Abstract
Background
Trichotillomania (repetitive hair-pulling) is an Axis I psychiatric disorder whose neurobiological basis is incompletely understood. Whole-brain trichotillomania neuroimaging studies are lacking.
Aims
To investigate grey and white matter abnormalities over the whole brain in patients with trichotillomania.
Method
Eighteen patients with DSM–IV trichotillomania and 19 healthy controls undertook structural magnetic resonance imaging after providing written informed consent. Differences in grey and white matter were investigated using computational morphometry.
Results
Patients with trichotillomania showed increased grey matter densities in the left striatum, left amygdalo-hippocampal formation, and multiple (including cingulate, supplementary motor, and frontal) cortical regions bilaterally.
Conclusions
Trichotillomania was associated with structural grey matter changes in neural circuitry implicated in habit learning, cognition and affect regulation. These findings inform animal models of the disorder and highlight key regions of interest for future translational research.
Trichotillomania is an impulse control disorder characterised by repetitive hair-pulling that leads to noticeable hair loss and functional impairment (DSM–IV).1 Unfortunately, the majority of sufferers have never been diagnosed and have never received treatment.2 Peak age at onset is 12–13 years, and hair-pulling most commonly affects the scalp and eyelashes/eyebrows.2 There have been no population-wide epidemiological studies of the condition. Based on a survey conducted in 2500 college students, lifetime prevalence has been estimated to be 0.6–2.5%.3 Trichotillomania has phenomenological overlap with obsessive–compulsive disorder and Tourette syndrome, and consequently represents a candidate member of the obsessive–compulsive spectrum.4 Neurobiological models of these other conditions posit dysregulation of neural circuitry involved in habit formation and top-down inhibitory control, based on tiers of evidence from neuroimaging and elsewhere.5,6 There have been no brain-wide structural studies of trichotillomania, which hampers our understanding of its neurobiological profile and overlap with other obsessive–compulsive disorders.5
In comparison with other related conditions where compulsivity is also a prominent component, trichotillomania offers advantages in terms of neuroscientific investigation. Studies of obsessive–compulsive disorder and Tourette syndrome have often been confounded by current medications. The lack of established treatment guidelines for trichotillomania, and lack of public/clinician awareness, facilitates recruitment of patients who are not medicated to avoid this confound. It is difficult to model intrusive obsessional thoughts or complex vocal tics in animals. By contrast, hair-pulling is a relatively specific behaviour that occurs across species and several promising animal models exist. Mice with disruption of the HoxB8 gene, which is involved in neuronal development, exhibit pathological grooming behaviour.7 The Hoxb8 gene is expressed in multiple brain regions, including the striatum and cingulate cortex. Mice with genetic deletion of a postsynaptic scaffolding protein expressed in the striatum (SAP90/PSD95-associated protein) exhibit compulsive grooming behaviour leading to hair-loss and skin lesions.8
Although these translational models implicate developmental abnormalities of the striatum and cortex in pathological hair-pulling, and neurobiological overlap between trichotillomania and obsessive–compulsive disorder has been suggested, there have been no whole-brain studies of the disorder with which to validate these approaches. Extant trichotillomania neuroimaging studies have all used region-of-interest approaches, rather than exploring distributed abnormalities over the whole brain. Therefore, critically implicated regions may have been overlooked. This is particularly relevant when considering obsessive–compulsive-spectrum disorders, which are theoretically underpinned by abnormalities in large-scale brain systems, i.e. neurocognitive circuits, rather than lesions within a discrete region.9,10
O’Sullivan et al11 reported reduced left putamen volumes in a sample of 10 patients with trichotillomania v. 10 healthy controls. However, these results were described by the authors as preliminary owing to the relatively small sample size and lack of correction for multiple comparisons. Stein et al found no evidence for caudate volume abnormalities in 7 patients with trichotillomania compared with 12 controls using magnetic resonance imaging (MRI) (putamen volumes were not assessed).12 Keuthen et al reported reduced cerebellar volumes in a sample of 14 patients with trichotillomania v. 12 controls, using MRI parcellation techniques.13 Grachev investigated MRI abnormalities in 10 patients with trichotillomania v. 10 controls.14 No significant abnormalities were detected in the initial analysis, although a broader analysis of 48 parcellated regions (without correction for multiple comparisons) identified reduced left inferior frontal gyrus volumes and increased right cuneal cortex volumes. Thus, there exists inconsistent evidence for structural abnormalities of the striatum, frontal regions and cerebellum in trichotillomania.
