Abstract
Isolated acetabular revision can be associated with variable patient outcomes; there is a risk of hip instability. We evaluated 42 isolated acetabular revision operations and investigated the impact of patient age, diagnosis, bone stock, bone loss, bone augmentation, and obesity on pain and the Harris hip score. Preoperative radiographs were graded according to Paprosky et al. Postoperative radiographs were graded according to Moore et al. and for implant position, prosthetic fixation, and osteolysis. Complications, patient outcome, reoperations, and acetabular rerevisions were recorded. All patients had complete clinical and radiographic followup with a minimum followup of 2 years (mean, 6.4 years; range, 2–13 years). The mean pain score and the mean Harris hip score improved postoperatively. There was one infection 6 months after operation. There were no dislocations. There were three acetabular rerevisions (7%) for aseptic loosening. Patient age, preoperative diagnosis, bone loss, and pelvic bone augmentation had no influence on pain or Harris hip scores. Before operation, obese patients tended to have less pain than nonobese patients but at followup obese patients had less improvement in pain scores than nonobese patients.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The most common reason for failure of THA is periprosthetic osteolysis and loosening of hip implants [14]. When periprosthetic osteolysis and implant loosening are associated with pain and reduced function or when osteolysis threatens implant fixation, revision hip arthroplasty can be considered for treatment.
Isolated acetabular revision is indicated when an acetabular implant is associated with pain, reduced function, instability, or loosening, while the femoral implant is in satisfactory position and is well fixed to bone. Isolated acetabular revision, which reportedly accounts for 12.7% of revision hip arthroplasty [1], can be a technically challenging operation due to limitations of exposure associated with an intact femoral implant, pelvic bone loss, requirements for pelvic bone augmentation, ability to achieve fixation of a revision acetabular implant, difficulty balancing the soft tissues, and ability to construct a stable hip. The literature does not clarify, however, whether any preoperative variables influence pain relief or functional scores.
We (1) described pain relief and functional scores of isolated acetabular revision operations and (2) explored the influence of patient age, diagnosis, bone stock, bone loss, bone augmentation, and obesity on pain relief and functional scores.
Patients and Methods
We retrospectively reviewed all 42 isolated acetabular revision hip arthroplasties performed in 39 patients by one surgeon between February 1993 and November 2005. Thirty-two of the 42 acetabular implants (76%) were revised for painful loosening, six (14%) for asymptomatic periprosthetic osteolysis, and four (10%) for hip instability. All operative reports were reviewed. Data were collected prospectively in a joint arthroplasty database and reviewed retrospectively for all patients. Clinical and radiographic followup was available for all hips. The average age of the patients was 69 years (range, 27–87 years) at the time of surgery. There were 22 (52%) male and 17 female patients. The average height was 166.6 cm (range, 144.8–182.9 cm). The average weight was 79.9 kg (range, 40.5–109.1 kg). The average body mass index (BMI) was 27.8 kg/m2 (range, 12–38.7 kg/m2). Obesity was defined as a BMI of 30 kg/m2 or more [17]. Fifteen patients (36%) were obese and 27 (64%) patients were not obese. The average BMI of the obese group was 32.7 kg/m2, while the nonobese group had an average BMI of 25.0 kg/m2. The minimum followup was 2 years (average, 6.4 years; range, 2–13 years). No hips were lost to followup.
Clinical data were collected prospectively with a patient questionnaire filled out preoperatively and at each followup visit. Patients were asked to rate pain on a 10-point visual analog scale (VAS) for pain, with 0 being no pain and 10 representing severe pain. The Harris hip score [5] was calculated for each patient.
The mean femoral index (a measure of bone stock) [6] was 0.53 (range, 0.45–0.62). Lower femoral index is associated with better bone stock, and higher femoral index is associated with less strong bone stock. Femoral index is a ratio of cortical thickness to diaphyseal thickness measured 8 cm distal to the lesser trochanter. Patients with femoral indices of greater than 0.56 were considered osteopenic. Preoperatively, osteopenic patients had lower (p = 0.006) Harris hip scores than patients with normal bone stock.
