Abstract
Pain is a highly subjective experience that can be substantially influenced by differences in individual susceptibility as well as personality. How susceptibility to pain and personality translate to brain activity is largely unknown. Here, we report that the functional connectivity of two key brain areas before a sensory event reflects the susceptibility to a subsequent noxious stimulus being perceived as painful. Specifically, the prestimulus connectivity among brain areas related to the subjective perception of the body and to the modulation of pain (anterior insular cortex and brainstem, respectively) determines whether a noxious event is perceived as painful. Further, these effects of prestimulus connectivity on pain perception covary with pain-relevant personality traits. More anxious and pain-attentive individuals display weaker descending connectivity to pain modulatory brain areas. We conclude that variations in functional connectivity underlie personality-related differences in individual susceptibility to pain.
Keywords: functional MRI, personality, susceptibility, insular cortex, brainstem
The perception of pain is not a simple reflection or linear readout of incoming sensory information but can be substantially influenced by variations in individual susceptibility. Under certain conditions, weak sensory stimuli can elicit significantly painful sensations, whereas in another context, much stronger stimuli do not yield any painful sensations at all (1). Such variations in the susceptibility to pain can occur as short-term fluctuations in perception (2, 3) but also depend on personality traits such as anxiety and attention to pain (4, 5). Within the brain, variation in the pain experience is subserved by a distributed network of brain areas, including but not exclusively involving somatosensory, cingulate, and insular cortices (6, 7). A recent study revealed that the neural activity of the cerebral pain network before a sensory event can predict subsequent pain perception, and thus relates to individual susceptibility to pain (2). However, the cerebral network of pain processing is complemented by a neural system dedicated to the modulation of pain that comprises descending projections from insular and prefrontal cortices via the brainstem periaqueductal gray (PAG) to the spinal cord (7, 8). Because a variety of experimental manipulations of the pain experience harness the descending pain modulatory system (9–13), the subjective experience of pain is likely to depend not only on the cerebral pain network but rather on the interaction (i.e., the connectivity) between the cerebral pain network and the pain modulatory system. However, how differences in the susceptibility to pain translate to the connectivity of the pain and pain modulatory networks, and eventually bias the perception of pain, is largely unknown. Here, we addressed this question in a functional MRI (fMRI) experiment. We hypothesized that the connectivity of the cerebral pain network to the pain modulatory system before a sensory event reflects the susceptibility to pain, and thus biases subsequent pain perception. We further speculated that the susceptibility to pain and the prestimulus connectivity between pain and pain modulatory systems are influenced by stable personality traits as well as by short-term changes in the perceptual and physiological state of the individual.
Results
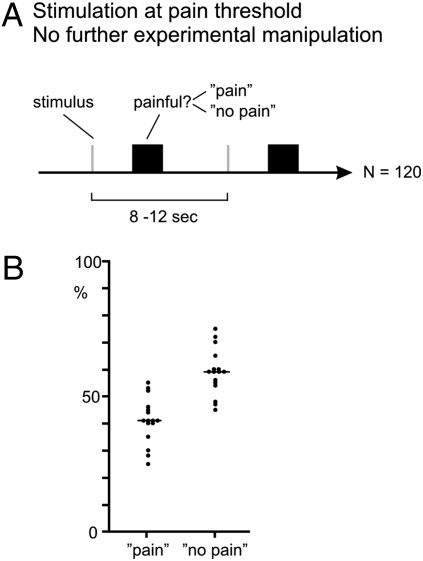
Sixteen healthy human subjects participated in a simple near-threshold pain detection paradigm (Fig. 1A). One hundred twenty brief radiant heat pulses were applied to the dorsal aspect of the subject’s right foot. Stimulus intensity was adjusted to pain threshold and was then kept constant throughout the experiment so that about half of the stimuli were perceived as painful and half were not. After each stimulus, the subject indicated with a button press whether the stimulus was perceived as painful (“pain” trials) or not (“no pain” trials). Across the whole group, the mean proportion of pain trials to no pain trials was 41 to 59 (Fig. 1B). Because objective stimulus intensity was kept constant throughout the experiment, we expected that the variation in perception (i.e., between pain and no pain trials) would at least partially reflect differences in the momentary susceptibility to pain rather than differences in sensory input. In the search for the cerebral mechanisms underlying the susceptibility to pain, we measured brain activity using fMRI.
Fig. 1.