The aim of the present study was to objectively investigate grey and white matter abnormalities over the whole brain in unmedicated patients with trichotillomania. We accomplished this by using cluster-based permutation analysis, which enabled automated, sensitive and unbiased analysis with correction for multiple comparisons.15,16 In light of the above discussion, it was predicted that trichotillomania would be associated with structural abnormalities of large-scale brain networks, including the striatum and cortex.
Method
Participants
Patients with trichotillomania were recruited via support websites, and controls were recruited via newspaper advertisements in the UK. Prior to enrolment, all participants undertook an extended clinical interview conducted by a member of the study team using the Mini International Neuropsychiatric Inventory (MINI), a well-validated screening instrument for DSM–IV Axis I disorders.17 Twenty people with trichotillomania and 19 healthy volunteers were enrolled after providing written informed consent and meeting eligibility criteria. For trichotillomania, inclusion criteria were fulfillment of DSM–IV diagnostic criteria (as ratified by a consultant psychiatrist), no treatment for >6 months, and no prior history of neurological conditions such as tic-spectrum disorders and epilepsy. Further, we excluded patients with current depression (defined as meeting MINI criteria and/or having a Montgomery–Åsberg Depression Scale (MADRS) total score >10)17,18 and current obsessive–compulsive disorder (defined as meeting MINI criteria and/or having a Yale–Brown Obsessive Compulsive Scale total score >10).17,19 We measured IQ using the National Adult Reading Test (NART).20 Trichotillomania disease severity was assessed using the Massachusetts General Hospital (MGH) Hair pulling Scale.21 Controls were included on the basis of no history of neurological or Axis I disorders. All volunteers were deemed safe for MRI by completion of a screening questionnaire and the study was approved by a local research ethics committee.
Neuroimaging
Structural MRI scans were acquired from all participants using a 1.5 T GE Signa system (General Electric, Milwaukee, USA) at the Department of Radiology, Addenbrooke’s Hospital, Cambridge, UK. Axial three-dimensional (3-D) T1-weighted images were obtained using a spoiled gradient recall sequence with the parameters: 124 slices of thickness 2 mm, repetition time (TR)=33 ms, echo time (TE)=3 ms, flip angle 40°, matrix size 256 × 256 and in-plane voxel dimensions 0.94 mm2. Axial dual-echo fast spin echo images were also acquired with the parameters: 40 slices of thickness 4 mm, TR=5625 ms, TE=20 ms (proton density-weighted) and 102 ms (T2-weighted) with 8-echo train length, matrix size 256 × 256 and in-plane voxel dimensions 0.94 mm2. Structural scans were visually inspected by a consultant radiologist independent of the research team for clinically significant abnormalities.
Images were preprocessed with tools from the FSL software package (www.fmrib.ox.ac.uk/fsl/). Non-brain tissues were first removed using an automated brain extraction procedure (Brain Extraction Tool).22 The resulting voxels were segmented using an automated tissue classification algorithm into probabilistic maps of grey matter, white matter, cerebrospinal fluid and ‘other’ using tissue-type segmentation and bias field correction (FSL Automated Segmentation Tool).23 For each voxel, the partial volume coefficient was calculated, which represented the probability of that voxel belonging to each of the four tissue classes. The resulting segmented grey and white partial volume maps were then registered into standard space (Montreal Neurological Institute, MNI) using affine intermodal image registration (FSL Linear Image Registration Tool).24,25 Prior to statistical inference, all segmented maps were smoothed via the Fourier domain, by a two-dimensional (2-D) Gaussian kernel with a standard deviation of 1.88 mm (2 voxels).