Two of us (BML, SS) classified the bone loss and femoral head migration on preoperative radiographs according to the classification system of Paprosky et al. [12]: 14 hips (33%) were Type I, 22 hips (52%) were Type II, and six hips (14%) were Type III. The interobserver kappa value for the Paprosky acetabular score is 0.42 [4]. Paprosky Type I defects display minimal acetabular deformity with no component migration and no ischial bone lysis. Paprosky Type II defects display destruction of the superior acetabular dome and medial wall with intact anterior and posterior columns. Type II subclasses include A, B, and C, with Subclass A defects showing superior migration, Subclass B lesions showing superolateral migration, and Subclass C lesions showing medial migration secondary to an absent medial wall. Paprosky Type III lesions display implant migration of greater than 2 cm and extensive bone loss. Type III subclasses include A and B, with Subclass B showing greater medial migration due to medial wall deficiency. Both IIIA and IIIB have destruction of the teardrop, with IIIB showing complete destruction. Patients with Paprosky Type I acetabula had less (p = 0.031) preoperative pain than patients with Types II and III deficiency.
Initial postoperative radiographs were compared to radiographs at last followup to evaluate implant position, implant migration, osteolysis, and acetabular implant osteointegration, using the method of Moore et al. [11]. Moore et al. [11] described five radiographic signs indicative of acetabular osseointegration, including the absence of radiolucent lines, the presence of a superolateral buttress, the presence of medial stress shielding, the presence of a radial trabecular pattern, and the presence of an inferomedial buttress. When three or more of these signs were present on the radiograph, the positive predictive value of osseointegration was 96.9% with a sensitivity of 89.6% [11].
A modified direct lateral approach to the hip was used for all operations. The femoral stem was in satisfactory position and well fixed to bone in all patients. All femoral stems were preserved. A tap-out, tap-in, recement technique was used for two femoral stems in two patients with monoblock femoral components. Six monoblock femoral stems were left in place during the operation. In 34 patients with a modular femoral stem, the stem was left in place and the femoral head was removed to improve surgical exposure. All acetabular cups, liners, and screws were removed. Pelvic bony defects were treated with morselized allograft graft in 21 (50%) patients, structural allograft in five (12%) patients, and trabecular metal in one patient (2%). No bone augmentation was used in 15 patients (38%). The acetabulum was underreamed by 1 to 2 mm for initial press-fit fixation. Several hemispherical, cementless acetabular implants were used (Table 1). Average revision cup size was 61.5 mm (range, 50–74 mm). Acetabular fixation was augmented with acetabular screws in 37 patients (88%), with an average of 3.5 screws (range, 0–7 screws). A new prosthetic femoral head was used to increase femoral head size, increase femoral neck length, or improve femoral offset for all 34 modular femoral stems. Twenty-two patients (52%) received a 28-mm femoral head and 20 patients (48%) received a 32-mm femoral head.
Table 1.
Patient data
| Variable | Preoperative | Followup | p Value |
|---|---|---|---|
| Number of acetabular revisions | 42 | 42 | |
| Number of patients | 39 | 39 | |
| Number of patients deceased | 6 | ||
| Age (years)* | 69 ± 12.2 (27–87) | 75 ± 12.4 (34–94) | |
| Gender | |||
| Male | 22 (52%) | ||
| Female | 17 (48%) | ||
| Side | |||
| Left | 19 (45%) | ||
| Right | 23 (55%) | ||
