Abstract
Portal vein thrombosis (PVT) is a relatively common complication in patients with liver cirrhosis, but might also occur in absence of an overt liver disease. Several causes, either local or systemic, might play an important role in PVT pathogenesis. Frequently, more than one risk factor could be identified; however, occasionally no single factor is discernable. Clinical examination, laboratory investigations, and imaging are helpful to provide a quick diagnosis, as prompt treatment might greatly affect a patient’s outcome. In this review, we analyze the physiopathological mechanisms of PVT development, together with the hemodynamic and functional alterations related to this condition. Moreover, we describe the principal factors most frequently involved in PVT development and the recent knowledge concerning diagnostic and therapeutic procedures. Finally, we analyze the implications of PVT in the setting of liver transplantation and its possible influence on patients’ future prognoses.
Keywords: Portal vein thrombosis, Portal hypertension, Thrombophilic factors, Liver cirrhosis, Liver transplantation, Anticoagulants
INTRODUCTION
The term portal vein thrombosis (PVT) refers to the complete or partial obstruction of blood flow in the portal vein, due to the presence of a thrombus in the vasal lumen[1]. Although in the general population PVT is considered a rare event, its prevalence among cirrhotic patients ranges between 4.4%-15%, and is responsible for about 5%-10% of overall cases of portal hypertension[2]. The first case of PVT was reported in 1868 by Balfour and Stewart, describing a patient presenting splenomegaly, ascites, and variceal dilation[3]. Several etiological causes, either of local or systemic origin, might be responsible for PVT development, although more than one factor is often identified. Furthermore, PVT clinical presentation is different in the context of acute or chronic onset and depends on the development and the extent of a collateral circulation. Intestinal congestion and ischemia, with abdominal pain, diarrhea, rectal bleeding, abdominal distention, nausea, vomiting, anorexia, fever, lactacidosis, sepsis, and splenomegaly are common features of acute PVT. In contrast, chronic PVT can be completely asymptomatic, or characterized by splenomegaly, pancytopenia, varices, and, rarely, ascites[3]. In the presence of portal hypertension, PVT must always be investigated, especially in cirrhotic patients, even if it is considered a rare event[2]. Indeed, an early diagnosis and appropriate management of secondary portal hypertension could be, in some cases, life-saving for the patient. Furthermore, in the diagnostic iter, the identification of possible local or systemic trigger factors is of primary importance however, occasionally no single factor is discernable.
Currently, several therapeutic options are available; however, their feasibility and efficacy are still being evaluated and the risks and benefits should be carefully considered for each patient.
In this review, we discuss the features of PVT, pointing out new insights into clinical, diagnostic, and therapeutic issues, making an overview of current beliefs regarding patient outcome and, finally, reporting controversies about the correct management of PVT in the setting of liver transplantation.
PATHOPHYSIOLOGY
As a consequence of portal vein obstruction, systemic and splanchnic hemodynamics undergo specific and important modifications[4]. On the cessation of portal blood flow, the liver loses about two thirds of its blood supply. Interestingly, this condition is usually well tolerated and patients are often asymptomatic, while an acute arterial obstruction always leads to a severe hepatic dysfunction, which is sometimes fatal. It is probably that the immediate activation of two compensatory mechanisms might supplement the loss of portal vein’s contribution to liver blood flow. The first mechanism is “arterial vasodilation” of the hepatic artery, similar to that observed in portal vein clamping during liver surgery[5]. This “arterial rescue” is a kind of vascular reflex present in every organ with both an arterial and a venous circulation and is capable of preserving liver function in the acute stages of PVT. The second compensatory mechanism is “venous rescue”, consisting of the rapid development of collaterals to bypass the obstruction. This vascular neo-formation begins in a few days after portal vein obstruction, and finalizes within 3 to 5 wk[6,7]. As a result, the thrombosed portal vein is replaced by a network of collateral vessels, called “cavernoma”, connecting the two patent portions proximally and distally to the thrombus. Usually, the original portal vein becomes a thin, fibrotic cord, which is difficult to visualize[8,9]. At this stage, the development of a hyperkinetic circulation, characterized by low systemic vascular resistance and a high cardiac output, is common[3].
Despite the activation of this complex system of support, the impairment of portal flow has important consequences on liver tissue. It has been demonstrated in rats, that the progressive obliteration of the portal vein stimulates apoptosis of hepatocytes in the hypoperfused lobe[10], while increasing the mitotic activity in the normal perfused one. The latter effect is well known, and is employed therapeutically in resective liver surgery. However, this process results in a progressive loss of tissue and might be responsible for the impairment of hepatic synthetic function observed in advanced stages of portal vein obstruction[11].
EPIDEMIOLOGY
The concept of PVT as a rare disease is mainly based on clinical series and case reports[2]. An epidemiological study performed in southern Sweden and based on autopsies, reported the incidental finding of a PVT in about 1% of the general population[12]. Cohen et al[13] confirmed these data and reported that most PVT patients were cirrhotics with a primary or metastatic liver cancer. Today, thanks to the availability of more sensitive and less invasive imaging, together with the existence of curative or palliative procedures, PVT is routinely investigated and recognized without any difficulty[14-16]. Thus, PVT seems more frequent than expected: it is estimated to be responsible for 5%-10% of the overall cases of portal hypertension, which can be 40% in developing countries[3]. The incidence among cirrhotic patients is still unknown, but recent data suggest a prevalence of about 0.6%-16%[17] (the highest) among orthotopic liver transplantation (OLT) candidates[2] and of about 6.5% in patients with a hepatocellular carcinoma at the time of diagnosis[16].
ETIOLOGY
Several causes can be involved in the pathogenesis of PVT and, frequently, more than one coexist. A simple classification distinguishes between local (70%) and systemic (30%) risk factors (Tables 1 and 2).
Table 1.
| Local risk factors for PVT (70%) |
| Cancer |
| Any abdominal organ |
| Focal inflammatory lesions |
| Neonatal omphalitis, ombilical vein catheterization |
| Diverticulitis, appendicitis |
| Pancreatitis |
| Duodenal ulcer |
| Cholecystitis |
| Tuberculous lymphadenitis |
| Crohn’s disease, ulcerative colitis |
| Cytomegalovirus hepatitis |
| Injury to the portal venous system |
| Splenectomy |
| Colectomy, gastrectomy |
| Cholecystectomy |
| Liver transplantation |
| Abdominal trauma |
| Surgical portosystemic shunting, TIPS |
| Iatrogenic (fine needle aspiration of abdominal masses etc.) |
| Cirrhosis |
| Preserved liver function with precipitating factors (splenectomy, surgical portosystemic shunting, TIPS dysfunction, thrombophilia) |
| Advanced disease in the absence of obvious precipitating factors |
PVT: Portal vein thrombosis; TIPS: Transjugular intrahepatic portosystemic shunt.
Table 2.
| Systemic risk factors for PVT (30%) |
| Inherited |
| Factor V Leiden mutation |
| Factor II (prothrombin) mutation |
| Protein C deficiency |
| Protein S deficiency |
| Antithrombin deficiency |
| Acquired |
| Myeloproliferative disorder |
| Antiphospholipid syndrome |
| Paroxysmal nocturnal hemoglobinuria |
| Oral contraceptives |
| Pregnancy or puerperium |
| Hyperhomocysteinemia |
| Malignancy |
Inflammatory abdominal foci (such as appendicitis, diverticulitis, inflammatory bowel diseases, pancreatitis, cholecystitis, hepatic abscesses, and cholangitis), liver cirrhosis or tumors, represent the most common local thrombotic risk factors[8,12,18].
Malignancies, frequently of hepatic or pancreatic origin, are responsible for 21%-24% of overall cases of PVT[13,19]. Direct vascular invasion, compression by tumor mass, or a hypercoagulable state are the mechanisms involved in neoplastic PVT development; hormonal factors might also play a role in this process, especially in men[16,20,21].
PVT is common in patients affected by liver cirrhosis, with a risk related to the severity of the disease; the prevalence ranges from 1%, at the earlier stages, to 30% in candidates for liver transplantation[8,17]. Moreover, in patients with a hepatocellular carcinoma, the incidence of PVT rises to 10%-40%[9].
Other less common PVT local causes are adenopathy, systemic inflammatory response syndrome, and surgical traumas to the portal venous system, such as portosystemic shunting, splenectomy, liver transplantation, ablative therapy for HCC, and fine needle aspiration of abdominal masses[1].
On the other hand, myeloproliferative disorders and prothrombotic conditions belong to the group of systemic risk factors, with a prevalence of about 40% and 60%, respectively (Table 3)[8,22].
Table 3.
Prevalence of thrombotic risk factors in series of routinely investigated, consecutive adult patients with non tumorous and non cirrhotic, acute or chronic, PVT[126]
| Risk factor | PVT patients (%) |
| Myeloproliferative disorders | 30-40 |
| Atypical | 14 |
| Classical | 17 |
| Antithrombin deficiency | 0-26 |
| Protein C deficiency | 0-26 |
| Protein S deficiency | 2-30 |
| Factor V Leiden mutation | 6-32 |
| Prothrombine mutation | 14-40 |
| TT677 methylene tetrahydrofolate reductase (MTHFR) genotype | 11-50 |
| Antiphospholipid syndrome | 6-19 |
| Hyperomocisteinemia | 12-22 |
| Recent pregnancy | 6-40 |
| Recent oral contraceptive use | 12 |
Factor V Leiden mutation is the most common thrombophilia predisposing to PVT, followed by protein C (PC) deficiency[23-26]. The role of protein S (PS) and antithrombin III (AT) deficiency in PVT etiology has not yet been confirmed, and it is difficult to evaluate the influence of anticoagulation therapy on the impairment in liver function. Indeed, in cirrhotic patients it is hard to distinguish between congenital and acquired deficiencies of natural coagulants and their role in PVT pathogenesis, because if liver function is impaired, levels of coagulation inhibitors, as well as those of pro-coagulation factors, are often decreased[27]. A clinical study conducted on eleven children with PVT[28], reported a significant improvement in PC, PS, factors II, V, and VII levels and prothrombin time after surgical correction with a Rex Shunt (mesenteric-left portal vein bypass). In contrast, a distal spleno-renal shunt or an H-type meso-caval shunt, in the same condition, didnot seem to be equally effective, probably due to insufficient residual portal vein flow and the consequent impairment in liver synthetic function[29]. However, the relatively low prevalence of genetic, in respect to acquired, thrombophilic disorders, might represent a potential diagnostic matter in PVT patients, and should be considered carefully in clinical practice[30]. To overcome this problem, an accurate genetic study of the patient and, eventually, his/her family (first degree relatives) might be useful in strongly suggestive cases. Unfortunately, in practice, this policy is not applicable without difficulty. A simple method to screen the deficiency of natural anticoagulants in patients with liver disease comprises the ratio of PS or PC or AT to [(factor II + factor X)/2]. If the result is less than 70%, a genetic deficiency has to be suspected and investigated[1].
