Abstract
In any given year, only about 10% of the nearly two million adolescents exhibiting substance abuse or dependence in the United States receive substance abuse treatment. Given this state of affairs, it is unlikely that the massive effort and expenditure of resources over the past decade on developing, testing, and disseminating effective treatments for adolescent substance abuse can have an appreciable impact on the prevalence of substance use disorders among the adolescent population. In order to substantially diminish the pervasive gap between levels of need for and utilization of adolescent substance abuse treatment, specialized assertive outreach strategies may be needed. This paper outlines a framework for assertive outreach for adolescents with substance use disorders, and proposes specific types of strategies for identifying and enrolling such adolescents into treatment. Implications for practice and policy pertaining to adolescent substance abuse treatment service delivery are considered.
Keywords: Assertive outreach, adolescent substance abuse treatment, treatment gap, treatment engagement, service utilization
It has been said that the middle to late 1990s marked the onset of a renaissance period in adolescent substance abuse treatment research.1,2 In particular, the past decade has witnessed the emergence of a variety of individual, group, and family-based substance abuse treatment models which are firmly grounded in adolescent developmental theory and research.3,4 A solid base of empirical support for the efficacy of such models has taken shape over dozens of randomized clinical trials conducted over this period (for comprehensive reviews, see 5,6). Based on an accumulation of scientific evidence, a number of treatment approaches for adolescent substance abuse and associated behavioral problems have been deemed “empirically supported” according to official criteria and guidelines for evidence-based practice.7,8 Further, several research-based adolescent treatments have been delineated as best-practice models by various blue-ribbon task forces, panels, and workgroups.9,10,11,12 (See also http://modelprograms.samhsa.gov; http://www.nida.nih.gov/BTDP/effective/Effective.html; http://www.colorado.edu/cspv/blueprints/index.html). Formal practice parameters for research-based adolescent substance abuse treatment have been specified over the past decade and continue to be updated and refined.13,14
By all accounts, the adolescent substance abuse treatment research renaissance continues to evolve and move forward in the present. A primary focus of contemporary empirical work in this area is on transporting and embedding empirically supported treatments for adolescent substance abuse into non-research clinical settings in local communities. Critical steps along this pathway have taken the form of two multi-site randomized field trials funded by the Substance Abuse and Mental Health Services Administration (SAMHSA), namely, the Cannabis Youth Treatment study and the Adolescent Treatment Model program.15, 16 In addition to these field investigations, a number of smaller-scale dissemination studies have examined the effectiveness of empirically supported adolescent treatments when implemented in clinical settings within local communities apart from the direct involvement of outside experts.17–21 Based on this collective body of research, a general conclusion is that a variety of empirically supported treatments for adolescent substance abuse and associated problem behaviors can be effective at the local level provided that such treatments are delivered competently and with sufficient adherence to prescribed treatment protocols. It appears, however, that levels of provider fidelity to research-based treatment models tend to diminish markedly in absence of expert oversight and supervision.17,18,20 Accordingly, a high priority for current and future research in this area is to delineate the organizational, structural, administrative, and clinical contexts conducive to the local sustainability of empirically supported treatments for adolescent substance abuse.22–29
A Public Health Perspective on Adolescent Substance Abuse Treatment Research
It is fair to say that the expansive body of empirical research to date on the development, testing, and dissemination of effective treatments for adolescent substance abuse has been conducted ultimately in the service of a single overarching objective. This objective is to lower the prevalence of substance abuse and associated high-risk behavior within the adolescent population to a degree which has significant public health benefits.30–32 The urgency and timeliness of this public health priority is underscored by recent prevalence estimates indicating that each year approximately two million adolescents in the United States between ages 12 and 17 exhibit levels of substance use consistent with official diagnostic criteria for substance abuse or dependence.33 It is well known that this vast group of adolescents (about 8% of the adolescent population in the United States) is at substantial risk for a myriad of adverse consequences and threats to short- and long-term physical, mental, and emotional health.34–39 This prognosis is largely attributable to the fact that once levels of substance use during adolescence reach levels of chronicity characterized by abuse or dependence, such problems are unlikely to abate naturally over time and, barring some form of intervention, typically carry over into adulthood.40,41 Unmitigated substance abuse persisting from adolescence into adulthood exacts heavy social and economic costs and therefore constitutes one of today’s most pressing public health concerns.42–46 The widespread dissemination of empirically supported and effective treatments for adolescent substance abuse is a primary component of current policy initiatives to reduce the prevalence of adolescent substance abuse as well as its massive public health consequences and costs to society.47
The superordinate objective of minimizing the prevalence of adolescent substance abuse is only partially addressed, however, by the mass dissemination of effective research-based treatments. An additional facet of this mission is ensuring that effective treatments, once put in place and made available on a widespread scale, are actually utilized by a significant proportion of the adolescent population in need of such services. Unfortunately, it is well known that for a variety of reasons the overwhelming majority of adolescents in the United States who are in need of substance abuse treatment do not receive it.48 Specifically, 90% of adolescents in the U.S. who abuse or are dependent on substances receive no formal substance abuse treatment services.33 Roughly 60% of this same group receives neither substance abuse nor mental health services. This gaping disparity between levels of need for and utilization of existing services threatens to undercut any potential public health returns on the incalculable investment of resources directed over the past decade toward the development, testing, and dissemination of effective treatments for adolescent substance abuse.
The need for innovative strategies to increase rates of treatment utilization among the population of adolescents with substance use disorders appears both clear and critical. Unfortunately, such innovations have been slow to emerge. There are undoubtedly many factors to which the dearth of strategic advances in this area may be attributed. One likely factor is the paucity of resources devoted to research on access and utilization of adolescent substance abuse treatments relative to the breadth and magnitude of support for testing the efficacy of such treatments49, 50 There are some encouraging signs, however, that a shift in this resource imbalance may be imminent. Specifically, in June of 2003 the National Institute on Drug Abuse (NIDA) convened the Health Services Research Blue Ribbon Task Force to assess the status of and make recommendations for improving the relevance and impact of NIDA’s portfolio of health services research.51,52 The final report of the Task Force emphasized the need for services research “concerned with understanding who enters and receives drug treatment as well as how to decrease barriers and improve access” to empirically supported and effective treatments (p. 16).52 The goals and recommendations of the Task Force contributed to the establishment or expansion of several programs to fund drug abuse services research.53, 54 Such funding initiatives hold great promise for stimulating the development of new strategies to enhance the widespread utilization of effective research-based treatments for adolescent substance abuse.47
Increasing the Rate of Adolescent Substance Abuse Treatment Utilization Through Assertive Outreach
One worthwhile focus for new research on strategies to increase rates of adolescent substance abuse treatment utilization is in the area of assertive outreach.55, 56 Briefly, assertive outreach is an emerging model for engaging and providing services to individuals from high-risk populations, which has evolved out of the Assertive Community Treatment (ACT) approach for severe mental illness.57 The ACT model has been described as a paradigm shift in mental health treatment which places great emphasis on the deinstitutionalization of the seriously mentally ill and other difficult-to-treat populations.58 The ACT approach stresses home- and community-based services as alternatives to traditional hospital and clinic settings for treatment delivery. Under the ACT model, clinical services are comprehensive, coordinated, delivered by multidisciplinary teams, highly tailored to individual needs, and available 24 hours per day.
As a component of ACT, the assertive outreach approach is implemented by workers who are familiar with the local community, who understand the culture of the target population, and who are viewed as trusted sources of information. Assertive outreach workers serve as role models, educators, and advocates for members of high-risk populations to engage in and receive essential services including prevention and treatment. As synopsized by Ryan and Morgan,56 an assertive outreach approach:
“Engages [individuals] … with complex needs who are resistant to contacting services
Proactively reaches out to people in their own ‘territory’ in the community
Assesses need comprehensively, develops individually tailored care packages and effectively coordinates care across agencies
Optimizes the recovery of potential service users (p. 12)”
Assertive outreach programs have been implemented successfully with a number of difficult-to-engage populations including substance abusing adult homeless persons with comorbid mental illness and risk for HIV.59–62
Assertive outreach has been suggested as a general strategy for increasing rates of treatment participation among substance abusing or dependent adolescents and their family members.63 It is likely, however, that assertive outreach as traditionally designed and implemented would fail to access and engage a significant proportion of the untreated substance abusing or dependent adolescent population. Specifically, assertive outreach is designed primarily around the needs of chronic, severely impaired, highly comorbid and multi-problem persons existing largely on the fringes of mainstream society beyond the reach of established service systems. As discussed further on, however, this description does not apply to a large proportion of adolescents with a clinically diagnosable substance use problem who are not in treatment. On the contrary, a substantial proportion of adolescents with substance use disorders may successfully elude the treatment system precisely because they do not exhibit emotional or behavioral comorbidities which could signal an apparent need for treatment. As such, it may be argued that adolescents with substance use disorders who are among the most difficult to engage into treatment are not found primarily on the margins of society, but rather are fully integrated within the social structures and systems comprising mainstream adolescent culture. Accordingly, strategic initiatives to reduce the prevalence of substance abuse and dependence among adolescents should incorporate assertive outreach strategies tailored to the relatively non-cormorbid and mainstream segment of this population.
Designing and Tailoring Assertive Outreach Strategies for Substance Abusing Adolescents
To be effective, assertive outreach strategies must be developed and implemented in a manner consistent with the clinical characteristics and needs of adolescents with substance use disorders. These characteristics have been well documented by a large volume of basic and applied clinical research conducted over the past several decades. Findings across this body of research are fairly consistent in portraying adolescents with substance use disorders as a generally chronic, antisocial, and recalcitrant population. Specifically, research indicates that such adolescents typically come from dysfunctional families, are poorly connected to school, and are entrenched within substance using and deviant peer networks.64–67 Moreover, the majority of such adolescents exhibits one or more comorbid clinical diagnoses including depression, conduct disorder, and ADHD.68–72 Furthermore, many adolescents with substance use disorders have been arrested and/or are on legal probation. 73–75 Compounding this complex constellation of risks is the fact that adolescents with substance use disorders are generally unmotivated to change and resistant toward participating in treatment.76, 77
In light of this profile, it is apparent that assertive outreach is needed to increase rates of substance abuse treatment utilization among the chronically antisocial, emotionally disturbed, and offending segments of the adolescent population.78,79 Such outreach efforts among this “deep-end” group are likely to be most successful when implemented in a manner consistent with the emerging Gateway Provider Model (GPM) of youth service access.80 Briefly, a GPM approach toward assertive outreach for substance abusing adolescents hinges on equipping providers within so-called gateway service systems for youth with the knowledge and tools to recognize substance use problems, and to work in a coordinated manner across agencies to link youth exhibiting such problems with appropriate treatment services.81, 82 Primary gateway service systems for adolescent substance abusers include juvenile justice,83,84 child and adolescent mental health,85 school-based counseling and other special programs,86,87 emergency rooms, hospitals, and primary medical care settings,85,88 child welfare and related social services,89 as well as shelters and other facilities serving runaway and homeless youth.90
A GPM approach toward identifying adolescents with substance use disorders holds great promise for directing a more substantial proportion of this population into treatment. Efforts based on the GPM to forge and strengthen collaborative linkages across service systems are generally consistent with contemporary models for child and adolescent mental health care reform.91–93 There is reason for concern, however, that treatment outreach strategies that are channeled through gateway social service programs and systems may have little impact on substance abusing or dependent adolescents who are least likely to access such services, namely, those without comorbid emotional or behavioral disorders. A recent cross-sectional survey by Garland et al.94 indicates that substance abusing or dependent adolescents without comorbid emotional or behavioral disorders are significantly less likely to access mental health and related gateway social services relative to their more seriously impaired and comorbid counterparts. In fact, survey findings indicate that in absence of a comorbid diagnosis adolescents with substance use disorders are no more likely to receive services than adolescents without any clinical diagnosis whatsoever.94 These results support the view that distinctive and specialized outreach strategies may be needed for adolescents whose substance use problems are unaccompanied by emotional or behavioral comorbidities, and who are therefore unlikely to make contact with the types of service systems which could provide an entryway into substance abuse treatment. As such, this segment of the adolescent population may be at particularly high risk given that, as noted previously, substance abuse or dependence during adolescence in absence of some form of clinical intervention is likely to progress toward more chronic stages of addiction during adulthood.
