Abstract
Individuals with “insecure” adult attachment styles have been shown to experience more pain than people with secure attachment, though results of previous studies have been inconsistent. We performed a cross-sectional study on a large population-based sample to investigate whether, compared to pain free individuals, subjects with chronic widespread pain were more likely to report insecure adult attachment style. Subjects in a population-based cross-sectional study completed a self-rated assessment of adult attachment style. Attachment style was categorised as secure (i.e., normal attachment style); or preoccupied, dismissing or fearful (insecure attachment styles). Subjects completed a pain questionnaire from which three groups were identified: pain free; chronic widespread pain; and other pain. Subjects rated their pain intensity and pain-related disability on an 11 point Likert scale. Subjects (2509) returned a completed questionnaire (median age 49.9 years (IQR 41.2–50.0); 59.2% female). Subjects with CWP were more likely to report a preoccupied (RRR 2.6; 95%CI 1.8–3.7), dismissing (RRR 1.9; 95%CI 1.2–3.1) or fearful attachment style (RRR 1.4; 95%CI 1.1–1.8) than those free of pain. Among CWP subjects, insecure attachment style was associated with number of pain sites (Dismissing: RRR 2.8; 95%CI 1.2–2.3, Preoccupied: RRR = 1.8, 95%CI 0.98–3.5) and degree of pain-related disability (Preoccupied: RRR = 2.1, 95%CI 1.0–4.1), but not pain intensity. These findings suggest that treatment strategies based on knowledge of attachment style, possibly using support and education, may alleviate distress and disability in people at risk of, or affected by, chronic widespread pain.
Keywords: Attachment, Chronic widespread pain, Epidemiology
1. Introduction
Adult attachment style is a psychological representation of self and others, determined by early childhood experiences of relationships with primary caregiver(s) [4]. Attachment style is considered to be a stable trait throughout adult life, determines how individuals relate to each other and is linked to strategies for managing threatening situations [4]. Bartholomew and Horowitz [1] proposed four sub-types of adult attachment style: one “secure” attachment style (characterized by a positive model of self and other in a relationship), and three insecure styles: “fearful” (negative model of self and other), “preoccupied” (negative model of self, positive model of other), and “dismissing” (positive model of self, negative model of other).
Recently, there has been increasing recognition of the importance of adult attachment style in the experience of pain [26,31]. Insecure attachment in healthy populations is associated with hypochondriacal beliefs [40], hypervigilance to pain [23], increased pain-related fears [23], reduced pain threshold [27] and poor pain coping [23,26]. Among subjects with chronic pain, insecure attachment has been linked to more negative appraisals of pain [6,28], increased pain perception and disability [24], increased psychological distress [6,29], impaired coping with pain [27] and greater healthcare utilisation [6]. These findings suggest that individuals with insecure attachment are more likely to develop pain, and once pain has developed they are more likely to perceive it as more intense, disabling and distressing. However, the data are equivocal with reports of no relationship between attachment style and pain intensity [6,27,29].
Small population sizes, varying classifications of pain and recruitment from highly specialised pain centres, such as pain rehabilitation services, may explain the inconsistency of results. Furthermore, since attachment style influences how individuals interact with healthcare services [7,17,30], reliance on patient samples for the study of the association between pain and attachment style, may introduce a selection bias that could amplify or attenuate the true association of attachment with pain experience.
The findings of a large, population-based study investigating the associations between attachment style and the experience of pain are reported here. Subjects with chronic widespread pain (CWP) were studied since it has been demonstrated previously that (1) CWP has a high prevalence in the general population, (2) it is possible to identify cases using self-rated assessments, and (3) there is a strong association of CWP with psychological and social factors [11,21]. By recruiting subjects from the general population it was intended that any selection bias associated with studying patients actively seeking healthcare was reduced. The following hypotheses were tested (1) compared to pain-free individuals, those with CWP would be more likely to report insecure attachment and (2) among individuals with CWP, those with insecure adult attachment style would report more intense pain, more pain sites, and more pain-related disability than those with secure attachment style.
