Abstract
BACKGROUND
Smoking cessation services in the Department of Veterans Affairs (VA) are currently provided via outpatient groups, while inpatient cessation programs have not been widely implemented.
OBJECTIVE
The objective of this paper is to describe the implementation of the Tobacco Tactics program for inpatients in the VA.
METHODS
This is a pre-/post-non-randomized control study initially designed to teach inpatient staff nurses on general medical units in the Ann Arbor and Detroit VAs to deliver the Tobacco Tactics intervention using Indianapolis as a control group. Coupled with cessation medication sign-off, physicians are reminded to give patients brief advice to quit.
RESULTS
Approximately 96% (210/219) of inpatient nurses in the Ann Arbor, MI site and 57% (159/279) in the Detroit, MI site have been trained, with an additional 282 non-targeted personnel spontaneously attending. Nurses’ self-reported administration of cessation services increased from 57% pre-training to 86% post-training (p = 0.0002). Physician advice to quit smoking ranged between 73–85% in both the pre-intervention and post-intervention period in both the experimental and control group. Volunteers made follow-up telephone calls to 85% (n = 230) of participants in the Ann Arbor site. Hospitalized smokers (N = 294) in the intervention group are reporting an increase in receiving and satisfaction with the selected cessation services following implementation of the program, particularly in regards to medications (p < 0.05).
CONCLUSION
A large proportion of inpatient nursing staff can rapidly be trained to deliver tobacco cessation interventions to inpatients resulting in increased provision of services.
KEY WORDS: implementation research, smoking cessation, veterans
BACKGROUND
Smokers have an increased risk of morbidity and mortality resulting in twice as many hospital stays, longer hospital stays, and greater expenses per admission than nonsmokers.1 Although smoking rates among veterans have decreased from 33% to 22.2% in recent years,2,3 smoking remains a problem in the Department of Veterans Affairs (VA), particularly in Veterans Integrated Service Network (VISN) 11, where 28.2% are current smokers compared to 20.9% of the general population.3 Inpatient smoking programs are efficacious 4 and have a high reach as they capitalize on a teachable moment, take advantage of cessation induced by hospital smoking bans, enroll a higher percentage of patients who smoke, and result in higher cessation rates.5 Although randomized clinical trials show the potential effectiveness of inpatient smoking cessation programs in VA hospitals,6,7 standard cessation services in the VA are currently provided in accordance with clinical guidelines8,9 via outpatient groups, which tend to be poorly attended.10
A large gap exists between the availability of effective smoking cessation interventions and their widespread dissemination and implementation in hospital settings including the VA.11 The challenge rests with incorporating smoking cessation interventions into standard practice.12 Our prior work13 has shown that 70% of inpatient smokers in the VA were motivated to quit, yet only 17% stated that they received some type of cessation services during their hospitalization. Most staff said the VA should be doing more to assist patients to quit, yet less than half said that they provided cessation services primarily due to lack of confidence/training and hesitancy to upset patients. Since the evidence for smoking cessation in clinical trials is strong, including a trial conducted by our team among outpatient smokers at the VA,14 this study was designed to implement and evaluate the efficacious Tobacco Tactics program for inpatient smokers in the VA.
Often conducted as a form of quality improvement, implementation research evaluates the use of strategies to introduce or change evidence-based health interventions within specific settings. VA/Health Services Research & Development (HSR&D) Quality Enhancement Research Initiative (QUERI) works to improve the quality of health care for veterans by implementing research findings into routine clinical practice. Within QUERI, there is less focus on summative (outcome) evaluation, with a greater focus on formative (process) evaluation or “how” the intervention was implemented in the real world setting.15 Formative evaluation includes rigorous assessment designed to identify potential and actual influences on the progress and effectiveness of implementation efforts16 utilizing collaborations with stakeholders and findings, methods, and theories from a variety of fields.17 Using the Precede-Proceed planning model as a guide for formative evaluation,18 this paper describes the implementation of the Tobacco Tactics program in the VA.
METHODS
Design
This implementation study used a pre-/post-intervention, non-randomized control design to teach inpatient staff nurses on general medical units in two VAs to deliver the Tobacco Tactics intervention using a third VA as a control group. Human studies approval was received from all sites. Since summative (outcome) evaluation remains in progress, quit rates are not presented in this manuscript. Instead, this paper focuses on the formative evaluation of the implementation of the Tobacco Tactics intervention drawing on both quantitative and qualitative data from a variety of sources.
