Abstract
Introduction
Complicated grief is a prolonged grief disorder with elements of a stress response syndrome. We have previously proposed a biobehavioral model showing the pathway to complicated grief. Avoidance is a component that can be difficult to assess and pivotal to treatment. Therefore we developed an avoidance questionnaire to characterize avoidance among patients with CG.
Methods
We further explain our complicated grief model and provide results of a study of 128 participants in a treatment study of CG who completed a 15-item Grief-related Avoidance Questionnaire (GRAQ).
Results of Avoidance Assessment
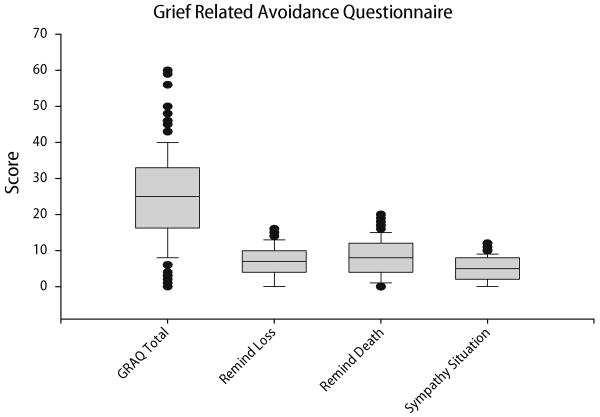
Mean (SD) GRAQ score was 25. 0 ± 12.5 with a range of 0–60. Cronbach's alpha was 0.87 and test re-test correlation was 0.88. Correlation analyses showed good convergent and discriminant validity. Avoidance of reminders of the loss contributed to functional impairment after controlling for other symptoms of complicated grief.
Discussion
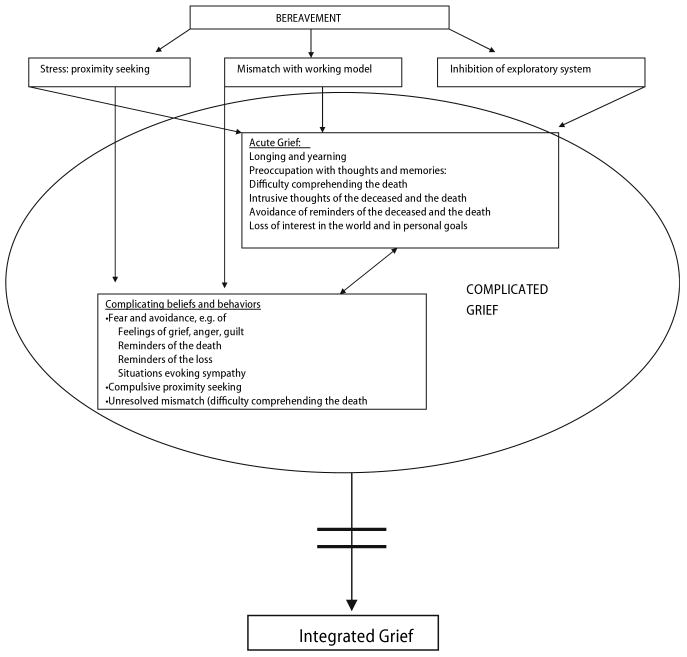
In this paper we extend our previously described attachment-based biobehavioral model of CG. We envision CG as a stress response syndrome that results from failure to integrate information about death of an attachment figure into an effectively functioning secure base schema and/or to effectively re-engage the exploratory system in a world without the deceased. Avoidance is a key element of the model.
Keywords: complicated grief, attachment, avoidance behaviour
Introduction
Bereavement is one of life's most painful experiences. Nevertheless, most people adjust to the trauma of death of a loved one, and continue to live full and satisfying lives. Adjustment to such a loss is very difficult, of course, and some people do not make an adaptive adjustment. Instead, they develop complicated grief with persistent separation distress and features of a chronic stress response syndrome [23, 27]. Bereaved individuals with complicated grief experience ongoing difficulty comprehending the death, intense yearning and longing for the person who died, guilt, anger and bitterness related to the death, recurrent pangs of painful emotions, preoccupation with thoughts and images of the deceased, sense of estrangement and emotional loneliness, and debilitating avoidance behaviors [25, 39].
Our group has been studying assessment and treatment of bereavement-related mental health problems for more than a decade [e.g., 16, 17, 19, 29, 30, 33, 36, 38, 40–45, 47, 50, 51, 54, 55]. We recently described a model of complicated grief [CG; 49] based upon Hofer's biobehavioral explanation of grief [21, 46]. The current paper further develops this by focusing on (1) a biobehavioral explanation for grief symptoms and (2) a more detailed description of complicated grief. Avoidance behavior, in particular, is a prominent component of CG. However, avoidance has been somewhat controversial as a CG symptom [e.g., 40]. Therefore, we provide data pertaining to the frequency and clinical significance of avoidance behaviors among a clinical population of individuals with CG.