The Prevalence of Emotional and Behavioral Comorbidities Among Adolescents with Substance Use Disorders
It is reasonable to question whether adolescents exhibiting substance use disorders without emotional or behavioral comorbidities constitute a subpopulation sizeable enough to warrant the development of specialized assertive outreach strategies. After all, it is generally held that the majority of adolescents with substance use disorders manifests at least one comorbid clinical condition.40 This view stems largely from studies of adolescents in substance abuse treatment among whom rates of comorbidity generally range from 70% to 90%.69,71,95,96 By contrast, a more limited body of research on substance use disorders among adolescents in the general population reveals considerably lower rates of comorbidity ranging from approximately 50% to 60%.66,95,96 Based on existing population-based estimates, it appears that roughly one-third to one-half of adolescents with substance use disorders may be relatively free of comorbid clinical conditions that could both signal the need for drug treatment and raise the chances of being referred to treatment through an existing service system.99
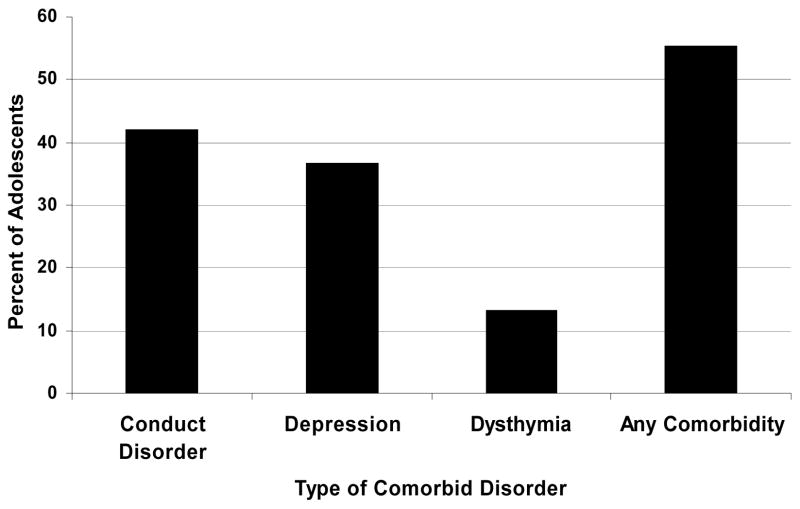
To further corroborate these population-based comorbidity estimates, the authors conducted a brief secondary analysis of data from the baseline version of the National Comorbidity Survey (NCS).100 Briefly, the baseline NCS is a large-scale national household survey (n = 8,098) conducted in the early 1990s assessing the prevalence of various emotional and behavioral disorders among individuals between ages 15 and 54 in the general population of the United States. The subgroup of NCS participants in the age 15–18 cohort meeting official diagnostic criteria for alcohol/drug abuse or dependence over the past 12 months (n = 60 out of 578 adolescents) was selected for the analysis. The analysis examined the proportion of adolescents in the sample meeting criteria for a comorbid emotional or behavioral diagnosis over the past 12 months including conduct disorder, major depression, and dysthymia. As shown in Figure 1, the results indicated that 55.3% of substance abusing or dependent adolescents in the general population manifest at least one of these three comorbid conditions (although this percentage may have been higher had ADHD been included in the survey). These results based on the NCS are quite consistent with those reported in other population-based studies indicating prevalence rates between 50% and 60% for diagnosable comorbid emotional or behavioral conditions among adolescents with substance use disorders.
Figure 1.
Percentages of Adolescents with Substance Abuse or Dependence Reporting Comorbid Depression, Conduct Disorder, Dysthymia, or Any Comorbid Disorder – National Comorbidity Survey.
The Role of Comorbidity in the Utilization of Adolescent Substance Abuse Treatment
The disparity between rates of comorbidity reported in clinical versus population-based research on adolescent substance abuse suggests that comorbidity may be associated with the likelihood of receiving substance abuse treatment.101 The authors investigated this hypothesis by conducting a brief analysis using data from the 2005 National Survey on Drug Use and Health (NSDUH).33 The NSDUH is an annual household survey of the prevalence and epidemiology of drug use in the general population of the United States. The survey is conducted on a multistage probability sample of individuals age 12 and over in all 50 states and the District of Columbia (n = 55,905). The survey covers a wide range of topics including alcohol, tobacco, and drug use, substance abuse treatment history and need for treatment, official diagnostic indicators of substance abuse and dependence, attitudes toward substance use, availability of drugs, physical and mental health, involvement in illegal activities, arrests, access to and utilization of health care services, social and family support, and school and work history. Individual responses are weighted to provide accurate population prevalence estimates. The current analysis included cases from the age 12 to 17 cohort meeting official diagnostic criteria for abuse or dependence on alcohol or illicit drugs in the past year (n = 1,649).
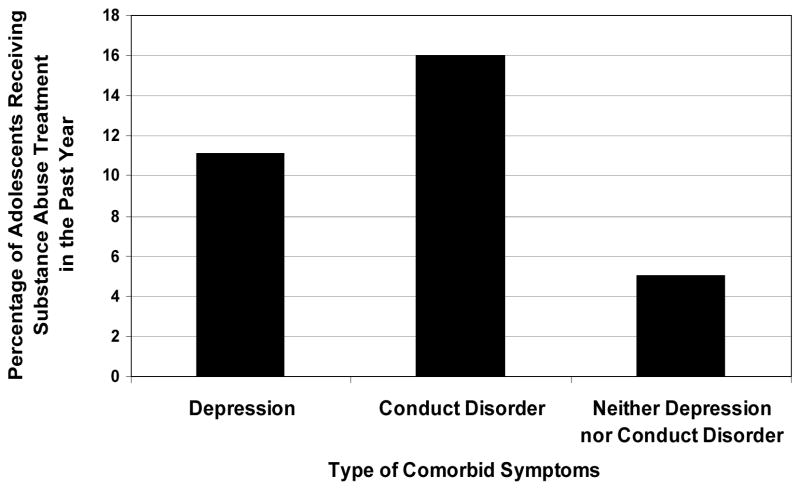
Within this sample of adolescents, the analysis examined the association between the presence of cormorbid symptoms of depression or conduct disorder over the past 12 months and the likelihood of receiving substance abuse treatment over that same period. Adolescents in the sample were classified (by the principal investigators on the NSDUH) as having exhibited depressive symptomatology if they reported experiencing a “major depressive episode” in the past year according to DSM-IV criteria. Furthermore, adolescents were classified (by the authors of this manuscript) as having exhibited symptoms of conduct disorder if they reported at least two of the following indicators over the past 12 months: (a) were involved in a serious fight at school or work, (b) were involved in a fight between two groups, (c) attacked another person with intent to cause serious harm, (d) carried a handgun, (e) sold illegal drugs, (f) stole or attempted to steal items worth at least $50, or (g) had formal legal system involvement including being arrested, on parole, or on probation. Based on these criteria, it was found that 11.3% of the sample exhibited symptoms of depression without conduct disorder, 38.7% exhibited symptoms of conduct disorder without depression, 10.9% exhibited symptoms of both depression and conduct disorder, and 39.2% exhibited neither symptoms of depression nor conduct disorder in the past year.
Chi-square tests for 2 × 2 contingency tables were used to examine the association between (a) the presence/absence of symptoms of depression and/or conduct order and (b) receiving/not receiving treatment for substance abuse in the past 12 months. As displayed in Figure 2, results indicated that adolescents with substance use disorders and comorbid depressive symptoms in the past year were over twice as likely to have received substance abuse treatment as those exhibiting neither depressive nor conduct disordered symptoms (11.1% versus 5.0%, odds ratio = 2.4, χ2 (1) = 12.7, p < .0001). Likewise, adolescents with substance use disorders and comorbid symptoms of conduct disorder were over three times as likely to have received substance abuse treatment in the past 12 months than their non-comorbid counterparts (16.0% versus 5.0%, odds ratio = 3.6, χ2 (1) = 43.3, p < .0001). These findings based on the 2005 NSDUH are consistent with (although do not definitively support) the contention that the presence of emotional or behavioral comorbidities substantially increases the likelihood that adolescents with substance use disorders will receive substance abuse treatment.
Figure 2.
Percentages of Adolescents with Substance Abuse or Dependence Receiving Substance Abuse Treatment During the Past Year by Type of Comorbid Symptoms (2005 NSDUH).
Several factors are likely to account for the potential role of comorbidity as a mechanism by which adolescents with substance use disorders may enter the treatment system. First, as alluded to previously, comorbid emotional or behavioral problems may increase the chances that adolescents with substance use disorders encounter a service system that can provide an entryway into substance abuse treatment [i.e., the so-called “no wrong door” policy].102,103 Consider, for instance, the juvenile justice system. It is known that about 40% of adolescents in substance abuse treatment are juvenile justice referrals, and over 60% have current juvenile justice involvement upon treatment entry.40,69,96,104 Evidence reviewed by Dennis et al.,73 however, suggests that most adolescents referred to substance abuse treatment by the juvenile justice system are arrested and charged with non-drug related crimes such as theft, assault, and vandalism. Relatively few are arrested solely for drug offenses. A critical implication of these findings is that only those adolescents with substance use disorders who also engage in delinquent behavior or criminal activity (besides drug use) are likely to be apprehended and subsequently referred to treatment by the juvenile justice system. Those not exhibiting such behavioral problems are relatively unlikely to enter substance abuse treatment via the juvenile justice system which is one of the most common routes into treatment for adolescents with substance use disorders.
A second factor which may help account for the link between comorbidity and the likelihood of receiving adolescent substance abuse treatment is the fact that comorbid emotional or behavioral problems may increase the detectability of adolescent substance abuse. It has been well documented that adolescents’ substance abuse problems often go undetected by “front-line” service providers in juvenile justice, primary care, mental health, education, and related social service systems.88,105–109 It is reasonable to suspect that adolescents whose substance abuse problems are most likely to go unnoticed are those without co-occurring emotional or behavioral problems which could help draw attention to existence of a substance abuse disorder. Because many social service personnel are not properly equipped to screen for adolescent substance abuse or make appropriate referrals for treatment, a great many non-cormorbid adolescents with substance use disorders manage to hover “under the radar” and elude detection and entry into the substance abuse treatment system.105–109
A third potential link between comorbidity and the likelihood of receiving adolescent substance abuse treatment has been termed in the literature as parental burden. Briefly, parental burden is conceptualized as the degree of strain and stress experienced by parents (and other family members) which is directly or indirectly imposed by the emotional and behavioral problems of their children.110–113 Such strains and stressors include disruptions of individual and family life, constraints on personal time and freedom, and financial losses. Substantial evidence in the child and adolescent mental health research literature indicates that degrees of parental burden are strong and consistent predictors of the likelihood of youth service utilization.111–113 Similar findings with regard to substance abusing adolescents are reported by Garland et al.94 Furthermore, it has been empirically demonstrated that levels of burden perceived by parents are positively associated with the number and severity of youth symptoms.110,112,115,116 Building on such findings, conceptual frameworks linking comorbidity in youth, parental burden, and service utilization have been proposed by Saya1113 and Logan and King.114 Both frameworks posit that the number and severity of youth symptoms elevate levels of parental burden which, in turn, raises parental awareness of the youth’s need for treatment. Parental recognition of child problems appears to be a key component of the help-seeking and treatment referral process.116,117
Within the context of the current discussion, the models proposed by Sayal113 and Logan and King114 suggest that parents of adolescents with substance use disorders that are unaccompanied by comorbid symptomatology may not experience inordinate levels of burden stemming from their adolescents’ substance use. Consequently, such parents may be relatively unaware of the extent or severity of their adolescents’ substance use problems and may not be sufficiently motivated to seek treatment for their adolescent. Parental motivation and ability to either persuade or compel adolescents to enter substance abuse treatment may be especially low in absence of support and leverage from an external system such as juvenile justice.
Summary
This discussion has attempted to establish the need for innovative assertive outreach strategies to direct a more substantial proportion of the population of adolescents with substance use disorders into treatment. Specifically, in addition to assertive outreach approaches based on the GPM, specialized strategies may be warranted for the subpopulation of adolescents whose substance use disorders are unaccompanied by comorbid emotional or behavioral disorders. Approximately one-third to one-half of the population of adolescents with substance use disorders may be relatively free of diagnosable cormobid conditions, which some evidence suggests may be associated with the likelihood of receiving substance abuse treatment. Specialized assertive outreach strategies may benefit this subpopulation given that such adolescents (a) are unlikely to make contact with existing service programs and systems that could provide an entryway into substance abuse treatment, (b) are relatively unlikely to have their substance use problems detected even if such contact is made, and (c) may have parents who are not fully aware of the severity of their substance use problems and who may be unmotivated or unable to persuade or compel them to enter substance abuse treatment. The remainder of this paper discusses some promising directions for developing assertive outreach strategies for this subpopulation. Specific examples of such strategies are offered. Finally, implications and recommendations for policy are considered.
Promising Assertive Outreach Strategies for Improving Rates of Adolescent Substance Abuse Treatment Utilization
In this section, several promising strategies for increasing rates of adolescent substance abuse treatment utilization are proposed and discussed. The specific strategies addressed are consistent with fundamental principles of assertive outreach including (a) proactively engaging adolescents within their natural environment, (b) comprehensive and multimodal assessment, (c) coordinating and mobilizing resources available within adolescents’ social ecology, (d) responsiveness to individual needs and circumstances, and (e) multidisciplinary and integrative service delivery. These principles are deemed to be essential ingredients of any approach toward identifying adolescents with substance use problems and engaging them in ways that facilitate their entry into substance abuse treatment. The strategies discussed in this paper are specifically designed to be effective for what may be among the most difficult-to-engage segments of the population of adolescents with substance use disorders – those without emotional or behavioral comorbidities. It should be emphasized, however, that the outreach strategies discussed further on are also likely to be effective for adolescents exhibiting substance abuse in addition to one or more comorbid emotional or behavioral disorders -- a subpopulation among whom the rate of treatment utilization is notoriously low as well.