2. Method
2.1. Participants
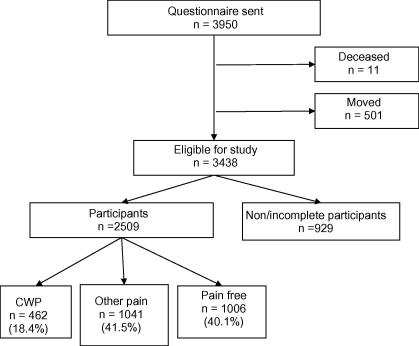
Subjects aged between 25 and 65 years, registered at one of three general practices in the north-west of England, who had previously participated in a postal survey [14] were mailed a questionnaire. (All participants gave permission for further contact.) Of the 3950 subjects mailed, 2509 subjects returned a completed questionnaire. After adjusting for those who had moved (N = 501, 12.7%) or died (N = 11, 0.3%) and therefore could not receive a questionnaire, the response rate was 73% (see Fig. 1). The mean age of participants was 49.0 (±10.2) years and 1482 (59.2%) were female.
Fig. 1.
Flowchart showing participation rates.
2.2. Procedures
Subjects were mailed a questionnaire which assessed pain status, attachment style and demographic factors. A cover letter was included that introduced the study. All subjects provided written consent to participate in the study. To avoid inappropriate mailings the study team were notified of all subjects who had either died or changed address. An additional check compared the address of subjects who had not responded to the questionnaire held by the general practice to that held by the Local Authority on a publicly accessible database. It was assumed that subjects had changed address when these did not match. The study was approved by the local NHS Research Ethics Committee.
2.3. Measures
2.3.1. Demographic information
Subjects were asked to report their age, gender and which one of five categories of marital status (single, married/cohabiting, separated, divorced, widowed) applied to them.
2.3.2. Pain status
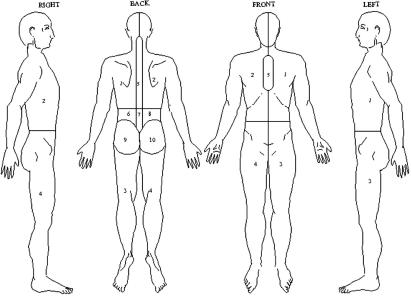
Subjects were asked to report if they had any ache or pain in the last month which had lasted for one day or longer. Subjects responding positively were asked to indicate on four line drawings of body manikins (front, back and sides) the site(s) where they experienced this pain. For coding purposes the body manikins were split into 10 regions, as illustrated in Fig. 2. Subjects with pain were asked to answer a further question that determined the chronicity of their pain symptoms: “Have you been aware of this pain for three months or longer?” Subjects who answered positively to this question were classified as having chronic pain. These methods are routinely used to determine the location and duration of pain [10,16]. Using the information on pain status, CWP was classified using the definition in the American College of Rheumatology (ACR) criteria for fibromyalgia [41]. These require that pain must have been present for at least three months and be present in two contra-lateral areas of the body, above and below the waist and in the axial skeleton. Based on these criteria subjects were categorised into 3 groups (i) pain free, (ii) “other pain” (i.e., subjects reporting pain but which did not satisfy the criteria for CWP) and (iii) CWP.
Fig. 2.
Body manikins used in questionnaire to determine pain sites. Ten regions used for classification of CWP are illustrated.
Participants were also asked to rate the intensity of their pain on an 11-point Likert scale ranging from 0 “no pain” to 10 “pain as bad as it could be”, and their pain-related disability (how much the pain had interfered with their day to day activities) on an 11-point Likert scale (ranging from 0 “no interference” to 10 “unable to carry out activities)”.
2.3.3. Assessment of adult attachment style
Subjects completed an assessment to identify their predominant adult attachment style, taken from the Relationship Questionnaire developed by Bartholomew and Horowitz [1]. Subjects were provided with four short paragraphs, each describing a prototypical attachment style as it applies to close adult peer relationships and were asked to select which of the four paragraphs best described the predominant characteristics of their adult relationships (for brevity, the continuous items from the Relationship Questionnaire were omitted). Using this questionnaire subjects’ attachment style was categorised as secure (a positive model of the self and the other in a relationship), preoccupied (negative model of the self but a positive model of the other), fearful (negative model of both the self and other), dismissing (positive model of the self but a negative view of the other) [13].
