Abstract
Proponents of the two-incision minimally invasive approach for THA have claimed recovery is dramatically better than after other methods of THA, but this has not been confirmed with any objective data. We designed a prospective randomized trial of the two-incision THA versus the mini-posterior technique to determine whether patients having two-incision THA, when compared with patients having mini-posterior THA, had evidence of less muscle damage as reflected by changes in hip muscle strength after surgery, a less antalgic gait as reflected by changes in the single-leg stance time and walking velocity, and better hip function as reflected by changes in the hip moments during level walking and stair climbing as assessed by comprehensive gait analysis testing. Twenty-one patients, including 13 men and eight women, were prospectively randomized to either the two-incision or the mini-posterior approach and completed preoperative and 6-week postoperative three-dimensional gait analyses and isometric strength testing. We found no evidence that patients who had two-incision THA had less muscle damage, less antalgic gait, or better gait kinematics than patients who had mini-posterior THA. Instead, when there was a difference in strength or gait parameters, it was the patients who had mini-posterior THA who tended to have quicker recovery.
Level of Evidence: Level II, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Proponents of the two-incision minimally invasive approach for THA have claimed the procedure can be performed without cutting or damaging any muscle or tendon and recovery after that procedure is dramatically better than after other methods of THA [4–6]. Some reports of the two-incision THA technique, however, have been in selected series of patients [5, 7, 9, 15]. Without suitable controls, it is unclear whether the observed rapid recovery of patients in those reports was attributable to the two-incision technique or to some combination of patient selection, changes in perioperative analgesia protocols, rapid rehabilitation schemes, or patient education [10, 19–21]. Also, few studies have been performed to compare objective outcomes, such as gait analysis, for recovery of function [2, 3, 24].
We hypothesized patients who had two-incision THA would recover faster than those who had mini-posterior incision THA. We specifically asked whether patients who underwent two-incision THA, when compared with patients who underwent mini-posterior THA, had evidence of (1) less muscle damage as reflected by changes in hip muscle strength after surgery, (2) a less antalgic gait as reflected by changes in the single-leg stance time and walking velocity, and (3) better hip function as reflected by changes in the hip moments during level walking and stair climbing.
Materials and Methods
We prospectively enrolled 24 patients with primary degenerative arthritis of the hip in whom THA was planned. The explicit inclusion criteria were patients aged 40 to 85 years presenting for THA with a diagnosis of primary degenerative arthritis of the hip. The explicit exclusion criteria were age younger than 40 years or older than 85 years; severe bone deformity about the hip such as Crowe type III or IV dysplasia; osteomyelitis or prior intraarticular infection of the hip; substantial neurologic or musculoskeletal disorders that would adversely affect gait or early weightbearing after surgery; metastatic cancer; congenital, developmental, or other bone disease that would in the surgeon’s judgment interfere with survival of the THA; retained hardware around the hip; and arthrodesis of the affected hip.
After patient enrollment, randomization to the two-incision or the mini-posterior THA group was performed via a computerized process that dynamically balanced the groups based on age, gender, and body mass index which ensured no differences in these variables between the two groups. On presentation to the gait laboratory preoperatively, three patients were unable to complete the comprehensive gait analysis because of incapacitating pain in the affected hip, leaving 21 patients with complete preoperative and postoperative gait analysis and strength testing. The 21 patients included 13 men and eight women with a mean age of 63 ± 13 years (range, 40–85 years) and a mean body mass index of 30 ± 6 (range, 21–47). Eleven patients had the two-incision surgical technique and 10 had the mini-posterior technique performed for their THA.
The two-incision THAs were performed using a technique described previously through a 6-cm anterior incision using the Smith-Petersen interval to expose the hip, cut the femoral neck, and prepare and place the socket [4]. Care was taken to protect the lateral femoral cutaneous nerve and to ligate vessels at the inferior aspect of the incision to minimize postoperative complications. A second incision of 3.8 to 5 cm was made in the buttock to then ream and broach the femur and place the real femoral component. Intraoperative fluoroscopy was used as needed at intervals throughout the procedure. Before initiation of this prospective randomized trial, the senior author (MWP) had been trained at a company-sponsored cadaveric training course (Zimmer Institute; Zimmer, Warsaw, IN) and had performed more than 100 THAs with the two-incision technique. The technique used in the current study followed that outlined in the company-sponsored training course.
