Abstract
BACKGROUND/OBJECTIVE
Brief alcohol counseling is a foremost US prevention priority, but no health-care system has implemented it into routine care. This study evaluated the effectiveness of an electronic clinical reminder for brief alcohol counseling (“reminder”). The specific aims were to (1) determine the prevalence of use of the reminder and (2) evaluate whether use of the reminder was associated with resolution of unhealthy alcohol use at follow-up screening.
METHODS
The reminder was implemented in February 2004 in eight VA clinics where providers routinely used clinical reminders. Patients eligible for this retrospective cohort study screened positive on the AUDIT-C alcohol screening questionnaire (February 2004–April 2006) and had a repeat AUDIT-C during the 1–36 months of follow-up (mean 14.5). Use of the alcohol counseling clinical reminder was measured from secondary electronic data. Resolution of unhealthy alcohol use was defined as screening negative at follow-up with a ≥2-point reduction in AUDIT-C scores. Logistic regression was used to identify adjusted proportions of patients who resolved unhealthy alcohol use among those with and without reminder use.
RESULTS
Among 4,198 participants who screened positive for unhealthy alcohol use, 71% had use of the alcohol counseling clinical reminder documented in their medical records. Adjusted proportions of patients who resolved unhealthy alcohol use were 31% (95% CI 30–33%) and 28% (95% CI 25–30%), respectively, for patients with and without reminder use (p-value = 0.031).
CONCLUSIONS
The brief alcohol counseling clinical reminder was used for a majority of patients with unhealthy alcohol use and associated with a moderate decrease in drinking at follow-up.
KEY WORDS: alcohol drinking, brief alcohol counseling, brief intervention, clinical reminder, implementation
INTRODUCTION
Unhealthy alcohol use is common and associated with substantial morbidity.1 Brief alcohol counseling for primary care patients with unhealthy alcohol use is widely recommended 2 because it reduces drinking3 and has been associated with improved outcomes and decreased costs.4 Based on the preventable burden of unhealthy alcohol use and the cost-effectiveness of brief alcohol counseling, it is ranked the 3rd highest US prevention priority for adults.5
However, to date no health-care system has successfully implemented sustained, routine brief alcohol counseling. Among primary care patients with unhealthy alcohol use, only 20% to 49% of men and 2% to 34% of women report being counseled about drinking,6–9 and patients with more severe unhealthy drinking or alcohol-related medical problems are more likely to report counseling.9–12 Neither alcohol screening alone nor screening and feedback to providers substantially increase rates of brief alcohol counseling.7,13,14
Clinical reminders in electronic medical records (EMR) can increase provision of recommended preventive care,15 and providers at practices that include use of clinical decision support systems are more likely to counsel patients with unhealthy alcohol use than those at practices without.16 However, no study has tested an electronic clinical reminder as a method of implementing brief alcohol counseling in the absence of other systematic interventions.
The Veterans Affairs (VA) Health Care System offers an important opportunity to test a clinical reminder as a method of implementing brief alcohol counseling. Over the last decade, the VA has improved its delivery of preventive care17 and has been recognized as a model for other large health-care systems.18 To support implementation of evidence-based care, clinical reminders in the EMR are commonly used in conjunction with national performance measures linked to financial incentives for the 21 VA network directors.19,20 Using these methods, the VA implemented annual alcohol screening in 2003, resulting in over 90% of all outpatients being screened for unhealthy alcohol use.13
We developed an electronic clinical reminder to encourage providers to offer brief alcohol counseling when their patients screened positive for unhealthy alcohol use. We designed the reminder to mimic implementation of brief alcohol counseling in randomized controlled trials demonstrating its efficacy. Specifically, we designed the reminder to: (1) prompt providers to offer brief alcohol counseling to patients who screened positive for unhealthy alcohol use, (2) educate providers about components of evidence-based brief alcohol counseling, (3) support assessment of alcohol use severity, (4) provide decision support for brief alcohol counseling or referral, and (5) document care into the patient’s EMR. The clinical reminder system in the VA’s EMR is passive, such that a provider must choose to review clinical reminders and then choose a specific reminder from a list of all indicated reminders (i.e., they do not “pop up”). For instance, if a patient screened positive for unhealthy alcohol use, the provider can choose to open and use the alcohol counseling reminder. Use of clinical reminders is variable across VA sites, and the decision to use reminders appears to be related to local clinical culture.17,21
We implemented the alcohol counseling clinical reminder at a multisite VA health-care system without any other provider training or support and observed high rates of use in the first 8 months.22 The aims of this study were to determine: (1) the proportion of patients with unhealthy alcohol use whose providers used the alcohol counseling reminder over a 2-year period and (2) whether use of the reminder was associated with resolution of unhealthy alcohol use at follow-up alcohol screening.
