Abstract
Background
An important goal for medical education today is professional development including gender equality and awareness of gender issues. Are medical teachers prepared for this task? We investigated gender awareness among physician teachers, expressed as their attitudes towards the role of gender in professional relationships, and how it varied with physician gender and specialty. We discuss how this might be related to the gender climate and sex segregation in different specialties.
Method
Questionnaires were sent to all 468 specialists in the clinical departments and in family medicine, who were engaged in educating medical students at a Swedish university. They were asked to rate, on visual analogue scales, the importance of physician and patient gender in consultation, of preceptor and student gender in clinical tutoring and of physician gender in other professional encounters. Differences between family physicians, surgical, and non-surgical hospital doctors, and between women and men were estimated by chi-2 tests and multivariate logistic regression analyses.
Results
The response rate was 65 %. There were differences between specialty groups in all investigated areas mainly due to disparities among men. The odds for a male family physician to assess gender important were three times higher, and for a male non-surgical doctor two times higher when compared to a male surgical doctor. Female teachers assessed gender important to a higher degree than men. Among women there were no significant differences between specialty groups.
Conclusions
There was an interaction between physician teachers' gender and specialty as to whether they identified gender as important in professional relationships. Male physicians, especially from the surgical group, assessed gender important to a significantly lower degree than female physicians. Physicians' degree of gender awareness may, as one of many factors, affect working climate and the distribution of women and men in different specialties. Therefore, to improve working climate and reduce segregation we suggest efforts to increase gender awareness among physicians, for example educational programs where continuous reflections about gender attitudes are encouraged.
Background
Medical school is the breeding ground not only for medical knowledge, but also for professional development and careers, including equal opportunities and gender equality. Consequently there are good reasons for gender issues to be considered in medical education.
A growing interest in highlighting women's health issues during the last decades has led to an emerging awareness of the importance of gender in medicine. This awareness has mostly focussed on differences between female and male patients and gendered management of illness and disease. However, there is more to gender than that.
When comparing men and women it is important to clarify the concepts of sex and gender and describe the gender perspective applied. Sex is a biological categorization based on reproductive organs and chromosomes while gender views women and men from a psychosocial and cultural perspective. When studying differences in health, behavior or attitudes it is generally not possible to know what is biological and what is social in origin. A constructivist perspective [1] of gender is then suitable since it underlines that sex and gender, biology and culture are related and inter-reliant. In this perspective gender refers to the constantly ongoing social construction of what is considered "feminine" and "masculine", based on sociocultural norms and power. Gender is not a fixed or 'natural' category, but subject to change and negotiation. We all "do gender" in all kinds of social interactions [2-4].
In professional everyday life, physicians, too, are doing gender. For example when they ask female patients more than male patients about their family situation [5] physicians contribute to maintain the gendered view that family matters are women's issues. Physicians do gender not only in their relation with patients [3], but also with colleagues [4], staff [4,6], and as role models for students. Physicians with an awareness of gender take into consideration power asymmetry and gendered expectations and preconceptions in such interactions. They are aware of the gender order [7], which affects women's health differently than men's health and which permeates into professional as well as private relations. Research has shown that gender insensitivity (lack of gender awareness) has consequences such as gender discrimination and sexual harassment in many domains of physicians' professional role and practice, for example medical education, [8,9] career opportunities, [10] and, not least, choice of specialty [11-13].
Today women constitute more than 30 % of professionally active doctors in many western countries [14] and more than 50% of physicians under 30 years of age are women [15]. In Sweden in 2002, 40 % of all physicians and 63% of those younger than 30, were women [16]. Specialty choices, however, continue to be segregated. Men are largely over-represented in surgical specialties [14,17,18]. In Sweden in 2002 close to 90 % of physicians in general surgery and most surgical sub-specialties were men [16]. Women "cluster" in fewer fields than men [12,18], nowadays especially disciplines that have to do with children's and women's health and with a high degree of patient contact such as family medicine and psychiatry [14]. There were 63 % women in child psychiatry, 53 % in gynecology and 48 % in psychiatry in Sweden in 2002 [16]. A hierarchy of medical specialties has long been described where surgical specialties have highest status [15,19]. The specialties where women concentrate have traditionally been considered less prestigious. A change towards a more equal gender distribution in some specialties is slowly taking place [14,17] but the medical profession is still sex segregated. The percentage of women in surgery and surgical subspecialties in Sweden changed no more than from 11 to 12 % between 1992 and 2002 [16]. During the same time the proportion of women in family medicine increased from 35 to 41 % (the same percentages of women as among the total number of physicians) and from 25 to 30 % in internal medicine.