For the mini-posterior technique, the surgical approach involved a 7- to 9.5-cm incision along the posterior aspect of the femur starting at the tip of the greater trochanter and proceeding distally [12]. The external rotators and hip capsule were incised and preserved as one layer with an attempt to preserve the insertion of the quadratus femoris on the femur. The hip was dislocated posteriorly, the femoral neck was cut in accordance with the preoperative plan, and the femur was reamed and broached. Acetabular retractors were positioned, the acetabulum was reamed, and the real acetabular component was placed. A trial reduction was performed. The real femur then was impacted into place, the real head assembled, and the hip reduced. The hip capsule and external rotators were meticulously repaired back to the greater trochanter through three drill holes with nonabsorbable Number 5 sutures placed in a locking-looped fashion.
The same femoral component design (Versys® Full-coat, Zimmer, Inc, Warsaw, IN) and the same acetabular component design (Trilogy® Modular Trabecular Metal, Zimmer) were used in every case. These fully porous-coated femoral components were prepared for a press-fit over a 4- to 5-cm segment of the femoral diaphysis and were prepared with 0.5 mm underreaming relative to the stated size of the implant. These acetabular components with porous metal coating were reamed line-to-line with the stated size of the real implant and were inserted without additional screws for fixation in all cases. The acetabular liners were of a highly cross-linked design (Longevity®; Zimmer) and all sockets had a flat liner without additional lips, buildup, or offset. The femoral head size was chosen based on the size of the acetabular component according to the following decision tree: 28-mm head for 48 mm or less cup sizes; 32-mm head for 50, 52, and 54 mm cup sizes; and 36-mm head for 56 mm or greater cup sizes.
All patients were treated with the same comprehensive multimodal anesthesia and analgesia protocol including peripheral nerve blocks [20]. There were no differences in analgesic medication requirement between the two groups. Preoperatively patients received a COX-II antiinflammatory and a sustained-release oral opioid medication. An ipsilateral peripheral nerve block of the lumbar plexus was performed preoperatively and an indwelling catheter was used to deliver local anesthetic for the first two nights after surgery. A short-acting spinal anesthetic was administered intraoperatively and supplemental intravenous sedation was used as needed for patient comfort. Postoperative analgesia was managed by a dedicated pain management team with a goal of minimizing the use of parenteral opioid medications. Patients were given acetaminophen, a COX-II antiinflammatory, and a sustained-release oral opioid on a schedule for the first 48 hours after surgery. For breakthrough pain, a short-acting oral opioid was used on an as-needed basis. No patient-controlled analgesia pumps or other parenteral opioid medication were required by any of the patients.
All patients were moved from bed to a chair on the day of surgery and began walking with weightbearing as tolerated the morning after surgery. Two sessions of supervised physical therapy were performed each day the patient remained in the hospital. Patients were discharged from the hospital when they could move in and out of bed with minimal assistance, walk 100 feet with a walker or crutches, get up and down three stairs, and control their pain with oral medication. No attempt was made to do the surgery on an outpatient basis. Traditional total hip dislocation precautions were not used; the only warning was for the patients who had mini-posterior THAs to avoid the combination of flexion greater than 100° and marked internal rotation of their hip; patients otherwise were encouraged to proceed with activities as tolerated allowing their hip symptoms to be their guide. The length of stay in the hospital was not different between the two groups, with a mean stay of 2.6 days for each group. There were no known complications in either group.