2.4. Statistical analysis
Mann–Whitney U test and χ2-analyses were used to examine differences between the three pain groups (i.e., pain free, CWP and other pain) in age, gender and attachment style. χ2-Analysis was also used to examine the relationship between attachment style and marital status. Multinomial regression analysis was used to examine the association between attachment style and pain status. The model was adjusted for age and gender. The referent category was the pain free group. Results are reported as relative risk ratios (RRRs) with 95% confidence intervals (CIs).
Separate multinomial regression models were constructed to examine the association between attachment style and pain intensity, number of pain sites, and pain-related disability within the CWP group. Pain intensity scores, number of pain sites (the total number of the pain sites reported which ranges from 0 to 10 sites [19] and pain disability scores were categorised into tertiles. The lowest tertile was classed as the referent category. The results are presented as relative risk ratios (RRRs) with 95% CIs. All analyses were conducted using the STATA statistical software [37].
3. Results
3.1. Response rates
The responders and non-responders did not differ in gender, however, the responders were significantly (p < 0.05) older than the non-responders (responders mean age = 49.0 years ±10.2; non-responders mean age = 46.3 years +10.7).
3.2. Attachment styles
Subjects (1361 (54.2%)) reported a secure attachment style. Of the 1148 (45.8%) subjects that reported an insecure attachment style, 715 (28.5% of participants) were classified as fearful, 289 (11.5%) preoccupied, and 144 (5.7%) dismissing. Compared to subjects with secure attachment, those with insecure attachment were more likely to be single (secure: 6.3%; insecure: 14.0% single) divorced (secure: 6.4%; insecure: 11.5% divorced) or separated (secure; 1.8%; insecure: 2.3% separated) and less likely to be female (secure: 62.5%; insecure: 55.1% female, χ2 = 14.11, p < 0.0005) or married (secure: 81.4%; insecure: 67.2%) (significance across categories of marital status χ2 = 74.43; p < 0.0005). There was no significant difference in age between the secure and insecure attachment subjects (p = 0.25).
3.3. Pain status
462 (18.4%) subjects reported CWP, 1041 (41.5%) reported other pain and 1006 (40.1%) subjects were pain free. Subjects with CWP were significantly older and more likely to be female than those who were pain free (see Table 1).
Table 1.
Subject characteristics for each pain group.
| Pain free N = 1006 |
Other pain N = 1041 |
CWP N = 462 |
p⁎ | |
|---|---|---|---|---|
| Median (95% CI) | Median (95% CI) | Median (95% CI) | ||
| Age | 48.9 (47.8–50.0) | 49.9 (49.0–50.7) | 52.1 (50.5–53.5) | 0.003 |
| Gender | n (%) | n (%) | n (%) | |
| Female | 551 (54.8) | 640 (61.5) | 291 (63.0) | 0.002 |
| Male | 455 (45.2) | 391 (38.5) | 171 (37.0) | |
| Attachment | ||||
| Secure | 576 (57.3) | 578 (55.5) | 207 (44.8) | |
| Insecure | 430 (42.7) | 463 (44.5) | 255 (55.2) | <0.0005⁎⁎ |
| -Preoccupied | 90 (8.9) | 124 (11.9) | 75 (16.2) | |
| -Dismissing | 51 (5.1) | 59 (5.7) | 34 (7.4) | |
| -Fearful | 289 (28.7) | 280 (26.9) | 146 (31.6) | |
All p-values χ2 except age, which is Kruskal–Wallis test.
p-value represents significance of χ2-analysis of secure attachment versus insecure attachment across the three pain groups.
3.4. Attachment style and the presence of pain
3.4.1. Analysis approach
To test the main hypotheses, the characteristics of pain were first compared between those with secure attachment versus insecure attachment (i.e., subjects with preoccupied, fearful and dismissing grouped together). Subsequent analyses then examined the specific associations of the individual insecure attachment styles (preoccupied, dismissing and fearful) and pain characteristics.