Assertive Outreach Strategies for Identifying Adolescents in Need of Substance Abuse Treatment
The initial component of the assertive outreach approach envisioned in this paper is identification. The term identification refers to the process of detecting and making contact with adolescents with substance use disorders in order to provide information about and to advocate for their entry into substance abuse treatment. In this regard, adolescent health and prevention specialists are increasingly recognizing and capitalizing on the rich opportunities that school settings provide for identifying youth in need of services.118–124 More so than any other gateway service system for youth including the juvenile justice system, schools offer direct access to the largest segment of the clinical populations targeted by youth prevention and treatment services. As such, schools have emerged as perhaps the primary avenue through which to identify and provide services to high-risk youth including substance abusing and dependent adolescents.86,87,92,123,125
A particularly promising school-based identification strategy with potential applications for adolescent substance abuse treatment is multiple gating screening which was originally developed as a method of identifying children at high risk for delinquency. 124,126–128 Briefly, multiple gating screening encompasses a comprehensive tiered assessment protocol implemented in the school setting which gathers information from teachers, students, and their parents to identify youth who are candidates for a given type of intervention or service. The initial assessment tier is typically a broad and relatively inexpensive screen administered to teachers who are asked to identify youths exhibiting certain types of emotional or behavioral risk factors. Progressively more detailed screenings are conducted with the initial set of identified youth as well as their parents. Information collected across informants and levels of assessment is used to delineate a final pool of youth who are likely candidates for specialized services. Individual youth and their parents in the final candidate pool are recruited to participate in appropriate services as indicated across the multiple levels of assessment.
One of the most rigorous and effective implementations of school-based multiple gating screening is the Fast Track prevention program.129–132 Briefly, Fast Track is a comprehensive school- and family based prevention intervention project targeting youth at high risk for conduct disorders. The challenges of identifying high-risk youth and recruiting them and their parents into the Fast Track intervention were addressed using the following multiple gating screening approach. First, program representatives formed collaborations with school administrators (superintendents, principals, board members) and received permission to implement the screening and recruitment procedures. A published report on the multiple gating screening used in Fast Track emphasizes that in most cases school officials were quite enthusiastic and willing to offer permission for these activities in their school.130 Next, teachers within each school were asked to complete behavioral ratings of each child in their classes using a well established behavioral rating scale for teachers. Subsequently, the parents of those youth whose teacher ratings were indicative of conduct problems were contacted and asked to participate in a brief phone interview regarding their child’s behavior at home, again using an established child behavior rating scale. Finally, parents of children receiving clinically elevated ratings on both assessments were re-contacted and offered the opportunity to participate in the Fast Track intervention. The Fast Track research group reports very high rates of success using this multiple gating screening process, with approximately 91% of parents consenting to participate in the initial interview about their child, and over 96% of parents and youth participating in the prevention intervention.130
Multiple gating screening procedures such as those used in the Fast Track project might also be effective as assertive outreach strategies for identifying adolescents with substance use problems who might otherwise go undetected especially in absence of comorbid emotional or behavioral symptomatology. Screening for substance abuse is more complicated than for delinquent or aggressive behavior, arguably, given that delinquency and aggression are overtly observable whereas substance abuse tends to be more covert and is often kept hidden from parents, teachers, and other authority figures. see 133 As such, the use of “indirect” assessments may be warranted to identify adolescents exhibiting characteristics known to be risk factors for substance abuse. see 134 Such characteristics include academic problems and truancy, aggressive and delinquent behavior, depression, as well as personality traits consistent with high sensation-seeking, extroversion, and disinhibition.65,66,135–138
Various assessment tools are available which could be used as screening instruments for these types of characteristics.124,134,139 At the most brief and inexpensive level, Hallfors et al.119 have shown that student grade point average and school attendance records can be valuable in identifying adolescents who may have substance use problems. Additionally, more comprehensive brief screening instruments may be administered to teachers and parents to identify students exhibiting configurations of emotional and behavioral characteristics consistent with substance abuse or dependence. Potentially useful instruments for such screening purposes include selected subscales of the Achenbach System of Empirically Based Assessments (ASEBA), which includes teacher and parent versions of the well validated and widely utilized Achenbach Child Behavior Checklist.140 Other established teacher- and parent-report screening instruments are reviewed by Severson et al.124 and Levitt et al.139
Once a candidate pool of adolescents has been delineated based on behavioral assessments derived using teacher and parent reports (perhaps in conjunction with school records), a somewhat more direct assessment administered to adolescents regarding substance use-related attitudes, traits, and behaviors is recommended. Specifically, adolescents may be screened regarding their attitudes toward substance use, perceptions of risk associated with substance use, their level of involvement with substance using peers, and personality characteristics associated with substance use. Each of these factors has been shown to be strongly associated with substance use behavior among adolescents.65,66,141 Simple and brief items assessing youth attitudes and perceptions regarding substance use as well as association with substance using peers may be adapted from the NSDUH.33 Along similar lines, a very brief 9-item screening tool for high-risk behavior among adolescents as been developed by Jankowski et al.134 Another promising avenue toward indirect screening for adolescent substance use disorders are instruments designed to measure the “Big Five” personality dimensions (extroversion, agreeableness, conscientiousness, emotional stability, and intellect).142,143 All of the Big Five personality traits have been shown to be predictive of substance use problems in adolescents.66,137,138 John and colleagues have developed and validated a fairly brief and quick 48-item scale for assessing the Big Five in adolescent males with delinquent behavior problems.144 A very brief 10-item Big Five measurement scale has been developed by Gosling and colleagues.145
The multiple gating screening procedures outlined above are intended to yield a pool of adolescents whose behavioral, personality, cognitive, and social characteristics are consistent with known risks for substance abuse or dependence. Once this final candidate pool is delineated, the next task is to work in coordination with parents to conduct a more formal substance abuse intake assessment with the adolescent. Those adolescents remaining in the candidate pool through the prior stages of screening despite not meeting criteria for substance abuse or dependence (i.e., false positive cases) would exit the candidate pool at this stage. On the other hand, adolescents for whom the results of this final stage of screening and assessment are positive for substance abuse or dependence would progress to the next phase of assertive outreach, which is discussed in the following section of this paper.
Assertive Outreach Strategies for Enrolling Adolescents into Substance Abuse Treatment
Through the lens of the “stages of change” model,146 the identification process described above may be viewed as facilitating a shift from a state of precontemplation, characterized by little or no awareness that a problem exists and no intention to take action in the foreseeable future, to a state of contemplation in which individuals have been made aware of problems and may be considering taking action, however have made no commitment to initiate such action. The successful transition from precontemplation to contemplation is a signal for assertive outreach workers to shift their mode of activity from identification to enrollment. The term enrollment refers to an interactive process intended to address barriers toward participating in treatment, foster motivation for change, and secure a commitment to enter treatment. Within the stages of change model, the enrollment process facilitates the shift from contemplation to a state of preparation in which individuals have declared an intention to change and have begun laying the groundwork for action.
Facilitating the movement of adolescents with substance use disorders into a state of preparation for change and willingness to engage in treatment almost invariably requires parental involvement. 114,147–149 Therefore, systematic efforts to enroll a more significant proportion of the population of adolescents with substance use disorders into treatment should routinely involve parents and mobilize family resources to sway adolescents to enter treatment. Unfortunately, working with and through parents to influence adolescents to enter treatment for substance abuse is hardly a straightforward endeavor. It has been well documented that parents of adolescents with serious emotional and behavioral problems, including substance abuse, typically manifest an array of obstacles and barriers toward treatment participation, any of which can undermine the treatment entry process.110, 150–155 Such obstacles include stressors associated with the logistics of participating in treatment (e.g., scheduling conflicts, transportation difficulties, child care). Financial hardships may also discourage many parents from seeking treatment for their adolescent. Other types of barriers toward treatment entry and participation are more perceptual in nature and include (a) unawareness, minimization, or denial of the adolescent’s drug use problems, (b) viewing the adolescent’s behavior as unchangeable, or (c) relinquishing authority over the decision to seek treatment to the teen.156 Furthermore, parents with little sense of their own involvement in the adolescent’s substance use problems or of their role in helping the adolescent change may be resistant toward being involved in the treatment process. It is also typical for parents to feel excessive guilt about their adolescent’s drug problems and thus be reluctant to seek treatment for fear of being blamed. In some cases parents have a negative view of the value and legitimacy of treatment, opting in many cases for strict and/or punitive disciplinary measures. Still other parents are unmotivated to participate in treatment efforts because they have given up trying to help their adolescent after many unsuccessful attempts. (See 157 for clinical examples of these types of parental attitudes and postures). Finally, deficits in parenting skill, heightened levels of family dysfunction (e.g., violence, abuse), as well as parental psychopathology and substance abuse may pose formidable barriers to parental involvement in adolescent treatment.158
Negotiating these layers of complexity involved in working with and through parents to influence adolescents with substance use disorders to enter treatment requires well developed family-based pretreatment engagement procedures. A review by Stanton159 attests to the substantial empirical effort which has been devoted to developing and testing family-focused strategies for influencing drug involved individuals to enter treatment (e.g.,160,161). According to Stanton,159 the two most rigorously tested and well supported family-based pretreatment engagement strategies are Structural-Strategic Systems Engagement (SSSE)156, 162 and Community Reinforcement and Family Training (CRAFT).163, 164 Briefly, the crux of SSSE involves the therapist (or outreach worker, in the present case) forming a strategic alliance with one or more family members deemed to have significant power in the family system. SSSE interventions are basic family therapy techniques [e.g., joining, reframing, restructuring165] implemented in ways that capitalize on influential family members’ ability to get resistant family members to participate in treatment. Typically SSSE is administered over the phone but may also be provided in the therapist’s office, the family home, or in other settings within the family’s social environment. SSSE is intended to begin with the initial contact with the family and culminate with the initial treatment session usually 3–4 weeks after the initial contact. The efficacy of SSSE compared to “engagement as usual” for adolescents with substance use problems has been demonstrated in three randomized clinical trials. 156, 166, 167
In the overall assertive outreach strategy discussed in this paper, it is recommended to commence the enrollment phase by conducting SSSE with parents, other family members, as well as adolescents in the final candidate pool delineated during the identification phase. If SSSE does not lead to the adolescent’s enrollment in substance abuse treatment, then CRAFT should be initiated. Relative to SSSE, CRAFT is a more intensive 12-session intervention program originally designed to engage resistant adult drug users into treatment by working directly with a “concerned significant other” (CSO) which is usually a spouse or parent. Fundamentally, CRAFT is a behavioral family therapy intervention conducted with one or more CSOs of treatment-refusing individuals with substance use disorders, where the primary objective is to persuade such individuals to enter treatment. The core components of CRAFT include: (a) education regarding the consequences of substance abuse and benefits of treatment, (b) contingency management training for the CSO to reinforce non-drug using behavior and to discourage drug use, (c) social skills training to improve interpersonal communication and problem-solving, (d) planning and practicing activities to interfere with the target person’s drug use, and (e) encouraging and reinforcing participation in drug abuse treatment.
A version of CRAFT for adolescents with substance use disorders who refuse to enter treatment has been developed and tested by Waldron and colleagues.168 Briefly, Waldron et al.’s CRAFT approach is implemented with parents of adolescents with substance use disorders who refuse to enter treatment despite parents’ and others’ best efforts to get them to do so. The CRAFT model for treatment-refusing adolescents is specially tailored to address the developmental needs of adolescents and focuses on the roles that parents typically play in adolescents’ involvement in as well as recovery from substance use disorders. In particular, the contingency management and communication training components of CRAFT are designed around the unique aspects of the parent-adolescent relationship as opposed to that between adult drug abusers and their parents or spouses. Waldron et al.168 reported the findings of a small-scale treatment development study (n = 42) of the CRAFT intervention for adolescents. The results of this investigation indicated that CRAFT can be feasibly and successfully implemented with parents of adolescents with substance use disorders. Furthermore, 70% of the initially treatment-refusing adolescent sample was enrolled in treatment following CRAFT.
Further development and testing is warranted of both SSSE and CRAFT as strategies for enrolling adolescents with substance use disorders into treatment. Both interventions have received encouraging empirical support and are promising means of addressing the pervasively low rate of adolescent substance abuse treatment utilization. Significant reductions in the adolescent substance abuse treatment gap appear unlikely without widespread dissemination of effective enrollment interventions such as SSSE and CRAFT, which are tailored to fit the unique developmental needs and contextual circumstances of adolescents with substance use disorders.
Implications for Behavioral Health
Existing clinical services cannot yield appreciable public health benefits if the majority of the target population does not utilize them. This reality characterizes the current state of affairs regarding the adolescent substance abuse treatment system in the United States. This is also the most likely future of the adolescent substance abuse treatment system unless much more concerted and widespread efforts are made to identify adolescents with substance use problems and enroll them into treatment. This paper has outlined a general assertive outreach approach and some specific outreach strategies that could be effective in this regard. Widespread implementation of the types of assertive outreach efforts discussed in this paper would require substantial organizational and financial support from federal, state, and local agencies charged with reducing the prevalence of adolescent substance abuse. In particular, new types of behavioral health policies would be needed to provide the directives, incentives, and the resources (including adequate staffing and personnel)b for assertive outreach among adolescents with substance use disorders.107 This paper concludes with a discussion of some of the substantive, ethical, and financial considerations surrounding policy changes needed to undergird the assertive outreach innovations outlined in this paper.