Patients were tested preoperatively 1 to 3 days before surgery and then 6 weeks postoperatively. We chose the 6 week end point to evaluate whether minimally invasive surgery would improve rapid rehabilitation in an earlier phase of recovery. Three-dimensional gait analysis was performed during level walking, stair ascent, and stair descent. Spatiotemporal-distance parameters measured included walking velocity, cadence, step length, stride length, and single-leg stance phase duration. Hip moments were calculated using real-time analysis in three ground conditions: level walking, stair ascent, and stair descent for abduction moment, adduction moment, flexion moment, extension moment, internal rotation moment, and external rotation moment. Isometric strength testing was performed with a Biodex® machine (Biodex Medical Systems, Shirley, NY) and included abduction, adduction, flexion, extension, internal rotation, and external rotation.
Differences between the variables preoperatively and postoperatively were analyzed. All variables were normally distributed and were analyzed with Student’s t test to determine differences between the groups.
Results
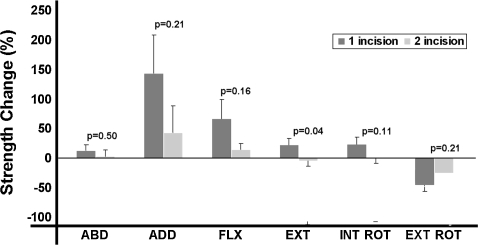
There was no evidence that patients who underwent two-incision THA had less muscle damage than patients who underwent mini-posterior THA as reflected by the change in isokinetic muscle strength from preoperatively to 6 weeks postoperatively (Fig. 1). Instead, the patients who had mini-posterior THA had greater improvement (p = 0.04) in hip extension strength as compared with patients who had the two-incision THA. Furthermore, there was a trend for the patients who had mini-posterior THA to have a greater increase in strength of the hip flexors (p = 0.16) and hip internal rotators (p = 0.11) as compared with patients who had the two-incision THA.
Fig. 1.
The graph shows the change in isokinetic muscle strength from preoperatively to 6 weeks postoperatively (expressed in percent strength change). The patients who had mini-posterior THAs had greater improvement in hip extension strength (p = 0.04) and a trend toward a greater increase in strength of the hip flexors (p = 0.16) and hip internal rotators (p = 0.11) compared with patients who had two-incision THAs. ABD = abduction; ADD = adduction; FLX = flexion; EXT = extension; INT ROT = internal rotation; EXT ROT = external rotation.
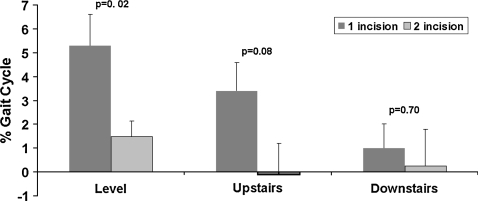
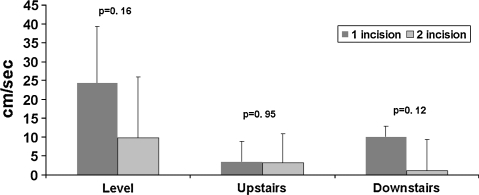
Patients who had the two-incision THA did not have evidence of a less antalgic gait compared with patients who had mini-posterior THA as reflected by changes in the single-leg stance time or walking velocity on level ground or when ascending or descending stairs. Instead, there was significantly greater improvement for the patients who had mini-posterior THA in single-leg stance time on level ground (p = 0.02) and a trend toward greater improvement when ascending stairs (p = 0.08) when comparing the preoperative values with the values at 6 weeks postoperatively (Fig. 2). Furthermore, there was a trend for the patients who had mini-posterior THA to have greater improvement in walking velocity on level ground (p = 0.16) and when descending stairs (p = 0.12) when comparing the preoperative values with the values at 6 weeks postoperatively (Fig. 3).
Fig. 2.
The graph shows patients who had mini-posterior THA had greater improvement for single-leg stance time on level ground and a trend toward greater improvement when ascending stairs (p = 0.08) from preoperative to 6-week postoperative gait assessment.
Fig. 3.
The graph shows patients who had mini-posterior THAs had a trend toward greater improvement in walking velocity on level ground and when descending stairs from preoperative to 6-week postoperative gait assessment.
