Abstract
AIM: To study the protein C activation system in human liver myofibroblasts, and the effects of activated protein C (APC) on these cells.
METHODS: Human liver myofibroblasts were obtained by outgrowth. Expression of protease activated receptor 1 (PAR-1), endothelial protein C receptor (EPCR) and thrombomodulin (TM) was analyzed by flow cytometry. Extracellular signal-regulated kinase (ERK)1/2 activation was assessed by Western blotting using anti-phospho-ERK antibodies. Collagen synthesis was studied with real-time reverse transcription-polymerase chain reaction (RT-PCR). Activation of protein C was studied by incubating liver myofibroblasts with zymogen protein C in the presence of thrombin and detecting the generation of APC with a colorimetric assay using a peptide substrate.
RESULTS: Primary cultures of human liver myofibroblasts expressed EPCR on their surface, together with PAR-1 and TM. This receptor system was functional since exposure of myofibroblasts to APC induced ERK1/2 phosphorylation in a dose- and time-dependent manner. Furthermore, APC significantly upregulated the expression of collagen mRNA, as shown by real-time RT-PCR. Collagen upregulation was controlled through the ERK pathway as it was inhibited when using the mitogen-activated protein/extracellular signal-regulated kinase kinase inhibitor PD98059. Finally, using a cell-based colorimetric assay, we showed that intact myofibroblasts converted protein C into APC in the presence of thrombin.
CONCLUSION: These data suggest that APC is a new modulator of liver myofibroblast activity and contributes to the pathophysiology of chronic liver diseases.
Keywords: Liver fibrosis, Thrombin, Activated protein C, Protease-activated receptor
INTRODUCTION
Liver myofibroblasts are key players in the pathogenesis of chronic liver diseases such as fibrosis and cancer. Liver fibrosis is a major health problem as it complicates every chronic liver disease, whether due to hepatitis viruses, alcohol, non-alcoholic steatohepatitis or other causes. Liver fibrosis may progress to cirrhosis, which is an important cause of morbidity. The cell types responsible for the deposition of the excess extracellular matrix characteristic of fibrosis have been identified as being predominantly hepatic stellate cells and portal fibroblasts[1,2]. During liver injury, these cells differentiate into myofibroblasts that proliferate and synthesize fibrosis components. Besides liver fibrosis, a number of studies have shown that the stroma of hepatocellular carcinoma, the major type of primary liver cancer, is populated with myofibroblasts that play major roles in promoting, for instance, extracellular matrix deposition and tumor cell invasion[3-7].
Recently, we and others have demonstrated that the serine proteinase thrombin, a key effector of blood coagulation, affects the phenotype of liver myofibroblasts[8-11] and behaves as a pro-fibrogenic molecule in the liver[12,13]. Experiments using either antagonists[12], or knock-out animals[14] have shown that the pro-fibrogenic effects of thrombin are dependent largely upon signal transduction through protease activated receptor-1 (PAR-1). Upon binding to PAR-1, thrombin cleaves the N terminus of the receptor and the new N terminus behaves as a tethered ligand that activates another PAR1 molecule, which leads to intracellular signaling[15]. Besides thrombin, PAR-1 is also a receptor for several other molecules that include matrix metalloproteinase-1[16] and especially activated protein C (APC)[17].
APC is generated from protein C (PC) by cleavage with thrombin. This requires that thrombin is bound to thrombomodulin (TM), and PC to its specific cell surface receptor, endothelial protein C receptor (EPCR). The best-known functions of APC are its anticoagulant properties through proteolytic inactivation of factors Va and VIIIa. However, cellular effects of APC have also been shown, which depend on PAR-1 signaling upon interaction with EPCR-bound APC. EPCR is deemed endothelium-specific, therefore, these effects have been studied mostly in endothelial cells where APC is credited with a cytoprotective effect. Recently, EPCR expression also has been demonstrated on a few other cell types, such as lung epithelial cells[18], leukocytes[19], keratinocytes[20], and vascular smooth muscle cells[21]. Liver myofibroblasts exhibit many common features with vascular smooth muscle cells, and it is already known that they express functional PAR-1, therefore, we questioned whether they express other cell surface components of the APC system and have functional responses to APC.
