptide Levels
Urinary angiotensinogen excretion was significantly higher in diabetic compared with control mice (66 ± 16 vs. 12 ± 2 ng/day, n = 8–10) (Fig. 3A) and was significantly correlated with urinary albumin excretion (r = 0.412, P < 0.01). Kidney ANG I and ANG II levels were not different between control and diabetic mice (110 ± 45 and 788 ± 99 vs. 113 ± 24 and 1,017 ± 165 fmol/g, n = 7–11) (Fig. 3, B and C). Plasma ANG II levels were similar in control and diabetic mice (391 ± 105 vs. 247 ± 26 fmol/ml, n = 10; P = 0.20) (Fig. 3C). Cardiac ANG I and ANG II levels were not different between control and diabetic mice (112 ± 25 and 836 ± 83; 129 ± 43 and 965 ± 147 fmol/g, n = 4–10, respectively) (Fig. 3, B and C). Despite reduced ACE activity, ANG II levels in diabetic kidneys were not different compared with control kidneys.
Fig. 3.
Urinary angiotensinogen excretion (A) was significantly higher in diabetic (filled bars, n = 8) compared with control (hatched bars, n = 10) mice. ANG I peptide levels (B) in kidney (n = 7, 10) and heart (n = 5, 4) were not significantly different between control and diabetic mice. Also, ANG II peptide levels (C) in plasma (n = 10, 10), kidney (n = 11, 11), and heart (n = 10, 10) were not different between control and diabetic mice. *P < 0.05 control vs. diabetic.
Baseline Afferent Arteriole Diameters
To determine the influence of the type II diabetic condition on afferent arteriole tone, baseline diameters from all arterioles from each group were pooled for statistical analysis. Baseline afferent arteriole diameters of kidneys from diabetic mice averaged 14.3 ± 0.5 μm (n = 44) and was significantly larger than in kidneys from control mice, which averaged 12.2 ± 0.3 μm (n = 45).
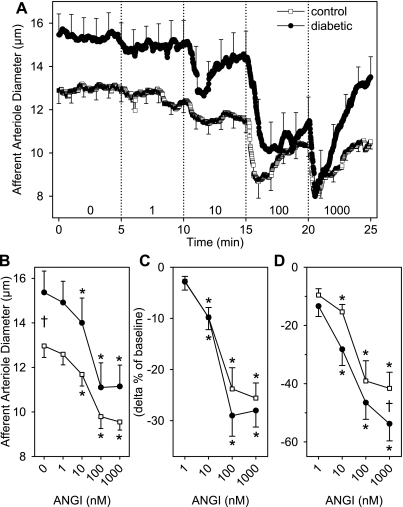
Afferent Arteriole Vasoconstrictor Responses to ANG I
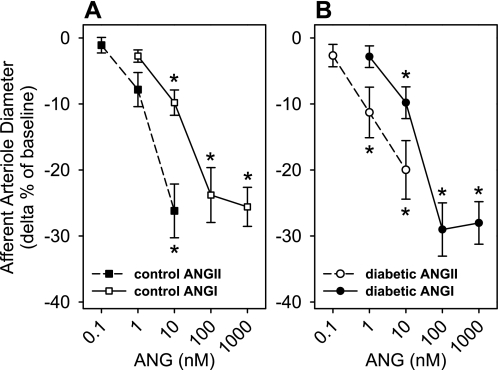
Figure 4A demonstrates the time course of the afferent arteriole vasoconstriction to 1, 10, 100, and 1,000 nM ANG I in kidneys of control and diabetic mice. ANG I produced a significant vasoconstriction of afferent arterioles of both groups. There was no significant difference in the waning effects (average response over the final 30 s of each dose) of ANG I (1, 10, 100, 1,000 nM) in control (−6 ± 2, −11 ± 2, −20 ± 3, −20 ± 3% of baseline) and diabetic (−2 ± 5, −4 ± 5, −25 ± 5, −15 ± 5% of baseline) kidneys, respectively. Figure 4B illustrates the average afferent arteriole responses plotted in micrometers, and Fig. 4C illustrates the average afferent arteriole responses plotted as the delta % of baseline to ANG I (1–1,000 nM) in kidneys from control and diabetic mice. Significant afferent arteriole vasoconstriction to 10, 100, 1,000 nM ANG I was observed in kidneys of control (−10 ± 2, −24 ± 4, −26 ± 3%, n = 12) and diabetic mice (−10 ± 2, −29 ± 4, −28 ± 3%, n = 11) (Fig. 4C). ANG I produced similar responses in afferent arterioles from control and diabetic mice (P = 0.3). Significant peak afferent arteriole vasoconstriction to 10, 100, and 1,000 nM ANG I was observed in kidneys of control (−15 ± 3, −39 ± 7, −42 ± 6%) and diabetic (−28 ± 6, −47 ± 6, −54 ± 6%) (Fig. 4D) mice. ANG I produced a significantly greater peak vasoconstriction in afferent arterioles from diabetic compared with control mice (P = 0.01). The time from application of the peptide to the peak vasoconstrictor responses to 1, 10, 100, and 1,000 nM ANG I in control (158 ± 34, 148 ± 28, 110 ± 22, 40 ± 8 s) and diabetic (151 ± 29, 116 ± 15, 133 ± 22, 34 ± 5 s) kidneys was similar (P = 0.7). The time to reach the peak vasoconstriction to 1,000 nM ANG I was significantly shorter than all of the lower doses of ANG I in kidneys of diabetic mice. The time to reach the peak vasoconstriction to 1,000 nM ANG I was significantly shorter than for 10 and 1 nM ANG I in kidneys of control mice. A maximal vasoconstriction was observed with 100 nM ANG I; 1,000 nM ANG I did not produce a further vasoconstriction. Afferent arteriole diameters of control and diabetic kidneys had not completely returned to the baseline values following the 15-min recovery period (93 ± 3 and 93 ± 2% of baseline, respectively). The afferent arteriole responses to ANG I are compared with the ANG II responses that we have previously published (28) in control (Fig. 5A) and diabetic (Fig. 5B) kidneys. Since the afferent arteriole responses to ANG II and ANG I were not significantly different between kidneys of control and diabetic mice, the data were collapsed. The EC50 values for ANG II and ANG I were 2.5 ± 0.5 (n = 21) and 48.2 ± 11.1 nM (n = 20), respectively. The EC50 values for ANG II and ANG I were significantly different (P = 0.0001). There was a 20-fold shift to the right in the vasoconstrictor response to ANG I compared with ANG II. The ANG I dose-response could not be repeated in the same kidney due to a significant 40% reduction in the afferent arteriole response to the second application of ANG I in diabetic kidneys (−29 ± 6 vs. −17 ± 5%, first vs. second, at 100 nM ANG I, n = 6). Two consecutive norepinephrine dose responses (100, 300, 1,000 nM) were performed with a 20-min recovery between the first and second applications in kidneys of C57BL6 mice (n = 6). There was no significant difference in the magnitude of the afferent arteriole vasoconstriction between of the first and second applications of norepinephrine (−11 ± 5, −24 ± 6, −36 ± 6% and −6 ± 3, −26 ± 7, −41 ± 7%, first vs. second). Afferent arterioles exhibited full recovery to baseline diameters upon removal of norepinephrine from the bath.
