Abstract
Although porous-coated hemispherical components are usually successful in acetabular revisions, the rate of failure is increased in hips with severe bone loss. Tantalum acetabular implants are characterized by higher friction, higher porosity, and greater osteoconductivity than titanium mesh or chrome-cobalt beads. We asked whether these components would provide stable short-term fixation without radiographic loosening in revisions at higher risk for failure. We prospectively followed 37 patients (39 hips) who had an acetabular revision with tantalum acetabular components. The minimum followup time was 2 years (mean, 3.3 years; range, 2–7 years). The acetabular defects were classified as Paprosky et al. Type 3 in 26, Type 2 in 11, and Type 1 in two hips. The mean postoperative Harris hip score was 86. Thirty-eight of the 39 (97%) tantalum components were radiographically well fixed. There was one mechanical failure at 6 months, rerevised with a larger tantalum component. Bone ingrowth was apparent in 38 hips and four hips had a radiolucent line. There were six other reoperations, three recurrent dislocations (constrained liners leaving the shell in place), two infections that seeded to the hip from elsewhere and treated with drainage, and one supracondylar femur fracture, but the tantalum component was left in place. Tantalum acetabular components provide stable fixation in difficult acetabular revisions.
Level of Evidence: Level IV, case series. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Uncemented porous-coated hemispherical components with screw fixation have been widely successful for acetabular revisions. Two studies have reported 12- and 15-year survival rates of 95% or greater [7, 9]. One study of 86 extra-large (≥ 62 mm in women, ≥ 66 mm in men) acetabular components also reported an 8-year survival rate of 93% [19]. However, uncemented hemispheres with either titanium mesh or cobalt-chrome bead coatings reportedly have higher rates of failure (7%–16%) in hips with severe bone loss, including D’Antonio et al. [5] Class IV defects, Paprosky et al. [13] Type 3 acetabular defects, and when there is less than 50% contact with living host bone [1, 13]. In addition, one study reported a higher rate of failure (6.5% versus 3.6%) in patients with weights of greater than 82 kg [9]. In one long-term followup study of 138 titanium mesh-coated hemispheres implanted at the time of revision arthroplasty, 19 (13.8%) were removed for infection, for recurrent dislocation, and with a femoral revision.
New acetabular components fabricated of tantalum were introduced after basic science studies demonstrated higher porosity (75%–80%), greater strength, higher surface friction, and greater osteoconductivity than other porous coatings such as titanium mesh and chrome-cobalt beads [2, 3]. This hemispherical acetabular component initially required a polyethylene liner to be cemented into the shell but later was available as a modular shell [10]. With the original shell, screws could be placed directly through the material for fixation. An augment system was also made available for segmental defects [12].
We asked (1) whether there would be a high rate of pain relief and secure radiographic fixation with tantalum acetabular components implanted in difficult acetabular revisions or those at higher risk for failure; and (2) whether the complication rate with this component would be lower than that reported with other porous-coated components in revision arthroplasty.
Materials and Methods
We prospectively followed 39 selected patients (41 hips) who underwent acetabular revisions using a tantalum acetabular component (Trabecular Metal™; Zimmer, Inc, Warsaw, IN) between August 2001 and December 2006. These components were implanted only in patients we judged at a high risk for failure: 37 patients with Type 3 deficiencies as judged by the classification of Paprosky et al. [13], or less than 50% living host bone in contact with the component [1, 13], and in two patients with weights of greater than 81 kg [9]. These 41 revisions were a subset (39%) of 104 uncemented acetabular revisions performed during this time. No acetabular cages were used. One patient died and one patient was lost to followup at less than 2 years. This left 39 tantalum acetabular components in 18 male and 19 female patients with a mean age of 65.1 years (range, 41–79 years). Two patients had two-stage revisions for infected prostheses. The mean patient weight was 82.1 kg (range, 54–107 kg) and the mean patient height was 148.5 cm (range, 132.8–166.5 cm). The mean patient body mass index was 29.3 (range, 20.2–43.7). The minimum followup time was 2 years (mean, 3.3 years; range, 2–7 years).
The acetabular revision was the first revision in 22 hips, the second in 13 hips, and the third in four hips. The component revised was uncemented in 29 hips, cemented in eight hips, and a protruded bipolar in two hips. The amount of acetabular bone loss was recorded using both the preoperative radiographs and intraoperative findings and described using both the method described by Paprosky et al. [13] and the D’Antonio et al. defect class [5]. There were 26 Paprosky et al. Type 3 (18 Type 3B, eight Type 3A), 11 Type 2, and two Type 1 acetabular defects. Using the system described by D’Antonio et al. [5], two hips had no defect after reaming, three had cavitary defects only, six had segmental defects, and 28 had combined deficiencies.
