Abstract
Purpose
AKT plays a central role in regulating tumor cell survival and cell cycle progression, and is regarded as a promising therapeutic target. We used genetically-defined mouse models that develop spontaneous tumors exhibiting activated Akt to determine if Akt inhibition by GSK690693 is effective in the treatment of cancer. The broad, long-term objective of this project was to use preclinical cancer models with precisely defined genetic lesions to elucidate the efficacy of targeting Akt with GSK690693.
Experimental Design
We tested the in vivo effects of GSK690693 in Lck-MyrAkt2 transgenic mice that develop lymphomas, heterozygous Pten+/− knockout mice that exhibit endometrial tumors, and TgMISIIR-TAg-DR26 mice that develop ovarian carcinomas, all of which exhibit hyperactivation of Akt. In addition to standard disease onset and histology, tumors arising in treated animals were examined by immunohistochemistry to verify down regulated Akt signaling relative to placebo-treated mice. When possible, drug response was evaluated in tumor cell cultures by standard proliferation and apoptosis assays and by immunoblotting with various phospho-specific antibodies.
Results
GSK690693 exhibited efficacy irrespective of the mechanism of Akt activation involved. Interestingly, GSK690693 was most effective in delaying tumor progression in Lck-MyrAkt2 mice expressing a membrane-bound, constitutively active form of Akt. Both tumors and primary cell cultures displayed down regulation of the Akt pathway, increased apoptosis and primarily decreased cell proliferation.
Conclusion
These results suggest that GSK690693 or other AKT inhibitors might have therapeutic efficacy in human cancers with hyperactivated AKT and/or a dependence on AKT signaling for tumor progression.
Keywords: AKT, PTEN, SV40 T antigens, small molecule inhibitors
Introduction
AKT/PKB kinases regulate a plethora of diverse cellular processes that contribute to tumor progression, including cell proliferation and survival, cell size and response to nutrient availability, tissue invasion, and angiogenesis. Hyperactivation of AKT signaling in numerous sporadic human cancers, as well as in several dominantly-inherited cancer syndromes, is commonly attributed to activation or overexpression of tyrosine kinase growth factor receptors, mutation/overexpression of phosphatidylinositol 3-kinase (PI3K), or inactivation/down regulation of the PTEN tumor suppressor, a negative regulator of AKT signaling (reviewed in 1). Consequently, there is considerable interest in targeting the PI3K/AKT pathway as a therapeutic strategy to combat human cancer.
GSK690393 is a novel ATP-competitive, pan-AKT inhibitor with strong selectivity for the AKT kinases (2). Initial studies showed potent pharmacodynamic and antitumor activity in several human tumor cell lines and xenografts (3), and more recently was shown to induce growth inhibition and apoptosis in acute lymphoblastic leukemia cell lines (4). To complement these studies, we used several genetically-defined mouse models of cancer to assess the efficacy of GSK690693 in a preclinical setting. GSK690693 has been evaluated in a dose escalation phase I clinical trial in patients with lymphoma or solid tumors (5, 6).
Frequent hyperactivation of AKT kinases has been identified in a wide assortment of human solid tumors and hematological malignancies (reviewed in 1). Among the various mechanisms that contribute to activation of the AKT pathway in human tumors are perturbations of upstream PTEN and PI3K through somatic genetic and/or epigenetic changes, activation of PI3K due to autocrine or paracrine stimulation of receptor tyrosine kinases, overexpression of growth factor receptors such as the epidermal growth factor receptor and/or Ras activation. Because the AKT signaling cascade is frequently deregulated in many types of cancer and has implications with regard to tumor aggressiveness and chemoresistance, there is potential utility in targeting components of the AKT pathway for cancer therapy and, possibly, cancer prevention.
Transgenic and knockout mouse models are valuable for delineating the role of Akt kinases in vivo. As preclinical models for testing the potential therapeutic efficacy of targeting Akt signaling with GSK690693, we used transgenic mice in which the Lck promoter drives expression of membrane bound, myristylated Akt (MyrAkt) in early thymocyte development. The Lck-MyrAkt2 transgenic mice develop spontaneous, aggressive thymic lymphomas within 10–20 wks (7-9), with the added advantage that the mutant transgene bypasses the need for activation of phosphoinositides 3,4,5-trisphosphate (PIP3) and PIP2 generated by PI3K and, thus, cannot be inhibited by Pten. The Lck-MyrAkt2 model exhibits recurrent chromosomal rearrangements that result in overexpression of c-Myc, which is frequently observed in human lymphomas and postulated to cooperate with activated Akt to drive tumor formation (10, 11).
