Abstract
Metal-on-metal hip resurfacing is offered as an alternative to traditional THA for the young and active adult with advanced osteoarthritis. However, patients undergoing hip resurfacing may be predisposed to persistent groin pain due to insufficient head/neck offset, an uncovered acetabular component, or both. We therefore determined the incidence of groin pain after metal-on-metal hip resurfacing, its impact on patient function, and possible risk factors contributing to groin pain. We evaluated 116 patients with a followup of at least 12 months after surgery (mean, 26 months; range, 12–61 months). The mean age was 48.8 years (range, 24.0–66.3 years), with 21 women (18%) and 95 men (82%). All patients were evaluated clinically and radiographically and had a Harris hip score, WOMAC, UCLA Activity Rating Scale, and the RAND-36 General Health measure; they were specifically asked if they experienced groin pain currently or since their surgery. Although all patients had functional improvements postoperatively, 21 of 116 of the patients (18%) reported groin pain; 12 of these (10% of the total) stated the pain limited their activities of daily living and 11 (10%) required medication for pain. Female patients were at greater risk of having groin pain. Of the patients with groin pain, three patients had muscle atrophy with a joint effusion on CT; one of these patients had revision surgery for the pain. Patients with metal-on-metal resurfacing may have a higher incidence of pain than those with conventional THA.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Metal-on-metal hip resurfacing is being offered as an alternative to traditional stem-type THA for the young and active adult with advanced osteoarthritis. It is currently one of the fastest growing arthroplasty procedures [28, 40]. Bone preservation, closer resemblance to normal anatomic biomechanics, and possibly superior function are some factors leading to its expanding indications [16, 35, 40]. Although early complications such as femoral neck fractures still remain a concern [2, 39], the functional outcomes have been comparable to stem-type THA, with the majority of patients returning to high levels of activity [14, 33, 37, 43, 45]. However, because the femoral head/neck junction is preserved, positioning of both the femoral and acetabular component is critical to maximize function and to minimize stresses within the femoral neck [7]. In addition, implantation of the monoblock acetabular component may pose some difficulties in achieving full coverage within the acetabular bony bed.
More importantly, lack of complete acetabular component coverage anteriorly can potentially lead to soft tissue irritation of the iliopsoas tendon, causing groin pain and compromising the overall functional outcome [30]. An additional risk of developing pain after hip resurfacing is from impingement [5]. Due to preservation of the femoral head/neck junction of the proximal femur, impingement can occur after resurfacing, leading to the development of groin pain [5]. Consequently, patients undergoing hip resurfacing may be predisposed to persistent groin pain due to insufficient head/neck offset, an uncovered acetabular component, or a combination of both. Despite the potential for an increased incidence of groin pain or psoas tendonitis after hip resurfacing the incidence of groin pain has not been reported in large series, although the incidence after conventional THA ranges between 0.3% and 4.3% [10, 29, 36].
We therefore determined (1) the incidence of groin pain after metal-on-metal hip resurfacing; (2) the impact of groin pain on patient function; and (3) possible risk factors contributing to groin pain, including the diagnostic evaluation of those who reported pain.
Patients and Methods
We performed 170 hip resurfacings between November 2001 and August 2006. From these we excluded six patients who had undergone revision of a previous resurfacing arthroplasty: two for femoral neck fracture, two for aseptic acetabular loosening, one for aseptic femoral loosening, and one for persistent unexplained hip pain. Between February and October 2008, we evaluated 116 of the remaining 164 patients (70%) who were at least 12 months postsurgery; all patients were being seen for regular followup. The mean age was 48.8 years (range, 24.0–66.3 years) with 21 women (18%) and 95 men (82%). The mean body mass index was 26.9 (range, 19.3–37.7). The minimum followup after surgery was 12 months (mean, 26 months; range, 12–61 months). No patients were lost to followup. Approval was obtained from the hospital’s institutional review board, and the research was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All patients gave their informed consent for participation in the study.
Because hip resurfacing has been the preferred implant at our center for patients under 60 years of age who are active (i.e., engage in a recreational sporting activity on a weekly basis), we do not have a comparable THA population. The incidence of groin pain and psoas tendonitis in the literature is reportedly up to 4.3% after conventional THA [36]; thus, we considered an incidence of 10% in the resurfacing population would be clinically important and greater than that for conventional THA. Based on these assumptions, and using an alpha of 0.05, a one-sided power analysis indicated a sample size of 106 patients would have 80% power to detect an incidence of 10% in the resurfacing sample, as compared to 4.3% in the THA population.