MATERIALS AND METHODS
Materials
Human PC was purified from plasma as described previously[22]. APC was generated using the Agkistrodon contortrix contortrix C snake venom protease that recognizes the thrombin cleavage site in PC[23]. Monoclonal anti-EPCR antibodies (JRK 1494 and HEPCR 1489) and anti-TM antibody (CTM 1009) were kindly provided by Dr. Charles Esmon. Anti-PAR-1 was from Santa Cruz Biotechnology Inc. (Santa Cruz, CA, USA; clone ATAP2), and anti-smooth muscle α-actin (ASMA) from Dako (clone 1A4). Human thrombin (1000 NIH U/mg) was from Sigma (St Louis, MO, USA; T4393).
Cell culture
Human hepatic myofibroblasts were obtained from explants of non-tumor liver resected during partial hepatectomy, and characterized as described previously[24,25]. Specifically, the procedure, based on the selective growth advantage of myofibroblasts in the culture conditions used, allowed for a 100% pure myofibroblast population, as shown by positive staining for ASMA and vimentin, and negative staining for CD68 (a Kupffer cell marker), von Willebrand factor (an endothelial cell marker) or cytokeratin (an epithelial cell marker). Myofibroblasts were used between the 3rd and the 6th passage, and were grown in DMEM that contained 5% fetal calf serum, 5% pooled human serum and 5 ng/mL epidermal growth factor (EGF). EGF was removed from the medium at least 3 d before the experiments were conducted.
Flow cytometry
Myofibroblasts were detached from culture plates by incubation in 2 mmol/L EDTA for 15 min at 37°C and collected by centrifugation. One to two hundred thousand cells were incubated with anti-EPCR (JRK 1494, 1/1000), anti-TM (1/50), or anti-PAR-1 (1/50) antibodies. Following a wash with PBS/0.1% BSA, cells were incubated with a secondary phycoerythrin-coupled antibody (1/200) for 15 min at 4°C. After a final wash, the cells were resuspended in PBS/0.1% BSA for analysis.
Mitogen-activated protein kinase (MAPK) phosphorylation
Extracellular signal-regulated kinase (ERK) phosphorylation was measured essentially as described previously[10]. Briefly, cells were grown to confluency and serum-starved for 2 d, and subsequently exposed to the required agonists in serum-free Waymouth medium. At the end of the incubation, cell lysates were prepared in the presence of proteases and phosphatase inhibitors as described previously[4]. Equivalent amounts of proteins were separated by SDS-PAGE, transferred to polyvinylidene difluoride membranes, and analyzed by Western blotting for MAPK phosphorylation using phospho-ERK antibody (Cell Signaling Technology, Beverly, MA, USA). The blots were washed and the appropriate peroxidase-conjugated secondary antibody was applied. Immuno-detected proteins were visualized by using an enhanced chemiluminescence assay (Amersham Biopharmacia, Orsay, France). Membranes were stripped and reblotted using antibody to total-ERK. Signals were acquired on a Macintosh computer connected to a Kodak Digital Science DC120 camera and were quantified by using NIH Imaging software.
APC generation
APC generation from PC by human liver myofibroblasts was demonstrated with a colorimetric method using commercial reagents (Spectrozyme aPC plasma specific chromogenic substrate; American Diagnostica, Greenwich, CT, USA). Briefly, confluent quiescent myofibroblasts were incubated for 30 min with purified PC with or without added thrombin 0.1 U/mL (1.8 nmol/L) in HBSS/0.1% BSA. Supernatants were collected and incubated with an APC chromogenic substrate. The optical density of the solution was measured at 405 nm in a Dynatech microplate reader (MTX Lab Systems, Inc., Vienna, VA, USA).
Reverse transcription-polymerase chain reaction (RT-PCR) for collagen I
Total RNA was extracted from liver samples using Nucleospin RNA II (Macherey Nagel, Düren, Germany). RNA was reverse transcribed using Superscript II (Promega, Charbonnieres-les-Bains, France). Nucleotide sequences of primers for collagen α1(I) and for RLP0 (which encodes the human acidic ribosomal phosphoprotein P0, used as a control) are shown in Table 1. Controls without template or reverse transcriptase were also performed.
Table 1.