Among the other thrombophilic disorders, a prothrombin gene mutation seems to be frequent among cirrhotics with PVT[2,31-34]. However, in the general population, its role in PVT development seems less clear, as it is considered a weak prothrombotic risk factor. Moreover, a homozygous methylene tetrahydrofolate reductase (MTHFR) gene mutation might be associated with PVT development alone or, if heterozygote, in the presence of other cofactors[13,35-39]. Amitrano et al[27] reported a strong correlation between the prothrombin A20210 mutation or the homozygous MTHFR C677-T genotype and PVT in cirrhotic patients without evidence of liver cancer.
Furthermore, the presence of anticardiolipin antibodies is quite frequent in patients with chronic liver disease; a transient positivity is often reported after infections, suggesting a relationship between microorganisms (i.e. Bacteroides species) and thrombotic events, such as PVT[40-43]. In contrast, other studies consider anticardiolipin antibodies simply as an epiphenomenon of liver damage[41,44]. Finally, the role of oral contraceptives, steroids, and pregnancy is still less clear[45-47].
In about 22%-48% of patients, PVT is a manifestation of a myeloproliferative disease (MPD)[2,20,48].
An intra-abdominal vascular thrombosis is often the sole presenting symptom and an overt MPD might successively develop in 51% of cases. In the Western Countries, 58% of idiopathic PVTs are associated with a latent MPD[49]. The principal diagnostic criteria are usually incompletely met in these patients, probably because of the atypical manifestation of the disease[50]. The 1849G→T point mutation in the gene encoding tyrosine-protein kinase JAK2, is a specific and easily detectable marker for MPDs, which can often be useful for a rapid diagnose in PVT patients[51-55]. Recent studies reported the presence of a JAK2 mutation in about 17%-35% of patients with PVT, but further studies are needed to confirm these data[56,57].
Occasionally, it is not possible to recognize any overt cause of PVT; generally, the clinical course is favorable for these patients, with a low incidence of complications. However, at present, “idiopathic PVT” is less frequent, thanks to the amelioration in diagnostics and to a more scrupulous attention to patients’ clinical history[12].
In conclusion, it is reasonable to routinely investigate the most common prothrombotic disorders and exclude a local trigger, to provide a correct management of PVT and its original cause. However, the mechanism of PVT development is complex and multifactorial, and is not always attributable to a single risk factor. In the presence of sporadic local or systemic promoting events, an underlying intrinsic predisposition might be the access key to thrombosis development[1,13].
CLASSIFICATION
PVT onset can be acute or chronic. This is an arbitrary distinction, which is sometimes difficult to apply in clinical practice; patients who develop symptoms, such as abdominal pain, nausea, and fever, within sixty days prior to hospital admission, might have an acute PVT development[58,59].
PVT can be classified into four categories, depending on the extension: (1) confined to the portal vein beyond the confluence of the splenic vein; (2) extended to the superior mesenteric vein, but with patent mesenteric vessels; (3) extended to the whole splanchnic venous system, but with large collaterals; or (4) with only fine collaterals[60]. This classification is useful to evaluate a patient’s operability and clinical outcome. In fact, when thrombosis is extended to both portal and mesenteric veins, the risk of bowel ischemia is considerable and mortality high, despite a lower risk of variceal bleeding[61].
CLINICAL PRESENTATION
PVT can occur either in childhood or in adulthood, with the same incidence[45]. Clinical presentation always depends on the onset and the extent of the thrombosis and the development of collateral circulation[62].
Acute PVT
Intestinal congestion and ischemia are typical manifestations of acute PVT; abdominal pain or distention, diarrhea, rectal bleeding, nausea, vomiting, anorexia, fever, lactacidosis, splenomegaly and sepsis might be variably present[63,64]. If the obstruction is not resolved quickly, intestinal perforation, peritonitis, shock, and death from multiorgan failure might occur[8]. On physical examination, the abdomen might be distended, but guarding is rare, except in case of intra-abdominal inflammation, intestinal infarction, and perforation[22]. The majority of patients exhibit splenomegaly, while ascites is rare or, eventually, present before the development of a collateral circulation. This mild, transient, ascites is due to intestinal venous congestion in the absence of the mechanisms activated in liver cirrhosis[63,64].
Chronic PVT
On the other hand, chronic PVT can be nearly asymptomatic, except for the presence of varices, cutaneous collaterals, or ascites[62]. Typically, patients with an advanced thrombosis do not always remember any previous trigger event or disease[22,63,64]. The majority of patients develop esophageal varices, in contrast to acute PVT; an episode of gastrointestinal bleeding is reported as the first presenting symptom in about 20%-40% of cases[9]. As this phenomenon is strictly time-dependent, it is advisable to screen all PVT patients endoscopically, at diagnosis[63]. In cirrhotics with PVT, the risk of variceal bleeding is nearly 80-120 times higher than in patients without liver disease, although the outcome seems better[65,66].
Furthermore, hypersplenism and, consequently, pancytopenia, are commonly present in chronic PVT[1]; however, if one branch of the portal vein is preserved and the portal pressure is quite normal, they may even be absent. Ascites and encephalopathy are uncommon and only transient. They are more frequent after an episode of gastrointestinal bleeding or associated with renal failure or sepsis in older patients[8,64,67]. Abnormalities of the extrahepatic biliary tree have been reported in more than 80% of patients with chronic PVT; compression by choledochal or periportal varices or by the cavernoma, pericholedochal fibrosis, and ischemic structuring are the principal reasons[67-71]. Another finding is the “pseudocholangiocarcinoma sign”[1,11,17], caused by the displacement, stricturing or thumbprinting of the biliary ducts produced by contiguous neo-formed vessels; it is present in at least 80% of PVT patients at endoscopic retrograde cholangiopancreatography[67], often mimicking a cholangiocellular cancer[72,73]. Physical examination and biochemical markers might be completely normal, but, sometimes, cholestasis, cholangitis, choledocholithiasis, cholecystitis and, at least, liver injury, might occur, configuring the so-called “portal biliopathy”[71,74].
DIAGNOSIS
Imaging
The diagnosis of PVT can be quickly established by demonstrating the presence of solid material within the vasal lumen (Table 4)[22]. Nowadays, in developed countries, PVT is usually recognized at an early stage; cavernomatous transformation or the occurrence of gastrointestinal bleeding are rare. The clinical suspicion is often based on the incidental finding of hypersplenism, signs of portal hypertension or, less frequently, symptoms of portal cholangiopathy. Ultrasonography (US) is usually the investigation of choice, with a sensitivity and specificity ranging between 60% and 100%[17]; it can reveal the presence of solid, hyperechoic material into a distended portal vein or its tributaries, the presence of collateral vessels or a cavernoma (Figures 1, 2 and 3)[18,22,75]. Doppler imaging can confirm the absence of flow in part or all the vasal lumen, and, if present, a cavernomatous transformation[22]. Recently, the endoscopic use of ultrasound (EUS) was demonstrated to be 81% sensitive and 93% specific in PVT diagnosis[76], and to be capable of detecting small and non-occluding thrombi. It appears to be more accurate than US or computed tomography (CT) scans in discovering portal invasion by tumors[77,78]. However, the limit of EUS is the presence of a relatively blind area, which cannot be investigated, involving the distal superior mesenteric vein and the intrahepatic portion of the portal vein[76].
Table 4.
AASLD recommendations for diagnosis of acute and chronic PVT[126]
| AASLD recommendations for diagnosis of acute PVT | AASLD recommendations for diagnosis of chronic PVT |
| Consider a diagnosis of acute PVT in any patient with abdominal pain of more than 24 h duration, whether or not there is also fever or ileus | Consider a diagnosis of chronic PVT in any patient with newly diagnosed portal hypertension |
| If acute PVT is suspected, computed tomography (CT) scan, before and after injection of vascular contrast agent, should be obtained for early confirmation of diagnosis. If CT scan is not rapidly available, obtain Doppler-sonography | Obtain Doppler-sonography, then either CT scan or MRI, before and after a vascular contrast agent, to make a diagnosis of chronic PVT |
| In patients with acute PVT and high fever, septic pylephlebitis should be considered, whether or not an abdominal source of infection has been identified, and blood cultures should be routinely obtained | Base the diagnosis on the absence of a visible normal portal vein and its replacement with serpiginous veins |
| In acute PVT, the possibility of intestinal infarction should be considered from presentation until resolution of pain. The presence of ascites, thinning of the intestinal wall, lack of mucosal enhancement of the thickened intestinal wall, or the development of multiorgan failure indicate that intestinal infarction is likely and surgical exploration should be considered |
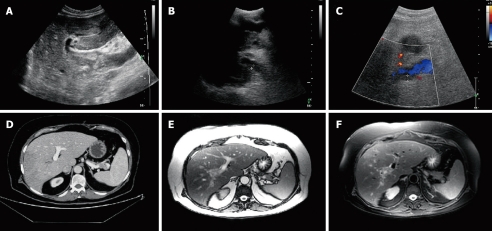
Figure 1.
Portal vein thrombosis. A: Complete thrombosis of the portal vein trunk (ultrasonography); B, C: Partial thrombosis of the right portal vein (ultrasonography and ultrasonography + doppler); D: Thrombosis of the right portal vein (CT scan); E, F: Thrombosis of the right portal vein (MRI).
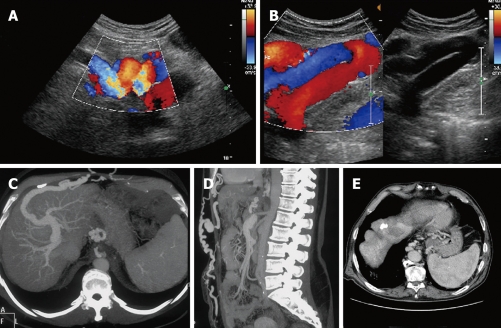
Figure 2.
Collateral circulation. A, B: Recanalization of paraumbilical vein (ultrasonography + doppler); C, D: Recanalization of paraumbilical vein (CT scan); E: Perigastric and paraesophageal varices (CT scan).