All resurfacings were implanted by two surgeons (PEB, PRK) experienced in adult hip reconstruction. Four surgical approaches were used (two by each surgeon): one surgeon used a direct lateral approach in three patients and a posterolateral in 64; the other used a trochanteric slide approach as described by Ganz et al. [20] in 34 patients and an anterior approach in 15. For all patients, the Conserve Plus® Hip Resurfacing (Wright Medical Technology, Memphis, TN) was used. Two sizes of acetabular components were used, standard size (3.75-mm wall thickness) and a thick shell (5-mm wall thickness), both of which had a porous beaded surface made of cobalt-chrome molybdenum alloy for osteointegration without supplemental screw fixation (Fig. 1). Before January 2003, only the thick shell option was available, and subsequent to this, the choice of cup was made intraoperatively based on each patient’s anatomic characteristics. Standard-sized cups were used in 100 patients (86%) and thick shells in 16 cases (14%). Cementless acetabular fixation was used and the femoral component was cemented according to the manufacturer’s recommendation.
Fig. 1.
A photograph shows the Conserve Plus® acetabular component (3.7-mm wall thickness) with porous beaded surface made of cobalt-chrome molybdenum alloy for osteointegration without supplemental screw fixation.
All patients followed a standardized postoperative physiotherapy regimen where they were mobilized on the first postoperative day and were 50% weightbearing on crutches for 4 weeks. Physiotherapy began at 4 weeks under the supervision of a professional physiotherapist including ROM exercises and a strengthening program. Patients were instructed to gradually resume their activities between 4 and 6 weeks postsurgery.
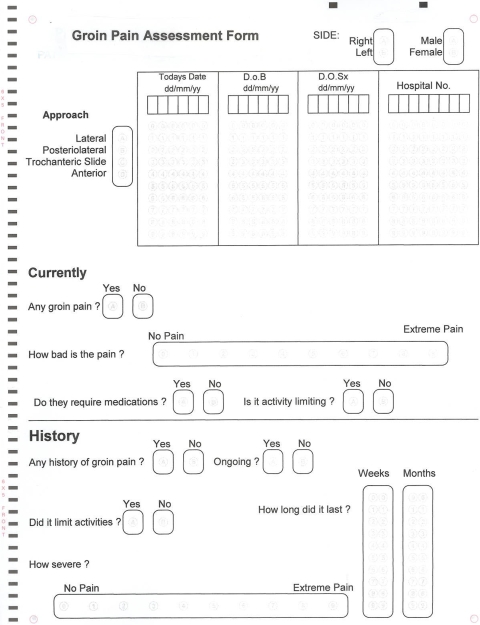
As a standard of care, patients were evaluated at 6 weeks and 3, 6, 12, and 24 months postsurgery. At the time of each followup visit, all patients were asked to complete functional outcome questionnaires including the Harris Hip score [22], WOMAC Osteoarthritis Index (pain, stiffness, and function subscales) [8], UCLA Activity Rating Scale [3], and RAND-36 General Health measure [25]. Total RAND scores were computed by taking the average of the eight individual subscales. For all measures, higher scores reflect better overall functioning. At last followup during the study period between February and October 2008, all patients were specifically asked about any symptoms of groin pain by a surgeon (ABN) not involved in the treatment. Those who reported groin pain were asked to document the severity of pain on a visual analog pain scale from 1 to 10, where higher scores reflect more pain. Using a standardized questionnaire (Appendix 1), patients were further asked whether the pain was present at rest or with activity, whether it limited their daily activities, whether they took any analgesics specifically for their groin pain, and whether any intervention was performed, either surgically or by means of injections. On physical examination, ROM was assessed by measuring the degree of internal rotation with the hip in 90° of flexion, the presence of an impingement sign (pain with flexion/adduction/internal rotation) [31], and the presence of groin pain on resisted straight leg raise.