As family physicians engaged in medical education and in developing good and fair working conditions we have met both interest and distrust when trying to introduce and discuss gender issues in medicine. We wanted to understand more about that. Via a questionnaire we therefore explored one important aspect of gender awareness among teaching physicians, namely their attitudes towards the role of gender in professional relations. We assume that finding gender important in relations should lead to an awareness of gender, which lowers the risk of gender discrimination and sexual harassment. The aims of this paper were:
• to analyze whether, and in that case how, identifying the importance of gender in different medical relationships varies with physician gender and specialty.
• to discuss how this might be related to working climate and the segregation of women and men in various medical specialties.
Method
Study design
Questionnaire
A questionnaire was designed in collaboration with a reference group of medical researchers from different specialties. Sex, specialty, age, academic degree, and years in the profession were independent items asked for. There were five outcome items about the importance of gender consisting of statements (listed in table 3) to agree or to disagree with on a 100 mm visual analogue scale (VAS). The tails of the scale read "I do not agree at all", and "I agree completely". Below each statement and VAS there were open-ended questions asking for examples and explanations. The statements and questions were tested for intelligibility in a group of 10 teaching/tutoring physicians. In this paper the VAS-responses to the five statements and a summary variable (described below) were analyzed. The answers to the open-ended questions have been further analysed and will be reported elsewhere, but a few open-ended comments are used as illustrations in the discussion section of this paper.
Table 3.
Percentage and number (within brackets) of respondents agreeing (scoring >50) to the five gender attitude statements and scoring high (>250) on "importance-of-gender"-scale. P-values from comparison between specialty groups and between men and women. (S = surgical doctors, NS = non-surgical doctors, FP = family physicians.)
| All respondents | Men | Women | ||||||||||||||
| Outcome variable | Total | S | NS | FP | p1 | Total | S | NS | FP | p1 | Total | S | NS | FP | p1 | p2 |
| Statements: | ||||||||||||||||
| 1. The patient's gender is of importance in consultation. | 69 (199) | 55 (47) | 74 (88) | 80 (41) | .002 | 66 (130) | 51 (36) | 71 (58) | 81 (22) | .007 | 76 (69) | 69 (11) | 81 (30) | 79 (19) | .601 | .061 |
| 2. My own gender is of importance in consultation. | 68 (196) | 48 (41) | 75 (88) | 84 (43) | <.001 | 62 (123) | 41 (28) | 69 (57) | 89 (24) | <.001 | 81 (73) | 76 (13) | 86 (31) | 79 (19) | .745 | .002 |
| 3. The gender of the medical student is of importance in clinical tutoring. | 53 (153) | 43 (37) | 55 (65) | 71 (36) | .007 | 47 (92) | 38 (26) | 52 (43) | 59 (16) | .084 | 68 (61) | 65 (11) | 61 (22) | 83 (20) | .175 | .001 |
| 4. My own gender is of importance in clinical tutoring. | 50 (142) | 42 (36) | 52 (60) | 67 (34) | .023 | 42 (80) | 37 (25) | 45 (36) | 52 (14) | .335 | 70 (62) | 65 (11) | 67 (24) | 83 (20) | .295 | <.001 |
| 5. My own gender is of importance in other professional relations, for example with colleagues, medical staff or in research. | 62 (177) | 51 (43) | 64 (76) | 79 (41) | .004 | 54 (107) | 43 (29) | 60 (50) | 71 (20) | .017 | 79 (70) | 82 (14) | 74 (26) | 87 (21) | .458 | <.001 |
| Summary variable: | ||||||||||||||||
| "Importance-of-gender"-scale | 63 (173) | 51 (42) | 67 (76) | 76 (38) | .008 | 56 (106) | 45 (30) | 61 (49) | 69 (18) | .046 | 78 (67) | 75 (12) | 79 (27) | 83 (20) | .873 | .001 |
p1 = p-values from chi-2 tests comparing specialty groups (2-sided, df = 2). p2 = p-values from chi-2 tests comparing men total, and women total (2-sided, df = 1)
Sample
Questionnaires were sent to all 468 specialists in the clinical departments of the university hospital and in family medicine in Umeå, Sweden in 1997. All were involved in teaching medical students and/or tutoring them in their clinical training. The names of the study population were obtained from the university and county council payroll list, which also provided specialty and age. We categorized specialty into three groups: family physicians, surgical (including gynecology and obstetrics), and non-surgical hospital specialties (Table 1). Age was dichotomized at 45.