Setting and Sample
Ann Arbor and Detroit are the intervention sites, and Indianapolis is the control site. None of the three hospitals has standardized cessation inpatient interventions, although each provides outpatient groups. Eligible units were general medical, surgical, intensive care, and extended care units. Together these units admit over 800 smokers per year. Psychiatric, substance abuse, and outpatient units were initially excluded because of concerns that smoking cessation may lead to exacerbation of symptoms and could result in problematic side effects, such as anxiety and depression.19
Procedures
Patients were surveyed about the tobacco cessation services received and satisfaction with these services in both the pre- and post-intervention period in both the experimental and control sites. Once pre-intervention data had been collected, the goal was to train all inpatient nurses (about 500) on the eligible units in the two experimental hospitals to administer the efficacious Tobacco Tactics intervention. The Cochrane Collaboration’s Effective Practice and Organization of Care Group found that interventions that are more active, such as educational outreach, train-the-trainer models, and the use of opinion leaders, were effective in changing health-care provider behavior.20 Hence, the plan was for research nurses in Ann Arbor and Detroit to work with each unit for approximately 2 months by role modeling the intervention and teaching the intervention to nurses using short educational sessions given at shift report. Starting on one unit and then moving to successive units allows for pilot testing and gradual change before wide-spread diffusion is undertaken. As research nurses gradually transfer the intervention over to the staff nurses, they continue to collect informal and formal feedback from patients and staff about barriers and facilitators to implementing the intervention, and changes are made to facilitate implementation. Opinion leaders serving as change agents included clinical nurse managers who were in support of the intervention as they needed to meet VA tobacco performance measures and nurse champions on the units who could use leadership in bringing the Tobacco Tactics intervention forward on their units as a criterion for promotion. Volunteers were trained to provide the post-discharge follow-up calls to patients in the Ann Arbor site.
Intervention
Nurse Level Intervention The Tobacco Tactics nurse toolkit includes: (1) one contact hour for training; (2) a PowerPoint presentation on behavioral and pharmaceutical interventions; (3) a pocket card “Helping Smokers Quit: A Guide for Clinicians” developed by the US Department of Health and Human Services Public Health Service21 and Tobacco-Free Nurses; (4) pharmaceutical and behavioral protocols; (5) a computerized template for nurse documentation.
Patient Level Intervention The Tobacco Tactics intervention is based on an efficacious intervention tested by our team,14 which incorporates the Agency for Healthcare Research and Quality (AHRQ) recommendations for treatment of smoking and tailors the intervention to the patient’s medical condition and lifestyle. The patient toolkit includes: (1) a smoking cessation brochure (Tips for Quitting Smoking); (2) the videotape “Smoking: Getting Ready to Quit”22; (3) Tobacco Tactics manual; (4) pharmaceuticals; (5) follow-up telephone calls; (6) the 1–800-QUIT-NOW help line.23 Providing the brochure, videotape, and manual in advance of cessation counseling saves the nurses’ time at the bedside.The patient reviews the videotape on their own (shown twice daily on the overhead television at breakfast and dinner time and also available on the unit portable VCR) and meets with the staff nurses for 10–20 min for cessation counseling. This counseling can be broken into smaller units (e.g. four 5-mi sessions) and conducted while providing routine care. A pharmaceutical protocol was developed, which is initiated by the nurse and solidified by the physician. See Appendix A and Appendix B for an outline of the behavioral and pharmaceutical protocols.
Physician Level Intervention Brief physician advice can be difficult to implement due to the high demands and monthly turnover of residents in many academic VA systems. While we considered physician reminders for brief advice, physicians told us they were inundated with reminders, and they were likely to be ignored. Hence, we chose to couple a reminder for brief advice as part of the smoking medication sign-off that had to be completed by a physician; this allowed for physician coaching without adding additional computerized reminders.
Volunteer Telephone Follow-Up Calls Studies, including a recent VA study, have shown that telephone counseling is efficacious to reinforce the initial intervention visit, promote skills building, and monitor pharmacologic treatment.24–26 In our pre-intervention assessment, we explored the possibility of nurse case managers providing the follow-up telephone counseling, but nurse case managers were clear that they would not have time to make follow-up calls. Hence, we are conducting a pilot study at the Ann Arbor VA that trains selected volunteers to provide telephone follow-up peer support to patients at 2, 14, 21, and 60 days post-discharge.Two dedicated non-smoking volunteers hand-picked by the volunteer coordinator were trained in cessation telephone counseling. Volunteer training consisted of: (1) participating in the 1-h Tobacco Tactics training program, (2) viewing the video shown to patients about smoking cessation, and (3) viewing a video about peer support that has been used in other studies.27 The staff supervised each volunteer while making phone calls until they were comfortable and followed the protocol appropriately. Volunteers were also given a back-up telephone number to provide veterans who need more in-depth medical attention. Documentation is a paper check list with prompts for counseling. Since volunteers are not able to access patient records, documentation is entered into the system by a patient health educator.
Measures
Staff Survey Staff nurses were surveyed about the Tobacco Tactics training and implementation at the VA approximately 1 month after they received the training. Survey questions rated on a 5-pont scale included: (1) confidence in abilities to provide tobacco cessation services; (2) perceived level of importance of providing services; (3) satisfaction with the material presented; (4) perception of understanding the elements of the smoking cessation intervention. Nurses were also asked: (1) if they personally provided smoking cessation services to veterans (yes/no); (2) anticipated barriers to implementation (yes/no and open-ended); (3) “is there anything that would make it easier for you to implement the smoking cessation intervention in your unit?” (open-ended).
Performance Measures For this study, the VA performance measures for smokers hospitalized with acute myocardial infarction (AMI) and heart failure were tracked. These percentages are calculated by number of patients (cigarette smokers) who receive smoking cessation advice or counseling during the hospital stay (numerator) divided by the number of patients with a history of smoking cigarettes anytime during the year prior to hospital arrival (denominator).28 These performance measures are calculated by the VA and made available on the VA intranet.