Primer sequences used for real-time quantitative reverse transcription-polymerase chain reaction (RT-PCR)
| Name | Primer sequence | Amplicon size (bp) |
| RLP0 | F: 5'-GGCGACCTGGAAGTCCAACT-3' | 149 |
| R: 5'-CCATCAGCACCACAGCCTTC-3' | ||
| Collagen α1(I) | F: 5'-ATGTTCAGCTTTGTGGACCT-3' | 92 |
| R: 5'-CAGCTGACTTCAGGGATGT-3' |
PCR reactions were performed using a Stratagene × 4000 thermocycler (Stratagene, Amsterdam, The Netherlands) and the SYBR Green PCR Core reagents kit (Bio-Rad, Marnes-la-Coquette, France). Five microliters of diluted cDNA samples (produced from 3 ng RNA) were added to 20 μL PCR master mix, and experiments were performed in duplicate. Data analysis was performed using Mx4000 version 4.2 (Stratagene). Gene expression results were first normalized to internal control RLP0[26], and the relative levels of expression were quantified by calculating 2-∆∆Ct[27].
Statistical analysis
Differences between multiple means were analyzed by the non-parametric Kruskal-Wallis test using the StatCrunch software (http://www.statcrunch.com). A value of P < 0.05 was considered significant.
RESULTS
Cultured myofibroblasts express the APC activating complex
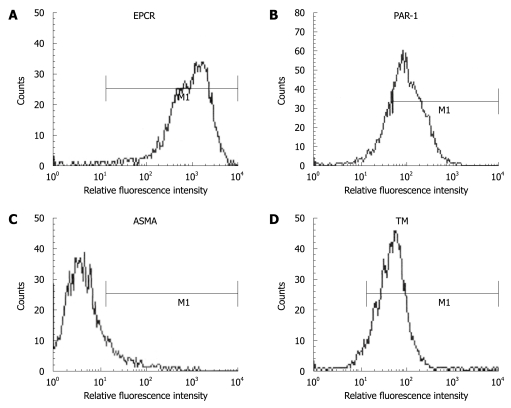
APC signaling requires the presence of EPCR and PAR-1 at the cell surface. We thus examined the expression of these two receptors on cultured human liver myofibroblasts, using flow cytometry on unpermeabilized cells. As shown in Figure 1, liver myofibroblasts expressed easily detectable EPCR and PAR-1. As a control to show that we detected only cell-surface-exposed molecules, we similarly labeled the cells with an antibody to ASMA, an abundant cytoplasmic protein, and found no signal (Figure 1C), although this protein could be demonstrated easily by Western blotting of cell extracts (data not shown). Thus, myofibroblasts express APC receptors on their surface. In addition, we also showed the expression of TM, the thrombin receptor required for PC cleavage (Figure 1D).
Figure 1.
Human liver myofibroblasts express endothelial protein C receptor (EPCR) (A), protease activated receptor 1 (PAR-1) (B), anti-smooth muscle α-actin (ASMA) (C) and thrombomodulin (TM) (D). Fixed unpermeabilized cells were labeled with antibodies to ASMA and thrombomodulin, and analyzed by flow cytometry. The signal obtained with a control antibody was superimposable with that of ASMA and was not shown for clarity.
APC induces intracellular signaling
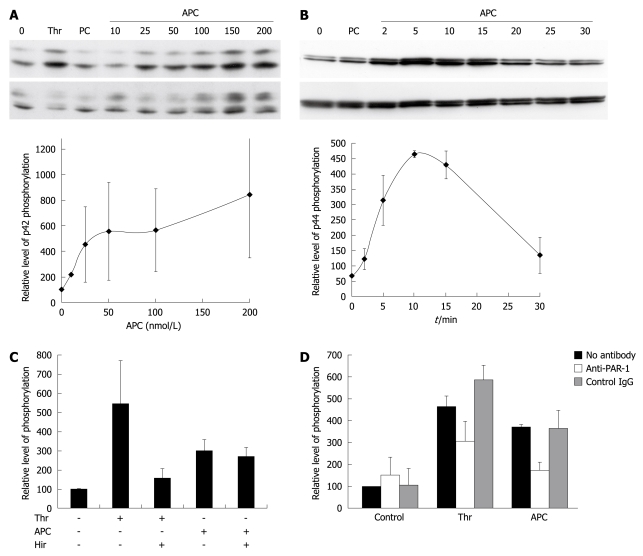
As a readout for the effects of APC, we measured the phosphorylation of the MAPKs ERK1 and ERK2, which is a hallmark of signaling via PAR-1. Western blotting demonstrated a dose-dependent increase in phosphorylation of ERK1/2. The maximum level of phosphorylation obtained at a concentration of 100 nmol/L was comparable with that obtained with 27 nmol/L thrombin (1 IU/mL) (Figure 2A). Non-activated PC had no detectable effect. The effect of APC reached a maximum after 10 min of stimulation (Figure 2B). Although the preparation of APC from PC avoided the use of thrombin, we made sure that the effects of APC were not due to trace amounts of thrombin. Thus, cells were pretreated with the specific thrombin inhibitor, hirudin, prior to APC addition. Although hirudin abolished the effects of thrombin on ERK1/2 phosphorylation, it didnot alter those of APC, which indicated that they were not caused by contaminating thrombin (Figure 2C).