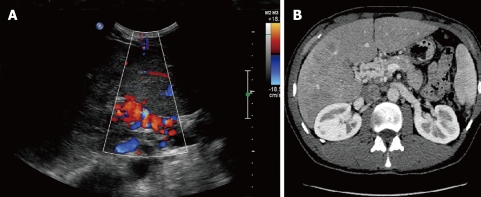
Figure 3.
Cavernomatous transformation of the portal vein. A: Ultrasonography + doppler; B: CT scan.
Incidentally, US is less reliable in determining the extension of the thrombus to the mesenteric circulation[79]. Instead, CT scanning and magnetic resonance imaging (MRI) can easily obtain this information, and, in addition, can estimate the impairment of the bowel and other adjacent organs (Figures 1-3). CT scanning is able to demonstrate hyperattenuating material in the portal vein lumen and the absence of enhancement after contrast injection. In addition, in hypoperfused areas, hepatic enhancement appears increased during the arterial phase and decreased during the portal phase. CT is also useful for the identification of the possible cause of the thrombosis or potential complications, such as bowel ischemia and perforation[22]. MRI might also confirm the vascular occlusion; at spin-echo MR, the clot appears isointense on T1- weighted images, or hyperintense if recent, and usually has a more intense signal on T2 images. Gradient-echo MR might help to better evaluate any confusing spin-echo MR image[80]. Furthermore, contrast-enhanced MR angiography is useful to assess flow direction in the portal venous system and its patency, to identify a cavernomatous transformation, to determine the presence of varices, and to verify the correct function of surgical shunts[81,82]. In addition, MR angiography has a high accuracy in the follow-up of the portal venous system before and after liver transplantation[82-85]. Moreover, MRI-true fast imaging with steady state precession (true FISP), might overcome the difficulty of contrast injection in cases of poor venous access and the degradation of the images by respiratory motion[86].
laboratory investigations
In PVT patients, liver function is typically conserved. Laboratory investigations will be normal or quite normal, unless there is coexistence of a liver disease. However, levels of prothrombin and other coagulation factors could be moderately decreased, while D-dimer is usually increased[8,22].
PVT is considered a milestone in the natural history of liver cirrhosis and it is related to serious complications, morbidity, and mortality, as previously discussed[87]. Thus, prevention is the first aim of PVT management in patients with an advanced liver disease. Recently, several studies tried to identify the strongest predictive factors for PVT development in these patients. In the past, male sex, previous surgery or interventional treatment for portal hypertension, previous variceal bleeding, low platelet count, and advanced liver failure have been associated with an increased risk of PVT development[2,31,85,88]. Interestingly, in a recent prospective study by Zocco et al[89], a portal flow velocity below 15 cm/s, at US-Doppler evaluation, was considered significantly predictive of PVT development, confirming the importance of Virchow’s triad in the pathogenesis of vascular thrombosis.
Original cause
As first, local causes such as cirrhosis, primary or metastatic malignancies, pylephlebitis, liver cysts, vascular abnormalities (webs or aneurysms), and pancreatitis have to be excluded. Imaging (US+Doppler, MRI or CT scan) or invasive procedures might be helpful[22]; needle biopsy of the obstructed portal vein might be specific, but also of relatively low sensitivity[90]. If no local risk factor is found, the presence of a thrombophilic disorder must be investigated. If no possible cause of the thrombosis is recognized, the PVT should be considered “idiopathic”. Incidentally, a subclinical prothrombotic state has been reported in about 72% of idiopathic PVT, including an overt or occult MPD[91-93].
Complications
Once the diagnosis has been reached, the severity of liver and other organs’ involvement should be assessed. Clinical and laboratory evaluation, as well as imaging, might be useful; the degree of the obstruction (complete or partial, limited or extensive) should be investigated. A partial thrombosis is often associated with few symptoms. Instead, a rapid and complete obstruction of the portal or mesenteric vein, without the involvement of the mesenteric venous arches, induces only intestinal congestion; the main feature is a diffuse thickening of the intestinal wall, visible even without alterations in contrast enhancement. Generally, there are no signs of other organ failures and liver function is usually preserved, probably because the increased hepatic arterial blood flow supplants portal obstruction. In addition, collateral circulation develops rapidly from pre-existing veins in the porta hepatis within 2 to 3 d after the onset of acute thrombosis, particularly in the gallbladder wall[61,94,95]. All these manifestations are completely reversible, even if a spontaneous recanalization or a cavernomatous transformation occurs. In contrast, when thrombosis spreads to mesenteric venous arches, the consequence is intestinal ischemia or infarction. Common radiological findings are the thinning of the intestinal wall and the presence of defects of enhancement after intravenous contrast injection[8].
PROGNOSIS
In non-cirrhotic and non-neoplastic patients, PVT has generally good outcome; exitus for gastrointestinal bleeding is uncommon[65,96,97]. Otherwise, prognosis depends on the underlying liver disease[1,12,22,79]. The overall mortality has been reported to be less than 10% in PVT chronic onset[18,98], except for patients with malignancy or cirrhosis - about 26%[63]. Moreover, advanced age, malignancy, cirrhosis, mesenteric vein thrombosis, absence of abdominal inflammation, and serum levels of aminotransferase and albumin are associated with reduced survival[65]. Systemic risk factors, like MPD or other prothrombotic disorders, seem not to affect short-term survival[99].
In addition, acute PVT, when recognized and treated before the occurrence of intestinal infarction, has good prognosis[61,100-103]. By contrast, in cases of bowel ischemia and multiorgan dysfunction or failure, patients in-hospital mortality rate is approximately 20%-50%[61].
PVT AND OLT
In the past, PVT was considered an absolute contraindication for liver transplantation. Currently, thanks to great innovations in medical care, surgical techniques, and radiological interventions, this belief has been confounded and PVT by itself can represent an indication for liver transplantation[11,64,104,105]. The first successful liver transplant in a patient with a thrombosed portal vein was reported by Shaw et al[106], in 1985. Several studies[107-111] showed that surgical thrombectomy, thromboendovenectomy with venous reconstruction, interposition of vein graft, porto-caval hemitransposition, and radiological endovascular interventions, can resolve venous obstruction in liver transplant recipients[112]. However, surgical options are various, and dependent on a correct intra-operatory grading of the thrombosis (Table 5); terminal to terminal portal vein anastomosis with or without thrombectomy is the common choice in low grade PVT, while porto-caval hemitransposition is mandatory in grade 4[85,113]. Comparisons of technical difficulties, postoperative complications, survival, and mortality, in recipients with or without PVT are contrasting. Several studies reported a more complex surgical procedure, with a greater requirement of blood transfusions, an increased risk of complications (such as primary non function or dysfunction, thrombosis of the hepatic artery, relaparotomy, postoperative pancreatitis, sepsis, and renal failure), a poorer survival, and a higher mortality[113-115]. However, these data have not been confirmed and features of liver transplantation, comparing recipients with PVT and those without, are similar[74,113-116]. Interestingly, PVT patients’ rates of survival at one and 5 years after OLT are equal, as if, once the peri-transplant period has been overcome, the future clinical destiny of recipients with or without a previous PVT could be overlapped. However, among patients with PVT, survival seems better in low grades of Yerdel classification; however, further studies are needed to confirm this data. Transplantation at grade 1 PVT seems to carry results comparable to non-PVT patients[74,85,117].
Table 5.
Intraoperatory grading of PVT extension[17]
| Yerdel’s grading |
| < 50% occlusion of the portal vein |
| > 50% occlusion of the portal vein (including total occlusion) |
| Complete thrombosis of both portal and proximal superior mesenteric vein |
| Complete thrombosis of portal vein and proximal and distal superior mesenteric vein |
The rate of thrombosis recurrence has been estimated within 9% to 42% although some authors reported a lower incidence[74,107,108,116,118-120]. Male sex, previous treatment for PVT, Child-Pugh class C, and alcoholic liver disease might be associated with recurrence[85,114]. Furthermore, patients with an obstruction of more than half of the portal vein, extended or not to the superior mesenteric vein, seem to have increased risk of severe peri-operative complications, higher mortality, and decreased long-term survival[85,107,115]. In cirrhotics with PVT, surgical procedure may be more difficult, often complicated by rethrombosis and reintervention, but with the same morbidity and mortality of non-cirrhotic patients[113,115,121,122].
After liver transplantation, PVT development is a rare but possible event, especially in the early postoperative period[60]. The incidence ranges between 1% and 2%[122-124], with a preferential localization at the anastomotic site; technical complications, small diameter of the portal vein, pediatric recipient, presence of PVT pre-OLT, surgical shunting pre-OLT, or splenectomy are the principal predisposing risk factors[124]. The occlusion of the portal vein is always more scarring than the thrombosis of the hepatic artery and may be seriously threatening for both graft and patient survival[122]. Acute liver failure, bleeding from esophageal varices, and massive ascites could rapidly occur and immediate retransplantation must be quickly attempted in case of severe worsening of liver function[124].
Thus, for all these reasons and the good results reported in literature, today PVT has no longer to be considered a contraindication but only a disadvantage and, in some cases, might present a possible indication to liver transplantation[114,116,124,125].
TREATMENT
Although spontaneous resolution of PVT has been reported in the literature[101,102], a specific therapeutic management is mandatory to resolve portal vein obstruction and avoid serious complications. The goal of treatment is similar in acute and chronic PVT, and consists in correction of causal factors, prevention of thrombosis extension, and achievement of portal vein patency. However, in case of long standing thrombosis, the management of complications related to portal hypertension and portal cholangiopathy has to be concurrently considered[126]. Nowadays, anticoagulant therapy is the best way to obtain portal vein recanalization; however, there is no consensus on its application. Other modalities of treatment should be adopted only in case of partial or absent PVT resolution[12,126]. Furthermore, some conditions should be considered in the assessment of anticoagulant therapy, such as recent vs old thrombosis, the presence of a thrombophilic condition, or a liver disease.
Anticoagulation in acute PVT
Although PVT might be compared to other cases of deep vein thrombosis, there is no randomized controlled trial regarding the use of anticoagulants in acute PVT[126]. After 6 mo of therapy, a complete recanalization has been reported in about 50% of patients, with good results in the case of mesenteric vein involvement, and a low incidence of complications. In contrast, in about 10% of cases, PVT is resistant to anticoagulants[96,97,100-103]. In addition, when intestinal infarction occurs, anticoagulants administered prior to laparotomy seem to have a consistent benefit on survival[127-129].