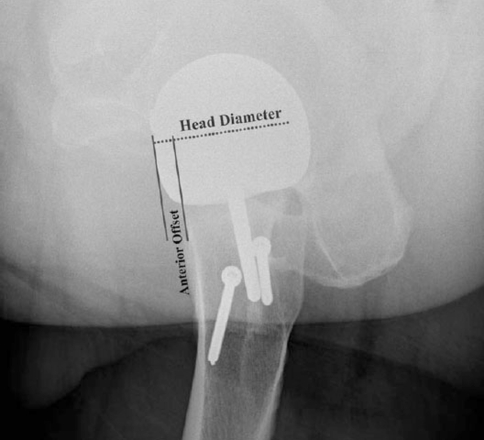
Radiographic assessment included a well-centered AP pelvis and cross-table lateral radiographs of the involved hip with the leg in 15° of internal rotation. All radiographic measurements were performed by one of us (ABN) not involved in the treatment. We assessed femoral component orientation on the AP pelvis and lateral radiographs, as well as the offset ratio of Eijer et al. on the cross-table lateral [5, 18] (Fig. 2). The literature reports an acceptable level of inter- and intraobserver agreement for measurement of head-neck offset on AP and cross-table lateral views, ranging from 0.52 to 0.73 [13]. Finally, acetabular cup uncoverage was assessed on both AP and lateral radiographs at the time of followup and on all films before followup; if the cup was uncovered in either view, it was defined as positive. The radiographic data collection was performed by a single observer who was blinded to patient and group identity. Lucencies were measured in the three DeLee-Charnley zones [15].
Fig. 2.
A cross-table lateral radiograph illustrates measurement of the offset ratio. Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery from Beaulé PE, Harvey N, Zaragoza E, LeDuff MJ, Dorey FJ. The femoral head/neck offset and hip resurfacing. J Bone Joint Surg Br. 2007;89:9–15.
To assess the impact of groin pain on patient function, we performed a paired t test to compare differences in functional scores from pre- to postsurgery for the group experiencing groin pain. We used independent t tests to determine differences in both pre- and postoperative functional outcome scores between (1) patients reporting groin pain versus those without pain; (2) patients taking medication for pain versus those not taking any analgesics for pain; and (3) patients not taking medication for pain versus those without pain. Using a logistic regression, we determined whether any of the following variables were associated with groin pain: surgical approach, cup thickness, body mass index, age, offset ratio, cup uncoverage, gender, internal rotation, impingement sign, groin pain on resisted straight leg raise, cup inclination, or stem shaft angle. The cases were divided into three equal groups based on surgeon experience, and a chi-square analysis was used to determine if surgeon experience was associated with the incidence of groin pain. All statistical analyses were performed using SPSS® 15.0 for Windows® (SPSS Inc, Chicago, IL).
Results
Twenty-one of the 116 resurfacing patients (18%) reported persistent groin pain, with a mean pain score of 5.19 of 10 (SD, 2.16; range, 2–8). The pain pattern was similar in all patients: deep anterior groin pain, aggravated by activity (eg, getting in and out of a car or bed) and partially relieved by NSAIDs. Eleven of the 21 patients with groin pain reported taking analgesics for their groin pain (10% of all 116 patients, or 52% of the 21 patients with pain). Twelve patients reported pain limited their activities (10% of all 116 patients, or 57% of the patients with groin pain), with a mean pain severity score of 5.50 (SD, 2.19; range, 2–8). Six of the 11 patients on analgesics (55%) reported their activities were limited by pain.
All patients with groin pain reported improvement on all functional scores except activity; however, all the postoperative functional outcome scores were lower compared to patients with no groin pain (Table 1). Patients with groin pain also scored lower at the preoperative assessment on WOMAC Pain and Function and RAND compared to patients with no groin pain (Table 1). Patients with groin pain who were taking analgesics (n = 11) scored lower on all functional outcome measures than those who were not taking medications for pain (n = 10) (Table 2). Again, these patients also tended to score lower at the preoperative assessment on all measures (except RAND) (Table 2). When looking at only the patients with groin pain not taking analgesics, their functional scores were not different from those with no groin pain, except at the baseline RAND assessment where those with no pain scored higher (Table 2).
Table 1.