The revision was performed through a posterolateral approach in all hips, with a standard or extended trochanteric osteotomy in six hips. Twelve of the 39 hips had a concomitant femoral component revision. Preparation of the acetabulum was performed using hemispherical reamers and plastic trial components. The tantalum component implanted matched the size of the final reamer. Fresh, frozen, crushed cancellous allograft was used in almost all hips, but no bulk allografts were used. The reverse reamer technique was used to impact the graft.
The tantalum acetabular component implanted was the nonmodular revision shell with cemented polyethylene liner in 12 hips and the modular shell in 27 hips (both Zimmer, Inc). Augments were used in four hips in which a bulk allograft might have been considered. Screw fixation was routinely used, with four screws in nine hips, three in 17 hips, two in 12 hips, and one in one hip. In six hips, screws were placed through holes drilled into the non-modular component. The acetabular liner implanted had an inner diameter of 28 mm in three hips, 32 mm in 19 hips, and 36 mm in 17 hips. Only two hips had a constrained liner placed in the index procedure. The mean size of the tantalum acetabular component was 62.8 mm (range, 54–72 mm). Using the Mayo Clinic definition for “extra-large” components (≥ 62 mm in women, ≥ 66 mm in men) [19], there were seven implanted in female patients and 11 in male patients. Twenty-seven of the 39 hips had an isolated acetabular revision and 12 had revision of both components.
Postoperatively, the patients walked with a walker or two crutches for 6 weeks; 29 wore a prophylactic hip orthosis to limit range of motion as a precaution against dislocation. All patients were prescribed hip precautions, but no formal physical therapy was prescribed.
We followed patients at 6 weeks postoperatively, 6 months, 1 year, and yearly thereafter. The patients were prospectively evaluated pre- and postoperatively by one experienced nurse (ESS) using the modified Harris hip score [8].
One of us (ESS) evaluated standardized anteroposterior and lateral radiographs at each followup visit for radiolucent lines and migration [9]. Radiolucent lines at the prosthesis bone interface were described according to the three zones defined by DeLee and Charnley [6]. Definite acetabular loosening was defined as a change in the cup angle of greater than 5° on the anteroposterior pelvic radiograph or a change in the vertical or horizontal position of the cup of greater than 2 mm [11]. Computed axial tomography of the hips was not performed.
Results
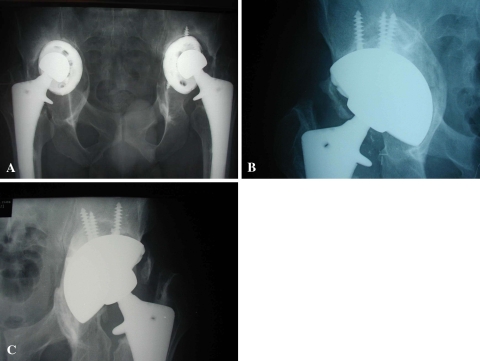
The mean Harris hip score increased from 48 points preoperatively to 86 points (range, 58–98 points) at the most recent followup. Thirty-six patients (38 hips) had no or slight pain (Fig. 1). One patient (one hip) had loosening and recurrent dislocation at 6 months.
Fig. 1A–C.
(A) A preoperative radiograph shows the hips of a 55-year-old man with bilateral migrated uncemented acetabular components and severe bone loss. (B) A 5-year followup radiograph of the right hip shows a less than 1 mm radiolucent line in Zone 3. (C) A 4-year followup radiograph of the left hip shows no radiolucent lines.
Thirty-eight of the tantalum acetabular components had no radiographic evidence of loosening at the most recent followup. One component had definite early loosening, with shift of the acetabular component into excessive abduction, and recurrent dislocations, with rerevision of the modular tantalum component to a 2-mm-larger nonmodular tantalum component with four screws placed through the component for fixation and cementation of a constrained liner [4]. The patient had a good result at 2 years.