Figure 2.
Effect of activated protein C (APC) on extracellular signal-regulated kinase (ERK) phosphorylation. A: Dose-response of APC. Cells were exposed for 10 min to 27 nmol/L thrombin (Thr), 100 nmol/L nonactivated protein C (PC), or APC. ERK phosphorylation was assessed using Western blotting. The upper panel shows a blot labeled with an antibody to phospho-ERK, and the lower panel shows the same blot re-hybridized with an antibody to total ERK. The graph shows the quantification of p42 phosphorylation in three similar independent experiments. Results are shown as mean ± SE. Phospho-p42 signals were normalized first to total p42 signals, and the results were expressed as a percentage of the non-stimulated control. Similar results were obtained when quantitating p44 phosphorylation; B: Kinetics of APC induced phosphorylation of ERK. Cells were exposed to 100 nmol/L APC. The upper panel shows a blot labeled with an antibody to phospho-ERK, and the lower panel shows the same blot re-hybridized with an antibody to total ERK. The graph shows the quantification of p44 phosphorylation in three similar independent experiments. Phospho-p44 signals were normalized first to total p44 signals, and the results were expressed as a percentage of the non-stimulated control. Similar results were obtained when quantitating p42 phosphorylation; C: APC effect is not due to contaminating thrombin. Cells were exposed for 10 min to 27 nmol/L Thr or 100 nmol/L APC. They were pretreated with or without hirudin. The graph shows the quantification of combined ERK1/ERK2 phosphorylation in four similar independent experiments; D: APC signals through PAR-1. Cells were exposed for 10 min to 27 nmol/L Thr or 100 nmol/L APC. They were preincubated with the indicated antibodies. The graph shows the quantification of combined ERK1/ERK2 phosphorylation in three similar independent experiments.
In order to know whether the effects of APC required PAR-1, cells were incubated with blocking antibodies to PAR-1 or control IgG before adding APC. The PAR-1 antibody blocked by 56.0% ± 8.7% the effect of APC on ERK1/2 phosphorylation, and as expected, also that of thrombin (37.6% ± 10.9%, P = 0.03 in both cases) (Figure 2D).
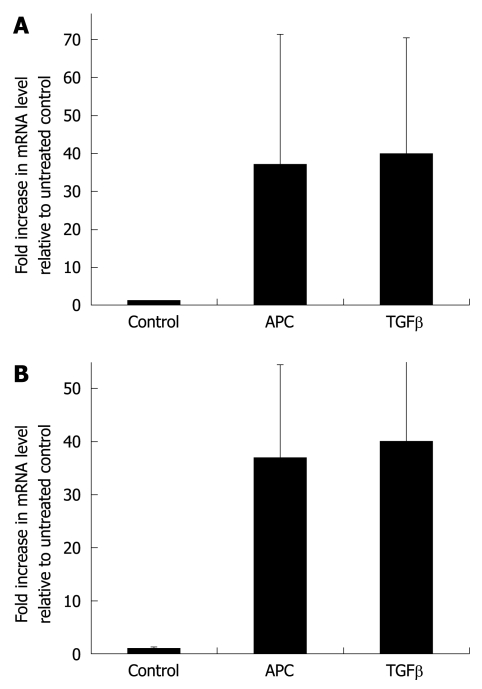
APC signaling leads to increased collagen synthesis
We found that exposure of cells to APC significantly increased the amount of α1(I) collagen transcripts as compared to the control conditions. Actually, under the conditions used, the effects of 100 nmol/L APC were equivalent to those of transforming growth factor-β, a prototypic inducer of extracellular matrix synthesis, used at a concentration of 1 ng/mL (Figure 3A). In order to know whether this effect of APC involved MAPK signaling, experiments were repeated with or without addition of the MAPK inhibitor PD98059. As shown in Figure 3B, treatment with PD98059 abrogated the effect of APC on α1(I) expression.