New Directions for Policy
Current policies intended to diminish the adolescent substance abuse treatment gap are favorably disposed toward mandatory drug testing in schools and compulsory substance abuse treatment for adolescents.45,107,169,170 Concerns with such policies abound, however, as one might suspect. First, mandatory drug testing of high school students is highly controversial and has received great opposition on legal and ethical grounds.171,172 A clear illustration of such opposition is a recent nationally representative survey of physicians revealing strong and widespread disapproval of federal policy initiatives to implement uniform drug testing of high school students.173 Second, there is virtually no compelling empirical support for the effectiveness of mandatory drug testing in schools on rates of substance use among students within schools implementing such policies and practices.171,172,174–176 In fact, some evidence suggests that mandatory drug testing of high school students may actually have iatrogenic effects on a number of attitudinal and perceptual risk factors risk associated with adolescent drug use.176 A third concern with such policies is that adolescents who are coerced or mandated to enter treatment are typically less motivated and more resistant toward clinical intervention than those entering treatment (at least partially) under their own volition.76,147 In turn, it is well established that adolescents entering treatment with high levels of resistance are less likely to complete or to benefit from treatment compared to those who are relatively less resistant toward treatment.177–180
A more promising policy direction may be to foster substance abusing or dependent adolescents’ motivation to enter treatment by cultivating and mobilizing sources of support within their social and community networks.171, see also 181 A prime example of this type of policy-driven initiative is the NIDA Community-Based Outreach Model to reduce and prevent the contraction and transmission of HIV among out-of-treatment intravenous drug users and their sexual partners.60,61 Briefly, the NIDA outreach model is designed to access large segments of the difficult-to-engage population of intravenous drug users using teams of indigenous assertive outreach workers who are trained to identify and make contact with such individuals in their natural social settings. Once identified and contacted, the outreach workers provide educational support and attempt to enlist participation in a brief preventative intervention. With support from NIDA, the outreach model has been implemented and evaluated on a widespread scale in communities across the United States and abroad. The model has been found to be effective for adults from a multitude of racial, ethnic, gender, socioeconomic, and geographic backgrounds manifesting varying types and levels of drug use and co-occurring disorders as well as risk for HIV.61,182,183
Ethical Concerns
As discussed earlier on, the components of the assertive outreach approach advocated in this paper, namely, (a) school-based multiple gating screening and identification and (b) family-based pre-treatment engagement and enrollment, are well developed and established practices with solid bases of empirical support among populations of at-risk children and adolescents. A vital consideration, nevertheless, is whether implementing such practices among adolescents with substance use disorders poses ethical risks, especially given the vulnerabilities of this population to violations of basic rights and civil liberties. Concerns and lively debates over the ethics of assertive outreach as a general practice have been prominent in the mental health literature for nearly a decade.56,184–187 Although these arguments will not fully be reiterated here, it is prudent to address two ethical concerns of particular salience for the targeted population of adolescents with substance use disorders, which is characterized as being “difficult to engage” not due to the multiplicity and severity of emotional and behavioral problems, per se, but rather an absence of comorbid symptomatology which could raise the attention of caregivers and frontline service providers and catalyze the treatment referral process. These ethical issues are coerciveness and confidentiality.
Coerciveness
The assertive outreach approach discussed in this paper may raise concerns that a proportion of adolescents exposed to such measures could be unjustly manipulated or forced to receive treatment. Such concerns may be especially pronounced with regard to adolescents with substance use disorders who have not been convicted of any crime and who may otherwise maintain relatively adaptive levels of functioning. It may be reasoned that assertive outreach efforts carry a risk of violating such adolescents’ rights to refuse treatment so long as their behavior poses no threat of acute harm to themselves or others.
A full discussion of adolescents’ capacities and legal rights to consent to or refuse treatment, and the implications of such for assertive outreach, is beyond the scope of this paper (see 188 for a review of such issues). It should be made clear, however, that under no circumstances are the engagement and enrollment strategies discussed in this paper (SSSE and CRAFT) intended or designed to be used in ways that infringe upon adolescents’ rights. In fact, it is counter to the clinical underpinnings and objectives of both SSSE and CRAFT that adolescents should end up feeling forcibly manipulated to enter treatment. On the contrary, both SSSE and CRAFT are designed to enhance adolescents’ willingness and motivation to enter treatment under their own volition by marshalling and mobilizing sources of support within the family, school, and other systems of care. It is well known that family members can serve as powerful sources of motivation for individuals with drug use problems to enter treatment, and the involvement of family members in this regard has become a standard practice in the substance abuse treatment field.159–164,189 With regard to adolescents in need of treatment, evidence suggests that increasing parents’ awareness of adolescent problem severity and the need for treatment has a positive impact on adolescents’ own problem recognition, motivation for change, and the likelihood of entering treatment.76,114–117,147,190–191
It is difficult to imagine, quite frankly, a more restrictive and coercive system for identifying and referring adolescents with substance use problems into treatment than that which is currently in place. Under the status quo, the majority adolescents receiving substance abuse treatment are legally mandated or otherwise coerced to enter treatment involuntarily.69,77,96,147 The assertive outreach strategies discussed in this paper are meant to reduce rather than exacerbate prevailing degrees of coerciveness inherent within the adolescent substance abuse treatment system. In fact, studies among adult populations indicate that assertive outreach is viewed favorably among service recipients, and has been shown to reduce perceptions of coerciveness as well as the use of restrictive rehabilitation services such as in-patient hospitalization.184,185 It seems likely that employing developmentally appropriate assertive outreach strategies for adolescents with substance use disorders would have similar favorable effects on both the perception and actual use of coercion as a means of service delivery within this population.
Confidentiality
In their review of emerging school-based screening methods and practices, Levitt and colleagues139 emphasize the preservation of student confidentiality as an utmost priority (pp. 183–184). Accordingly, Levitt et al.139 recommend that school personnel collaborate with outreach workers from the mental health system to develop comprehensive plans and procedures for protecting the confidentiality of all students. In accordance with Levitt et al.’s139 assertions, the authors of this paper propose a number of measures to help safeguard student confidentiality throughout the assertive outreach process. First, any screening activities involving student attendance and academic records should be conducted by personnel with authorized access to such records and who have provided signed written agreements to uphold confidentiality. Second, teachers should be informed and trained on the importance of maintaining confidentiality throughout the process of rating individual students, and should provide signed written confidentiality agreements as well. Third, with regard to assessments of “indirect” substance abuse risk factors (e.g., personality characteristics and attitudes toward substance use) administered to students themselves, it is recommended that all students in a given classroom, grade, or school be included in such assessments rather than only the subset of students in the candidate pool (along the lines of a universal student-wide screening survey). see 139 Although responses from only those students in the candidate pool would need to be screened, administering such assessments to all students avoids having the subset of students in the candidate pool identified as such were they to be the only ones being assessed. All students should be assured that the information they provide is strictly private, and students’ names should not appear anywhere on the assessment forms. Instead, individual assessment forms can be marked with a unique and confidential student ID number. Alternatively, in lieu of an ID number, the assessment forms of particular students in the candidate pool can be identified by cross-matching sets of characteristics which students would be asked to provide on their assessment forms such as gender, grade, date of birth, zip code, etc., as well as their home classroom and teacher. A final recommendation is that formal substance use assessments with students (and parents) remaining in the candidate pool until the final stage of screening occur off school grounds and be conducted by clinical personnel not directly affiliated with the school system. Such clinical personnel generally are well trained regarding the practice of maintaining client confidentiality.
Cost Considerations
A notable caveat regarding the discussion to this point is an obfuscation of the potential costs of implementing on a grand scale the assertive outreach practices and policies proposed herein. Although no precise cost estimates are available for such procedures, suffice it to say that these outreach activities would add substantially to the overall costs of providing substance abuse treatment to adolescents. These cost increases, however, should be considered in the context of other costs which have been and continue to be incurred in the effort to curtail the prevalence of adolescent substance abuse and dependence. Among these costs, as mentioned previously, is the massive expenditure of resources over the past decade and beyond on the development, testing, and dissemination of empirically supported and effective treatments for adolescent substance abuse. Cost-benefit analyses indicate that such treatments appear to be prudent investments in that each dollar spent on treatment yields a considerable rate of return on average by reducing the likelihood of costly long-term outcomes associated with substance abuse among adolescents including arrest and incarceration, hospitalization, admission to in-patient or residential clinical facilities, and other expensive out-of-home placements.192,193 The economic benefits of reducing such outcomes are of considerable appeal to policy makers and administrators charged with addressing substance abuse problems among the adolescent population.42,47,194 Unfortunately, such potential fiscal returns seem unlikely to be realized given the well documented adolescent substance abuse treatment gap discussed earlier in this paper. The types of assertive outreach strategies detailed in this paper could be well worth the investment if their implementation results in a substantial increase in the number of substance abusing adolescents who receive treatment and, in turn, a marked decrease in the utilization of more costly types of out-of-home placements such as those discussed above. Under current and prevailing conditions, not only do such potential economic benefits stand to go by the wayside, but the incalculable sum of money and other resources invested over the last decade on adolescent substance abuse treatment research could be largely for naught as well.c
In addition to the types of relatively short-term economic benefits discussed above (i.e., 6 months to 2 years post-treatment), the assertive outreach strategies described in this paper could yield substantial long-term economic benefits over a period spanning several decades beyond the termination of treatment. Specifically, numerous cost studies have estimated that the cumulative costs to society stemming from substance use across all age groups in the United States amount to approximately one half of a trillion dollars annually.53,195 This staggering estimate encompasses costs stemming from lost productivity due to substance abuse, health care expenditures for conditions related to substance abuse, expenses associated with drug- and alcohol-related accidents and crimes, etc.196 Although there are no concrete estimates of the proportion of these annual costs attributable specifically to the substance use problems of adolescents, admittedly this proportion is likely to be relatively low. However, the assertive outreach strategies highlighted in this paper have the potential to produce substantial long-term reductions in these overall costs to society by lowering the proportion of adolescents with substance abuse or dependence that go untreated and (with great likelihood) progress to more chronic stages of substance dependence or addiction during young adulthood and beyond. Consistent with this argument, a cost analysis by Cohen197 projects that the economic value of preventing or “saving” adolescents with substance use disorders from becoming addicted during adulthood is between $1.7 million and $2.3 million (in 1998 dollars) over the life of each saved addicted person. In light of these figures, even a modest long-term preventative effect of the assertive outreach strategies proposed in this paper on the number of adolescents who eventually become addicted to substances as adults would more than offset the marginal costs of incorporating such outreach procedures into existing adolescent substance abuse treatment services programs.
Summary
The widespread and systematic adoption of school-based screening procedures to identify and engage youth at risk for (or already exhibiting) emotional and behavioral disorders is rapidly gaining popularity across sectors of child and adolescent mental health research, practice, and policy, and is routinely recommended as a means of fortifying current prevention and treatment infrastructures.14,107,198–200 Against this backdrop, this article has attempted to make the case for developing specialized school- and family-based assertive outreach strategies to identify and enroll a more substantial proportion of the substance abusing or dependent adolescent population into treatment. The implications and recommendations for practice and policy proposed in this paper are in keeping with overarching ecological frameworks for child and adolescent clinical services. 67,92,201–205 While the bulk of contemporary ecologically focused clinical literature focuses on intervention design and implementation, the critical “pre-intervention” processes of identification and enrollment deserve fuller consideration. In fact, assertive outreach strategies for identification and enrollment should be regarded as components of the overall treatment process for adolescent substance abuse, and as such should be developed and evaluated with the same rigor as any other intervention component. Moreover, linkages between the processes and outcomes of identification, enrollment, and intervention should be conceptualized and evaluated within an ecological empirical framework.206 Ultimately, the integrative development, testing, and dissemination of effective identification, enrollment, and intervention procedures is essential for enhancing the public health impact of the adolescent substance abuse treatment system.
Acknowledgments
Support for this manuscript was provided by grants from the National Institute on Drug Abuse to Holly B. Waldron, Ph.D. (1R01DA15762, 5R01DA017023).
Footnotes
A prime example of a systematic and cutting edge GPM-based approach to assertive outreach for individuals with substance abuse problems is the Screening, Brief Intervention, Referral, and Treatment (SBIRT) cooperative agreement initiated in 2003 by the Substance Abuse and Mental Health Services Administration (SAMHSA) (see http://www.samhsa.gov/Matrix/programs_treatment_SBIRT.aspx). Briefly, the SBIRT cooperative agreement initiative is a five-year $108 million program to support comprehensive substance use screening for individuals receiving health care services in a range of settings including hospitals, general medical clinics, emergency rooms, urgent care centers, and so forth.194 The screening is conducted by a specially trained medical professional. If a substance use problem is detected, the screener is equipped to provide a brief informational and motivational intervention on the spot, as well as to provide a referral for more comprehensive substance abuse treatment services as needed. Preliminary results regarding the impact of the SBIRT protocol on substance use among medical patients are somewhat positive, although uncertainties have been expressed pertaining to the dissemination and adoption of SBIRT among front-line service providers.207
Although concrete guidelines for personnel and staffing of the outreach activities discussed in this paper remain to be developed, the authors’ position that the majority of the effort and burden should be shouldered by specially trained outreach workers from the substance abuse treatment system. The authors are not in favor of imposing additional layers of burden and responsibility upon teachers or other staff members within the school system.