In Shear and Shair [46] we posit that the symptoms of acute grief result from a temporary failure of biobehavioral regulatory functions subserved by the mental representation of the deceased person. Our model, integrates ideas proposed by Hofer [22] with findings from adult attachment studies, adult bereavement studies and clinical observations of bereaved people with complicated grief. In the current paper we extend our explication of complicated grief, by explaining the relationship between bereavement-induced regulatory failure and clinical symptoms, as well as complications that impede resolution of acute grief and comprise a component of the syndrome of complicated grief.
Central to our model is the proposition that the death of an attachment figure presents a decisive and temporarily irreconcilable mismatch between an unrevised mental representation of a loved one and a dramatic change in the ongoing relationship with that person. This mismatch has 4 consequences that largely explain the symptoms of acute grief: (1) the unrevised working model produces a continuing sense of the presence of the deceased. (2) The stress of bereavement activates attachment proximity seeking triggering a strong sense of yearning and longing for the deceased, as well as activation of thoughts and memories of the person. (3) Effective functioning of the working model is temporarily disrupted leading to loss of regulation emotion, attention and physiological process, and (4) Strong activation of attachment is associated with inhibition of the exploratory system, resulting in loss of interest in the world and inhibition of goal seeking.
In summary, acute grief is a preoccupying experience in which feelings of yearning and longing for the deceased are accompanied by pangs of intense emotions, often experienced as unfamiliar and difficult to control. The bereaved person is consumed with thoughts and memories of the deceased and relatively uninterested in other people and usual life occupations. In most cases, acute grief resolves as the permanence of the loss is comprehended, and this knowledge is integrated into attachment-related long term memory. Engagement in constructive daily occupations is reestablished, and effective attachment functioning is again secured. Thoughts and memories of the deceased remain accessible but are no longer preoccupying. After such integration there is diminished intensity of sadness, and retreat of preoccupying thoughts. CS Lewis described the experience of beginning integration, “…my heart was lighter than it had been for many weeks. …suddenly at the very moment when, so far, I mourned H. least, I remembered her best. Indeed it was something (almost) better than memory; an instantaneous, unanswerable impression. … It was as if the lifting of sorrow removed a barrier. (Lewis p.57) Metaphorically speaking, when integration is accomplished, it is as though the deceased releases her grip on the mind of the mourner, in order to reside quietly in his heart. Yet this process can be arduous, proceeding in fits and starts.
Adjustment to the death of a loved one can sometimes be complicated by maladaptive attitudes and behaviors. For example, blame of self or others, fear of the intensity of grief and/or the prospect of life without the deceased, and a disinclination to engage in activities that were shared with the deceased may impede the resolution of grief [1–3]. Sometimes practical and/or interpersonal problems complicate the adjustment process and impede the progress of grief. Persistent avoidance of reminders of the loss is another major impediment to adjustment. When resolution of acute grief is blocked, the result is complicated grief that can persist for years or even decades, with prolonged suffering and failure to find avenues for constructive activities in a world without the deceased. Symptoms of complicated grief contain elements of acute grief along with maladaptive cognitions, restricting avoidance behaviors and unsolved life problems.
In our model, CG is viewed as a stress response syndrome [23, 27] that results from failure to integrate information about death of an attachment figure into an effectively functioning secure base schema [52] and/or inability to effectively re-engage the exploratory system in a world without the deceased. This model informs our efficacious treatment for CG. Avoidance is a component of this model that can be difficult to assess, and pivotal to effective treatment. We provide data obtained from patients with complicated grief using a grief-related avoidance questionnaire.
Grief-related avoidance behavior
Avoidance is usually considered to be related to fear, and associated with anxiety disorders. However, avoidance can also occur in an effort to manage other distressing affects [35]. Avoidance behavior can resemble depressive withdrawal in restriction of activities. Bereaved people are inclined to refrain from engaging in activities they enjoyed with the deceased because of fear of intensifying sadness and yearning for the person who died [e.g., 28]. Among people with CG, grief-related avoidance, intended to regulate strong emotions and/or avoid confronting the painful reality of the death, can be pervasive and impairing. Most descriptions of clinical populations include avoidance, yet people with CG often fail to endorse avoidance when asked a global question such as “Is there anything you avoid because of the death?” By contrast, specific questioning uncovers a range of activities the person has stopped doing. Therefore, to better characterize avoidance behaviors, and determine the importance of these symptoms, we developed the Grief-related Avoidance Questionnaire (GRAQ), a self-report rating of 15 situations that bereaved individuals frequently refrain from doing. We tested this instrument in a sample of treatment-seeking individuals with CG.
Participants (n = 128; 103 women) were recruited for a treatment study of complicated grief [44], signed written informed consent, and underwent baseline assessment including the Grief-related Avoidance Questionnaire. All were ≥18 years of age (mean 47.2 ± 12.5 years). All scored ≥30 on the Inventory of Complicated Grief (ICG) (3) (mean 46.5 ± 10.7), were bereaved for at least 6 months, and did not have current or past bipolar disorder, current substance abuse or dependence, dementia, ongoing domestic violence, current or past history of psychosis or any uncontrolled general medical illness. Death of a loved one occurred by violent means (homicide/accident/suicide) for 35% (n = 45) and for the remainder by natural causes; 29% lost a spouse, 28% a parent, 27% a child and 16% a close friend or relative. Median time since the loss was 2.6 years, with a range of 6 months to 36 years.