Paradigm. (A) One hundred twenty brief radiant heat pulses were applied to the dorsal aspect of the right foot at an intensity around pain threshold without further experimental manipulation. After each trial, subjects indicated with a button press whether the stimulus was painful (pain) or not (no pain). Because stimulus intensity was kept constant throughout the experiment, differences in stimulus perception are likely to be at least partially attributable to fluctuations in the susceptibility to pain. (B) Individual and group mean proportion of pain and no pain trials.
Brain Responses Related to the Subjective Experience of Pain.
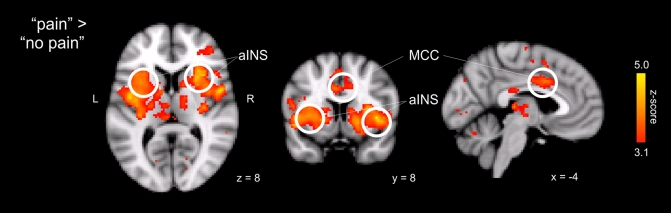
Initially, we compared brain responses to pain and no pain trials to define neural activity that is particularly related to the subjective perception of pain. Stimuli resulting in a perception of pain (pain trials) yielded stronger activation of the cerebral pain network (6, 7), including thalamus and somatosensory, midcingulate, and insular cortices, than identical stimuli that were not perceived as painful (no pain trials; Fig. 2 and Table 1). In addition, pain trials activated dorsolateral prefrontal cortex and putamen, which is probably related to perceptual decision (14) and motor (15) processes. However, although the intensity of stimulation was kept constant, a contribution of small unavoidable differences in sensory input (e.g., attributable to skin properties) to the measured differences in neural responses to pain and no pain trials cannot be ruled out.
Fig. 2.
Brain responses related to the subjective perception of pain. Brain areas in which neural responses are greater for pain than for no pain trials are shown. Activations are reported at a statistical threshold of P < 0.001, uncorrected, except for a priori hypothesized regions, which were thresholded at P < 0.005, uncorrected (see Materials and Methods). For visualization, activations are shown at a threshold of P < 0.001, uncorrected. aINS, anterior insular cortex; MCC, midcingulate cortex.
Table 1.
Brain areas responding to painful stimuli as revealed by the contrast between pain and no pain
| Area | Side | z | Coordinates |
| Anterior insular cortex | L | 4.8 | −48, 4, −2 |
| R | 4.9 | 30, 22, 10 | |
| Posterior insular cortex | L | 4.8 | −44, −4, 10 |
| R | 4.3 | 34, −16, 8 | |
| S2 | L | 3.8 | −52, −24, 20 |
| R | 4.8 | 50, 2, 6 | |
| IPC | L | 4.0 | −46, −36, 42 |
| R | 4.0 | 50, −32, 26 | |
| MCC | 4.3 | −2, 10, 34 | |
| SMA | 3.6 | −2, −12, 68 | |
| DLPFC | L | 4.0 | −38, 32, 23 |
| R | 3.8 | 32, 46, 12 | |
| Thalamus | L | 3.8 | −12, −14, 10 |
| R | 3.7 | 14, −6, 8 | |
| Putamen | L | 4.4 | −30, −2, 0 |
| R | 4.4 | 20, 6, −4 | |
| Midbrain | 4.0 | 4, −22, −20 |
Activations are reported at a statistical threshold of P < 0.001, uncorrected, except for a priori hypothesized regions, which were thresholded at P < 0.005, uncorrected (see Materials and Methods). DLPFC, dorsolateral prefrontal cortex; IPC, intraparietal cortex; MCC, midcingulate cortex; S2, secondary somatosensory cortex; SMA, supplementary motor area.
Prestimulus Brain Activity Reflecting the Susceptibility to Pain.
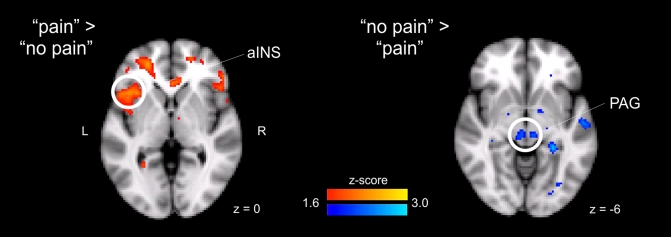
In contrast, because differences in neural activity before stimulus application cannot be attributed to sensory input, they likely reflect the susceptibility to a sensory event that then determines the subsequent perception of pain. We therefore compared neural activity in brain areas related to pain and pain modulation detected in a 3-sec period before pain and no pain trials. It was in the left anterior insular cortex where we observed stronger activity not only in response to but before pain and no pain trials (Fig. 3). The reverse contrast, no pain > pain, showed stronger activity in the PAG (Fig. 3 Right), which represents a central area of the descending pain modulatory system (7, 8). Therefore, the neural activity of key areas of the cerebral pain network and the pain modulatory system before a sensory event reflects the susceptibility to pain and biases subsequent perception without any experimental manipulation of the behavioral context.