It should be noted that these relatively short-term cost benefits would be realized if the assertive outreach procedures discussed in this paper were successful in directing a larger proportion of the relatively more chronic and comorbid segments of the adolescent substance abusing population into treatment. Undoubtedly, the majority of the short-term costs of untreated substance abuse (e.g., drug-related crimes, arrests, incarcerations, probation, etc) are attributable to this more severely impaired group of adolescents. In contrast, it is expected that substantial cost benefits from implementing assertive outreach among relatively less chronic and non-comorbid adolescents with substance use disorders may be realized over a much longer time period extending into the young adult years of such adolescents and beyond. Such long-term preventative cost benefits are discussed in the following paragraph.
Reference List
- 1.Dennis M. The Current Renaissance of Adolescent Treatment [Online]. Paper presented at the Project Fresh Light Partnership Meeting; Madison, WI. [Accessed October 30, 2007]. Available at http://www.chestnut.org/LI/Posters/1-The_Current_Renaissance_of_Adolescent_Treatment_4-17-06.pps. [Google Scholar]
- 2.Liddle HA. Connection: A Newsletter Linking the Users and Producers of Drug Abuse Services Research. Washington, DC: Academy for Health Services Research and Health Policy; May, 2002. The research renaissance in adolescent substance abuse treatment; pp. 4–5. [Google Scholar]
- 3.Liddle HA, Rowe CL. Adolescent Substance abuse: Research and Clinical Advances. New York: Cambridge University Press; 2006. [Google Scholar]
- 4.Wagner EF, Waldron HB, editors. Innovations in Adolescent Substance Abuse Interventions. New York: Pergamon; 2001. [PubMed] [Google Scholar]
- 5.Waldron HB, Turner CW. Psychosocial treatments for adolescent substance abuse: A review and meta-analyses. Journal of Clinical Child and Adolescent Psychology. 2008;37:1–24. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- 6.Williams RJ, Chang SY. A comprehensive and comparative review of adolescent substance abuse treatment outcomes. Clinical Psychology: Science and Practice. 2000;7(2):138–66. [Google Scholar]
- 7.Kzdin AE, Weisz JR, editors. Evidence-Based Psychotherapies for Children and Adolescents. New York: The Guilford Press; 2003. [Google Scholar]
- 8.Weisz JR. Psychotherapy for Children and Adolescents: Evidence-Based Treatments and Case Examples. New York: Cambridge University Press; 2004. [Google Scholar]
- 9.Center for Substance Abuse Treatment. Treatment of Adolescents with Substance Use Disorders. Rockville, MD: United States Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment; 1999. DHHS Publication No. 99–3345. [PubMed] [Google Scholar]
- 10.Commission on Adolescent Substance and Alcohol Use. Treatment of substance use disorders. In: Evans DL, Foa EB, Gur RE, et al., editors. Treating and Preventing Adolescent Mental Health Disorders: What We Know and Don’t Know. A Research Agenda for Improving the Mental Health of Our Youth. New York: Oxford University Press; 2005. pp. 391–410. [Google Scholar]
- 11.Drug Strategies. Treating Teens: A Guide to Adolescent Drug Programs. Washington, DC: Drug Strategies; 2003. [Google Scholar]
- 12.National Institute on Drug Abuse. Principles of Drug Addiction Treatment: A Research-based Guide. Rockville, MD: National Institutes of Health; 1999. DHHS Publication No. 99–4180. [Google Scholar]
- 13.American Academy of Child and Adolescent Psychiatry. Practice parameters for assessment and treatment of children and adolescents with substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(Supplement):140S–156S. doi: 10.1097/00004583-199710001-00009. [DOI] [PubMed] [Google Scholar]
- 14.American Academy of Child and Adolescent Psychiatry. Practice parameters for assessment and treatment of children and adolescents with substance use disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:609–621. doi: 10.1097/01.chi.0000159135.33706.37. [DOI] [PubMed] [Google Scholar]
- 15.Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27(3):197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Morral AR, McCaffrey DF, Ridgeway G, et al. The Relative Effectiveness of 10 Adolescent Substance Abuse Programs in the United States. Santa Monica, CA: RAND Corporation; 2006. Report No. 326. [Google Scholar]
- 17.Henggeler SW, Melton GB, Brondino MJ, et al. Multisystemic Therapy with violent and chronic juvenile offenders and their families: The role of treatment fidelity in successful dissemination. Journal of Consulting and Clinical Psychology. 1997;65(5):821–833. doi: 10.1037//0022-006x.65.5.821. [DOI] [PubMed] [Google Scholar]
- 18.Henggeler SW, Pickrel SG, Brondino MJ. Multisystemic treatment of substance abusing and dependent delinquents: Outcomes, treatment fidelity, and transportability. Mental Health Services Research. 1999;1:171–184. doi: 10.1023/a:1022373813261. [DOI] [PubMed] [Google Scholar]
- 19.Liddle HA, Rowe CL, Quille TJ, et al. Transporting a research-based adolescent drug treatment into practice. Journal of Substance Abuse Treatment. 2002;22(4):231–243. doi: 10.1016/s0740-5472(02)00239-8. [DOI] [PubMed] [Google Scholar]
- 20.Washington State Institute for Public Policy. Outcome Evaluation of Washington State’s Research-Based Programs for Juvenile Offenders. Retrieved November 10, 2006, from http://www.wsipp.wa.gov/pub.asp?docid=04-01-1201.
- 21.Timmons-Mitchell J, Bender MB, Kishna MA, et al. An independent effectiveness trial of Multisystemic Therapy with juvenile justice youth. Journal of Clinical Child and Adolescent Psychology. 2006;35:227–236. doi: 10.1207/s15374424jccp3502_6. [DOI] [PubMed] [Google Scholar]
- 22.Gotham HJ. Diffusion of mental health and substance abuse treatments: Development dissemination, and implementation. Clinical Psychology: Science and Practice. 2004;11(2):161–76. [Google Scholar]
- 23.Henggeler SW, Schoenwald SK, Liao JG, et al. Transporting efficacious treatments to field settings: The link between supervisory practices and therapist fidelity in MST programs. Journal of Clinical Child and Adolescent Psychology. 2002;31(2):155–67. doi: 10.1207/S15374424JCCP3102_02. [DOI] [PubMed] [Google Scholar]
- 24.Miller WR, Sorensen JL, Selzer JA, et al. Disseminating evidence-based practices in substance abuse treatment: A review with suggestions. Journal of Substance Abuse Treatment. 2006;31(1):25–39. doi: 10.1016/j.jsat.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Robbins MS, Bachrach K, Szapocznik J. Bridging the research-practice gap in adolescent substance abuse treatment: The case of brief strategic family therapy. Journal of Substance Abuse Treatment. 2002;23(2):123–32. doi: 10.1016/s0740-5472(02)00265-9. [DOI] [PubMed] [Google Scholar]
- 26.Schoenwald SK, Sheidow AJ, Letourneau EJ. Toward effective quality assurance in evidence-based practice: Links between expert consultation, therapist Fidelity, and child outcomes. Journal of Clinical Child and Adolescent Psychology. 2004;33(1):94–104. doi: 10.1207/S15374424JCCP3301_10. [DOI] [PubMed] [Google Scholar]
- 27.Schoenwald SK, Sheidow AJ, Letourneau EJ, et al. Transportability of Multisystemic Therapy: Evidence for multilevel influences. Mental Health Services Research. 2003;5(4):223–239. doi: 10.1023/a:1026229102151. [DOI] [PubMed] [Google Scholar]
- 28.Simpson DD. A conceptual framework for transferring research to practice. Journal of Substance Abuse Treatment. 2002;22(4):171–82. doi: 10.1016/s0740-5472(02)00231-3. [DOI] [PubMed] [Google Scholar]
- 29.Liddle HA, Rowe CL, Gonzalez A, et al. Changing provider practices, program environment, and improving outcomes by transporting Multidimensional Family Therapy to an adolescent drug treatment setting. The American Journal on Addictions. 2006;15:102–112. doi: 10.1080/10550490601003698. [DOI] [PubMed] [Google Scholar]
- 30.Biglan A. Translating what we know about the context of antisocial behavior into a lower pervalence of such behavior. Journal of Applied Behavior Analysis. 1995;28:479–492. doi: 10.1901/jaba.1995.28-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schoenwald SK, Henggeler SW. A public health perspective on the transport of evidence-based practices. Clinical Psychology: Science and Practice. 2004;11(4):360–363. [Google Scholar]
- 32.Spoth RL, Kavanaugh KA, Dishion TJ. Family-centered preventive intervention science: Toward benefits to larger populations of children, youth, and families. Prevention Science. 2002;3(3):145–152. doi: 10.1023/a:1019924615322. [DOI] [PubMed] [Google Scholar]
- 33.Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: Office of Applied Studies; 2006. DHHS Pub. No. (SMA)06-4194. [Google Scholar]
- 34.Duncan SC, Alpert A, Duncan TE, et al. Adolescent alcohol use development and young adult outcomes. Drug and Alcohol Dependence. 1997;49(1):39–48. doi: 10.1016/s0376-8716(97)00137-3. [DOI] [PubMed] [Google Scholar]
- 35.Oesterle S, Hill KG, Hawkins JD, et al. Adolescent heavy episodic drinking trajectories and health in young adulthood. Journal of Studies on Alcohol. 2004;65:204–212. doi: 10.15288/jsa.2004.65.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Newcomb MD, Scheier LM, Bentler PM. Effects of adolescent drug use on adult mental health: A prospective study of a community sample. Experimental and Clinical Psychopharmacology. 1993;1:215–241. [Google Scholar]
- 37.Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescents from harm: Findings from the National Longitudinal Study on Adolescent Health. JAMA: Journal of the American Medical Association. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 38.Rohde P, Lewinsohn PM, Seeley JR, et al. Psychosocial functioning of adults who experienced substance use disorders as adolescents. Psychology of Addictive Behaviors. 2007;21(2):155–164. doi: 10.1037/0893-164X.21.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Trim RS, Meehan BT, King KM, et al. The Relation between adolescent substance use and young adult internalizing symptoms: Findings from a high-risk longitudinal sample. Psychology of Addictive Behaviors. 2007;21(1):97–107. doi: 10.1037/0893-164X.21.1.97. [DOI] [PubMed] [Google Scholar]
- 40.Dennis ML, Dawud-Noursi S, Muck RD, et al. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent Substance Abuse Treatment in the United States: Exemplary Models from a National Evaluation Study. New York: The Haworth Press; 2003. pp. 3–34. [Google Scholar]
- 41.Patton GC, Coffey C, Lynskey MT, et al. Trajectories of adolescent alcohol and cannabis use into young adulthood. Addiction. 2007;102(4):607–615. doi: 10.1111/j.1360-0443.2006.01728.x. [DOI] [PubMed] [Google Scholar]
- 42.French MT, Maclean JC. Underage alcohol use, delinquency, and criminal activity. Health Economics. 2006;15(12):1261–1281. doi: 10.1002/hec.1126. [DOI] [PubMed] [Google Scholar]
- 43.French MT, McCollister KE, Kebreau A, et al. Revolving roles in drug-related crime: The cost of chronic drug users as victims and perpetrators. Journal of Quantitative Criminology. 2004;20(3):217–241. [Google Scholar]
- 44.Irwin CEJ, Burg SJ, Cart CU. America’s adolescents: Where have we been, where are we going? Journal of Adolescent Health. 2002;31(Suppl6):91–121. doi: 10.1016/s1054-139x(02)00489-5. [DOI] [PubMed] [Google Scholar]
- 45.Office of the National Drug Control Policy. What you need to know about starting a student drug-testing program. Washington, D.C.: U.S. Government Printing Office; 2004. [Google Scholar]
- 46.Miller TR, Levy DT, Spicer RS, et al. Societal costs of underage drinking. Journal of Studies on Alcohol. 2006;67(4):519–528. doi: 10.15288/jsa.2006.67.519. [DOI] [PubMed] [Google Scholar]
- 47.Flanzer JP. Health services with drug-abusing adolescents: The next frontier of research. In: Liddle HA, Rowe CL, editors. Adolescent Substance Abuse: Research and Clinical Advances. New York: Cambridge University Press; 2006. pp. 204–219. [Google Scholar]
- 48.Office of Applied Studies. Substance abuse treatment need among adolescents: 2003–2004. Rockville, MD: Office of Applied Studies, Substance Use and Mental Health Services Administration; 2006. [Google Scholar]
- 49.Perl HI. Implementation and adoption of evidence-based practices: What do we know today and what will we need to do tomorrow?. Paper presented at the annual Joint Meeting on Adolescent Treatment Effectiveness; Baltimore, MD. March 27, 2006. [Google Scholar]