Psychiatric Diagnosis was established using the Structured Clinical Interview for DSM-IV [14] administered by trained raters. Eighty (63%) met criteria for current Major Depression. Severity of depression and anxiety were assessed using the rater-administered 17-item Hamilton Depression (HRSD) [18] and Hamilton Anxiety (SIGH-A) [43, 46] Rating Scales. Complicated grief severity was assessed using the Inventory of Complicated Grief (ICG) [39]. Participants also completed the Impact of Events Scale [24], including intrusion and avoidance subscales and the Pittsburgh Sleep Quality Index (PSQI) [10]. We assessed functional impairment using the Work and Social Adjustment Scale (WSAS) [34], asking respondents to indicate how their grief affected their work, home management, social leisure, private leisure and/or ability to form close relationships.
Cronbach's alpha for the GRAQ total score was 0.87. Mean (SD) for 24 treatment nonresponders was 25.0 ± 13.0 at baseline and 25.5 ± 14.9 at post treatment. Baseline and post treatment scores were highly correlated (r = 0.88) indicating good test re-test reliability. A principal component exploratory factor analyses, with varimax rotation, revealed 3 factors, corresponding to avoidance of places and things that are reminders of the death (e.g., the final resting place or the place where the person died), avoidance of activities that are reminders of the loss (e.g., things the deceased did frequently, enjoyed, or was looking forward to doing), and avoidance of situations related to illness or death that ordinarily evoke sympathy (e.g., going to funerals or visiting ill people). Three items included in the GRAQ total score were omitted from the factor-based scores because of ambiguous loadings.
Figure 1 shows the distribution of GRAQ total and each factor-based subscale among the study participants. Mean score on this instrument (25.0 ± 9.0) indicated that on average, participants engaged in a moderate level of avoidance.
Fig. 1.
Distribution of Scores on the Grief-related Avoidance Questionnaire
Pearson correlation coefficients were calculated to investigate convergent and discriminant validity and to examine the clinical correlates of avoidance, including functional impairment, both before and after other CG symptoms and depression were partialled out. GRAQ showed significant correlation with the Impact of Events Avoidance subscale (r = 0.52; P < 0.0001) indicating good convergent validity. Discriminant validity was documented by the absence of correlation with the Pittsburgh Sleep Quality Index (r = 0.07; P = 0.346). Correlation with the Hamilton Anxiety Scale was r = 0.25; P = 0.006, and with the HRSD r = 0.34; P = 0.0001. Scores on the ICG correlated with GRAQ total scores (r = 0.40; P < 0.0001) and with scores on reminders of the loss subscale (r = 0.46; P < 0.0001) reminders of the death subscale (r = 0.19; P = 0.04) and sympathy situations subscale (r = 0.31; P = 0.0005).
WSAS correlated significantly with GRAQ total (r = 0.33; P = 0.0002) reminders of the loss subscale (r = 0.50; P < 0.0001) and sympathy situations (r = 0.18; P = 0.05) but not reminders of the death (r = 0.07; P < 0.41). After partialling out the contribution of ICG, the reminders of the loss subscale remained significantly correlated with WSAS (r = 0.30; P = 0.0008), and r = 0.21; P = 0.02, when we further partialled out the contribution of depression. Table 1 lists the items that comprise the reminders of the loss subscale of the GRAQ.
Table 1.
Avoidance of the Loss Subscale of Grief-related Avoidance Questionnaire (GRAQ; Items scored from 0 1 2 3 4: Never, Rarely, Sometimes, Often, Always)
|
We conclude that among help-seeking individuals with complicated grief, avoidance appears to be frequent and an important contributor to functional impairment. Boelen et al. [3] measured avoidance on a 5-item scale, postulating that such behavior is instrumental in failure to adjust to an important loss. Correlation of their scale with the ICG (r = 0.38) was similar to our findings for the correlation of the GRAQ with the ICG. Langner and Maercker [27] examined features of complicated grief using a questionnaire that included items related to avoidance. Results suggested that complicated grief is comprised of avoidance, intrusion and failure to adapt, similar to PTSD, but without hyper-arousal.
Bonanno and colleagues [5] examined the course of grief in the United States and the Peoples Republic of China at 4 and 18 months after a loss. A deliberate grief avoidance scale assessed avoidance of thinking, talking or expressing feelings about the deceased with close family members, and with friends. Grief processing was also measured in this study, using questions pertaining to thinking, talking about and expressing feelings about the deceased, as well as having positive memories and searching for meaning. Grief processing and deliberate avoidance were uncorrelated. Moreover, grief processing decreased over time while grief avoidance was stable. Deliberate avoidance at 4 months predicted poorer perceived health at 14 months in both countries and more psychological distress, further underscoring the importance of grief-related avoidance. Taken together, these results confirm that avoidance is an important feature of CG. We turn now to a discussion of our attachment-based grief model, including explaining how avoidance fits in this model.