Functional outcome measures for patients with and without groin pain
| Functional outcome | Patients with groin pain | Preoperative | Postoperative | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | P value | Pain | No pain | P value | Pain | No pain | P value | |
| WOMAC pain | 40.0 (17.2) | 80.0 (22.8) | 0.001 | 41.3 (16.9) | 57.3 (17.6) | 0.005 | 78.3 (20.6) | 95.7 (9.9) | 0.002 |
| WOMAC stiffness | 42.1 (17.9) | 70.5 (28.1) | 0.001 | 42.7 (17.2) | 48.7 (17.8) | 0.294 | 71.5 (25.3) | 86.6 (15.5) | 0.025 |
| WOMAC function | 38.1 (19.8) | 73.4 (23.9) | 0.002 | 39.7 (19.5) | 56.4 (16.6) | 0.004 | 76.1 (21.1) | 94.3 (8.8) | 0.002 |
| Harris hip score | 53.2 (14.5) | 78.2 (14.5) | 0.004 | 57.6 (15.6) | 59.9 (9.1) | 0.623 | 79.9 (14.8) | 96.5 (5.9) | 0.006 |
| RAND | 36.5 (20.1) | 62.3 (25.9) | 0.027 | 37.1 (19.3) | 58.2 (19.9) | 0.001 | 64.9 (24.5) | 83.9 (13.6) | 0.005 |
| UCLA activity | 5.7 (3.0) | 5.9 (1.8) | 0.845 | 5.5 (2.9) | 6.4 (2.3) | 0.287 | 6.5 (2.0) | 7.5 (1.7) | 0.037 |
Values are expressed as mean, with SD in parentheses.
Table 2.
Functional outcome measures for patients with and without groin pain and with and without medication
| Functional outcome | Preoperative | Postoperative | Preoperative | Postoperative | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain/meds | Pain/no meds | P value | Pain/meds | Pain/no meds | P value | Pain/no meds | No pain | P value | Pain/no meds | No pain | P value | |
| WOMAC pain | 27.0 (5.7) | 51.43 (14.6) | 0.006 | 71.7 (19.8) | 85.0 (20.2) | 0.176 | 51.43 (14.6) | 57.32 (17.6) | 0.399 | 85.0 (20.2) | 95.7 (9.9) | 0.153 |
| WOMAC stiffness | 32.5 (16.8) | 50.0 (14.4) | 0.081 | 61.1 (22.9) | 81.9 (24.3) | 0.080 | 50.0 (14.4) | 48.7 (17.8) | 0.849 | 81.9 (24.3) | 86.6 (15.5) | 0.427 |
| WOMAC function | 27.6 (12.8) | 49.8 (19.0) | 0.055 | 68.9 (19.8) | 83.3 (20.9) | 0.154 | 49.8 (19.0) | 56.4 (16.6) | 0.361 | 83.3 (20.9) | 94.3 (8.8) | 0.159 |
| Harris hip score | 52.3 (21.0) | 62.2 (8.3) | 0.271 | 77.4 (11.3) | 81.7 (17.5) | 0.679 | 62.2 (8.3) | 59.9 (9.1) | 0.522 | 81.7 (17.5) | 96.5 (5.9) | 0.093 |
| RAND | 38.0 (15.3) | 36.4 (23.4) | 0.887 | 60.1 (21.3) | 69.6 (27.8) | 0.429 | 36.4 (23.4) | 58.2 (19.9) | 0.010 | 69.6 (27.8) | 83.9 (13.6) | 0.164 |
| UCLA activity | 4.4 (2.2) | 6.6 (3.3) | 0.248 | 5.2 (1.5) | 7.8 (1.6) | 0.003 | 6.6 (3.3) | 6.4 (2.3) | 0.859 | 7.8 (1.6) | 7.5 (1.7) | 0.670 |
Values are expressed as mean, with SD in parentheses; meds = medication.
Gender was associated (p = 0.03) with groin pain. Eight of 21 females (38%) reported persistent groin pain as compared to 13 of 95 males (14%). Groin pain on resisted straight leg raise was more frequent in the group who reported groin pain (p = 0.06); 11 of the 21 patients with pain (52%) reported pain on resisted straight leg raise as compared to 10 of the 95 patients (11%) with no persistent groin pain. We found no association between groin pain and surgical approach (p = 0.99), cup thickness (p = 0.35), body mass index (p = 0.65), age (p = 0.63), offset ratio (p = 0.58), cup uncoverage (p = 0.83), internal rotation (p = 0.80), impingement sign (p = 0.11), cup inclination (p = 0.73), or stem shaft angle (p = 0.72). Surgeon experience was not associated (p = .84) with the incidence of groin pain.