- 50.Glasgow RE. Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health. 2003;93(8):1261–1267. doi: 10.2105/ajph.93.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Compton WM, Stein JB, Robertson EB, et al. Charting a course for health services research at the National Institute on Drug Abuse. Journal of Substance Abuse Treatment. 2005;29(3):167–172. doi: 10.1016/j.jsat.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Institute on Drug Abuse. Report of the Blue Ribbon Task Force on Health Services Research at the National Institute on Drug Abuse. Rockville, MD: National Institutes of Health; 2004. [Google Scholar]
- 53.National Institute on Drug Abuse. Health services research on the prevention and treatment of drug and alcohol abuse. PA-05-139. Rockville, MD: National Institutes of Health; 2005. [Google Scholar]
- 54.National Institute on Drug Abuse. Health services research on practice improvement utilizing community treatment programs within the National Institute on Drug Abuse Clinical Trials Network. PA-06-495. Rockville, MD: National Institutes of Health; 2006. [Google Scholar]
- 55.Burns T, Firn M. Assertive Outreach in Mental Health: A Manual for Practitioners. New York: Oxford University Press; 2002. [Google Scholar]
- 56.Ryan P, Morgan S. Assertive Outreach: A Strengths Approach to Policy and Practice. New York: Churchill Livingstone; 2004. [Google Scholar]
- 57.Stein LI, Santos AB. Assertive Community Treatment of Persons with Severe Mental Illness. New York: W.W. Norton & Company; 1998. [Google Scholar]
- 58.Meisler N, Santos AB. From the hospital to the community: The great american paradigm shift. In: Henggeler SW, Santos AB, editors. Innovative Approaches for Difficult-to-Treat Populations. Washington, DC: American Psychiatric Press, Inc.; 1997. pp. 167–90. [Google Scholar]
- 59.Fisk D, Rakfeldt J, McCormack E. Assertive outreach: An effective strategy for engaging homeless persons with substance use disorders into treatment. American Journal of Drug and Alcohol Abuse. 2006;32(3):479–486. doi: 10.1080/00952990600754006. [DOI] [PubMed] [Google Scholar]
- 60.Himmelgreen DA, Singer M. HIV, AIDS, and other health risks: Findings from a multisite study--an introduction. American Journal of Drug and Alcohol Abuse. 1998;24(2):187–97. doi: 10.3109/00952999809001708. [DOI] [PubMed] [Google Scholar]
- 61.National Institute on Drug Abuse. The NIDA community-based outreach model: A manual to reduce the risk of HIV and other blood-borne infections in drug users. Rockville, MD: National Institutes of Health; 2000. NIH Publication No. 00-4812. [Google Scholar]
- 62.Rowe M, Fisk D, Frey J, et al. Engaging persons with substance use disorders: Lessons from homeless outreach. Administration and Policy in Mental Health. 2002;29(3):263–73. doi: 10.1023/a:1015147710813. [DOI] [PubMed] [Google Scholar]
- 63.White MK, Godley SH, Passetti LL. Adolescent and parent perceptions of outpatient substance abuse treatment: A qualitative study. Journal of Psychoactive Drugs. 2004;36(1):65–74. doi: 10.1080/02791072.2004.10399724. [DOI] [PubMed] [Google Scholar]
- 64.Dishion TJ, Reid JB, Patterson GR. Empirical guidelines for a family intervention for adolescent drug use. Journal of Chemical Dependency Treatment. 1988;1(2):189–224. [Google Scholar]
- 65.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychological Bulletin. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 66.Petratis J, Flay BR, Miller TQ, Torpy EJ, Geriner B. Illicit substance use among adolescents: A matrix of prospective predictors. Substance Use and Misuse. 1998;33:2561–604. doi: 10.3109/10826089809059341. [DOI] [PubMed] [Google Scholar]
- 67.Szapocznik J, Coatsworth JD. An ecodevelopmental framework for organizing the influences on drug abuse: A developmental model of risk and protection. In: Glantz MD, Hartel CR, editors. Drug Abuse: Origins and Interventions. Washington DC: American Psychological Association; 1999. pp. 331–366. [Google Scholar]
- 68.Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology. 2002;70(6):1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- 69.Grella C. The Drug Abuse Treatment Outcomes Studies: Outcomes with adolescent substance abusers. In: Liddle HA, Rowe CL, editors. Adolescent Substance Abuse: Research and Clinical Advances. New York: Cambridge University Press; 2006. pp. 148–173. [Google Scholar]
- 70.Tims FM, Dennis ML, Hamilton N, et al. Characteristics and problems of 600 adolescent cannabis abusers in outpatient treatment. Addiction. 2002;97(Suppl 1):46–57. doi: 10.1046/j.1360-0443.97.s01.7.x. [DOI] [PubMed] [Google Scholar]
- 71.Turner WC, Muck RD, Muck RJ, et al. Co-occurring disorders in the adolescent mental health and substance abuse treatment systems. Journal of Psychoactive Drugs. 2004;36:455–462. doi: 10.1080/02791072.2004.10524428. [DOI] [PubMed] [Google Scholar]
- 72.Weinberg NZ, Rahdert E, Colliver JD, et al. Adolescent substance abuse: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(3):252–261. doi: 10.1097/00004583-199803000-00009. [DOI] [PubMed] [Google Scholar]
- 73.Dennis M, Babor RF, Roebuck C, et al. Changing the focus: The case for recognizing and treating cannabis use disorders. Addiction. 2002;97(Suppl1):4–15. doi: 10.1046/j.1360-0443.97.s01.10.x. [DOI] [PubMed] [Google Scholar]
- 74.Kinlock TW, Gordon MS, Battjes RJ. Pretreatment illegal activities of a nationwide sample of adolescent substance abuse clients. Journal of Psychoactive Drugs. 2004;36(1):5–12. doi: 10.1080/02791072.2004.10399719. [DOI] [PubMed] [Google Scholar]
- 75.Rounds-Bryant JL, Kristiansen PL, Hubbard RL. Drug abuse treatment outcome study of adolescents: A comparison of client characteristics and pretreatment behaviors in three treatment modalities. American Journal of Drug and Alcohol Abuse. 1999;25(4):573–591. doi: 10.1081/ada-100101880. [DOI] [PubMed] [Google Scholar]
- 76.Battjes RJ, Gordon MS, O’Grady KE, et al. Factors that predict adolescent motivation for substance abuse treatment. Journal of Substance Abuse Treatment. 2003;24(3):221–232. doi: 10.1016/s0740-5472(03)00022-9. [DOI] [PubMed] [Google Scholar]
- 77.Breda C, Heflinger CA. Predicting incentives to change among adolescents with substance abuse disorder. American Journal of Drug and Alcohol Abuse. 2004;30:251–267. doi: 10.1081/ada-120037377. [DOI] [PubMed] [Google Scholar]
- 78.Henggeler SW, Schoenwald SK, Bourdin CM, et al. Multisystemic Treatment of Antisocial Behavior in Children and Adolescents. New York: The Guilford Press; 1998. [Google Scholar]
- 79.Henggeler SW, Schoenwald SK, Rowland MD, et al. Serious Emotional Disturbance in Children and Adolescents: Multisystemic Therapy. New York: The Guildford Press; 2002. [Google Scholar]
- 80.Stiffman AR, Pescolsolido B, Cabassa LJ. Building a model to understand youth service access: The gateway provider model. Mental Health Services Research. 2004;6(4):189–198. doi: 10.1023/b:mhsr.0000044745.09952.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nissen LB, Hunt SR, Bullman S, et al. Systems of care for treatment of adolescent substance use disorders: Background, principles and opportunities. Journal of Psychoactive Drugs. 2004;36:429–438. doi: 10.1080/02791072.2004.10524426. [DOI] [PubMed] [Google Scholar]
- 82.Stiffman AR, Hadley-Ives E, Dore P, et al. Youths’ access to mental health services: The role of providers’ training, resource connectivity and assessment of need. Mental Health Services Research. 2000;2(3):141–54. doi: 10.1023/a:1010189710028. [DOI] [PubMed] [Google Scholar]
- 83.Belenko S, Logan TK. Delivering more effective treatment to adolescents: Improving the juvenile drug court model. Journal of Substance Abuse Treatment. 2003;25(3):189–211. doi: 10.1016/s0740-5472(03)00123-5. [DOI] [PubMed] [Google Scholar]
- 84.Henggeler SW, Halliday-Boykins CA, Cunningham PB, et al. Juvenile drug court: Enhancing outcomes by integrating evidence-based treatments. Journal of Consulting and Clinical Psychology. 2006;74:42–54. doi: 10.1037/0022-006X.74.1.42. [DOI] [PubMed] [Google Scholar]
- 85.Lee SY, Morrissey JP, Thomas KC, et al. Assessing the service linkages of substance abuse agencies with mental health and primary care organizations. American Journal of Drug and Alcohol Abuse. 2006;32(1):69–86. doi: 10.1080/00952990500328620. [DOI] [PubMed] [Google Scholar]
- 86.Brown SA, Anderson KG, Schulte MT, et al. Facilitating youth self-change through school-based intervention. Addictive Behaviors. 2005;30(9):1797–1810. doi: 10.1016/j.addbeh.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 87.Wagner EF, Tubman JG, Gil AG. Implementing school-based substance abuse interventions: Methodological dilemmas and recommended solutions. Addiction. 2004;99(Suppl2):106–119. doi: 10.1111/j.1360-0443.2004.00858.x. [DOI] [PubMed] [Google Scholar]
- 88.Mason MJ, Adger H. Screening for drug abuse in an adolescent primary health care clinic. Journal of Child and Adolescent Substance Abuse. 1997;7(1):33–43. [Google Scholar]
- 89.Chamberlain P, Fisher PA, Moore K. Multidimensional treatment foster care: Applications of the OSLC intervention model to high-risk youth and their families. In: Reid JB, Patterson GR, Snyder J, editors. Antisocial Behavior in Children and Adolescents: A Developmental Analysis and Model for Intervention. Washington, DC: American Psychological Association; 2002. pp. 203–218. [Google Scholar]
- 90.Slesnick N, Meyers RJ, Meade M, et al. Bleak and hopeless no more: Engagement of reluctant substance-abusing runaway youth and their families. Journal of Substance Abuse Treatment. 2000;19(3):215–22. doi: 10.1016/s0740-5472(00)00100-8. [DOI] [PubMed] [Google Scholar]
- 91.Hoagwood K, Olin S. The NIMH Blueprint for Change report: Research priorities in child and adolescent mental health. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(7):760–767. doi: 10.1097/00004583-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 92.Huang L, Stroul B, Friedman R, et al. Transforming mental health care for children and their families. American Psychologist. 2005;60(6):615–627. doi: 10.1037/0003-066X.60.6.615. [DOI] [PubMed] [Google Scholar]
- 93.Tolan PH, Dodge KA. Children’s mental health as a primary care and concern: A system for comprehensive support and service. American Psychologist. 2005;60(6):601–614. doi: 10.1037/0003-066X.60.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Garland AF, Aarons GA, Brown SA, et al. Diagnostic profiles associated with use of mental health and substance abuse services among high-risk youths. Psychiatric Services. 2003;54(4):562–564. doi: 10.1176/appi.ps.54.4.562. [DOI] [PubMed] [Google Scholar]
- 95.Diamond G, Panichelli-Mindel SD, Dennis M, et al. Psychiatric syndromes in adolescents with marijuana abuse and dependency in outpatient treatment. Journal of Child and Adolescent Substance Abuse. 2006;15(4):37–54. [Google Scholar]
- 96.Titus JC, Dennis ML. Cannabis Youth Treatment intervention: Preliminary findings and implications. In: Liddle HA, Rowe CL, editors. Adolescent Substance Abuse: Research and Clinical Advances. New York: Cambridge University Press; 2006. pp. 104–126. [Google Scholar]
- 97.Essau CA, Stigler H, Scheipl J. Epidemiology and comorbidity. In: Essau CA, editor. Substance Abuse and Dependence in Adolescence: Epidemiology, Risk Factors, and Treatment. New York: Taylor & Francis, Inc; 2002. pp. 63–85. [Google Scholar]
- 98.Roberts RE, Roberts CR, Xing Y. Comorbidity of substance use disorders and other psychiatric disorders among adolescents: Evidence from an epidemiologic survey. Drug and Alcohol Dependence. 2007:88. doi: 10.1016/j.drugalcdep.2006.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Glantz MD, Leshner AI. Drug abuse and developmental psychopathology. Development and Psychopathology. 2000;12(4):795–814. doi: 10.1017/s0954579400004120. [DOI] [PubMed] [Google Scholar]
- 100.Kessler RC. National Cormorbidity Survey: Baseline (NCS-1) Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 1990. University of Michigan SRC, editor. [ICPSR06693-v3] [Google Scholar]
- 101.Goodman SH, Lahey BB, Fielding B, et al. Representativeness of clinical samples of youths with mental disorders: A preliminary population-based study. Journal of Abnormal Psychology. 1997;106(1):3–14. doi: 10.1037//0021-843x.106.1.3. [DOI] [PubMed] [Google Scholar]
- 102.Clark HW. Bridging the gap between substance abuse practice and research: The National Treatment Plan Initiative. Journal of Drug Issues. 2002;32:757–768. [Google Scholar]
