Abstract
BACKGROUND:
Universal access to health care is valued in Canada but increasing wait times for services (eg, cardiology consultation) raise safety questions. Observations suggest that deficiencies in the process of care contribute to wait times. Consequently, an outpatient clinic was designed for Ensuring Access and Speedy Evaluation (Cardiac EASE) in a university group practice, providing cardiac consultative services for northern Alberta. Cardiac EASE has two components: a single-point-of-entry intake service (prospective testing using physician-approved algorithms and previsit triage) and a multidisciplinary clinic (staffed by cardiologists, nurse practitioners and doctoral-trained pharmacists).
OBJECTIVES:
It was hypothesized that Cardiac EASE would reduce the time to initial consultation and a definitive diagnosis, and also increase the referral capacity.
METHODS:
The primary and secondary outcomes were time from referral to initial consultation, and time to achieve a definitive diagnosis and management plan, respectively. A conventionally managed historical control group (three-month pre-EASE period in 2003) was compared with the EASE group (2004 to 2006). The conventional referral mechanism continued concurrently with EASE.
RESULTS:
A comparison between pre-EASE (n=311) and EASE (n=3096) revealed no difference in the mean (± SD) age (60±16 years), sex (55% and 52% men, respectively) or reason for referral, including chest pain (31% and 40%, respectively) and arrhythmia (27% and 29%, respectively). Cardiac EASE reduced the time to initial cardiac consultation (from 71±45 days to 33±19 days) and time to a definitive diagnosis (from 120±86 days to 51±58 days) (P<0.0001). The annual number of new referrals increased from 1512 in 2002 to 2574 in 2006 due to growth in the Cardiac EASE clinic. The number of patients seen through the conventional referral mechanism and their wait times remained constant during the study period.
CONCLUSIONS:
Cardiac EASE reduced wait times, increased capacity and shortened time to achieve a diagnosis. The EASE model could shorten wait times for consultative services in Canada.
Keywords: Canada Health Act, Health services, Nurse practitioner, Outpatient consultation, PharmD, Wait time
Abstract
HISTORIQUE :
L’universalité des soins est un principe important au Canada, mais l’attente de plus en plus longue pour accéder aux services (p. ex., consultations en cardiologie) soulève des questions de sécurité. Selon certaines observations, des lacunes quant au déroulement des soins ne seraient pas étrangères aux temps d’attente. C’est pourquoi la clinique ambulatoire Cardiac EASE (Ensuring Access and Speedy Evaluation) a été mise sur pied dans une pratique de groupe universitaire offrant des services de consultations en cardiologie dans le Nord de l’Alberta. Le programme Cardiac EASE comporte deux volets : un service d’accès centralisé (analyses prospectives établies selon des algorithmes approuvés par les médecins et triage précédant la consultation) et une clinique pluridisciplinaire (offrant les services de cardiologues, d’infirmières praticiennes et de pharmaciens de niveau doctoral).
OBJECTIF :
Vérifier l’hypothèse selon laquelle le programme Cardiac EASE pourrait réduire le délai pour une consultation initiale et un diagnostic définitif, tout en accroissant la capacité de gérer les demandes de consultation.
MÉTHODES :
Les paramètres principal et secondaire étaient le délai entre la demande de consultation et la première consultation et le délai avant l’obtention d’un diagnostic définitif et d’un plan de traitement, respectivement. Un groupe témoin historique traité de la façon habituelle (période de trois mois précédant l’application du programme EASE en 2003) a été comparé au groupe EASE (de 2004 à 2006). Le processus habituel de demande de consultation a été maintenu pendant l’application du programme EASE.
RÉSULTATS :
Une comparaison entre les groupes pré-EASE (n = 311) et EASE (n = 3 096) n’a révélé aucune différence quant à l’âge moyen (± É. T.) (60 ± 16 ans), quant au sexe (55 % et 52 % d’hommes, respectivement) ou quant à la raison de la demande de consultation, soit DRS (31 % et 40 %, respectivement) et arythmie (27 % et 29 %, respectivement). Le programme Cardiac EASE a abrégé l’intervalle avant une première consultation en cardiologie (de 71 ± 45 jours à 33 ± 19 jours) et l’intervalle avant un diagnostic définitif (de 120 ± 86 jours à 51 ± 58 jours) (p < 0,0001). Le nombre annuel de nouvelles demandes de consultation est passé de 1 512 en 2002 à 2 574 en 2006 en raison de la croissance de la clinique Cardiac EASE. Le nombre de patients vus au moyen du processus habituel de demande de consultation et leurs temps d’attente sont demeurés constants pendant la durée de l’étude.