Table 1.
Specialty categorization.
| SURGICAL SPECIALTIES | NON-SURGICAL SPECIALTIES |
| Anesthesiology and intensive care | Pediatrics |
| General surgery | Dermatology – venereology |
| Pediatric surgery | General internal medicine |
| Hand surgery | Endocrinology |
| Neurological surgery | Cardiology |
| Orthopedics | Infectious diseases |
| Plastic and reconstructive surgery | Respiratory medicine |
| Thoracic surgery | Nephrology |
| Urology | Rheumatology |
| Obstetrics and gynecology | Geriatrics |
| Gynecological oncology | Occupational & environmental medicine |
| Ophthalmology | Clinical physiology |
| Otorhinolaryngology | Transfusion medicine |
| Clinical neurophysiology | |
| Neurology | |
| FAMILY PHYSICIANS | Psychiatry |
| Family physicians in public health | Child & adolescent psychiatry |
| care | Community and social medicine |
| Diagnostic radiology | |
| Oncology | |
| Rehabilitation medicine | |
| Clinical genetics |
Procedure
Questionnaires, covering letters ensuring confidentiality, and numbered and pre-stamped envelopes for the answers were distributed by post. When response had been registered in the original name list the envelope was destroyed and the questionnaire was given a new number. Thus no response can be identified with a person. The non-respondents received one follow-up letter.
The Umeå Clinical Research Ethics Committee approved the study.
Analysis
The marks on the VAS were translated into scores between 0 and 100, the higher the figure, the more the respondent agreed. A summary variable was created by adding the figures from each of the five statements, getting a scale ranging from 0 to 500. This summary variable was labeled "importance-of-gender "-scale, and the score was assigned to characterize the degree of gender awareness in professional relations.
For the statistical analyses the scales of the outcome variables were dichotomized in the middle, as agreeing/disagreeing (>50/≤ 50) for the five gender attitude statements, and as high/low (>250/≤250) for the "importance-of-gender "-scale
Bivariate associations between outcome variables (including the " importance-of-gender "-scale) and respondent specialty and respondent gender respectively, were assessed by chi-2 tests. P-values <0.05 were considered statistically significant. Multivariate logistic regression analyses were used to adjust for respondent sex, age, academic degree and years in the profession. A 95% confidence interval (CI) was used. The analyses regarding specialty were performed also for men and women separately. SPSS 8,0 was used.
Results
Demographics and dropouts
The characteristics known about the study sample are shown in table 2. There was a higher percentage of women among family physicians (45 %) than in the non-surgical (30 %) and the surgical doctor group (19 %). There was an uneven distribution of men and women also in sub-groups regarding age, academic degree and years in the profession. This was in concordance with the distribution within the total body of physicians in Sweden. [16]
Table 2.
Gender, age and speciality of respondents and non-respondents (N). Aacademic degree and years in profession of respondents (N), response rate (%) and women among respondents (N and %). (S = surgical doctors, NS = non-surgical doctors, FP = family physicians.)
| All | Respondents | Non-Respondents | Response Rate | Women among respondents‡ | |||||
| N | N | N | % | S | FP | NS | N | % | |
| Speciality† | |||||||||
| Surgical drs | 163 | 94 | 69 | 58 | 17 | 19 | |||
| Family physicians | 82 | 57 | 25 | 70 | 24 | 45 | |||
| Non-surgical drs | 223 | 152 | 71 | 68 | 38 | 30 | |||
| Gender† | |||||||||
| Men | 333 | 211 | 122 | 63 | 56 | 69 | 68 | ||
| Women | 135 | 92 | 43 | 68 | 63 | 71 | 69 | 92 | 30 |
| Age*† | |||||||||
| ≤45 | 178 | 102 | 76 | 57 | 50 | 71 | 58 | 45 | 42 |
| >45 | 276 | 196 | 80 | 71 | 66 | 68 | 75 | 46 | 24 |
| Academic degree‡ | |||||||||
| PhD | 135 | 24 | 18 | ||||||
| MD | 157 | 65 | 41 | ||||||
| Years in profession‡ | |||||||||
| ≤15 | 101 | 43 | 43 | ||||||
| >15 | 190 | 45 | 24 | ||||||
| Total | 468 | 303 | 165 | 65 | 92 | 30 | |||
† Data from original name list; ‡ Data from answers to the questionnaire; *Age is missing for 14 persons.
