Abstract
We report the first case of single port laparoscopic right hemicolectomy for advanced colon cancer. An abdominal 3 cm length incision was made via the umbilicus. A small wound retractor and a surgical glove were used as a single port. All soft tissue anterior to the superior mesenteric vein was completely removed and D3 lymph node dissection was achieved. The total operative time was 180 min with minimal blood loss (< 50 mL). The size of the tumor was 5 cm × 3 cm and its tumor stage was T3N0. Sixty-nine lymph nodes were harvested and none were positive. We believe that single port surgery for colon cancer is a feasible and safe procedure with surgical results comparable to conventional laparoscopic procedures.
Keywords: Single port laparoscopic surgery, Colon cancer, D3 lymph node dissection
INTRODUCTION
The laparoscopic approach for colorectal surgery has been shown to result in shorter hospital stays, faster return of bowel function, less pain and better cosmetic results than open surgery[1,2]. Moreover, the long term recurrence and survival results of laparoscopic surgery for advanced colon cancer are not different from those of conventional surgery[3,4]. Therefore, laparoscopic surgery has been considered the best treatment for colon cancer. Natural orifice transluminal endoscopic surgery (NOTES) has recently been developed and introduced for certain procedures in humans. However, there are many technical limitations for the use of NOTES in colon resection and anastomosis. Until now, experimental studies of NOTES for colon surgery have only been performed using animals or cadavers[5,6]. Single port laparoscopic surgery (SPLS) has advantages over NOTES in ease of instrument use and operative technique. This is the first report on SPLS performed for a right hemicolectomy in advanced colon cancer with D3 lymph node dissection.
CASE REPORT
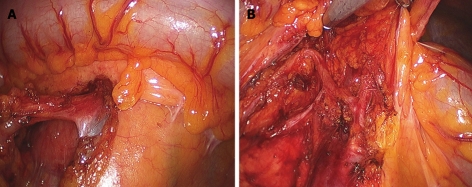
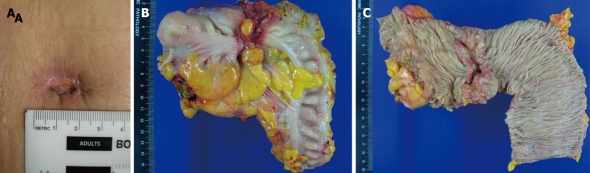
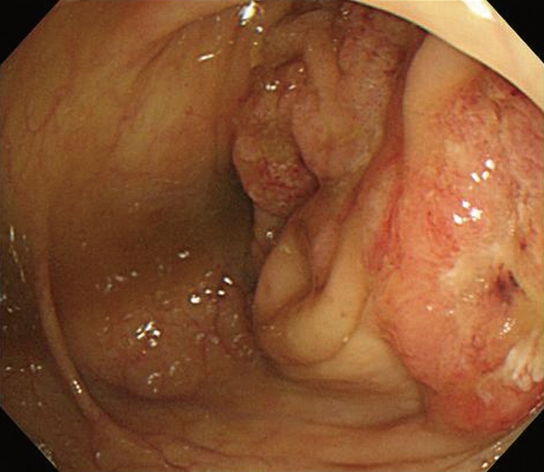
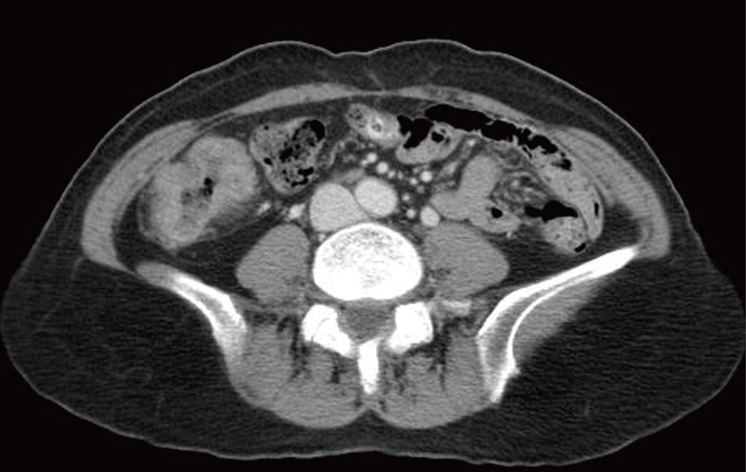
Our patient was a 60-year-old woman who was diagnosed with ascending colon cancer. Colonoscopy revealed an encircling mass in the ascending colon and biopsy demonstrated adenocarcinoma (Figure 1). An abdominopelvic computed tomography scan showed enhanced wall thickening in the ascending colon and no distant metastasis (Figure 2). The patient’s body mass index was 25. The patient’s consent about single port surgery was obtained. A 3 cm abdominal incision was made via the umbilicus using the method reported by Casciola et al[7]. A small wound retractor (ALEXIS wound retractor S, Applied Medical, Santa Margarita, CA, USA) and a surgical glove were used as a single port, as in previous reports[8,9] (Figure 3). The surgical technique was similar to laparoscopic right hemicolectomy and involved a medial to lateral approach using a 0 degree 10 mm scope. We used a hook type monopolar suction irrigator and 5 mm standard straight laparoscopic instrument for dissection of lymph nodes and vessels. We successfully removed all lymph nodes and connective tissue around the ileocolic