METHODS
Setting, Data Collection and Participants
This retrospective cohort study was conducted at a VA health-care system with eight associated sites spread over 200 miles in the Western US where providers routinely used clinical reminders. The alcohol counseling reminder was activated for all primary care and mental health providers within this health-care system in February 2004. This study relied exclusively on secondary clinical and administrative data extracted for the period between February 2003 and May 2006 from both the study site’s local EMR, where clinical reminder data are stored, and the VA’s national patient care databases, where electronic clinical and administrative data are stored.
Patients were eligible for the study if they: screened positive for unhealthy alcohol use on the Alcohol Use Disorders Identification Test Consumption (AUDIT-C) questionnaire after February 2004 (8,759 of 36,191 screened), had a subsequent AUDIT-C 1–36 months later (4,206/8,759), and had a documented visit during the study (4,198/4,206). Patients seen at multiple sites were assigned to a single site using an algorithm based on where alcohol screening was conducted, clinics most frequently visited, and facility size. This study was conducted with waivers of written informed consent and HIPAA authorization, and approved by the Human Subjects Divisions at both the University of Washington and the study site.
Measures
Unhealthy alcohol use AUDIT-C scores were used to measure unhealthy alcohol use. The AUDIT-C is routinely employed in the VA 13 and identifies the spectrum of unhealthy alcohol use from drinking above recommended limits to meeting diagnostic criteria for alcohol use disorders.23,24 A positive screen for unhealthy alcohol use was defined as ≥3 points for women or ≥4 points for men out of a total of 12 points, based on VA validation studies.23,24 Patients were considered to have resolved unhealthy alcohol use if they screened positive at baseline, but screened negative at follow-up with at least a 2-point reduction in score.
Use of the Alcohol Counseling Clinical Reminder The alcohol counseling clinical reminder was labeled such that, when a provider clicked on a box in the clinical reminder, a data element was sent to the patient’s EMR. Although some of the data elements initially labeled for extraction were edited at the local site, labels on primary components of appropriate follow-up of positive alcohol screening remained intact. Patients were considered to have “use of the alcohol counseling clinical reminder” (or “reminder use”) if their medical record indicated a provider had used the reminder between AUDIT-C assessments to document: (1) advice to reduce drinking below recommended limits, (2) advice to abstain from drinking, (3) referral to addictions treatment or mental health, and/or (4) patient refusal of referral.
Covariates Covariates were selected based on a review of the literature to identify factors associated with both receipt of brief alcohol counseling and changes in drinking.Baseline demographic variables included age, gender, race, marital status, and socio-economic status.10–12,25 Patients who were 50% or more disabled due to military service (“service-connected disability”) received VA care without co-payments, and this status was used as a measure of access to VA care.Severity of unhealthy drinking is associated with receipt of brief alcohol counseling7,9–12 and changes in drinking.25,26 Five measures of severity were derived including AUDIT-C scores,27 formal VA addictions treatment in the year prior to baseline alcohol screening, and three measures based on International Classification of Diseases 9th Edition (ICD-9) codes in the year prior to alcohol screening: (1) any inpatient or outpatient alcohol use disorder, (2) any alcohol-attributable medical diagnosis (e.g., “alcoholic cirrhosis”),5 and (3) any medical condition associated with AUDIT-C scores (liver disease, upper GI bleeding, pancreatitis, fractures, and serious dislocations or injuries).28,29ICD-9 codes for tobacco use disorder (dichotomous) and other illicit drug use (none, 1, or 2 or more classes of drugs) documented in the year prior to alcohol screening were used as measures of other diagnosed substance use disorders.11,25 Inpatient and outpatient ICD-9 codes in the year prior to alcohol screening were used to derive measures of physical and mental health comorbidity. The validated Deyo Comorbidity Index30 measured physical comorbidity. The number of mental health diagnoses was counted and used as a tri-level covariate (0, 1, >1).11,26
Analyses
For Aim 1, we described the proportion of patients who screened positive for unhealthy alcohol use at baseline whose providers used the alcohol counseling clinical reminder and compared patient characteristics across reminder use using chi-square statistics. To determine whether reminder use was associated with resolution of unhealthy alcohol use (Aim 2), we fit unadjusted and adjusted logistic regression models to estimate the odds of resolution associated with reminder use. Both models were adjusted for site in order to account for differences across geographic location; the adjusted model included all measured covariates. Adjusted proportions of patients who resolved unhealthy alcohol use and 95% confidence intervals (CI) were determined using mean values of all covariates in the study sample. All analyses were performed using Stata, version 10.1.31
RESULTS
Overall, 4,198 patients screened positive for unhealthy alcohol use on an initial AUDIT-C and had repeat alcohol screening during follow-up (M = 14.5 months) (Table 1). Use of the alcohol counseling reminder was documented for 71% of patients (n = 2,975) and was more likely for men, those who were single, over 50% disabled due to military service, or had mental health diagnoses (p-values all <0.05). No other measures of alcohol severity, other substance use, or physical comorbidity were associated with reminder use.