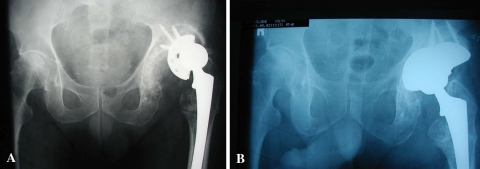
Nonprogressive radiolucent lines were present in four hips (11%): three of 27 hips with the modular component and one of 12 hips with the nonmodular component. In three hips, there was a radiolucent line in Zone 3 (two were < 1 mm; one was 1–2 mm) and one hip had a 1- to 2-mm radiolucent line in Zone 1 adjacent to bone graft material. There were no radiolucent lines adjacent to the augments (Fig. 2). The mean acetabular abduction angle was 40° (range, 25°–54°).
Fig. 2A–B.
(A) A preoperative radiograph shows the hips of an active 79-year-old man with early (6-month) failure of a beaded surface uncemented revision acetabular component. The acetabulum was classified as Paprosky et al. Type 3B. (B) A 3-year followup radiograph shows no radiolucent lines. The patient has no pain and a very slight limp.
Five hips dislocated (at 2 to 8 weeks postoperatively) and four underwent reoperation for recurrent dislocation. For these four, the revision was their second or third acetabular revision. Three had a constrained liner cemented into the original nonmodular tantalum component, which was left in place, and the other (previously mentioned) had the loose 68-mm modular tantalum component rerevised to a 70-mm nonmodular component with cementation of a constrained liner. Two patients (one with rheumatoid arthritis and one with sickle cell anemia) had late infections, which spread to the hip from pneumonia and a remote, untreated skin abscess, respectively, and had emergent incision, drainage, and antibiotic treatment. The tantalum components were not removed and both patients remain on an oral antibiotic indefinitely due to their underlying disorders. One patient had a traumatic supracondylar fracture of the ipsilateral femur treated with plate fixation.
Discussion
Uncemented acetabular components with titanium mesh or chrome-cobalt bead coatings, fixed with screws, have been successful for a large percentage of acetabular revisions. However, higher rates of failure have been reported in hips with severe bone loss, Paprosky et al. Type 3 or D’Antonio et al. combined defects, and patients weighing more than 82 kg [1, 7, 9, 13]. It was in these difficult revisions at high risk for failure that the use of a new acetabular component with an enhanced ingrowth surface, tantalum, was studied. Basic science studies demonstrated greater porosity, higher surface friction, and greater osteoconductivity with this material [2, 3]. We asked whether there would be a high rate of pain relief and secure radiographic fixation with the tantalum component in acetabular revisions at a higher risk of failure.
The study is limited by several factors. First, the absence of a control group with a surface coating other than tantalum in these difficult revisions. We did not compare these revisions to those in a previous study [9] due to multiple confounding variables. Second, the followup of 2 to 7 years (mean, 3 years) is not sufficient to determine the rate of success at longer-term followup. However, it is a relatively large cohort of acetabular revisions considered at high risk for failure due to severe bone loss or patient characteristics. The tantalum component was used in 40% of the acetabular revisions we performed during this time span. Although the cost of the new component is greater than a titanium mesh-coated component, the rate of success and infrequency of radiolucent lines of the tantalum component have encouraged us to use these components more frequently and in all cases with severe bone loss.
To our knowledge, six other published studies report the use of this component in revision arthroplasty [12, 14–18]. Unger et al. [17] reported the results of 60 consecutive revisions with a nonmodular tantalum acetabular component at a mean followup of 42 months (range, 18–68 months). However, screw fixation was used in only five hips and there were only eight hips (seven Paprosky Type 3A and one Type 3B) with severe bone loss in that study. The remaining 52 hips could likely have been treated successfully with other uncemented acetabular components. We analyzed the results of tantalum acetabular revisions from six centers (Table 1). Including the present study, there were 233 acetabular revisions with a tantalum component. There was severe preoperative bone loss, defined as Paprosky et al. Type 3, in 155 hips (67%). The vast majority of components had multiple-screw fixation. At a mean followup of 2.9 years (range, 2.5–3.1 years), there were seven hips (3%) that failed and underwent rerevision. Thus, at relatively short followup, this enhanced surface component has been successful in difficult acetabular revisions.
Table 1.