Statistical analyses
Between-group measurement of grey and white matter differences were performed using permutation tests implemented in Cambridge Brain Analysis (CAMBA) software in Linux (version 1.3.2; www-bmu.psychiatry.cam.ac.uk/software). An analysis of covariance (ANCOVA) model was fitted at each intracerebral voxel in standard space, with global grey matter density, age and MADRS scores as covariates. We tested the null hypothesis of no differences in brain structure between the two groups by permutation at the level of spatially contiguous 3-D voxel clusters, as described in detail elsewhere.15,26 This non-parametric method of analysis incorporates spatial information and is generally more powerful than other tests, such as those informed only by data at the single voxel level.26 For between-group comparisons, we used probability thresholds for cluster testing so that the average number of false-positive clusters expected per map was less than one (equivalent P50.004), with the voxel threshold set to P50.05. Clusters showing significant between-group differences were then described in terms of their peak coordinates, and the automated anatomical labelling template image regions contained therein.27 An additional permutation analysis was conducted to explore relationships between grey/white matter densities and symptom scores in patients, again such that the expected number of false-positive clusters per map was less than one, and the voxel threshold was set to P50.05. Correlational analysis was performed in patients between mean grey/white densities in those clusters showing group differences and symptom scores in patients (Pearson’s r).
Results
Routine clinical screening of MRI scans identified significant structural abnormalities in two patients, whose data were excluded from the subsequent analysis. One patient’s scans showed a basal ganglia signal hyperintensity; this was deemed of uncertain clinical significance and the patient was asked to monitor for worsening of symptoms or onset of new symptoms. The other patient’s scans showed evidence of a brainstem event, leading to urgent clinic follow-up. Thus, the final sample size was 18 patients and 19 controls. As can be seen in Table 1, the two study groups did not differ significantly in terms of age, NART IQ, male:female ratio, and handedness. Total MADRS scores for both groups were well below threshold for clinically significant depression; as anticipated, patients showed significantly higher scores than healthy controls. The mean total MGH score at the time of study participation for the patients was 15.11 (s.d.=4.54), consistent with mild to moderate disease severity. One patient met DSM criteria for current panic disorder and agoraphobia; the others were free from current Axis I comorbidities according to MINI screen. The mean age of symptom onset reported by patients was 11.89 years (s.d.=6.85).
Table 1.
Demographic and clinical characteristics of controls and patients with trichotillomania
| Variable | Trichotillomania (n=18) | Controls (n=19) | F (d.f.=1,36) | P |
|---|---|---|---|---|
| Age, years: mean (s.d.) | 37.39 (11.65) | 33.05 (9.09) | 1.61 | 0.21 |
| NART IQ score, mean (s.d.) | 115.52 (7.11) | 111.73 (9.20) | 1.95 | 0.17 |
| Males:females | 1:17 | 3:16 | 1.00 | 0.32a |
| Left:right handedness | 3:15 | 2:17 | 0.30 | 0.59a |
| MADRS score, mean (s.d.) | 3.17 (4.71) | 0.21 (0.63) | 7.37 | 0.01* |
| MGH total score, mean (s.d.) | 15.11 (4.54) | |||
| Age at onset, years: mean (s.d.) | 11.89 (6.85) |
MADRS, Montgomery—Åsberg Depression Scale; MGH, Massachusetts General Hospital Hair pulling Scale; NART, National Adult Reading Test.
a. Chi-squared test.
*P <0.05; significant difference between groups.