Principles of attachment theory relevant to grief
Attachment behavior, with maternal proximity seeking and pronounced separation reactions, appears to be strongly conserved in mammalian infants and remarkably similar across species [38]. Extensive research confirms continuing operation of attachment throughout the lifespan [e.g., 6–8, 13, 20, 31, 32]. Bereavement is the state that results from loss of an attachment figure.
According to researchers [e.g., 9, 52] attachment theory rests on two fundamental principles: (1) a well functioning attachment relationship affords a secure base that serves to optimize autonomy and goal strivings, as well as provide support and comfort under stress, and (2) attachment relationships are internalized in the form of working models that subsume many of the secure base functions. Attachment figures can be reliably identified as individuals to whom we seek proximity, from whom we resist separation, to whom we turn when in distress, and from whom we garner support and encouragement as we explore the world, engage in meaningful activities and strive to master new challenges [15]. Loss of such a person creates a great disruption that is easily recognized as acute grief. Resolution of acute grief requires successful adjustment to far reaching effects of the loss, both practical and psychological. CG occurs when resolution is impeded.
Four principles of attachment functioning are helpful in understanding complicated grief: (1) Attachment relationships provide support for psychophysiologic functions, (2) Mental representations of attachment figures contain schemas that guide expectations for sensitive responsive caregiving under stress (3) Stress activates proximity seeking and the safe haven function of attention, while inhibiting the exploratory system, and (4) Among adults, providing is valued equally or even more than receiving care. We briefly explain how each of these pertains to understanding normal and complicated grief.
In adults, the attachment working model largely supplants the need for ongoing input from an attachment figure. This means we need to consider the effects of bereavement upon functioning of the working model. Bowlby's concept of internalized working models was based on early cognitive neuroscience. He postulated that attachment representations are a special form of long term memory organized to regulate affect and guide expectations of self and others. Working models operate through schema that are out of awareness [52], subserve internalized regulatory functions [22], and influence a wide range of psychological functions. Working models contain information about specific attachment relationships, guide ongoing interaction with the relevant attachment figure, and contribute to sense of self and expectations about relationships generally. The working model provides the means by which a person can have a meaningful attachment, including a felt sense of connectedness, to someone who is not physically present. To function effectively, the model must contain a reasonably accurate representation of features salient to the attachment relationship, so it is revised as needed.
Attachment representations are thought to be stable and not altered by transient variation in behavior [9]. Yet working models must be revised when important change occurs. Bowlby reasoned that the working model would incorporate change through a process of assimilation that is biased toward information that is most frequent and consistent. If so, even a change as obvious and fundamental as death would require sufficient time for assimilation before it is incorporated into the working model. The period of time required might be reduced when death is anticipated, but there is still some period during which the reality of the death is not comprehended. Immediately after its occurrence, perception of a loved one's death presents information that is incompatible with the working model of that person, largely operating out of awareness. The mismatch results in the sense of disbelief, confusion and disorientation.
Attachment and caregiving
Attachment theory places emphasis on the importance of caregiving. In order for someone to receive comfort under stress or support for exploration, a caregiver must provide these functions. Bowlby posited the existence of an instinctive caregiving system with a set goal of sensitive and responsive efforts to protect the physical and emotional wellbeing of another person. During infancy and early childhood, caregiving is provided by parents and received by their offspring. However adults both provide and receive care in attachment relationships. A recent paper suggests that being an effective caregiver may be more important than being well cared for in producing a sense of wellbeing [11]. Therefore, death of an attachment figure is additionally experienced as a failure of caregiving. Feelings of failure as a caregiver can trigger depression. Self-blame or survivor guilt can lead to restriction in specific kinds of satisfying activities to avoid feelings of guilt. It is not unusual for a bereaved person to rebuke herself for failing to prevent the death and/or to make it easier. Survivor guilt, triggered by a sense of joy in being alive, can accompany perceived caregiving failure. Survivor guilt is likely to be another motivation for avoidance of pleasurable activities and re-engagement in satisfying relationships.
Bereavement as a traumatic experience
Bereavement meets DSM IV criterion A. Recent studies confirm that PTSD occurs following natural death [53]. A further hallmark of a traumatic experience is the mismatch between information in the working model, fundamental to a sense of security, and reality [26]. Trauma resolution requires integration of troubling disparate information a into a revised cognitive affective framework [12], in this case the attachment working model. Acute grief includes oscillating intrusions and numbing/avoidance symptoms characteristic of a stress response syndrome [seen after a trauma 23]. However, trauma related to loss of a loved person differs in important ways from trauma due to a highly threatening event.
Violent events are time delimited, threaten sense of safety, incite fear, and produce hypervigilance to danger. Avoidance following a threatening event occurs as a response to cue-conditioned fear. Preoccupying thoughts and memories are centered on the horrific event. By contrast, loss of a loved one is a permanent ongoing reality that engenders sadness and longing, and produces hypervigilance for the lost person. Images, thoughts and memories of the deceased, even when intrusive, evoke a bittersweet mix of sadness and yearning. Preoccupying thoughts and memories related to grief are person- rather than event centered. Avoidance occurs commonly during bereavement. However, grief-related avoidance is used to regulate painful longing and/or reminders of the permanence of the loss rather than occurring in response to cues that trigger fear.