Fig. 4.
Afferent arteriole diameter responses to ANG I (0, 1, 10, 100, 1,000 nM) in kidneys of control (□, n = 12) and diabetic (·, n = 11) mice. The average time course (A, μm), average diameter (B, μm; C, delta % of baseline), and peak diameter (D, delta % baseline) responses to increasing ANG I concentrations are shown for kidneys from control and diabetic mice. Afferent arterioles from control and diabetic mice responded with a significant reduction in diameter with increasing concentrations of ANG I (P < 0.05). The magnitude of the average afferent arteriolar vasoconstrictor responses was not significantly different between control and diabetic mice, although the peak afferent arteriole responses were significantly different. The average afferent arteriolar responses of kidneys from control and diabetic mice to 1,000 nM ANG I was not significantly different from the responses at 100 nM ANG I, indicating a maximal response at 100 nM ANG I. Baseline afferent arteriole diameters were significantly larger in diabetic compared with control mice. *P ≤ 0.05 vs. baseline diameter. †P ≤ 0.05 control vs. diabetic.
Fig. 5.
Afferent arteriole responses (delta % of baseline) to ANG I (1–1,000 nM, solid lines) and ANG II (0.1–1 nM, dashed lines) in kidneys from control (A, squares) and diabetic (B, circles) mice. The afferent arteriole responses to ANG II of control and diabetic mice have been replotted from our previously published study (28). The EC50 values for ANG II and ANG I were 2.5 ± 0.5 (n = 21) and 48.2 ± 11.1 nM (n = 20), respectively (P < 0.05). *P ≤ 0.05 vs. baseline diameter.
Afferent Arteriole Responses to ANG I in the Presence of AT1 Receptor Blockade
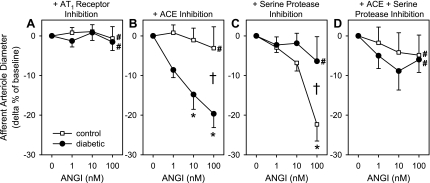
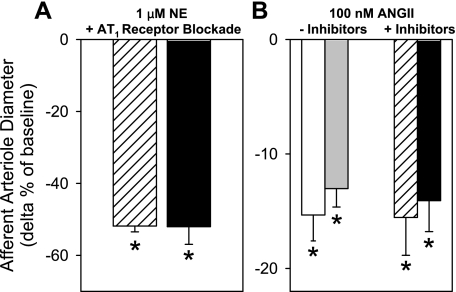
The afferent arteriole vasoconstrictor response to ANG I was significantly attenuated by AT1 receptor blockade in both groups (Fig. 6A). Pretreatment with an AT1 receptor blocker (100 μM candesartan) did not produce a change from the baseline diameter in either group. In the presence of AT1 receptor blockade, afferent arteriole diameters were 1 ± 2 and −1 ± 3% of the baseline in control (n = 6) and 1 ± 2 and −2 ± 2% of baseline in diabetic (n = 7) mice in response to 10 and 100 nM ANG I, respectively. During the recovery periods, afferent arteriole diameters of control and diabetic kidneys were not significantly different than baseline diameters. Renal microvascular responses to 1 μM norepinephrine were determined in the same vessels that demonstrated attenuated vasoconstrictor responsiveness to ANG I in the presence of AT1 receptor blockade. Norepinephrine produced a rapid and significant vasoconstriction in afferent arterioles of control and diabetic kidneys (−52 ± 2, −52 ± 5%; n = 6–7, respectively) (Fig. 7A), and there was no significant difference between the groups.
Fig. 6.
Afferent arteriole average diameter responses (delta % of baseline) to ANG I (0, 1, 10, 100 nM) in the presence of AT1 receptor blockade (A; n = 6, 7), ACE inhibition (B; n = 6, 6), serine protease inhibition (C; n = 6, 6), or combined ACE and serine protease inhibition (D; n = 7, 6) in kidneys of control (□) and diabetic (·) mice. Afferent arteriole vasoconstriction produced by ANG I was significantly attenuated by AT1 receptor blockade, ACE inhibition, combined ACE and serine protease inhibition, but not by serine protease inhibition alone in kidneys of control mice. Afferent arteriole vasoconstriction produced by ANG I was significantly attenuated by AT1 receptor blockade, serine protease inhibition, and combined ACE and serine protease inhibition, but not by ACE inhibition alone in kidneys of diabetic mice. *P ≤ 0.05 vs. baseline diameter. †P ≤ 0.05 control vs. diabetic. #P ≤ 0.05 vs. ANG I alone.