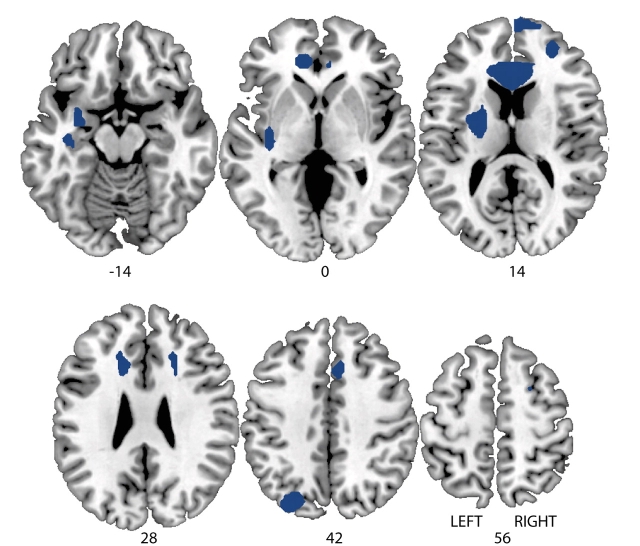
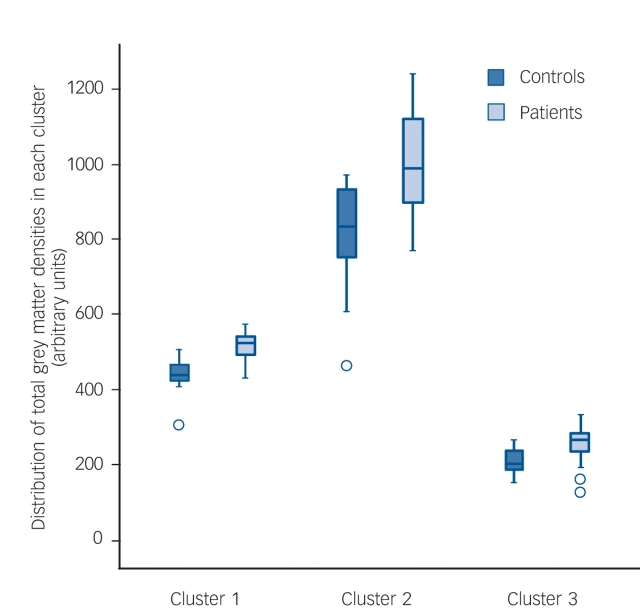
The patients did not differ significantly from controls in terms of global grey matter density (trichotillomania 9.26 arbitrary units (s.d.=0.47) v. controls 9.14 (s.d.=0.66); P=0.51). In comparison with the healthy volunteers, patients with trichotillomania showed grey matter density excesses in three clusters (see Fig. 1 and Table 2 for anatomical details and peak MNI coordinates). These comprised: (a) a mean density increase of 18% in the striatum (left putamen) and limbic system (left amygdalo-hippocampal complex); (b) a mean density increase of 23% in bilateral frontal regions (cingulate, supplemental motor, and superior cortices); and (c) a mean density increase of 21% in left occipital and parietal regions (Fig. 2). These results were not dependent on entering age as a covariate, since when the analysis was rerun without age as a covariate, the core results were still evident (i.e. increased grey matter in the left amygdalo-hippocampal formation, bilateral cingulate, and right middle/superior frontal cortices). There were no significant regions of relative grey matter reductions or changes in white matter (increases or decreases) in the patients. No clusters were found in which density covaried significantly with symptom severity in the patients. No significant correlations were found between mean grey matter densities and patient disease severity scores, in those clusters identified in the between-group analysis (P40.10).
Fig. 1.
Map of grey matter volume excesses (red) in patients with trichotillomania compared with controls in (Montreal Neurological Institute (MNI) space, superimposed onto a standard template. Representative slices with z-coordinates indicated. Expected number of false positive cluster tests <1 over the whole map (equivalent P<0.004).
Table 2.
Regions of increased grey matter in patients with trichotillomania (n=18) compared with controls (n=19)
| Automated anatomical labelling regions within each cluster | MNI coordinates of peak (x,y,z) | Voxels |
|---|---|---|
| Left hippocampus, left amygdala, left putamen | -22, -10, 14 | 912 |
| Bilateral anterior/middle cingulate, bilateral supplemental motor area, bilateral frontal superior cortex, bilateral frontal superior medial cortex | -4, 34, 10 | 2464 |
| Left superior occipital cortex, left middle occipital cortex, left superior parietal cortex, left inferior parietal cortex | -24, -74, 44 | 414 |
MNI, Montreal Neurological Institute.
Fig. 2.
Grey matter densities in healthy controls and patients with trichotillomania for each of the three clusters identified in the permutation analysis.
Cluster 1, left hippocampus, left amygdala, left putamen; Cluster 2, bilateral anterior/middle cingulate, bilateral supplemental motor area, bilateral fronto-superior cortices; Cluster 3, left superior/middle occupital cortex, left superior/inferior parietal cortex.