| Height (cm)* | 166.6 (144.8-182.9) | ||
| Weight (kg)* | 79.9 (40.5–109.1) | ||
| Body mass index (kg/m2) | 27.8 ± 4.9 (12–38.7) | ||
| Diagnosis | |||
| Painful loosening | 32 (76%) | ||
| Osteolysis | 6 (14%) | ||
| Instability | 4 (10%) | ||
| Visual analog scale pain score (0–10)* | 6.7 (1–10) | 1.2 (0–7) | < 0.0001 |
| Harris hip score* | 49.8 (7.4–88.7) | 80.0 (40.2–99.8) | < 0.0001 |
| Femoral index* | 0.53 (0.45–0.62) | ||
| Radiographs (preoperative: Paprosky type) | |||
| Type I | 14 (33%) | ||
| Type II | 22 (52%) | ||
| Type III | 6 (14%) | ||
| Radiographs (postoperative: Moore et al. grade) | |||
| 3–5 signs of osseointegration | 34 (81%) | ||
| 2 signs of osseointegration | 8 (19%) | ||
| Radiographs (postoperative stability) | 3 (7%) superior migration 1 (2%) broken screw 1 (2%) osteolysis |
||
| Bone augmentation | |||
| None | 15 (38%) | ||
| Morselized allograft | 21 (50%) | ||
| Structural allograft | 5 (12%) | ||
| Trabecular Metal | 1 (2%) | ||
| Acetabular implants utilized† | |||
| Duraloc | 13 (30%) | ||
| Pinnacle | 12 (29%) | ||
| PCA | 7 (17%) | ||
| Vitalock | 6 (14%) | ||
| TMI | 2 (5%) | ||
| Constrained | 2 (5%) | ||
| Revision cup size (outer diameter) (mm)* | 61.5 (50–74) | ||
| Acetabular screws used | |||
| Yes | 37 (88%) | ||
| No | 5 (12%) | ||
| Number of screws used* | 3.5 (0–7) | ||
| Femoral head size used | |||
| 28 mm | 22 | ||
| 32 mm | 20 | ||
| Followup (years)* | 6.4 (2.5–13.4) | ||
| Acute complications | 0 | ||
| Dislocations | 0 | ||
| Infections | 1 (2%) | ||
| Acetabular rerevisions for aseptic loosening | 3 (7.3%) |
* Values are expressed as mean or mean ± SD, with range in parentheses; †implants included: Duraloc, Depuy Orthopaedics, Inc, Warsaw, IN; Pinnacle, Depuy; PCA, Howmedica, Rutherford, NJ; Vitalock, Howmedica; TMI, Zimmer, Inc, Warsaw, IN; and Constrained, Osteonics Corp, Allendale, NJ.
All patients received 24 hours of prophylactic intravenous antibiotics postoperatively. Radiographs were obtained in the postanesthesia unit. Patients received warfarin for thromboembolic prophylaxis. Patients’ activity included foot flat partial weight bearing, and patients worked with physical therapy on mobilization.
The initial outpatient followup occurred 2 weeks postoperatively for wound check and medical management. We clinically and radiographically followed patients at six weeks, six months, and one year, and then followup was recommended at 3, 5, 7, and 10 years after operation. We determined differences in the VAS pain score and Harris hip score between preoperative and followup time periods with Student’s t test. We examined differences in the VAS pain score, Harris hip score, BMI, surgical age, and followup years between elderly/nonelderly (age > 65 years), obese/not obese (BMI > 30), large bone stock (femoral index > 0.56), and if graft was performed with Student’s t test. The average age of 16 younger patients was 56.8 years (range, 27–65 years) and the average age of 26 older patients was 76.2 (range, 65–87 years). We determined differences between Harris hip score, VAS pain score, BMI, and followup years between preoperative diagnosis groups and Paprosky type groups, with a one-way ANOVA. Relationships between patients’ surgical age, preoperative pain, Harris hip score, BMI, bone stock, cup size, reamed size, and Paprosky type were examined using a Pearson’s correlation. We determined differences between complications and reoperations in the Paprosky type, preoperative diagnosis, elderly/nonelderly (age > 65 years), obese/not obese (BMI > 30), large bone stock (femoral index > 0.56), and if graft was performed using a Fisher exact test. A Kaplan-Meier curve was used to calculate implant survivorship.