CONCLUSION :
Le programme Cardiac EASE a réduit les temps d’attente, augmenté le volume de patients et abrégé l’intervalle avant l’obtention du diagnostic. Le modèle EASE pourrait contribuer à abréger les temps d’attente pour l’accès aux services de consultation au Canada.
Cardiovascular disease is the leading cause of mortality in Canada and its prevalence is increasing as the population ages (1). Cardiac consultation is often the point of entry into the health care system for diagnostic testing and intervention among patients with heart disease. Within central and northern Alberta, patients deemed ‘nonemergent’ wait three to five months for an initial cardiology consultation (2). This delay has remained constant over the past five years and is attributable to various remediable shortcomings that are endemic within the Canadian health care system. Patients awaiting consultation are at an undefined increased risk of adverse outcomes (eg, myocardial infarction and death) because management of cardiovascular disease is either not implemented or not optimized (3). Moreover, during the waiting period, there is no triage system, which is distinct from patients awaiting cardiac surgery.
Furthermore, the conventional referral process often suboptimally prepares patients for an initial cardiac consultation due to failure to prospectively collect pertinent information and perform indicated tests. These ‘intake’ errors are compounded by a failure to coordinate the consultant cardiologists so that patients are assessed by the ‘first available’ cardiologist or the cardiologist with the most applicable subspecialty. Consequently, during the first visit, an inordinate amount of time is used for data acquisition and often, additional diagnostic testing is necessary. This requires repeated visits, which is inefficient for the physician and costly for patients, who often travel great distances and have limited resources. Inefficient preparation also lengthens the time to render a final diagnostic decision and institute a treatment plan. Unless an alternate approach to cardiology consultation is implemented, these challenges will be amplified because the volume of consultation will increase in our aging population, while the number of cardiologists trained is constrained by the government.
The Canadian health care system is founded on the philosophy that universal health care should be available and accessible to all Canadians on an equal basis (4). Canadians are losing faith in health care delivery (5) and the federal government has acknowledged these concerns, highlighting that decreasing wait times should be given a high priority (6).
To this end, a program Ensuring Access and Speedy Evaluation (Cardiac EASE) was funded in response to an investigator-initiated grant proposal to the Medical Services Delivery Innovation Fund of the Alberta government. The grant proposed a new model to improve access to and the efficiency of nonemergent, tertiary care outpatient cardiology consultative services. The three-year pilot program was funded ($1 million) with the pledge that Capital Health would assume responsibility for the program if it were successful.
Cardiac EASE features a single-point-of-entry intake service that prospectively collects patient information, arranges testing (based on cardiologist-approved, evidence-based algorithms) and triages referrals (based on patient acuity). Once all testing is complete, the patient is seen in the rapid-response Multidisciplinary Consultative Clinic by a cardiologist, along with a nurse practitioner (NP) or doctoral-trained pharmacist (PharmD). This approach is designed to capitalize on the skills of alternative health care providers who are capable of performing designated functions (eg, NPs and PharmDs) and thereby uses limited cardiologist resources more efficiently, while not deviating from the Canada Health Act. We assessed the hypothesis that, in comparison with the conventional referral model (general practitioner to specific cardiologists), the Cardiac EASE model would reduce wait times for initial cardiology consultation and shorten the time to a definitive final diagnosis and disposition. A secondary hypothesis was that Cardiac EASE would increase the total number of new referrals seen (capacity) because the conventional mechanism would remain relatively constant.
METHODS
The number of new referrals received by the conventional referral mechanisms was tracked annually using the MedTech database (MedTech Global Ltd, Australia), into which all referrals were entered for scheduling and billing purposes. During the pre-EASE period (March 2003 to June 2003), all new consultations were tracked to document dates when the referrals for cardiac consultations were received. Billing and physician records were reviewed to determine the date of initial consultation, diagnostic testing, and definitive diagnosis and disposition. The pre-EASE group was compared with the patients seen in EASE (all patients referred to Cardiac EASE between January 2004 and December 2006). An implementation phase (July 2003 to December 2003) was excluded to allow clinic operations to be refined. The conventional referral model ran concurrently, but patients and referring general practitioners were offered the choice of enrolling in Cardiac EASE. Participation of consultant cardiologists in Cardiac EASE was voluntary and began with four cardiologists, but ultimately, most cardiologists in the division chose to participate (both by staffing the clinic and allowing patients referred to them to be diverted to the clinic, when appropriate). The EASE protocol was approved by the Human Research Ethics Board at the University of Alberta Hospital (Edmonton, Alberta) and all EASE patients provided informed consent for their participation in this experimental clinic model.