Patient Surveys To determine the provision of cessation services during their recent hospitalization in both the pre- and post-intervention period, inpatient smokers in the experimental and control sites were surveyed 6 months post-discharge. Survey questions asked whether or not (yes/no) they received a variety of tobacco cessation services including nicotine replacement therapy, other medications, hand-out materials, informational video, or follow-up telephone calls. Additional questions asked about patient satisfaction with the tobacco cessation services rated on a scale of 1 to 5 ranging from not satisfied to extremely satisfied.
Data Analysis
Frequencies were examined for all variables. Chi-square tests were used to examine nurse report of provision of smoking cessation services. For data of patient report of receipt or satisfaction with smoking cessation services, frequencies were examined by experimental vs. control group, and pre- vs. post-intervention period of the Tobacco Tactics program. Satisfaction was recategorized into a dichotomous variable of ‘extremely/somewhat satisfied’ versus ‘neutral/somewhat/extremely not satisfied.’ Bivariate analyses, comparing pre- vs. post-intervention patient receipt of or satisfaction with smoking cessation services, were conducted using chi-square or Fisher’s Exact tests.
Since all of the respondents did not answer all of the questions, the sample size varied for different results. Those with missing data for a particular question were not included in the analysis. Values for P < 0.05 were considered significant.
RESULTS
Changes in Implementation Strategy
Throughout the implementation process, the research team collected suggestions and feedback from nurses and key stakeholders regarding barriers and facilitators to the Tobacco Tactics intervention allowing for changes to be made to the initial implementation strategy. While the initial plan, developed with input from nurses and leadership, was to train one unit at a time, this was not successful as only a few nurses could be released for training at a time and it interfered with unit flow. Hence, the strategy was changed to offer rolling trainings across all shifts and unit managers from all units released a few staff at a time. These training sessions were initially poorly attended (two to three nurses per session). However, continuing to work with unit managers and advertising in newsletters increased participation rates by approximately 20–30 nurses per session. Advertisements also brought nurses from units not targeted (psychiatric, substance abuse, and outlying Community Based Outpatient Clinics) as well as non-nurses (such as physicians, social workers, nursing assistants, etc.). Since our goal was dissemination, no one was turned away from the training sessions.
Changes in Target Population
We initially intended to target the intensive care units (ICUs), but the Human Studies Committee felt that ICUs were inappropriate for this intervention. However, once the training started, ICU nurses requested inclusion citing that there were smokers on these units with whom they could initiate the intervention. Hence, we appealed to the Human Studies Committee, which reconsidered the evidence and allowed ICUs to participate.
Likewise, psychiatric and substance abuse units requested inclusion as they house a large number of smokers. Moreover, these units were facing problems with their patients being confined for the first 3 days after admission and not being able to smoke, resulting in agitation. Based on their request, we obtained Human Studies approval to include these units and actually worked with them first so as to respond to their plea for immediate assistance.
Staff Participation Rates
In Ann Arbor, 353 staff including 96% (210/219) of targeted inpatient RN and LPN staff nurses have been trained. The Detroit intervention site had less participation with 298 staff, including 57% (159/279) of targeted inpatient RN and LPN nurses trained. Across both sites, 282 additional, non-targeted providers participated in the training, including mostly outpatient nurses (n = 92), inpatient non-targeted nurses (e.g., graduate nurse technician, student nurse technician) (n = 71), nursing assistants (n = 45), physicians (n = 29), social workers (n = 11), respiratory therapists (n = 5), and others (e.g., students/residents, research, quality management, education, occupational therapy, and physician assistant) (n = 29).
Staff Response to Training
Post-training surveys showed that 60% of staff felt very or extremely confident about providing cessation services, 86% felt providing cessation services was important or very important, 57% were extremely satisfied with the training, and 89% felt they had an understanding of the components of tobacco cessation (see Table 1). Potential barriers identified were patients not interested, not enough staff, lack of time, lack of support from physicians, and difficulty locating resources. Suggestions included designated cessation counselors, planned counseling sessions for patients, making resources available, and improving the documentation template. Prior to implementing the Tobacco Tactics intervention, 57.1% (N = 40) of nurses surveyed reported that they provided smoking cessation services compared to 85.7% (N = 60) post-intervention (P = 0.0002).
Table 1.