vessels and midcolic vessels. The vessels were divided using Ligasure V (Covidien, Valleylab, Norwalk, CT, USA). All of the soft tissue anterior to the superior mesenteric vein was completely removed and D3 lymph node dissection was achieved (Figure 4A and B). The specimen was put into a plastic bag within the abdominal cavity and was retrieved through the umbilical port without wound extension. Extracorporeal anastomosis was performed using staplers. The total operative time was 180 min with minimal blood loss (< 50 mL). The patient’s total hospital stay was 4 d and she was discharged without complications (Figure 5A). The surgical specimen was 27.5 cm in length with 10 cm surgical margins and the tumor size was 5 cm × 3 cm (Figure 5B and C). There were 69 harvested lymph nodes and there were no positive lymph nodes. The pathologic staging of the tumor was T3N0M0.
Figure 1.
Encircling mass in the ascending colon visualized during colonoscopy.
Figure 2.
Abdominal CT showed enhanced wall thickening in the ascending colon.
Figure 3.

Operative photograph of the single port setting with multiple trocars and instruments.
Figure 4.
Single port laparoscopic right hemicolectomy with D3 node dissection around the superior mesenteric vein (A) and artery (B).
Figure 5.
Surgical wound around the umbilicus (A) and surgical specimen of the resected colon (B and C).
DISCUSSION
Laparoscopic surgery for advanced colon cancer provides increased patient satisfaction with improvements in postoperative pain, cosmetic results, and recovery[1-4]. However, laparoscopic surgery typically requires 5-6 trocars with 5-12 mm-sized incisions for each trocar, with associated risks for trocar site bleeding, herniation of the viscera, wound infection, wound pain and unwanted cosmetic outcomes[10,11]. Single port surgery has been reported in nephrectomy, appendectomy, cholecystectomy, adnexal mass resection, and sacrocolpopexy[12-15]. Like laparoscopic surgery, SPLS was developed and, gradually, more complex and difficult procedures have been performed. Bucher et al[16]reported a successful single port access right hemicolectomy operation for a 5 cm sized polyp in the ascending colon. They respected oncologic principles for cancer surgery. The surgical specimen length was 38 cm with a 10 cm surgical margin and 33 lymph nodes were retrieved. Leroy et al[17] performed a sigmoidectomy using a single port access for a patient with diverticular disease in the sigmoid colon. In this procedure, the surgeons used a specific single port (ASC Triport, Advanced Surgical Concepts, Wicklow, Ireland), magnets and endoscopy for bowel traction. This Triport allows the passage of 1 large-caliber instrument (up to 12 mm) and 2 other instruments of smaller diameter (up to 5 mm each). The surgical specimen was 40 cm long and anastomosis was located 10 cm from the anal margin. Although these reports demonstrated the technical feasibility and safety of single port surgery, it remains a complex and intricate procedure. Single port surgery has limitations with regard to movement range, adequate traction and triangulation for dissection.