Discussion
The key finding of this study was that unmedicated patients with trichotillomania exhibited abnormally increased grey matter densities compared with matched healthy controls in the left amygdalo-hippocampal complex, left striatum and multiple cortical regions. These distributed structural abnormalities occurred in the absence of medication confounds and appeared to be unrelated to disease severity.
Increased grey matter has also been reported in studies of focal dystonia, Tourette syndrome and obsessive–compulsive disorder28–31 albeit not consistently.5 These novel findings support the notion that trichotillomania shares some neurobiological overlap with other putative obsessive–compulsive-spectrum disorders, with implications for upcoming diagnostic revisions. Peak onset of trichotillomania is at 12–13 years of age. Adolescence is a critical time for neurodevelopment and multiple studies have reported intense reductions of grey matter tissue in the pubescent period.32–35 These grey matter excesses detected in patients with trichotillomania could reflect deviation from normal developmental trajectories. Alternatively, they may reflect neuro-plastic changes occurring through use of brain regions involved in grooming and habit learning, there being some evidence that increases in grey matter can occur through motor-skill training.36
The striatum is thought to play a critical role in habit learning and in the chunking of automated action sequences, according to tiers of evidence from animals and humans.37 Striatal damage in rats has been shown to disrupt the ability to perform choreographed grooming sequences.38 In humans, clinical data suggest that the striatum is responsible for the gradual incremental learning of associations typical of habit learning.39 Striatal involvement in trichotillomania is reminiscent of obsessive–compulsive disorder, and supports a similar conceptualisation emphasising the role of the basal ganglia in the development of pathological habits.5,40
Cortical regions such as the cingulate and prefrontal lobes are involved in multiple high-level cognitive processes.41 The structural abnormalities detected in these regions in trichotillomania could mediate cognitive problems previously identified in patients, which likely impede quality of life. In neuropsychological studies, patients with trichotillomania showed deficits on tests of divided attention,42 response inhibition and working memory.43,44 The relationship between grey matter excesses and cognitive deficits in patients with trichotillomania merits follow-up, since these neural regions and their dependent cognitive functions represent targets for novel cognitive enhancers.45
The finding of amygdalo-hippocampal abnormalities was not predicted a priori. The amygdalo-hippocampal formation constitutes part of the limbic system, which regulates arousal and emotional learning processes.46 Several studies support a causal relationship between increased or decreased arousal and hair-pulling episodes, and between negative affect and hair-pulling episodes.47–49 Furthermore, trichotillomania has been associated with childhood trauma and post-traumatic stress disorder. In one survey, the majority of patients reported physical abuse and/or emotional neglect as a trigger in childhood.50
Positive features of this study include the use of permutation cluster analysis to maximise power while facilitating corrected whole-brain analysis, and the inclusion of patients who were untreated for at least 6 months prior to scanning. None the less, several caveats must be considered. Details of past treatments (beyond 6 months) received by patients were not available, to explore whether past treatment-seekers differed from non-treatment-seekers. It remains to be seen whether the present findings generalise to other groups of patients with trichotillomania who differ in terms of their clinical characteristics (past treatments, disease severity, comorbidities). Another potential limitation is that patients showed significantly higher MADRS (dysphoric mood) scores than controls, despite being free from DSM–IV depression. However, we controlled for this by entering MADRS scores as a covariate into the imaging analysis. Finally, voxel-based morphometry techniques carry potential limitations such as confounds due to choice of smoothing kernel size and potential misalignment of brain structures during normalisation. On the other hand, such techniques enable objective and sensitive analysis, with stringent correction for false positives over the whole brain.15,16
This study, using a cluster-level technique to investigate trichotillomania, provides an objective whole-brain-based analysis that directs researchers to areas that are abnormal in this disorder, namely cortical regions, the amygdalo-hippocampal formation and the striatum. These results suggest overlap with other putative obsessive–compulsive-spectrum disorders in terms of neurobiology.6,40 The functional significance of these grey matter abnormalities requires clarification in follow-up longitudinal studies, and in studies of unaffected first-degree relatives (asymptomatic individuals at increased genetic risk). The further application of translational neuroscientific techniques to the study of trichotillomania will extend these findings and provide new insights into its neurobiology, with implications for diagnosis and treatment of trichotillomania and related obsessive–compulsive-spectrum disorders.