- 103.Center for Substance Abuse Treatment. Changing the conversation: Improving substance abuse treatment: The National Treatment Plan Initiative. Rockville, MD: U. S. Department of Health and Human Services; 2002. [Google Scholar]
- 104.Hser YI, Grella CE, Hubbard RL, et al. An evaluation of drug treatments for adolescents in 4 US cities. Archives of General Psychiatry. 2001;58(7):689–695. doi: 10.1001/archpsyc.58.7.689. [DOI] [PubMed] [Google Scholar]
- 105.Johnson TP, Booth AL, Johnson P. Physician beliefs about substance misuse and its treatment: Findings from a U.S. survey of primary care practitioners. Substance Use and Misuse. 2005;40(8):1071–1084. doi: 10.1081/JA-200030800. [DOI] [PubMed] [Google Scholar]
- 106.Kramer TL, Robbins JM, Phillips SD, et al. Detection and outcomes of substance use disorders in adolescents seeking mental health treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(11):1318–1326. doi: 10.1097/01.chi.0000084833.67701.44. [DOI] [PubMed] [Google Scholar]
- 107.McLellan AT, Meyers K. Contemporary addiction treatment: A review of systems problems for adults and adolescents. Biological Psychiatry. 2004;56(10):764–770. doi: 10.1016/j.biopsych.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 108.Stiffman AR, Chen Y, Elze D, et al. Adolescents’ and providers’ perspectives on the need for and use of mental health services. Journal of Adolescent Health. 1997;21(5):335–342. doi: 10.1016/S1054-139X(97)00046-3. [DOI] [PubMed] [Google Scholar]
- 109.Kulig JW. The Committee on Substance Abuse. The Role of the pediatrician in prevention, identification, and management of substance abuse. Pediatrics. 2005;115:816–821. doi: 10.1542/peds.2004-2841. [DOI] [PubMed] [Google Scholar]
- 110.Brannan AM, Heflinger CA. Caregiver, child, family, and service system contributors to caregiver strain in two child mental health service systems. The Journal of Behavioral Health Services and Research. 2006;33(4):408–422. doi: 10.1007/s11414-006-9035-1. [DOI] [PubMed] [Google Scholar]
- 111.Brannan AM, Heflinger CA, Foster ME. The role of caregiver strain and other family variables in determining children’s use of mental health services. Journal of Emotional and Behavioral Disorders. 2003;11:77–91. [Google Scholar]
- 112.Angold A, Messer SC, Stangl D, et al. Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health. 1998;88(1):75–80. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sayal K. The role of parental burden in child mental health service use: Longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(11):1328–33. doi: 10.1097/01.chi.0000138353.83357.fa. [DOI] [PubMed] [Google Scholar]
- 114.Logan DE, King CA. Parental facilitation of adolescent mental health services utilization: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2001;8(3):319–333. [Google Scholar]
- 115.Sayal K. Annotation: Pathways to care for children with mental health problems. Journal of Child Psychology and Psychiatry. 2006;47(7):649–659. doi: 10.1111/j.1469-7610.2005.01543.x. [DOI] [PubMed] [Google Scholar]
- 116.Teagle SE. Parental problem recognition and child mental health service use. Mental Health Services Research. 2002;4(4):257–266. doi: 10.1023/a:1020981019342. [DOI] [PubMed] [Google Scholar]
- 117.Zwaanswijk M, Van Der Ende J, Verhaak PFM, et al. The different stages and actors involved in the process leading to the use of adolescent mental health services. Clinical Child Psychology and Psychiatry. 2007;12:567–582. doi: 10.1177/1359104507080985. [DOI] [PubMed] [Google Scholar]
- 118.Dishion TJ, Kavanaugh K, Schneiger A, et al. Preventing early adolescent substance use: A family-centered strategy for the public middle school. Prevention Science. 2002;3(3):191–201. doi: 10.1023/a:1019994500301. [DOI] [PubMed] [Google Scholar]
- 119.Hallfors D, Cho H, Brodish PH, et al. Identifying high school students “at risk” for substance use and other behavioral problems: implications for prevention. Substance Use and Misuse. 2006;41(1):1–15. doi: 10.1080/10826080500318509. [DOI] [PubMed] [Google Scholar]
- 120.Reid JB, Eddy JM. Preventive efforts during the elementary school years: The Linking the Interests of Families and Teachers Project (LIFT) In: Reid JB, Patterson GR, Snyder J, editors. Antisocial Behavior in Children and Adolescents: A Developmental Analysis and Model for Intervention. Washington, DC: American Psychological Association; 2002. pp. 219–33. [Google Scholar]
- 121.Robinson WL, Harper GW, Schoeny ME. Reducing substance use among African American adolescents: Effectiveness of school-based health centers. Clinical Psychology: Science and Practice. 2003;10:491–504. doi: 10.1093/clipsy.bpg049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Slade EP. Effects of school-based mental health programs on mental health service use by adolescents at school and in the community. Mental Health Services Research. 2002;4(3):151–166. doi: 10.1023/a:1019711113312. [DOI] [PubMed] [Google Scholar]
- 123.Mills C, Stephan SH, Moore E, et al. The President’s New Freedom Commission: Capitalizing on opportunities to advance school-based mental health services. Clinical Child and Family Psychology Review. 2006;9:149–161. doi: 10.1007/s10567-006-0003-3. [DOI] [PubMed] [Google Scholar]
- 124.Severson HH, Walker HM, Hope-Doolittle J, et al. Proactive, early screening to detect behaviorally at-risk students: Issues, approaches, emerging innovations, and professional practices. Journal of School Psychology. 2007;45:193–223. [Google Scholar]
- 125.Hoagwood K, Johnson J. School psychology: A Public health framework I. From evidence-based practices to evidence-based policies. Journal of School Psychology. 2003;41(1):3–21. [Google Scholar]
- 126.Feil EG, Severson HH, Walker HM. Screening for emotional and behavioral delays: The Early Screening Project. Journal of Early Intervention. 1998;21(3):252–266. [Google Scholar]
- 127.Feil EG, Severson HH, Walker HM. Early screening and intervention to prevent the development of aggressive, destructive behavior patterns among at-risk children. In: Shinn MR, Walker HM, Stoner G, editors. Interventions for Academic and Behavior Problems II: Preventative and Remedial Approaches. Bethesda, MD: National Association of School Psychologists; 2002. pp. 143–160. [Google Scholar]
- 128.Loeber R, Dishion TJ, Patterson G. Multiple gating: A multistage assessment procedure for identifying youths at risk for delinquency. Journal of Research in Crime and Delinquency. 1984;21:7–32. [Google Scholar]
- 129.Conduct Problems Prevention Research Group. Initial impact of the Fast Track prevention trial for conduct problems: I. The high-risk Sample. Journal of Consulting and Clinical Psychology. 1999;67:631–647. [PMC free article] [PubMed] [Google Scholar]
- 130.Conduct Problems Prevention Research Group. The implementation of the Fast Track program: An example of a large-scale science efficacy trial. Journal of Abnormal Child Psychology. 2002;30:1–17. [PMC free article] [PubMed] [Google Scholar]
- 131.Lochman JE The Conduct Problems Prevention Research Group. Screening of child behavior problems for prevention programs at school entry. Journal of Substance Abuse Treatment. 1995;22:231–243. doi: 10.1037//0022-006x.63.4.549. [DOI] [PubMed] [Google Scholar]
- 132.McMahon RJ, Slough NM . The Conduct Problems Prevention Research Group. Family-based intervention in the Fast Track program. In: Peters RD, McMahon RJ, editors. Preventing Childhood Disorders, Substance Abuse, and Delinquency. Thousand Oaks, CA: Sage Publication; 1996. pp. 90–110. [Google Scholar]
- 133.McCambridge J, Strang J. The reliability of drug use data collected in the classroom: What is the problem, why does it matter and how should it be approached? Drug and Alcohol Review. 2006;25:413–418. doi: 10.1080/09595230600868496. [DOI] [PubMed] [Google Scholar]
- 134.Jankowski MK, Rosenberg HJ, Sengupta AS, et al. Development of a screening tool to identify adolescents engaged in multiple problem behaviors: The Adolescent Risk Behavior Screen (ARBS) Journal of Adolescent Health. 2007;40:180.e19–a80.e26. doi: 10.1016/j.jadohealth.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 135.Grekin ER, Sher KJ, Wood PK. Personality and substance dependence symptoms: Modeling substance-specific traits. Psychology of Addictive Behaviors. 2006;20(4):415–424. doi: 10.1037/0893-164X.20.4.415. [DOI] [PubMed] [Google Scholar]
- 136.Wills TA, Walker C, Mendoza D, et al. Behavioral and emotional self-control: Relations to substance use in samples of middle and high school students. Psychology of Addictive Behaviors. 2006;20(3):265–278. doi: 10.1037/0893-164X.20.3.265. [DOI] [PubMed] [Google Scholar]
- 137.Anderson KG, Tapert SF, Moadab I, et al. Personality risk profile for conduct disorder and substance use disorders in youth. Addictive Behaviors. 2007;32:2377–2382. doi: 10.1016/j.addbeh.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 138.Merenäkk L, Harro M, Kiive E, et al. Association between substance use, personality traits, and platelet MAO activity in preadolescents and adolescents. Addictive Behaviors. 2003;28:1507–1514. doi: 10.1016/s0306-4603(02)00270-8. [DOI] [PubMed] [Google Scholar]
- 139.Levitt JM, Saka N, Romanelli LH, et al. Early identification of mental health problems in schools: The status of instrumentation. Journal of School Psychology. 2007;45:163–191. [Google Scholar]
- 140.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington VT: University of Vermont Research Center for Children, Youth & Families; 2001. [Google Scholar]
- 141.Wright D, Pemberton M. Risk and Protective Factors for Adolescent Drug Use: Findings from the 1999 Household Survey on Drug Abuse. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2004. DHHS Publication No. SMA 04-3874, Analytic Series A-19. [Google Scholar]
- 142.McCrae RR, Costa PTJ. A five-factor theory of personality. In: Pervin LA, John OP, editors. Handbook of Personality: Theory and Research. 2. New York: Guilford; 1999. pp. 139–154. [Google Scholar]
- 143.Goldberg LR. The structure of phenotypic personality traits. American Psychologist. 1993;48:26–34. doi: 10.1037//0003-066x.48.1.26. [DOI] [PubMed] [Google Scholar]
- 144.John OP, Caspi A, Robins RW, et al. The “Little Five”: Exploring the nomological network of the Five-Factor model of personality in adolescent boys. Child Development. 1994;65(1):160–178. [PubMed] [Google Scholar]
- 145.Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the Big-Five personality domains. Journal of Research in Personality. 2003;37(6):504–528. [Google Scholar]
- 146.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 147.Broome KM, Joe GW, Simpson DD. Engagement models for adolescents in DATOS-A. Journal of Adolescent Research. 2001;16(6):608–623. [Google Scholar]
- 148.Saunders SM, Resnick M, Hoberman HM, et al. Formal help-seeking behavior of adolescents identifying themselves as having mental health problems. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(5):718–728. doi: 10.1097/00004583-199406000-00013. [DOI] [PubMed] [Google Scholar]
- 149.Dakof GA, Tejeda M, Liddle HA. Predictors of engagement in adolescent drug abuse treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:274–281. doi: 10.1097/00004583-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 150.Nock MK, Ferriter C. Parent management of attendance and adherence in child and adolescent therapy: A conceptual and empirical review. Clinical Child and Family Psychology Review. 2005;8(2):149–166. doi: 10.1007/s10567-005-4753-0. [DOI] [PubMed] [Google Scholar]
- 151.Nock MK, Photos V. Parent motivation to participate in treatment: Assessment and prediction of subsequent participation. Journal of Child and Family Studies. 2006;15(3):345–358. [Google Scholar]
- 152.Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology. 1997;65(3):453–63. doi: 10.1037//0022-006x.65.3.453. [DOI] [PubMed] [Google Scholar]
- 153.Morrissey-Kane E, Prinz RJ. Engagement in child and adolescent treatment: The role of parental cognitions and attributions. Clinical Child and Family Psychology Review. 1999;2(3):183–198. doi: 10.1023/a:1021807106455. [DOI] [PubMed] [Google Scholar]
- 154.Nock MK, Kazdin AE. Parent expectancies for child therapy: Assessment and relation to participation in treatment. Journal of Child and Family Studies. 2001;10(2):155–180. [Google Scholar]