3.4.2. Secure attachment vs. insecure attachment
After adjusting for age and gender individuals with CWP were 70% more likely to report an insecure attachment style than pain free subjects (RRR: 1.7; 95%CI 1.4–2.2) (see Table 2). Subjects reporting other pain were not more likely to have an insecure attachment style than pain free subjects, however.
Table 2.
Association between attachment style and pain for secure and insecure attachments styles and subtypes of attachment style.
| Attachment style | Other pain RRR (95%CI) | CWP RRR (95%CI) |
|---|---|---|
| Secure | 1 (–) | 1 (–) |
| Insecure | 1.10 (0.9–1.3) | 1.69 (1.35–2.21) |
| Secure | 1 (–) | 1 (–) |
| Preoccupied | 1.42 (1.06–1.91) | 2.57 (1.81–3.65) |
| Dismissing | 1.17 (0.79–1.74) | 1.91 (1.20–3.05) |
| Fearful | 0.98 (0.80–1.20) | 1.39 (1.08–1.80) |
Adjusted for age and gender.
3.4.3. Subtypes of attachment style
Individuals with CWP were 2.6 times more likely to report a preoccupied attachment style (RRR 2.6; 95%CI 1.8–3.7), 1.9 times more likely to report a dismissing attachment style (RRR 1.9; 95%CI 1.2–3.1) and 1.4 times more likely to report a fearful attachment style (RRR 1.4; 95%CI 1.1–1.8) than those free of pain (all adjusted for age and gender) (see Table 2). Whilst individuals with other pain were 40% more likely to report a preoccupied attachment style they were not more likely to report dismissing or fearful attachment styles.
3.4.4. Association of attachment style, pain intensity, number of pain sites, pain-related disability
Within the group of CWP subjects, there was no significant association between attachment style and pain intensity for any of the attachment styles (see Table 3). CWP subjects with a preoccupied attachment style were 1.8 times more likely to report a higher number of pain sites (RRR 1.8; 95%CI 0.98–3.5) than those with a secure attachment style, although the confidence intervals spanned unity. CWP subjects with a dismissing attachment style were 2.8 times more likely to report a higher number of pain sites (RRR 2.8; 95%CI 1.2–2.3) than those with a secure attachment style. A fearful attachment style was not significantly associated with reporting a higher number of pain sites. CWP subjects with a preoccupied attachment style were also more likely to report a high level of pain-related disability (RRR 2.1; 95%CI 1.0–4.1) than those with a secure attachment style. Fearful and dismissing attachment styles were not significantly associated with pain-related disability.
Table 3.
Association between attachment style and: pain intensity; number of pain sites; pain-related disability within CWP group.
| Attachment style | Pain intensity⁎(N = 451) | Number of pain sites⁎⁎(N = 461) | Pain-related disability⁎⁎⁎(N = 450) | |||
|---|---|---|---|---|---|---|
| 6–7 | 8–10 | 8 | 9–10 | 4–7 | 8–10 | |
| RRR (95%CI) | RRR (95%CI) | RRR (95%CI) | RRR (95%CI) | RRR (95%CI) | RRR (95%CI) | |
| Preoccupied | 1.7 (0.9–3.2) | 1.5 (0.7–3.0) | 1.5 (0.8–3.0) | 1.8 (0.98–3.5) | 1.5 (0.8–2.9) | 2.1 (1.0–4.1) |
| Dismissing | 1.2 (0.5–2.7) | 0.98 (0.4–2.5) | 1.3 (0.5–3.6) | 2.8 (1.2–6.3) | 0.6 (0.5–1.5) | 1.3 (0.5–3.2) |
| Fearful | 0.9 (0.5–1.5) | 1.1 (0.7–1.9) | 1.6 (0.9–2.6) | 1.3 (0.8–2.3) | 1.0 (0.6–1.7) | 1.2 (0.7–2.2) |
Referent secure attachment style, pain intensity 0–5.
Referent secure attachment style, number of pain sites 3–7.
Referent secure attachment style, pain-related disability 0–3.