Nurse Responses after Tobacco Tactics Training
| n | Percent | |
|---|---|---|
| How confident are you in your abilities to provide smoking cessation services to inpatient smokers? (N = 144) | ||
| Extremely confident | 23 | 16.0 |
| Very confident | 64 | 44.4 |
| Moderately confident | 49 | 34.0 |
| Somewhat/not at all confident | 8 | 5.6 |
| How important do you think it is to provide the Smoking Cessation Intervention in your unit? (N = 143) | ||
| Very important | 66 | 46.2 |
| Important | 57 | 39.9 |
| Neutral | 17 | 11.9 |
| Not very/not at all important | 3 | 2.1 |
| How satisfied were you with the material presented? (N = 145) | ||
| Extremely satisfied | 83 | 57.2 |
| Somewhat satisfied | 47 | 32.4 |
| Neutral/undecided | 9 | 6.2 |
| Somewhat/extremely dissatisfied | 6 | 4.2 |
| Do you feel you have a good understanding of the elements of the Smoking Cessation Intervention? (N = 145) | ||
| Strongly agree | 41 | 28.3 |
| Agree | 88 | 60.7 |
| Neutral | 13 | 9.0 |
| Disagree | 3 | 2.1 |
| Do you foresee any barriers to implementing this intervention? (N = 143) | ||
| Yes | 104 | 72.7 |
| No | 39 | 27.3 |
| If yes, what are these possible barriers? (N = 104) | ||
| Patients not interested | 67 | 64.4 |
| Not enough time | 60 | 57.7 |
| Not enough staff | 31 | 29.8 |
| Other (N = 39) | ||
| Patient condition not appropriate for teaching | 13 | 33.3 |
| Lack of support from physicians | 7 | 17.9 |
| Difficulty locating resources | 11 | 28.2 |
| Difficulty using the computerized patient records system template | 3 | 7.7 |
| Is there anything that would make it easier for you to implement the Smoking Cessation Intervention in your unit? (N = 45) | ||
| Designate key personal to perform or coordinate smoking cessation interventions | 10 | 22.2 |
| Designate planned sessions for counseling | 5 | 11.1 |
| Have resources readily available | 5 | 11.1 |
| Make the documentation template for smoking cessation more user-friendly | 3 | 6.7 |
Physician Support
To alleviate nurses’ concerns about lack of physician support, residents were given a brief (less than 5-min) overview of the program along with the medication algorithm during orientation. Anecdotally, physicians told us they were glad that additional services were being considered for veterans who smoke. Physician advice to quit smoking (as reported by patients on their 6-month surveys) was high in both the pre-intervention and post-intervention period in both the experimental and control group ranging between 73–85%.
Volunteer Follow-up Calls
In the Ann Arbor site only, two volunteers made 1,776 attempts (no more than 3 attempts per time point) to reach 270 patients, of which 85% were reached at least once. An average of two follow-up calls per patient were made to 230 patients for a total of 552 patient contacts. Volunteers are extremely enthusiastic about having the opportunity to provide cessation follow-up calls “rather than folding brochures,” as they really want to “make a difference in the lives of veterans.”
Use of Materials
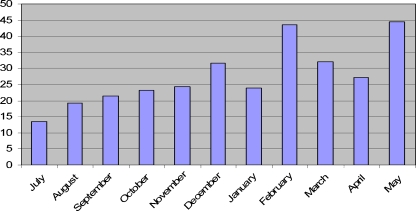
As more nurses were trained, the number of Tobacco Tactics manuals used on the units steadily increased, as shown in Fig. 1. Units where materials were stagnating were given extra attention. The piece of the patient toolkit that is used the most (taken by patients and visitors) is the plastic 1–800-QUIT-NOW card, which connects smokers with the state-supported quit line.
Figure 1.
Tobacco Tactics Manuals used by month during the intervention period in the Ann Arbor VA, July 2007-May 2008.
Performance Measures
Counseling to quit smoking in patients admitted for heart failure in Ann Arbor over the intervention period improved from 43% to 80–100% from quarter 4 2007 to quarter 2 2009. Counseling to quit smoking in patients admitted for heart attack in Ann Arbor over the same period improved from 88% to 100% from quarter 4 2007 to quarter 2 2009. The Detroit intervention site and Indianapolis site were high throughout.
Patients Report on Cessation Services Received
Thus far, 533 veteran smokers in all three sites returned 6-month surveys for a return rate of 55% (533/970). Smokers surveyed in the intervention sites reported an increase in cessation services provided while in the hospital from pre-intervention to post-intervention (see Table 2). From pre- to post-intervention, there was a 2.5-fold increase in patients in the experimental group reporting receipt of nicotine gum for smoking cessation (P = 0.02) and 2-fold increase in receipt of other medications (P = 0.03).
Table 2.
Patients 6-Month Post-Discharge Description of Tobacco Services Received During Hospitalization Pre- and Post Intervention in Experimental and Control Groups
| Pre-intervention | Post-intervention | ||
|---|---|---|---|
| Experimental = 178 | Experimental = 116 | ||
| Control = 55 | Control = 55 | ||
| N (%) | N (%) | P-value | |
| Received nicotine patch | |||
| Experimental | 65 (37.8) | 44 (41.5) | 0.54 |
| Control | 16 (30.2) | 13 (24.1) | 0.48 |
| Received nicotine gum | |||
| Experimental | 8 (4.8) | 13 (12.4) | 0.02 |
| Control | 4 (7.6) | 6 (11.3) | 0.51 |
| Received other medications to help quit smoking | |||
| Experimental | 20 (11.6) | 22 (21.2) | 0.03 |
| Control | 6 (11.5) | 3 (5.9) | 0.49 |
| Received hand-out materials to help quit smoking | |||
| Experimental | 81 (47.4) | 63 (57.8) | 0.09 |
| Control | 31 (59.6) | 31 (57.4) | 0.82 |
| Received video about quitting smoking | |||
| Experimental | 11 (6.4) | 12 (11.2) | 0.15 |
| Control | 4 (7.6) | 6 (11.3) | 0.51 |
| Received phone calls about quitting smoking after discharge | |||
| Experimental | 15 (8.7) | 12 (11.0) | 0.53 |
| Control | 5 (9.4) | 3 (5.7) | 0.72 |
Bold values represent p < 0.05
Several pre-intervention percentages in the control group were higher than in the experimental groups, and some rates in the control group also increased. Upon closer examination, it was noted that the control site recruited a greater number of psychiatric patients compared to the intervention sites with 45% (150/333) in Indianapolis versus 14% (109/774) in Ann Arbor/Detroit. Due to a hiring freeze, the control site also started later than the intervention sites, resulting in a smaller sample size in the control site.