Results
There were no acute postoperative complications or dislocations. VAS pain scores improved (p < 0.0001) from a preoperative mean of 6.7 (range, 1–10) to a followup mean of 1.2 (range, 0–7). Harris hip scores improved (p < 0.0001) from a preoperative mean of 49.8 (range, 7–89) to a followup mean of 80.0 (range, 40–100) (Table 1). Five hips (12%) were reoperated. Three hips (7.3%) had acetabular rerevision for aseptic acetabular loosening at 6.7 years, 7.0 years, and 11.3 years. One hip was treated for infection at 6 months with successful two-stage resection and reimplantation. One hip had an isolated femoral revision with retention of the revised acetabulum for a traumatic femoral fracture at 9 years. The criteria of Moore et al. [11] were used to assess osseointegration of all hips at last followup. Of the 42 hips evaluated, 34 (81%) showed at least three radiographic signs of osseointegration. Preoperative classifications of the eight cups showing only two signs of osseointegration were three Paprosky Type I, four Paprosky Type II, and one Paprosky Type III. None of these patients required rerevision and had an average postoperative VAS pain score of 1.1 (range, 0–3). The 34 remaining hips all had at least three radiographic signs of osseointegration, indicating a 96.9% positive predictive value for bony ingrowth.
At last followup, there were no differences between the younger and older patients in terms of complications, pain scores, Harris hip scores, reoperation, or rate of revision (Table 2).
Table 2.
Impact of age
| Variable | Age ≤ 65 years | Age > 65 years | p Value |
|---|---|---|---|
| Number | 16 (38%) | 26 (62%) | |
| Followup (years)* | 5.7 (2–13) | 6.5 (2–12) | 0.727 |
| Age (years)* | 56.8 (27–65) | 76.2 (65–87) | 0.001 |
| Body mass index (kg/m2)* | 27.5 (20.1–34.5) | 28.0 (12.2–38.7) | 0.729 |
| Preoperative visual analog scale pain score* | 6.3 (1–10) | 6.9 (2–10) | 0.322 |
| Followup visual analog scale pain score* | 1.3 (0–5) | 1.2 (0–4) | 0.912 |
| Pain improvement* | 5.0 (0–9) | 5.7 (0–10) | 0.373 |
| Preoperative Harris hip score* | 56.2 (31.8–85.8) | 45.8 (7.4–88.7) | 0.063 |
| Followup Harris hip score* | 82.3 (58.4–99.8) | 78.5 (40.2–99.7) | 0.392 |
| Harris hip score improvement* | 26.1 (0.1–55.6) | 32.7 (6.3–72.6) | 0.206 |
| Infection | 0 | 1 (4%) | 1.000 |
| Reoperations | 3 (19%) | 2 (8%) | 0.352 |
* Values are expressed as mean, with range in parentheses.
Preoperative diagnosis, whether it was painful loosening (n = 32), asymptomatic osteolysis (n = 6), or instability (n = 4), did not affect pain or the Harris hip score or the improvement in pain or Harris hip score at last followup (Table 3).
Table 3.
Impact of diagnosis
| Variable | Painful loosening | Osteolysis | Instability | p Value |
|---|---|---|---|---|
| Number | 32 | 6 | 4 | |
| Followup (years)* | 5.8 (2–13.5) | 6.8 (2.5–12) | 7.5 (3–10) | 0.369 |
| Body mass index (kg/m2)* | 27.3 ± 4.8 | 29.7 ± 5.9 | 29.0 ± 2.9 | 0.492 |
| Preoperative visual analog scale pain score* | 7.1 ± 1.6 | 4.6 ± 3.3 | 6.0 ± 1.0 | 0.022 |
| Followup visual analog scale pain score* | 1.2 (0–7) | 0.8 (0–2) | 1.2 (0–2) | 0.830 |
| Pain improvement* | 5.8 ± 2.4 | 3.8 ± 2.7 | 4.8 ± 1.5 | 0.177 |
| Preoperative Harris hip score* | 48.1 ± 16.3 | 57.2 ± 24.5 | 52.4 ± 8.5 | 0.498 |
| Followup Harris hip score* | 79.5 (40.2–99.8) | 82.0 (68.8–97.8) | 80.9 (64–93) | 0.909 |
| Harris hip score improvement* | 31.4 ± 16.7 | 24.9 ± 18.6 | 28.5 ± 3.2 | 0.666 |
| Infection | 1 (2%) | 0 | 0 | 0.335 |
| Reoperations | 4 (12%) | 1 (17%) | 0 | 0.711 |
* Values are expressed as mean or mean ± SD, with range in parentheses.
At followup, osteopenic patients demonstrated a greater (p = 0.048) improvement in Harris hip score than patients with better bone stock. There was no difference in complications or reoperation (Table 4).