Fig. 3.
Differences in prestimulus neural activity before pain and no pain trials. (Left) Brain areas in which signals detected in a 3-sec prestimulus period were greater before pain trials than before no pain trials. (Right) Reverse contrast. Activations are reported at a statistical threshold of P < 0.001, uncorrected, except for a priori hypothesized regions, which were thresholded at P < 0.005, uncorrected (see Materials and Methods). For visualization, prestimulus activations are shown at a threshold of P < 0.05 uncorrected. aINS, anterior insular cortex (coordinates −40, 20, 2; z = 2.6); PAG (coordinates 4, −26, −8 and − 6, −24, −8; z = 2.6).
Prestimulus Brain Connectivity Reflecting the Susceptibility to Pain.
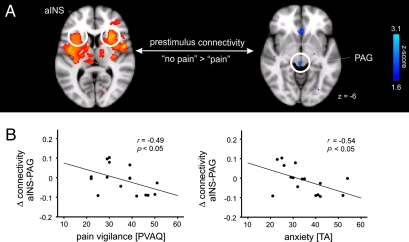
What we perceive may not only be influenced by the regional activity of brain areas but also by their functional integration (i.e., how they interact and communicate) (16). To address this question, we next compared cerebral connectivity before pain and no pain trials. The anterior insular cortex exhibited the strongest differences in prestimulus activity and poststimulus responses between pain and no pain trials, indicating that this brain region is particularly linked to the subjective perception of pain. Moreover, the anterior insular cortex is extensively connected to other brain areas of the pain and pain modulatory networks (17). We therefore hypothesized that the prestimulus functional connectivity of the bilateral anterior insular cortex to the PAG, as a key area of the pain modulatory system (7, 8), may reflect the susceptibility to pain and affect subsequent stimulus perception. Thus, we performed a psychophysiological interaction (PPI) analysis (18) of the prestimulus activity in the bilateral anterior insular cortex. PPI analyses reveal changes in functional connectivity between brain areas related to changes in a psychological variable. In our case, the functional connectivity of the bilateral anterior insular cortex during the prestimulus period was related to subsequent stimulus perception as indicated by the pain vs. no pain decision. We found that a stronger functional connectivity of the anterior insular cortex with the PAG predicted the occurrence of no pain trials (Fig. 4A). Therefore, the functional state and connectivity profile of these brain areas appear to reflect the individual’s momentary susceptibility to potentially painful stimuli. The next question to explore is what drives an individual’s momentary connectivity profile.
Fig. 4.
Prestimulus connectivity to the anterior insular cortex (aINS). (A) Differences in prestimulus connectivity to the bilateral aINS in a 3-sec prestimulus period as assessed by a PPI analysis. Brain areas whose connectivity to the anterior insular cortex is greater before no pain trials than before pain trials are shown. PAG (coordinates 4, −28, −4; z = 2.3). For coordinates of aINS, see Table 1. Voxels showing differences in connectivity to the left and right aINS were reported at a threshold of P < 0.05, small volume-corrected for the PAG (see Materials and Methods). For visualization, contrasts are shown at a threshold of P < 0.05 uncorrected. (B) Correlation between pain vigilance and anxiety and the difference between prestimulus insular and PAG connectivity. Pain vigilance and anxiety were assessed using the PVAQ, and the trait anxiety (TA) part of the STAI. Differences in connectivity between pain and no pain trials are given in effect sizes in arbitrary units. PAG coordinates were 0, −26, −16.
Personality, Susceptibility, and Brain Connectivity.
It is well known that personality traits such as anxiety and attention to pain influence an individual’s susceptibility to pain (4, 5). These traits could explain the interindividual differences in the susceptibility to pain that we observed. In this study, we assessed these traits with well-established questionnaires [State-Trait Anxiety Inventory (STAI) and Pain Vigilance and Awareness Questionnaire (PVAQ)]. Significant negative correlations of pain thresholds to measures of these traits corroborate the relevance of these personality measures for biasing susceptibility to pain [anxiety (STAI score): r = −0.51, P < 0.05; attention to pain (PVAQ score): r = −0.67, P < 0.01] in our study.