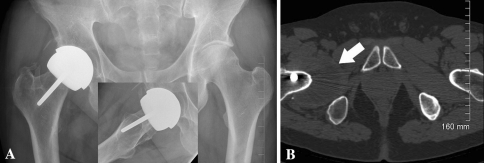
Of the 21 patients who reported groin pain, five underwent a Marcaine® (Sanofi Aventis US, LLC, Bridgewater, NJ) corticosteroid injection into the psoas sheath under ultrasound guidance; two patients had temporary resolution of their pain for two weeks. One patient received a second injection. Five patients underwent imaging with CT scans, which demonstrated muscle atrophy of the piriformis, obturator internus, and gluteal musculature on their affected side compared to their nonoperative side and atrophic changes to the iliopsoas musculature. Implants appeared well-fixed. Fluid accumulation in the affected hip was noted in three patients (Fig. 3). One was revised and the other two patients had a moderate-sized fluid complex seen within the iliacus/psoas tendon sheath but are not scheduled for revision surgery.
Fig. 3A–B.
(A) An AP radiograph shows the hips of a 43-year-old man complaining of persistent groin pain 3.5 years after metal-on-metal hip resurfacing (Conserve Plus®). The inset is a lateral of the hip showing some femoral neck narrowing. (B) A CT scan shows a massive amount of fluid inferior to the hip, with the lining being thickened and nodular. As indicated by the arrow, the area of fluid distention measured 7 × 4.5 × 2.3 cm.
Discussion
Although hip resurfacing can provide an excellent functional outcome, the procedure is associated with a unique set of complications such as femoral neck fractures [2, 39], femoral neck narrowing [4, 26], and localized soft tissue masses [41]. Suboptimal implant positioning can lead to premature failure [6] and persistent pain [5, 7, 32]. One complication that may be prone to occur is persistent groin pain secondary to component malposition with associated iliopsoas tendonitis [7, 32]. Because of the lack of data on the incidence of groin pain after hip resurfacing, we conducted a cross-sectional study to determine (1) the incidence of groin pain after metal-on-metal hip resurfacing, (2) the impact of groin pain on patient function, and (3) possible risk factors contributing to groin pain, including the diagnostic evaluation of those who reported pain.
We acknowledge several limitations of this observational study. First, this report was of a nonconsecutive list of patients. However, it was sufficiently powered to detect an incidence of 10% in the resurfacing sample, as compared to 4.3% in the THA population [36]. Second, the operative procedures were performed by two surgeons via multiple surgical approaches, although we did not find an association between surgical approach and the incidence of groin pain. Third, because hip resurfacing is the implant of choice for this patient population, we had no comparative THA group for determining the incidence of groin pain, although our results can be compared to the reported incidence of 4.3% in the THA population [36]. Finally, the natural history of the groin pain was not evaluated in this series. However, the findings presented here do provide useful information on the incidence of groin pain and indicate the need for longitudinal and matched comparative groups to better understand the etiology and treatment options for this possible complication of hip resurfacing arthroplasty.
We found an 18% incidence of persistent groin pain after metal on metal hip resurfacing arthroplasty, with 10% being limited in their activities or taking medicine for it. Although no other studies have reported on the incidence of groin pain after hip resurfacing, the incidence reported in this series is higher than the varying incidence of 0.3% to 4.3% [1, 10, 36] after THA. However, this is consistent with a recent paper by Fowble et al. [19] who also reported patients who had undergone a resurfacing procedure had a higher incidence of persistent hip pain than those who had undergone a conventional total hip arthroplasty.
Given this relatively high incidence of groin pain, it becomes important to assess the presence of groin pain on the patient’s overall function. Overall, the functional outcome scores of our patient group were comparable to those reported with THA and hip resurfacing [37, 43, 45]. Even for those patients with groin pain, their functional scores improved substantially after surgery. Of particular note is the finding that the patients who reported groin pain but were not taking analgesics were no different in their functional outcome scores from the patients who did not have pain. More importantly, those patients with groin pain also tended to report more pain preoperatively, which is consistent with a previous study where the preoperative functional score was a predictor of postoperative function in patients undergoing THA [21].
Female gender emerged as the variable most predictive of persistent groin pain. This is consistent with previous studies showing females tend to report lower functional outcome scores than males after THA [27, 38] and have up to a threefold higher risk of developing psoas tendonitis after THA [36]. Noble et al. [34] have suggested females may have a larger proximal femoral flare, which may impinge on the psoas tendon, leading to psoas tendonitis. This theory may partially explain the higher incidence of groin pain in females after hip resurfacing. Why the female gender would be more prone to a suboptimal outcome is most likely multifactorial; however, the asymmetric profile of the acetabulum may provide an anatomic explanation. In a recent cadaveric study, Vandenbussche et al. [44] found the psoas valley had three distinct shapes with ranging distributions in the population: 79% curved, 11% angular, 10% irregular, and 0% straight, with females exhibiting a shallower psoas valley, making them more vulnerable to irritation from a prominent cup edge.
