Abstract
In THA, anterior or posterior tilt of the pelvis changes the position of the acetabular component on the coronal plane of the body as compared with its anatomic position in the pelvic bone. To understand the occurrence and clinical importance for patients with pelvic tilt on an operating room table in the lateral decubitus position, we studied 436 patients (477 hips) undergoing primary THA using an imageless computer navigation system that measured tilt. We determined the distribution and magnitude of pelvic tilt, especially tilt of 10° or greater. The distribution of tilt had a range of 25° posterior to 20° anterior. Twenty-nine of 477 (6.1%) hips had zero tilt; 251 (52.6%) had tilt of 1° to 5°; 120 (25.2%) had tilt of 6° to 9°; and 77 (16.1%) had tilt of 10° or greater. The conversion factor for acetabular anteversion has been determined by a mathematical formula by Lembeck et al. and was confirmed by us in practice. Measurement of pelvic tilt during the performance of THA will improve the accuracy of cup position, especially allowing anteversion to be measured on the coronal plane.
Level of Evidence: Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
During performance of THA, the pelvis can be tilted different from the coronal plane of the body [3, 5, 13, 17]. Surgeons expect the cup to be on the radiographic plane described by Murray [16]. The radiographic plane is the coronal plane of the body and is the plane on which radiographs are taken. Radiographs are the common measurement of cup position. The anterior pelvic plane has been used commonly with computer navigation for THA, and cup inclination and anteversion relative to the anterior pelvic plane are measured by the navigation software [5, 6, 11, 14, 19]. The anterior pelvic plane measures the cup only in the bony pelvis and does not consider the acetabulum as connected to the longitudinal plane (coronal plane) of the body [5, 13].
The difference between the anterior pelvic plane and the coronal plane is defined as pelvic anterior or posterior tilt [3, 13]. This tilt has a change on cup anteversion when measured on the coronal plane, which has been quantified as 0.7° for each degree of tilt in normal volunteers [13]. A nomogram developed by CT scans and radiographs in patients undergoing THA also has a conversion factor of 0.7° [3]. One study [18] of THA with or without computer navigation using the anterior pelvic plane for cup position found 57% of cups in the freehand group were outliers compared with 20% in the navigation group using the safe zone described by Lewinnek et al. [14]. The failure to compensate for pelvic tilt was suggested as the cause of these outliers.
Imageless computer navigation can measure tilt in a clinical application. Using this technology, we (1) determined the distribution and magnitude of pelvic tilt, especially tilt of 10° or greater, in patients undergoing THA in the lateral decubitus position and (2) confirmed whether tilt in the performance of THA would have cup anteversion with the same geometric mathematical conversion factor of 0.7 as determined by Lembeck et al. [13].
Patients and Methods
We prospectively studied 436 patients (477 hips) who had primary THAs between September 2004 and May 2007 using the Navitrack® Imageless Computer Navigation System (Orthosoft, Inc, Montreal, Canada). There were 216 men and 220 women with a mean age of 62.9 years (range, 23–89 years) (Table 1). Five hundred ninety-nine primary THAs were performed during the period of this study; 113 patients (122 hips) did not have computer navigation.
Table 1.
Demographic and diagnosis data
| Variable | Value |
|---|---|
| Gender | |
| Male | 216 (241 hips) |
| Female | 220 (236 hips) |
| Age (years)* | 62.9 (23–89) |
| Height (m)* | 1.7 (1.4–2.0) |
| Weight (kg)* | 81.7 (37.2–172.4) |
| Body mass index* | 27.3 (17.2–52.7) |
| Side | |
| Left | 227 hips |
| Right | 250 hips |
| Diagnosis | |
| Osteoarthritis | 406 |
| Congenital disease of hip | 43 |
| Posttraumatic osteoarthritis | 3 |
| Rheumatoid arthritis | 9 |
| Avascular necrosis | 16 |
* Values expressed as means, with ranges in parentheses.
With the patient in the supine position on the operating table, and a pelvic tracker fixed to the pelvis, the anterior pelvic plane was registered by percutaneously touching the bone of the most prominent point of both anterior-superior iliac spines and the pubis near the pubic tubercles. The registration pointer had a sharp tip that perforated skin so the iliac crest bone was contacted in thin patients. In patients with more than 2 to 3 mm of fat over the anterior-superior iliac spines, a stab wound was made to the bone with a Number 15 scalpel blade to allow the registration guide to touch bone. In all patients, the skin and fat of the mons pubis were punctured to the pubic bone [7].