Next, we examined whether these traits influenced the prestimulus functional connectivity that was related to pain susceptibility in our study. We correlated the trait measures of anxiety and attention to pain with the difference in the prestimulus insular-PAG connectivities between pain and no pain trials. The results reveal that ratings of anxiety and attention to pain covaried significantly with the prestimulus difference in insular-PAG connectivity (anxiety: r = −0.54, P < 0.05; attention to pain: r = −0.49, P < 0.05; Fig. 4B). Thus, subjects with higher ratings of anxiety and attention to pain showed smaller differences in prestimulus insular-PAG connectivity between pain and no pain trials. Because anatomical insular-PAG connections are almost exclusively descending projections from the insular cortex to the PAG (19), these findings suggest that more anxious and vigilant subjects activate the descending pain modulatory system less efficiently. Vice versa, a less efficient activation of the pain modulatory system may result in higher ratings of anxiety and attention to pain.
Discussion
Here, we show that the functional connectivity of brain areas before a sensory event reflects the susceptibility to a subsequent noxious event. Specifically, the connectivity between brain areas of the cerebral pain network and the pain modulatory system significantly influences whether a noxious event is perceived as painful. Intriguingly, these effects of prestimulus connectivity on pain perception covary with pain-relevant personality traits. Therefore, our findings support the notion that variations in cerebral connectivity underlie personality-related differences in individual susceptibility to pain.
In a simple near-threshold pain detection paradigm, we observed that the neural connectivity before a sensory event can affect the subsequent perception of pain. It is important to note that these differences in neural activity before a sensory event cannot be attributed to differences in skin physiology, stimulus characteristics, or detection and/or discrimination functions of the task. A recent study related prestimulus neural activity to the perception of pain (2). In line with our study, the results of that study showed that higher prestimulus activity in bilateral anterior insular and anterior cingulate cortices predicted increased pain perception of subsequent stimuli. Further studies in other modalities indicated that intrinsic prestimulus neural activity in sensory and motor systems as well as in attentional and default mode networks determines task-related activations and task performance (20–26). The present observations extend these findings significantly by revealing that it is not only regional neural activity that biases perception; critically, it is also the prestimulus functional integration or connectivity among brain areas and functional systems that fundamentally influences perception. Furthermore, we have shown that these effects of prestimulus connectivity are significantly influenced by personality.
The sources of prestimulus differences in neural activity and connectivity are unknown yet. In different functional systems of the brain, perceptual fluctuations (3) and spontaneous intrinsic fluctuations of neural activity have been observed at low frequencies below 0.1 Hz (27). The present differences in prestimulus activity may therefore likewise represent intrinsic fluctuations of neural activity. Alternatively, because pain and no pain trials clustered during the experiment (see Materials and Methods), preceding stimuli could have modulated the baseline activity of pain and pain modulatory networks. Because the general linear model (GLM) includes separate regressors for pain and no pain trials, the contamination of prestimulus or baseline activity by stimulus-evoked activity is unlikely. Nonetheless, we cannot exclude contamination of baseline activity by cognitive influences that are not fully modeled. These influences include anticipation during the clustering of trials; it is intriguing that the anterior insular cortex is significantly more active before pain trials, because this region has been shown to be related to pain anticipation and how this amplifies the pain experienced (28). Based on the present data, we cannot, however, readily disentangle the differential intrinsic, stimulation-related, and cognitive contributions to baseline activity but rather note their relevance for influencing perception.
In the present study, the neural activity of the bilateral anterior insular cortex was particularly linked to the subjective perception of pain. This close association between the anterior insular cortex and the subjective experience of pain is in accordance with previous studies (2, 29, 30) and compatible with the hypothesis that this extensively connected (17) brain area integrates sensory and contextual information (31–33) to generate a predictive model (34–36) and a higher order representation (34–36) of interoception (i.e., the subjective state of the body).
Moreover, our results show that the prestimulus connectivity between the bilateral anterior insular cortex and the PAG predicts the susceptibility to pain and eventually determines pain perception. These findings indicate that the complex role of the anterior insula in the perception of pain does not only include integrative and interoceptive but also modulatory functions (34–36). Taken together, the present findings extend recent observations of an association between the neural activity of pain and pain modulatory brain networks and different cognitive and emotional manipulations of the pain experience (9–13). The connectivity between key areas of the pain and pain modulatory networks is thus likely to represent a central functional link in the complex brain network subserving pain perception. Specifically, the connectivity of the anterior insular cortex to the PAG may flexibly adjust the momentary susceptibility to pain according to the current behavioral demands of the individual.
