Abstract
Larger diameter metal-on-metal (MOM) bearing hips offer the possibility of low wear and reduced risk of dislocation. We reviewed the first 126 patients (131 hips) who had a large-head (36-mm) MOM bearing surface to report the early clinical outcome and especially to determine the occurrence of dislocation and wear-related concerns. The minimum followup was 5 years (mean, 5.6 years; range, 5–7 years). We found a 98% survivorship free of component revision. No hips had been revised for dislocation. Three hips (2%) had small femoral osteolytic lesions. Because this series of patients did not completely represent our experience with this bearing surface, we queried our database for the 828 patients (945 hips) that had the same bearing surface from April 2001 to December 2008. Three patients (0.3%) had a local reaction to the MOM bearing surface on revision-retrieved tissue. All three patients presented with elevated inflammatory indices, and a purulent-appearing joint effusion at revision. The possibility of infection and the delay in diagnosing a reaction to the MOM bearing with pathology complicated management of these three patients. We continue to use this bearing surface because the 5-year results are comparable to other bearing surfaces, however, we counsel patients that a local adverse reaction to the MOM bearing surface may be a factor contributing to reoperation.
Level of Evidence: Level IV, retrospective clinical cohort. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Metal-on-metal (MOM) bearings for total hip arthroplasty are an alternative to traditional polyethylene bearing surfaces [12, 17]. One current estimate suggests they are used in 35% of total hip arthroplasties performed in the United States [2]. Hip simulators demonstrate MOM bearings have lower wear volume than metal-on-polyethylene bearings and the amount of wear decreases as head size increases [9, 22]. Therefore manufacturers have developed MOM bearings with larger head diameters than is possible with other bearing surfaces. Dislocation is currently the most common reason for reoperation in the United States, representing 22.5% of hip revisions [3]. The combination of low wear and larger head sizes to reduce dislocation explains the popularity of this bearing surface [12]. However, clinical reports have identified concerns related to osteolysis, metal ion release, and local adverse tissue reactions to the MOM bearings [4, 6, 11–13, 19]. There are three components to this manuscript: (1) a 5-year reporting on the first 126 patients who had a large-head MOM total hip arthroplasty with one design; (2) a query of all 828 patients from our institution with the same bearing surface for failures associated with an adverse tissue reaction to the bearing surface, included because the 5-year clinical review of the first patients did not fully address our experience with this bearing; and (3) a description of the presentation and treatment of the three patients that had revision-retrieved tissue consistent with an adverse local reaction possibly attributable to the MOM bearing surface.
The rationale for reporting the first 126 patients with this bearing surface was to confirm that the early results using a large-head MOM bearing are acceptable and to document dislocation or wear-related findings [7, 8, 15, 16, 18, 20, 21]. Although there are several reports of hip arthroplasty with larger diameter MOM bearing surfaces, most focus on a hybrid total resurfacing arthroplasty [1, 4, 5, 14, 23]. Component-to-component impingement and dislocation which are reported with 28-mm MOM implants are, in theory, less likely with a 36-mm bearing surface [7, 16].
The rationale for including the database query of 828 patients with this bearing surface, as a second component, was to allow a reporting of all known reoperations and especially those that had an adverse local reaction possibly attributable to the MOM bearing surface. Local adverse tissue reactions to MOM bearings are difficult to diagnose [13] and can mimic a prosthetic infection [19]. Complications that are difficult to diagnose and occur infrequently require a large number of cases to determine a frequency and may not be noted at all in smaller series.
The rationale for reporting the three cases that had revision retrieved tissue consistent with a reaction to a MOM bearing was to describe our learning curve in these patients. Illustrating the difficulty treating these patients will help the reader understand our evolving algorithm employed when faced with a patient that has a failing metal-on-metal bearing hip.