Our data also showed an association between groin pain and pain on resisted straight leg raise, which is also consistent with the diagnosis of iliopsoas tendonitis. This diagnosis is made clinically by the pain pattern, which usually involves pain on resisted leg raise, groin pain when getting up from a seated position, and the “car sign” [29]. Indeed, although the exact etiology of groin pain after THA is most likely multifactorial, iliopsoas tendonitis secondary to acetabular component malposition and/or uncoverage [17, 36, 42] has been one of the most commonly identified causes. The iliopsoas tendon runs over the anterior edge of the acetabulum, over the head/neck junction of the proximal femur, and winds back around the femoral neck to attach to the lesser trochanter, which is situated posteromedially [12]. Sites of irritation would include the anterior edge of the acetabulum and femoral neck [36]. Hence, a prominent acetabular cup (ie, where the anterior rim of the acetabular component extends beyond the anterior rim of the osseous acetabulum) or osteophytes on the preserved anterior neck may cause irritation of the iliopsoas tendon sheath, leading to a clinical presentation of anterior groin pain. These findings have been confirmed after THA in studies that included histologic examination of the psoas tendon at these sites [29]. The diagnosis of iliopsoas tendonitis is also made by local anesthetic/corticosteroid injection into the psoas tendon under radiographic guidance. In our series, two patients did have temporary relief from tendon sheath injections. It is unclear if a repeat injection would be of further benefit or if surgical release of the psoas tendon would be preferable. Our limited experience with psoas tendon injection is consistent with other larger series of psoas tendinitis after THA where surgical release of the psoas tendon was more effective [17, 36].
Other possible causes of groin pain after THA can be related to component loosening and adverse soft tissue reaction [23, 41]. Although we do not have an established protocol to evaluate painful hip resurfacing at our institution, further imaging of the patients with persistent groin pain showed two of them with substantial fluid masses. These fluid collections may be related to either an allergic response to the metal implant or to the metallic wear debris itself [11], which can lead to the development of substantial soft tissue masses, which have also been seen with metal-on-polyethylene bearings but after a longer time of implantation [9, 24]. In the one case revised, the implants were well-fixed with no soft tissue reaction.
In conclusion, we found the incidence of groin pain after metal-on-metal hip resurfacing arthroplasty to be 18% in a cross-sectional observational series with 10% of patients requiring medication for the pain. The cause is most likely multifactorial, ranging from iliopsoas tendinitis to an adverse soft tissue reaction to metal debris. Further longitudinal studies and diagnostic investigational protocols are required to better understand the etiology and natural history of groin pain after hip resurfacing.
Acknowledgments
We thank Heather Belanger, RN, BScN (Ottawa Hospital–General Campus, Ottawa, ON, Canada) for her assistance with data collection and the coordination of this research project.
Appendix 1
Footnotes
One or more of the authors (Paul E. Beaulé, Paul R. Kim) have received funding from Wright Medical Technology, Memphis, TN, in support of this research.