Figure 3.
APC upregulates collagen transcripts. A: Cells were exposed for 24 h to 100 nmol/L APC or 1 ng/mL transforming growth factor-β1. Collagen transcripts were measured by real-time reverse transcription-polymerase chain reaction and normalized to those of the RPL0 gene. Results are expressed as fold increase over control values and are the mean ± SE of five experiments; B: Cells were exposed for 6 h to 100 nmol/L APC, in the presence or absence of the mitogen-activated protein kinase (MAPK) inhibitor PD98059 (50 μmol/L), before measuring collagen transcripts. Results are the mean ± SE of three experiments.
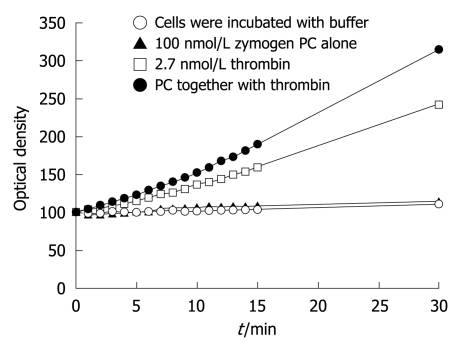
Myofibroblasts generate APC from PC
Human liver myofibroblasts expressed all components of the APC-generating system, therefore, we asked whether they provided a suitable surface for APC generation from PC. We thus incubated cells with the PC zymogen alone or together with thrombin. As shown in Figure 4, incubation of myofibroblasts with PC in the absence of thrombin didnot lead to cleavage of the chromogenic substrate. Thrombin alone had a known nonspecific effect[28], which was abolished by hirudin (data not shown). However, when PC and thrombin were added, the amount of peptide cleavage was considerably greater, which indicated that APC was generated.
Figure 4.
Human liver myofibroblasts can generate APC from PC. Supernatants were collected and incubated with an APC chromogenic substrate. The graph shows the optical density at 405 nmol/L, which resulted from cleavage of the substrate, which was proportional to the amount of APC generated. It represents the mean of two separate experiments.
DISCUSSION
We show here that human liver myofibroblasts express EPCR. EPCR is functional since treatment of myofibroblasts with APC leads to enhanced ERK phosphorylation, a hallmark of PAR-1 activation[29]. We found that APC upregulated collagen mRNA levels, which suggests its role in extracellular matrix metabolism, which is one of the major functions of liver myofibroblasts. It has been shown previously that APC signaling via PAR-1 and EPCR leads to extracellular matrix remodeling[20]. It is thus possible that APC contributes, together with thrombin, to the liver wound-healing response.
We further showed that myofibroblasts also express TM, the thrombin receptor required for activation of PC to APC. This raised the hypothesis that myofibroblasts could provide a suitable surface for generation of APC from PC in the presence of thrombin. This was indeed proven in the cell-based assay that we ran. Thus, liver myofibroblasts, in addition to endothelial cells, are among the rare cell types that can generate APC. APC generation by liver myofibroblasts could prove extremely important for these cells to respond to APC under physiological or pathophysiological conditions. Indeed, APC and thrombin share the same signaling receptor, PAR-1, but efficient activation by APC requires concentrations about 10 000-fold higher than those of thrombin[30]. It is thus not yet entirely clear how APC, which requires thrombin for its generation, can still activate PAR-1 in the presence of thrombin. However, recent evidence suggests that APC signaling is much more efficient when APC is locally generated from PC than when provided exogenously[31]. This may be linked to the observation that receptors for PC activation and APC signaling are co-localized within lipid rafts[32]. Our finding that human liver myofibroblasts can generate APC makes it very likely that they can respond efficiently to endogenously generated APC. There is evidence that thrombin, which is required for PC activation, is generated in the fibrotic liver, as demonstrated by the presence of fibrin deposition in experimental[33] or human liver disease[34]. Therefore, our data suggest that APC can indeed contribute to the pathophysiology of chronic liver diseases through effects on liver myofibroblasts, in addition to endothelial cells.