Fig. 7.
A: afferent arteriole responses (delta % of baseline) to 1 μM norepinephrine in the presence of AT1 receptor blockade in kidneys from control (hatched bar, n = 6) and diabetic (filled bar, n = 7) mice. There were no significant differences in the magnitude of the afferent arteriole vasoconstrictor responses to norepinephrine in control compared with diabetic mice. B: afferent arteriole responses to 100 nM ANG II in the absence (control, open bar, n = 11; diabetic, gray bar, n = 12) or presence (control, hatched bar, n = 18; diabetic, filled bar, n = 16) of enzymatic inhibition of ANG I conversion to ANG II. There were no significant differences in the magnitude of afferent arteriole vasoconstriction to ANG II in the absence compared with the presence of inhibitors in kidneys of diabetic compared with control mice. *P ≤ 0.05 vs. baseline diameter.
Afferent Arteriole Vascular Responses to ANG I in the Presence of ACE Inhibition
The vasoconstriction produced by conversion of ANG I to ANG II was significantly attenuated by ACE inhibition in control mice (−1 ± 3, −3 ± 5% at 10 and 100 nM ANG I, respectively, n = 6) (Fig. 6B). However, in the kidneys of diabetic mice the average afferent arteriole vasoconstriction produced by cleavage of ANG I to ANG II was not altered by ACE inhibition (−15 ± 4, −20 ± 4% at 10 and 100 nM ANG I, respectively, n = 6) (Fig. 6B). There was a significant difference in the magnitude of the peak afferent arteriole vasoconstriction to ANG I in the presence of ACE inhibition between control (−10 ± 2, −10 ± 5%) and diabetic (−22 ± 4, −32 ± 4% at 10 and 100 nM ANG I) mice, respectively. There was a significant difference in the enzymatic conversion of ANG I to ANG II during ACE inhibition between kidneys of diabetic and control mice. Afferent arteriole diameters were not different from baseline at the end of the recovery periods in the two groups.
Afferent Arteriole Vascular Responses to ANG I in the Presence of Serine Protease Inhibition
To identify an ACE-independent pathway that might be responsible for the conversion of ANG I to ANG II in kidneys of diabetic mice, experiments were conducted using serine protease inhibition. The average afferent arteriole vasoconstriction produced by ANG I to ANG II was significantly attenuated by serine protease inhibition in diabetic mice (−2 ± 3, −6 ± 6% at 10 and 100 nM ANG I, respectively, n = 6) (Fig. 6C). However, afferent arteriole vasoconstriction produced by cleavage of ANG I to ANG II was not altered by serine protease inhibition in control mice (−7 ± 2, −22 ± 4% at 10 and 100 nM ANG I, respectively, n = 6) (Fig. 6C). There was a significant difference in the magnitude of the peak afferent arteriole vasoconstriction to ANG I in the presence of serine protease inhibition between control (−15 ± 3, −34 ± 7%) and diabetic (−9 ± 3, −13 ± 6% at 10 and 100 nM ANG I) mice, respectively. There was a significant difference in the enzymatic conversion of ANG I under serine protease inhibition between the kidneys of diabetic and control mice. The afferent arteriole vasoconstrictor response due to the conversion of ANG I to ANG II was not affected by the solvent used for dissolving PMSF (0.33% EtOH; n = 8). There was no significant difference in the effect of 0.33% EtOH on the conversion of ANG I to ANG II compared with vasoconstrictor response to ANG I alone in kidneys of diabetic (n = 8) and control (n = 8) mice.
ANG I in the Presence of both ACE and Serine Protease Inhibition
Afferent arteriole vasoconstriction produced by conversion of ANG I to ANG II was significantly attenuated by the combination of ACE and serine protease inhibition compared with the responses to ANG I alone in kidneys of diabetic and control mice (Fig. 6D). There was no significant difference in the responses to ANG I in the presence of combined blockade of ACE and serine protease between diabetic and control kidneys. Afferent arteriole diameters following the recovery period were not different compared with baseline diameters in both groups.
In summary, in control mice, average afferent arteriole vasoconstriction produced by conversion of ANG I to ANG II was significantly attenuated by AT1 receptor blockade, ACE inhibition, and combined ACE and serine protease inhibition (−1 ± 3, −3 ± 5, and −5 ± 5% of baseline at 100 nM ANG I), but not by serine protease inhibition alone (−22 ± 4%). Importantly, the average afferent arteriole vasoconstriction produced by conversion of ANG I to ANG II was not altered by ACE inhibition (−20 ± 3% of baseline at 100 nM ANG I) in diabetic mice. Afferent arteriole vasoconstriction produced by cleavage of ANG I to ANG II was prevented by AT1 receptor blockade, serine protease inhibition, and combined ACE and serine protease inhibition (−2 ± 2, −6 ± 6, and −6 ± 3% of baseline at 100 nM ANG I) in kidneys of diabetic mice.
A significant afferent arteriole vasoconstriction to a single dose of ANG II (100 nM) was observed in control (−15 ± 2%, n = 11) and diabetic (−13 ± 2%, n = 12) kidneys in the absence of enzymatic inhibitors (Fig. 7B). At the conclusion of the enzyme inhibitor experiments, afferent arteriole contractile responsiveness to ANG II remained intact in control (−15 ± 3%, n = 18) and diabetic (−14 ± 3%, n = 16) kidneys (Fig. 7B). The magnitude of the ANG II-induced vasoconstriction in the absence or presence of pharmacological inhibitors of ACE and/or serine protease was not significantly different between kidneys of control and diabetic mice.