Table 4.
Impact of bone stock
| Variable | Femoral index ≤ 0.56 | Femoral index > 0.56 | p Value |
|---|---|---|---|
| Number | 29 (69%) | 13 (31%) | |
| Body mass index (kg/m2)* | 28.4 (12.2–38.7) | 26.5 (20–34.2) | 0.278 |
| Preoperative visual analog scale pain score* | 7.3 (1–10) | 6.3 (5–10) | 0.143 |
| Followup visual analog scale pain score* | 1.3 (0–7) | 1.0 (0–3) | 0.571 |
| Pain improvement* | 5.0 (1–8) | 6.3 (3–10) | 0.114 |
| Preoperative Harris hip score* | 54.6 (31.1–88.7) | 39.0 (7.4–63.7) | 0.006 |
| Follow up Harris hip score* | 81.5 (40.2–99.8) | 76.6 (60.8–87.9) | 0.285 |
| Harris hip score improvement* | 26.9 (0.1–55.6) | 37.6 (18–72.6) | 0.048 |
| Infection | 0 | 1 (8%) | 0.528 |
| Reoperations | 3 (10%) | 2 (15%) | 0.637 |
* Values are expressed as mean, with range in parentheses.
All reoperations and complications were in Paprosky Type II hips, but there was no difference between the Paprosky type groups with respect to complications or reoperation (Table 5).
Table 5.
Impact of bone deficiency
| Variable | Paprosky Type I | Paprosky Type II | Paprosky Type III | p Value |
|---|---|---|---|---|
| Number | 14 (36%) | 22 (52%) | 6 (14%) | |
| Followup (years)* | 6.9 (2.5–13) | 6.0 (2.5–13.5) | 4.5 (2–7) | 0.521 |
| Body mass index (kg/m2)* | 29.2 (20–38.7) | 27.1 (12.2–35.8) | 27.1 (20.1–34.2) | 0.477 |
| Preoperative visual analog scale pain score* | 5.5 ± 1.8 | 7.1 ± 2.1 | 7.7 ± 1.8 | 0.031 |
| Followup visual analog scale pain score* | 0.8 (0–2) | 1.7 (0–7) | 0.3 (0–2) | 0.115 |
| Pain improvement* | 4.6 ± 1.9 | 5.5 ± 2.6 | 7.3 ± 1.9 | 0.094 |
| Preoperative Harris hip score* | 56.4 (27.6–88.7) | 48.3 (7.4–85.8) | 39.9 (15.3–56.7) | 0.134 |
| Followup Harris hip score* | 81.8 (63.7–97.8) | 80.1 (40.2–99.8) | 75.1 (62.7–87.9) | 0.602 |
| Harris hip score improvement* | 25.5 (1–47.1) | 31.8 (0.1–58.9) | 35.2 (30.5–72.6) | 0.390 |
| Infection | 0 | 1 (2%) | 0 | 0.788 |
| Reoperations | 0 | 5 (23%) | 0 | 0.076 |
* Values are expressed as mean or mean ± standard deviation, with range in parentheses.
Pre- and postoperative pain levels were similar regardless of type of pelvic augmentation. There was no impact of bone augmentation on complications or reoperation. Patients who received structural pelvic augmentation had more (p = 0.024) improvement in pain score at followup compared to patients who did not receive structural pelvic augmentation (Table 6).
Table 6.
Impact of pelvic bone augmentation
| Variable | No structural pelvic augmentation | Structural pelvic augmentation | p Value |
|---|---|---|---|
| Number | 36 (86%) | 6 (14%) | |
| Followup (years)* | 7.6 ± 2.9 (3–13) | 5.9 ± 3.1 (2–13.5) | 0.101 |
| Body mass index (kg/m2)* | 28.1 ± 4.2 (20–33.7) | 25.9 ± 4.5 (12.2–38.7) | 0.314 |
| Preoperative visual analog scale pain score* | 6.5 ± 1.5 | 7.3 ± 2.4 | 0.411 |
| Followup visual analog scale pain score* | 1.3 (0–7) | 0.5 (0–4) | 0.247 |
| Pain improvement* | 5.2 ± 2.0 | 6.8 ± 2.8 | 0.024 |
| Preoperative Harris hip score* | 49.9 ± 18.7 (7.4–73) | 49.2 ± 17.7 (15.3–88.7) | 0.935 |
| Followup Harris hip score* | 80.2 (40.2–95) | 79.9 (58.4–99.8) | 0.830 |
| Harris hip score improvement* | 30.3 ± 10.4 (3.1–58.8) | 29.6 ± 17.3 (0.1–72.6) | 0.775 |
| Infection | 0 | 1 (2%) | 1.000 |
| Reoperations | 5 (19%) | 0 | 1.000 |
* Values are expressed as mean or mean ± SD, with range in parentheses.