4. Discussion
The aim of this study was to test the hypotheses that an insecure attachment style would be associated with CWP, pain intensity, the number of pain sites, and pain-related disability. In a large, population-based study almost half of subjects reported an insecure adult attachment. Insecure attachment was associated with almost two times the prevalence of CWP. Of the various attachment styles the presence of CWP was most strongly associated with preoccupied attachment. Dismissing and fearful attachment were associated with CWP but to a lesser extent. Among subjects with CWP insecure attachment was associated with a higher number of pain sites (preoccupied and dismissing) and a higher level of pain-related disability (preoccupied) but not with higher pain intensity.
A number of possible mechanisms by which abnormal attachment may contribute to the development of CWP have been proposed in the research literature investigating links between childhood trauma (such as physical and sexual abuse) and the development of subsequent medically unexplained symptoms, including fibromyalgia [3,34,36]. Mechanisms that may explain the observed relationships include (i) persistent tendency to dissociate when stressed [33,35,39], (ii) a tendency to communicate in terms of physical symptoms instead of emotional feelings [12] and (iii) abnormalities in the way affected individuals perceive/respond to threats and engage support from others [7,31]. Abnormalities in hypothalamic–pituitary–adrenal (HPA) axis function have also been implicated as potential biological mechanisms mediating the association between attachment and the development of CWP. In particular, observations from animal and human studies have indicated that early life stresses and abnormal attachment result in altered HPA axis function [5,9,15,25,32]. Furthermore, we have reported that dysregulation of the HPA axis predicts the onset of new episodes of CWP, independent of the effects of psychological distress [20,22].
Of the individual subtypes of insecure attachment, we found that preoccupied attachment style was most strongly associated with the experience of CWP, the extent of pain-related disability and the number of pain sites. This is consistent with other studies that have found that individuals who are anxious about the availability and responsiveness of support (fearful or preoccupied attachment using the categories of Bartholomew and Horowitz) perceive their pain more negatively [6] and cope less well [27]. It is not clear why dismissing attachment style was associated with number of pain sites, though not pain intensity or related disability. The stability of this finding requires replication in further studies.
These findings support the predictions made in earlier research, that an awareness of attachment issues may assist in the management of people with CWP [26,31]. Assessments of attachment have potential to identify those at high risk of developing chronic pain (e.g., from individuals with acute pain), those who are at risk of coping poorly with chronic pain or those who may have difficulty in engaging with healthcare services. Further prospective studies are now required to clarify the nature of the associations of insecure attachment with pain experience. Inclusion of individuals with different pain syndromes, recruited from different settings will establish the generalisability of the importance of attachment in populations with chronic pain. Investigation of the role of neuro-developmental and psychosocial variables may clarify the direction and mechanisms of effect of attachment on chronic pain development and experience. Novel interventions based on knowledge of attachment issues, for example using support and education, targeting patients, their carers or their healthcare providers need to be developed. The impact of such treatment strategies on health outcomes (e.g., engagement with services, satisfaction with treatment, distress, disability and health-related quality of life), requires assessment in future intervention trials.
The study has a number of methodological strengths. First, subjects were recruited from three general practices in the North West of England. Given the high response rate to the study we are confident that the subjects were representative of the population in the area where the study was conducted. Individuals responding to the questionnaire were slightly older than the non-responders though, since attachment was not associated with age we do not feel this difference in age undermines the findings. Second, by studying a population-based sample, as opposed to patients actively seeking healthcare, we aimed to avoid the recruitment bias that might result from the influence of attachment style on healthcare seeking behaviour. Third, we focused the investigations on subjects with CWP, identified using standardised criteria, to increase the homogeneity of the sample and hence the generalisability of the findings.
The main weakness of the study was that we assessed attachment using a brief, self-report measure. The assessment of attachment therefore reflects individuals’ subjective perceptions of their close relationships, which may be vulnerable to reporting bias. As such, other concurrent factors may have influenced reporting of attachment style, such as the presence of anxiety or depression, or the experience of pain [8,18]. Whilst other more comprehensive assessments of attachment, delivered by self-rated questionnaire or interview, were available, these were considered too lengthy for inclusion in the postal assessments. Despite its brief nature, however, 46% of participants had insecure patterns of attachment, which is similar to the proportion among other non-patient samples [8,27,40]. Furthermore, similar to other studies, we showed that attachment was associated with marital status [2,7,38], with those subjects with insecure attachment being almost twice as likely to be single, separated or divorced. Since details of marital status are likely to be reliable, this provides some evidence of construct validity for the measure of attachment. Additional information about co-morbidities was not collected in this survey and we cannot examine the role of co-morbidities in the associations reported.