DISCUSSION
The most significant finding of the present study is the identification of serine proteases as the major pathway for the formation of ANG II in the type II diabetic leptin receptor-deficient mouse kidney. Intrarenally formed ANG II from the substrate ANG I produces a potent afferent arteriole vasoconstriction in the presence of ACE inhibition in the diabetic kidney. However, in the normal kidney, afferent arteriolar vasoconstriction to intrarenally formed ANG II is blocked by ACE inhibition. Inhibition of serine proteases abolished the afferent arteriole response to intrarenal conversion of ANG I to ANG II in the diabetic kidney, but not the control kidney. These studies provide a potential explanation for the mechanism involved in the superior effects of combining an ACE inhibitor with an AT1 receptor antagonist relative to ACE inhibitor therapy alone to provide additional protection from diabetic nephropathy in humans (1, 13). In addition, the presence of this ACE-independent pathway for ANG II formation may explain the continued proteinuria in some patients on maximal ACE inhibitor therapy (5). We suggest that ACE inhibitor monotherapy may allow for the continued generation of ANG II via these ACE-independent pathways.
The experimental model selected to perform these studies involves the adult (18 wk) male type II diabetic mouse which exhibits obesity, hyperglycemia, hyperleptinemia, hyperinsulinemia, and albuminuria. Renal hypertrophy was not observed, although heart weight was reduced in our study. Previous studies have indicated that renal hypertrophy is only observed in younger (8 wk) diabetic db/db mice (34). The changes in body weight and organ weight were not related to a change in tibial length, suggesting that the growth of diabetic mice is not different from control mice.
Recently, Ye et al. (46) reported that renal cortical ACE activity and protein expression are reduced, while ACE2 activity is elevated in young, female diabetic db/db mice which do not display signs of diabetic renal disease. These alterations in ACE and ACE2 activity were not observed in the diabetic heart (46). Additionally, proximal tubule immunohistochemical protein expression of ACE was reduced, while ACE2 protein expression was elevated in diabetic compared with control mice (46). We performed the present study to determine whether an imbalance of intrarenal ACE and ACE2 also exists in the older male diabetic mouse with renal disease. In agreement with Ye et al., we also found that renal cortical ACE activity was reduced in kidneys of diabetic compared with control mice, while renal cortical ACE2 activity was elevated. There was no difference in ACE or ACE2 activity in the heart between the groups, indicating that this effect may be kidney specific. Wysocki et al. (45) have demonstrated that renal cortical ACE protein expression is reduced, while ACE2 protein expression is elevated in streptozocin-induced type I diabetic compared with control mice. Additionally, proximal tubule expression of ACE was reduced and ACE2 was elevated in streptozocin-induced type I diabetic compared with control mice (37). Therefore, the pattern of change in intrarenal ACE and ACE2 is similar in mouse models of types I and II diabetes and suggests that hyperglycemia may be the common regulator. In addition, Ferrario et al. (8) have shown that inhibition of ACE results in augmented renal cortical ACE2 activity. Since ACE is involved in the formation of ANG II from ANG I while ACE2 degrades ANG II to ANG1-7, one might predict that a decreased ACE/ACE2 ratio might result in lower intrarenal ANG II peptide levels in diabetes. However, kidney ANG peptide levels were not measured in these earlier studies.
We performed the next series of experiments to determine the impact of reduced ACE activity and elevated ACE2 activity on intrarenal ANG II peptide levels in the diabetic kidney. To our surprise, ANG I and ANG II levels in the kidney were not different between control and diabetic mice. Plasma ANG II levels and cardiac ANG I and ANG II levels were also similar in control and diabetic mice. Wei et al. (43) have shown that although plasma ANG II is undetectable and kidney ACE activity is significantly reduced in ACE null mice, the elevation in ACE-independent (likely chymase) ANG II formation produces kidney ANG II levels that are not different from wild-type mice. However, Campbell et al. (4) demonstrated a significant suppression of ANG II in the kidney of mice with reduced somatic ACE gene expression. The data of Wei et al. (43) in the ACE null mice are consistent with our findings of reduced ACE activity, yet similar ANG I and ANG II peptide levels in the diabetic kidney, and suggest that intrarenal ACE-independent pathways for ANG II formation may predominate in the diabetic kidney.
Additionally, the urine concentration of angiotensinogen was determined in our study. We found a significant increase in the urinary excretion of angiotensinogen in diabetic compared with control mice, suggesting that substrate availability is increased in the diabetic kidney and may support ACE-independent formation of ANG II. Singh et al. (35) have shown that increased formation of ANG II in glomerular mesangial cells cultured in high glucose is mediated by increased angiotensinogen and ANG I levels. Miyata et al. (26) have shown increased intrarenal angiotensinogen protein levels in type II diabetic rats. Also, in the present study, urinary excretion of angiotensinogen was significantly correlated with urinary excretion of albumin, suggesting that the rise in intrarenal production of angiotensinogen correlates with the severity of the renal disease. Although urinary protein excretion in deoxycorticosterone acetate salt-induced volume-dependent hypertensive rats was increased to the same or greater extent than in ANG II-dependent hypertensive rats, urinary angiotensinogen excretion was significantly lower in volume-dependent than in ANG II-dependent hypertensive rats and was not greater than in control rats (17). Kobori et al. (18) have demonstrated that urinary angiotensinogen levels were enhanced in chronic kidney disease patients compared with control subjects. The source of urinary angiotensinogen is thought to be from angiotensinogen that is formed and secreted by the proximal tubules and not from plasma (15). Therefore, our data are consistent with recent studies indicating that urinary angiotensinogen levels could be a new therapeutic diagnostic test for the progression of diabetic renal disease.