- 155.Orrell-Valente JK, Pinderhughes EE, Valente E, Jr, et al. If it’s offered, will they come? Influences on parents’ participation in a community-based conduct problems prevention program. American Journal of Community Psychology. 1999;27(6):753–783. doi: 10.1023/a:1022258525075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Santisteban DA, Szapocznik J, Perez-Vidal A, et al. Efficacy of intervention for engaging youth and families into treatment and some variables that may contribute to differential effectiveness. Journal of Family Psychology. 1996;10(1):35–44. [Google Scholar]
- 157.Diamond GS, Liddle HA. Transforming negative parent-adolescent interactions: From impasse to dialogue. Family Process. 1999;38:5–26. doi: 10.1111/j.1545-5300.1999.00005.x. [DOI] [PubMed] [Google Scholar]
- 158.Fals-Stewart W, Fincham FD, Kelly ML. Substance-abusing parents’ attitudes toward allowing their custodial children to participate in treatment: A comparison of mothers versus fathers. Journal of Family Psychology. 2004;18(4):666–671. doi: 10.1037/0893-3200.18.4.666. [DOI] [PubMed] [Google Scholar]
- 159.Stanton MD. Getting reluctant substance abusers to engage in treatment/self-help: A review of outcomes and clinical options. Journal of Marital and Family Therapy. 2004;30(2):165–182. doi: 10.1111/j.1752-0606.2004.tb01232.x. [DOI] [PubMed] [Google Scholar]
- 160.Garrett J, Landau-Stanton J, Stanton MD, et al. ARISE: A method for engaging reluctant alcohol- and drug-dependent individuals in treatment. Journal of Substance Abuse Treatment. 1997;14(3):235–248. doi: 10.1016/s0740-5472(96)00159-6. [DOI] [PubMed] [Google Scholar]
- 161.Garrett J, Stanton MD, Landau J, et al. The “concerned other” call: Using family links and networks to overcome resistance to addiction treatment. Substance Use and Misuse. 1999;34(3):363–382. doi: 10.3109/10826089909035651. [DOI] [PubMed] [Google Scholar]
- 162.Szapocznik J, Perez-Vidal A, Hervis O, et al. Innovations in family therapy: Strategies for overcoming resistance to treatment. In: Wells RA, Gianetti VJ, editors. Handbook of Brief Psychotherapies: Applied Clinical Psychology. New York: Plenum Press; 1990. pp. 93–114. [Google Scholar]
- 163.Meyers RJ, Miller WR, Hill DE, et al. Community reinforcement and family training (CRAFT): Engaging unmotivated drug users in treatment. Journal of Substance Abuse. 1999;10:291–308. doi: 10.1016/s0899-3289(99)00003-6. [DOI] [PubMed] [Google Scholar]
- 164.Meyers RJ, Miller WR, Smith JE. Community reinforcement and family training. In: Meyers RJ, Miller WR, editors. A Community Reinforcement Approach to Addiction Treatment: International Research Monographs in the Addictions. New York: Cambridge University Press; 2001. pp. 147–160. [Google Scholar]
- 165.Minuchin S, Fishman HC. Family Therapy Techniques. Cambridge, MA: Harvard University Press; 1981. [Google Scholar]
- 166.Coatsworth JD, Santisteban DA, McBride CK, et al. Brief strategic family therapy versus community control: Engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Family Process. 2001;40(3):313–332. doi: 10.1111/j.1545-5300.2001.4030100313.x. [DOI] [PubMed] [Google Scholar]
- 167.Szapocznik J, Perez-Vidal A, Brickman AL, et al. Engaging adolescent drug abusers and their families in treatment: A strategic structural systems approach. Journal of Consulting and Clinical Psychology. 1988;56(4):552–557. doi: 10.1037//0022-006x.56.4.552. [DOI] [PubMed] [Google Scholar]
- 168.Waldron HB, Kern-Jones S, Turner CW, et al. Engaging resistant adolescents in drug abuse treatment. Journal of Substance Abuse Treatment. 2007;32(2):133–142. doi: 10.1016/j.jsat.2006.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Office of Juvenile Justice and Deliquency Prevention. Developing a Policy for Controlled Substance Testing of Juveniles. Washington, D.C.: U.S. Government Printing Office; 2000. [Google Scholar]
- 170.Knight JR, Levy S. The national debate on drug testing in schools. Journal of Adolescent Health. 2007;41:419–420. doi: 10.1016/j.jadohealth.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 171.Irwin CEJ. Editorial. To test or not to test: Screening for substance use in adolescents. Journal of Adolescent Health. 2006;38:329–331. doi: 10.1016/j.jadohealth.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 172.American Academy of Pediatrics, Committee on Substance Abuse and Council on School Health. Testing for drugs of abuse in children and adolescents: Addendum—Testing in schools and at home. Pediatrics. 2007;119:627–630. doi: 10.1542/peds.2006-3688. [DOI] [PubMed] [Google Scholar]
- 173.Levy S, Harris SK, Sherritt L, et al. Drug testing of adolescents in general medical clinics, in school and at home: Physician attitudes and practices. Journal of Adolescent Health. 2006;38(4):336–342. doi: 10.1016/j.jadohealth.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 174.Yamaguchi R, Johnston LD, O’Malley PM. Youth, Education, and Society (YES) Occasional Paper Number 2. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2003. Drug Testing in Schools: Policies, Practices, and Association with Student Drug Use. [Google Scholar]
- 175.Yamaguchi R. Relationships between school drug searches and student substance use in U.S. schools. Educational Evaluation and Policy Analysis. 2004;26(4):329–341. [Google Scholar]
- 176.Goldberg L, Elliott DL, MacKinnon DP, et al. Outcomes of a prospective trial of student-athlete drug testing: The Student Athlete Testing Using Random Notification (SATURN) study. Journal of Adolescent Health. 2007;41:421–429. doi: 10.1016/j.jadohealth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 177.Breda CS, Heflinger CA. The impact of motivation to change on substance use among adolescents in treatment. Journal of Child and Adolescent Substance Abuse. 2007;16(3):109–124. [Google Scholar]
- 178.Cady ME, Winters KC, Jordan DA, et al. Motivation to change as a predictor of treatment outcome for adolescent substance abusers. Journal of Child and Adolescent Substance Abuse. 1996;5(1):73–91. [Google Scholar]
- 179.Melnick G, DeLeon G, Hawke J, et al. Motivation and readiness for therapeutic community treatment among adolescents and adult substance abusers. American Journal of Drug and Alcohol Abuse. 1997;3(4):485–506. doi: 10.3109/00952999709016891. [DOI] [PubMed] [Google Scholar]
- 180.Friedman AS, Granick S, Kreisher C. Motivation of adolescent drug abusers for help and treatment. Journal of Child and Adolescent Substance Abuse. 1994;3(1):69–88. [Google Scholar]
- 181.Irwin CEJ, Duncan PM. Health futures of youth II: Pathways to adolescent health, Executive summary and overview. Journal of Adolescent Health. 2002;31:82–89. doi: 10.1016/s1054-139x(02)00513-x. [DOI] [PubMed] [Google Scholar]
- 182.Needle RH, Burrows D, Friedman SR, et al. Effectiveness of community-based outreach in preventing HIV/AIDS among injecting drug users. International Journal of Drug Policy. 2005;16(suppl 1):45–57. [Google Scholar]
- 183.World Health Organization. Evidence for Action: Effectiveness of Community-Based Outreach in Preventing HIV/AIDS Among Injecting Drug Users. Geneva, Switzerland: World Health Organization; 2004. [Google Scholar]
- 184.Davidson G, Campbell J. An examination of the use of coercion by assertive outreach and community mental health teams in Northern Ireland. British Journal of Social Work. 2007;37:537–555. [Google Scholar]
- 185.McGrew JH, Wilson RG, Bond GR. An exploratory study of what clients like least about assertive community treatment. Psychiatric Services. 2002;53:761–763. doi: 10.1176/appi.ps.53.6.761. [DOI] [PubMed] [Google Scholar]
- 186.Phillips SD, Burns BJ, Edgar ER, et al. Moving assertive community treatment into standard practice. Psychiatric Services. 2001;52:771–779. doi: 10.1176/appi.ps.52.6.771. [DOI] [PubMed] [Google Scholar]
- 187.Williamson T. Ethics of assertive outreach (assertive community treatment) Current Opinion in Psychiatry. 2002;15:543–547. doi: 10.1097/00001504-200209000-00013. [DOI] [PubMed] [Google Scholar]
- 188.Forehand L, Jr, Ciccone JR. The competence of adolescents to consent to treatment. In: Flaherty LT, editor. Adolescent Psychiatry: Developmental and Clinical Studies. Vol. 28. Mahwah, NJ: Analytic Press; 2004. pp. 5–27. [Google Scholar]
- 189.Stanton MD, Heath AH. Family/couples approaches to treatment engagement and therapy. In: Lowinson JH, Millman RB, Langrod JG, editors. Substance Abuse: A Comprehensive Textbook. Baltimore, MD: Lippincott, Williams & Wilkins; 2005. pp. 680–690. [Google Scholar]
- 190.Logan DE, King CA. Parental identification of depression and mental health service use among depressed adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:296–304. doi: 10.1097/00004583-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 191.Zwaanswijk M, Van der Ende J, Vehhaak PFM, et al. Factors associated with adolescent mental health service need and utilization. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:692–700. doi: 10.1097/01.CHI.0000046862.56865.B7. [DOI] [PubMed] [Google Scholar]
- 192.Aos S, Phipps P, Baronski R, Leib R. The Comparative Costs and Benefits of Programs to Reduce Crime. Olympia, WA: Washington State Institute for Public Policy; 2001. [Google Scholar]
- 193.Schoenwald SK. Multisystemic Therapy treatment of substance abusing or dependent adolescent offenders: Costs of reducing incarceration, inpatient, and residential placement. Journal of Child and Family Studies. 1996;5(4):431–444. [Google Scholar]
- 194.Cavanaugh DA. Maximizing potential: Federal financing for treatment of adolescents with substance use disorders. Journal of Psychoactive Drugs. 2004;36:415–427. doi: 10.1080/02791072.2004.10524425. [DOI] [PubMed] [Google Scholar]
- 195.Miller TR, Hendrie D. How should governments spend the drug prevention dollar? A buyer’s guide. In: Toumbourou JW, Loxley W, Stockwell T, et al., editors. Preventing Harmful Substance Use: The Evidence Base for Policy and Practice. New York: John Wiley & Sons; 2005. pp. 415–431. [Google Scholar]
- 196.McCollister KE, French MT. The relative contribution of outcome domains in the total economic benefit of addiction interventions: A review of first findings. Addiction. 2003;98(12):1647–1659. doi: 10.1111/j.1360-0443.2003.00541.x. [DOI] [PubMed] [Google Scholar]
- 197.Cohen MA. The monetary value of saving high-risk youth. Journal of Quantitative Criminology. 1998;14:5–33. [Google Scholar]
- 198.Albers CA, Glover TA, Kratochwill TR. Editorial. Introduction to the special issue: How can universal screening enhance educational and mental health outcomes? Journal of School Psychology. 2007;45:113–116. [Google Scholar]
- 199.Hallfors D, Van Dorn RA. Strengthening the role of two key institutions in the prevention of adolescent substance abuse. Journal of Adolescent Health. 2002;30:17–28. doi: 10.1016/s1054-139x(01)00322-6. [DOI] [PubMed] [Google Scholar]
- 200.Nemeroff R, Levitt JM, Faul L, et al. Establishing ongoing, early identification programs for mental health problems in our school: A feasibility study. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:328–338. doi: 10.1097/CHI.0b013e318160c5b1. [DOI] [PubMed] [Google Scholar]
- 201.Hawkins JD, Catalano RF, Arthur MW. Promoting science-based prevention in communities. Addictive Behaviors. 2002;27(6):951–976. doi: 10.1016/s0306-4603(02)00298-8. [DOI] [PubMed] [Google Scholar]
- 202.Schoenwald SK, Henggeler SW. Mental health services research and family-based treatment: Bridging the gap. In: Liddle HA, Santisteban DA, Levant RF, et al., editors. Family Psychology: Science-based Interventions. Washington, DC: American Psychological Association; 2002. pp. 259–282. [Google Scholar]
- 203.Stormshak EA, Dishion TJ. An ecological approach to child and family clinical and counseling psychology. Clinical Child and Family Psychology Review. 2002;5(3):197–215. doi: 10.1023/a:1019647131949. [DOI] [PubMed] [Google Scholar]
- 204.Stroul BA, Friedman RM. A System of Care for Severely Emotionally Disturbed Children and Youth. Washington, D. C.: Georgetown University Child Development Center; 1986. [Google Scholar]
- 205.Tolan PH, Guerra NG, Kendall PC. A developmental ecological perspective on antisocial behavior in children and adolescents: Toward a unified risk and intervention framework. Journal of Consulting and Clinical Psychology. 1995;63(4):579–584. doi: 10.1037//0022-006x.63.4.579. [DOI] [PubMed] [Google Scholar]
- 206.Biglan A. Changing Cultural Practices: A Functional Contextualist Framework for Intervention Research. Reno, NV: Context Press; 1995. [Google Scholar]
- 207.Cherpital CJ. Alcohol-related injury and the emergency department: Research and policy questions for the next decade. Addiction. 2006;101:1225–1227. doi: 10.1111/j.1360-0443.2006.01567.x. [DOI] [PubMed] [Google Scholar]