The patients who had two-incision THA had no evidence of better hip function compared with patients who had mini-posterior THA as reflected by changes in gait kinematics reflected in the hip moments during level walking and stair climbing. Instead the patients who had mini-posterior THA had greater improvement (p = 0.05) in hip flexor moment compared with patients who had the two-incision THA. Furthermore, there was a trend for the hip abductor moment (p = 0.11), hip extensor moment (p = 0.16), and hip external rotator moment (p = 0.19) to have improved more in the patients who had the mini-posterior THA compared with patients who had the two-incision THA.
Discussion
Minimally invasive THA has captured the attention of patients and surgeons [4, 5, 7, 11, 16, 23, 25]. To date, however, relatively little direct comparison data have been published comparing minimally invasive THA techniques with one another or with an established THA technique [9, 13, 22]. We were particularly interested to see if one widely touted technique, the two-incision approach, provided substantial early functional benefits over another form of THA. We performed a prospective randomized trial and specifically sought whether patients who underwent two-incision THA, when compared with patients who underwent mini-posterior THA, had evidence of (1) less muscle damage as reflected by changes in hip muscle strength after surgery, (2) a less antalgic gait as reflected by changes in the single-leg stance time and walking velocity, and (3) better hip function as reflected by changes in the hip moments during level walking and stair climbing.
We note the following limitations of our prospective randomized strength and gait analysis study of the two-incision THA versus the mini-posterior THA. First, the lack of substantial published data on the expected improvements in strength or in the gait analysis parameters during the early postoperative period made it impossible to perform an a priori power analysis [2, 3, 24]. For that reason, we chose to consider this a pilot study to establish baseline strength testing and gait analysis differences in these minimally invasive THA techniques and chose to enroll a minimum of 10 patients in each of the two study groups. Second, none of our patients had preoperative physical therapy to teach them how to ambulate with crutches or a walker and this may have slowed their early progress compared with patients in other series with a rapid rehabilitation protocol [5]. Third, although we did not limit patient activities after surgery, we may not have pushed them to return to activities as aggressively as patients returned to activities in another study [4]. Our patients were told to progress with activities as tolerated, to discontinue ambulatory aids when they felt comfortable, and to wean themselves from oral pain medications as the pain subsided, but we did not suggest guidelines for when those events should occur. Other reports of the two-incision technique noted physical therapists and patients were explicitly encouraged to advance activities as quickly as possible and patients were seen in followup 1 week, 2 weeks, 6 weeks, and 12 weeks after surgery [4, 5]. That close followup may have encouraged some otherwise reluctant patients to progress more quickly through some of the functional milestones. In our study, a telephone call was made to patients 2 weeks postoperatively to check their progress, but the first office visit was 8 weeks after surgery. Although these limitations may have affected the absolute time to attain the various functional milestones in our study, it is unlikely the limitations adversely impacted the relative difference in recovery times between the two-incision and mini-posterior techniques in this prospective, randomized trial.
In our study, patients who had two-incision THA had worse hip strength than patients who had mini-posterior THA at 6 weeks. To our knowledge, this is the first objective quantification of muscle strength after minimally invasive THA. One study suggested a group of 33 patients who had minimally invasive THA had substantial improvements in ability to climb stairs at 3 months and ability to climb stairs and distance walked at 6 months compared with patients who had THA using traditional techniques [8]. However, it is not clear whether these outcomes were reflected by physical testing or by subjective questionnaire. Cadaveric studies have shown measurable muscle damage with minimally invasive techniques [16, 17]. Greater injuries of the gluteus minimus and medius muscles have been observed with the two-incision technique than with the mini-posterior approach [16]. Observation using MRI of muscles and tendons in patients who had a two-incision technique showed a decreased incidence of postoperative alterations in hip muscles when compared with standard posterolateral and direct lateral approaches [1]. However, these MRI scans were performed at least 18 months after THA, and it is difficult to know whether these data correlate with early muscle damage from the surgical approach.