Patient Satisfaction with Cessation Services Received
Albeit not statistically significant, overall patient satisfaction with the Tobacco Tactics intervention improved by nine percentage points in the experimental group compared to relatively no change in the control group. While the sample sizes were small for many of the satisfaction variables, the trend was in the expected direction for most of the variables except for handout materials and video. There was a significant increase in pre- and post-satisfaction with nicotine patch in the experimental group (p = 0.005) (see Table 3).
Table 3.
Patients 6-Month Post-Discharge Satisfaction with Tobacco Services Received During Hospitalization Pre- and Post Intervention in Experimental and Control Groups
| Pre-intervention | Post-intervention | |
|---|---|---|
| N (%) | N (%) | |
| Satisfied with smoking cessation services in the VA | ||
| Experimental | 99 (57.2) | 72 (66.1) |
| Control | 26 (50.0) | 27 (50.9) |
| Satisfied with nicotine patch | ||
| Experimental | 23 (39.0) | 29 (67.4)* |
| Control | 7 (43.8) | 5 (38.5) |
| Satisfied with nicotine gum | ||
| Experimental | 4 (57.1) | 7 (58.3) |
| Control | 2 (66.7) | 1 (16.7) |
| Satisfied with other medications | ||
| Experimental | 7 (53.9) | 11 (57.9) |
| Control | 5 (83.3) | 1 (50.0) |
| Satisfied with handout materials | ||
| Experimental | 43 (61.4) | 26 (45.6) |
| Control | 16 (59.3) | 15 (55.6) |
| Satisfied with video | ||
| Experimental | 6 (60.0) | 5 (45.5) |
| Control | 2 (50.0) | 3 (60.0) |
| Satisfied with follow-up phone calls | ||
| Experimental | 9 (64.3) | 6 (66.7) |
| Control | 3 (60.0) | 1 (33.3) |
*P = 0.005
Note: Includes only those patients who reported receiving services
Sustainability
The program is now part of orientation for all new nurses. In addition, we are negotiating a booster into the VA Learning Management System (LMS) that provides ongoing continuing education to all VA personnel. Fourteen nurse champions from all of the units will be responsible for sustaining the intervention once the research nurses are withdrawn. Since there was no one person to assume responsibility for the plan, we opted to turn over various components of the intervention to those positions where these components “fit.” Oversight of the program was transferred to the Tobacco Cessation Counselor (a pharmacist) who has 10% full-time equivalent (FTE) for this work. Staff education was turned over to the staff education coordinators, and patient education materials were assigned to Patient Care Services. In this way, no one person had to take on a large amount of duties in addition to their other daily responsibilities.
DISCUSSION
This study shows that a 1-h training for nurses in the Tobacco Tactics intervention can result in high confidence for providing cessation services and increased self report of providing these services. Increased self-confidence in delivering cessation interventions has been shown to be associated with a greater likelihood that cessation interventions will be delivered.29,30 When cessation programs are offered to smokers, cessation rates increase, potentially reducing mortality.31
While there was skepticism from many that nurses could be trained and that cessation services could be integrated into routine care, one of our best measures of success is the higher than anticipated interest and participation that we have received from units that were included in the initial study as well as other units that requested to participate, particularly in the Ann Arbor site. Participation rates were lower in Detroit where the nursing shortage is greater, making release time for training more difficult. Despite these challenges, over half of the inpatient nurses in the Detroit VA were trained as well as some other staff and, as new nurses are hired and receive the training during orientation, the percentages of those trained will rise.
The greatest barrier to implementation was negotiating release time for the nurses to attend the 1-h training. A variety of strategies were used, including providing the training on the units, taking it to the midnight shift, and negotiating “comp time” for nurses to stay after their shift. Once trained, nurses were actually enthusiastic about being empowered to deliver cessation services. Enthusiasm was enhanced when nurses saw that their feedback was actually being incorporated into the implementation strategy.
Patients reported an increase in receiving selected cessation services from pre- to post intervention, particularly in regards to medications that doubled and tripled, in some cases. Overall satisfaction and selected measures of satisfaction with cessation services also improved from pre- to post-intervention. While we expected greater improvements than those shown, there may have been a recall bias in that the post-intervention surveys were conducted 6-months after discharge. Another possibility is that, due to competing demands, nurses may not have delivered the intervention as intensively as needed.
Nurses suggested having a dedicated cessation counselor, and we considered this possibility as the fidelity of the intervention is likely to be greater if one nurse implements it versus 200 nurses implementing it in conjunction with their other responsibilities. However, this idea was not implemented because a dedicated FTE for this was not supported by administration and would therefore not be sustainable. Moreover, feedback from another VA researcher that used dedicated counselors noted that it took four to five attempts to locate the patient while in the hospital. Provision of cessation services by nurses, supported by physicians, is likely to have a much greater reach as these providers have access to and rapport with the patient. Even brief advice has been shown to improve quit rates,8 and as medication rates increase, quit rates will be further enhanced.32
There was considerable effort expended to make the intervention as transparent as possible to both nurses and physicians. The idea of packaging the intervention into a toolkit, providing a simple medication algorithm, brief physician training, offering rolling trainings on different shifts, offering incentives, prepping the patient with a video, publishing the Tobacco Tactics manual for patients, making materials easily available on the unit, and developing an easy to use documentation template enhanced the success of implementation. All of these efforts are likely to make the intervention more transportable to other VAs. Generalizability of the intervention is expected to be high as a huge amount of feedback from key opinion leaders, nurses, and patients was used to develop the intervention. Other similar studies,33,34 including a study that included a VA hospital,35 have shown high generalizability when institutionalizing inpatient cessation interventions.