The study indicates an association between insecure attachment and the experience of CWP, even among subjects recruited from the general population. Thus, previous similar observations among patient samples have not been due solely to a selection bias reflecting an influence of attachment style on health seeking behaviour. The cross-sectional nature of the study, however, means we are not able to draw inferences on the direction of causation between adult attachment and pain experience. One possible interpretation of these findings is that individuals with insecure attachment may be twice as likely to develop and experience CWP compared to those with secure attachment. This interpretation would be consistent with previous empirical findings that insecure adult attachment is associated with factors implicated in the development of chronic pain, including with lower pain thresholds, less pain control, more pain-related fear, hypervigilance to pain, catastrophising about pain, even among pain-free individuals [23,27]. From the data, however, we cannot rule out the possibility that reporting insecure attachment simply reflects current pain state.
In conclusion, this study further highlights the importance of insecure adult attachment in possibly contributing to the development of chronic pain among pain-free individuals and in contributing to worse pain experience in those affected by CWP. Further research is now required to investigate the importance of adult attachment among other pain groups from other settings, and to develop novel interventions to promote more effective treatment among individuals with pain who have an insecure adult attachment style.
Acknowledgements
We would like to thank the staff and patients at the general practices involved in the study. This study was funded by the Arthritis Research Campaign, Grant Number: 17552. The authors declare no conflicts of interest.
References
- 1.Bartholomew K., Horowitz L.M. Attachment styles among young adults: a test of a four-category model. J Pers Soc Psychol. 1991;61:226–244. doi: 10.1037//0022-3514.61.2.226. [DOI] [PubMed] [Google Scholar]
- 2.Bifulco A., Moran P.M., Ball C., Lillie A. Adult attachment style. II. Its relationship to psychosocial depressive-vulnerability. Soc Psychiatry Psychiatr Epidemiol. 2002;37:60–67. doi: 10.1007/s127-002-8216-x. [DOI] [PubMed] [Google Scholar]
- 3.Boisset-Pioro M.H., Esdaile J.M., Fitzcharles M.A. Sexual and physical abuse in women with fibromyalgia syndrome. Arthritis Rheum. 1995;38:235–241. doi: 10.1002/art.1780380212. [DOI] [PubMed] [Google Scholar]
- 4.Bowlby J. Basic Books; New York: 1982. Attachment and loss, vol. 1. [Google Scholar]
- 5.Buss C., Lord C., Wadiwalla M., Hellhammer D.H., Lupien S.J., Meaney M.J., Pruessner J.C. Maternal care modulates the relationship between prenatal risk and hippocampal volume in women but not in men. J Neurosci. 2007;27:2592–2595. doi: 10.1523/JNEUROSCI.3252-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ciechanowski P., Sullivan M., Jensen M., Romano J., Summers H. The relationship of attachment style to depression, catastrophizing and health care utilization in patients with chronic pain. Pain. 2003;104:627–637. doi: 10.1016/S0304-3959(03)00120-9. [DOI] [PubMed] [Google Scholar]
- 7.Ciechanowski P.S., Walker E.A., Katon W.J., Russo J.E. Attachment theory: a model for health care utilization and somatization. Psychosom Med. 2002;64:660–667. doi: 10.1097/01.psy.0000021948.90613.76. [DOI] [PubMed] [Google Scholar]
- 8.Ciechanowski P.S., Worley L.L., Russo J.E., Katon W.J. Using relationship styles based on attachment theory to improve understanding of specialty choice in medicine. BMC Med Educ. 2006;6:3. doi: 10.1186/1472-6920-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connan F., Campbell I.C., Katzman M., Lightman S.L., Treasure J. A neurodevelopmental model for anorexia nervosa. Physiol Behav. 2003;79:13–24. doi: 10.1016/s0031-9384(03)00101-x. [DOI] [PubMed] [Google Scholar]