Patients and Methods
We retrospectively reviewed our first 126 patients (131 hips) who had total hip arthroplasties using a 36-mm Ultamet ball (DePuy Inc, Warsaw, IN) and liner matched with a Pinnacle acetabular shell (DePuy) and either an AML (DePuy) or Prodigy (DePuy) extensively porous-coated implant between April 2001 and November 2002. The mean patient age at the time of surgery was 53 ± 10 years (range, 25–78 years) and 57% were men. The mean body mass index was 29. The primary diagnosis was osteoarthritis (77%), followed by developmental dysplasia (8%), avascular necrosis (7%), fracture (5%), and rheumatoid arthritis (3%). Of the 126 patients (131 hips), 114 patients (119 hips) either died with a current followup or had a minimum 5-year evaluation. This represents 91% of the hips and 90% of the first patients to receive this bearing surface. This bearing surface was chosen for higher-demand patients and the occasional patient at risk for dislocation. During those dates, 631 primary hip surgeries were performed at our institution with the 131 from this study representing 21% of the hip surgeries. The patients who did not receive a 36-mm MOM bearing had a mean age of 66 years (range, 35–97 years) and 42% were men. We had prior IRB approval.
To determine the frequency of histology documented local MOM bearing surface reactions, we queried our database for all 828 patients (945 hips) operated by us using the 36-mm Ultamet MOM bearing surface. These surgeries were performed between April 2001 and December 2008 and include the first 126 patients previously mentioned. Of the 945 hips in the database, 153 (16%) had more than a 5-year followup, 231 (24%) had been followed between 2 and 5 years, and 274 (29%) had less than 2 years of followup. In addition, we report all other known component revisions in the cohort of 945 hips and the percentage of those revisions that were known to have a possible tissue reaction to the MOM bearing.
The AML and Prodigy stems are chrome cobalt extensively porous-coated femoral implants. The Pinnacle acetabular shell is a porous-coated titanium shell that has a self-locking peripheral taper to accommodate the Ultamet metal acetabular liner (Fig. 1). The Ultamet liner and ball are wrought high carbon content alloys. The manufacturer’s clearance for this bearing surface is 100 μm ± 20 μm.
Fig. 1.
A picture of the bearing surface is shown so that readers unfamiliar with the implant can better understand the design. It is possible that the design and manufacturing of metal-on-metal bearing surfaces may influence the results. The Pinnacle titanium porous-coated cup with locking taper is shown. The bearing surface consists of a high carbon content Ultamet liner and 36-mm ball with 100 μm ± 20 μm clearance.
Patients are asked to return for followup at 4 weeks, 4 months, 1, 2 and 5 years after surgery. Preoperatively and at each visit we recorded the Harris hip scores. For the first 131 hips, we determined implant stability and the presence of osteolysis on serial low anterior posterior pelvis radiographs suitable for measuring both femoral and acetabular migration. All radiographic evaluations were performed by a single reviewer (CAE Jr). Femoral stability was defined as loose, fibrous stable, or bone ingrown using cementless implant stability criterion [10]. Acetabular components were either stable or loose. Loose acetabular components demonstrated migration of 3 mm or more or an inclination change of more than 5° on serial radiographs. Acetabular inclination and migration were measured from the interteardrop line. Osteolysis was defined as a geographic area of decreased periprosthetic bone density with a clearly defined border that was not present on the immediate postoperative radiograph [25].
The diagnosis of a local adverse reaction attributable to the metal-on-metal bearing surface is based on a light microscopic analysis of hematoxylin and eosin stained periarticular tissue performed by a single independent pathologist with expertise in metal-on-metal bearing surface pathology [4, 6, 24].
We performed a Kaplan-Meier survivorship analysis with an endpoint of component exchange on the current followup of all 126 patients (131 hips). A Kaplan-Meier survivorship analysis with an endpoint of revision associated with a local adverse reaction attributable to the metal-on-metal bearing was then performed on the current followup of all 945 hips.