Intriguingly, the effects of insular-PAG connectivity on pain perception covaried with personality traits as temporally stable determinants of the susceptibility to pain. Individual personality-related patterns of interoceptive pain modulatory connectivity could shape individual susceptibility to pain. Alternatively, but not mutually exclusively, cerebral connectivity patterns may influence the susceptibility to pain, which, in turn, shapes pain-relevant personality traits. A longitudinal study would be required to determine which order of events occurs. Importantly, personality traits represent temporally stable characteristics of the individual that shape the susceptibility to pain in the long term. However, our results indicate that personality traits also influence short-term changes in the physiological and perceptual state of the individual that are superimposed on the baseline susceptibility and allow the individual to adjust his or her momentary susceptibility to pain. In the healthy subjects participating in the present study, these processes are likely to provide an adaptive balance between the maintenance of behavioral flexibility and the strong behavioral drive that pain imposes on the individual (1). However, abnormal connectivity patterns between the cerebral pain network and the pain modulatory system could well yield perceptual imbalances that may contribute to the generation of chronic pain states (37).
In conclusion, the present results reveal that the functional connectivity of the bilateral anterior insular cortex and the PAG as key areas of pain and pain modulatory networks relates to the susceptibility to pain. Variations in these connectivity patterns, which appear to relate to pain-relevant personality traits, may underlie intra- and interindividual differences in the susceptibility to pain. Current concepts of the neural substrates of pain should therefore consider the intrinsic functional integration among the pain and pain modulatory networks as important personality-related determinants of the subjective experience of pain.
Materials and Methods
Subjects.
Sixteen healthy male human subjects with a mean age of 27 years (range: 20–33 years) participated in the experiment. Informed consent was obtained from all subjects before participation. The study was approved by the local ethics committee and conducted in conformity with the Declaration of Helsinki.
Paradigm.
In each subject, 120 cutaneous laser stimuli around pain threshold were applied to the dorsum of the right foot. Intensity of stimulation around pain threshold implies that some of the stimuli were perceived as painful and some as nonpainful. Three to 5 sec after each stimulus, subjects were prompted by a visual cue to decide whether they perceived the applied stimulus as painful or not (Fig. 1A). Subjects indicated their pain or no pain ratings by button presses of the index or middle finger of the right hand. Assignment of pain and no pain to buttons was varied between subjects. The duration of the rating period was 3 sec. The next stimulus was applied 5-7 sec after the rating period. Stimuli were cutaneous laser stimuli, which selectively activate nociceptive fibers without concomitant activation of tactile fibers (38). At painful intensities, these stimuli yield a pinprick-like sensation, whereas at nonpainful intensities, stimuli are perceived as warm or not perceived at all. The laser device was a neodymium:yttrium-aluminum-perovskite (Nd:YAP) laser (DEKA) with a wavelength of 1340 nm; pulse duration was 4 ms and spot diameter was 6 mm. To avoid tissue damage and sensitization or habituation effects, the site of stimulation was slightly changed after each stimulus. The stimulus intensity for the fMRI experiment was individually adjusted to pain threshold requiring a mean stimulus intensity of 3.4 J (range: 3–4.25 J). Pain thresholds were determined using the ascending and descending method of limits. The ascending series started with laser stimuli at low undetectable intensities. Stimulus intensity was then increased in 0.25-J steps until a pinprick-like painful sensation was reported. Next, stimulus intensity was increased by 0.5 J, and the descending series was started in 0.25-J steps until no painful sensation was reported any more. This procedure was performed twice, and the most often reported threshold intensity was chosen for a practice session. In the practice session, 20 stimuli were applied. If the percentage of pain trials in the practice session was 50 ± 10%, the same stimulus intensity was chosen for the experiment. If not, stimulus intensity was decreased or increased by 0.25 J and another practice session was performed. This procedure was repeated until the percentage of pain trials was 50 ± 10%.
The mean percentage of pain trials during the experiment was 41% (range: 25–55%). The percentage of pain trials did not correlate with stimulus intensity (r = 0.36, P = 0.18), PVAQ score (r = −0.22, P = 0.42), or STAI score (r = −0.21, P = 0.43). The duration of the preceding interstimulus interval did not differ between pain and no pain trials (paired t test, P = 0.81). Clustering of trials was analyzed by calculating intervals between pain trials and the last preceding pain trial as well as between no pain trials and the last preceding pain trial. Intervals to the last preceding pain trial were significantly shorter for pain trials than for no pain trials (paired t test, P = 0.001) indicating a clustering of pain and no pain trials during the experiment. The mean number of transitions between pain and no pain trials, and vice versa, was 23 (range: 19–28). The number of transitions did not correlate with the PVAQ score (r = 0.24, P = 0.38) or STAI score (r = 0.19, P = 0.48).
Debriefing of subjects included questionnaires on trait anxiety (STAI) (39) and pain vigilance (PVAQ) (40).