Cardiac EASE was designed to streamline the efficiency of consultation by cardiologists. Two linked components of the program were created: the EASE Intake Service, offering a single point of entry, intake and triage; and the EASE Multidisciplinary Consultative Clinic, offering prompt coordination and completion of diagnostic testing and therapy.
EASE Intake Service
The EASE Intake Service is staffed by an NP and a secretary, and is overseen by the medical director (a cardiologist who provides guidance on case management and triage during pre- and postconsultation periods). Rather than having requests for consultation transmitted from the referring physician’s secretary to the secretary of individual cardiologists, all referrals are sent to a single location (typically via fax) and reviewed by the EASE NP. This enables the intake team to order diagnostic testing in advance of the cardiac consultation and determine which cardiologist is best suited to see the patient, based on specialty and availability. The intake team follows a symptom-based testing algorithm to ensure that all relevant information is collected (Supplementary Figures 1 to 5 [available online at www.canjcardiol.com or www.pulsus.com]). Prospective testing is based on presenting symptoms or provisional diagnoses including shortness of breath/congestive heart failure, chest pain/angina, palpitations/syncope, murmur/valve disease and atrial fibrillation. The testing algorithms were developed by EASE cardiologists, based on American College of Cardiology and American Heart Association guidelines (Supplementary Figures 1 to 5 [available online at www.canjcardiol.com or www.pulsus.com]). The preconsultation acquisition of pertinent information and diagnostic testing established a provisional diagnosis, and increased the likelihood that a definitive diagnosis and treatment plan would be achieved at the initial cardiology consultation.
The NP performs triage based on the collection of the preconsultation information including patient symptoms, diagnostic testing available or ordered by the EASE intake team, and information from the referring physician. EASE patients are coded using a simple four-point scoring system ranging from 0 to 3 (only patients in categories 1 and 2 are considered for EASE):
0. Emergent: not eligible for EASE (eg, angina at rest, decompensated heart failure) – these patients were sent to the emergency department.
1. Urgent (eg, increasing anginal chest pain) – these patients were scheduled for EASE within one week.
2. Stable (eg, atypical chest pain, palpitations, management of atrial fibrillation, asymptomatic heart murmur) – these ‘typical’ EASE patients were designated to be seen within four to six weeks.
3. Elective (eg, risk factor reduction follow-up) – these patients were deemed not to need follow-up within three months and were not entered in EASE but referred back to their general practitioner.
EASE Multidisciplinary Consultative Clinic
The EASE Intake Service would be of only modest benefit if a new means of organizing cardiologists and extending their impact was not established. The EASE Multidisciplinary Consultative Clinic capitalizes on the capabilities of other health care providers (NPs and PharmDs) to perform a history and physical assessments, collate diagnostic testing results and present this information to the cardiologist. This enables the consultant to focus the history and examination on the most pertinent aspects of the case, providing more time to discuss diagnosis and treatment plans with the patient. While the cardiologist completes the dictation to the referring physician, the NP or PharmD reinforces the care plan, and coordinates follow-up testing and procedures. They also provide patient education, typically dealing with medication issues (compliance, adverse effects, etc), explaining the disease processes, and encouraging prevention and participation in the care plan. Cardiac EASE is designed to optimize initial consultations and is not intended for repeat visits. Patients requiring more than two visits are transferred to a cardiologist’s individual clinic.
Study design and analysis
A comparison group from the past was used; hence, the nature of the study was a ‘historical control cohort study’. The unit of analysis was the patients. The patients in the pre-EASE group were independent from patients in the EASE group. The main analysis compared the wait time for cardiology consultation before and during the Cardiac EASE program. Two primary outcomes were defined: the difference between EASE and conventional care in the time between receipt of referral and the date the patient was first seen in consultation; and the date when a definitive diagnosis or treatment plan was established.
For each of these continuous measures, a summary score was presented (mean ± SD) and compared between the two groups using t tests. Due to the unbalanced distribution of patients in these groups, a log transformation of the primary outcome was considered. Because the significance of the difference in wait times was validated by the log-transformed data, it was decided that the absolute values would be used. Bivariate associations between the collected variables and the primary outcome were examined using χ2 tests for categorical data (sex, referral reason and referring region) and Wilcoxon’s test for non-parametric data (age). Multivariate linear regression models were used to check the influence of possible interactions and to adjust for baseline imbalances in statistically significant (P<0.05) covariates (including interactions) between the two groups.