Renal hemodynamic dysfunction plays a central role in the pathophysiological consequences of diabetic renal disease. We have previously reported that db/db diabetic mice display normal blood pressure and reductions in circadian blood pressure amplitude, heart rate, and locomotor activity (28). In addition, renal microvascular vasoconstrictor responses to bath-applied ANG II were not altered in diabetic compared with control mice (28). The afferent arteriole responses to ANG II were not significantly different in kidneys of control and diabetic kidneys incubated under acute euglycemic or hyperglycemic conditions (28). However, the vasoconstrictor response to bath-applied ANG I has not been previously reported in juxtamedullary afferent arterioles of rodent kidneys. In our studies, the baseline afferent arteriole diameter was significantly larger in diabetic compared with control kidneys as we have previously reported (28). Intrarenal conversion of ANG I to ANG II by ACE and/or ACE-independent pathways produced a rapid and potent dose-dependent afferent arteriole vasoconstriction in diabetic and control mice. The average afferent arteriole responses to conversion of ANG I to ANG II were not different between diabetic and control kidneys, although the magnitude of the peak response to ANG I was significantly greater in the diabetic compared with control kidneys. ANG II synthesized via ACE and/or ACE-independent pathways within the renal endothelium, microvasculature, glomerulus, and/or interstitium may act in an autocrine/paracrine manner via binding to plasma membrane AT1 receptors located on afferent arteriolar vascular smooth muscle cells. The afferent arteriole responses to intrarenal conversion of ANG I to ANG II are mediated by AT1 receptors, as evidenced by complete blockade of the responses in the presence of candesartan in diabetic and control mice. The time to reach peak afferent arteriole vasoconstriction to ANG I was not different between diabetic and control kidneys. This may indicate that the AT1 receptor intracellular signaling response time is the same and/or enzymatic rates of conversion of ANG I to ANG II via ACE-dependent and ACE-independent pathways are similar. We found rapid and significant arteriolar vascular contractile response to norepinephrine in the presence of AT1 receptor blockade. Therefore, we document a maintained vascular contractile responsiveness of the arterioles which lacked a response to ANG I in the presence of AT1 receptor blockade. Future studies will determine the major enzymatic pathways for ANG II formation in the efferent arterioles of diabetic and control mice.
It is generally thought that ACE is the primary route of ANG II formation in the kidney. Campbell et al. (4) have demonstrated a 97 and 92% reduction in plasma and kidney ANG II levels, respectively, following acute ACE inhibitor treatment in mice, indicating that ACE is the predominant pathway of ANG II formation in blood and tissues of normal mice. In agreement with these reports, we found that afferent arteriole vasoconstriction produced by intrarenal conversion of ANG I to ANG II was blocked by ACE inhibition in control kidneys. Interestingly, ACE inhibition did not affect afferent arteriole vasoconstriction produced by intrarenal conversion of ANG I to ANG II in diabetic kidneys. Inhibition of conversion of ANG I to ANG II by captopril indicates that ACE is the predominant pathway for ANG II formation in the normal mouse kidney. Our findings support a novel role of ACE-independent formation of ANG II in the diabetic kidney.
In the present study, afferent arteriole vasoconstriction produced by ANG I to ANG II was significantly attenuated by serine protease inhibition in kidneys of diabetic mice, but not in control mice. Afferent arteriole vasoconstriction produced by intrarenal conversion of ANG I to ANG II was attenuated by the combination of ACE and serine protease inhibition in both diabetic and control kidneys. These data support our hypothesis that serine proteases are the major enzymatic pathway for ANG II formation in diabetes.
A review by Urata et al. (41) carefully outlines the involvement of ACE inhibitor-insensitive ANG II formation in the cardiovascular system and highlights the importance of these pathways for the mechanisms that contribute to pathophysiological changes in cardiovascular diseases. Less is known about ACE-independent formation of ANG II in renal disease. Urata et al. have demonstrated that in normal human serum, ANG II formation is completely inhibited by the ACE inhibitor captopril, but not by SBTI or PMSF, indicating that ACE is the main enzyme involved in plasma ANG II formation. Interestingly, the majority of the ANG II-forming activity in the human heart is not inhibited by ACE inhibitors or aprotinin, but is inhibited by the serine protease inhibitors SBTI or PMSF, suggesting that chymase is the main enzyme involved in ANG II formation in the human heart in vitro. It has been shown that the formation of ANG II from ANG I in human coronary arteries is dependent on both ACE (captopril inhibitable) and ACE-independent (chymostatin inhibitable) pathways (23). Seventy percent of the vasoconstrictor effect of ANG I is due to ACE, while serine proteases account for the remaining 30% in rat afferent and muscular efferent arterioles (39). Therefore, formation of ANG II by serine proteases contributes a minor effect on pre-and postglomerular responses in the rat kidney. Our findings of a major influence of ACE-independent formation of ANG II in the diabetic kidney are consistent with the predominant ACE-independent ANG II-forming pathways in the human heart.
Alternative pathways for converting ANG I to ANG II that do not require ACE have been recognized for a long time. There is accumulating evidence in humans and experimental animals of a major contribution of ACE-independent ANG II formation in the heart, vasculature, and kidney. Studies carried out in cultured myocytes, vascular smooth muscle cells, mesangial cells, and podocytes suggest that high glucose is a regulator of ACE-dependent and ACE-independent ANG II formation. ANG II peptide formation was increased in concert with increased protein expression of angiotensinogen, renin, and chymase in myocytes exposed to high glucose, although ACE protein expression was not altered (36). High glucose decreased expression of ACE, downregulated ACE-dependent ANG II generation, and upregulated chymase-dependent ANG II generation in rat vascular smooth muscle cells (20). Singh et al. (35) have shown increased formation of ANG I and ANG II in glomerular mesangial cells cultured in high glucose. Durvasula and Shankland (6) recently reported that hyperglycemia-induced activation of chymase-dependent ANG II formation in podocytes may promote progressive podocyte injury and loss in diabetic nephropathy. Activation of ANG II formation by ACE-independent mechanisms by high-glucose conditions indicates the need for new therapeutic strategies for treatment of vascular complications in diabetes.