Data Acquisition.
MRI scanning was performed on a 3-T Varian MRI scanner. We used an optimized echo planar imaging (EPI) T2*-sensitive sequence for blood oxygenation level-dependent contrast (41). The influence of in-plane susceptibility gradients was reduced by tilting the imaging slice by 30° from an axial-to-coronal orientation. Through-plane susceptibility gradients were compensated by means of a moderate preparation gradient pulse similar to z-shimming. Each volume comprised 41 axial slices of 3-mm thickness with 3 × 3 mm in-plane resolution, repetition time was 3 sec, echo time (TE) was 30 msec, field of view (FOV) was 192 × 192 mm, and matrix size was 64 × 64 pixels. Field maps were obtained using a symmetrical-asymmetrical spin-echo sequence (TE = 20 ms, 2.5-ms dwell time, FOV and matrix identical to EPI). A T1-weighted structural image (1-mm3 voxel) was acquired to aid registration of T2*-weighted images to standard stereotactic space [Montreal Neurological Institute (MNI)-152 template].
Data Analysis.
Data were analyzed using the Functional Magnetic Resonance Imaging of the Brain (FMRIB) Software Library (FSL; http://www.fmrib.ox.ac.uk/fsl/). Preprocessing included removal of the initial four volumes, motion correction, B0-unwarping using field maps, spatial smoothing using a Gaussian kernel of full-width-half-maximum of 8 mm, and temporal high-pass filtering with a cutoff of 100 sec.
Data analysis was performed using the GLM. The model consisted of separate regressors for the pain and no pain stimuli and for the rating period, which were convolved with the canonical hemodynamic response function (mean lag of 6 sec, full-width-half-maximum of 6 sec) to generate regressors for the model (implemented in FSL). To investigate the influence of the prestimulus period on stimulus perception, a 3-sec prestimulus period before pain and no pain trials was added to the model. The prestimulus period was not convolved with the hemodynamic response function to ensure that it did not include any signal from the poststimulus period and not to restrict the analysis to a particular shape of a response function. Importantly, this model also included regressors for the pain and no pain stimuli, and thus accounts for the influence of the previous response on the next trial.
Voxel-wise regression coefficients for all regressors (prestimulus pain, prestimulus no pain, stimulus pain, stimulus no pain, and rating) were estimated by using a mixed-effects GLM comprising a fixed-effects first-level individual analysis and random-effects second-level group analysis (42). Activations are reported at a statistical threshold of P < 0.001, uncorrected, except for a priori hypothesized regions, which were thresholded at P < 0.005, uncorrected (note: only clusters involving five or more contiguous voxels are reported) (43, 44). A priori regions included pain areas S1 and S2 and insular and anterior cingulate cortex as well as orbitofrontal, medial, and lateral prefrontal cortex and the PAG as brain areas related to the modulation of pain.
To investigate the influence of prestimulus connectivity on the perception of pain, we performed a PPI analysis (18). The physiological variable was the time course of the left and right anterior insular cortex, because this was the brain area that showed the closest relation to the subjective experience of pain in the contrast of brain responses to pain vs. no pain trials. Time courses were calculated from 8-mm spheres centered on activation foci of this contrast. Time courses from these spheres were extracted as separate regressors, which were then individually demeaned. The psychological variable was the contrast between the 3-sec prestimulus periods before pain and no pain trials. The PPI regressor was computed as the product of the demeaned activity of the left and right anterior insula and a vector coding for the prestimulus period (−1 for no pain trials, 1 for pain trials). This PPI analysis tests for differences in connectivity to the insular cortex before pain and no pain trials. Voxels showing differences in connectivity to the left and right anterior insular cortex were reported at a threshold of P < 0.05, small volume-corrected for 8-mm spheres around PAG foci as defined during the prestimulus period. PPIs were calculated separately for left and right insula, and an inclusive masking procedure for both effects was performed. Individual differences in the influence of connectivity on pain perception were related to personality traits as assessed by the STAI and PVAQ (see above). Specifically, a large difference in connectivity before pain and no pain trials can be assumed to reflect a strong influence of connectivity on perception, whereas a small prestimulus difference in connectivity is likely to reflect a weak influence of connectivity on pain perception. This strength was related to personality traits calculating Pearson’s correlation coefficients while controlling for the percentage of pain and no pain trials as a possible confound.