Highly stressful experiences activate attachment proximity seeking. Availability of an attachment figure mitigates fear and other dysphoric emotions related to the traumatic experience, helps re-establish normal routines and serves as a biobehavioral regulator. When the stress is loss of the attachment figure, calls for the loved one go unanswered. The result is intensified proximity seeking that becomes the central preoccupation of the bereaved person. We suggest that there are two fundamentally different forms of traumatic experience, one that occurs following a violent incident, and the other related to the demise or permanent loss of a love object. The ensuing stress response syndrome has some shared features, but differs if it is traumatic stress or traumatic loss. Failure to integrate information about a violent event results in PTSD while failure to integrate the permanent loss of an attachment figure produces CG. Death of a loved one can trigger either reaction.
Acute grief is the expected biobehavioral response to the death of a loved one [see Fig. 1 in 49]. Although painful and disruptive, data indicates that this response usually resolves in a satisfactory manner [4]. It is unclear whether grief work, defined as active problem solving and effortful emotion regulation, is required for successful resolution of grief, or whether such resolution unfolds naturally as the reality of the death is comprehended. Integration of the loss seems to occur through a process of oscillating attention toward and away from thoughts and memories of the deceased. The magnitude of oscillation is initially very large, swinging from intrusions, on the one hand to denial and numbing on the other. The oscillating process is gradually entrained and damped to a comfortable rhythm of engagement with, and then setting aside, thoughts and memories of the deceased.
We believe this naturally oscillating process is optimal for effecting a revision of the working model of the attachment figure. Periods of disengagement is important for restoration of satisfying relationships and daily life activities. The natural oscillation engendered by mechanisms for processing intense emotions fit hand-in-glove with dual process coping that is needed to adjust effectively to the loss. In a sense, the enticement of ongoing life provides the motivation for comprehending the death, while increasing comprehension of the death frees motivational and attentional resources. When the death has been incorporated into the working model, trauma-like symptoms resolve, proximity seeking recedes and grief intensity abates.
Stroebe and Schut point out that bereavement is often accompanied by a host of life problems, both related and unrelated to the deceased and maintain that resolution of acute grief must proceed hand in hand with coping with associated life stresses. These authors have proposed an interesting “dual process” coping model that interdigitates nicely with Horowitz's ideas about natural oscillation of intrusion and denial. According to the dual process model, effective coping requires addressing both loss and restoration-related stress. The model postulates that the two groups of stressors are best addressed contemporaneously, with attention oscillating between the two. This coping model extends Horowitz's disequilibrium model, that is focused more narrowly on the intrinsic biobehavioral process of integrating trauma. Stroebe and Schut's model suggests that bereavement works best when coping processes synergize with this intrinsic oscillating process. We accept this model though we keep separate Horowitz's biobehavioral thinking. The treatment we developed postulates a natural process of grief that is facilitated when loss and restoration-related stress are addressed contemporaneously. The combined dysequilibrium/dual process model guides our thinking about how resolution of acute grief can be waylaid. If wide oscillations are not damped, this hampers the progress of grief, since both intensely emotional intrusions and denial/numbing limit access to the working model. Additionally, if coping with important life problems is ineffective, this complicates the grief.
Bereavement is a complex state, which entails both disrupted internal processes and interruptions in relationships with other people as well as various activities. Internal processes include dysregulated emotions accompanied by potentially problematic thoughts and behaviors guided by attachment, caregiving and exploratory systems. There is a felt need for others, accompanied by a pronounced and sometimes uncomfortable disinterest in these people. Attention must be paid to outside affairs for which there may be little motivation or sense of competence. Integration of the loss can be blocked or complicated by intrinsic psychological processes that do not progress smoothly, problems with interpersonal support or difficult situational problems. If integration is blocked the bereaved person is caught in a seemingly endless state of acute grief, complicated by thoughts, feelings and behaviors that are impeding progress. This becomes a vicious cycle in which more grief adds to complicating emotions, thoughts and behaviors and these, in turn, strengthen barriers to grief resolution (see Fig. 2).
Fig. 2.
Complicated grief pathway elaborated from Shear and Shair [46]
We note that in addition to avoidance behaviors, proximity seeking is triggered by bereavement and can be a part of an adaptive grief process. However, when pronounced, each of these, along with maladaptive cognitions [1–3] and failure to effectively re-engage in ongoing life, can be a complicating impediment to integration of the loss. For some individuals, proximity seeking takes on an intense, compulsive quality. A person may spend inordinate amounts of time doing things that are helpful when not excessive. For example, spending long hours at the cemetery or in activities such as looking at pictures, constructing memorials or engaging in pleasurable reveries. Similarly, while it is helpful to set aside painful feelings for a time, some bereaved people engage in excessive avoidance and this becomes an impediment to both loss-related and restoration-related processes. In our experience, proximity seeking remits spontaneously without direct attention once the grief process is on track, while avoidance can be concealed and refractory. It is particularly important to uncover and treat avoidance in patients with complicated grief.