Acknowledgments
The Behavioural and Clinical Neuroscience Institute is supported by a joint award from the Medical Research Council and Wellcome Trust. This research was supported by a grant from the Wellcome Trust (076274/Z/04/Z awarded to T.W.R. and B.J.S.). Software development was supported by a Human Brain Project grant from the National Institute of Biomedical Imaging & Bioengineering and the National Institute of Mental Health, USA. S.R.C was supported by a priority studentship from the Medical Research Council. L.A.M. was supported by the Harnett Fund, University of Cambridge. The authors wish to thank the study participants and radiographers at the Magnetic Resonance Imaging Service, Addenbrooke’s Hospital, Cambridge, UK.
Declaration of interest
None. Funding detailed in Acknowledgements.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th edn, text revised) (DSM–IV–TR). APA, 2000.
- 2.Cohen LJ, Stein DJ, Simeon D, Spadaccini E, Rosen J, Aronowitz B, Hollander E. Clinical profile, comorbidity, and treatment history in 123 hair pullers: a survey study. J Clin Psychiatry 1995; 56: 319–26. [PubMed] [Google Scholar]
- 3.Christenson GA, Pyle RL, Mitchell JE. Estimated lifetime prevalence of trichotillomania in college students. J Clin Psychiatry 1991; 52: 415–7. [PubMed] [Google Scholar]
- 4.Stein DJ, Simeon D, Cohen LJ, Hollander E. Trichotillomania and obsessive-compulsive disorder. J Clin Psychiatry 1995; 56 (suppl 4): 28–34. [DOI] [PubMed] [Google Scholar]
- 5.Chamberlain SR, Menzies L, Sahakian BJ, Fineberg NA. Lifting the veil on trichotillomania. Am J Psychiatry 2007; 164: 568–74. [DOI] [PubMed] [Google Scholar]
- 6.Singer HS, Minzer K. Neurobiology of Tourette’s syndrome: concepts of neuroanatomic localization and neurochemical abnormalities. Brain Dev 2003; 25 (suppl 1): s70–84. [DOI] [PubMed] [Google Scholar]
- 7.Greer JM, Capecchi MR. Hoxb8 is required for normal grooming behavior in mice. Neuron 2002; 33: 23–34. [DOI] [PubMed] [Google Scholar]
- 8.Welch JM, Lu J, Rodriguiz RM, Trotta NC, Peca J, Ding JD, Feliciano C, Chen M, Adams JP, Luo J, Dudek SM, Weinberg RJ, Calakos N, Wetsel WC, Feng G. Cortico-striatal synaptic defects and OCD-like behaviours in Sapap3-mutant mice. Nature 2007; 448: 894–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev 2008; 32: 525–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Menzies L, Achard S, Chamberlain SR, Fineberg N, Chen CH, del Campo N, Sahakian BJ, Robbins TW, Bullmore E. Neurocognitive endophenotypes of obsessive-compulsive disorder. Brain 2007; 130: 3223–36. [DOI] [PubMed] [Google Scholar]
- 11.O’Sullivan RL, Rauch SL, Breiter HC, Grachev ID, Baer L, Kennedy DN, Keuthen NJ, Savage CR, Manzo PA, Caviness VS, Jenike MA. Reduced basal ganglia volumes in trichotillomania measured via morphometric magnetic resonance imaging. Biol Psychiatry 1997; 42: 39–45. [DOI] [PubMed] [Google Scholar]
- 12.Stein DJ, Coetzer R, Lee M, Davids B, Bouwer C. Magnetic resonance brain imaging in women with obsessive-compulsive disorder and trichotillomania. Psychiatry Res 1997; 74: 177–82. [DOI] [PubMed] [Google Scholar]
- 13.Keuthen NJ, Makris N, Schlerf JE, Martis B, Savage CR, McMullin K, Seidman LJ, Schmahmann JD, Kennedy DN, Hodge SM, Rauch SL. Evidence for reduced cerebellar volumes in trichotillomania. Biol Psychiatry 2007; 61: 374–81. [DOI] [PubMed] [Google Scholar]
- 14.Grachev ID. MRI-based morphometric topographic parcellation of human neocortex in trichotillomania. Psychiatry Clin Neurosci 1997; 51: 315–21. [DOI] [PubMed] [Google Scholar]
- 15.Bullmore ET, Suckling J, Overmeyer S, Rabe-Hesketh S, Taylor E, Brammer MJ. Global, voxel, and cluster tests, by theory and permutation, for a difference between two groups of structural MR images of the brain. IEEE Trans Med Imaging 1999; 18: 32–42. [DOI] [PubMed] [Google Scholar]
- 16.Suckling J, Bullmore E. Permutation tests for factorially designed neuroimaging experiments. Hum Brain Mapp 2004; 22: 193–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM–IV and ICD–10. J Clin Psychiatry 1998; 59 (suppl 20): 22–33. [PubMed] [Google Scholar]
- 18.Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134: 382–9. [DOI] [PubMed] [Google Scholar]
- 19.Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS. The Yale–Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 1989; 46: 1006–11. [DOI] [PubMed] [Google Scholar]
- 20.Nelson HE. National Adult Reading Test (NART): Test Manual. nfer-Nelson, 1982.