- 10.Croft P.R., Rigby A.S., Boswell R., Schollum J., Silman A.J. The prevalence of chronic widespread pain in the general population. J Rheumatol. 1993;20:710–713. [PubMed] [Google Scholar]
- 11.Davies KA, Silman AJ, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, McBeth J. The association between neighbourhood socio-economic status and the onset of chronic widespread pain. Results from the EPIFUND study. Eur J Pain 2008. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 12.De G.V., Heiser W. Alexithymia and somatisation: quantitative review of the literature. J Psychosom Res. 2003;54:425–434. doi: 10.1016/s0022-3999(02)00467-1. [DOI] [PubMed] [Google Scholar]
- 13.Griffin D., Bartholomew K. Metaphysics of measurement: the case of adult attachment. In: Bartholomew K., Perlman D., editors. Advances in personal relationships. Attachment processes in adulthood, vol. 5. Advance; London: 1994. pp. 17–52. [Google Scholar]
- 14.Gupta A., Silman A.J., Ray D., Morriss R., Dickens C., Macfarlane G.J., Chiu Y.H., Nicholl B., McBeth J. The role of psychosocial factors in predicting the onset of chronic widespread pain: results from a prospective population-based study. Rheumatology (Oxford) 2007;46:666–671. doi: 10.1093/rheumatology/kel363. [DOI] [PubMed] [Google Scholar]
- 15.Heim C., Nemeroff C.B. The impact of early adverse experiences on brain systems involved in the pathophysiology of anxiety and affective disorders. Biol Psychiatry. 1999;46:1509–1522. doi: 10.1016/s0006-3223(99)00224-3. [DOI] [PubMed] [Google Scholar]
- 16.Hunt I.M., Silman A.J., Benjamin S., McBeth J., Macfarlane G.J. The prevalence and associated features of chronic widespread pain in the community using the ‘Manchester’ definition of chronic widespread pain. Rheumatology (Oxford) 1999;38:275–279. doi: 10.1093/rheumatology/38.3.275. [DOI] [PubMed] [Google Scholar]
- 17.Kolb L.C. Attachment behavior and pain complaints. Psychosomatics. 1982;23:413–425. doi: 10.1016/S0033-3182(82)73404-8. [DOI] [PubMed] [Google Scholar]
- 18.MacDonald G., Kingsbury R. Does physical pain augment anxious attachment? J Soc Pers Relat. 2006;23:291–304. [Google Scholar]
- 19.Macfarlane G.J., Croft P.R., Schollum J., Silman A.J. Widespread pain: is an improved classification possible? J Rheumatol. 1996;23:1628–1632. [PubMed] [Google Scholar]
- 20.McBeth J., Chiu Y.H., Silman A.J., Ray D., Morriss R., Dickens C., Gupta A., Macfarlane G.J. Hypothalamic–pituitary–adrenal stress axis function and the relationship with chronic widespread pain and its antecedents. Arthritis Res Ther. 2005;7:R992–R1000. doi: 10.1186/ar1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McBeth J., Macfarlane G.J., Benjamin S., Silman A.J. Features of somatization predict the onset of chronic widespread pain: results of a large population-based study. Arthritis Rheum. 2001;44:940–946. doi: 10.1002/1529-0131(200104)44:4<940::AID-ANR151>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 22.McBeth J., Silman A.J., Gupta A., Chiu Y.H., Ray D., Morriss R., Dickens C., King Y., Macfarlane G.J. Moderation of psychosocial risk factors through dysfunction of the hypothalamic–pituitary–adrenal stress axis in the onset of chronic widespread musculoskeletal pain: findings of a population-based prospective cohort study. Arthritis Rheum. 2007;56:360–371. doi: 10.1002/art.22336. [DOI] [PubMed] [Google Scholar]