The response rate was 65 % (n = 303). Primary care and non-surgical doctors had a higher response rate than surgical doctors in the total study group as well as in all sub-samples concerning sex and age. Table 2 shows comparison between respondents and non-respondents regarding sex, specialty and age using data from the original name list. Not all respondents provided answers to every item. The largest internal dropout figure concerned specialty which 35 respondents omitted. Of respondents 274 (90 % of 303) answered all five statements.
Low gender awareness in the teaching/tutoring situation
Table 3 shows how physician teachers agree to the five statements. They agreed least with the importance of gender in relationships with students and most with the importance of gender in consultation. This pattern was consistent in all three specialty groups and among male as well as female physicians. The male physician group, in contrast to the female one, also assessed gender of relatively low importance in contact with colleagues and staff.
Low gender awareness among surgical doctors
Figure 1a shows the dispersion of ratings on "importance-of-gender"-scale as divided into quintiles. There were no family physicians scoring in the lowest quintile. The distribution was similar for each statement. Table 3 (column "all respondents") illustrates that significantly higher proportions of family physicians and non-surgical doctors, compared to surgical doctors, agreed to the importance of gender in their professional relationships. For example, on "importance-of-gender "-scale 76 % of family physicians and 67 % of non-surgical doctors scored high (>250) compared to 51 % of surgical doctors. When adjusting for respondent gender, age, academic degree, and years in the profession the difference between specialty groups remained statistically significant for all outcome variables except for statement 4. The results for the "importance-of-gender"-scale are seen in table 4. The odds for a family physician to score high on "importance-of-gender"-scale were almost three times higher, and for a non-surgical doctor almost two times higher when compared to a surgical doctor.
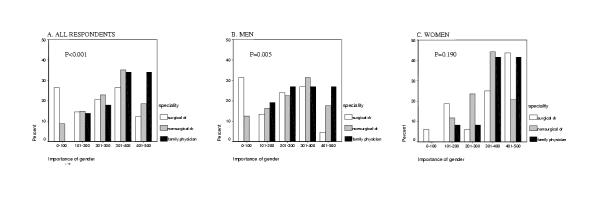
Figure 1.
Distribution of ratings on "importance-of-gender"-scale. P-values from chi-2 tests (2-sided, df = 8)
Table 4.
Number (N) and percentage (%) of respondents scoring >250 on "importance-of-gender"-scale (agreeing to the importance of gender in professional relationships). Adjusted OR (95 % confidence interval) for scoring > 250 on "importance-of-gender"-scale (multivariate logistic regression analysis).
| All respondents | Men | Women | |||||||
| N | % | OR (CI) | N | % | OR (CI) | N | % | OR (CI) | |
| Total | 173 | 63 | |||||||
| Gender | |||||||||
| Men | 106 | 56 | 1 | ||||||
| Women | 67 | 78 | 2.4 (1.2 – 4.6) | ||||||
| Specialty | |||||||||
| Surgical drs | 42 | 51 | 1 | 30 | 45 | 1 | 12 | 75 | 1 |
| Non-surgical drs | 76 | 67 | 1.9 (1.0 – 3.5) | 49 | 61 | 2.1 (1.0 – 4.2) | 27 | 79 | 1.2 (0.2 – 8.1) |
| Family physicians | 38 | 76 | 2.8 (1.1 – 6.4) | 18 | 69 | 3.2 (1.1 – 8.8) | 20 | 83 | 1.3 (0.2 – 7.8) |
| Age | |||||||||
| ≤45 | 71 | 71 | 1 | 39 | 67 | 1 | 32 | 76 | 1 |
| >45 | 102 | 59 | 0.6 (0.3 – 1.2) | 67 | 52 | 0.4 (0.1 – 1.1) | 35 | 81 | 1.3 (0.4 – 4.0) |
| Academic degree | |||||||||
| PhD | 71 | 60 | 1 | 55 | 57 | 1 | 16 | 73 | 1 |
| MD | 98 | 67 | 0.8 (0.4 – 1.5) | 49 | 57 | 0.7 (0.3 – 1.5) | 49 | 80 | 1.1 (0.2 – 4.7) |
| Years worked | |||||||||
| ≤15 | 67 | 69 | 1 | 36 | 63 | 1 | 31 | 78 | 1 |
| >15 | 102 | 60 | 0.9 (0.4 – 1.9) | 68 | 54 | 0.9 (0.3 – 2.3) | 34 | 81 | 1.3 (0.4 – 4.0) |
Differences between specialty groups only among men – lowest gender awareness among male surgical doctors
Figure 1b and 1c shows the dispersion of ratings on the "importance-of-gender"-scale as divided into quintiles for men and women separately. There were almost no women scoring in the lowest quintile. The distribution was similar for each statement. Table 3 (columns "total") demonstrates that women physicians assessed gender important to a higher degree than men did on all variables. The adjusted OR for a woman compared to a man to score high on " importance-of-gender "-scale was 2.4 (table 4).