What is certain is that, in acute PVT onset, the sooner the treatment is given the better the outcome will be; the rate of recanalization is about 69%, if anticoagulation is instituted within the first week after diagnosis, while it falls to 25% when instituted at the second week[9,59,130].
Anticoagulation in chronic PVT
Opinions regarding therapeutic options in chronic PVT are more controversial and significantly variable. At present, anticoagulant treatment is administered to only 30% of patients with chronic PVT, reflecting concerns about the use of anticoagulation in the presence of gastro-esophageal varices, low platelet counts, and coagulation dysfunctions[79]. However, the number of bleeding episodes in PVT patients receiving anticoagulant therapy didnot increased, and in long-term follow-up studies, anticoagulants seem to be effective in preventing new thrombotic events with a low mortality[66,126]. Incidentally, a pragmatic approach, such as endoscopical eradication of varices prior to commencement of anticoagulation, should be reasonable[79].
Dose and duration of anticoagulants
If thrombosis is recent and there is no underlying thrombophilic condition, anticoagulation should be administered for 3-6 mo, as a complete portal vein recanalization can occasionally be delayed[79,100,101,131-133]. Recently, a panel of experts recommended the application of anticoagulant therapy only in PVT patients with a proven thrombophilic disorder or familial history of venous thrombosis[133,134], thereby obtaining an improvement in survival and reduction in risk of gastrointestinal bleeding[135,136].
Anticoagulation in cirrhotic patients
The ubiquitous and long-term use of anticoagulants in cirrhotic patients with PVT should not be considered correct practice, until their safety and efficacy has been completely tested[62]. However, signs of intestinal ischemia or infarction, or an underlying prothrombotic disorder should be considered an indication for anticoagulants in cirrhotic patients, although only after an adequate prophylaxis for variceal bleeding[2,126]. In candidates for liver transplantation with a high risk PVT (obstruction of more than 50% of the portal vein), anticoagulation should be recommended, even if a scheduled prophylactic treatment has not yet been assessed[64,74,85,108,117].
Other treatments
Thrombolytic therapy, given either into the systemic venous circulation, the superior mesenteric artery, or the portal vein via a transjugular or transhepatic route, is also effective to provide recanalization in acute PVT[137-142]. However, efficacy is significantly lower and mortality increased in patients who undergo thrombolysis, if compared to conservative treatment[59,143,144]. Despite the high incidence of side effects, thrombolysis should be considered when initial anticoagulant therapy fails, even if there is no consistent evidence concerning in which conditions it should be preferred to anticoagulation[137]. Surgical thrombectomy is usually not recommended, as high morbidity and mortality have been reported; percutaneous transhepatic mechanical thrombectomy might also be effective in recent thrombosis, but vascular traumas are frequent and may stimulate rethrombosis[145].
Other approaches, such as transjugular intrahepatic portosystemic shunt placement, should be reserved for patients developing acute PVT before or after liver transplantation, or in alternative to thrombolysis when anticoagulation fails[146,147]. It seems to be effective in resolving portal biliopathy, ascites, and portal hypertension, but it is not feasible if portal vein is not catheterizable or a cavernomatous vein cannot be dilated[148-150].
Finally, shunt surgery (distal splenorenal shunt or Rex shunt, in children) might be applied as the last choice, and only in absence of splenic or superior mesenteric vein thrombosis[151].
CONCLUSION
PVT is relatively uncommon in the general population, but is more frequent among cirrhotic patients and represents a “milestone” in the natural evolution of liver disease. Local or systemic pro-thrombotic factors, alone or together, can play an important role in PVT pathogenesis, which is complex and different in each clinical context and in each patient. The consequent changes in hepatic and splanchnic hemodynamic are responsible for a mild impairment in liver function, in absence of an overt liver disease, or can precipitate a preexistent metastable clinical status in cirrhotic patients. Moreover, PVT might have indirect effects on other abdominal organs, causing intestinal ischemia and infarction, or predisposition to vascular neoformation and gastrointestinal bleeding. The identification of protean manifestations of PVT is essential to provide a prompt diagnosis, as the removal of the original trigger factor and an early therapeutic management is crucial to preserve patient health and, sometimes, life. The history of PVT has been characterized by difficulties in diagnosis and treatment, which, today, have almost been overcome. In the future, due to innovations in imaging and pharmaceuticals, clinical attention must be focused on the realization of a scheduled, preemptive, therapeutic approach to the patient, to better define the profile of toxicity and reduce side effects, especially in cirrhotic patients.
Acknowledgments
We give special thanks to Fondazione Ricerca in Medicina.
Footnotes
Peer reviewers: Hiroshi Yoshida, MD, First Department of Surgery, Nippon Medical School, 1-1-5 Sendagi, Bunkyo-ku, Tokyo 113-8603, Japan; Diego Garcia-Compean, MD, Professor, Faculty of Medicine, University Hospital, Department of Gastroenterology, Autonomous University of Nuevo Leon, Ave Madero y Gonzalitos, 64700 Monterrey, NL, México
S- Editor Tian L L- Editor Stewart GJ E- Editor Ma WH
References
- 1.Bayraktar Y, Harmanci O. Etiology and consequences of thrombosis in abdominal vessels. World J Gastroenterol. 2006;12:1165–1174. doi: 10.3748/wjg.v12.i8.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amitrano L, Guardascione MA, Brancaccio V, Margaglione M, Manguso F, Iannaccone L, Grandone E, Balzano A. Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol. 2004;40:736–741. doi: 10.1016/j.jhep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Wang JT, Zhao HY, Liu YL. Portal vein thrombosis. Hepatobiliary Pancreat Dis Int. 2005;4:515–518. [PubMed] [Google Scholar]
- 4.Lebrec D, Bataille C, Bercoff E, Valla D. Hemodynamic changes in patients with portal venous obstruction. Hepatology. 1983;3:550–553. doi: 10.1002/hep.1840030412. [DOI] [PubMed] [Google Scholar]
- 5.Henderson JM, Gilmore GT, Mackay GJ, Galloway JR, Dodson TF, Kutner MH. Hemodynamics during liver transplantation: the interactions between cardiac output and portal venous and hepatic arterial flows. Hepatology. 1992;16:715–718. doi: 10.1002/hep.1840160316. [DOI] [PubMed] [Google Scholar]
- 6.Ohnishi K, Okuda K, Ohtsuki T, Nakayama T, Hiyama Y, Iwama S, Goto N, Nakajima Y, Musha N, Nakashima T. Formation of hilar collaterals or cavernous transformation after portal vein obstruction by hepatocellular carcinoma. Observations in ten patients. Gastroenterology. 1984;87:1150–1153. [PubMed] [Google Scholar]
- 7.De Gaetano AM, Lafortune M, Patriquin H, De Franco A, Aubin B, Paradis K. Cavernous transformation of the portal vein: patterns of intrahepatic and splanchnic collateral circulation detected with Doppler sonography. AJR Am J Roentgenol. 1995;165:1151–1155. doi: 10.2214/ajr.165.5.7572494. [DOI] [PubMed] [Google Scholar]
- 8.Condat B, Valla D. Nonmalignant portal vein thrombosis in adults. Nat Clin Pract Gastroenterol Hepatol. 2006;3:505–515. doi: 10.1038/ncpgasthep0577. [DOI] [PubMed] [Google Scholar]
- 9.Hoekstra J, Janssen HL. Vascular liver disorders (II): portal vein thrombosis. Neth J Med. 2009;67:46–53. [PubMed] [Google Scholar]
- 10.Ogren M, Bergqvist D, Wåhlander K, Eriksson H, Sternby NH. Trousseau’s syndrome - what is the evidence? A population-based autopsy study. Thromb Haemost. 2006;95:541–545. doi: 10.1160/TH05-10-0694. [DOI] [PubMed] [Google Scholar]
- 11.Harmanci O, Bayraktar Y. Portal hypertension due to portal venous thrombosis: etiology, clinical outcomes. World J Gastroenterol. 2007;13:2535–2540. doi: 10.3748/wjg.v13.i18.2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogren M, Bergqvist D, Björck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. 2006;12:2115–2119. doi: 10.3748/wjg.v12.i13.2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen J, Edelman RR, Chopra S. Portal vein thrombosis: a review. Am J Med. 1992;92:173–182. doi: 10.1016/0002-9343(92)90109-o. [DOI] [PubMed] [Google Scholar]
- 14.Alpern MB, Rubin JM, Williams DM, Capek P. Porta hepatis: duplex Doppler US with angiographic correlation. Radiology. 1987;162:53–56. doi: 10.1148/radiology.162.1.3538152. [DOI] [PubMed] [Google Scholar]