COMMENTS
Background
A number of recent studies have emphasized the interface between liver fibrosis and the blood hemostasis system, by showing the deleterious role of thrombin and its cellular receptors on the progression of liver fibrosis.
Research frontiers
Activated protein C (APC) is a major inhibitor of coagulation but also has cytokine-like properties by interacting with a complex of cell surface receptors. Besides endothelial cells, few cells have been shown to express such functional receptors.
Innovations and breakthroughs
In this study, the authors showed that human liver myofibroblasts, the major fibrogenic cell type in the liver, can bind and activate protein C (PC). Furthermore, they demonstrate that APC triggers collagen synthesis in these cells, which suggests that the local generation of APC by myofibroblasts in the liver may modulate the liver wound-healing process.
Applications
This study gives new insight into the interplay between blood hemostasis components and liver fibrogenesis.
Terminology
PC is a circulating protein that can be activated following binding to the endothelial protein C receptor by thrombin, itself bound to thrombomodulin. APC is a major inhibitor of blood coagulation. It can also bind to cell surface protease activated receptor-1 and induce intracellular signals, like a cytokine.
Peer review
The manuscript is clear and the results are convincing. The data add important new details about pro-fibrogenic activity of liver myofibroblasts.
Acknowledgments
We thank Dr. C Esmon for antibodies.
Footnotes
Peer reviewer: Dr. Katja Breitkopf, Department of Medicine II, University Hospital Mannheim, University of Heidelberg, Theodor-Kutzer-Ufer 1-3, 68167 Mannheim, Germany
S- Editor Tian L L- Editor Kerr C E- Editor Zheng XM
References
- 1.Lotersztajn S, Julien B, Teixeira-Clerc F, Grenard P, Mallat A. Hepatic fibrosis: molecular mechanisms and drug targets. Annu Rev Pharmacol Toxicol. 2005;45:605–628. doi: 10.1146/annurev.pharmtox.45.120403.095906. [DOI] [PubMed] [Google Scholar]
- 2.Friedman SL. Mechanisms of hepatic fibrogenesis. Gastroenterology. 2008;134:1655–1669. doi: 10.1053/j.gastro.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Faouzi S, Le Bail B, Neaud V, Boussarie L, Saric J, Bioulac-Sage P, Balabaud C, Rosenbaum J. Myofibroblasts are responsible for collagen synthesis in the stroma of human hepatocellular carcinoma: an in vivo and in vitro study. J Hepatol. 1999;30:275–284. doi: 10.1016/s0168-8278(99)80074-9. [DOI] [PubMed] [Google Scholar]
- 4.Neaud V, Faouzi S, Guirouilh J, Le Bail B, Balabaud C, Bioulac-Sage P, Rosenbaum J. Human hepatic myofibroblasts increase invasiveness of hepatocellular carcinoma cells: evidence for a role of hepatocyte growth factor. Hepatology. 1997;26:1458–1466. doi: 10.1053/jhep.1997.v26.pm0009397985. [DOI] [PubMed] [Google Scholar]
- 5.Le Bail B, Faouzi S, Boussarie L, Guirouilh J, Blanc JF, Carles J, Bioulac-Sage P, Balabaud C, Rosenbaum J. Osteonectin/SPARC is overexpressed in human hepatocellular carcinoma. J Pathol. 1999;189:46–52. doi: 10.1002/(SICI)1096-9896(199909)189:1<46::AID-PATH392>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 6.Ooi LP, Crawford DH, Gotley DC, Clouston AD, Strong RW, Gobe GC, Halliday JW, Bridle KR, Ramm GA. Evidence that "myofibroblast-like" cells are the cellular source of capsular collagen in hepatocellular carcinoma. J Hepatol. 1997;26:798–807. doi: 10.1016/s0168-8278(97)80245-0. [DOI] [PubMed] [Google Scholar]