Analyzing each outcome variable, men and women separately, demonstrated that differences between specialty groups reached significance among male physicians only (table 3). In the multivariate regression analyses these differences among men remained statistically significant (exemplified in table 4, columns "men" and "women"). The odds for a male family physician to assess gender important were three times higher, and for a male non-surgical doctor two times higher when compared to a male surgical doctor. Age, academic degree, and years in profession were not related to the outcome variables in the multivariate logistic regression analyses (table 4).
Discussion
This study at a Swedish university showed that physician teachers assessed gender less important in contact with students, colleagues, and staff than in contact with patients. The study also demonstrated differences in gender awareness between specialty groups. Family physicians were most likely to score the importance of gender high and surgical doctors to score low. The differences between specialty groups were mainly due to disparities among male physicians. Male surgical doctors assessed the role of gender in professional relations significantly less important than male family physicians and male non-surgical doctors. Women were more likely than men to assess the importance of gender high and among women there were no significant differences between specialty groups.
On method
Of the sample 35 % did not answer the questionnaire. Did only persons interested in gender answer? It does not seem so. There were many low ratings and some open-ended remarks display very questioning attitudes and opinions. For instance, one low-scoring physician wrote: "I hope health care professionals stop thinking about gender and start dedicating themselves to helping poor women as well as poor men who suffer in the health care system and in society!"
Male surgical doctors scored lowest. They also had a low response rate. Had more of them answered the differences between specialty groups and between men and women that we found might have been more pronounced.
Our study took place at Umeå University in northern Sweden, one of six universities with medical schools in Sweden. The education and curricula do not differ in any particular way from other medical universities in Sweden. The specialization pattern is the same as in the rest of the country and in the western world. We have no grounds to believe that the medical faculty in our study differs from those of other western universities. Still one must be cautious when trying to generalize our results, as the sample referred to only one medical school.
When we categorized specialties into groups we classified all operating specialties and also anesthetists as part of the surgical doctor group. Consequently, and in contrast to many reports about surgical specialties, our surgical doctor group included gynecologists, obstetricians, ENT-doctors, ophthalmologists, and anesthetists. This difference must be taken into account when comparing our results with other research. Gynecology and obstetrics are specialties that have many women doctors, in our sample eight out of seventeen. This made the proportion of woman in our surgical group as high as 19 %, almost twice the figure if only general surgery and subspecialties had been considered. Since women assessed gender important to a higher degree than men, the differences we demonstrated between specialty groups might have been larger if we had omitted gynecologists and obstetricians from the surgical specialty group.
Using a continuous VAS might imply problems, since one cannot assume that the distance between points in the middle of the scale line has the same significance as the same distance between points at the ends of the scale. However we did not use continuous values. In our regression analyses and for most chi-2 tests we dichotomized the scales in the middle.
We wanted to assess gender attitudes of physicians engaged in education. We found no gender-attitude questionnaire used before so we created one. We used statements about the importance of gender in professional relationships since we consider finding gender important in relations as one significant indicator of gender awareness and as a prerequisite for introducing and discussing gender issues and applying a gender perspective in medicine. However, it might be argued that doctors' own assessments on the scales do not disclose attitudes and behavior and that our statements and "the importance-of-gender"-scale do not reveal or characterize gender awareness. Other methods, such as open-ended interviews or observations might have been more valid. Still, we argue that the marks on the scales could well be considered to represent gender awareness. We consider it less likely that a person who is interested in and aware of gender issues and the role of gender should find gender of low importance in professional relations. In our open-ended answers there were no reflections about psychosocial conditions or power from low-scoring doctors but quite a few from those with high scores. For example one high-scoring doctor wrote: "Do I take more seriously demands about investigations and treatment from male patients? Do I understand women's symptoms as less important, easier to underestimate? If you score gender of low importance you are most likely not aware of the gender order that influences all human interactions. Several comments on the open-ended answers support this presumption. For instance one low-scoring man wrote: "I like to think that we are all human beings and can understand each other." On the other hand, a person less aware or a person who did not understand the questions might be provoked by the statements and in a few cases handle this by marking high on the scales, trying to be politically correct. However, there were few open-ended remarks about not understanding the questions.