The idea of training dedicated volunteers for follow-up calls was a novel strategy that was initially met with some resistance from nursing and medical administrators. However, once a VA policy was identified that stated volunteers are allowed to provide patient care (VHA Handbook 1620.1, July 2005), providers were agreeable to pilot the program. Peer support has been shown to be effective in improving a number of health conditions.36
Tobacco performance measures improved in Ann Arbor, but were high throughout the other sites. While helpful, performance measures should be interpreted cautiously as sample sizes are typically small, and documentation to meet performance measures may not reflect the quality of care provided.37,38 Nonetheless, performance measures are often the driving force behind changes in organizational behavior, and improvements in these measures can increase support from management for sustaining the intervention.
While the overall demographic and clinical characteristics of patients are fairly equal in the two intervention sites versus the control site, three times as many psychiatric patients were recruited by the research assistant in the control site versus the intervention sites. Compared to staff on general medical units, staff on psychiatric units may be more accustomed to providing behavioral interventions such as smoking cessation, especially since many of their patients smoke. Thus, differences in services received may be explained by an unequal case mix in the intervention versus control site and the smaller sample size in the control site due to a late start in recruiting. As the sample size increases and summative (outcome) evaluation is conducted, further analyses will need to control for this difference between sites, as patients with selected diagnoses have been shown to have differential quit rates.4
In this last year of the study, the research team has been totally withdrawn and the intervention left in the hands of providers. During this time, we expect some decline in implementation, but expect that rates will be higher than pre-intervention levels. The ultimate success of the program will be determined by 6-month self-reported quit rates verified by urine cotinine measures.
CONCLUSION
A large proportion of inpatient nursing staff can be rapidly trained to deliver tobacco cessation advice to inpatients. This training can improve confidence of the staff in providing these services and increase service delivery. Since staff nurses are the largest group of inpatient providers, educating staff nurses along with physician support can increase the reach of cessation interventions. Based on this experience, we recommend that unified cessation programs be adopted by VA facilities so that all staff can provide a consistent message to patients at all points of contact. Population-based strategies with direct outreach to smokers and treating tobacco use as a chronic disease have been recommended by others as a paradigm for what tobacco treatment in the health-care setting might look like in the future.39–42
ACKNOWLEDGMENTS
First and foremost, the authors would like to express our heartfelt appreciation to the Ann Arbor and Detroit nurses and other staff who included the intervention in their already busy work schedules. In particular, we would like to thank the nurse champions that contributed to spear-heading Tobacco Tactics on their units, including Christine Bulifant, Yamil Casillas-Hernandez, Denise Crawford, Bryan Facione, Kelly Johnston, Patricia Lello, Bettie Martinez, Carey Michel, Sarah Palmateer, Melissa Powers, Ruth Riley, Mary Jane Roth, Diane Sobecki-Ryniak, Cecilia Sosnowski, Patricia Teague, Arik Theeke, Sylvia Wallace, Charles Washington, Vicki Washington, Lori Wilson, and Patrick Wozny. Special thanks go to Ann Arbor VA volunteers Edward Florence and Thomas Griffiths for providing the follow-up phone calls to nearly 270 patients. Moreover, we would like to acknowledge the administrative staff who supported the integration of the Tobacco Tactics program into the organization, including, but not limited to, Pamela Reeves, Christopher Hermann, Stacey Breedveld, Micki Wheaton, Pamela McCoy, Linda Seck, Suzanne Mohler, Patricia Gurley, Barbara Clarke, Thomas Heller, Cindy Shepler, Diane Jamrog, and Beverly Leneski. Special thanks go to Rodney Hayward, Sarah Krein, and Laura Damschroder for their editorial comments. Most importantly, we would like to thank the veterans that participated in this study. Lastly, we would like to thank the Department of Veterans Affairs for their generous support of this Service Directed Project (SDP 06–003).
Conflict of interest None disclosed.
Appendix
Appendix A. Smoking Cessation Behavioral Management Protocol
Assess if patient is interested in quitting.
If patient is not interested, leave a brochure at bedside.
If patient is interested, leave a brochure and arrange for patient to view videotape.
After videotape, provide patient with Tobacco Tactics manual to read if able.
- Using patient manual, assist patient with behavioral intervention including:
- Self assessment
- Smoker type
- Smoking costs
- Handling cravings
- Relapse prevention
- Medication options
Along with patient, identify and arrange for cessation medications (see pharmaceutical protocol).
Arrange for volunteer follow-up calls.
Appendix B. Smoking Cessation Pharmaceutical Management Protocol
- Recommend nicotine replacement (patch, gum, or lozenge) if:
- Never used patch, gum, or lozenge before.