In summary, the model that informs our CG treatment considers bereavement to be a traumatic experience entailing loss of an attachment figure. Acute grief is the biobehavioral response to such loss, a painful, preoccupying state that resolves as the death is integrated into the working model of attachment. Acute grief and the process of integrating the loss usually occur naturally and without the need for active effort. Once the loss is integrated, yearning and searching diminishes, grief intensity declines, and there is often a deep feeling of connection to the deceased. CS Lewis describes this transition, “For as I have discovered, passionate grief does not link us with the dead but cuts us off from them. …It is just at those moments when I feel least sorrow…that H. rushes upon my mind in her full reality, her otherness.” [28 p. 67–68].
Individuals suffering from complicated grief fail to experience reprieve from pain and longing. Caught in a loop of prolonged grief symptoms and complicating psychological and/or life problems, time seems to stand still, frozen at the time of the death. The intervention we devised for complicated grief is guided by a the dual process coping model in which the natural oscillation of intrusion and denial is entrained by deliberate efforts to alternately engage and set aside painful recognition of the loss. We incorporate efficacious techniques from several schools of therapy in order to identify and address complicating psychological and environmental problems that complicated the natural grief process. The basic components of this treatment are listed in Table 2. We recently completed a randomized controlled trial of this treatment, in which we demonstrated efficacy compared to an alternative grief-focused treatment with well documented efficacy for major depression. We believe the effectiveness of this complicated grief treatment provides indirect support for the validity of the underlying model, though clearly there is a need for studies directly testing specific components of this model.
Table 2.
Complicated grief treatment goals and strategies
| Loss-focused strategies | Restoration-focused strategies |
|---|---|
| Goal: Move the loved one from the mind to the heart | Goal: Restore satisfying activities and relationships |
| Strategies and Techniques | |
| Imaginal revisiting exercises | Self care and personal goals work |
| Work with memories and pictures | Work on interpersonal disputes and/or role transition |
| Imaginal conversation with the deceased | |
| Situational revisiting exercises |
Acknowledgments
This work was supported by grants from the National Institute of Mental Health: MH60783, AG020677, AG13396, P30MH30915, and P30MH52247.
Contributor Information
Katherine Shear, Email: ks2394@columbia.edu, Columbia University School of Social Work, 1255 Amsterdam Avenue, New York, NY 10027, USA, Tel.: +1-212/851-2122, Fax: +1-212/851-2129.
Timothy Monk, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
Patricia Houck, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
Nadine Melhem, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
Ellen Frank, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
Charles Reynolds, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
Russell Sillowash, Department of Psychiatry, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA.
References
- 1.Boelen PA, van den Bout J, van den Hout M. The role of negative interpretations of grief reactions in emotional problems after bereavement. J Behav Ther Exp Psychiatr. 2003a;34:225–238. doi: 10.1016/j.jbtep.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Boelen PA, van den Bout J, van den Hout MA. The role of cognitive variables in psychological functioning after the death of a first degree relative. Behav Res Ther. 2003b;41:1123–1136. doi: 10.1016/s0005-7967(02)00259-0. [DOI] [PubMed] [Google Scholar]
- 3.Boelen PA, van den Bout J, van den Hout MA. Negative cognitions and avoidance in emotional problems after bereavement: a prospective study. Behav Res Ther. 2006;44:1657–1672. doi: 10.1016/j.brat.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 5.Bonanno GA, Papa A, Lalande K, Zhang N, Noll JG. Grief processing and deliberate grief avoidance: a prospective comparison of bereaved spouses and parents in the United States and the People's Republic of China. J Consult Clin Psychol. 2005;73:86–98. doi: 10.1037/0022-006X.73.1.86. [DOI] [PubMed] [Google Scholar]
- 6.Bowlby J. Attachment. Basic Books; New York: 1969. Attachment and Loss. [Google Scholar]
- 7.Bowlby J. Loss. III. Basic Books; New York: 1980. Attachment and Loss. [Google Scholar]
- 8.Bowlby J. Attachment and loss: retrospect and prospect. Am J Orthopsychiat. 1982;52:664–678. doi: 10.1111/j.1939-0025.1982.tb01456.x. [DOI] [PubMed] [Google Scholar]