Results
Among the first 126 patients with this bearing we performed two component revisions. Neither was associated with an adverse reaction to the MOM bearing surface. The 5-year survivorship free of component revision is 98% (95% confidence interval, 96–100%). Two patients gave a history consistent with a self-reducing hip subluxation occurring at 1 and 5 years after surgery. One patient had a closed reduction of a hip dislocation at 2 years after surgery. The radiographic review revealed one additional patient with a loose femoral component that was asymptomatic, and two patients with fibrous stable femoral components. There are no cases of loose acetabular components. Three patients had radiographic evidence of osteolysis. All three osteolytic lesions occurred in the proximal femur. Two involved Gruen Zone 7, and one was located in Gruen Zone 1 (Fig. 2A–C). The postoperative Harris hip score was 89 (range, 49–100), increased from the preoperative Harris hip score 48 (range, 20–71). Thirteen patients had a postoperative Harris hip score less than 70.
Fig. 2A–C.
(A) An immediate postoperative AP radiograph is shown for comparison to later radiographs. (B) A 5.6-year followup radiograph of the same patient shows greater trochanteric osteolysis having a geographic pattern and well-defined boarders. (C) A lateral view of same osteolytic lesion is shown. The occurrence of radiographically visible osteolysis may be indicative of a reaction to metal-on-metal wear.
The database query on all 828 patients with the same bearing surface identified eight patients with a known component revision (Table 1). Those eight cases include the two femoral revisions already reported. Three of the eight revisions from our database had histology consistent with a reaction to a MOM bearing. Of the eight revisions, five had tissue available for review, and three of the five were positive. The three cases of the 945 hips performed results in a 0.3% occurrence of a local tissue reaction probably attributable to a MOM implant. A survivorship analysis of the 945 hips reveals a 1% (95% confidence interval, 0–2%) chance at 3 years that revision retrieved tissue consistent with a reaction to a MOM bearing will be identified.
Table 1.
Revisions
| Case | Date of revision | Reason for revision | Years to revision | Tissue available | Hypersensitivity positive | Revision procedure and bearing |
|---|---|---|---|---|---|---|
| 1 | 4/03 | Failure femoral fixation | 0.2 | Yes | Negative | Femoral revision to new MOM† |
| 2 | 2/05 | Stem fracture | 1.7 | Yes | Positive | Two-stage complete conversion to MOP |
| 3 | 5/05 | Failure femoral fixation | 0.4 | No | N/A | Femoral revision using same MOM‡ |
| 4* | 6/05 | Failure femoral fixation | 3 | Yes | Negative | Femoral revision using same MOM‡ |
| 5* | 2/06 | Stem fracture | 4.6 | No | N/A | Primary conversion to new MOM† |
| 6 | 5/06 | Failure femoral fixation | 0.8 | No | N/A | Femoral revision using same MOM‡ |
| 7 | 3/07 | Failure femoral fixation | 2.1 | Yes | Positive | Two-stage complete conversion to MOP |
| 8 | 9/08 | Hypersensitivity | 3.2 | Yes | Positive | Primary conversion to MOP with abx. suppression |
* These cases are reported in the consecutive cohort with minimum 5-year followup.
†These patients had a new 36-mm metal ball placed in the existing Ultamet liner.
‡These patients had only a femoral component exchange. The original 36-mm ball was placed back in the existing Ultamet liner.