In an analogous fashion, the interval between the receipt of the referral and the prespecified secondary end point (completion of the cardiology consultation defined as a final diagnostic decision or implementation of a treatment plan) was examined. The proportion of patients with appropriate diagnostic testing ordered at triage and available by the time of initial cardiac consultations was also measured. Cardiac EASE was also designed to provide prompt feedback to the referring physician. Consequently, the interval between consultation and the date the letter was transcribed was compared between the pre-EASE and EASE groups. Finally, although it was not a prespecified end point, the volume and wait times in the conventional referral program were tracked.
Statistics
Values are presented as mean ± SD. An unpaired Student’s t test was used to compare pre-EASE and EASE wait times, time to completion of consultation and time to transcription of the consultative letter. To determine whether Cardiac EASE altered the reason for referral or geographic origin of referrals, the age, sex, referring region and reason for referral in the pre-EASE and EASE periods were compared using a two-way ANOVA. Statistical analysis was performed using SAS version 9.1 (SAS Institute Inc, USA).
RESULTS
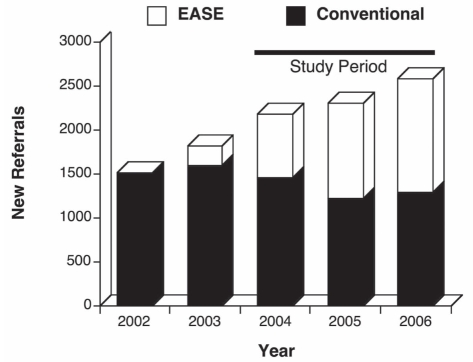
There were 1512 new referrals in the year before Cardiac EASE was implemented. The annual referral volume increased to 2574 by 2006, at which time, one-half of these new referrals per year were EASE patients (Figure 1). A total of 311 patients were assessed in the pre-EASE period, while 3096 were assessed during EASE (Table 1). The median age (61 years in both groups) and sex (55% and 52% male, respectively) were similar in the pre-EASE and EASE groups, and did not change significantly during the study. Likewise, referrals originated from similar regions of Alberta (two-thirds from within Edmonton’s Capital Health Region), and the common reasons for referral – chest pain (31% and 40%, respectively) and rhythm disturbances (27% and 29%, respectively) – were similar between the pre-EASE and EASE groups (Table 1).
Figure 1).
The increasing number of patients seen in Cardiac EASE (Ensuring Access and Speedy Evaluation) over time. Note the increase in new referrals via the EASE mechanism was due to ‘new capacity’. Cardiac EASE added to and did not decrease new referrals seen by the conventional mechanism
TABLE 1.
Baseline characteristics of pre-EASE (Ensuring Access and Speedy Evaluation) and EASE patients
| Characteristic | Pre-EASE (n=311) | EASE (n=3096) | P |
|---|---|---|---|
| Age, years | 0.99 | ||
| Mean ± SD | 60±16 | 60±16 | |
| Median (range) | 61 (50.2–72.6) | 60.9 (49.3–72.3) | |
| Age group, % | 0.64 | ||
| <40 years | 12.2 | 11.1 | |
| 40–60 years | 34.4 | 36.9 | |
| >60 years | 53.4 | 52.0 | |
| Male sex, % | 54.7 | 51.9 | 0.35 |
| Reason for referral, % | <0.0001 | ||
| Chest pain | 31.2 | 39.7 | |
| Coronary artery disease assessment, hypertension, other | 19.6 | 4.8 | |
| Abnormal ECG, arrhythmia, atrial fibrillation, palpitations | 26.7 | 28.8 | |
| Presyncope, syncope, valve disease | 11.6 | 12.2 | |
| CHF, shortness of breath | 6.1 | 11.0 | |
| Preoperative consultation | 4.8 | 3.7 | |
| Referral region, % | 0.0021 | ||
| Palliser, Calgary, David Thompson and East Central | 25.1 | 19.3 | |
| Capital Health* | 64.0 | 62.8 | |
| Aspen, Peace Country and Northern Lights | 8.4 | 11.1 | |
| Out of province (NWT, Yukon, BC, SK) | 2.6 | 6.8 |
Capital Health is the site of the EASE clinic. BC British Columbia; CHF Congestive heart failure; ECG Electrocardiogram; NWT Northwest Territories; SK Saskatchewan
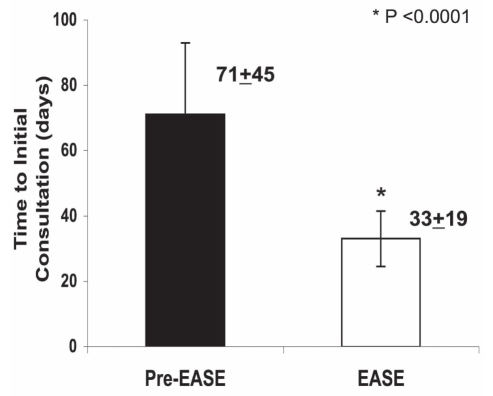
The mean wait time (interval between receipt of referral and date seen in consultation) was reduced from 71±45 days in the pre-EASE group to 33±19 days in the EASE group (P<0.0001) (Figure 2). Interactions between the treatment groups and all four baseline covariates were considered for wait time. The results of the multivariate regression showed different treatment effects across referral regions. Wait times for pre-EASE patients originating from within the Capital Health region were longer than those for patients referred from outside the region; however, this effect was attenuated with Cardiac EASE (Table 2). The mean wait time adjusted for baseline confounders, age and geographical origin of the referral still showed a significant treatment effect (P<0.0001). The interval between the date of referral and the date first booked also confirmed the group effect in waiting times (P<0.0001).