Table 1.
Characteristics of Study Sample (N = 4,198)
| Characteristics | N | (%) |
|---|---|---|
| Age category | ||
| <50 | 731 | (17.4) |
| 50–64 | 1,790 | (42.6) |
| ≥65 | 1,677 | (40.0) |
| Female | 246 | (5.9) |
| Race | ||
| American Indian/Alaskan Native | 35 | (0.8) |
| Asian/Pacific Islander | 102 | (2.4) |
| Black | 425 | (10.1) |
| Unknown/missing | 632 | (15) |
| White | 3,004 | (71.6) |
| Marital status | ||
| Married | 2,043 | (48.7) |
| Never married | 578 | (13.8) |
| Separated, divorced, widowed | 1,499 | (35.7) |
| Unknown | 78 | (1.9) |
| ≥50% service connected disability | 850 | (20.3) |
| Diagnosis for tobacco abuse or dependence¥ | 284 | (6.8) |
| Number of drug use disorder diagnoses¥ | ||
| 1 | 87 | (2.1) |
| ≥2 | 30 | (0.7) |
| Diagnosis for alcohol abuse or dependence¥ | 337 | (8.0) |
| One or more alcohol-attributable medical diagnoses (e.g., alcoholic cirrhosis)¥ | 37 | (0.9) |
| One or more medical conditions associated with unhealthy alcohol use (e.g., cirrhosis, not specifically alcohol-attributable)¥ | 280 | (6.7) |
| VA addictions treatment | 96 | (2.3) |
| Mean AUDIT-C score at baseline* (SD) | 5.42 | (2.21) |
| Mean Deyo Index score¥** (SD) | 1.67 | (1.20) |
| Number of mental health diagnoses¥*** | ||
| 1 | 395 | (9.4) |
| ≥2 | 203 | (4.8) |
¥Based on ICD-9 diagnoses or visit dates obtained for the year prior to baseline alcohol screening
*Range 3–12
**Among the 895 patients who had any comorbid diagnoses
***Does not include diagnoses for substance use disorders
On follow-up AUDIT-Cs, 31% of patients resolved unhealthy alcohol use (n = 1,302). The mean decrease in AUDIT-C score was 1.54 (SD = 3.0). The proportion of patients who resolved unhealthy alcohol use differed significantly across all measured covariates except alcohol use disorders, alcohol-attributable medical diagnoses, and the Deyo Comorbidity Index. Younger, female, non-White, single, service-disabled patients and those with more severe unhealthy alcohol use or other substance use and mental health diagnoses were more likely to resolve unhealthy alcohol use (p-values all <0.05).
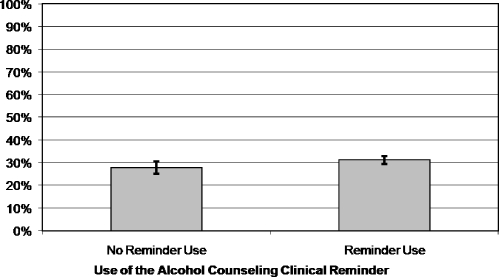
In unadjusted analyses, resolution of unhealthy alcohol use differed significantly between patients with and without reminder use—32% (95% CI 30–34%) and 28% (26–31%; p = 0.011). The mean decrease in AUDIT-C scores from baseline to follow-up among patients with and without reminder use was 1.65 and 1.28, respectively (p = 0.0003). The adjusted odds of resolution of unhealthy alcohol use was 1.18 (95% CI 1.02–1.37; p = 0.031), and adjusted proportions of patients resolving unhealthy alcohol use were 31% (95% CI 30–33%) and 28% (95% CI 25–30%), for those with and without reminder use, respectively (Fig. 1).
Figure 1.
Population-adjusted proportions of patients who resolved unhealthy alcohol use stratified by use of the alcohol counseling clinical reminder.
Because the association was unexpectedly unchanged after adjustment for multiple potential confounders, we evaluated whether factors associated with resolution of unhealthy alcohol use differed for patients with and without reminder use (Table 2). Among patients with no reminder use, resolution of unhealthy alcohol use was associated with tobacco, alcohol, or drug use disorders or alcohol-attributable medical diagnoses. Among patients whose providers used the reminder, these associations were not observed.
Table 2.