- 7.Amann T, Bataille F, Spruss T, Mühlbauer M, Gäbele E, Schölmerich J, Kiefer P, Bosserhoff AK, Hellerbrand C. Activated hepatic stellate cells promote tumorigenicity of hepatocellular carcinoma. Cancer Sci. 2009;100:646–653. doi: 10.1111/j.1349-7006.2009.01087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaça MD, Zhou X, Benyon RC. Regulation of hepatic stellate cell proliferation and collagen synthesis by proteinase-activated receptors. J Hepatol. 2002;36:362–369. doi: 10.1016/s0168-8278(01)00285-9. [DOI] [PubMed] [Google Scholar]
- 9.Mallat A, Gallois C, Tao J, Habib A, Maclouf J, Mavier P, Préaux AM, Lotersztajn S. Platelet-derived growth factor-BB and thrombin generate positive and negative signals for human hepatic stellate cell proliferation. Role of a prostaglandin/cyclic AMP pathway and cross-talk with endothelin receptors. J Biol Chem. 1998;273:27300–27305. doi: 10.1074/jbc.273.42.27300. [DOI] [PubMed] [Google Scholar]
- 10.Neaud V, Duplantier JG, Mazzocco C, Kisiel W, Rosenbaum J. Thrombin up-regulates tissue factor pathway inhibitor-2 synthesis through a cyclooxygenase-2-dependent, epidermal growth factor receptor-independent mechanism. J Biol Chem. 2004;279:5200–5206. doi: 10.1074/jbc.M306679200. [DOI] [PubMed] [Google Scholar]
- 11.Gillibert-Duplantier J, Neaud V, Blanc JF, Bioulac-Sage P, Rosenbaum J. Thrombin inhibits migration of human hepatic myofibroblasts. Am J Physiol Gastrointest Liver Physiol. 2007;293:G128–G136. doi: 10.1152/ajpgi.00031.2007. [DOI] [PubMed] [Google Scholar]
- 12.Fiorucci S, Antonelli E, Distrutti E, Severino B, Fiorentina R, Baldoni M, Caliendo G, Santagada V, Morelli A, Cirino G. PAR1 antagonism protects against experimental liver fibrosis. Role of proteinase receptors in stellate cell activation. Hepatology. 2004;39:365–375. doi: 10.1002/hep.20054. [DOI] [PubMed] [Google Scholar]
- 13.Duplantier JG, Dubuisson L, Senant N, Freyburger G, Laurendeau I, Herbert JM, Desmoulière A, Rosenbaum J. A role for thrombin in liver fibrosis. Gut. 2004;53:1682–16827. doi: 10.1136/gut.2003.032136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rullier A, Gillibert-Duplantier J, Costet P, Cubel G, Haurie V, Petibois C, Taras D, Dugot-Senant N, Deleris G, Bioulac-Sage P, et al. Protease-activated receptor 1 knockout reduces experimentally induced liver fibrosis. Am J Physiol Gastrointest Liver Physiol. 2008;294:G226–G235. doi: 10.1152/ajpgi.00444.2007. [DOI] [PubMed] [Google Scholar]
- 15.Coughlin SR. How the protease thrombin talks to cells. Proc Natl Acad Sci USA. 1999;96:11023–11027. doi: 10.1073/pnas.96.20.11023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boire A, Covic L, Agarwal A, Jacques S, Sherifi S, Kuliopulos A. PAR1 is a matrix metalloprotease-1 receptor that promotes invasion and tumorigenesis of breast cancer cells. Cell. 2005;120:303–313. doi: 10.1016/j.cell.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 17.Riewald M, Ruf W. Protease-activated receptor-1 signaling by activated protein C in cytokine-perturbed endothelial cells is distinct from thrombin signaling. J Biol Chem. 2005;280:19808–19814. doi: 10.1074/jbc.M500747200. [DOI] [PubMed] [Google Scholar]
- 18.Shimizu S, Gabazza EC, Taguchi O, Yasui H, Taguchi Y, Hayashi T, Ido M, Shimizu T, Nakagaki T, Kobayashi H, et al. Activated protein C inhibits the expression of platelet-derived growth factor in the lung. Am J Respir Crit Care Med. 2003;167:1416–1426. doi: 10.1164/rccm.200206-515OC. [DOI] [PubMed] [Google Scholar]
- 19.Sturn DH, Kaneider NC, Feistritzer C, Djanani A, Fukudome K, Wiedermann CJ. Expression and function of the endothelial protein C receptor in human neutrophils. Blood. 2003;102:1499–1505. doi: 10.1182/blood-2002-12-3880. [DOI] [PubMed] [Google Scholar]