- 23.McWilliams L.A., Asmundson G.J. The relationship of adult attachment dimensions to pain-related fear, hypervigilance, and catastrophizing. Pain. 2007;127:27–34. doi: 10.1016/j.pain.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 24.McWilliams L.A., Cox B.J., Enns M.W. Impact of adult attachment styles on pain and disability associated with arthritis in a nationally representative sample. Clin J Pain. 2000;16:360–364. doi: 10.1097/00002508-200012000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Meaney M.J., Aitken D.H., van B.C., Bhatnagar S., Sapolsky R.M. Effect of neonatal handling on age-related impairments associated with the hippocampus. Science. 1988;239:766–768. doi: 10.1126/science.3340858. [DOI] [PubMed] [Google Scholar]
- 26.Meredith P., Ownsworth T., Strong J. A review of the evidence linking adult attachment theory and chronic pain: presenting a conceptual model. Clin Psychol Rev. 2008;28:407–429. doi: 10.1016/j.cpr.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 27.Meredith P., Strong J., Feeney J.A. Adult attachment, anxiety, and pain self-efficacy as predictors of pain intensity and disability. Pain. 2006;123:146–154. doi: 10.1016/j.pain.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 28.Meredith P.J., Strong J., Feeney J.A. Evidence of a relationship between adult attachment variables and appraisals of chronic pain. Pain Res Manag. 2005;10:191–200. doi: 10.1155/2005/745650. [DOI] [PubMed] [Google Scholar]
- 29.Meredith P.J., Strong J., Feeney J.A. Adult attachment variables predict depression before and after treatment for chronic pain. Eur J Pain. 2007;11:164–170. doi: 10.1016/j.ejpain.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Mikail S.F., Henderson P.R., Tasca G.A. An interpersonally based model of chronic pain: an application of attachment theory. Clin Psychol Rev. 1994;14:1–16. [Google Scholar]
- 31.Porter L.S., Davis D., Keefe F.J. Attachment and pain: recent findings and future directions. Pain. 2007;128:195–198. doi: 10.1016/j.pain.2007.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quirin M., Pruessner J.C., Kuhl J. HPA system regulation and adult attachment anxiety: individual differences in reactive and awakening cortisol. Psychoneuroendocrinology. 2008;33:581–590. doi: 10.1016/j.psyneuen.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 33.Salmon P., Skaife K., Rhodes J. Abuse, dissociation, and somatization in irritable bowel syndrome: towards an explanatory model. J Behav Med. 2003;26:1–18. doi: 10.1023/a:1021718304633. [DOI] [PubMed] [Google Scholar]
- 34.Sansone R.A., Wiederman M.W., Sansone L.A. Adult somatic preoccupation and its relationship to childhood trauma. Violence Vict. 2001;16:39–47. [PubMed] [Google Scholar]
- 35.Saxe G.N., Chinman G., Berkowitz R., Hall K., Lieberg G., Schwartz J., van der Kolk B.A. Somatization in patients with dissociative disorders. Am J Psychiatry. 1994;151:1329–1334. doi: 10.1176/ajp.151.9.1329. [DOI] [PubMed] [Google Scholar]
- 36.Spertus I.L., Yehuda R., Wong C.M., Halligan S., Seremetis S.V. Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse Negl. 2003;27:1247–1258. doi: 10.1016/j.chiabu.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 37.STATA. Stata reference manual 3.1, College Station, TX: STATA Corporation; 1993.
- 38.Taylor R.E., Mann A.H., White N.J., Goldberg D.P. Attachment style in patients with unexplained physical complaints. Psychol Med. 2000;30:931–941. doi: 10.1017/s0033291799002317. [DOI] [PubMed] [Google Scholar]
- 39.Walker E.A., Katon W.J., Neraas K., Jemelka R.P., Massoth D. Dissociation in women with chronic pelvic pain. Am J Psychiatry. 1992;149:534–537. doi: 10.1176/ajp.149.4.534. [DOI] [PubMed] [Google Scholar]
- 40.Wearden A., Perryman K., Ward V. Adult attachment, reassurance seeking and hypochondriacal concerns in college students. J Health Psychol. 2006;11:877–886. doi: 10.1177/1359105306069086. [DOI] [PubMed] [Google Scholar]
- 41.Wolfe F., Smythe H.A., Yunus M.B., Bennett R., Bombardier C. The American College of Rheumatology 1990 Criteria for the Classification of fibromyalgia. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]