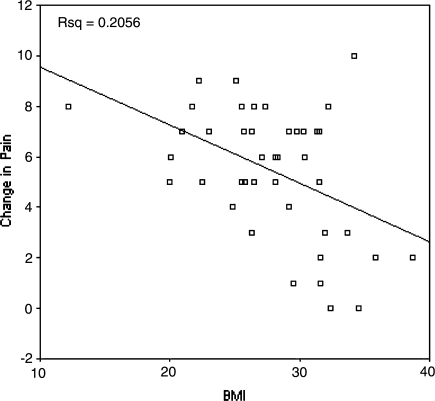
At followup, obese patients had higher (p = 0.179) pain scores than nonobese patients, and obese patients had less (p = 0.016) improvement in pain scores. There was no difference in the rate of complications or the need for reoperation in obese and nonobese patients (p = 1.000 and 0.329, respectively) (Table 7). There was a linear relationship (p = 0.038) when BMI was plotted against pain improvement (Fig. 1). The relationship was inversely proportional; as BMI increased, patients had less improvement in pain after isolated acetabular revision.
Table 7.
Impact of obesity
| Variable | Body mass index < 30 | Body mass index ≥ 30 | p Value |
|---|---|---|---|
| Number | 27 (64%) | 15 (36%) | |
| Followup (years)* | 6.1 ± 2.8 (2–12) | 7.0 ± 3.8 (2.5–13.5) | 0.89 |
| Body mass index (kg/m2) | 25.0 ± 3.8 (12.2–29.8) | 32.7 ± 2.2 (30.3–38.7) | < 0.0001 |
| Preoperative visual analog scale pain score* | 7.1 ± 1.5 | 5.8 ± 2.7 | 0.067 |
| Followup visual analog scale pain score* | 1.0 (0–3) | 1.7 (0–7) | 0.179 |
| Pain improvement* | 6.1 ± 1.9 (1–9) | 4.2 ± 3.1 (0–10) | 0.016 |
| Preoperative Harris hip score* | 46.2 ± 15.9 (7.4–78.9) | 56.3 ± 19.6 (15.3–88.7) | 0.072 |
| Followup Harris hip score* | 79.3 (58.4–99.8) | 81.3 (40.2–97.8) | 0.647 |
| Harris hip score improvement* | 33.1 ± 14.7 (3–59) | 25.0 ± 19.1 (0–72.6) | 0.124 |
| Infection | 1 (4%) | 0 | 1.000 |
| Reoperations | 2 (8%) | 3 (20%) | 0.329 |
* Values are expressed as mean or mean ± standard deviation, with range in parentheses.
Fig. 1.
As patient BMI increases, improvement in pain postoperatively decreases (p = 0.038).
Discussion
An estimated 51,236 revision hip arthroplasties were performed in the United States in 2007, and the prevalence of revision THA is expected to increase 137% to 96,700 operations in 2030 [10]. Revision hip arthroplasties include several different procedures: revision of the acetabulum and femur (CPT 27134); isolated revision of the acetabulum (CPT 27137); isolated revision of the femur (CPT 27138); and isolated revision of the bearing surface (femoral head and/or acetabular liner). We evaluated the surgical results of 42 isolated acetabular revision operations and investigated the impact of various patient and operative variables on clinical and radiographic outcomes.