- 9.Bretherton I, Munholland KA. Internal working models in attachment relationships: a construct revisited. In: Cassidy J, Shaver PR, editors. Handbook of attachment: theory, research and clinical applications. Guilford Press; New York: 1999. pp. 89–114. [Google Scholar]
- 10.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index (PSQI): a new instrument for psychiatric research and practice. Psychiatr Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 11.Deci EL, La Guardia JG, Moller AC, Scheiner MJ, Ryan RM. On the benefits of giving as well as receiving autonomy support: mutuality in close friendships. Pers Soc Psychol Bull. 2006;32:313–327. doi: 10.1177/0146167205282148. [DOI] [PubMed] [Google Scholar]
- 12.Ehlers A. Understanding and treating complicated grief: what can we learn from posttraumatic stress disorder? Clin Psychol: Sci Prac. 2006;13:135–140. doi: 10.1111/j.1468-2850.2006.00015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feeney BC. A secure base: responsive support of goal strivings and exploration in adult intimate relationships. J Pers Soc Psychol. 2004;87:631–648. doi: 10.1037/0022-3514.87.5.631. [DOI] [PubMed] [Google Scholar]
- 14.First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM IV axis I disorders. New York State Psychiatric Institute; New York, NY: 1996. [Google Scholar]
- 15.Fraley RC, Davis K. Attachment formation and transfer in young adults' close friendships and romantic relationships. Pers Relationship. 1997;4:131–144. [Google Scholar]
- 16.Germain A, Shear K, Monk TH, Houck PR, Reynolds CF, III, Frank E, Buysse DJ. Treating complicated grief: effects on sleep quality. Behav Sleep Med. 2006;4:152–163. doi: 10.1207/s15402010bsm0403_2. [DOI] [PubMed] [Google Scholar]
- 17.Hall MH, Buysse DJ, Dew MA, Prigerson HG, Kupfer DJ, Reynolds CF. Intrusive thoughts and avoidance behaviors are associated with sleep disturbances in bereavement-related depression. Depress Anxiety. 1997;6(3):106–112. [PubMed] [Google Scholar]
- 18.Hamilton M. A rating scale for depression. J Neurol Neurosur Ps. 1960;25:56–67. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harkness K, Shear MK, Frank E, Silberman R. Complicated grief treatment: case histories of four patients. J Clin Psychiatr. 2002;63:1113–1120. doi: 10.4088/jcp.v63n1205. [DOI] [PubMed] [Google Scholar]
- 20.Hazan C, Zeifman D. Pair bonds as attachments: evaluating the evidence. In: Cassidy J, Shaver PR, editors. Handbook of attachment: theory, research, and clinical applications. Guilford Press; New York: 1999. pp. 336–354. [Google Scholar]
- 21.Hofer MA. Relationships as regulators: a psychobiologic perspective on bereavement. Psychosom Med. 1984;46:183–197. doi: 10.1097/00006842-198405000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Hofer MA. On the nature and consequences of early loss. Psychosom Med. 1996;58:570–581. doi: 10.1097/00006842-199611000-00005. Review 50 refs. [DOI] [PubMed] [Google Scholar]
- 23.Horowitz MJ. Title Stress response syndromes. Oxford, England: Jason Aronson; 1976. [Google Scholar]
- 24.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Horowitz MJ, Siegel B, Holen A, Bonanno GA. Diagnostic criteria for complicated grief disorder. Am J Psych. 1997;154:904–910. doi: 10.1176/ajp.154.7.904. [DOI] [PubMed] [Google Scholar]
- 26.Janoff-Bulman R. Shattered assumptions. Free Press; New York NY: 1992. [Google Scholar]
- 27.Langner R, Maercker A. Complicated grief as a stress response disorder: evaluating diagnostic criteria in a German sample. J Psychosomatic Res. 2005;58:235–242. doi: 10.1016/j.jpsychores.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 28.Lewis CS. A grief observed. HarperCollins; NY: 1961. [Google Scholar]
- 29.Melhem N, Shear MK, Rosales C, Reynolds C, Frank E, Karageorge J. Comorbidity of axis 1 disorders in patients with complicated grief. J Clin Psychiat. 2001;62(11):884–887. doi: 10.4088/jcp.v62n1108. [DOI] [PubMed] [Google Scholar]
- 30.Melhem NM, Day N, Shear MK, Day R, Reynolds CF, 3rd, Brent D. Traumatic grief among adolescents exposed to a peer's suicide. Am J Psychiatr. 2004;161:1411–1416. doi: 10.1176/appi.ajp.161.8.1411. [DOI] [PubMed] [Google Scholar]
- 31.Mikulincer M, Gillath O, Shaver PR. Activation of the attachment system in adulthood: threat-related primes increase the accessibility of mental representations of attachment figures. J Pers Soc Psychol. 2002;83:881–895. [PubMed] [Google Scholar]
- 32.Mikulincer M, Shaver PR, Pereg D. Attachment theory and affect regulation: the dynamics, development, and cognitive consequences of attachment-related strategies. Motiv Emotion. 2003;27:77–102. [Google Scholar]
- 33.Monk TH, Houck PR, Shear MK. The daily life of complicated grief patients–What gets missed, what gets added? Death Stud. 2006;30:77–85. doi: 10.1080/07481180500348860. [DOI] [PubMed] [Google Scholar]