When research focuses differences between women and men there is always the risk of strengthening existing gender-related dichotomies. We do not think of "femininity" and "masculinity" as opposites but rather highly overlapping categories also interacting with other contextual hierarchical categories such as class, ethnicity and age. In our study, for instance, there is an interaction between gender and the medical specialty hierarchy. Still there are unmotivated gender differences on the group level and their consequences have to be addressed and challenged. It is a delicate matter, in research as in everyday life, to find a way to do so, which does not reinforce sociocultural norms of gender.
On findings
Two out of three physician teachers found gender important in doctor – patient encounters. This is promising for the future since it increases the likelihood that gender is recognized as an important factor for health problems and that physicians will reflect upon gendered expectations and preconceptions. It might be due to the last decade's emphasis on women's health issues, to awakening reports on gender-biased treatment of women and men, and to an ongoing discussion about power and gender in consultation research [20,21].
However, relatively few physician teachers, especially men, and certainly in surgical specialties, assessed gender important in clinical tutoring and in relationships with colleagues and staff. This unawareness is unquestionably worth addressing. Numerous studies illustrate how gender reflects in hierarchies and division of labor in medical schools [8,11,22], wards [6,23], and health care centers [24]. Research also confirm the importance of role models and gender climate for the students' career choice [12,25] and that both female and male students prefer same-gender role-models [26]. One woman in our study commented like this about importance of gender in clinical tutoring: "When I was a student my role models were almost all men. I had a hard time finding a way to behave as a doctor. There was no one to 'imitate'."
In the following we will discuss how our findings might be related to the distribution of men and women and to the working climate in different specialties.
The proportion of women and men
The variation in gender awareness between different specialty groups partly mirrors the skewed representation of women and men. Women were more likely than men to assess gender important. As a consequence, a higher proportion of women in a specialty group increased the probability of high gender awareness. Still, varying proportions of women were not the sole explanation for differences in specialty groups, as these remained significant also when respondent gender was taken into account.
Gender climate
Apart from the number of women, what might there be in the working conditions of the specialty itself that can explain the different gender attitudes? Family doctors, more than hospital specialists, explore health and illness in a wider psychosocial context, including gender-specific circumstances. There are studies that show that medical students who wish to become family physicians have higher patient-centeredness than those who wish to become surgeons [27]. This might be part of the explanation why family physicians assess gender more important than other specialties.
The surgical specialties assessed the importance of gender low in our study. In what context can this be understood? One well-known opinion is that surgeons operate on sedated bodies, and therefore gender is not on the agenda – under the skin organs are mainly the same! If you think of surgical operations only, these arguments are reasonable, gender is of little importance. However there are more tasks than operations for a surgical doctor.
Another conception is that surgery is not suitable for women. This specialty demands, it is said, action, decisiveness, long working hours and leadership abilities [4,6]. A common stereotype in society and even among doctors is that "surgeons are kings, they're the real men" [19]. These arguments are extreme and part of a chauvinistic jargon, but never the less they help promote the perception of surgery as a "boys' club" [28] and may cause closure mechanisms for women [14,18,29]. A Norwegian study showed that female medical graduates were as likely as male ones to start a working career in surgery but they completed surgical training to a much lesser degree [29]. An analysis of attrition in a general surgery training program in Texas revealed that women were more than twice as likely as men to withdraw [30].
What can be done?
There are ways described to heighten awareness of gender and promote integration in segregated specialties; for example more women teachers [31], courses on gender issues among teaching physicians [32], and development of gender in the curricula of medical schools [33].
Women role models
As role models physician teachers considerably influence the career choice of medical students [19]. Absence or low representation of female role models in surgical specialties has been reported as an important reason why women reject or hesitate to enter these specialties [13,34,35]. Seven medical schools in USA, with varying proportions of women surgeons on the faculty, were compared. It was shown that female graduates chose surgery in relation to the proportion of women in the surgical faculty [31]. Considering this, more attention has to be given to the importance of equal representation of women and men as teachers and role models in medical education.
Implementation of gender among teachers and into curricula
Teachers' attitudes, interest and knowledge are crucial factors for implementing gender issues into medical curricula. Gender programs for teaching physicians is a way to encourage them to continuously reflect on their attitudes to gender and how gender affects their professional work and duties [32]. Such programs also help to make gender a question of competence and knowledge. Looking for and trying to eliminate gender-based stereotypes and androcentricity in medical curricula has been described as an accessible way to implement a gender perspective [33]. Experiences show that a strong, clear commitment from the faculty leadership is required to prevent backlash [32].