The case reports of patients who had a histologically confirmed adverse local reaction likely related to the bearing surface illustrate the difficulties we encountered. The first two patients presented with failed femoral components 1.7 and 2.1 years after their MOM bearings were implanted. The erythrocyte sedimentation rates (ESR) were 70 mm/hr (normal 0.0–30 mm/hr) and 99 mg/hr (normal 0–10 mm/hr) while the C-reactive proteins (CRP) were 31 mg/L (normal 0.0–4.9 mg/L) and 93 mg/L (normal 0–9 mg/L) in both patients. At surgery, a creamy fluid presumed to be purulence was encountered. A decision was made to do a two-stage revision for a presumed infection. Cultures were negative and histology consultation after the revisions revealed a dense lymphoplasmacytic infiltrate consistent with a local tissue reaction probably related to the MOM bearing (Fig. 3). Both patients currently have a metal-on-polyethylene bearing hip. The third patient developed trochanteric bursitis symptoms 7 months after surgery. By 29 months, he had increased pain, buttock swelling, an ESR of 93 mm/hr (normal 0–20 mm/hr) and a CRP of 119 mg/L (normal 0–8 mg/L). An aspiration at an outside hospital was negative. Because hypersensitivity was suspected, a MRI was obtained. The report described a “massively expanded pseudocapsule, extending through dehiscent abductors and creating a large fluid collection that contains bulky low signal intensity debris, consistent with severe particle disease.” The musculoskeletal radiologist further stated that “the diagnosis of particle disease is strongly favored over that of active infection.” The preoperative diagnosis was a MOM hypersensitivity, and a bearing surface conversion to a metal-on-polyethylene bearing was performed with retention of the femoral and acetabular components. At surgery a creamy purulent-appearing fluid was noted along with a thickened hip capsule, and tissue necrosis of the hip abductors. Subsequent cultures were positive for coagulase-negative Staphylococcus aureus. A pathology consultation on the capsular tissue revealed a predominance of plasma cells which, although unusual, was consistent with a metal sensitivity reaction. The patient is currently on IV antibiotic suppression.
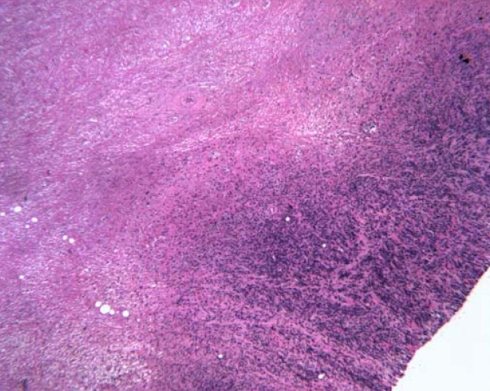
Fig. 3.
A photomicrograph shows tissue from case 2. There is a high-density and extent of lymphocyte infiltration in this section of capsular tissue. (Stain, hematoxylin and eosin; original magnification, ×40.)
Discussion
The rationale for this manuscript was to report our center’s experience with a modular 36-mm MOM bearing surface. There are three components to this study. The first component comprises the results of the first patients at our institution to have a 36-mm modular MOM bearing surface. We were interested in a 5-year survivorship, dislocations, and osteolysis. Because we had encountered failures associated with an adverse local tissue response possibly related to the MOM not apparent in the initial series, we queried our database for all revisions of this bearing surface. This was the second component of the manuscript in which we wanted to determine the incidence of these reactions. The third component was a presentation of the failures attributable to an adverse local reaction occurring in these patients with a MOM bearing. This component highlights the difficulty differentiating these occurrences from infection [19].
The manuscript is limited by the fact that the patients with an adverse local reaction occurring with this MOM bearing surface were the first we encountered. As such they represent our learning curve. The diagnosis appears to be uncommon and requires retrieval and pathologic review of tissue obtained at revision. Because tissue was not analyzed in all revisions, the results may underestimate the frequency of this finding. However, this is a limitation of most other publications that have included histologic analysis of MOM revision cases [4, 14–16, 20, 24]. This limitation exists because a local tissue reaction possibly attributable to a MOM bearing is diagnosed only after revision, is a relatively new diagnosis, and there has not been an adequate period of time to put in place prospective protocols to determine the frequency of its occurrence [11, 13].
The first portion of the manuscript reports 98% survivorship of this bearing surface at 5 years. This survivorship is comparable to other studies with a MOM bearing (Table 2) [7, 8, 15, 16, 18, 20, 21]. A source of concern is the three incidences (2%) of femoral osteolysis. One of the reasons MOM bearing implants have been adopted is the hope that low wear will result in a reduction of periprosthetic osteolysis [8, 12, 13, 17]. Dislocation is a cause of revision in some 28-mm MOM bearing surface reports [7, 8, 16]. Although we had one hip (0.7%) with a dislocation, there have been no reoperations for dislocation in our series. Implant-to-implant impingement, while being noted in some MOM series with smaller heads, was not seen in this series with a 36-mm head [8, 22].