Acknowledgments
We thank Ray Dolan for mentoring the Feodor Lynen Research Fellowship (to M.P.). The study was supported by a Feodor Lynen Research Fellowship (to M.P.) of the Alexander von Humboldt Foundation.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
References
- 1.Melzack R, Casey KL. Sensory, motivational, and central control determinants of pain: A new conceptual model. In: Kenshalo DRJ, editor. The Skin Senses. Springfield, IL: Charles C. Thomas; 1968. pp. 423–439. [Google Scholar]
- 2.Boly M, et al. Baseline brain activity fluctuations predict somatosensory perception in humans. Proc Natl Acad Sci USA. 2007;104:12187–12192. doi: 10.1073/pnas.0611404104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deco G, Romo R. The role of fluctuations in perception. Trends Neurosci. 2008;31:591–598. doi: 10.1016/j.tins.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Crombez G, Van Damme S, Eccleston C. Hypervigilance to pain: An experimental and clinical analysis. Pain. 2005;116:4–7. doi: 10.1016/j.pain.2005.03.035. [DOI] [PubMed] [Google Scholar]
- 5.Rhudy JL, Meagher MW. The role of emotion in pain modulation. Curr Opin Psychiatry. 2001;14:241–245. [Google Scholar]
- 6.Apkarian AV, Bushnell MC, Treede RD, Zubieta JK. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005;9:463–484. doi: 10.1016/j.ejpain.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron. 2007;55:377–391. doi: 10.1016/j.neuron.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Fields HL, Basbaum AI, Heinricher MM. Central nervous system mechanisms of pain modulation. In: McMahon SB, Koltzenburg M, editors. Wall and Melzack’s Textbook of Pain. Philadelphia: Elsevier; 2006. pp. 125–142. [Google Scholar]
- 9.Petrovic P, Kalso E, Petersson KM, Ingvar M. Placebo and opioid analgesia—Imaging a shared neuronal network. Science. 2002;295:1737–1740. doi: 10.1126/science.1067176. [DOI] [PubMed] [Google Scholar]
- 10.Tracey I, et al. Imaging attentional modulation of pain in the periaqueductal gray in humans. J Neurosci. 2002;22:2748–2752. doi: 10.1523/JNEUROSCI.22-07-02748.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wager TD, et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science. 2004;303:1162–1167. doi: 10.1126/science.1093065. [DOI] [PubMed] [Google Scholar]
- 12.Bingel U, Schoell E, Herken W, Büchel C, May A. Habituation to painful stimulation involves the antinociceptive system. Pain. 2007;131:21–30. doi: 10.1016/j.pain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Valet M, et al. Distraction modulates connectivity of the cingulo-frontal cortex and the midbrain during pain—An fMRI analysis. Pain. 2004;109:399–408. doi: 10.1016/j.pain.2004.02.033. [DOI] [PubMed] [Google Scholar]
- 14.Heekeren HR, Marrett S, Ungerleider LG. The neural systems that mediate human perceptual decision making. Nat Rev Neurosci. 2008;9:467–479. doi: 10.1038/nrn2374. [DOI] [PubMed] [Google Scholar]
- 15.Alexander GE, DeLong MR, Strick PL. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci. 1986;9:357–381. doi: 10.1146/annurev.ne.09.030186.002041. [DOI] [PubMed] [Google Scholar]
- 16.Friston K. Beyond phrenology: What can neuroimaging tell us about distributed circuitry? Annu Rev Neurosci. 2002;25:221–250. doi: 10.1146/annurev.neuro.25.112701.142846. [DOI] [PubMed] [Google Scholar]
- 17.Mesulam MM, Mufson EJ. The insula of Reil in man and monkey. In: Peters A, Jones EG, editors. Cerebral Cortex. New York: Plenum; 1985. pp. 179–226. [Google Scholar]
- 18.Friston KJ, et al. Psychophysiological and modulatory interactions in neuroimaging. Neuroimage. 1997;6:218–229. doi: 10.1006/nimg.1997.0291. [DOI] [PubMed] [Google Scholar]
- 19.Carrive P, Morgan MM. In: Periaqueductal gray. The Human Nervous System. Paxinos G, Mai JK, editors. San Diego: Elsevier Academic; 2004. pp. 393–423. [Google Scholar]
- 20.Arieli A, Sterkin A, Grinvald A, Aertsen A. Dynamics of ongoing activity: Explanation of the large variability in evoked cortical responses. Science. 1996;273:1868–1871. doi: 10.1126/science.273.5283.1868. [DOI] [PubMed] [Google Scholar]
- 21.Fox MD, Snyder AZ, Vincent JL, Raichle ME. Intrinsic fluctuations within cortical systems account for intertrial variability in human behavior. Neuron. 2007;56:171–184. doi: 10.1016/j.neuron.2007.08.023. [DOI] [PubMed] [Google Scholar]