- 15.Bradbury MS, Kavanagh PV, Bechtold RE, Chen MY, Ott DJ, Regan JD, Weber TM. Mesenteric venous thrombosis: diagnosis and noninvasive imaging. Radiographics. 2002;22:527–541. doi: 10.1148/radiographics.22.3.g02ma10527. [DOI] [PubMed] [Google Scholar]
- 16.Pirisi M, Avellini C, Fabris C, Scott C, Bardus P, Soardo G, Beltrami CA, Bartoli E. Portal vein thrombosis in hepatocellular carcinoma: age and sex distribution in an autopsy study. J Cancer Res Clin Oncol. 1998;124:397–400. doi: 10.1007/s004320050189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chawla Y, Duseja A, Dhiman RK. Review article: the modern management of portal vein thrombosis. Aliment Pharmacol Ther. 2009;30:881–894. doi: 10.1111/j.1365-2036.2009.04116.x. [DOI] [PubMed] [Google Scholar]
- 18.Denninger MH, Chaït Y, Casadevall N, Hillaire S, Guillin MC, Bezeaud A, Erlinger S, Briere J, Valla D. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2000;31:587–591. doi: 10.1002/hep.510310307. [DOI] [PubMed] [Google Scholar]
- 19.Witte CL, Brewer ML, Witte MH, Pond GB. Protean manifestations of pylethrombosis. A review of thirty-four patients. Ann Surg. 1985;202:191–202. doi: 10.1097/00000658-198508000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valla DC, Condat B. Portal vein thrombosis in adults: pathophysiology, pathogenesis and management. J Hepatol. 2000;32:865–871. doi: 10.1016/s0168-8278(00)80259-7. [DOI] [PubMed] [Google Scholar]
- 21.Bick RL. Coagulation abnormalities in malignancy: a review. Semin Thromb Hemost. 1992;18:353–372. doi: 10.1055/s-2007-1002575. [DOI] [PubMed] [Google Scholar]
- 22.Kocher G, Himmelmann A. Portal vein thrombosis (PVT): a study of 20 non-cirrhotic cases. Swiss Med Wkly. 2005;135:372–376. doi: 10.4414/smw.2005.11035. [DOI] [PubMed] [Google Scholar]
- 23.Janssen HL, Meinardi JR, Vleggaar FP, van Uum SH, Haagsma EB, van Der Meer FJ, van Hattum J, Chamuleau RA, Adang RP, Vandenbroucke JP, et al. Factor V Leiden mutation, prothrombin gene mutation, and deficiencies in coagulation inhibitors associated with Budd-Chiari syndrome and portal vein thrombosis: results of a case-control study. Blood. 2000;96:2364–2368. [PubMed] [Google Scholar]
- 24.Mohanty D, Shetty S, Ghosh K, Pawar A, Abraham P. Hereditary thrombophilia as a cause of Budd-Chiari syndrome: a study from Western India. Hepatology. 2001;34:666–670. doi: 10.1053/jhep.2001.27948. [DOI] [PubMed] [Google Scholar]
- 25.Bhattacharyya M, Makharia G, Kannan M, Ahmed RP, Gupta PK, Saxena R. Inherited prothrombotic defects in Budd-Chiari syndrome and portal vein thrombosis: a study from North India. Am J Clin Pathol. 2004;121:844–847. doi: 10.1309/F2U1-XBV4-RXYU-AYG0. [DOI] [PubMed] [Google Scholar]
- 26.Dutta AK, Chacko A, George B, Joseph JA, Nair SC, Mathews V. Risk factors of thrombosis in abdominal veins. World J Gastroenterol. 2008;14:4518–4522. doi: 10.3748/wjg.14.4518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amitrano L, Brancaccio V, Guardascione MA, Margaglione M, Iannaccone L, D’Andrea G, Marmo R, Ames PR, Balzano A. Inherited coagulation disorders in cirrhotic patients with portal vein thrombosis. Hepatology. 2000;31:345–348. doi: 10.1002/hep.510310213. [DOI] [PubMed] [Google Scholar]
- 28.Mack CL, Superina RA, Whitington PF. Surgical restoration of portal flow corrects procoagulant and anticoagulant deficiencies associated with extrahepatic portal vein thrombosis. J Pediatr. 2003;142:197–199. doi: 10.1067/mpd.2003.93. [DOI] [PubMed] [Google Scholar]
- 29.Dubuisson C, Boyer-Neumann C, Wolf M, Meyer D, Bernard O. Protein C, protein S and antithrombin III in children with portal vein obstruction. J Hepatol. 1997;27:132–135. doi: 10.1016/s0168-8278(97)80292-9. [DOI] [PubMed] [Google Scholar]
- 30.Fisher NC, Wilde JT, Roper J, Elias E. Deficiency of natural anticoagulant proteins C, S, and antithrombin in portal vein thrombosis: a secondary phenomenon? Gut. 2000;46:534–539. doi: 10.1136/gut.46.4.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amitrano L, Brancaccio V, Guardascione MA, Margaglione M, Sacco M, Martino R, De Nucci C, Mosca S, Iannaccone L, Ames PR, et al. Portal vein thrombosis after variceal endoscopic sclerotherapy in cirrhotic patients: role of genetic thrombophilia. Endoscopy. 2002;34:535–538. doi: 10.1055/s-2002-33210. [DOI] [PubMed] [Google Scholar]
- 32.Erkan O, Bozdayi AM, Disibeyaz S, Oguz D, Ozcan M, Bahar K, Karayalcin S, Ozden A, Bozkaya H, Yurdaydin C, et al. Thrombophilic gene mutations in cirrhotic patients with portal vein thrombosis. Eur J Gastroenterol Hepatol. 2005;17:339–343. doi: 10.1097/00042737-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Guyatt G. Determining prognosis and creating clinical decision rules. In: Haynes B, Sackett DL, Guyatt G, Tulliez M, editors. Clinical epidemiology. Lippincott Williams & Wilkins; 2006. pp. 323–355. [Google Scholar]
- 34.Walker AP. Portal vein thrombosis: what is the role of genetics? Eur J Gastroenterol Hepatol. 2005;17:705–707. doi: 10.1097/01.meg.0000170927.60979.1d. [DOI] [PubMed] [Google Scholar]
- 35.Sherlock S, Dooley J. The portal venous system and portal hypertension. In: Disease of the liver and biliary system, 10th ed., editors. London: Blackwell Science; 1997. pp. 135–180. [Google Scholar]
- 36.Poort SR, Rosendaal FR, Reitsma PH, Bertina RM. A common genetic variation in the 3’-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood. 1996;88:3698–3703. [PubMed] [Google Scholar]
- 37.Chamouard P, Pencreach E, Maloisel F, Grunebaum L, Ardizzone JF, Meyer A, Gaub MP, Goetz J, Baumann R, Uring-Lambert B, et al. Frequent factor II G20210A mutation in idiopathic portal vein thrombosis. Gastroenterology. 1999;116:144–148. doi: 10.1016/s0016-5085(99)70238-6. [DOI] [PubMed] [Google Scholar]
- 38.Madonna P, De Stefano V, Coppola A, Cerbone AM, Di Minno G. G20210A prothrombin gene mutation and other trombophilic polymorphisms in patients with portal or hepatic venous thrombosis. Gastroenterology. 2001;120:1059–1060. doi: 10.1053/gast.2001.23083. [DOI] [PubMed] [Google Scholar]
- 39.Martinelli I, Sacchi E, Landi G, Taioli E, Duca F, Mannucci PM. High risk of cerebral-vein thrombosis in carriers of a prothrombin-gene mutation and in users of oral contraceptives. N Engl J Med. 1998;338:1793–1797. doi: 10.1056/NEJM199806183382502. [DOI] [PubMed] [Google Scholar]
- 40.Oksüzoglu G, Bayraktar Y, Arslan S, Celik I, Arslan M, Sivri B, Kirazli S, Kayhan B. Portal vein thrombosis in cirrhotics: related with anticardiolipin antibodies? Hepatogastroenterology. 2003;50:1527–1530. [PubMed] [Google Scholar]
- 41.Mangia A, Margaglione M, Cascavilla I, Gentile R, Cappucci G, Facciorusso D, Grandone E, Di Minno G, Rizzetto M, Andriulli A. Anticardiolipin antibodies in patients with liver disease. Am J Gastroenterol. 1999;94:2983–2987. doi: 10.1111/j.1572-0241.1999.01447.x. [DOI] [PubMed] [Google Scholar]
- 42.Wahl DG, Guillemin F, de Maistre E, Perret-Guillaume C, Lecompte T, Thibaut G. Meta-analysis of the risk of venous thrombosis in individuals with antiphospholipid antibodies without underlying autoimmune disease or previous thrombosis. Lupus. 1998;7:15–22. doi: 10.1191/096120398678919688. [DOI] [PubMed] [Google Scholar]
- 43.Liappis AP, Roberts AD, Schwartz AM, Simon GL. Thrombosis and infection: a case of transient anti-cardiolipin antibody associated with pylephlebitis. Am J Med Sci. 2003;325:365–368. doi: 10.1097/00000441-200306000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Gervais A, Czernichow B, Grunebaum L, Wiesel ML, Auperin A, Rivalland D, Gabanyi J, Goldstein L, Cazenave JP, Doffoël M. [Serum cardiolipin antibodies in patients with alcoholic cirrhosis] Gastroenterol Clin Biol. 1996;20:736–742. [PubMed] [Google Scholar]
- 45.Webb LJ, Sherlock S. The aetiology, presentation and natural history of extra-hepatic portal venous obstruction. Q J Med. 1979;48:627–639. [PubMed] [Google Scholar]
- 46.Capron JP, Lemay JL, Muir JF, Dupas JL, Lebrec D, Gineston JL. Portal vein thrombosis and fatal pulmonary thromboembolism associated with oral contraceptive treatment. J Clin Gastroenterol. 1981;3:295–298. doi: 10.1097/00004836-198109000-00016. [DOI] [PubMed] [Google Scholar]
- 47.Lonardo A, Grisendi A, Frazzoni M, Pulvirenti M, Della Casa G. Portal vein thrombosis (PVT) associated with oral contraceptive steroids (OCS) J Gastroenterol Hepatol. 1994;9:314. doi: 10.1111/j.1440-1746.1994.tb01733.x. [DOI] [PubMed] [Google Scholar]
- 48.De Stefano V, Teofili L, Leone G, Michiels JJ. Spontaneous erythroid colony formation as the clue to an underlying myeloproliferative disorder in patients with Budd-Chiari syndrome or portal vein thrombosis. Semin Thromb Hemost. 1997;23:411–418. doi: 10.1055/s-2007-996117. [DOI] [PubMed] [Google Scholar]
- 49.Valla D, Casadevall N, Huisse MG, Tulliez M, Grange JD, Muller O, Binda T, Varet B, Rueff B, Benhamou JP. Etiology of portal vein thrombosis in adults. A prospective evaluation of primary myeloproliferative disorders. Gastroenterology. 1988;94:1063–1069. doi: 10.1016/0016-5085(88)90567-7. [DOI] [PubMed] [Google Scholar]