Characteristics of the Study Sample Compared Across Resolution of Unhealthy Alcohol Use in Patients with and without Use of the Alcohol Counseling Clinical Reminder
| No use of the clinical reminder (n = 1,223) | Use of the clinical reminder (n = 2,975) | |||||
|---|---|---|---|---|---|---|
| Characteristics | No resolution | Resolution | p-value | No resolution | Resolution | p-value |
| n = 875 (72%) | n = 345 (28%) | n = 2,018 (68%) | n = 957 (32%) | |||
| Age category | <0.001 | <0.001 | ||||
| <50 | 141 (16%) | 82 (24%) | 273 (14%) | 235 (25%) | ||
| 50–64 | 334 (38%) | 153(44%) | 852 (42%) | 451 (47%) | ||
| ≥65 | 403 (46%) | 110 (32%) | 893 (44%) | 271 (28%) | ||
| Female | 61 (7%) | 38 (11%) | 0.019 | 86 (4%) | 61 (6%) | 0.016 |
| Race | 0.023 | <0.001 | ||||
| Unknown | 130 (15%) | 51 (15%) | 317 (16%) | 134 (14%) | ||
| White | 646 (74%) | 233 (68%) | 1,484 (74%) | 641 (67%) | ||
| Black | 78 (9%) | 53 (15%) | 163 (8%) | 131 (14%) | ||
| Asian/Pacific Islander | 17 (2%) | 5 (1%) | 38 (2%) | 42 (4%) | ||
| American Indian/Alaskan Native | 7 (1%) | 3 (1%) | 16 (1%) | 9 (1%) | ||
| Marital status | <0.001 | <0.001 | ||||
| Unknown | 15 (2%) | 4 (1%) | 44 (2%) | 15 (2%) | ||
| Never married | 129 (15%) | 66 (19%) | 241 (12%) | 142 (15%) | ||
| Married | 478 (54%) | 139 (40%) | 1025 (51%) | 401 (42%) | ||
| Separated, divorced, widowed | 256 (29%) | 136 (39%) | 708 (35%) | 399 (42%) | ||
| ≥50% Service connected disability | 147 (17%) | 60 (17%) | 0.785 | 399 (20%) | 244 (26%) | <0.001 |
| Diagnosis for tobacco abuse or dependence¥ | 56 (6%) | 33 (10%) | 0.053 | 125 (6%) | 70 (7%) | 0.249 |
| Number of drug use disorder diagnoses¥ | 0.006 | 0.033 | ||||
| 1 | 13 (1%) | 12 (3%) | 37 (2%) | 25 (3%) | ||
| ≥2 | 4 (0%) | 6 (2%) | 9 (0%) | 11 (1%) | ||
| Diagnosis for alcohol abuse or dependence¥ | 56 (6%) | 35 (10%) | 0.024 | 164 (8%) | 82 (9%) | 0.683 |
| One or more alcohol-attributable medical diagnosis (e.g., alcoholic cirrhosis)¥ | 3 (0%) | 5 (1%) | 0.031 | 21 (1%) | 8 (1%) | 0.596 |
| One or more medical conditions associated with unhealthy alcohol use (e.g., cirrhosis, not specifically alcohol-attributable)¥ | 55 (6%) | 25 (7%) | 0.532 | 123 (6%) | 77 (8%) | 0.047 |
| VA addictions treatment | 11 (1%) | 10 (3%) | 0.046 | 44 (2%) | 31 (3%) | 0.085 |
| Mean AUDIT-C score at baseline* (SD) | 5.09 (2.03) | 5.61 (2.33) | <0.001 | 5.39 (2.19) | 5.73 (2.32) | <0.001 |
| Mean Deyo Index score** (SD) | 1.65 (1.06) | 1.77 (1.34) | 0.4377 | 1.65 (1.18) | 1.71 (1.30) | 0.5832 |
| Number of mental health diagnoses¥*** | <0.001 | <0.001 | ||||
| 1 | 65 (7%) | 28 (8%) | 183 (9%) | 119 (12%) | ||
| ≥2 | 19 (2%) | 25 (7%) | 93 (5%) | 66 (7%) | ||
¥Based on ICD-9 diagnoses or visit dates obtained for the year prior to baseline alcohol screening
*Range 3–12
**Means and SDs were derived for the 603 patients without CR use who had any comorbid diagnoses (n = 432 with no resolution and 171 with resolution) and the 1,488 patients with CR use who had any comorbid diagnoses (n = 1,022 with no resolution and 466 with resolution)
***Does not include diagnoses for substance use disorders
DISCUSSION
This study of VA outpatients from eight sites where providers routinely used clinical reminders found that providers used a passive alcohol counseling clinical reminder for 71% of patients who screened positive for unhealthy alcohol use over a 2-year period. This percentage was consistent with results from the first 8 months after implementation of the reminder 22 and substantially higher than the 28% of VA outpatients with unhealthy alcohol use who reported advice on a national satisfaction survey during the same period.13 Moreover, among patients with unhealthy alcohol use, those who had reminder use were significantly more likely to report having resolved unhealthy alcohol use at follow-up.