- Used patch, gum, or lozenge successfully in the past (smoke-free >3 months).
- Recommend Bupropion if:
- Failed nicotine replacement monotherapy in the past (smoke-free <3 months).
- Patch, gum, or lozenge intolerant (i.e., rash, etc.).
- History of depression or currently has depressive symptoms.
- Recommend combination nicotine replacement (patch, gum, or lozenge) and Bupropion if:
- Failed nicotine replacement and Bupropion monotherapy in the past.
- Recommend Varenicline if:
- Intolerance or treatment failure to nicotine replacement and bupropion.
Footnotes
The members of the VISN 11 Tobacco Tactics Team in alphabetical order are Timothy Carmody, Carmelite Dalmacy, Petra Flanagan, Amanda Fore, Judy Heath, Thomas Hicks, David Ronis, and Richard White
References
- 1.Haapanen-Niemi N, Miilunpalo S, Vuori I, Pasanen M, Oja P. The impact of smoking, alcohol consumption, and physical activity on use of hospital services. Am J Public Health. 1999;89:691–698. doi: 10.2105/AJPH.89.5.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Health Behaviors of Veterans in the VHA: Tobacco Use. 1999 Large Health Survey of Enrollees. Washington, D.C.: Veterans Health Administration; 2001. [Google Scholar]
- 3.Department of Veterans Affairs, Veterans Health Administration, Office of the Assistant Deputy Under Secretary for Health for Policy and Planning. 2005 Survey of Veteran Enrollees’ Health and Reliance Upon VA. Washington DC; 2006.
- 4.Rigotti NA, Munafo MR, Stead LF. Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med. 2008;168:1950–1960. doi: 10.1001/archinte.168.18.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith PM, Taylor CB. Implementing an Inpatient Smoking Cessation Program. Mahwah, NJ: Lawrence Erlbaum Associates; 2006. [Google Scholar]
- 6.Simon JA, Solkowitz SN, Carmody TP, Browner WS. Smoking cessation after surgery. A randomized trial. Arch Intern Med. 1997;157:1371–1376. doi: 10.1001/archinte.157.12.1371. [DOI] [PubMed] [Google Scholar]
- 7.Simon JA, Carmody TP, Hudes ES, Snyder E, Murray J. Intensive smoking cessation counseling versus minimal counseling among hospitalized smokers treated with transdermal nicotine replacement: a randomized trial. Am J Med. 2003;114:555–562. doi: 10.1016/S0002-9343(03)00081-0. [DOI] [PubMed] [Google Scholar]
- 8.Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2000. [Google Scholar]
- 9.VA/DoD Clinical Practice Guideline Working Group: Management of Tobacco Use. Washington, DC. Office of Quality and Performance Publication 10Q-CPG/TUC-04: Veterans Health Administration, Department of Veterans Affairs and Health Affairs, Department of Defense; 2004.
- 10.Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA. 1997;278:1759–1766. doi: 10.1001/jama.278.21.1759. [DOI] [PubMed] [Google Scholar]
- 11.Taylor CB, Curry SJ. Implementation of evidence-based tobacco use cessation guidelines in managed care organizations. Ann Behav Med. 2004;27:13–21. doi: 10.1207/s15324796abm2701_3. [DOI] [PubMed] [Google Scholar]
- 12.Rice VH, Stead LF. Nursing interventions for smoking cessation. Cochrane Database Syst Rev. 2008;1:CD001188. doi: 10.1002/14651858.CD001188.pub3. [DOI] [PubMed] [Google Scholar]
- 13.Duffy SA, Reeves P, Hermann C, Karvonen C, Smith P. In-hospital smoking cessation programs: what do VA patients and staff want and need? Appl Nurs Res. 2008;21:199–206. doi: 10.1016/j.apnr.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Duffy SA, Ronis DL, Valenstein M, et al. A tailored smoking, alcohol, and depression intervention for head and neck cancer patients. Cancer Epidemiol Biomarkers Prev. 2006;15:2203–2208. doi: 10.1158/1055-9965.EPI-05-0880. [DOI] [PubMed] [Google Scholar]
- 15.Department of Veterans Affairs. QUERI implementation guide. Available at: http://www.queri.research.va.gov/implementation/. Accessed July 9, 2009.
- 16.Stetler CB, Legro MW, Wallace CM, et al. The role of formative evaluation in implementation research and the QUERI experience. J Gen Intern Med. 2006;21(Suppl 2):S1–S8. doi: 10.1007/s11606-006-0267-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Department of Health and Human Services. Dissemination and implementation research in health (R01). Available at: http://grants.nih.gov/grants/guide/pa-files/PAR-06-039.html. Accessed July 9, 2009.
- 18.Green LW, Kreuter MW. Health Promotion Planning: An Educational and Ecological Approach (4th ed.) New York, NY: McGraw-Hill; 2005. [Google Scholar]
- 19.Lyon ER. A review of the effects of nicotine on schizophrenia and antipsychotic medications. Psychiatr Serv. 1999;50:1346–1350. doi: 10.1176/ps.50.10.1346. [DOI] [PubMed] [Google Scholar]
- 20.Thomson O’Brien MA, Freemantle N, Oxman AD, Wolf F, Davis DA, Herrin J. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2001;1:CD003030. doi: 10.1002/14651858.CD003030. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Department of Health and Human Services, Public Health Service. Helping Smokers Quit: A Guide for Clinicians. Available at: http://www.ahrq.gov/clinic/tobacco/clinhlpsmksqt.pdf. Accessed July 9, 2009.