- 50.Lamy T, Devillers A, Bernard M, Moisan A, Grulois I, Drenou B, Amiot L, Fauchet R, Le Prise PY. Inapparent polycythemia vera: an unrecognized diagnosis. Am J Med. 1997;102:14–20. doi: 10.1016/s0002-9343(96)00351-8. [DOI] [PubMed] [Google Scholar]
- 51.Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, Vassiliou GS, Bench AJ, Boyd EM, Curtin N, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365:1054–1061. doi: 10.1016/S0140-6736(05)71142-9. [DOI] [PubMed] [Google Scholar]
- 52.James C, Ugo V, Le Couédic JP, Staerk J, Delhommeau F, Lacout C, Garçon L, Raslova H, Berger R, Bennaceur-Griscelli A, Villeval JL, Constantinescu SN, Casadevall N, Vainchenker W. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434:1144–1148. doi: 10.1038/nature03546. [DOI] [PubMed] [Google Scholar]
- 53.Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR, Tichelli A, Cazzola M, Skoda RC. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352:1779–1790. doi: 10.1056/NEJMoa051113. [DOI] [PubMed] [Google Scholar]
- 54.Xavier SG, Gadelha T, Pimenta G, Eugenio AM, Ribeiro DD, Gomes FM, Bonamino M, Zalcberg IR, Spector N. JAK2V617F Mutation in Patients with Splanchnic Vein Thrombosis. Dig Dis Sci. 2009:Epub ahead of print. doi: 10.1007/s10620-009-0933-y. [DOI] [PubMed] [Google Scholar]
- 55.Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ, Boggon TJ, Wlodarska I, Clark JJ, Moore S, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;7:387–397. doi: 10.1016/j.ccr.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 56.Colaizzo D, Amitrano L, Tiscia GL, Scenna G, Grandone E, Guardascione MA, Brancaccio V, Margaglione M. The JAK2 V617F mutation frequently occurs in patients with portal and mesenteric venous thrombosis. J Thromb Haemost. 2007;5:55–61. doi: 10.1111/j.1538-7836.2006.02277.x. [DOI] [PubMed] [Google Scholar]
- 57.Primignani M, Barosi G, Bergamaschi G, Gianelli U, Fabris F, Reati R, Dell’Era A, Bucciarelli P, Mannucci PM. Role of the JAK2 mutation in the diagnosis of chronic myeloproliferative disorders in splanchnic vein thrombosis. Hepatology. 2006;44:1528–1534. doi: 10.1002/hep.21435. [DOI] [PubMed] [Google Scholar]
- 58.Gertsch P, Matthews J, Lerut J, Luder P, Blumgart LH. Acute thrombosis of the splanchnic veins. Arch Surg. 1993;128:341–345. doi: 10.1001/archsurg.1993.01420150101018. [DOI] [PubMed] [Google Scholar]
- 59.Malkowski P, Pawlak J, Michalowicz B, Szczerban J, Wroblewski T, Leowska E, Krawczyk M. Thrombolytic treatment of portal thrombosis. Hepatogastroenterology. 2003;50:2098–2100. [PubMed] [Google Scholar]
- 60.Jamieson NV. Changing perspectives in portal vein thrombosis and liver transplantation. Transplantation. 2000;69:1772–1774. doi: 10.1097/00007890-200005150-00006. [DOI] [PubMed] [Google Scholar]
- 61.Kumar S, Sarr MG, Kamath PS. Mesenteric venous thrombosis. N Engl J Med. 2001;345:1683–1688. doi: 10.1056/NEJMra010076. [DOI] [PubMed] [Google Scholar]
- 62.Northup PG, Sundaram V, Fallon MB, Reddy KR, Balogun RA, Sanyal AJ, Anstee QM, Hoffman MR, Ikura Y, Caldwell SH. Hypercoagulation and thrombophilia in liver disease. J Thromb Haemost. 2008;6:2–9. doi: 10.1111/j.1538-7836.2007.02772.x. [DOI] [PubMed] [Google Scholar]
- 63.Sogaard KK, Astrup LB, Vilstrup H, Gronbaek H. Portal vein thrombosis; risk factors, clinical presentation and treatment. BMC Gastroenterol. 2007;7:34. doi: 10.1186/1471-230X-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sobhonslidsuk A, Reddy KR. Portal vein thrombosis: a concise review. Am J Gastroenterol. 2002;97:535–541. doi: 10.1111/j.1572-0241.2002.05527.x. [DOI] [PubMed] [Google Scholar]
- 65.Janssen HL, Wijnhoud A, Haagsma EB, van Uum SH, van Nieuwkerk CM, Adang RP, Chamuleau RA, van Hattum J, Vleggaar FP, Hansen BE, et al. Extrahepatic portal vein thrombosis: aetiology and determinants of survival. Gut. 2001;49:720–724. doi: 10.1136/gut.49.5.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Condat B, Pessione F, Hillaire S, Denninger MH, Guillin MC, Poliquin M, Hadengue A, Erlinger S, Valla D. Current outcome of portal vein thrombosis in adults: risk and benefit of anticoagulant therapy. Gastroenterology. 2001;120:490–497. doi: 10.1053/gast.2001.21209. [DOI] [PubMed] [Google Scholar]
- 67.Sarin SK, Agarwal SR. Extrahepatic portal vein obstruction. Semin Liver Dis. 2002;22:43–58. doi: 10.1055/s-2002-23206. [DOI] [PubMed] [Google Scholar]
- 68.Perlemuter G, Béjanin H, Fritsch J, Prat F, Gaudric M, Chaussade S, Buffet C. Biliary obstruction caused by portal cavernoma: a study of 8 cases. J Hepatol. 1996;25:58–63. doi: 10.1016/s0168-8278(96)80328-x. [DOI] [PubMed] [Google Scholar]
- 69.Dhiman RK, Puri P, Chawla Y, Minz M, Bapuraj JR, Gupta S, Nagi B, Suri S. Biliary changes in extrahepatic portal venous obstruction: compression by collaterals or ischemic? Gastrointest Endosc. 1999;50:646–652. doi: 10.1016/s0016-5107(99)80013-3. [DOI] [PubMed] [Google Scholar]
- 70.Colle I, Van Vlierberghe H, Pattyn P, Troisi R, Vogelaers D, de Hemptinne B, De Vos M. Cholestasis as presenting symptom of portal cavernoma. Hepatol Res. 2003;25:32–37. doi: 10.1016/s1386-6346(02)00172-9. [DOI] [PubMed] [Google Scholar]
- 71.Chandra R, Kapoor D, Tharakan A, Chaudhary A, Sarin SK. Portal biliopathy. J Gastroenterol Hepatol. 2001;16:1086–1092. doi: 10.1046/j.1440-1746.2001.02562.x. [DOI] [PubMed] [Google Scholar]
- 72.Bayraktar Y, Balkanci F, Kayhan B, Ozenç A, Arslan S, Telatar H. Bile duct varices or “pseudo-cholangiocarcinoma sign” in portal hypertension due to cavernous transformation of the portal vein. Am J Gastroenterol. 1992;87:1801–1806. [PubMed] [Google Scholar]
- 73.Bayraktar Y, Balkanci F, Ozenc A, Arslan S, Koseoglu T, Ozdemir A, Uzunalimoglu B, Telatar H, Gurakar A, Van Thiel DH. The “pseudo-cholangiocarcinoma sign” in patients with cavernous transformation of the portal vein and its effect on the serum alkaline phosphatase and bilirubin levels. Am J Gastroenterol. 1995;90:2015–2019. [PubMed] [Google Scholar]
- 74.Molmenti EP, Roodhouse TW, Molmenti H, Jaiswal K, Jung G, Marubashi S, Sanchez EQ, Gogel B, Levy MF, Goldstein RM, et al. Thrombendvenectomy for organized portal vein thrombosis at the time of liver transplantation. Ann Surg. 2002;235:292–296. doi: 10.1097/00000658-200202000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Belli L, Puttini M, Marni A. Extrahepatic portal obstruction: Clinical experience and surgical treatment in 105 patients. J Cardiovasc Surg (Torino) 1980;21:439–448. [PubMed] [Google Scholar]
- 76.Lai L, Brugge WR. Endoscopic ultrasound is a sensitive and specific test to diagnose portal venous system thrombosis (PVST) Am J Gastroenterol. 2004;99:40–44. doi: 10.1046/j.1572-0241.2003.04020.x. [DOI] [PubMed] [Google Scholar]
- 77.Sugiyama M, Hagi H, Atomi Y, Saito M. Diagnosis of portal venous invasion by pancreatobiliary carcinoma: value of endoscopic ultrasonography. Abdom Imaging. 1997;22:434–438. doi: 10.1007/s002619900227. [DOI] [PubMed] [Google Scholar]
- 78.Brugge WR, Lee MJ, Kelsey PB, Schapiro RH, Warshaw AL. The use of EUS to diagnose malignant portal venous system invasion by pancreatic cancer. Gastrointest Endosc. 1996;43:561–567. doi: 10.1016/s0016-5107(96)70191-8. [DOI] [PubMed] [Google Scholar]
- 79.Webster GJ, Burroughs AK, Riordan SM. Review article: portal vein thrombosis -- new insights into aetiology and management. Aliment Pharmacol Ther. 2005;21:1–9. doi: 10.1111/j.1365-2036.2004.02301.x. [DOI] [PubMed] [Google Scholar]
- 80.Ueno N, Sasaki A, Tomiyama T, Tano S, Kimura K. Color Doppler ultrasonography in the diagnosis of cavernous transformation of the portal vein. J Clin Ultrasound. 1997;25:227–233. doi: 10.1002/(sici)1097-0096(199706)25:5<227::aid-jcu2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 81.Haddad MC, Clark DC, Sharif HS, al Shahed M, Aideyan O, Sammak BM. MR, CT, and ultrasonography of splanchnic venous thrombosis. Gastrointest Radiol. 1992;17:34–40. doi: 10.1007/BF01888505. [DOI] [PubMed] [Google Scholar]
- 82.Ito K, Siegelman ES, Stolpen AH, Mitchell DG. MR imaging of complications after liver transplantation. AJR Am J Roentgenol. 2000;175:1145–1149. doi: 10.2214/ajr.175.4.1751145. [DOI] [PubMed] [Google Scholar]
- 83.Okumura A, Watanabe Y, Dohke M, Ishimori T, Amoh Y, Oda K, Dodo Y. Contrast-enhanced three-dimensional MR portography. Radiographics. 1999;19:973–987. doi: 10.1148/radiographics.19.4.g99jl02973. [DOI] [PubMed] [Google Scholar]
- 84.Glockner JF, Forauer AR, Solomon H, Varma CR, Perman WH. Three-dimensional gadolinium-enhanced MR angiography of vascular complications after liver transplantation. AJR Am J Roentgenol. 2000;174:1447–1453. doi: 10.2214/ajr.174.5.1741447. [DOI] [PubMed] [Google Scholar]