- 22.Supèr H, van der Togt C, Spekreijse H, Lamme VA. Internal state of monkey primary visual cortex (V1) predicts figure-ground perception. J Neurosci. 2003;23:3407–3414. doi: 10.1523/JNEUROSCI.23-08-03407.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sapir A, d’Avossa G, McAvoy M, Shulman GL, Corbetta M. Brain signals for spatial attention predict performance in a motion discrimination task. Proc Natl Acad Sci USA. 2005;102:17810–17815. doi: 10.1073/pnas.0504678102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weissman DH, Roberts KC, Visscher KM, Woldorff MG. The neural bases of momentary lapses in attention. Nat Neurosci. 2006;9:971–978. doi: 10.1038/nn1727. [DOI] [PubMed] [Google Scholar]
- 25.Hesselmann G, Kell CA, Eger E, Kleinschmidt A. Spontaneous local variations in ongoing neural activity bias perceptual decisions. Proc Natl Acad Sci USA. 2008;105:10984–10989. doi: 10.1073/pnas.0712043105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Lafuente V, Romo R. Neuronal correlates of subjective sensory experience. Nat Neurosci. 2005;8:1698–1703. doi: 10.1038/nn1587. [DOI] [PubMed] [Google Scholar]
- 27.Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat Rev Neurosci. 2007;8:700–711. doi: 10.1038/nrn2201. [DOI] [PubMed] [Google Scholar]
- 28.Ploghaus A, et al. Dissociating pain from its anticipation in the human brain. Science. 1999;284:1979–1981. doi: 10.1126/science.284.5422.1979. [DOI] [PubMed] [Google Scholar]
- 29.Craig AD, Chen K, Bandy D, Reiman EM. Thermosensory activation of insular cortex. Nat Neurosci. 2000;3:184–190. doi: 10.1038/72131. [DOI] [PubMed] [Google Scholar]
- 30.Koyama T, McHaffie JG, Laurienti PJ, Coghill RC. The subjective experience of pain: Where expectations become reality. Proc Natl Acad Sci USA. 2005;102:12950–12955. doi: 10.1073/pnas.0408576102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coghill RC, et al. Distributed processing of pain and vibration by the human brain. J Neurosci. 1994;14:4095–4108. doi: 10.1523/JNEUROSCI.14-07-04095.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Starr CJ, et al. Roles of the insular cortex in the modulation of pain: insights from brain lesions. J Neurosci. 2009;29:2684–2694. doi: 10.1523/JNEUROSCI.5173-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paulus MP, Stein MB. An insular view of anxiety. Biol Psychiatry. 2006;60:383–387. doi: 10.1016/j.biopsych.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 34.Craig AD. How do you feel? Interoception: The sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3:655–666. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- 35.Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol. 2005;493:154–166. doi: 10.1002/cne.20749. [DOI] [PubMed] [Google Scholar]
- 36.Craig AD. How do you feel—Now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10:59–70. doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- 37.Edwards RR. Individual differences in endogenous pain modulation as a risk factor for chronic pain. Neurology. 2005;65:437–443. doi: 10.1212/01.wnl.0000171862.17301.84. [DOI] [PubMed] [Google Scholar]
- 38.Plaghki L, Mouraux A. How do we selectively activate skin nociceptors with a high power infrared laser? Physiology and biophysics of laser stimulation. Neurophysiol Clin. 2003;33:269–277. doi: 10.1016/j.neucli.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 39.Spielberger CD. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- 40.McCracken LM. ‘Attention’ to pain in persons with chronic pain: A behavioral approach. Behav Ther. 1997;28:271–284. [Google Scholar]
- 41.Deichmann R, Gottfried JA, Hutton C, Turner R. Optimized EPI for fMRI studies of the orbitofrontal cortex. NeuroImage. 2003;19:430–441. doi: 10.1016/s1053-8119(03)00073-9. [DOI] [PubMed] [Google Scholar]
- 42.Woolrich MW, Behrens TE, Beckmann CF, Jenkinson M, Smith SM. Multilevel linear modelling for FMRI group analysis using Bayesian inference. NeuroImage. 2004;21:1732–1747. doi: 10.1016/j.neuroimage.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 43.Singer T, et al. Empathic neural responses are modulated by the perceived fairness of others. Nature. 2006;439:466–469. doi: 10.1038/nature04271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Summerfield C, et al. Predictive codes for forthcoming perception in the frontal cortex. Science. 2006;314:1311–1314. doi: 10.1126/science.1132028. [DOI] [PubMed] [Google Scholar]