In the kidney, markedly increased chymase expression and upregulated ACE expression in mesangial and vascular smooth muscle cells in human diabetes have been reported (12). The involvement of renal mast cell chymase activity in ANG II generation has also been reported in patients with autosomal dominant polycystic kidney disease (24). Upregulation of ACE-independent ANG II production is observed in the clipped kidney, but not the nonclipped kidney of renal vascular hypertensive rats, contributing to the maintenance of similar ANG II levels in clipped and nonclipped kidneys (32). These data suggest that ACE-independent pathways may be activated in the absence of hyperglycemia and may be driven by ischemia. Most importantly, our data represent that serine protease inhibition produced a complete blockade of the ANG I-to-ANG II-induced vasoconstriction in diabetic kidney. These data indicate a major pathway for serine protease-dependent ANG II formation in diabetic kidneys. Therefore, the concept of ACE-independent production of ANG II in pathogenic conditions involving the heart, vasculature, and kidney seem to solidify the concept that inhibition of these pathways may lead to new effective therapeutic approaches.
In summary, we demonstrated that ACE-independent mechanisms and increased intrarenal synthesis of angiotensinogen contribute to the intrarenal production of ANG II in diabetes. In kidneys of control mice, afferent arteriole vasoconstrictor responses are mediated by ACE-dependent conversion of ANG I to ANG II. In contrast, afferent arteriole vasoconstrictor responses to conversion of ANG I to ANG II in kidneys of diabetic mice were not altered by ACE inhibition. Interestingly, in the diabetic kidney, afferent arteriole vasoconstriction is mediated by serine protease-dependent conversion of ANG I to ANG II. Our future studies will determine whether chymase is responsible for serine protease-dependent ANG II formation in the diabetic kidney. Therefore, taken together, our findings in the diabetic kidney of reduced renal ACE activity and protein expression, maintained renal ANG I and ANG II peptide levels, elevated intrarenal formation of angiotensinogen, combined with functional afferent arteriolar vasoconstrictor responses to intrarenally produced ANG II from ANG I which are serine protease inhibitable and unresponsive to ACE inhibition, we conclude that serine protease-dependent formation of ANG II may be a new pharmacotherapeutic target for reducing diabetic renal vascular disease.
GRANTS
This work was supported by National Institutes of Health (NIH) Grants DK62003 (to L. M. Harrison-Bernard), P20 RR018766 (to L. M. Harrison-Bernard and E. Lazartigues), P20RR017659 (to D. M. Seth and H. Kobori), and HL-56973 (to M. C. Chappell) and by American Heart Association (AHA) Predoctoral Grant 0715445B (to S. Park).
Portions of this work have been published in abstract form in Hypertension 50: e99, 21, 2007; J Am Soc Nephrol 18: 167A, 2007; and FASEB J. 22: 944.1–944.5, 2008.
DISCLOSURES
No conflicts of interest are declared by the authors.
ACKNOWLEDGMENTS
The authors acknowledge the excellent technical assistance of Dr. Akemi Sato in the measurements of urinary angiotensinogen concentration and Dr. Yumei Feng for ACE and ACE2 activity analyses. Dr. Anders Ljunggren (Astra Hassle, Gothenburg, Sweden) generously provided the AT1 receptor antagonist candesartan.
REFERENCES
- 1.Abe H, Minatoguchi S, Ohashi H, Murata I, Minagawa T, Okuma T, Yokoyama H, Takatsu H, Takaya T, Nagano T, Osumi Y, Kakami M, Tsukamoto T, Tanaka T, Hiei K, Fujiwara H. Renoprotective effect of the addition of losartan to ongoing treatment with an angiotensin converting enzyme inhibitor in type-2 diabetic patients with nephropathy. Hypertens Res 30: 929–935, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Azizi M, Chatellier G, Guyene TT, Murieta-Geoffroy D, Menard J. Additive effects of combined angiotensin-converting enzyme inhibition and angiotensin II antagonism on blood pressure and renin release in sodium-depleted normotensives. Circulation 92: 825–834, 1995 [DOI] [PubMed] [Google Scholar]
- 3.Breyer MD, Bottinger E, Brosius FC, III, Coffman TM, Harris RC, Heilig CW, Sharma K. Mouse models of diabetic nephropathy. J Am Soc Nephrol 16: 27–45, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Campbell DJ, Alexiou T, Xiao HD, Fuchs S, McKinley MJ, Corvol P, Bernstein KE. Effect of reduced angiotensin-converting enzyme gene expression and angiotensin-converting enzyme inhibition on angiotensin and bradykinin peptide levels in mice. Hypertension 43: 854–859, 2004 [DOI] [PubMed] [Google Scholar]
- 5.Cohen DL, Townsend RR. Is there added value to adding ARB to ACE inhibitors in the management of CKD? J Am Soc Nephrol 20: 1666–1668, 2009 [DOI] [PubMed] [Google Scholar]
- 6.Durvasula RV, Shankland SJ. Activation of a local renin angiotensin system in podocytes by glucose. Am J Physiol Renal Physiol 294: F830–F839, 2008 [DOI] [PubMed] [Google Scholar]