- 34.Mundt JC, Marks IM, Shear MK, Greist JH. The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatr. 2002;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- 35.Ottenbreit N, Dobson K. Avoidance and depression: the construction of the Cognitive–Behavioral Avoidance Scale. Behav Res Ther. 2004;42:293–313. doi: 10.1016/S0005-7967(03)00140-2. [DOI] [PubMed] [Google Scholar]
- 36.Pasternak RE, Reynolds CF, Schlernitzauer M, Hoch CC, et al. J Clin Psychiatr. 1991;52:307–310. [PubMed] [Google Scholar]
- 37.Polan HJ, Hofer MA. Psychobiological origins of infant attachment and separation responses. In: Cassidy J, Shaver PR, editors. Handbook of attachment: theory, research and clinical applications. Guilford Press; New York: 1999. pp. 162–180. [Google Scholar]
- 38.Prigerson HG, et al. Inventory of Complicated Grief: a scale to measure maladaptive symptoms of loss. Psychiatr Res. 1995;59:65–79. doi: 10.1016/0165-1781(95)02757-2. [DOI] [PubMed] [Google Scholar]
- 39.Prigerson HG, Monk TH, Reynolds CF, Begley A, Houck PR, Bierhals A, Kupfer DJ. Lifestyle regularity and activity level as protective factors against bereavement-related depression in late life. Depression. 1995–6;3(6):297–302. [Google Scholar]
- 40.Prigerson HG, Shear MK, Jacobs SC, Reynolds CF, Maciejewski PK, Davidson JRT, Pilkonis PA, Wortman CB, Williams JBW, Widiger TA, Frank E, Kupfer DJ, Zisook S. Consensus criteria for Complicated grief. Br J Psychiatr. 1999;174:67–73. doi: 10.1192/bjp.174.1.67. [DOI] [PubMed] [Google Scholar]
- 41.Reynolds CF, et al. Treatment of bereavement-related major depressive episodes in later life: a randomized, double-blind, placebo-controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatr. 1999;156:202–208. doi: 10.1176/ajp.156.2.202. [DOI] [PubMed] [Google Scholar]
- 42.Reynolds Charles F, Hoch Carolyn C, Buysse Daniel J, Houck Patricia R, et al. Electroencephalographic sleep in spousal bereavement and bereavement-related depression of late life. Biol Psychiatr. 1992;31:69–82. doi: 10.1016/0006-3223(92)90007-m. [DOI] [PubMed] [Google Scholar]
- 43.Shear MK, Frank E, Foa E, Cherry C, Reynolds CF, 3rd, Vander Bilt J, Masters S. Traumatic grief treatment: a pilot study. Am J Psychiatr. 2001b;158:1506–1508. doi: 10.1176/appi.ajp.158.9.1506. [DOI] [PubMed] [Google Scholar]
- 44.Shear K, Frank E, Houck P, Reynolds CF. Treatment of Complicated Grief: a randomized controlled trial. JAMA. 2005;293(21):2601–2608. doi: 10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shear K, Jackson C, Essock S, Donahue S, Felton C. Screening for complicated grief among Project Liberty service recipients after September 11th. Psychiatr Ser. 2006;57:1291–1297. doi: 10.1176/ps.2006.57.9.1291. [DOI] [PubMed] [Google Scholar]
- 46.Shear MK, Shair H. Attachment, loss and complicated grief. Dev Psychobiol. 2005;47:253–267. doi: 10.1002/dev.20091. [DOI] [PubMed] [Google Scholar]
- 47.Shear MK, Vander Bilt J, Rucci P, Endicott J, Lydiard B, Otto MW, Pollack MH, Chandler L, Williams J, Ali A, Frank DM. Reliability and Validity of a Structured Interview Guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depress Anxiety. 2001a;13:166–178. [PubMed] [Google Scholar]
- 48.Simon NM, Pollack MH, Fischmann BA, Perlman CA, Muriel A, Moore CW, Nierenberg AA, Shear K. Complicated grief and its correlates in patients with bipolar disorder. J Clin Psychiatr. 2005;66:1105–1110. doi: 10.4088/jcp.v66n0903. [DOI] [PubMed] [Google Scholar]
- 49.Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. 1999;23:197–224. doi: 10.1080/074811899201046. [DOI] [PubMed] [Google Scholar]
- 50.Szanto K, Prigerson HG, Houck PR, Reynolds CF. Suicidal ideation in elderly bereaved: the role of complicated grief. Suicide Life Threat Behav. 1997;27(2):194–207. [PubMed] [Google Scholar]
- 51.Szanto K, Shear K, Houck P, Reynolds CF, Frank E, Caroff K, Silowash R. Indirect self-destructive behavior and overt suicidality in patients with traumatic grief. J Clin Psychiatr. 2006;67:233–239. doi: 10.4088/jcp.v67n0209. [DOI] [PubMed] [Google Scholar]
- 52.Waters HS, Waters E. The attachment working models concept: among other things, we build script-like representations of secure base experiences. Attach Hum Dev. 2006;3:185–197. doi: 10.1080/14616730600856016. [DOI] [PubMed] [Google Scholar]
- 53.Zisook S, Chentsova-Dutton Y, Shuchter SR. PTSD following bereavement. Ann Clin Psychiatr. 1998;10:157–163. doi: 10.1023/a:1022342028750. [DOI] [PubMed] [Google Scholar]
- 54.Zuckoff A, Shear MK, Frank E, Daley DC, Seligman K, Silowash R. Treating complicated grief and substance use disorders: a pilot study. J Subst Abuse Treat. 2006;30:205–211. doi: 10.1016/j.jsat.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 55.Zygmont M, Prigerson HG, Houck PR, Miller MD, Shear MK, Jacobs S, Reynolds CF., 3rd A post hoc comparison of paroxetine and nortriptyline for symptoms of traumatic grief. J Clin Psychiatr. 1998;59:241–245. doi: 10.4088/jcp.v59n0507. [DOI] [PubMed] [Google Scholar]