- 21.Keuthen NJ, O’Sullivan RL, Ricciardi JN, Shera D, Savage CR, Borgmann AS, Jenike MA, Baer L. The Massachusetts General Hospital (MGH) Hairpulling Scale: 1. development and factor analyses. Psychother Psychosom 1995; 64: 141–5. [DOI] [PubMed] [Google Scholar]
- 22.Smith SM. Fast robust automated brain extraction. Hum Brain Mapp 2002; 17: 143–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Y, Brady M, Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans Med Imaging 2001; 20: 45–57. [DOI] [PubMed] [Google Scholar]
- 24.Jenkinson M, Bannister P, Brady M, Smith S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage 2002; 17: 825–41. [DOI] [PubMed] [Google Scholar]
- 25.Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TE, Johansen-Berg H, Bannister PR, De Luca M, Drobnjak I, Flitney DE, Niazy RK, Saunders J, Vickers J, Zhang Y, De Stefano N, Brady JM, Matthews PM. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage 2004; 23 (suppl 1): s208–19. [DOI] [PubMed] [Google Scholar]
- 26.Pantelis C, Velakoulis D, McGorry PD, Wood SJ, Suckling J, Phillips LJ, Yung AR, Bullmore ET, Brewer W, Soulsby B, Desmond P, McGuire PK. Neuroanatomical abnormalities before and after onset of psychosis: a cross-sectional and longitudinal MRI comparison. Lancet 2003; 361 281–8. [DOI] [PubMed] [Google Scholar]
- 27.Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, Mazoyer B, Joliot M. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage 2002; 15: 273–89. [DOI] [PubMed] [Google Scholar]
- 28.Kim JJ, Lee MC, Kim J, Kim IY, Kim SI, Han MH, Chang KH, Kwon JS. Grey matter abnormalities in obsessive–compulsive disorder. Statistical parametric mapping of segmented magnetic resonance images. Br J Psychiatry 2001; 179: 330–4. [DOI] [PubMed] [Google Scholar]
- 29.Etgen T, Muhlau M, Gaser C, Sander D. Bilateral grey-matter increase in the putamen in primary blepharospasm. J Neurol Neurosurg Psychiatry 2006; 77: 1017–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singer HS, Reiss AL, Brown JE, Aylward EH, Shih B, Chee E, Harris EL, Reader MJ, Chase GA, Bryan RN. Volumetric MRI changes in basal ganglia of children with Tourette’s syndrome. Neurology 1993; 43: 950–6. [DOI] [PubMed] [Google Scholar]
- 31.Garraux G, Goldfine A, Bohlhalter S, Lerner A, Hanakawa T, Hallett M. Increased midbrain gray matter in Tourette’s syndrome. Ann Neurol 2006; 59: 381–5. [DOI] [PubMed] [Google Scholar]
- 32.Pfefferbaum A, Mathalon DH, Sullivan EV, Rawles JM, Zipursky RB, Lim KO. A quantitative magnetic resonance imaging study of changes in brain morphology from infancy to late adulthood. Arch Neurol 1994; 51: 874–87. [DOI] [PubMed] [Google Scholar]
- 33.Steen RG, Ogg RJ, Reddick WE, Kingsley PB. Age-related changes in the pediatric brain: quantitative MR evidence of maturational changes during adolescence. AJNR Am J Neuroradiol 1997; 18: 819–28. [PMC free article] [PubMed] [Google Scholar]