- 7.Feng Y, Yue X, Xia H, Bindom SM, Hickman PJ, Filipeanu CM, Wu G, Lazartigues E. Angiotensin-converting enzyme 2 overexpression in the subfornical organ prevents the angiotensin II-mediated pressor and drinking responses and is associated with angiotensin II type 1 receptor downregulation. Circ Res 102: 729–736, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrario CM, Jessup J, Gallagher PE, Averill DB, Brosnihan KB, Ann TE, Smith RD, Chappell MC. Effects of renin-angiotensin system blockade on renal angiotensin-(1-7) forming enzymes and receptors. Kidney Int 68: 2189–2196, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Garabelli PJ, Modrall JG, Penninger JM, Ferrario CM, Chappell MC. Distinct roles for angiotensin-converting enzyme 2 and carboxypeptidase A in the processing of angiotensins within the murine heart. Exp Physiol 93: 613–621, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harrison-Bernard LM, Cook AK, Oliverio MI, Coffman TM. Renal segmental microvascular responses to ANG II in AT1A receptor null mice. Am J Physiol Renal Physiol 284: F538–F545, 2003 [DOI] [PubMed] [Google Scholar]
- 11.Harrison-Bernard LM, Navar LG, Ho MM, Vinson GP, El-Dahr SS. Immunohistochemical localization of angiotensin II AT1 receptor in the adult rat kidney using a monoclonal antibody. Am J Physiol Renal Physiol 273: F170–F177, 1997 [DOI] [PubMed] [Google Scholar]
- 12.Huang XR, Chen WY, Truong LD, Lan HY. Chymase is upregulated in diabetic nephropathy: implications for an alternative pathway of angiotensin II-mediated diabetic renal and vascular disease. J Am Soc Nephrol 14: 1738–1747, 2003 [DOI] [PubMed] [Google Scholar]
- 13.Jacobsen P, Andersen S, Rossing K, Jensen BR, Parving HH. Dual blockade of the renin-angiotensin system versus maximal recommended dose of ACE inhibition in diabetic nephropathy. Kidney Int 63: 1874–1880, 2003 [DOI] [PubMed] [Google Scholar]
- 14.Kobori H, Harrison-Bernard LM, Navar LG. Expression of angiotensinogen mRNA and protein in angiotensin II-dependent hypertension. J Am Soc Nephrol 12: 431–439, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kobori H, Harrison-Bernard LM, Navar LG. Urinary excretion of angiotensinogen reflects intrarenal angiotensinogen production. Kidney Int 61: 579–585, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kobori H, Katsurada A, Miyata K, Ohashi N, Satou R, Saito T, Hagiwara Y, Miyashita K, Navar LG. Determination of plasma and urinary angiotensinogen levels in rodents by newly developed ELISA. Am J Physiol Renal Physiol 294: F1257–F1263, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kobori H, Nishiyama A, Harrison-Bernard LM, Navar LG. Urinary angiotensinogen as an indicator of intrarenal angiotensin status in hypertension. Hypertension 41: 42–49, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kobori H, Ohashi N, Katsurada A, Miyata K, Satou R, Saito T, Yamamoto T. Urinary angiotensinogen as a potential biomarker of severity of chronic kidney diseases. J Am Soc Hypertens 2: 349–354, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koya D, Haneda M, Nakagawa H, Isshiki K, Sato H, Maeda S, Sugimoto T, Yasuda H, Kashiwagi A, Ways DK, King GL, Kikkawa R. Amelioration of accelerated diabetic mesangial expansion by treatment with a PKC beta inhibitor in diabetic db/db mice, a rodent model for type 2 diabetes. FASEB J 14: 439–447, 2000 [DOI] [PubMed] [Google Scholar]
- 20.Lavrentyev EN, Estes AM, Malik KU. Mechanism of high glucose induced angiotensin II production in rat vascular smooth muscle cells. Circ Res 101: 455–464, 2007 [DOI] [PubMed] [Google Scholar]
- 21.Lazartigues E, Feng Y, Lavoie JL. The two fACEs of the tissue renin-angiotensin systems: implication in cardiovascular diseases. Curr Pharm Des 13: 1231–1245, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Lee GH, Proenca R, Montez JM, Carroll KM, Darvishzadeh JG, Lee JI, Friedman JM. Abnormal splicing of the leptin receptor in diabetic mice. Nature 379: 632–635, 1996 [DOI] [PubMed] [Google Scholar]
- 23.MaassenVanDenBrink A, de VR, Saxena PR, Schalekamp MA, Danser AH. Vasoconstriction by in situ formed angiotensin II: role of ACE and chymase. Cardiovasc Res 44: 407–415, 1999 [DOI] [PubMed] [Google Scholar]
- 24.McPherson EA, Luo Z, Brown RA, LeBard LS, Corless CC, Speth RC, Bagby SP. Chymase-like angiotensin II-generating activity in end-stage human autosomal dominant polycystic kidney disease. J Am Soc Nephrol 15: 493–500, 2004 [DOI] [PubMed] [Google Scholar]
- 25.Menard J, Campbell DJ, Azizi M, Gonzales MF. Synergistic effects of ACE inhibition and Ang II antagonism on blood pressure, cardiac weight, and renin in spontaneously hypertensive rats. Circulation 96: 3072–3078, 1997 [DOI] [PubMed] [Google Scholar]