Figure 2).
Wait times for initial consultation decreased during Cardiac EASE (Ensuring Access and Speedy Evaluation)
TABLE 2.
Wait times for referrals by region
| Referral region |
Pre-EASE |
EASE |
||
|---|---|---|---|---|
| n | Wait time, days* | n | Wait time, days* | |
| David Thompson, East Central, Palliser, Calgary | 78 | 59.6±43.5 | 597 | 31.4±16.8 |
| Capital Health | 199 | 76.5±45.2 | 1944 | 33.0±18.9 |
| Aspen, Peace Country and Northern Lights | 26 | 66.4±39.1 | 345 | 34.8±18.4 |
| Out of province (NWT, Yukon, BC, SK) | 8 | 50.9±34.3 | 210 | 36.3±29.1 |
Data presented as mean ± SD. BC British Columbia; EASE Ensuring Access and Speedy Evaluation; NWT Northwest Territories; SK Saskatchewan
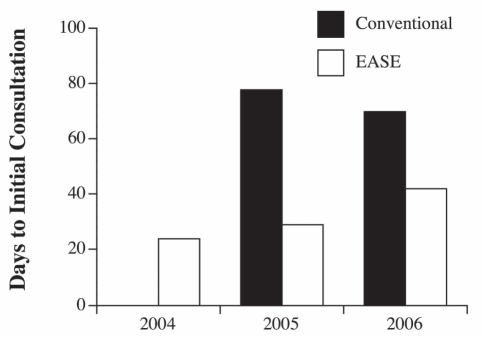
There were dramatic increases in the volume of patients seen by Cardiac EASE, with a growth of nearly 50% in 2005 relative to 2004 and 19% in 2006 relative to 2005 (Figure 1). As EASE volumes increased, an increase in wait times was observed, growing from 24±13 days in 2004 to 42±20 days in 2006 (P<0.05) (Figure 3). Nonetheless, patients were seen significantly sooner in each year of EASE than had been the case in the pre-EASE period (P<0.0001), even in the third year of the program.
Figure 3).
Time to initial consultation increased during Cardiac EASE (Ensuring Access and Speedy Evaluation) but remained shorter than in the conventional track. Despite the increase in wait times within EASE in 2006, wait times remained substantially shorter than in patients seen through the conventional mechanism. Data for wait times in the conventional pathway were not available for 2004 because of a change in the office medical record billing system during that year
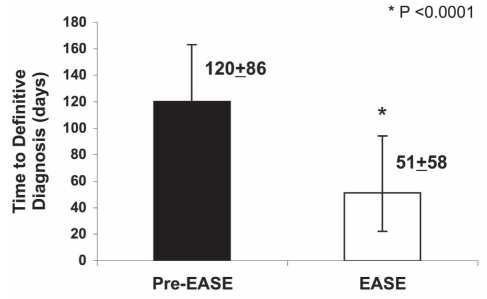
Patients seen in the Cardiac EASE clinic had a significantly shorter wait to the rendering of a definitive diagnostic decision and treatment plan compared with pre-EASE (51±58 days and 120±86 days, respectively; P<0.0001) (Figure 4). The most common discharge diagnosis for both pre-EASE and EASE patients was noncardiac chest pain (Table 3). Other diagnoses common in both groups included risk factor management for hyperlipidemia, angina and arrhythmia (Table 3).
Figure 4).