Table 2.
Metal-on-metal total hip arthroplasty results
| Reference | Hips | Age | Followup (years) | Osteolysis | Dislocation | Revisions | Survivorship |
|---|---|---|---|---|---|---|---|
| Delaunay [7] | 100 | 60 | 6 | 2% | 5% | 5% | 97% at 8 years |
| Korovessis et al. [15] | 217 | 55 | 6.4 | 3.7% | 0.9% | 6.5% | 98% cup and 93% stem at 9 years |
| Milosev et al. [20] | 640 | 57 | 7.1 | 2.5% | 0.3% | 5.3% | 91% at 10 years |
| Migaud et al. [18] | 39 | 40 | 5.7 | None | None | None | 100% at 5 years |
| Long et al. [16] | 161 | 55 | 6.5 | None | 2.5% | 3.7% | Not reported |
| Park et al. [21] | 169 | 55 | 2.3 | 5.9% | Not reported | 1.2% | Not reported |
| Dorr et al. [8] | 70 | 70 | 5.2 | None | 4% | 4.2% | 94% at 7 years |
| Engh Jr et al. [current study] | 131 | 53 | 5.6 | 2% | 0.7% | 1.5% | 98% at 5 years |
The second portion of this report utilizes our database to account and classify the cause of all know failures with this 36-mm MOM bearing surface at our institution (Table 1). In particular, we were interested in patients thought to have an adverse local tissue reaction possibly attributable to the MOM bearing. We have compared our experience with other reports that also include a tissue diagnosis of a reaction possibly related to the MOM bearing (Table 3). These studies report a range from 0% to 4% of patients compared to the 0.3% occurrence of a possible reaction to a MOM bearing in our study. One possible explanation for this difference is that variations in metallurgy and clearance could cause different MOM bearings to have different results. Other factors could be the relatively new nature of this finding and the absence of a strict pathologic criterion for diagnosis.
Table 3.
Publications with histology documented MOM adverse reactions
| Reference | Implant | Total cases | Revisions | Histology | When positive histology |
|---|---|---|---|---|---|
| Park et al. [21] | Ultima 28 mm THA | 169 | 2 (1.2%) | 2 (1.2%) | 1—recurrent dislocation 1—osteolysis |
| Korovessis et al. [15] | Sikomet 28 THA | 217 | 14 (6.5%) | 11 (5%) | 9—loosening 2—infection |
| Milosev et al. [20] | Sikomet 28 THA | 640 | 34 (5%) | 13 (2%) | 11—loosening 2—unexplained pain |
| Jameson et al. [14] | ASR Total resurfacing | 254 | 8 (3.1%) | 3 (1.2%) | 3—unexplained pain |
| Campbell et al. [4] | BHR Total Resurfacing | 1500 estimated | Not reported | 4 (0.3%) | 4—unexplained pain |
| Engh Jr et al. [current study] | Ultamet 36 THA | 945 | 8 (1%) | 3 (0.3%) | 1—broken stem, 1—loosening, 1—unexplained pain |
| Combined reports | 3725 | 66 (2%) | 36 (1%) | 10—unexplained pain 21—loosening 5—other |
The final component of our manuscript illustrates the difficulty we had treating three patients that we found to have tissue positive for a possible reaction to a MOM bearing hip. In two of our cases, the creamy, purulent-appearing fluid caused us to perform a two-stage complete revision, although subsequent cultures from the fluid were negative. These cases might have been successfully treated with a single-stage bearing surface conversion to a non-MOM bearing. In our last case, knowledge of the two previous aseptic cases, the patient’s presentation with pain, elevated inflammatory indices, a negative aspiration, and the operative findings of creamy fluid with tissue necrosis influenced our decision to do an isolated bearing surface exchange. In that case, the patient had a Gram-positive infection and a tissue reaction consistent with a MOM bearing surface reaction. The difficulty of treatment relates to the surprise intraoperative finding of purulent-appearing fluid consistent with infection. Currently we consider a reaction to a MOM bearing a possible diagnosis in all failed MOM bearing hips. An ESR, CRP, and a hip aspiration for culture and sensitivity are performed preoperatively. If the ESR and CRP are normal, then infection and a metal reaction are less likely. If the ESR and CRP are elevated, then infection and a metal reaction are differentiated from each other by the aspiration culture results. If the culture is negative we consider a bearing surface exchange to a non-MOM implant even if purulent-appearing fluid and a thickened capsule are seen at revision. Although not obtained in these cases, we believe ion levels from blood and joint fluid along with cell counts of joint fluid should be done. Skin testing for metal allergy, blood lymphocyte proliferation assay, and imaging studies such as CT and MRI should be considered. As more cases are encountered these tests will find their way into an algorithm for diagnosis and treatment.