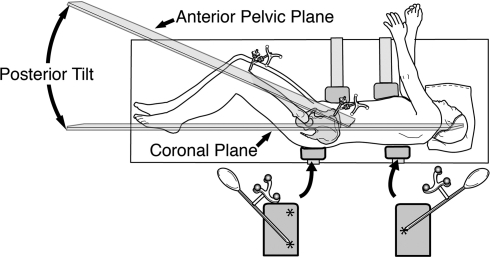
The patient was turned to the lateral position after the pelvic plane registration (flip technique). In the lateral position, the patient was aligned so the tip of the shoulder, high point of the iliac crest, and tip of the greater trochanter were in a straight line representing the longitudinal axis of the body. The patient was secured with two chest supports and two pelvic supports, which maintain this longitudinal plane of the body during surgery (Fig. 1). The rigid posterior supports were attached to the side rail of the operating room table and could not slide in any direction. These supports substituted for the operating table, which is registered as the longitudinal plane of the body when the patient is operated on while supine [3]. The coronal plane (the longitudinal plane) of the body was registered by touching two points on the posterior pelvic support and one on the posterior chest support in the shape of a triangle. Pelvic anterior or posterior tilt was calculated by the software comparing the anterior pelvic plane with the coronal plane. The anteversion selected for the cup was always that adjusted by the computer for tilt (adjusted to the coronal plane).
Fig. 1.
The patient is secured in the lateral position with two chest supports and two pelvic supports with the high point of the shoulder, iliac crest, and greater trochanter aligned in a straight line. The coronal plane (the longitudinal axis plane of the body) is registered by touching two points on the posterior pelvic support and one on the posterior chest support in the shape of a triangle. (Reprinted with permission from the University of Iowa from Dorr LD, Hishiki Y, Wan Z, Newton D, Yun A. Development of imageless computer navigation for acetabular component position in total hip replacement. Iowa Orthop J. 2005;25:1–9.)
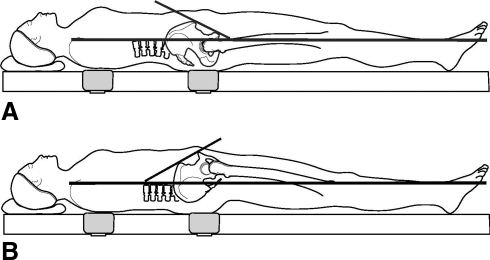
Anterior or posterior pelvic tilt is defined as the angle between the anterior pelvic plane and the coronal plane of the body [19]. (Pelvic tilt also has been called pelvic inclination and reclination [2, 4].) Zero pelvic anteroposterior tilt occurs when the anterior pelvic plane is parallel to the coronal plane [13]. Pelvic anterior tilt is present when the distance between the middle point of the two anterior-superior iliac spines and the coronal plane is longer than the distance between the anterior surface of the symphysis pubis and the coronal plane (Fig. 2A). The opposite relationship is pelvic posterior tilt (Fig. 2B). Although the anterior-posterior pelvic plane was measured with the patient supine, we measured the tilt of the pelvis when the patient was in the lateral decubitus position on the operating table. The value of anteversion measured on the anterior pelvic plane was adjusted to the radiographic coordinate system of Murray [16] on the coronal plane. This change is according to the formula described by Murray [16]. All calculations were completed by the computer software so the nonadjusted (anterior pelvic plane) and adjusted (coronal plane) anteversions were shown on the computer screen.
Fig. 2A–B.
(A) A diagram shows anterior pelvic tilt. The distance between the middle point of two anterior-superior iliac spines and the coronal plane is longer than that between the anterior surface of the pubic symphysis and the coronal plane. (B) Pelvic tilt is seen in this diagram. The distance between the middle point of the two anterior-superior iliac spines and the coronal plane is shorter than that between the anterior surface of the pubic symphysis and the coronal plane. (Reprinted with permission from The Association of Bone and Joint Surgeons from Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467:32–42.)