Time to definitive diagnosis or disposition decreased during Cardiac EASE (Ensuring Access and Speedy Evaluation)
TABLE 3.
Comparison of the final diagnosis between pre-EASE (Ensuring Access and Speedy evaluation) and EASE patients
| Discharge diagnosis | Pre-EASE, % | EASE, % |
|---|---|---|
| Chest pain | ||
| Noncardiac | 16.1 | 19.5 |
| Cardiac (angina) | 14.2 | 8.5 |
| Pericarditis | 0.0 | 0.1 |
| Other | 0.2 | 0.2 |
| Risk factor modification | ||
| Hyperlipidemia | 12.5 | 11.2 |
| Hypertension | 8.2 | 9.4 |
| Smoking cessation | 2.9 | 2.4 |
| Obesity | 0.7 | 1.3 |
| Diabetes management | 0.7 | 1.5 |
| Cardiac rehabilitation | 0.2 | 0.4 |
| Stress management | 0.0 | 0.1 |
| Cardiac rehabilitation | 0.2 | 0.4 |
| Arrhythmia | ||
| Palpitation | 2.7 | 9.5 |
| Atrial fibrillation/flutter | 9.4 | 7.6 |
| Other | 10.4 | 3.4 |
| Dyspnea | ||
| Cardiomyopathy/congestive heart failure | 3.1 | 3.3 |
| Other | 0.5 | 3.8 |
| Valvular or congenital heart disease | 6.8 | 5.1 |
| Preoperative assessment | 3.6 | 3.3 |
| Abnormal electrocardiogram | 0.2 | 2.7 |
| Syncope and presyncope | ||
| Cardiac or vasovagal | 1.0 | 1.4 |
| Noncardiac | 0.5 | 1.5 |
| Other | 1.2 | 0.8 |
| Pulmonary hypertension | 0.0 | 0.5 |
| Other | 4.8 | 2.5 |
Within Cardiac EASE, 95% of patients were deemed to have had sufficient diagnostic testing by the time of the initial cardiac consultation. Of the 5% of tests not completed in advance of the initial consultation, the majority were radionuclide stress tests (47%) or transthoracic echocardiograms (25%).
Follow-up
After being seen in Cardiac EASE, the vast majority of patients had follow-up scheduled with their primary care physician (98%). A total of 20% of patients also had a completed follow-up with a cardiologist, while 3% were referred to specialty clinics within cardiology (ie, a heart function clinic, anticoagulation clinic or pulmonary hypertension clinic). A total of 3% of all EASE patients were admitted to hospital. In contrast, follow-up was less complete in pre-EASE patients; only 85% had a completed follow-up confirmed. A total of 14% had outstanding testing or appointments that could not be tracked, and 0.6% were admitted to the hospital.
The rapidity of feedback to the referring physician in the form of a transcribed letter was not significantly different between the pre-EASE and EASE groups, taking 8±22 days and 9±14 days, respectively (P=0.51). However, there was more consistency in time to transcription in the EASE group (as indicated by the smaller SD).
DISCUSSION
This investigator-initiated program was created to address systematic shortcomings observed within the Canadian health care system. With an increasing burden of cardiovascular disease and a limited supply of cardiologists, this multidisciplinary program aimed to improve the access to and efficiency of cardiology consultation for nonemergent outpatients. Overall, the impact of Cardiac EASE was dramatic and sustained, resulting in reduced wait times for patients awaiting nonemergent cardiac consultation, more rapid definitive diagnosis and increased capacity for referral. It is noteworthy that the wait times for patients seen through the conventional referral process did not decline during the study period, suggesting that it was the Cardiac EASE process that accounted for the shortening of time to consultation (Figure 3).
Compared with pre-EASE, significantly shorter wait times were observed across all years of EASE, with reductions in the time to completion of the initial consultation, and time to rendering of a diagnostic decision and treatment plan (Figures 2 and 4). This was largely attributable to the vast majority of patients (95%) having noninvasive diagnostic testing completed, with results available at the time of initial consultation.