- 20.Xue M, Campbell D, Sambrook PN, Fukudome K, Jackson CJ. Endothelial protein C receptor and protease-activated receptor-1 mediate induction of a wound-healing phenotype in human keratinocytes by activated protein C. J Invest Dermatol. 2005;125:1279–1285. doi: 10.1111/j.0022-202X.2005.23952.x. [DOI] [PubMed] [Google Scholar]
- 21.Bretschneider E, Uzonyi B, Weber AA, Fischer JW, Pape R, Lötzer K, Schrör K. Human vascular smooth muscle cells express functionally active endothelial cell protein C receptor. Circ Res. 2007;100:255–262. doi: 10.1161/01.RES.0000255685.06922.c7. [DOI] [PubMed] [Google Scholar]
- 22.Kisiel W. Human plasma protein C: isolation, characterization, and mechanism of activation by alpha-thrombin. J Clin Invest. 1979;64:761–769. doi: 10.1172/JCI109521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kisiel W, Kondo S, Smith KJ, McMullen BA, Smith LF. Characterization of a protein C activator from Agkistrodon contortrix contortrix venom. J Biol Chem. 1987;262:12607–12613. [PubMed] [Google Scholar]
- 24.Win KM, Charlotte F, Mallat A, Cherqui D, Martin N, Mavier P, Preaux AM, Dhumeaux D, Rosenbaum J. Mitogenic effect of transforming growth factor-beta 1 on human Ito cells in culture: evidence for mediation by endogenous platelet-derived growth factor. Hepatology. 1993;18:137–145. [PubMed] [Google Scholar]
- 25.Blazejewski S, Preaux AM, Mallat A, Brocheriou I, Mavier P, Dhumeaux D, Hartmann D, Schuppan D, Rosenbaum J. Human myofibroblastlike cells obtained by outgrowth are representative of the fibrogenic cells in the liver. Hepatology. 1995;22:788–797. [PubMed] [Google Scholar]
- 26.Bièche I, Noguès C, Paradis V, Olivi M, Bedossa P, Lidereau R, Vidaud M. Quantitation of hTERT gene expression in sporadic breast tumors with a real-time reverse transcription-polymerase chain reaction assay. Clin Cancer Res. 2000;6:452–459. [PubMed] [Google Scholar]
- 27.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 28.Iakhiaev A, Idell S. Activation and degradation of protein C by primary rabbit pleural mesothelial cells. Lung. 2006;184:81–88. doi: 10.1007/s00408-005-2566-z. [DOI] [PubMed] [Google Scholar]
- 29.Riewald M, Petrovan RJ, Donner A, Mueller BM, Ruf W. Activation of endothelial cell protease activated receptor 1 by the protein C pathway. Science. 2002;296:1880–1882. doi: 10.1126/science.1071699. [DOI] [PubMed] [Google Scholar]
- 30.Feistritzer C, Riewald M. Endothelial barrier protection by activated protein C through PAR1-dependent sphingosine 1-phosphate receptor-1 crossactivation. Blood. 2005;105:3178–3184. doi: 10.1182/blood-2004-10-3985. [DOI] [PubMed] [Google Scholar]
- 31.Feistritzer C, Schuepbach RA, Mosnier LO, Bush LA, Di Cera E, Griffin JH, Riewald M. Protective signaling by activated protein C is mechanistically linked to protein C activation on endothelial cells. J Biol Chem. 2006;281:20077–20084. doi: 10.1074/jbc.M600506200. [DOI] [PubMed] [Google Scholar]
- 32.Bae JS, Yang L, Rezaie AR. Receptors of the protein C activation and activated protein C signaling pathways are colocalized in lipid rafts of endothelial cells. Proc Natl Acad Sci USA. 2007;104:2867–2872. doi: 10.1073/pnas.0611493104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neubauer K, Knittel T, Armbrust T, Ramadori G. Accumulation and cellular localization of fibrinogen/fibrin during short-term and long-term rat liver injury. Gastroenterology. 1995;108:1124–1135. doi: 10.1016/0016-5085(95)90211-2. [DOI] [PubMed] [Google Scholar]
- 34.Marsden PA, Ning Q, Fung LS, Luo X, Chen Y, Mendicino M, Ghanekar A, Scott JA, Miller T, Chan CW, et al. The Fgl2/fibroleukin prothrombinase contributes to immunologically mediated thrombosis in experimental and human viral hepatitis. J Clin Invest. 2003;112:58–66. doi: 10.1172/JCI18114. [DOI] [PMC free article] [PubMed] [Google Scholar]