We performed single port surgery in an advanced colon cancer patient. Before the single port laparoscopic right hemicolectomy (SPLRH) procedure, we had experience with SPLS in 10 cases of appendectomy and 1 case of colectomy for colon polyps. In those patients, we used a simple single port that was made using a conventional small wound retractor and a surgical glove. We used conventional straight laparoscopic instruments. Surprisingly, SPLRH with conventional instruments was not a difficult procedure. We were able to achieve operating space with adequate forward and backward movements of the scope and instruments. Of note, balanced scope movement according to movement of the laparoscopic instruments is important. Difficulties with scissoring and interference between instruments will probably be overcome with new instruments and scopes in the near future. Limitations which make SPLS difficult to apply across cases include internal and external conflicts between instruments and difficulty achieving traction for triangulation formation. We offer the following technical tips to avoid these limitations. Low tension under the tissue to be dissected is overcome by using cut mode in electrosurgery instead of coagulation mode. To avoid internal conflict between two working laparoscopic instruments, we first established a surgical field to grasp tissue which is not located too close to the area to dissect. To avoid internal conflict between the scope and dissecting instruments, we recommend drawing the scope to the level of the abdominal wound or out of the wound, if it is possible once the right surgical plane could be found in the close view. External conflicts can be categorized into interference between trocars and interference between instruments. Use of a surgical glove is helpful to overcome these conflicts because it is flexible enough to minimize the trocar conflict. Therefore, surgeons can easily avoid trocar conflict by pushing the trocar forward slightly. SPLS for colon cancer is a challenging procedure and it is essential to develop multiport single access and instruments for single port surgery[18]. Recently many commercial ports have been developed. New port systems include the R-Port (ASC, Wicklow, Ireland)[18], the ASC Triport[17] and the Pnavel Uni-XTM Single Site Laparoscopic System[19] (Pnavel System, Morganville, NJ, USA). New instruments have also been developed specifically to reach curved or articulating structures[20]. Camera systems have also been improved. Cadeddu et al[21] used a magnetically anchored camera system during appendectomy and nephrectomy. The system showed fewer instrument collisions and improved surgical space[21].
Given the evolution of single port surgery, we assume that laparoscopic surgeons will perform more technically difficult procedures including advanced cancer surgery with a single port. This is the first report of single port surgery for colon cancer. We believe that SPLS for colon cancer is an effective, minimally invasive procedure and a bridge to NOTES for colon resection.
Footnotes
Peer reviewer: Seon Hahn Kim, MD, Department of Surgery, Korea University Anam Hospital, #126-1, 5-ga, Anam-dong, Sungbook-gu, Seoul 136-705, South Korea
S- Editor Wang YR L- Editor O'Neill M E- Editor Tian L
References
- 1.Lacy AM, García-Valdecasas JC, Piqué JM, Delgado S, Campo E, Bordas JM, Taurá P, Grande L, Fuster J, Pacheco JL. Short-term outcome analysis of a randomized study comparing laparoscopic vs open colectomy for colon cancer. Surg Endosc. 1995;9:1101–1105. doi: 10.1007/BF00188996. [DOI] [PubMed] [Google Scholar]
- 2.Braga M, Vignali A, Gianotti L, Zuliani W, Radaelli G, Gruarin P, Dellabona P, Di Carlo V. Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg. 2002;236:759–766; disscussion 767. doi: 10.1097/01.SLA.0000036269.60340.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25:3061–3068. doi: 10.1200/JCO.2006.09.7758. [DOI] [PubMed] [Google Scholar]
- 4.Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Nelson H. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655–62; discussion 662-664. doi: 10.1097/SLA.0b013e318155a762. [DOI] [PubMed] [Google Scholar]