An English-language PubMed literature search, conducted before initiating Cardiac EASE and again in 2006, using appropriate search terms, failed to detect examples of new approaches to the delivery of consultative cardiology. There was a report of the Rapid Access Heart Failure Clinic in a district general hospital in London (United Kingdom), designed to diagnose and manage new cases of heart failure presenting for the first time in the community (7). Although this program was also beneficial, it differed from Cardiac EASE in that the initial assessment of patients was performed by a physician (specialist registrar in cardiology) rather than an NP or PharmD. Moreover, this clinic saw 383 patients in approximately 15 months, which was a much smaller number than in Cardiac EASE. Thus, the program described by Fox et al (7) is quite different from Cardiac EASE (it was small, physician-based, focused only on heart failure and did not use algorithms and prospective testing). To our knowledge, Cardiac EASE is a new model for delivering general cardiology consultative services, with three novel aspects – proactive solicitation of information, prospective performance of diagnostic testing guided by algorithms, and use of both NPs and PharmDs to enhance services (Supplementary Figures 1 to 5 [available online at www.canjcardiol.com or www.pulsus.com]).
Following the initiation of Cardiac EASE, the Council of the Canadian Cardiovascular Society commissioned a working group to propose targets for acceptable wait times (8). The proposed ‘acceptable’ wait times for cardiac consultation for indications ranging from chest pain to palpitations was four to six weeks, which was the target achieved by EASE (Figure 3). Patients seen before the implementation of EASE waited an average of 10 weeks to see a cardiologist. This wait time is consistent with that reported in a survey (9) conducted among academic specialists with certification in cardiology (median 9.1 weeks). Patients seen in the Cardiac EASE clinic in 2004, 2005 and 2006 waited a mean of 3.4, 4.1 and six weeks, respectively, to see a cardiologist. Because the space available and budget for the Cardiac EASE program were fixed, while the referral volume increased, it is not surprising that wait times gradually increased, ultimately approaching the upper ‘acceptable’ limit (Figure 3). Strategic planning for growth is needed to ensure that timely access and efficiency are maintained. However, this physician-initiated clinic was relatively inexpensive to create and operate, and additional work was performed (ie, the referral volume seen in the cardiology division by the conventional mechanism did not decline over the study period [Figure 1]).
As indicated in the results section, 98% of EASE patients versus 85% of conventional track patients were referred back to and saw their general practitioner. Thus, the Cardiac EASE clinic not only saw the patients sooner but also got them back to their referring doctor more reliably.
Limitations
There are limitations to the present study, notably that it was not a randomized clinical trial. As a pilot program to improve health care, the terms of the grant did not permit random assignment of patients. In defense of the Cardiac EASE program, the sparse results of our literature review suggest that few practices quantify or report their consultative process in any manner.
In a historical cohort study, data such as those for the study group and the historical group may not be comparable in kind and quality. Moreover, the observed difference (the decrease in wait time) over time could theoretically be due to changes in variables other than intervention (Cardiac EASE). Arguing against this, the demographics of the EASE and conventional groups were nearly identical, and the wait times in the conventional referral group remained unchanged during the study period. The present study does have a drawback in that the historical control group had a small sample size compared with that of the EASE group. However, although data on pre-EASE patients were collected retrospectively, the investigators ensured information was limited to that available from chart review, the quality of data collection and proper analysis tools. Moreover, a previous survey of our medical centre wait times confirmed that the magnitude of delay to consultation has remained relatively long and stable for many years (2). Furthermore, we monitored the volume and wait times for consultation through the conventional process and the volume remained constant while wait times continued to exceed two months (Figure 3).
A final limitation of the study is that formal physician satisfaction surveys and economic impact analyses were not performed. Satisfaction by referring physicians may be inferred by the increasing volume of patients sent to the Cardiac EASE clinic over time, despite the absence of any advertising of the program. While there are limitations, this physician-designed program, with a three-year budget of less than $1 million, added approximately 3000 new cardiology consultations beyond the conventional referral rate (which remained constant) and decreased the time to consultation by more than 50%.
Cardiac EASE did not spawn ‘unnecessary’ referrals or bring out the ‘worried well’. To avoid this possibility, the intake team screened out patients who were not appropriate for the Cardiac EASE program during the preconsultation triage phase. Evidence that this worked is seen in Tables 1 and 3, which show similar reasons for referral and final diagnoses in the EASE and non-EASE referrals. The Cardiac EASE clinic simply made the process faster and more efficient. It is also noteworthy that there was no advertising for the Cardiac EASE program; the availability of the service was spread by word of mouth.
CONCLUSIONS
By shortening wait times to initial consultation and obtaining a definitive diagnosis, Cardiac EASE improved access to and the efficiency of patient care. The clinic also doubled the number of new referrals seen by the cardiology group and did not decrease use of the conventional referral mechanism. Capitalizing on health care providers (namely NPs and PharmDs) who are able to perform delegated tasks, such as patient assessment, triage, coordination of noninvasive diagnostic testing, and the collection and presentation of information to the cardiologist, was key to the success of Cardiac EASE. Cardiac EASE successfully implemented an approach that addressed barriers to timely care that were identified at the grassroots level. EASE could serve as a prototype for achieving target-based wait times in other tertiary care centres.