In summary, the 5-year survivorship of our first patients is good and dislocations are uncommon. Osteolysis present in 2% of our cases warrants further followup and is not inconsistent with other clinical cohorts. However, our experience with the first group of patients did not fully describe our experience with this bearing surface. A database review identified an adverse tissue reaction possibly related to the MOM bearing in 0.3% of hips. In hindsight, if we had known to consider a local metal sensitivity as a diagnosis we might have treated these patients differently. Currently we consider a local reaction to a MOM bearing as a possible diagnosis in all failed MOM bearing surfaces. We rule out infection and change the bearing surface to a non-MOM bearing at the time of revision. We continue to use this bearing surface in our own patients but believe it is important to counsel patients about the possibility that a tissue reaction to bearing surface wear could be a factor associated with reoperation.
Acknowledgments
We thank Pat Campbell PhD,Director, Implant Retrieval Lab, Orthopaedic Hospital UCLA, Los Angeles, California for performing the tissue analysis on our cases.
Footnotes
The institution of the authors (Anderson Orthopaedic Research Institute) has received funding from Inova Health Services, Alexandria, VA. The authors’ institution has received funding from a cooperative agreement that was awarded and administered by the U.S. Army Medical Research & Materiel Command (USAMRMC), and the Telemedicine & Advanced Technology Research Center (TATRC), under Contract Number W81XWH-05-2-0079. Two of the authors (CAE, CAE Jr.) are consultants of DePuy Orthopaedics, Inc. (Warsaw, IN) and receive royalty from DePuy Orthopaedics, Inc.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC, Beaulé PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J. Bone Joint Surg. Am. 2004;86:28–39. [PubMed] [Google Scholar]
- 2.Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:1614–1620. doi: 10.2106/JBJS.H.01220. [DOI] [PubMed] [Google Scholar]
- 3.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 4.Campbell P, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J. Arthroplasty. 2008;23:1080–1085. doi: 10.1016/j.arth.2007.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J. Bone Joint Surg. Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 6.Davies AP, Willert HG, Campbell PA, Learmonth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J. Bone Joint Surg. Am. 2005;87:18–27. doi: 10.2106/JBJS.C.00949. [DOI] [PubMed] [Google Scholar]
- 7.Delaunay CP. Metal-on-metal bearings in cementless primary total hip arthroplasty. J. Arthroplasty. 2004;19(8 Suppl 3):35–40. doi: 10.1016/j.arth.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation, Four to seven-year results. J. Bone Joint Surg. Am. 2000;82:789–798. doi: 10.2106/00004623-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Dowson D, Hardaker C, Flett M, Isaac GH. A hip joint simulator study of the performance of metal-on-metal joints: Part II: design. J. Arthroplasty. 2004;19(8 Suppl 3):124–130. doi: 10.1016/j.arth.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 10.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin. Orthop. Relat. Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 11.Hallab N, Merritt K, Jacobs JJ. Metal sensitivity in patients with orthopaedic implants. J. Bone Joint Surg. Am. 2001;83:428–436. doi: 10.1302/0301-620X.83B3.9674. [DOI] [PubMed] [Google Scholar]