Conclusion
Our study showed an interaction between gender and specialty of physicians for their attitudes to the importance of gender in professional relationships. Male physician teachers compared to female, especially in the surgical doctor group, perceived the importance of gender low. We assume that these disparities in attitudes among physicians represent differences in their awareness of how gender is expressed in physicians' role and practice. The proportion of women is low in the specialties where male physicians' gender awareness was low and vice versa. We therefore suggest that both the proportion of women and gender awareness among male physicians in a specialty might have some influence on the working climate. Improving the working climate by increasing gender awareness might then be one way to reduce sex segregation. To focus on gender attitudes we suggest that gender issues should be included and reflected upon in medical education.
Competing interests
None declared.
Authors' contributions
All authors conceived and designed the research. GR undertook the analyses and interpretation of the data and drafted the article. EJ and KH participated in the analyses and interpretation, and revised the article critically for important intellectual content. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
Grants from The Swedish Foundation for Health Care Sciences and Allergy Research and The Umeå Medical District, the County Council of Västerbotten supported this study. We also thank Göran Westman for important comments on the manuscript and Hans Stenlund for statistical advice.
Contributor Information
Gunilla Risberg, Email: guarig97@student.umu.se.
Katarina Hamberg, Email: Katarina.Hamberg@fammed.umu.se.
Eva E Johansson, Email: eva.johansson@fammed.umu.se.
References
- Berger P, Luckman P. The social construction of reality. A treatise in the sociology of knowledge. London, Penguin books. 1991.
- Acker J. Gendering organizational theory. In: Mills AJ, Tancred P, editor. Gendering organizational analysis. London: Sage publications; 1992. [Google Scholar]
- West C. Reconceptualizing gender in physician-patient relationships. Soc Sci Med. 1993;36:57–66. doi: 10.1016/0277-9536(93)90305-N. [DOI] [PubMed] [Google Scholar]
- Cassel J. Doing gender, doing surgery: Women surgeons in a man's profession. Human Organization. 1997;56:47–52. [Google Scholar]
- Hamberg K, Risberg G, Johansson EE, Westman G. Gender bias in physicians' management of neck pain: A study of the answers in a Swedish national examination. J Women's Health & Gender-Based Medicine. 2002;11:653–666. doi: 10.1089/152460902760360595. [DOI] [PubMed] [Google Scholar]
- Davies K. Disturbing gender. On the doctor-nurse relationship. Lund: Dept of sociology, Lund University. 2001.
- Connell RW. Masculinities. Cambridge: Polity Press. 1995.
- Bickel J. Gender equity in undergraduate medical education: A status report. J Women's Health & Gender-Based Medicine. 2001;10:261–270. doi: 10.1089/152460901300140013. [DOI] [PubMed] [Google Scholar]
- Nicholson S. 'So you row, do you? You don't look like a rower.' An account of medical students' experience of sexism. Med Educ. 2002;36:1057–1063. doi: 10.1046/j.1365-2923.2002.01332.x. [DOI] [PubMed] [Google Scholar]
- Reed V, Buddeberg-Fischer B. Career obstacles for women in medicine: an overview. Med Educ. 2001;35:139–147. doi: 10.1046/j.1365-2923.2001.00837.x. [DOI] [PubMed] [Google Scholar]
- Sonnad SS, Colletti LM. Issues in the recruitment and success of women in academic surgery. Surgery. 2002;132:415–419. doi: 10.1067/msy.2002.127694. [DOI] [PubMed] [Google Scholar]
- Nora LM, McLaughlin MA, Fosson SE, Jacob SK, Schmidt JL, Witzke D. Does exposure to gender discrimination and sexual harassment impact medical students' specialty choices and residency program selections? Acad Med. 1996;71:S22–S24. doi: 10.1097/00001888-199610000-00033. [DOI] [PubMed] [Google Scholar]
- Baxter N, Cohen R, McLeod R. The impact of gender on the choice of surgery as a career. Am J Surg. 1996;172:373–376. doi: 10.1016/S0002-9610(96)00185-7. [DOI] [PubMed] [Google Scholar]
- Gjerberg E. Medical women – towards full integration? An analysis of the specialty choices made by two cohorts of Norwegian doctors. Soc Sci Med. 2001;52:331–43. doi: 10.1016/S0277-9536(00)00138-6. [DOI] [PubMed] [Google Scholar]
- Riska E. Towards gender balance: but will women physicians have an impact on medicine? Soc Sci Med. 2001;52:179–187. doi: 10.1016/S0277-9536(00)00218-5. [DOI] [PubMed] [Google Scholar]
- Swedish Medical Association Physicians in Sweden. Statistics. 1992-2002.