- 85.Yerdel MA, Gunson B, Mirza D, Karayalçin K, Olliff S, Buckels J, Mayer D, McMaster P, Pirenne J. Portal vein thrombosis in adults undergoing liver transplantation: risk factors, screening, management, and outcome. Transplantation. 2000;69:1873–1881. doi: 10.1097/00007890-200005150-00023. [DOI] [PubMed] [Google Scholar]
- 86.Smith CS, Sheehy N, McEniff N, Keogan MT. Magnetic resonance portal venography: use of fast-acquisition true FISP imaging in the detection of portal vein thrombosis. Clin Radiol. 2007;62:1180–1188. doi: 10.1016/j.crad.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 87.Garcia-Pagan JC, Valla DC. Portal vein thrombosis: a predictable milestone in cirrhosis? J Hepatol. 2009;51:632–634. doi: 10.1016/j.jhep.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 88.Francoz C, Belghiti J, Vilgrain V, Sommacale D, Paradis V, Condat B, Denninger MH, Sauvanet A, Valla D, Durand F. Splanchnic vein thrombosis in candidates for liver transplantation: usefulness of screening and anticoagulation. Gut. 2005;54:691–697. doi: 10.1136/gut.2004.042796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zocco MA, Di Stasio E, De Cristofaro R, Novi M, Ainora ME, Ponziani F, Riccardi L, Lancellotti S, Santoliquido A, Flore R, et al. Thrombotic risk factors in patients with liver cirrhosis: correlation with MELD scoring system and portal vein thrombosis development. J Hepatol. 2009;51:682–689. doi: 10.1016/j.jhep.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 90.De Sio I, Castellano L, Calandra M, Romano M, Persico M, Del Vecchio-Blanco C. Ultrasound-guided fine needle aspiration biopsy of portal vein thrombosis in liver cirrhosis: results in 15 patients. J Gastroenterol Hepatol. 1995;10:662–665. doi: 10.1111/j.1440-1746.1995.tb01367.x. [DOI] [PubMed] [Google Scholar]
- 91.Plemmons RM, Dooley DP, Longfield RN. Septic thrombophlebitis of the portal vein (pylephlebitis): diagnosis and management in the modern era. Clin Infect Dis. 1995;21:1114–1120. doi: 10.1093/clinids/21.5.1114. [DOI] [PubMed] [Google Scholar]
- 92.Tsujikawa T, Ihara T, Sasaki M, Inoue H, Fujiyama Y, Bamba T. Effectiveness of combined anticoagulant therapy for extending portal vein thrombosis in Crohn’s disease. Report of a case. Dis Colon Rectum. 1996;39:823–825. doi: 10.1007/BF02054451. [DOI] [PubMed] [Google Scholar]
- 93.Hassn AM, Al-Fallouji MA, Ouf TI, Saad R. Portal vein thrombosis following splenectomy. Br J Surg. 2000;87:362–373. doi: 10.1046/j.1365-2168.2000.01383-16.x. [DOI] [PubMed] [Google Scholar]
- 94.Ide T, Ohno Y, Nakanuma Y, Kanematsu T. Early development of cavernomatous vasculatures in portal venous thrombosis: morphometric kinetics in rabbit model. Hepatol Res. 2003;27:136–142. doi: 10.1016/s1386-6346(03)00208-0. [DOI] [PubMed] [Google Scholar]
- 95.Schettino GC, Fagundes ED, Roquete ML, Ferreira AR, Penna FJ. Portal vein thrombosis in children and adolescents. J Pediatr (Rio J) 2006;82:171–178. doi: 10.2223/JPED.1484. [DOI] [PubMed] [Google Scholar]
- 96.Plessier A, Murad SD, Hernandez-Guerra M. A prospective multicentric follow-up study on 105 patients with acute portal vein thrombosis (PVT): Results from the european network for vascular disorders of the liver (en-vie) Hepatology. 2007;46:310a–a. [Google Scholar]
- 97.Amitrano L, Guardascione MA, Scaglione M, Pezzullo L, Sangiuliano N, Armellino MF, Manguso F, Margaglione M, Ames PR, Iannaccone L, et al. Prognostic factors in noncirrhotic patients with splanchnic vein thromboses. Am J Gastroenterol. 2007;102:2464–2470. doi: 10.1111/j.1572-0241.2007.01477.x. [DOI] [PubMed] [Google Scholar]
- 98.Voorhees AB Jr, Price JB Jr. Extrahepatic portal hypertension. A retrospective analysis of 127 cases and associated clinical implications. Arch Surg. 1974;108:338–341. doi: 10.1001/archsurg.1974.01350270068012. [DOI] [PubMed] [Google Scholar]
- 99.Kiladjian JJ, Cervantes F, Leebeek FWG. Role of JAK 2 mutation detection in budd-chiari syndrome (BCS) and portal vein thrombosis (PVT) associated to MPD. Blood. 2006;108:116a–a. [Google Scholar]
- 100.Sheen CL, Lamparelli H, Milne A, Green I, Ramage JK. Clinical features, diagnosis and outcome of acute portal vein thrombosis. QJM. 2000;93:531–534. doi: 10.1093/qjmed/93.8.531. [DOI] [PubMed] [Google Scholar]
- 101.Condat B, Pessione F, Helene Denninger M, Hillaire S, Valla D. Recent portal or mesenteric venous thrombosis: increased recognition and frequent recanalization on anticoagulant therapy. Hepatology. 2000;32:466–470. doi: 10.1053/jhep.2000.16597. [DOI] [PubMed] [Google Scholar]
- 102.Baril N, Wren S, Radin R, Ralls P, Stain S. The role of anticoagulation in pylephlebitis. Am J Surg. 1996;172:449–452; discussion 452-453. doi: 10.1016/S0002-9610(96)00220-6. [DOI] [PubMed] [Google Scholar]
- 103.Lagasse JP, Bahallah ML, Salem N, Debillon G, Labarrière D, Serve MP, Advenier V, Causse X, Legoux JL. [Acute thrombosis of the portal system. Treatment with alteplase and heparin or with heparin alone in 10 patients] Gastroenterol Clin Biol. 1997;21:919–923. [PubMed] [Google Scholar]
- 104.Gao PJ, Zhu JY, Li GM, Leng XS. [Liver transplantation for the patients with end stage liver disease and portal vein thrombosis.] Beijing Daxue Xuebao. 2009;41:558–560. [PubMed] [Google Scholar]
- 105.Van Thiel DH, Schade RR, Starzl TE, Iwatsuki S, Shaw BW Jr, Gavaler JS, Dugas M. Liver transplantation in adults. Hepatology. 1982;2:637–640. doi: 10.1002/hep.1840020517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Shaw BW Jr, Iwatsuki S, Bron K, Starzl TE. Portal vein grafts in hepatic transplantation. Surg Gynecol Obstet. 1985;161:66–68. [PMC free article] [PubMed] [Google Scholar]
- 107.Manzanet G, Sanjuán F, Orbis P, López R, Moya A, Juan M, Vila J, Asensi J, Sendra P, Ruíz J, et al. Liver transplantation in patients with portal vein thrombosis. Liver Transpl. 2001;7:125–131. doi: 10.1053/jlts.2001.21295. [DOI] [PubMed] [Google Scholar]
- 108.Dumortier J, Czyglik O, Poncet G, Blanchet MC, Boucaud C, Henry L, Boillot O. Eversion thrombectomy for portal vein thrombosis during liver transplantation. Am J Transplant. 2002;2:934–938. doi: 10.1034/j.1600-6143.2002.21009.x. [DOI] [PubMed] [Google Scholar]
- 109.Gerunda GE, Merenda R, Neri D, Angeli P, Barbazza F, Valmasoni M, Feltracco P, Zangrandi F, Gangemi A, Miotto D, et al. Cavoportal hemitransposition: a successful way to overcome the problem of total portosplenomesenteric thrombosis in liver transplantation. Liver Transpl. 2002;8:72–75. doi: 10.1053/jlts.2002.30404. [DOI] [PubMed] [Google Scholar]
- 110.Egawa H, Tanaka K, Kasahara M, Takada Y, Oike F, Ogawa K, Sakamoto S, Kozaki K, Taira K, Ito T. Single center experience of 39 patients with preoperative portal vein thrombosis among 404 adult living donor liver transplantations. Liver Transpl. 2006;12:1512–1518. doi: 10.1002/lt.20777. [DOI] [PubMed] [Google Scholar]
- 111.Selvaggi G, Weppler D, Nishida S, Moon J, Levi D, Kato T, Tzakis AG. Ten-year experience in porto-caval hemitransposition for liver transplantation in the presence of portal vein thrombosis. Am J Transplant. 2007;7:454–460. doi: 10.1111/j.1600-6143.2006.01649.x. [DOI] [PubMed] [Google Scholar]
- 112.Gómez-Gutierrez M, Quintela J, Marini M, Gala B, Suarez F, Cao I, Sellés CC, Aguirrezabalaga J, Otero A, Mosteiro S. Portal vein thrombosis in patients undergoing orthotopic liver transplantation: intraoperative endovascular radiological procedures. Transplant Proc. 2005;37:3906–3908. doi: 10.1016/j.transproceed.2005.10.063. [DOI] [PubMed] [Google Scholar]
- 113.Lladó L, Fabregat J, Castellote J, Ramos E, Torras J, Jorba R, Garcia-Borobia F, Busquets J, Figueras J, Rafecas A. Management of portal vein thrombosis in liver transplantation: influence on morbidity and mortality. Clin Transplant. 2007;21:716–721. doi: 10.1111/j.1399-0012.2007.00728.x. [DOI] [PubMed] [Google Scholar]
- 114.Gimeno FA, Calvo J, Loinaz C, Meneu JC, Pérez B, Gomez R, Jiménez C, Abradelo M, Moreno A, Sesma A, et al. Comparative analysis of the results of orthotopic liver transplantation in patients with and without portal vein thrombosis. Transplant Proc. 2005;37:3899–3903. doi: 10.1016/j.transproceed.2005.10.085. [DOI] [PubMed] [Google Scholar]
- 115.Lendoire J, Raffin G, Cejas N, Duek F, Barros Schelotto P, Trigo P, Quarin C, Garay V, Imventarza O. Liver transplantation in adult patients with portal vein thrombosis: risk factors, management and outcome. HPB (Oxford) 2007;9:352–356. doi: 10.1080/13651820701599033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Arcadipane A, Nadalin S, Gruttadauria S, Panarello G, Burgio G, Vizzini G, Luca A, Gridelli B. The recipient with portal thrombosis and/or previous surgery. Transplant Proc. 2008;40:1183–1186. doi: 10.1016/j.transproceed.2008.03.073. [DOI] [PubMed] [Google Scholar]
- 117.Seu P, Shackleton CR, Shaked A, Imagawa DK, Olthoff KM, Rudich SR, Kinkhabwala M, Busuttil RW. Improved results of liver transplantation in patients with portal vein thrombosis. Arch Surg. 1996;131:840–844; discussion 844-845. doi: 10.1001/archsurg.1996.01430200050009. [DOI] [PubMed] [Google Scholar]