- 34.Giedd JN, Blumenthal J, Jeffries NO, Castellanos FX, Liu H, Zijdenbos A, Paus T, Evans AC, Rapoport JL. Brain development during childhood and adolescence: a longitudinal MRI study. Nat Neurosci 1999; 2: 861–3. [DOI] [PubMed] [Google Scholar]
- 35.Whitford TJ, Rennie CJ, Grieve SM, Clark CR, Gordon E, Williams LM. Brain maturation in adolescence: concurrent changes in neuroanatomy and neurophysiology. Hum Brain Mapp 2007; 28: 228–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Draganski B, Gaser C, Busch V, Schuierer G, Bogdahn U, May A. Neuroplasticity: changes in grey matter induced by training. Nature 2004; 427: 311–2. [DOI] [PubMed] [Google Scholar]
- 37.Graybiel AM. The basal ganglia and chunking of action repertoires. Neurobiol Learn Mem 1998; 70: 119–36. [DOI] [PubMed] [Google Scholar]
- 38.Cromwell HC, Berridge KC. Implementation of action sequences by a neostriatal site: a lesion mapping study of grooming syntax. J Neurosci 1996; 16: 3444–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knowlton BJ, Mangels JA, Squire LR. A neostriatal habit learning system in humans. Science 1996; 273: 1399–402. [DOI] [PubMed] [Google Scholar]
- 40.Graybiel AM, Rauch SL. Toward a neurobiology of obsessive-compulsive disorder. Neuron 2000; 28: 343–7. [DOI] [PubMed] [Google Scholar]
- 41.Robbins TW. From arousal to cognition: the integrative position of the prefrontal cortex. Prog Brain Res 2000; 126: 469–83. [DOI] [PubMed] [Google Scholar]
- 42.Stanley MA, Hannay HJ, Breckenridge JK. The neuropsychology of trichotillomania. J Anxiety Disord 1997; 11: 473–88. [DOI] [PubMed] [Google Scholar]
- 43.Chamberlain SR, Fineberg NA, Blackwell AD, Robbins TW, Sahakian BJ. Motor inhibition and cognitive flexibility in obsessive–compulsive disorder and trichotillomania. Am J Psychiatry 2006; 163: 1282–4. [DOI] [PubMed] [Google Scholar]
- 44.Bohne A, Savage CR, Deckersbach T, Keuthen NJ, Wilhelm S. Motor inhibition in trichotillomania and obsessive-compulsive disorder. J Psychiatr Res 2008; 42: 141–50. [DOI] [PubMed] [Google Scholar]
- 45.Chamberlain SR, Sahakian BJ. The neuropsychiatry of impulsivity. Curr Opin Psychiatry 2007; 20: 255–61. [DOI] [PubMed] [Google Scholar]
- 46.McGaugh JL. The amygdala modulates the consolidation of memories of emotionally arousing experiences. Annu Rev Neurosci 2004; 27: 1–28. [DOI] [PubMed] [Google Scholar]
- 47.Christenson GA, Mackenzie TB, Mitchell JE. Characteristics of 60 adult chronic hair pullers. Am J Psychiatry 1991; 148: 365–70. [DOI] [PubMed] [Google Scholar]
- 48.Christenson GA, Ristvedt SL, Mackenzie TB. Identification of trichotillomania cue profiles. Behav Res Ther 1993; 31: 315–20. [DOI] [PubMed] [Google Scholar]
- 49.du Toit PL, van Kradenburg J, Niehaus DJ, Stein DJ. Characteristics and phenomenology of hair-pulling: an exploration of subtypes. Compr Psychiatry 2001; 42: 247–56. [DOI] [PubMed] [Google Scholar]
- 50.Boughn S, Holdom JJ. The relationship of violence and trichotillomania. J Nurs Scholarsh 2003; 35: 165–70. [DOI] [PubMed] [Google Scholar]