Tantalum acetabular revisions
| Study | Number of hips | Paprosky et al. [13] Type 3 (number of hips) | Mean followup (years) | Failure (number of hips) |
|---|---|---|---|---|
| Nehme et al. [12] | 16 | 11 | 2.5 | 0 |
| Unger et al. [17] | 60 | 8 | 3.5 | 1 |
| Sporer and Paprosky [15] | 28 | 28 | 3.1 | 1 |
| Sporer and Paprosky [16] | 13 | 13 | 2.6 | 1 |
| Weeden and Schmidt [18] | 43 | 43 | 2.8 | 1 |
| Siegmeth et al. [14] | 34 | 27 | 2.8 | 2 |
| Lachiewicz and Soileau (current study) | 39 | 26 | 3.3 | 1 |
The most frequent complication of acetabular revisions with the tantalum components in this study was dislocation, five of 39 hips (13%). This is not surprising, given the index surgery was the second or third acetabular revision for 17 hips and four of the five dislocations occurred in these 17 hips. These four patients had reoperations for recurrent dislocation, with implantation of a constrained liner. In two large series of acetabular revisions with unconstrained liners, the rate of dislocation was 12% [9, 19]. It is also the most frequent complication of acetabular revisions in which “extra-large” components have been implanted [19]. Our policy has been to use the largest femoral head possible and avoid the use of constrained liners initially with revision arthroplasty. A hip orthosis is used routinely if patient habitus permits. However, when there is a deficient abductor mechanism, severe osteolysis or nonunion of a greater trochanter, or a noncompliant patient, a constrained liner should be strongly considered initially when the tantalum component is implanted.
This recently developed ingrowth surface, tantalum, has expanded the indications for porous-coated hemispherical components rather than cages or bulk allografts in difficult acetabulum revisions with severe bone loss. The nonmodular tantalum component allows placing screws through the metal itself rather than through preexisting screw holes. The use of tantalum augments has virtually eliminated the need for bulk allografts. We believe the absence of radiographic loosening in 97% at a followup of 2 to 7 years is encouraging. Additional followup will be necessary to determine the long-term success of this component.
Footnotes
One of the authors (PFL) is an unpaid consultant, paid speaker’s bureau and has received institutional research support from Zimmer, Inc, Warsaw, IN.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Berry DJ. Revision total hip arthroplasty: uncemented acetabular components. In: Callaghan JJ, Rosenberg AG, Rubash HE, editors. The Adult Hip. 2. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 1371–1381. [Google Scholar]
- 2.Bobyn JD, Stackpool GJ, Hacking SA, Tanzer M, Krygier JJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999;81:907–914. doi: 10.1302/0301-620X.81B5.9283. [DOI] [PubMed] [Google Scholar]
- 3.Bobyn JD, Toh KK, Hacking SA, Tanzer M, Krygier JJ. Tissue response to porous tantalum acetabular cups: a canine model. J Arthroplasty. 1999;14:347–354. doi: 10.1016/S0883-5403(99)90062-1. [DOI] [PubMed] [Google Scholar]
- 4.Burroughs BR, Golladay GJ, Hallstrom B, Harris WH. A novel constrained acetabular liner design with increased range of motion. J Arthroplasty. 2001;16:31–36. doi: 10.1054/arth.2001.28361. [DOI] [PubMed] [Google Scholar]
- 5.D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;243:126–137. [PubMed] [Google Scholar]
- 6.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 7.Della Valle CN, Berger RA, Rosenberg AG, Galante JO. Cementless acetabular reconstruction in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;420:96–100. doi: 10.1097/00003086-200403000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 9.Jones CP, Lachiewicz PF. Factors influencing the longer-term survival of uncemented acetabular components used in total hip revisions. J Bone Joint Surg Am. 2004;86:342–347. doi: 10.1302/0301-620X.86B6.15000. [DOI] [PubMed] [Google Scholar]
- 10.Levine B, Valle CJ, Jacobs JJ. Applications of porous tantalum in total hip arthroplasty. J Am Acad Orthop Surg. 2006;14:646–655. doi: 10.5435/00124635-200611000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration: an experimental study. J Arthroplasty. 1989;4:245–251. doi: 10.1016/S0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 12.Lewallen Nehme A, DG Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res. 2004;429:201–208. doi: 10.1097/01.blo.0000150133.88271.80. [DOI] [PubMed] [Google Scholar]
- 13.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a six year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 14.Siegmeth A, Duncan CP, Masri BA, Kim WY, Garbuz DS. Modular tantalum augments for acetabular defects in revision hip arthroplasty. Clin Orthop Relat Res. 2009;467:199–205. doi: 10.1007/s11999-008-0549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sporer SM, Paprosky WG. The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty. 2006;21:83–86. doi: 10.1016/j.arth.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Sporer SM, Paprosky WG. Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty. 2006;21:87–90. doi: 10.1016/j.arth.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 17.Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002–1009. doi: 10.1016/j.arth.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 18.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22:151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 19.Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001;83:1352–1357. doi: 10.2106/00004623-200109000-00010. [DOI] [PubMed] [Google Scholar]