We note several limitations. First, the small size of this series resulted in small numbers in the subcohort analysis with inadequate power available to detect true differences in between subcohorts. However, there are few large series of isolated acetabular revisions in the literature; these include those of Chen et al. [2] and Manning et al. [8] with 55 and 26 patients, respectively. Our single surgeon series was performed with a consistent surgical technique that would reduce some variability, and all patients had complete clinical and radiographic followup.
Pain, osteolysis, and instability were successfully treated in our study of 42 isolated acetabular revision operations. Saleh et al. [15] performed a meta-analysis of 39 articles reporting outcomes after revision hip surgery. They concluded revision hip operations had a comparable longevity to primary hip arthroplasty but carried increased morbidity and mortality and decreased postoperative functional outcomes. Different methods of reporting throughout the original articles prevented further analysis of patient variables [15]. In this series, one surgical technique including acetabular implant resection, bone augmentation as necessary, underreaming, press-fit implantation, and cup screw fixation through a modified direct lateral approach was associated with predictable pain relief, functional improvement, and hip stability.
Patient age did not affect patient outcome in our series. This finding is in agreement with Davis et al. [3] who reviewed outcome measures in 126 hip revisions. Their results were applied to all total hip revision arthroplasties, though a small subset of patients underwent isolated acetabular revisions. Their data showed no difference in functional outcomes or pain levels postoperatively when patient age was studied as a variable. However, there was a nonsignificant trend toward older individuals having higher pain levels at 2-year followup [3].
Patient diagnosis or the reason for isolated acetabular revision did not affect patient outcome or pain in this series. To our knowledge, there are no previous studies evaluating preoperative diagnosis as a possible reason for differences in postoperative patient outcomes.
Bone loss as defined by Paprosky et al. [12] did not affect outcomes, pain levels, or rerevisions in our series. Weeden and Paprosky [16] found patients with Paprosky Type I or II defects had a low rerevision rate (2%), and patients with Paprosky Type III defects had a high rerevision rate (19%). They did not comment on pain or functional outcomes in their series [16]. The authors did not use structural allograft in any of the acetabular revisions in their series. They recommended the use of structural allograft with peripheral screws to augment the stability of revision acetabular components having a Paprosky Type III defect. The rerevision rate in this series was 8% for Types I and II and 0% for Type III. The use of structural allograft in our series may explain the lower rerevision rate for hips with Paprosky Type III acetabular defects when compared to Weeden and Paprosky [16].
Bone stock was assessed with the femoral index, and 0.56 or greater represented osteopenic bone. Patients with lower femoral indices had higher functional scores preoperatively. Postoperative scores seemed to improve more with a higher osteopenic femoral index. The reason for these results is unclear. To our knowledge, no study has evaluated the relationship between bone stock and clinical outcome after hip revision arthroplasty.
In our series, obese patients had lower preoperative pain scores than nonobese patients. After acetabular revision, obese patients had less improvement in pain scores than nonobese patients. This could be related to lower activity in the obese cohort. This assumption is supported by the data of McClung et al. [9] who quantified the daily activity level of 209 patients with a pedometer and found obese patients were less active.
Kim et al. [7] studied the outcomes of revision hip arthroplasties of nonobese versus obese patients. They reported obese patients were six times more likely to sustain dislocations than nonobese patients, and obese patients were two times more likely to undergo repeat revision surgery than nonobese patients. All revisions were included in this cohort (isolated acetabular, isolated femoral, and total revision). All procedures were performed through the posterior approach. The authors also defined obesity as a BMI of greater than 35 kg/m2 and nonobese as less than 30 kg/m2. Patients in between these two values were not included in the study [7]. Another study of 229 patients by Perka et al. [13] reported overweight patients had an increased operative time in revision hip surgery but no other increase in perioperative complications. Long-term outcomes were not reported [13].
Complications and rerevisions were low in our series. The lack of postoperative instability may be associated with surgical technique and the experience of the surgeon. This favorable finding is surprising and difficult to explain. The surgeon has considerable experience with hip surgery, and the direct lateral approach is associated with low rates of instability. The surgical technique included acetabular cup positioning at 45° abduction and 10° anteversion, restoration of femoral offset, and careful soft tissue balancing in the reconstructed hip.