To further test the efficacy of drug treatment with GSK690693, we employed a Pten+/− knockout model that is susceptible to endometrial neoplastic lesions with full penetrance and characterized by activation of Akt in the endometrium (12). The Pten+/− model has relevance to human cancer in that loss of PTEN is one of the earliest detectable abnormalities in the endometrioid subtype of human endometrial cancer, and loss of PTEN results in deregulation and subsequent constitutive activation of AKT kinase (12). In addition, we also employed a transgenic mouse model of spontaneous epithelial ovarian cancer with expression of SV40 Tag/tag under transcriptional control of the MISIIR promoter (13), which we previously used to test a chemoprevention strategy for targeting Akt/mTor signaling with RAD001 (everolimus; Novartis Pharma AG) (14). SV40 tag binds protein phosphatase PP2A and inhibits its activity, resulting in activation of PI3K-AKT and MAPK signaling (15), and SV40 Tag binds to and functionally inactivates products of the Tp53 and Rb1 genes, which are frequently mutated in human ovarian cancer (16).
Overall, we found that genetically-defined murine tumor models known to be strongly dependent on Akt activity for tumor development exhibited marked response to GSK690693 in terms of delayed tumor progression, decreased phosphorylation of downstream targets of Akt, and decreased cell proliferation and/or increased apoptosis. Collectively, the pharmacologic profile of GSK690693 is consistent with a selective AKT kinase inhibitor, and elevated AKT phosphorylation in tumors may be considered a useful indicator of patients who may benefit from the use of an AKT kinase inhibitor.
Materials and Methods
Reagents
GSK690693 is an AKT kinase inhibitor derived from the aminofurazan chemical series synthesized at GlaxoSmithKline. For all in vitro studies, GSK690693 was dissolved in DMSO at a concentration of 10 mmol/L prior to use. For the tumor xenograft studies, GSK690693 was formulated in 5% dextrose (pH 4.0).
Anti-phospho (P)-AKT (Ser473), anti-AKT, P-AKT blocking peptide, anti-P-mTOR (Ser2448), anti-mTOR, anti-P-p70S6K (Thr389), anti-p70S6K, anti-P-GSK3α/β (Ser21/9), anti-GSK3α/β, anti-P-FOXO1/3 (Thr24/32), P-FOXO1/3 blocking peptide, anti-FOXO, anti-P-PRAS40/Akt1s1 (Thr246) and anti-PRAS40/Akt1s1 and anti-cleaved caspase-3 antibodies were from Cell Signaling (Beverly, MA). Anti-β-actin was from Sigma (St. Louis, MO), and anti-Ki-67 was obtained from Vector Laboratories (Burlingame, CA). Anti-mouse Ki-67 rat monoclonal antibody was from Dako (Carpinteria, CA).
Transgenic Mice and Treatments
Animal experiments were approved by our Institutional Animal Care and Usage Committee in accordance with NIH guidelines. Genetically defined mouse models were genotyped by PCR using previously described methodology (9, 12, 13). Treatment regimens for each mouse model were customized based on previously reported tumor latency of untreated mice. For each study, mice were assigned to two groups receiving either GSK690693 or placebo. For in vivo drug studies of the Lck-MyrAkt2 transgenic mouse model, GSK690693 was injected intraperitoneally at a dose of 30 mg/kg daily, 5 days per wk. Treatment was begun at 8 wks of age and continued for 4 wks duration, at which point all mice were euthanized. Treatment of Pten+/− knockout mice with 30 mg/kg GSK690693 was initiated at 5 mo of age and consisted of 3 cycles of 3 wks of i.p. injections, followed by 1 wk rest, for a total treatment duration of 12 wks. Treatment of TgMISIIR-TAg-DR26 mice with 30 mg/kg GSK690693 was initiated at 14 wks and continued for 4 wks duration. For all preclinical studies, mice were weighed weekly, and dosage was adjusted accordingly, so that the dose could be decreased if there was weight loss. No significant weight loss of greater than 10% of the initial body weight was observed in the GSK690693-treated or placebo-treated groups. Tumor volumes in Lck-MyrAkt2 and TgMISIIR-TAg-DR26 mice were calculated as follows: V = L x W x D x π/6, where V is volume, L is length, W is width, and D is depth. Pten+/− mice were examined histologically for lesions. Tumors from Lck-MyrAkt2 and TgMISIIR-TAg-DR26 mice also were examined histologically.
Immunohistochemistry
Tumors were fixed in 10% neutral buffered formalin and embedded in paraffin. Slides containing formalin-fixed, paraffin-embedded samples were deparaffinized, hydrated in water and subjected to antigen retrieval in 10 mM citrate buffer, pH 6.0. Anti-P-AKT (Ser 473), anti-P-FOXO1/3 (Thr24/32), anti-Ki-67, and anti-cleaved caspase-3 (each defined above) were detected with biotinylated secondary antibodies. Specificity for anti-AKT and anti-FOXO1/3 antibodies was confirmed by preincubation with antigen-specific blocking peptide. Tissue sections were stained with DAB chromogen and counterstained with hematoxylin.