- 26.Miyata K, Ohashi N, Suzaki Y, Katsurada A, Kobori H. Sequential activation of the reactive oxygen species/angiotensinogen/renin-angiotensin system axis in renal injury of type 2 diabetic rats. Clin Exp Pharmacol Physiol 35: 922–927, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mogensen CE, Neldam S, Tikkanen I, Oren S, Viskoper R, Watts RW, Cooper ME. Randomised controlled trial of dual blockade of renin-angiotensin system in patients with hypertension, microalbuminuria, and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. BMJ 321: 1440–1444, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park S, Bivona BJ, Feng Y, Lazartigues E, Harrison-Bernard LM. Intact renal afferent arteriolar autoregulatory responsiveness in db/db mice. Am J Physiol Renal Physiol 295: F1504–F1511, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park S, Harrison-Bernard LM. Augmented renal vascular nNOS and renin protein expression in angiotensin type 1 receptor null mice. J Histochem Cytochem 56: 401–414, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prieto-Carrasquero MC, Harrison-Bernard LM, Kobori H, Ozawa Y, Hering-Smith KS, Hamm LL, Navar LG. Enhancement of collecting duct renin in angiotensin II-dependent hypertensive rats. Hypertension 44: 223–229, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richard V, Hurel-Merle S, Scalbert E, Ferry G, Lallemand F, Bessou JP, Thuillez C. Functional evidence for a role of vascular chymase in the production of angiotensin II in isolated human arteries. Circulation 104: 750–752, 2001 [DOI] [PubMed] [Google Scholar]
- 32.Sadjadi J, Kramer GL, Yu CH, Burress WM, III, Chappell MC, Gregory MJ. Angiotensin converting enzyme-independent angiotensin ii production by chymase is up-regulated in the ischemic kidney in renovascular hypertension. J Surg Res 127: 65–69, 2005 [DOI] [PubMed] [Google Scholar]
- 33.Sakamoto-Ihara T, Suzuki Y, Kurusu A, Yamashita M, Horikoshi S, Tomino Y. Possible involvement of mast cells in renal fibrosis in patients with IgA nephropathy. Inflamm Res 56: 421–427, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Sharma K, McCue P, Dunn S. Diabetic kidney disease in the db/db mouse. Am J Physiol Renal Physiol 284: F1138–F1144, 2003 [DOI] [PubMed] [Google Scholar]
- 35.Singh R, Singh AK, Alavi N, Leehey DJ. Mechanism of increased angiotensin II levels in glomerular mesangial cells cultured in high glucose. J Am Soc Nephrol 14: 873–880, 2003 [DOI] [PubMed] [Google Scholar]
- 36.Singh VP, Le B, Bhat VB, Baker KM, Kumar R. High-glucose-induced regulation of intracellular ANG II synthesis and nuclear redistribution in cardiac myocytes. Am J Physiol Heart Circ Physiol 293: H939–H948, 2007 [DOI] [PubMed] [Google Scholar]
- 37.Soler MJ, Wysocki J, Ye M, Lloveras J, Kanwar Y, Batlle D. ACE2 inhibition worsens glomerular injury in association with increased ACE expression in streptozotocin-induced diabetic mice. Kidney Int 72: 614–623, 2007 [DOI] [PubMed] [Google Scholar]
- 38.Speth RC, Karamyan VT. The significance of brain aminopeptidases in the regulation of the actions of angiotensin peptides in the brain. Heart Fail Rev 13: 299–309, 2008 [DOI] [PubMed] [Google Scholar]
- 39.ter Wee PM, Forster HG, Epstein M. Video-microscopic assessment of the role of tissue angiotensin-converting enzyme in the control of the renal microcirculation. J Pharmacol Exp Ther 281: 434–439, 1997 [PubMed] [Google Scholar]
- 40.Urata H, Kinoshita A, Misono KS, Bumpus FM, Husain A. Identification of a highly specific chymase as the major angiotensin II-forming enzyme in the human heart. J Biol Chem 265: 22348–22357, 1990 [PubMed] [Google Scholar]
- 41.Urata H, Nishimura H, Ganten D. Chymase-dependent angiotensin II forming system in humans. Am J Hypertens 9: 277–284, 1996 [DOI] [PubMed] [Google Scholar]
- 42.Walker M, III, Harrison-Bernard LM, Cook AK, Navar LG. Dynamic interaction between myogenic and TGF mechanisms in afferent arteriolar blood flow autoregulation. Am J Physiol Renal Physiol 279: F858–F865, 2000 [DOI] [PubMed] [Google Scholar]
- 43.Wei CC, Tian B, Perry G, Meng QC, Chen YF, Oparil S, Dell'Italia LJ. Differential ANG II generation in plasma and tissue of mice with decreased expression of the ACE gene. Am J Physiol Heart Circ Physiol 282: H2254–H2258, 2002 [DOI] [PubMed] [Google Scholar]
- 44.Welker P, Krämer S, Groneberg DA, Neumayer HH, Bachmann S, Amann K, Peters H. Increased mast cell number in human hypertensive nephropathy. Am J Physiol Renal Physiol 295: F1103–F1109, 2008 [DOI] [PubMed] [Google Scholar]
- 45.Wysocki J, Ye M, Soler MJ, Gurley SB, Xiao HD, Bernstein KE, Coffman TM, Chen S, Batlle D. ACE and ACE2 activity in diabetic mice. Diabetes 55: 2132–2139, 2006 [DOI] [PubMed] [Google Scholar]
- 46.Ye M, Wysocki J, Naaz P, Salabat MR, LaPointe MS, Batlle D. Increased ACE 2 and decreased ACE protein in renal tubules from diabetic mice: a renoprotective combination? Hypertension 43: 1120–1125, 2004 [DOI] [PubMed] [Google Scholar]
- 47.Ziyadeh FN, Hoffman BB, Han DC, Iglesias-De La Cruz MC, Hong SW, Isono M, Chen S, McGowan TA, Sharma K. Long-term prevention of renal insufficiency, excess matrix gene expression, and glomerular mesangial matrix expansion by treatment with monoclonal antitransforming growth factor-beta antibody in db/db diabetic mice. Proc Natl Acad Sci USA 97: 8015–8020, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]