Patients who had two-incision THAs did not have a less antalgic gait compared with patients who had mini-posterior THAs at 6 weeks postoperatively, as reflected by changes in single-leg stance time or walking velocity. That finding agrees with those of a recent study that evaluated three different groups of minimally invasive surgical approaches (mini-posterior, anterolateral, and anterior Judet). That study found no difference between the three approaches for stride length, cadence, velocity, single-limb support time, or double-limb support time at 6 weeks or 3 months postoperatively [24]. Another prospective blinded study showed no benefit of a minimally invasive surgical approach over a traditional posterior approach in terms of gait velocity, cadence, step length, or increased stance phase duration of the affected leg [2]. Bennett et al. verified their results in a larger study population [3].
Previous gait analyses have established surgical approach for THA does influence the postoperative result, with patients having posterior approaches exhibiting greater characteristics of nonpathologic gait and greater range of functional ability [14, 26]. In our study, the patients who had two-incision THA had no evidence of better hip function compared with patients who had mini-posterior THA, as reflected by changes in gait kinematics during level walking and stair climbing. These gait kinematics are similar to those reported in a recent prospective analysis showing no difference in normalized abductor torque at midstance between three minimally invasive surgical approaches [18]. Additionally, in a prospective blinded study, there was no demonstrable benefit of a minimally invasive technique compared with a THA with a traditional technique as judged by changes in pelvic tilt, range of motion in the sagittal plane, hip abduction and adduction, or rotation of the hip and foot [2].
We found no evidence that the 6-week functional outcome after two-incision THA was better than outcome after other methods of THA. Instead, when there were differences in strength or gait parameters, the patients who had mini-posterior THA tended to have quicker recovery.
Acknowledgments
We thank James M. Leone, MD and Emily Berg for their substantial contributions of initial protocol submission and data collection, respectively.
Footnotes
One of the authors (MWP) received royalties from Zimmer Orthopaedics (Warsaw, IN). Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Mayo Clinic, Rochester, MN.
References
- 1.Bal B, Lowe J. Muscle damage in minimally invasive total hip arthroplasty: MRI evidence that it is not significant. Instr Course Lect. 2008;57:223–229. [PubMed] [Google Scholar]
- 2.Bennett D, Ogonda L, Elliott D, Humphreys L, Beverland DE. Comparison of gait kinematics in patients receiving minimally invasive and traditional hip replacement surgery: a prospective blinded study. Gait Posture. 2006;23:374–382. doi: 10.1016/j.gaitpost.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 3.Bennett D, Ogonda L, Elliott D, Humphreys L, Lawlor M, Beverland D. Comparison of immediate postoperative walking ability in patients receiving minimally invasive and standard-incision hip arthroplasty: a prospective blinded study. J Arthroplasty. 2007;22:490–495. doi: 10.1016/j.arth.2006.02.173. [DOI] [PubMed] [Google Scholar]
- 4.Berger R. Total hip arthroplasty using the minimally invasive two-incision approach. Clin Orthop Relat Res. 2003;417:232–241. doi: 10.1097/01.blo.0000096828.67494.95. [DOI] [PubMed] [Google Scholar]
- 5.Berger R, Jacobs J, Meneghini R, Valle C, Paprosky W, Rosenberg A. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 6.Berger RA, Duwelius PJ. The two-incision minimally invasive total hip arthroplasty: technique and results. Orthop Clin North Am. 2004;35:163–172. doi: 10.1016/S0030-5898(03)00110-X. [DOI] [PubMed] [Google Scholar]
- 7.Berry DJ, Berger RA, Callaghan JJ, Dorr LD, Duwelius PJ, Hartzband MA, Lieberman JR, Mears DC. Symposium: Minimally invasive total hip arthroplasty. development, early results, and a critical analysis. J Bone Joint Surg Am. 2003;85:2235–2246. [PubMed]