Isolated acetabular revision operation with cementless hip implants is a reliable procedure to relieve pain and improve function for patients with loose osteolytic acetabula or unstable hips. Obese patients with a BMI of greater than 30 kg/m2 should be counseled on their potential limitation of benefit with regard to pain improvement.
Acknowledgments
We thank Mr. John Garfi for his assistance with data collection and manuscript preparation.
Footnotes
The senior author (WLH) has a consulting agreement and a product development agreement with DePuy Orthopaedics, Inc, Warsaw, IN.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 2.Chen XD, Waddell JP, Morton J, Schemitsch EH. Isolated acetabular revision after total hip arthroplasty: results at 5–9 years of follow-up. Int Orthop. 2005;29:277–280. doi: 10.1007/s00264-005-0674-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis AM, Agnidis Z, Badley E, Kiss A, Waddell JP, Gross AE. Predictors of functional outcome two years following revision hip arthroplasty. J Bone Joint Surg Am. 2006;88:685–691. doi: 10.2106/JBJS.E.00150. [DOI] [PubMed] [Google Scholar]
- 4.Gozzard C, Blom A, Taylor A, Smith E, Learmonth I. A comparison of the reliability and validity of bone stock loss and classification systems used for revision hip surgery. J Arthroplasty. 2003;18:638–642. doi: 10.1016/S0883-5403(03)00107-4. [DOI] [PubMed] [Google Scholar]
- 5.Harris W. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 6.Healey JH, Vigorita VJ, Lane JM. The coexistence and characteristics of osteoarthritis and osteoporosis. J Bone Joint Surg Am. 1985;67:586–592. [PubMed] [Google Scholar]
- 7.Kim Y, Morshed S, Joseph T, Bozic K, Ries MD. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin Orthop Relat Res. 2006;453:142–146. doi: 10.1097/01.blo.0000238874.09390.a1. [DOI] [PubMed] [Google Scholar]
- 8.Manning DW, Ponce BA, Chiang PP, Harris WH, Burke DW. Isolated acetabular revision through the posterior approach: short-term results after revision of a recalled acetabular component. J Arthroplasty. 2005;20:723–729. doi: 10.1016/j.arth.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 9.McClung CD, Zahiri CA, Higa JK, Amstutz HC, Schmalzried TP. Relationship between body mass index and activity in hip or knee arthroplasty patients. J Orthop Res. 2000;18:35–39. doi: 10.1002/jor.1100180106. [DOI] [PubMed] [Google Scholar]
- 10.Mendenhall S. 2008 hip and knee implant review. Orthop Network News. 2008;19:1. www.orthopedicnetworknews.com. Accessed January 10, 2009.
- 11.Moore MS, James MP, Young AM, Engh CA. Radiographic signs of osseointegration in porous-coated acetabular components. Clin Orthop Relat Res. 2006;444:176–183. doi: 10.1097/01.blo.0000201149.14078.50. [DOI] [PubMed] [Google Scholar]
- 12.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 13.Perka C, Labs K, Muschik M, Buttgereit F. The influence of obesity on perioperative morbidity and mortality in revision total hip arthroplasty. Arch Orthop Trauma Surg. 2000;120:267–271. doi: 10.1007/s004020050462. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg A. Revision total hip arthroplasty: indications and contra-indications. In: Lieberman JR, Daniel J, Berry D, eds. Advanced Hip Reconstruction. Rosemont, IL: AAOS; 2005:281–283.
- 15.Saleh KJ, Celebrezze M, Kassim R, Dykes DC, Gioe TJ, Callaghan JJ, Salvati EA. Functional outcome after revision hip arthroplasty: a metaanalysis. Clin Orthop Relat Res. 2003;416:254–264. doi: 10.1097/01.blo.0000093006.90435.43. [DOI] [PubMed] [Google Scholar]
- 16.Weeden SH, Paprosky WG. Porous-ingrowth revision acetabular implants secured with peripheral screws. J Bone Joint Surg Am. 2006;88:1266–1271. doi: 10.2106/JBJS.E.00540. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization Guidelines 2004. Available at: www.who.int/topics/obesity/en/. Accessed May 15, 2006.