- 5.Whiteford MH, Denk PM, Swanström LL. Feasibility of radical sigmoid colectomy performed as natural orifice translumenal endoscopic surgery (NOTES) using transanal endoscopic microsurgery. Surg Endosc. 2007;21:1870–1874. doi: 10.1007/s00464-007-9552-x. [DOI] [PubMed] [Google Scholar]
- 6.Sylla P, Willingham FF, Sohn DK, Gee D, Brugge WR, Rattner DW. NOTES rectosigmoid resection using transanal endoscopic microsurgery (TEM) with transgastric endoscopic assistance: a pilot study in swine. J Gastrointest Surg. 2008;12:1717–1723. doi: 10.1007/s11605-008-0637-1. [DOI] [PubMed] [Google Scholar]
- 7.Casciola L, Codacci-Pisanelli M, Ceccarelli G, Bartoli A, Di Zitti L, Patriti A. A modified umbilical incision for specimen extraction after laparoscopic abdominal surgery. Surg Endosc. 2008;22:784–786. doi: 10.1007/s00464-007-9584-2. [DOI] [PubMed] [Google Scholar]
- 8.Hong TH, Kim HL, Lee YS, Kim JJ, Lee KH, You YK, Oh SJ, Park SM. Transumbilical single-port laparoscopic appendectomy (TUSPLA): scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2009;19:75–78. doi: 10.1089/lap.2008.0338. [DOI] [PubMed] [Google Scholar]
- 9.Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy : scarless cholecystectomy. Surg Endosc. 2009;23:1393–1397. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 10.Wang PH, Yen MS, Yuan CC, Liang SC, Lin JY. Incarcerated hernia in a 5-mm cannula wound. J Am Assoc Gynecol Laparosc. 2001;8:449–452. doi: 10.1016/s1074-3804(05)60349-0. [DOI] [PubMed] [Google Scholar]
- 11.Leggett PL, Churchman-Winn R, Miller G. Minimizing ports to improve laparoscopic cholecystectomy. Surg Endosc. 2000;14:32–36. doi: 10.1007/s004649900006. [DOI] [PubMed] [Google Scholar]
- 12.Kaouk JH, Haber GP, Goel RK, Desai MM, Aron M, Rackley RR, Moore C, Gill IS. Single-port laparoscopic surgery in urology: initial experience. Urology. 2008;71:3–6. doi: 10.1016/j.urology.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 13.Ateş O, Hakgüder G, Olguner M, Akgür FM. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg. 2007;42:1071–1074. doi: 10.1016/j.jpedsurg.2007.01.065. [DOI] [PubMed] [Google Scholar]
- 14.Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999;9:361–364. doi: 10.1089/lap.1999.9.361. [DOI] [PubMed] [Google Scholar]
- 15.Lim MC, Kim TJ, Kang S, Bae DS, Park SY, Seo SS. Embryonic natural orifice transumbilical endoscopic surgery (E-NOTES) for adnexal tumors. Surg Endosc. 2009:Epub ahead of print. doi: 10.1007/s00464-009-0408-4. [DOI] [PubMed] [Google Scholar]
- 16.Bucher P, Pugin F, Morel P. Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis. 2008;23:1013–1016. doi: 10.1007/s00384-008-0519-8. [DOI] [PubMed] [Google Scholar]
- 17.Leroy J, Cahill RA, Asakuma M, Dallemagne B, Marescaux J. Single-access laparoscopic sigmoidectomy as definitive surgical management of prior diverticulitis in a human patient. Arch Surg. 2009;144:173–179; discussion 179. doi: 10.1001/archsurg.2008.562. [DOI] [PubMed] [Google Scholar]
- 18.Rané A, Rao P, Rao P. Single-port-access nephrectomy and other laparoscopic urologic procedures using a novel laparoscopic port (R-port) Urology. 2008;72:260–263; discussion 263-264. doi: 10.1016/j.urology.2008.01.078. [DOI] [PubMed] [Google Scholar]
- 19.Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Colorectal Dis. 2008;10:823–826. doi: 10.1111/j.1463-1318.2008.01660.x. [DOI] [PubMed] [Google Scholar]
- 20.Horgan S, Mintz Y, Jacobsen GR, Sandler BJ, Cullen JP, Spivack A, Easter DW, Chock A, Savu MK, Ramamoorthy S, et al. Video. NOTES: transvaginal cholecystectomy with assisting articulating instruments. Surg Endosc. 2009;23:1900. doi: 10.1007/s00464-009-0471-x. [DOI] [PubMed] [Google Scholar]
- 21.Cadeddu J, Fernandez R, Desai M, Bergs R, Tracy C, Tang SJ, Rao P, Desai M, Scott D. Novel magnetically guided intra-abdominal camera to facilitate laparoendoscopic single-site surgery: initial human experience. Surg Endosc. 2009;23:1894–1899. doi: 10.1007/s00464-009-0459-6. [DOI] [PubMed] [Google Scholar]