Algorithm for assessment of patients with a presenting complaint of chest pain. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CAD Coronary artery disease; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; INR International normalized ratio; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; PT Prothrombin time
Algorithm for assessment of patients with a presenting complaint of congestive heart failure (CHF) or shortness of breath. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; ER Emergency room; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; MD Medical doctor; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist
Algorithm for assessment of patients with a presenting complaint of palpitations or syncope. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; TSH Thyroid-stimulating hormone
Algorithm for assessment of patients with a presenting complaint of atrial fibrillation. A FIB Atrial fibrillation; ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; INR International normalized ratio; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; PT Prothrombin time; TSH Thyroid-stimulating hormone
Algorithm for assessment of patients with a presenting complaint of valve disease. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; INR International normalized ratio; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; PT Prothrombin time
Acknowledgments
Evelyn Maier RN MN NP is acknowledged for her selfless efforts as the initial NP in cardiology. Her efforts aided the launching of Cardiac EASE.
Footnotes
FUNDING: SL Archer is supported by the Canadian Institutes of Health Research, a National Institutes of Health grant (HL071115 and HL099462-01) and the Medical Services Delivery Innovation Fund.
REFERENCES
- 1.Heart and Stroke Foundation of Canada Taking control: Lowering your risk of heart disease and stroke<ww2.heart&stroke.ca/PageID-1975&articleID-53317&Sfc-stroke&From-subCategory> (Version current at December 18, 2006).
- 2.Capital Region Medical Staff Association Capital region physician access survey: Survey of wait times to access physician services (Physician Access Survey)<http://www.crmsa.ab.ca/Archives/cr_physician_access99.htm> (Survey Part 5, Version current at August 24, 2009).
- 3.Teo KK, Spoor M, Pressey T, et al. Impact of managed waiting for coronary artery bypass graft surgery on patients’ perceived quality of life. Circ. 1998;98(19 Suppl):29–33. [PubMed] [Google Scholar]
- 4.Health Canada The Canada Health Act. 1984.
- 5.Romanow RJ. Building on values: The future of health care in Canada final report. National Library of Canada. 2002.
- 6.Wait Time Alliance for Timely Access to Health Care. It’s about time: Achieving benchmarks and best practices in wait time management – final report. <http://www.wcwl.org> (Version current at August 24, 2009).
- 7.Fox KF, Cowie MR, Wood DA, Coats AJ, Poole-Wilson PA, Sutton GC. A Rapid Access Heart Failure Clinic provides a prompt diagnosis and appropriate management of new heart failure presenting in the community. Eur J Heart Fail. 2000;2:423–9. doi: 10.1016/s1388-9842(00)00108-2. [DOI] [PubMed] [Google Scholar]
- 8.Knudtson ML, Beanlands R, Brophy JM, et al. Treating the right patient at the right time: Access to specialist consultation and noninvasive testing. Can J Cardiol. 2006;22:819–24. doi: 10.1016/s0828-282x(06)70299-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Massel D. Access to an outpatient cardiology consultation in southwestern Ontario. Can J Cardiol. 1999;15:879–83. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Algorithm for assessment of patients with a presenting complaint of chest pain. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CAD Coronary artery disease; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; INR International normalized ratio; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; PT Prothrombin time
Algorithm for assessment of patients with a presenting complaint of congestive heart failure (CHF) or shortness of breath. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; ER Emergency room; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; MD Medical doctor; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist
Algorithm for assessment of patients with a presenting complaint of palpitations or syncope. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; TSH Thyroid-stimulating hormone
Algorithm for assessment of patients with a presenting complaint of atrial fibrillation. A FIB Atrial fibrillation; ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; INR International normalized ratio; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; PT Prothrombin time; TSH Thyroid-stimulating hormone
Algorithm for assessment of patients with a presenting complaint of valve disease. ALT Alanine aminotransferase; AST Aspartate aminotransferase; CBC Complete blood count; CXR Chest x-ray; EASE Ensuring Access and Speedy Evaluation; ECG Electrocardiogram; ECHO Echocardiogram; INR International normalized ratio; LAT Lateral; LBBB Left bundle branch block; LVH Left ventricular hypertrophy; MIBI Methoxyisobutylisonitrile test; NP Nurse practitioner; PA Posteroanterior view; PharmD Doctoral-trained pharmacist; PT Prothrombin time