Previous studies have demonstrated that patients are more likely to receive brief alcohol counseling if they have more severe unhealthy alcohol use.7,9–12 In contrast, in the present study, there were no significant differences in measures of severity between patients with and without reminder use. Further, factors significantly associated with resolution of unhealthy alcohol use differed for patients with and without reminder use. These findings suggest that the reminder might counteract the inclination of providers to primarily counsel only patients with the most severe unhealthy alcohol use. Although no study has addressed this question for unhealthy alcohol use, a recent review found that use of clinical reminders helps reduce disparities in provision of preventive care across racial/ethnic groups.32
Despite the ability of electronic clinical reminders to improve provision of preventive care for multiple conditions, 15 associations between clinical reminder use and improved patient outcomes have typically been small or undetectable.15,33,34 Similarly, patients in this study whose providers used the alcohol counseling clinical reminder had a modest but significant increase in resolution of unhealthy alcohol use at follow-up compared to patients without reminder use. Randomized controlled trials of brief alcohol counseling have had much larger effects.3
To our knowledge no health-care system has achieved sustained implementation of brief alcohol counseling for patients who screen positive for unhealthy alcohol use,35,36 and implementation research programs have had positive but not sustained impact.37,38 Only one previous study has tested an electronic clinical decision support system as a method of implementing alcohol screening and counseling.39 In that study, the clinical decision support system was coupled with academic detailing, and 51% of screen-positive intervention patients had documented counseling compared to 30% in control clinics.39 Although that rate was substantially higher than in previous implementation efforts without clinical reminders,38,40 it is unknown whether rates of screening and counseling were sustained after study termination. Our finding that 71% of all patients who screened positive for unhealthy alcohol use had use of the alcohol counseling reminder is high relative to previous studies 38–40 and was sustained for 2 years without any other intervention.22 While there was a national VA performance measure for alcohol screening tied to incentives for VA Network Directors, there was no such performance measure for brief alcohol counseling during this study.13,22
The ability of the clinical reminder to move brief alcohol counseling onto the busy clinical agenda for patients irrespective of the severity of unhealthy alcohol use at this VA facility was an important first step toward implementation. However, it is unknown whether these findings will be replicated at VA or non-VA sites where clinical reminder use is not routine. Further, there is no consensus on the “active ingredients” of brief alcohol counseling,22 but advice and feedback offered in an empathetic, patient-centered manner41 are common components of most effective brief alcohol counseling interventions. It is unclear whether providers are prepared to offer effective counseling in the absence of education and coaching, even when prompted.42,43 Trials of brief alcohol counseling with the largest effects4,44 have included in-depth education for providers, often including principles of motivational interviewing.45 Our finding that use of the clinical reminder was associated with modest increases in resolution of unhealthy alcohol use at follow-up screening may reflect that some providers have the necessary skills to offer effective brief alcohol counseling43 or that the actual content of the counseling is less important than the fact that a provider raised the issue of drinking with patients who screen positive.3,46 Additional research is needed to evaluate the quality of counseling offered when reminders are used to prompt providers to counsel patients in real world settings, and to determine educational needs of providers and efficient approaches to meeting them.
This study has several limitations. Findings regarding decreased drinking after brief alcohol counseling could reflect biased reporting by patients. Patients may be more likely to under-report alcohol consumption after they have received brief alcohol counseling. This might be especially true if providers included recommended drinking limits in their counseling as they were prompted to do by the clinical reminder. Further research is needed to establish the validity of changes in alcohol screening scores as a measure of changes in drinking. Despite adjustment for many important covariates, the observed association between reminder use and resolution of unhealthy alcohol use may also reflect bias by indication or residual confounding due to limitations of secondary clinical and administrative measures. In particular, our use of administrative diagnostic data to measure potential confounders likely underestimates prevalence, especially tobacco and other substance use disorders and psychiatric comorbidities.47 Finally, use of a clinical reminder and secondary electronic data to evaluate implementation of brief alcohol counseling has limitations. First, only brief alcohol counseling documented using the clinical reminder is captured. Second, although we labeled elements of the alcohol counseling clinical reminder with unique data elements, clinical reminder labels are editable locally in the VA. Third, although use of merged secondary data allowed us to capture use of the clinical reminder, we were unable to link patients to particular primary care providers or measure provider characteristics. Previous studies have identified considerable variability in use of clinical reminders across providers. 21,48 It is likely that provider characteristics contributed to whether or not, and how, the reminder was used.49,50 Finally, because clinical reminder data are only stored locally in the VA, the evaluation relied on merging local data with national clinical and administrative data, limiting the ability of this study to compare changes in AUDIT-C scores at this site with other sites.