The precision and bias of the adjusted cup position for tilt have been validated with the true value being a postoperative CT scan [10]; for inclination, the bias was 0.03° and the precision was 4.4°, and for anteversion, the bias was 0.73° and the precision was 4.1°. Precision and bias were calculated according to the American Standards for Testing and Materials criteria [1]. The precision of a measurement process is the closeness of agreement between test results from the measurement process being evaluated. The bias of a measurement process is a consistent or systemic difference between a set of test results from the process and an accepted reference value (true value) of the property being measured.
The accuracy of pelvic tilt measurement was validated with a phantom pelvis [15, 20]. The phantom model was constructed to scale and to reproduce an anatomic pelvis maintaining distances between the anterior-superior iliac spines and the pubic tubercles. The anterior pelvic plane was constructed by embedding three metal markers to represent the right and left anterior-superior iliac spines and the pubic tubercle midpoint. These landmarks were the reference points marking the anterior pelvic plane for clinical navigation. A block was placed at the apex of the phantom so that different tilt positions were generated: 0° tilt and with anterior and posterior tilt measurements were made at 6°; and the computer navigation value of tilt could be compared with it. The precision was 1° and the bias was 0.5° of computer navigation-measured tilt [15, 20].
The data for each operation were recorded and stored in our computerized patient database. The distribution of the tilt was recorded, as were acetabular inclination and anteversion on the anterior pelvic plane (Murray’s anatomic definition) and acetabular inclination and anteversion on the coronal plane (Murray’s radiographic definition) [16]. The relationship between tilt and anteversion adjusted to the coronal plane was compared to confirm the conversion factor of 0.7 reported by Lembeck et al. [13]. The magnitude of tilt for each of the 477 hips was measured and distributed into those having zero tilt, posterior tilt or anterior tilt of 1° to 5°; posterior or anterior tilt of 6° to 9°; and posterior or anterior tilt of 10° or greater (Table 2).
Table 2.
Distribution of pelvic anteroposterior tilt in 477 hips
| Pelvic anteroposterior tilt | Mean ± SD (º) | Number of hips | Percentage |
|---|---|---|---|
| Posterior tilt ≥ 10º | 13.6 ± 3.3 | 56 | 11.7% |
| Posterior tilt 6°–9º | 7.3 ± 1.1 | 71 | 14.9% |
| Posterior tilt 1°–5º | 2.9 ± 1.4 | 138 | 28.9% |
| Zero pelvic tilt | 0 | 29 | 6.1% |
| Anterior tilt 1°–5º | 2.9 ± 1.4 | 113 | 23.7% |
| Anterior tilt 6°–9º | 7.3 ± 1.0 | 49 | 10.3% |
| Anterior tilt ≥ 10º | 11.8 ± 2.3 | 21 | 4.4% |
SD = standard deviation.
Results
The distribution of tilt showed posterior tilt was more common than anterior tilt in the lateral decubitus position (Table 2). The magnitude of tilt in these hips ranged from −25° (posterior) to +20° (anterior). Overall, pelvic posterior tilt occurred in 265 of 477 hips (55.5%; range, −1° to −25°) and pelvic anterior tilt occurred in 183 hips (38.4%; range, 1°–20°). Twenty-nine hips (6.1%) had zero tilt. Seventy-seven of 477 hips (16.1%) had anterior or posterior pelvic tilt of 10° or greater.
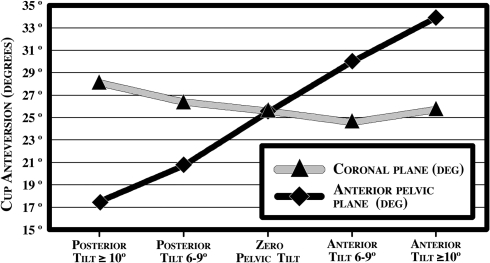
As tilt increases, the discrepancy between the anterior pelvic plane and the coronal plane widens (Fig. 3). Each degree of anterior or posterior tilt changed cup anteversion by 0.8°. Seventy-seven hips (16.1%) with anterior or posterior pelvic tilt of 10° or greater had a range of cup anteversion from 8° to 20°. For this series of hips, 101 (21.2%) had cup anteversion changed between 5° to 9° and 36 hips (7.5%) had a change in cup anteversion of 10° or greater from the anterior pelvic plane to the coronal plane.