- 22.Milner-Fenwick, Inc. Smoking: Getting Ready to Quit (2nd ed.). Available at: www.milner-fenwick.com/products/gn51/index.asp#details. Accessed July 9, 2009.
- 23.Smokefree.gov. Available at: http://www.smokefree.gov/expert.html. Accessed July 9, 2009.
- 24.An LC, Zhu SH, Nelson DB, et al. Benefits of telephone care over primary care for smoking cessation: a randomized trial. Arch Intern Med. 2006;166:536–542. doi: 10.1001/archinte.166.5.536. [DOI] [PubMed] [Google Scholar]
- 25.Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, Boles SM. Telephone counseling for smoking cessation: rationales and meta-analytic review of evidence. Health Educ Res. 1996;11:243–257. doi: 10.1093/her/11.2.243. [DOI] [PubMed] [Google Scholar]
- 26.Smith PM, Cameron R, McDonald PW, Kawash B, Madill C, Brown KS. Telephone counseling for population-based smoking cessation. Am J Health Behav. 2004;28:231–241. doi: 10.5993/ajhb.28.3.4. [DOI] [PubMed] [Google Scholar]
- 27.Lawrence K, Heisler M, Resnicow K, Halasyamani L, Mase R, Monroe M. Tools for Being a Helpful Peer Partner (video recording). Supported by the National Heart, Lung, and Blood Institute. Developed by the University of Michigan and St. Joseph Mercy Health System. Ann Arbor: The Regents of the University of Michigan. 2007.
- 28.Department of Veterans Affairs, Office of Quality & Performance. Performance Measurement Technical Manual. Available at: http://vaww.oqp.med.va.gov/default.htm (available on VA Intranet only). Accessed July 9, 2009.
- 29.Borrelli B, Hecht JP, Papandonatos GD, Emmons KM, Tatewosian LR, Abrams DB. Smoking-cessation counseling in the home. Attitudes, beliefs, and behaviors of home healthcare nurses. Am J Prev Med. 2001;21:272–277. doi: 10.1016/S0749-3797(01)00369-5. [DOI] [PubMed] [Google Scholar]
- 30.Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41:327–350. doi: 10.1007/s10464-008-9165-0. [DOI] [PubMed] [Google Scholar]
- 31.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Friend K, Levy DT. Smoking treatment interventions and policies to promote their use: a critical review. Nicotine Tob Res. 2001;3:299–310. doi: 10.1080/14622200110072165. [DOI] [PubMed] [Google Scholar]
- 33.Houston Miller N, Smith PM, DeBusk RF, Sobel DS, Taylor CB. Smoking cessation in hospitalized patients. Results of a randomized trial. Arch Intern Med. 1997;157:409–415. doi: 10.1001/archinte.157.4.409. [DOI] [PubMed] [Google Scholar]
- 34.Smith PM, Reilly KR, Houston Miller N, DeBusk RF, Taylor CB. Application of a nurse-managed inpatient smoking cessation program. Nicotine Tob Res. 2002;4:211–222. doi: 10.1080/14622200210123590. [DOI] [PubMed] [Google Scholar]
- 35.Taylor CB, Miller NH, Cameron RP, Fagans EW, Das S. Dissemination of an effective inpatient tobacco use cessation program. Nicotine Tob Res. 2005;7:129–137. doi: 10.1080/14622200412331328420. [DOI] [PubMed] [Google Scholar]
- 36.Wilson W, Pratt C. The impact of diabetes education and peer support upon weight and glycemic control of elderly persons with noninsulin dependent diabetes mellitus (NIDDM) Am J Public Health. 1987;77:634–635. doi: 10.2105/AJPH.77.5.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stark JF, Stark J. Performance measurement in congenital heart surgery: benefits and drawbacks. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2003;6:171–183. doi: 10.1053/pcsu.2003.50010. [DOI] [PubMed] [Google Scholar]
- 38.Eddy DM. Performance measurement: problems and solutions. Health Aff (Millwood) 1998;17:7–25. doi: 10.1377/hlthaff.17.4.7. [DOI] [PubMed] [Google Scholar]
- 39.Steinberg MB, Schmelzer AC, Richardson DL, Foulds J. The case for treating tobacco dependence as a chronic disease. Ann Intern Med. 2008;148:554–556. doi: 10.7326/0003-4819-148-7-200804010-00012. [DOI] [PubMed] [Google Scholar]
- 40.Sherman SE. A framework for tobacco control: lessons learnt from Veterans Health Administration. BMJ. 2008;336:1016–1019. doi: 10.1136/bmj.39510.805266.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ellerbeck EF, Mahnken JD, Cupertino AP, et al. Effect of varying levels of disease management on smoking cessation: a randomized trial. Ann Intern Med. 2009;150:437–446. doi: 10.7326/0003-4819-150-7-200904070-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rigotti NA. The future of tobacco treatment in the health care system. Ann Intern Med. 2009;150:496–497. doi: 10.7326/0003-4819-150-7-200904070-00011. [DOI] [PubMed] [Google Scholar]