- 118.Stieber AC, Zetti G, Todo S, Tzakis AG, Fung JJ, Marino I, Casavilla A, Selby RR, Starzl TE. The spectrum of portal vein thrombosis in liver transplantation. Ann Surg. 1991;213:199–206. doi: 10.1097/00000658-199103000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Davidson BR, Gibson M, Dick R, Burroughs A, Rolles K. Incidence, risk factors, management, and outcome of portal vein abnormalities at orthotopic liver transplantation. Transplantation. 1994;57:1174–1177. doi: 10.1097/00007890-199404270-00006. [DOI] [PubMed] [Google Scholar]
- 120.Robles R, Fernandez JA, Hernández Q, Marín C, Ramírez P, Sánchez-Bueno F, Luján JA, Rodríguez JM, Acosta F, Parrilla P. Eversion thromboendovenectomy in organized portal vein thrombosis during liver transplantation. Clin Transplant. 2004;18:79–84. doi: 10.1111/j.1399-0012.2004.00120.x. [DOI] [PubMed] [Google Scholar]
- 121.Pan C, Shi Y, Zhang JJ, Deng YL, Zheng H, Zhu ZJ, Shen ZY. Single-center experience of 253 portal vein thrombosis patients undergoing liver transplantation in China. Transplant Proc. 2009;41:3761–3765. doi: 10.1016/j.transproceed.2009.06.215. [DOI] [PubMed] [Google Scholar]
- 122.Duffy JP, Hong JC, Farmer DG, Ghobrial RM, Yersiz H, Hiatt JR, Busuttil RW. Vascular complications of orthotopic liver transplantation: experience in more than 4,200 patients. J Am Coll Surg. 2009;208:896–903; discussion 903-905. doi: 10.1016/j.jamcollsurg.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 123.Langnas AN, Marujo W, Stratta RJ, Wood RP, Shaw BW Jr. Vascular complications after orthotopic liver transplantation. Am J Surg. 1991;161:76–82; discussion 82-83. doi: 10.1016/0002-9610(91)90364-j. [DOI] [PubMed] [Google Scholar]
- 124.Lerut J, Tzakis AG, Bron K, Gordon RD, Iwatsuki S, Esquivel CO, Makowka L, Todo S, Starzl TE. Complications of venous reconstruction in human orthotopic liver transplantation. Ann Surg. 1987;205:404–414. doi: 10.1097/00000658-198704000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sharma R, Kashyap R, Jain A, Safadjou S, Graham M, Dwivedi AK, Orloff M. Surgical Complications Following Liver Transplantation in Patients with Portal Vein Thrombosis-A Single-Center Perspective. J Gastrointest Surg. 2009:Epub ahead of print. doi: 10.1007/s11605-009-1111-4. [DOI] [PubMed] [Google Scholar]
- 126.DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of the liver. Hepatology. 2009;49:1729–1764. doi: 10.1002/hep.22772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Clavien PA. Diagnosis and management of mesenteric infarction. Br J Surg. 1990;77:601–603. doi: 10.1002/bjs.1800770602. [DOI] [PubMed] [Google Scholar]
- 128.Brunaud L, Antunes L, Collinet-Adler S, Marchal F, Ayav A, Bresler L, Boissel P. Acute mesenteric venous thrombosis: case for nonoperative management. J Vasc Surg. 2001;34:673–679. doi: 10.1067/mva.2001.117331. [DOI] [PubMed] [Google Scholar]
- 129.Abdu RA, Zakhour BJ, Dallis DJ. Mesenteric venous thrombosis--1911 to 1984. Surgery. 1987;101:383–388. [PubMed] [Google Scholar]
- 130.Turnes J, García-Pagán JC, González M, Aracil C, Calleja JL, Ripoll C, Abraldes JG, Bañares R, Villanueva C, Albillos A, et al. Portal hypertension-related complications after acute portal vein thrombosis: impact of early anticoagulation. Clin Gastroenterol Hepatol. 2008;6:1412–1417. doi: 10.1016/j.cgh.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 131.Rahmouni A, Mathieu D, Golli M, Douek P, Anglade MC, Caillet H, Vasile N. Value of CT and sonography in the conservative management of acute splenoportal and superior mesenteric venous thrombosis. Gastrointest Radiol. 1992;17:135–140. doi: 10.1007/BF01888529. [DOI] [PubMed] [Google Scholar]
- 132.Sarin SK, Sollano JD, Chawla YK, Amarapurkar D, Hamid S, Hashizume M, Jafri W, Kumar A, Kudo M, Lesmana LA, et al. Consensus on extra-hepatic portal vein obstruction. Liver Int. 2006;26:512–519. doi: 10.1111/j.1478-3231.2006.01269.x. [DOI] [PubMed] [Google Scholar]
- 133.de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167–176. doi: 10.1016/j.jhep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 134.Garcia-Pagán JC, Hernández-Guerra M, Bosch J. Extrahepatic portal vein thrombosis. Semin Liver Dis. 2008;28:282–292. doi: 10.1055/s-0028-1085096. [DOI] [PubMed] [Google Scholar]
- 135.Orr DW, Harrison PM, Devlin J, Karani JB, Kane PA, Heaton ND, O’Grady JG, Heneghan MA. Chronic mesenteric venous thrombosis: evaluation and determinants of survival during long-term follow-up. Clin Gastroenterol Hepatol. 2007;5:80–86. doi: 10.1016/j.cgh.2006.09.030. [DOI] [PubMed] [Google Scholar]
- 136.Kitchens CS, Weidner MH, Lottenberg R. Chronic oral anticoagulant therapy for extrahepatic visceral thrombosis is safe. J Thromb Thrombolysis. 2007;23:223–228. doi: 10.1007/s11239-006-9017-4. [DOI] [PubMed] [Google Scholar]
- 137.Schäfer C, Zundler J, Bode JC. Thrombolytic therapy in patients with portal vein thrombosis: case report and review of the literature. Eur J Gastroenterol Hepatol. 2000;12:1141–1145. doi: 10.1097/00042737-200012100-00012. [DOI] [PubMed] [Google Scholar]
- 138.Henao EA, Bohannon WT, Silva MB Jr. Treatment of portal venous thrombosis with selective superior mesenteric artery infusion of recombinant tissue plasminogen activator. J Vasc Surg. 2003;38:1411–1415. doi: 10.1016/s0741-5214(03)01052-8. [DOI] [PubMed] [Google Scholar]
- 139.Tateishi A, Mitsui H, Oki T, Morishita J, Maekawa H, Yahagi N, Maruyama T, Ichinose M, Ohnishi S, Shiratori Y, et al. Extensive mesenteric vein and portal vein thrombosis successfully treated by thrombolysis and anticoagulation. J Gastroenterol Hepatol. 2001;16:1429–1433. doi: 10.1046/j.1440-1746.2001.02557.x. [DOI] [PubMed] [Google Scholar]
- 140.Aytekin C, Boyvat F, Kurt A, Yologlu Z, Coskun M. Catheter-directed thrombolysis with transjugular access in portal vein thrombosis secondary to pancreatitis. Eur J Radiol. 2001;39:80–82. doi: 10.1016/s0720-048x(01)00289-3. [DOI] [PubMed] [Google Scholar]
- 141.Lopera JE, Correa G, Brazzini A, Ustunsoz B, Patel S, Janchai A, Castaneda-Zuniga W. Percutaneous transhepatic treatment of symptomatic mesenteric venous thrombosis. J Vasc Surg. 2002;36:1058–1061. doi: 10.1067/mva.2002.127526. [DOI] [PubMed] [Google Scholar]
- 142.Kercher KW, Sing RF, Watson KW, Matthews BD, LeQuire MH, Heniford BT. Transhepatic thrombolysis in acute portal vein thrombosis after laparoscopic splenectomy. Surg Laparosc Endosc Percutan Tech. 2002;12:131–136. doi: 10.1097/00129689-200204000-00013. [DOI] [PubMed] [Google Scholar]
- 143.Hollingshead M, Burke CT, Mauro MA, Weeks SM, Dixon RG, Jaques PF. Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. J Vasc Interv Radiol. 2005;16:651–661. doi: 10.1097/01.RVI.0000156265.79960.86. [DOI] [PubMed] [Google Scholar]
- 144.Grisham A, Lohr J, Guenther JM, Engel AM. Deciphering mesenteric venous thrombosis: imaging and treatment. Vasc Endovascular Surg. 2005;39:473–479. doi: 10.1177/153857440503900603. [DOI] [PubMed] [Google Scholar]
- 145.Rosendaal FR. Venous thrombosis: a multicausal disease. Lancet. 1999;353:1167–1173. doi: 10.1016/s0140-6736(98)10266-0. [DOI] [PubMed] [Google Scholar]
- 146.Ciccarelli O, Goffette P, Laterre PF, Danse E, Wittebolle X, Lerut J. Transjugular intrahepatic portosystemic shunt approach and local thrombolysis for treatment of early posttransplant portal vein thrombosis. Transplantation. 2001;72:159–161. doi: 10.1097/00007890-200107150-00030. [DOI] [PubMed] [Google Scholar]
- 147.Liatsos C, Vlachogiannakos J, Patch D, Tibballs J, Watkinson A, Davidson B, Rolles K, Burroughs AK. Successful recanalization of portal vein thrombosis before liver transplantation using transjugular intrahepatic portosystemic shunt. Liver Transpl. 2001;7:453–460. doi: 10.1053/jlts.2001.23914. [DOI] [PubMed] [Google Scholar]
- 148.Senzolo M, Tibbals J, Cholongitas E, Triantos CK, Burroughs AK, Patch D. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with and without cavernous transformation. Aliment Pharmacol Ther. 2006;23:767–775. doi: 10.1111/j.1365-2036.2006.02820.x. [DOI] [PubMed] [Google Scholar]
- 149.Bilbao JI, Elorz M, Vivas I, Martínez-Cuesta A, Bastarrika G, Benito A. Transjugular intrahepatic portosystemic shunt (TIPS) in the treatment of venous symptomatic chronic portal thrombosis in non-cirrhotic patients. Cardiovasc Intervent Radiol. 2004;27:474–480. doi: 10.1007/s00270-004-0241-z. [DOI] [PubMed] [Google Scholar]
- 150.Van Ha TG, Hodge J, Funaki B, Lorenz J, Rosenblum J, Straus C, Leef J. Transjugular intrahepatic portosystemic shunt placement in patients with cirrhosis and concomitant portal vein thrombosis. Cardiovasc Intervent Radiol. 2006;29:785–790. doi: 10.1007/s00270-005-0090-4. [DOI] [PubMed] [Google Scholar]
- 151.Wolff M, Hirner A. Current state of portosystemic shunt surgery. Langenbecks Arch Surg. 2003;388:141–149. doi: 10.1007/s00423-003-0367-5. [DOI] [PubMed] [Google Scholar]