Fig. 3.
The magnitude of the effect of tilt on cup anteversion is shown.
The mean change of inclination between the anterior pelvic plane and coronal plane in all 477 hips was less than 2° (mean ± standard deviation, 1.7° ± 1.5°). Therefore, discussion of the impact of pelvic tilt on cup position was confined to anteversion.
Discussion
Tilt affects cup position when it is measured on the coronal plane of the body [3, 5, 13, 17]. Lembeck et al. [13] determined a mathematical relationship of acetabular anteversion to pelvic tilt that we confirmed in practice. We were interested in how often tilt of the pelvis occurred during THA and to what magnitude. A 10° magnitude of tilt creates an absolute error of 8° in judging the cup on the coronal plane and this is additive to measurement errors of the surgeon’s estimate [9]. Additional error in the combined anteversion will occur in judgment of the femoral stem anteversion, which cannot be ignored because the hip is being reconstructed. The safe zone for combined anteversion is 37° ± 12°, so an error of 8° acetabular anteversion by 10° of pelvic tilt leaves little room for measurement error of the cup and stem. We therefore (1) determined the distribution and magnitude of pelvic tilt in patients undergoing THA in the lateral decubitus position, especially tilt of 10° or greater, and (2) confirmed whether the geometric mathematical conversion factor of 0.7, previously determined by Lembeck et al. [13], would be consistent with the findings in the performance of THA.
We acknowledge several limitations. First, the pelvic anterior or posterior tilt was tested only with one computer navigation system. The accuracy of tilt in this software was validated [15, 20]. Second, the longitudinal plane was not validated quantitatively, but the patient was secured in the same position for every procedure so the coronal plane in all patients was in the qualitatively same position. Furthermore, the distance between the two supports was more than 500 mm. By mathematics, this distance between the supports means 5 mm of change in distance between the posterior chest wall and the midcoronal plane of the patient will result in error of the coronal plane of less than 0.6°. This effect is too small to affect the measurements. The two posterior supports are no different from the operating table, which is accepted as the longitudinal plane for patients who undergo surgery in the supine position [3]. Third, the values we obtained for anteversion and inclination are valid only for software using Murray’s radiographic definition [16] for the anterior pelvic plane and the coronal plane. Other computer systems using the operative or anatomic definition of Murray would differ. Fourth, the computer navigation cup inclination and anteversion depend on accurate registration of the anterior pelvic plane. These patients were operated on after we had learned the techniques necessary for accurate registration [7, 8]. The accuracy of registration is validated by CT scan results [10]. Last was the need to use a flip technique for operating in the lateral position. However, use of the posterior supports for the longitudinal plane of the body gives reproducible results for cup anteversion as measured by computer navigation, radiographs, and CT scans [7, 8].
The importance of our data is documenting the frequency and magnitude of pelvic tilt when patients undergo THA in the lateral position. We confirmed in practice the mathematical geometric relationship of acetabular anteversion to pelvic tilt as described by Lembeck et al. [13]. Pelvic tilt affects the expected cup anteversion on the coronal plane. The coronal plane is the functional cup position and placing the cup on this plane provides the anteversion the surgeon expects when measuring its radiographic position. Sixteen percent of hips had cup anteversion 8° to 20° different on the coronal plane from that expected from its position in the pelvis. Tilt varied from a mean of 25° posterior to a mean of 20° anterior. The pelvis tilts a mean of approximately 4° to 5° as patients move from the supine to the lateral position, supine to standing position, and between the preoperative and postoperative supine position [3, 5, 13, 17]. All these authors who studied pelvic positions concluded tilt should be considered when implanting an acetabular component and a constant anteversion angle should not be selected. Current knowledge of the influence of pelvic tilt [3, 10, 13, 18, 20] and the importance of combining cup anteversion with cementless stem anteversion for a safe combined anteversion [9, 21, 22] suggests a paradigm shift from the traditional technique of targeting cup anteversion in the safe zone on the anterior pelvic plane described by Lewinnek et al. [14].