- Goldacre MJ, Davidson JM, Lamberth TW. Career choices at the end of the pre-registration year of doctors who qualified in the United Kingdom in 1996. Med Educ. 1999;33:882–889. doi: 10.1046/j.1365-2923.1999.00560.x. [DOI] [PubMed] [Google Scholar]
- Crompton R, LeFeuvre N, Birkelund GE. The restructuring of gender relations within the medical profession. In: Crompton R, editor. Restructuring gender relations and employment. The decline of the male breadwinner. New York: Oxford University Press; 1999. pp. 179–200. [Google Scholar]
- Hinze SW. Gender and the body of medicine or at least some body parts: (re)constructing the prestige hierarchy of medical specialties. The Sociological Quarterly. 1999;40:217–239. [Google Scholar]
- Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication. A meta-analytic review. JAMA. 2002;288:756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- Malterud K, Hollnagel H. Talking with women about personal health resources in general practice. Key questions about salutogenesis. Scand J Prim Health Care. 1998;16:66–71. doi: 10.1080/028134398750003188. [DOI] [PubMed] [Google Scholar]
- Nonnemaker L. Women in academic medicine. New insights from cohort studies. N Engl J Med. 2000;342:399–405. doi: 10.1056/NEJM200002103420606. [DOI] [PubMed] [Google Scholar]
- Kvaerner KJ, Aasland OG, Botten GS. Female medical leadership: cross sectional study. BMJ. 1999;318:91–94. doi: 10.1136/bmj.318.7176.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks F. Women in general practice: responding to the sexual division of labour? Soc Sci Med. 1998;47:181–193. doi: 10.1016/S0277-9536(98)00058-6. [DOI] [PubMed] [Google Scholar]
- Wright S, Wong A, Nevill C. The impact of role models on medical students. J Gen Int Med. 1997;12:53–56. doi: 10.1046/j.1525-1497.1997.12109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peronne KM, Zanardelli G, Worthington EL, Jr, Chartrand JM. Role model influence on the career decidedness of college students. Coll Stud J. 2002;36:109–111. [Google Scholar]
- Batenburg V, Smal JA, Lodder A, de Melker RA. Are professional attitudes related to gender and medical specialty? Med Educ. 1999;33:489–492. doi: 10.1046/j.1365-2923.1999.00333.x. [DOI] [PubMed] [Google Scholar]
- Lillemoe KD, Ahrendt GM, Yeo CJ, Herlong HF, Cameron JL. Surgery – Still an "old boys' club"? Surgery. 1994;116:255–261. [PubMed] [Google Scholar]
- Gjerberg E. Gender similarities in doctors' preferences – and gender differences in final specialisation. Soc Sci Med. 2002;54:591–605. doi: 10.1016/S0277-9536(01)00054-5. [DOI] [PubMed] [Google Scholar]
- Bergen PC, Turnage RH, Carrico CJ. Gender-related attrition in a general surgery training program. J Surg Res. 1998;77:59–62. doi: 10.1006/jsre.1998.5335. [DOI] [PubMed] [Google Scholar]
- Neumayer L, Kaiser S, Anderson K, Barney L, Curet M, Jacobs D, et al. Perceptions of women medical students and their influence on career choice. Am J Surg. 2002;183:146–150. doi: 10.1016/S0002-9610(01)00863-7. [DOI] [PubMed] [Google Scholar]
- Jacobs CD, Bergen MR, Korn D. Impact of a program to diminish gender insensitivity and sexual harassment at a medical school. Acad Med. 2000;75:464–469. doi: 10.1097/00001888-200005000-00017. [DOI] [PubMed] [Google Scholar]
- Philips S. Evaluating women's health and gender http://www.med.monash.edu.au/mrh/gendermed/resources/Canadian_curriculum.html [DOI] [PubMed]
- Williams C, Cantillon P. A surgical career? The views of junior women doctors. Med Educ. 2000;34:602–607. doi: 10.1046/j.1365-2923.2000.00666.x. [DOI] [PubMed] [Google Scholar]
- Richardson HC, Redfern N. Why do women reject surgical careers? Ann R Coll Surg Engl (Suppl) 2000;82:290–293. [PubMed] [Google Scholar]