Despite these limitations, this study has noteworthy strengths. It is the first study to our knowledge to evaluate an electronic clinical reminder alone as a method of implementing brief alcohol counseling—in the absence of other systematic interventions. Moreover, we evaluated the clinical reminder in a naturalistic setting among a large population of outpatients from a multi-site health-care system, thereby mitigating the potential for selection or measurement bias due to recruitment of and interaction with providers or patients. Finally, administrative data were used to adjust analyses for five measures of alcohol use severity.
We found that a substantial majority of patients with unhealthy alcohol use had documented use of the alcohol counseling clinical reminder and that rates of use did not differ markedly based on the severity of unhealthy alcohol use. Further, we found that use of the alcohol counseling clinical reminder was associated with significantly greater resolution of unhealthy alcohol use at follow-up screening, even after adjustment for multiple measures of alcohol use severity. These findings support the feasibility of using clinical reminders in EMRs to increase brief alcohol counseling in real-world settings where clinical reminder use is routine. Further research is needed to replicate findings at other sites and to evaluate the quality of counseling, educational needs of providers, and validity of changes in alcohol screening scores as a surrogate outcome after brief alcohol counseling.
Acknowledgements
The clinical reminder evaluated in this study was developed with funding from The Robert Wood Johnson Foundation’s Generalist Physicians Faculty Scholars Program. This study was supported by the Veteran’s Affairs (VA) Substance Use Disorders Quality Enhancement Research Initiative (SUD QuERI) and the VA’s Northwest Center of Excellence for Health Services Research and Development. The authors gratefully acknowledge Haili Sun, PhD, for data extraction and management and Thomas M. Wickizer, PhD, Thomas D. Koepsell, MD, MPH, and Patrick J. Heagerty, PhD, for careful review of and helpful comments on the analytical plan.
Conflict of Interest None disclosed.
Footnotes
The clinical reminder evaluated in this study was developed with funding from The Robert Wood Johnson Foundation’s Generalist Physicians Faculty Scholars Program. This study was supported by the Veteran’s Affairs (VA) Substance Use Disorders Quality Enhancement Research Initiative (SUD QuERI) and the VA’s Northwest Center of Excellence for Health Services Research and Development. Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the University of Washington. Preliminary versions of this work were presented at the 2008 Addiction Health Services Research annual meeting and included in the dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy from the University of Washington (completed by ECW June 2009).
References
- 1.Room R, Babor T, Rehm J. Alcohol and public health. Lancet. 2005;365:519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Preventive Services Task Force Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- 3.Kaner E, Beyer F, Dickinson H, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. 2007:CD004148. [DOI] [PubMed]
- 4.Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res. 2002;26:36–43. [PubMed] [Google Scholar]
- 5.Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse ranking its health impact and cost effectiveness. Am J Prev Med. 2008;34:143–152. doi: 10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- 6.Bradley KA, Epler AJ, Bush KR, Sporleder JL, Dunn CW, Cochran NE, et al. Alcohol-related discussions during general medicine appointments of male VA patients who screen positive for at-risk drinking. J Gen Intern Med. 2002;17:315–326. doi: 10.1046/j.1525-1497.2002.10618.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conigliaro J, Lofgren RP, Hanusa BH. Screening for problem drinking: impact on physician behavior and patient drinking habits. J Gen Intern Med. 1998;13:251–256. doi: 10.1046/j.1525-1497.1998.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richmond R, Kehoe L, Heather N, Wodak A, Webster I. General practitioners’ promotion of healthy life styles: what patients think. Aust NZ J Public Health. 1996;20:195–200. doi: 10.1111/j.1753-6405.1996.tb01818.x. [DOI] [PubMed] [Google Scholar]
- 9.Volk RJ, Steinbauer JR, Cantor SB. Patient factors influencing variation in the use of preventive interventions for alcohol abuse by primary care physicians. J Stud Alcohol. 1996;57:203–209. doi: 10.15288/jsa.1996.57.203. [DOI] [PubMed] [Google Scholar]