We quantified distribution of anterior or posterior pelvic tilt as measured by computer navigation in patients having THA. The wide variability of tilt and flexibility of the pelvis we observed confirmed previous studies [5, 13, 17]. Anterior or posterior pelvic tilt has the greatest potential to become clinically relevant for affecting cup position when it exceeds 10° and this was seen in 77 of 477 (16.1%) hips. The use of an imageless computer navigation system that converts anatomic cup anteversion to coronal plane cup anteversion may compensate for the interindividual variability of pelvic tilt. The use of coronal plane anteversion mated with femoral stem anteversion inside a combined anteversion safe zone of 25° to 50° seems to be the safe position of THA components and emphasizes the importance of quantifying tilt [9, 12, 21, 22].
Acknowledgments
We thank Patricia Paul for assistance in preparing this manuscript.
Footnotes
One or more of the authors (LDD) have received funding from the Dorr Arthritis Research Foundation.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research and that informed consent for participation in the study was obtained.
References
- 1.Annual Book of American Society for Testing and Materials Standards. West Conshohocken, PA: ASTM International; 2002. [Google Scholar]
- 2.Anda S, Svenningsen S, Grontvedt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum: a radiographic, computed tomographic and clinical investigation. Acta Radiol. 1990;31:389–394. [PubMed] [Google Scholar]
- 3.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–365. doi: 10.2106/JBJS.F.00628. [DOI] [PubMed] [Google Scholar]
- 4.Chen E, Goertz W, Lill CA. Implant position calculation for acetabular cup placement considering pelvic lateral tilt and inclination. Comput Aided Surg. 2006;11:309–316. doi: 10.1080/10929080601090516. [DOI] [PubMed] [Google Scholar]
- 5.DiGioia AM, Hafez MA, Jaramaz B, Levison TJ, Moody JE. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272–276. doi: 10.1097/01.blo.0000238862.92356.45. [DOI] [PubMed] [Google Scholar]
- 6.DiGioia AM, Jaramaz B, Blackwell M, Simon DA, Morgan F, Moody JE, Nikou C, Colgan BD, Aston CA, Labarca RS, Kischell E, Kanade T. The Otto Aufranc Award. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res. 1998;355:8–22. doi: 10.1097/00003086-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Dorr LD. Hip Arthroplasty: Minimally Invasive Techniques and Computer Navigation. Philadelphia, PA: Saunders Elsevier; 2006. [Google Scholar]
- 8.Dorr LD, Hishiki Y, Wan Z, Newton D, Yun A. Development of imageless computer navigation for acetabular component position in total hip replacement. Iowa Orthop J. 2005;25:1–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467:119–127. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–99. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 11.Ecker TM, Tannast M, Murphy SB. Computed tomography-based surgical navigation for hip arthroplasty. Clin Orthop Relat Res. 2007;465:100–105. doi: 10.1097/BLO.0b013e3181591c7d. [DOI] [PubMed] [Google Scholar]
- 12.Komeno M, Hasegawa M, Sudo A, Uchida A. Computed tomographic evaluation of component position on dislocation after total hip arthroplasty. Orthopedics. 2006;29:1104–1108. doi: 10.3928/01477447-20061201-05. [DOI] [PubMed] [Google Scholar]
- 13.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–523. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 14.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 15.Malik A, Wan Z, Jaramaz B, Bowman G, Dorr LD. A validation model for measurement of acetabular component position. J Arthroplasty. 2009 June 22 [Epub ahead of print]. [DOI] [PubMed]
- 16.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 17.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140–151. doi: 10.1097/01.blo.0000069891.31220.fd. [DOI] [PubMed] [Google Scholar]
- 18.Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty: a prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494–499. doi: 10.2106/JBJS.F.00529. [DOI] [PubMed] [Google Scholar]
- 19.Tannast M, Langlotz U, Siebenrock KA, Wiese M, Bernsmann K, Langlotz F. Anatomic referencing of cup orientation in total hip arthroplasty. Clin Orthop Relat Res. 2005;436:144–150. doi: 10.1097/01.blo.0000157657.22894.29. [DOI] [PubMed] [Google Scholar]
- 20.Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467:32–42. doi: 10.1007/s11999-008-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39:1315–1323. doi: 10.1016/j.jbiomech.2005.03.008. [DOI] [PubMed] [Google Scholar]