- 12.Huo MH, Gilbert NF. What’s new in hip arthroplasty. J. Bone Joint Surg. Am. 2005;87:2133–2146. doi: 10.2106/JBJS.E.00474. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs JJ, Hallab NJ. Loosening and osteolysis associated with metal-on-metal bearings: A local effect of metal hypersensitivity? J. Bone Joint Surg. Am. 2006;88:1171–1172. doi: 10.2106/JBJS.F.00453. [DOI] [PubMed] [Google Scholar]
- 14.Jameson SS, Langton DJ, Natu S, Nargol TV. The influence of age and sex on early clinical results after hip resurfacing: an independent center analysis. J. Arthroplasty. 2008;23(6 Suppl 1):50–55. doi: 10.1016/j.arth.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 15.Korovessis P, Petsinis G, Repanti M, Repantis T. Metallosis after contemporary metal-on-metal total hip arthroplasty. Five to nine-year follow-up. J. Bone Joint Surg. Am. 2006;88:1183–1191. doi: 10.2106/JBJS.D.02916. [DOI] [PubMed] [Google Scholar]
- 16.Long WT, Dorr LD, Gendelman V. An American experience with metal-on-metal total hip arthroplasties: a 7-year follow-up study. J. Arthroplasty. 2004;19(8 Suppl 3):29–34. doi: 10.1016/j.arth.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 17.MacDonald SJ. Metal-on-metal total hip arthroplasty: the concerns. Clin. Orthop. Relat. Res. 2004;429:86–93. doi: 10.1097/01.blo.0000150309.48474.8b. [DOI] [PubMed] [Google Scholar]
- 18.Migaud H, Jobin A, Chantelot C, Giraud F, Laffargue P, Duquennoy A. Cementless metal-on-metal hip arthroplasty in patients less than 50 years of age: comparison with a matched control group using ceramic-on-polyethylene after a minimum 5-year follow-up. J. Arthroplasty. 2004;19(8 Suppl 3):23–28. doi: 10.1016/j.arth.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Mikhael MM, Hanssen AD, Sierra RJ. Failure of metal-on-metal total hip arthroplasty mimicking hip infection. A report of two cases. J. Bone Joint Surg. Am. 2009;91:443–446. doi: 10.2106/JBJS.H.00603. [DOI] [PubMed] [Google Scholar]
- 20.Milosev I, Trebse R, Kovac S, Cör A, Pisot V. Survivorship and retrieval analysis of Sikomet metal-on-metal total hip replacements at a mean of seven years. J. Bone Joint Surg. Am. 2006;88:1173–1182. doi: 10.2106/JBJS.E.00604. [DOI] [PubMed] [Google Scholar]
- 21.Park YS, Moon YW, Lim SJ, Yang JM, Ahn G, Choi YL. Early osteolysis following second-generation metal-on-metal hip replacement. J. Bone Joint Surg. Am. 2005;87:1515–1521. doi: 10.2106/JBJS.D.02641. [DOI] [PubMed] [Google Scholar]
- 22.Rieker CB, Schön R, Köttig P. Development and validation of a second-generation metal-on-metal bearing: laboratory studies and analysis of retrievals. J. Arthroplasty. 2004;19(8 Suppl 3):5–11. doi: 10.1016/j.arth.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 23.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J. Bone Joint Surg. Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 24.Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Köster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J. Bone Joint Surg. Am. 2005;87:28–36. doi: 10.2106/JBJS.A.02039pp. [DOI] [PubMed] [Google Scholar]
- 25.Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J. Bone Joint Surg. Am. 1995;77:432–439. doi: 10.2106/00004623-199503000-00013. [DOI] [PubMed] [Google Scholar]