Each author certifies that his or her institution has approval for the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Ala Eddine T, Remy F, Chantelot C, Giraud F, Migaud H, Duquennoy A. Anterior iliopsoas impingement after total hip arthroplasty: diagnosis and conservative treatment in 9 cases [in French] Rev Chir Orthop Reparatrice Appar Mot. 2001;87:815–819. [PubMed] [Google Scholar]
- 2.Amstutz HC, Le Duff MJ, Campbell PA. Fracture of the neck of the femur after surface arthroplasty of the hip. J Bone Joint Surg Am. 2004;86:1874–1877. doi: 10.2106/00004623-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 4.Beaule PE, Dorey FJ, LeDuff MJ, Gruen T, Amstutz HC. Risk factors affecting outcome of metal on metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. doi: 10.1097/00003086-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Beaule PE, Harvey N, Zaragoza EJ, LeDuff M, Dorey FJ. The femoral head/neck offset and hip resurfacing. J Bone Joint Surg Br. 2007;89:9–15. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 6.Beaule PE, Lee J, LeDuff M, Dorey FJ, Amstutz HC, Ebramzadeh E. Orientation of femoral component in surface arthroplasty of the hip: A biomechanical and clinical analysis. J Bone Joint Surg Am. 2004;86:2015–2021. doi: 10.2106/00004623-200409000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Beaule PE, Poitras P. Femoral component sizing and positioning in hip resurfacing arthroplasty. Instr Course Lect. 2007;56:163–169. [PubMed] [Google Scholar]
- 8.Bellamy N, Buchanan WW, Goldsmith CH. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes following total or knee arthroplasty in osteoarthritis. J Orthop Rheumatol. 1988;1:95–108. [PubMed] [Google Scholar]
- 9.Binek R, Levinsohn EM. Enlarged iliopsoas bursa: An unusual cause of thigh mass and hip pain. Clin Orthop Relat Res. 1987;224:158–163. [PubMed] [Google Scholar]
- 10.Bricteux S, Beguin L, Fessy MH. Iliopsoas impingement in 12 patients with total hip arthroplasty [in French] Rev Chir Orthop Reparatrice Appar Mot. 2001;87:820–825. [PubMed] [Google Scholar]
- 11.Campbell PA, Shimmin A, Walter L, Solomon M. Metal sensitivity as a cause of groin pain in metal-on-metal hip resurfacing. J Arthroplasty. 2008;23:1080–1085. doi: 10.1016/j.arth.2007.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Chandler SB. The iliopsoas bursa in man. Anat Rec. 1934;58:235. doi: 10.1002/ar.1090580304. [DOI] [Google Scholar]
- 13.Clohisy JC, Nunley RM, Otto RJ, Shoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 14.Daniel J, Pynsent PB, McMinn DJW. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 15.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 16.Della Valle CJ, Nunley RM, Raterman SJ, Barrack RL. Initial American experience with hip resurfacing following FDA approval. Clin Orthop Relat Res. 2009;467:72–78. doi: 10.1007/s11999-008-0563-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dora C, Houweling M, Koch P, Sierra RJ. Iliopsoas impingement after total hip replacement. J Bone Joint Surg Br. 2007;89:1031–1035. doi: 10.1302/0301-620X.89B8.19208. [DOI] [PubMed] [Google Scholar]
- 18.Eijer H, Leunig M, Mahomed N, Ganz R. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int. 2001;11:37–41. [Google Scholar]
- 19.Fowble VA, dela Rosa MA, Schmalzried TP. A comparison of total hip resurfacing and total hip arthroplasty - patients and outcomes. Bull NYU Hosp Jt Dis. 2009;67:108–112. [PubMed] [Google Scholar]
- 20.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip. A new technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 21.Garbuz DS, Xu M, Duncan CP, Masri BA, Sobolev B. Delays worsen quality of life outcome of primary total hip arthroplasty. Clin Orthop Relat Res. 2006;447:79–84. doi: 10.1097/01.blo.0000203477.19421.ed. [DOI] [PubMed] [Google Scholar]
- 22.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 23.Hart AJ, Sabah S, Henckel J, Lewis A, Cobb J, Sampson B, Mitchell A, Skinner JA. The painful metal-on-metal hip resurfacing. J Bone Joint Surg Br. 2009;91:738–744. doi: 10.1302/0301-620X.91B6.21682. [DOI] [PubMed] [Google Scholar]
- 24.Hattrup SJ, Bryan RS, Gaffey TA, Stanhope CR. Pelvic mass causing vesical compression after total hip arthroplasty. Clin Orthop Relat Res. 1988;227:184–189. [PubMed] [Google Scholar]
- 25.Hays RD, Sherbourne CD, The MazelRM, ND RA. 36-Item Health Survey 1.0. Health Econ. 1993;2:217–227. doi: 10.1002/hec.4730020305. [DOI] [PubMed] [Google Scholar]