- 10.Kaner EFS, Heather N, Brodie J, Lock CA, McAvoy BR. Patient and practitioner characteristics predict brief alcohol intervention in primary care. Br J Gen Pract. 2001;51:822–827. [PMC free article] [PubMed] [Google Scholar]
- 11.Burman ML, Kivlahan DR, Buchbinder MB, Broglio K, Zhou XH, Merrill JO, et al. Alcohol-related advice for VA primary care patients: who gets it, who gives it? J Stud Alc. 2004;65:621–630. doi: 10.15288/jsa.2004.65.621. [DOI] [PubMed] [Google Scholar]
- 12.Arndt S, Schultz SK, Turvey C, Petersen A. Screening for alcoholism in the primary care setting: are we talking to the right people? J Fam Pract. 2002;51:41–46. [PubMed] [Google Scholar]
- 13.Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Manag Care. 2006;12:597–606. [PubMed] [Google Scholar]
- 14.Saitz R, Horton NJ, Sullivan LM, Moskowitz MA, Samet JH. Addressing alcohol problems in primary care: a cluster randomized, controlled trial of a systems intervention. The screening and intervention in primary care (SIP) study. Ann Intern Med. 2003;138:372–382. doi: 10.7326/0003-4819-138-5-200303040-00006. [DOI] [PubMed] [Google Scholar]
- 15.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. Jama. 2005;293:1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 16.Hung DY, Rundall TG, Tallia AF, Cohen DJ, Halpin HA, Crabtree BF. Rethinking prevention in primary care: applying the chronic care model to address health risk behaviors. Milbank Q. 2007;85:69–91. doi: 10.1111/j.1468-0009.2007.00477.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kerr EA, Fleming B. Making performance indicators work: experiences of US Veterans Health Administration. BMJ. 2007;335:971–973. doi: 10.1136/bmj.39358.498889.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oliver A. Public-sector health-care reforms that work? A case study of the US Veterans Health Administration. Lancet. 2008;371:1211–1213. doi: 10.1016/S0140-6736(08)60528-0. [DOI] [PubMed] [Google Scholar]
- 19.Kizer KW, Dudley RA. Extreme makeover: transformation of the veterans health care system. Annu Rev Public Health. 2009;30:313–339. doi: 10.1146/annurev.publhealth.29.020907.090940. [DOI] [PubMed] [Google Scholar]
- 20.Fung CH, Woods JN, Asch SM, Glassman P, Doebbeling BN. Variation in implementation and use of computerized clinical reminders in an integrated healthcare system. Am J Manag Care. 2004;10:878–885. [PubMed] [Google Scholar]
- 21.Saleem JJ, Patterson ES, Militello L, Render ML, Orshansky G, Asch SM. Exploring barriers and facilitators to the use of computerized clinical reminders. J Am Med Inform Assoc. 2005;12:438–447. doi: 10.1197/jamia.M1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bradley KA, Williams EC, Achtmeyer CE, Hawkins EJ, Harris AH, Frey MS, et al. Measuring performance of brief alcohol counseling in medical settings:a review of the options and lessons from the Veterans Affairs (VA) health care system. Subst Abus. 2007;28:133–149. doi: 10.1300/J465v28n04_05. [DOI] [PubMed] [Google Scholar]
- 23.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol use disorders identification test. Arch Intern Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 24.Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, et al. Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163:821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- 25.Matzger H, Delucchi K, Weisner C, Ammon L. Does marital status predict long-term drinking? Five-year observations of dependent and problem drinkers. J Stud Alcohol. 2004;65:255–265. doi: 10.15288/jsa.2004.65.255. [DOI] [PubMed] [Google Scholar]
- 26.Weisner C, Matzger H, Kaskutas LA. How important is treatment? One-year outcomes of treated and untreated alcohol-dependent individuals. Addiction. 2003;98:901–911. doi: 10.1046/j.1360-0443.2003.00438.x. [DOI] [PubMed] [Google Scholar]
- 27.Bradley KA, Kivlahan DR, Zhou XH, Sporleder JL, Epler AJ, McCormick KA, et al. Using alcohol screening results and treatment history to assess the severity of at-risk drinking in Veterans Affairs primary care patients. Alcohol Clin Exp Res. 2004;28:448–455. doi: 10.1097/01.ALC.0000117836.38108.38. [DOI] [PubMed] [Google Scholar]
- 28.Au DH, Kivlahan DR, Bryson CL, Blough D, Bradley KA. Alcohol screening scores and risk of hospitalizations for GI conditions in men. Alcohol Clin Exp Res. 2007;31:443–451. doi: 10.1111/j.1530-0277.2006.00325.x. [DOI] [PubMed] [Google Scholar]
- 29.Harris AH, Bryson CL, Sun H, Blough D, Bradley KA. Alcohol screening scores predict risk of subsequent fractures. Subst Use Misuse. 2009;44:1055–1069. doi: 10.1080/10826080802485972. [DOI] [PubMed] [Google Scholar]
- 30.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 31.StataCorp. Stata Statistical Software: Release Special Edition 10.1. College Station TX: Stata Corporation 2007.