- 8.DiGioia AM, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18:123–128. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 9.Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE. Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty: a prospective, randomized, blinded study. J Bone Joint Surg Am. 2007;89:1153–1160. doi: 10.2106/JBJS.F.00940. [DOI] [PubMed] [Google Scholar]
- 10.Duwelius P, Dorr L. Minimally invasive total hip arthroplasty: an overview of the results. Instr Course Lect. 2008;57:215–222. [PubMed] [Google Scholar]
- 11.Huo MH, Brown BS. What’s new in hip arthroplasty. J Bone Joint Surg Am. 2003;85:1852–1864. doi: 10.2106/00004623-200309000-00041. [DOI] [PubMed] [Google Scholar]
- 12.Inaba Y, Dorr L, Wan Z, Sirianni L, Boutary M. Operative and patient care techniques for posterior mini incision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:104–114. doi: 10.1097/01.blo.0000193811.23706.3a. [DOI] [PubMed] [Google Scholar]
- 13.Lugade V, Klausmeier V, Jewett B, Collis D, Chou LS. Short-term recovery of balance control after total hip arthroplasty. Clin Orthop Relat Res. 2008;466:3051–3058. doi: 10.1007/s11999-008-0488-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madsen M, Ritter M, Morris H, Meding J, Berend M, Faris P, Vardaxis V. The effect of total hip arthroplasty surgical approach on gait. J Orthop Res. 2004;22:44–50. doi: 10.1016/S0736-0266(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 15.Malik A, Dorr L. The science of minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2007;463:74–84. doi: 10.1097/BLO.0b013e3181468766. [DOI] [PubMed] [Google Scholar]
- 16.Mardones R, Pagnano M, Nemanich J, Trousdale R. Muscle damage after total hip arthroplasty done with the two-incision and mini-posterior techniques. Clin Orthop Relat Res. 2005;441:63–67. doi: 10.1097/01.blo.0000194727.55372.04. [DOI] [PubMed] [Google Scholar]
- 17.Meneghini R, Pagnano M, Trousdale R, Hozack W. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453:293–298. doi: 10.1097/01.blo.0000238859.46615.34. [DOI] [PubMed] [Google Scholar]
- 18.Meneghini R, Smits S, Swinford R, Bahamonde R. A randomized, prospective study of 3 minimally invasive surgical approaches in total hip arthroplasty: comprehensive gait analysis. J Arthroplasty. 2008;23:68–73. doi: 10.1016/j.arth.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes: a prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701–710. doi: 10.2106/JBJS.D.02645. [DOI] [PubMed] [Google Scholar]
- 20.Pagnano M, Hebl J, Horlocker T. Assuring a painless total hip arthroplasty: a multimodal approach emphasizing peripheral nerve blocks. J Arthroplasty. 2006;4:80–84. doi: 10.1016/j.arth.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Pagnano M, Trousdale R, Meneghini R, Hanssen A. Patients preferred a mini-posterior THA to a contralateral two-incision THA. Clin Orthop Relat Res. 2006;453:156–159. doi: 10.1097/01.blo.0000238858.38992.2d. [DOI] [PubMed] [Google Scholar]
- 22.Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:1000–1006. doi: 10.2106/JBJS.G.00804. [DOI] [PubMed] [Google Scholar]
- 23.Waldman B. Minimally invasive total hip replacement and perioperative management: early experience. J South Orthop Assoc. 2002;11:213–217. [PubMed] [Google Scholar]
- 24.Ward S, Jones R, Long W, Thomas D, Dorr L. Functional recovery of muscles after minimally invasive total hip arthroplasty. Instr Course Lect. 2008;57:249–254. [PubMed] [Google Scholar]
- 25.Wenz J, Gurkan I, Jibodh S. Mini-incision total hip arthroplasty: a comparative assessment of perioperative outcomes. Orthopedics. 2002;25:1031–1043. doi: 10.3928/0147-7447-20021001-14. [DOI] [PubMed] [Google Scholar]
- 26.Whatling G, Dabke H, Holt C, Jones L, Madete J, Alderman P, Roberts P. Objective functional assessment of total hip arthroplasty following two common surgical approaches: the posterior and direct lateral approaches. Proc Inst Mech Eng [H]. 2008;222:897–905. doi: 10.1243/09544119JEIM396. [DOI] [PubMed] [Google Scholar]