- 26.Hing CB, Young DA, Dalziel RE, Bailey M, Back DL, Shimmin AJ. Narrowing of the neck in resurfacing arthroplasty of the hip: a radiological study. J Bone Joint Surg Br. 2007;89:1019–1024. doi: 10.1302/0301-620X.89B8.18830. [DOI] [PubMed] [Google Scholar]
- 27.Holtzman J, Saleh KJ, Kane R. Gender differences in functional status and pain in a Medicare population undergoing electivetotal hip arthroplasty. Med Care. 2002;40:461–470. doi: 10.1097/00005650-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Huo MH, Gilbert NF, Parvizi J. What’s new in total hip arthroplasty. J Bone Joint Surg Am. 2007;89:1874–1885. doi: 10.2106/JBJS.G.00509. [DOI] [PubMed] [Google Scholar]
- 29.Jasani V, Richards P, Wynn-Jones C. Pain related to the psoas muscle after total hip replacement. J Bone Joint Surg Br. 2002;84:991–993. doi: 10.1302/0301-620X.84B7.13194. [DOI] [PubMed] [Google Scholar]
- 30.Khanduja A, Villar RN. The role of arthroscopy in resurfacing arthroplasty of the hip. Arthroscopy. 2008;24:122.e1–122.e3. doi: 10.1016/j.arthro.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 31.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 32.Lavigne M, Boddu Siva Rama KR, Roy A, Vendittoli PA. Painful impingement of the hip joint after total hip resurfacing: a report of two cases. J Arthroplasty. 2008;23:1074–1079. doi: 10.1016/j.arth.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 33.Lavigne M, Masse V, Girard J, Roy AG, Vendittoli PA. Return to sport after hip resurfacing or total hip arthroplasty: a randomized study [in French] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:361–367. doi: 10.1016/j.rco.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 34.Noble PC, Box GG, Kamaric E, Fink MJ, Alexander JW, Tullos HS. The effect of aging on the shape of the proximal femur. Clin Orthop Relat Res. 1995;316:31–44. [PubMed] [Google Scholar]
- 35.O’Neill M, Beaule PE, Bin Nasser A, Garbuz D, Lavigne M, Duncan CP, Kim PR, Schemitsch E. Canadian academic experience with metal-on-metal hip resurfacing. Bull NYU Hosp Jt Dis. 2009;67:128–131. [PubMed] [Google Scholar]
- 36.O’Sullivan M, Tai CC, Richards S, Skyrme AD, Walter WL, Walter WK. Iliopsoas Tendonitis. A complication after total hip arthroplasty. J Arthroplasty. 2007;22:166–170. doi: 10.1016/j.arth.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 37.Pollard TCB, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip. Two to seven year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. doi: 10.1302/0301-620X.88B5.17354. [DOI] [PubMed] [Google Scholar]
- 38.Roder C, Parvizi J, Eggli S, Berry DJ, Muller ME, Busato A. Demographic factors affecting long-term outcome of total hip arthroplasty. Clin Orthop Relat Res. 2003;417:62–73. doi: 10.1097/01.blo.0000096812.78689.f0. [DOI] [PubMed] [Google Scholar]
- 39.Shimmin A, Back D. Femoral neck fractures following Birmingham hip resurfacing. A national review of 50 cases. J Bone Joint Surg Br. 2005;87B:463–464. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 40.Shimmin AJ, Beaule PE, Campbell PA. Current concepts: metal on metal hip resurfacing. J Bone Joint Surg Am. 2008;90:637–654. doi: 10.2106/JBJS.G.01012. [DOI] [PubMed] [Google Scholar]
- 41.Toms AP, Marshall TJ, Cahir J, Darrah C, Nolan J, Donell ST, Barker T, Tucker JK. MRI of early symptomatic metal-on-metal total hip arthroplasty: a retrospective review of radiological findings in 20 hips. Clin Radiol. 2008;63:49–58. doi: 10.1016/j.crad.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 42.Trousdale RT, Cabanela ME, Berry DJ. Anterior iliopsoas impingement after total hip arthroplasty. J Arthroplasty. 1995;10:546–549. doi: 10.1016/S0883-5403(05)80160-3. [DOI] [PubMed] [Google Scholar]
- 43.Vail TP, Mina CA, Yergler D, Pietrobon R. Metal-on-metal hip resurfacing compares favorably with THA at 2 years followup. Clin Orthop Relat Res. 2006;453:123–131. doi: 10.1097/01.blo.0000238852.08497.92. [DOI] [PubMed] [Google Scholar]
- 44.Vandenbussche E, Saffarini M, Taillieu F, Mutschler C. The asymmetric profile of the acetabulum. Clin Orthop Relat Res. 2008;466:417–423. doi: 10.1007/s11999-007-0062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vendittoli PA, Lavigne M, Roy AG, Lusignan D. A prospective randomized clinical trial comparing metal-on-metal total hip arthroplasty and metal-on-metal total hip resurfacing in patients less than 65 years old. Hip Int. 2006;16:S73–S81. doi: 10.1177/112070000601604S14. [DOI] [PubMed] [Google Scholar]