- 32.Beach MC, Gary TL, Price EG, Robinson K, Gozu A, Palacio A, et al. Improving health care quality for racial/ethnic minorities: a systematic review of the best evidence regarding provider and organization interventions. BMC Public Health. 2006;6:104. doi: 10.1186/1471-2458-6-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnston ME, Langton KB, Haynes RB, Mathieu A. Effects of computer-based clinical decision support systems on clinician performance and patient outcome. A critical appraisal of research. Ann Intern Med. 1994;120:135–142. doi: 10.7326/0003-4819-120-2-199401150-00007. [DOI] [PubMed] [Google Scholar]
- 34.Dexheimer JW, Talbot TR, Sanders DL, Rosenbloom ST, Aronsky D. Prompting clinicians about preventive care measures: a systematic review of randomized controlled trials. J Am Med Inform Assoc. 2008;15:311–320. doi: 10.1197/jamia.M2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nilsen P, Aalto M, Bendtsen P, Seppa K. Effectiveness of strategies to implement brief alcohol intervention in primary healthcare. A systematic review. Scand J Prim Health Care. 2006;24:5–15. doi: 10.1080/02813430500475282. [DOI] [PubMed] [Google Scholar]
- 36.Kuehn BM. Despite benefit, physicians slow to offer brief advice on harmful alcohol use. JAMA. 2008;299:751–753. doi: 10.1001/jama.299.7.751. [DOI] [PubMed] [Google Scholar]
- 37.Kaner EF, Wutzke S, Saunders JB, Powell A, Morawski J, Bouix JC. Impact of alcohol education and training on general practitioners’ diagnostic and management skills: findings from a World Health Organization collaborative study. J Stud Alcohol. 2001;62:621–627. doi: 10.15288/jsa.2001.62.621. [DOI] [PubMed] [Google Scholar]
- 38.Babor TF, Higgins-Biddle JC. Cutting back (R): Managed care screening and brief intervention for risky drinking. The Robert Wood Johnson Foundation. 2004. Available at: http://www.rwjf.org/reports/npreports/cuttingback.htm. Accessed August 10, 2009.
- 39.Rose HL, Miller PM, Nemeth LS, Jenkins RG, Nietert PJ, Wessell AM, et al. Alcohol screening and brief counseling in a primary care hypertensive population: a quality improvement intervention. Addiction. 2008;103:1271–1280. doi: 10.1111/j.1360-0443.2008.02199.x. [DOI] [PubMed] [Google Scholar]
- 40.Anderson P, Kaner E, Wutzke S, Funk M, Heather N, Wensing M, et al. Attitudes and managing alcohol problems in general practice: an interaction analysis based on findings from a WHO collaborative study. Alcohol Alcohol. 2004;39:351–356. doi: 10.1093/alcalc/agh072. [DOI] [PubMed] [Google Scholar]
- 41.Samet JH, Rollnick S, Barnes H. Beyond CAGE. A brief clinical approach after detection of substance abuse. Arch Intern Med. 1996;156:2287–2293. doi: 10.1001/archinte.156.20.2287. [DOI] [PubMed] [Google Scholar]
- 42.Beich A, Gannik D, Malterud K. Screening and brief intervention for excessive alcohol use: qualitative interview study of the experiences of general practitioners. BMJ. 2002;325:1–5. doi: 10.1136/bmj.325.7369.870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McCormick KA, Cochran NE, Back AL, Merrill JO, Williams EC, Bradley KA. How primary care providers talk to patients about alcohol: a qualitative study. J Gen Intern Med. 2006;21:966–972. doi: 10.1007/BF02743146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ockene J, Adams A, Hurley T, Wheeler E, Hebert J. Brief physician- and nurse practitioner-delivered counseling for high-risk drinkers: does it work? Arch Intern Med. 1999;159:2198–2205. doi: 10.1001/archinte.159.18.2198. [DOI] [PubMed] [Google Scholar]
- 45.Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–283. doi: 10.1007/s11606-006-5063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miller WR. Rediscovering fire: small interventions, large effects. Psychol Addict Behav. 2000;14:6–18. doi: 10.1037/0893-164X.14.1.6. [DOI] [PubMed] [Google Scholar]
- 47.Hamlett-Berry K, Davison J, Kivlahan DR, Matthews MH, Hendrickson JE, Almenoff PL. Evidence-based national initiatives to address tobacco use as a public health priority in the Veterans Health Administration. Mil Med. 2009;174:29–34. doi: 10.7205/milmed-d-00-3108. [DOI] [PubMed] [Google Scholar]
- 48.Patterson ES, Nguyen AD, Halloran JP, Asch SM. Human factors barriers to the effective use of ten HIV clinical reminders. J Am Med Inform Assoc. 2004;11:50–59. doi: 10.1197/jamia.M1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schellhase KG, Koepsell TD, Norris TE. Providers’ reactions to an automated health maintenance reminder system incorporated into the patient’s electronic medical record. J Am Board Fam Pract. 2003;16:312–317. doi: 10.3122/jabfm.16.4.312. [DOI] [PubMed] [Google Scholar]
- 50.Mayo-Smith MF, Agrawal A. Factors associated with improved completion of computerized clinical reminders across a large healthcare system. Int J Med Inform. 2007;76:710–716. doi: 10.1016/j.ijmedinf.2006.07.003. [DOI] [PubMed] [Google Scholar]