Photographs of endometrium and ovarian tumors were captured with an Eclipse E600 microscope (Nikon Instruments, Melville, NY) fitted with a Nikon DXM1200 digital camara. Nikon ACT-1 version 2 software was used for acquisition of digital pictures using a 40x objective. Photographs of thymic lymphomas were captured with an Arcturus PixCell IIe microscope (Molecular Devices, Sunnyvale, CA), using a 20x objective and version 2.0.0 software.
Ki-67 stain was scored counting either the percent of stained nuclei (endometrial lesions) (n= 400–500 per slide, 5 slides per lesion and treatment group) or the number of stained nuclei per high magnification field (lymphomas and ovarian tumors) (at least 5 fields per tumor and treatment group). The other immunohistochemical stains were scored using a semi-quantitative scale based on stain intensity, i.e. 0= negative, +/− = marginal, 1+ = low intensity stain, 2+ = moderate intensity stain, and 3+ = very intense stain.
Cell Culture
T cells were isolated from thymic lymphomas of Lck-MyrAtk2 mice by passing tumor tissue through a 100-μM nylon mesh (BD Falcon, Bedford, MA) and culturing in Iscove’s-MDM containing 20% FBS, as previously described (9). Mouse ovarian carcinoma (MOVCAR) cell lines were obtained from ascites of TgMISIIR-TAg mice (13). Cell lines were cultured at 37°C in DMEM containing 4% FBS, 1% 1x ITS, penicillin/streptomycin (100 units/ml and 100 μg/ml, respectively), and 2 mM glutamine in a humidified atmosphere of 5% CO2. Primary mouse cell cultures were derived from different mice prior to this study. SKOV3 cells from the American Type Culture Collection (Rockville, MD) were cultured in McCoy’s 5A with 10% FBS. Experiments were performed with growth medium containing 10% serum.
Cell Viability Assay
An MTT assay was used to analyze the effect of GSK690693 on cell viability. Cells were cultured overnight in 96-well plates (5 × 103 cells/well). Cell viability was assessed after addition of GSK690693 at the indicated concentrations for 72 hrs. In brief, the tetrazolium compound MTT (3-[4, 5-dimethylthiazol-2-yl]-2, 5-diphenyltetrazolium bromide) was added to the wells, and the cells were incubated 2 hrs at 37°C. Detergent was added to the wells to solubilize the formazan dye crystals for 4 hrs at 37°C, and then absorbance at 595 nm was determined. Cell viability is expressed as follows: Aexp group/Acontrol × 100.
In Vitro Detection of Apoptosis or Cell Cycle Arrest
Cells were treated for 72 hrs with 0, 10 or 20 μM GSK690693 and then double labeled with propidium iodide (PI) and annexin V for flow cytometry analysis. Analysis of apoptosis was performed with a fluorescence activated cell sorter (FACS)can (Becton Dickinson, San Jose, CA) using Cell Quest software (Becton Dickinson). Alternately, cells were lysed, and DNA fragmentation was detected using a Cell Death Detection ELISA Kit (Roche, Penzberg, Germany) per the manufacturer’s instructions.
For cell cycle analysis, cells were treated for 72 hrs with 0, 10 or 20 μM GSK690693, fixed in 70% ethanol at −20°C, then washed and stained with 10 μg/ml propidium iodide (Sigma, St. Louis, MO). Cell cycle analyses were performed with FACS using Flowjo software (Tree Star, Ashland, Oregon).
Western Blot Analysis
Cells were treated with either DMSO (vehicle) or 10 μM GSK690693 for 8 hrs (thymic lymphoma cells) or overnight (ovarian cells). Cells were washed twice with ice-cold PBS and transferred to lysis buffer (20 mM Tris-HCl, 150 mM NaCl, 1 mM EDTA, 1 mM EGTA, 1 mM Na3VO4, 1 mM β-glycerophosphate, 2.5 mM sodium pyrophosphate, 1 mM 4-(2-aminoethyl)benzenesulfonyl fluoride hydrochloride, 10 μg/ml aprotinin, 1 μg/ml leupeptin, and 1% Triton X-100) for 10 min at 4°C. Lysates were centrifuged at 12,000 X g at 4°C for 15 min, and protein concentrations of the supernatants were determined using Bio-Rad protein assay reagent. Equal amounts of proteins were separated by SDS-PAGE and transferred to nitrocellulose membranes. Blocking was performed with 5% nonfat milk in 1X Tris-buffered saline. Western blot analyses were carried out with various specific primary antibodies. Immunoblots were visualized with horseradish peroxidase-coupled goat anti-rabbit or anti-mouse immunoglobulin by using the enhanced chemiluminescence Western blotting system (Perkin Elmer, Boston MA). Western blot results were confirmed in at least duplicate or triplicate runs.
Results
We recently described independently derived founder lines in which the Lck promoter was used to direct expression of myristylated, constitutively active Akt2 in immature T lymphocytes (9, 10). Tumors from Lck-MyrAkt2 founder line 55 exhibited a median tumor latency of 16.5 wks (10) and activated Akt was found in histologically normal thymus from 4-wk-old transgenic mice as well as in thymic lymphomas (9, 10).
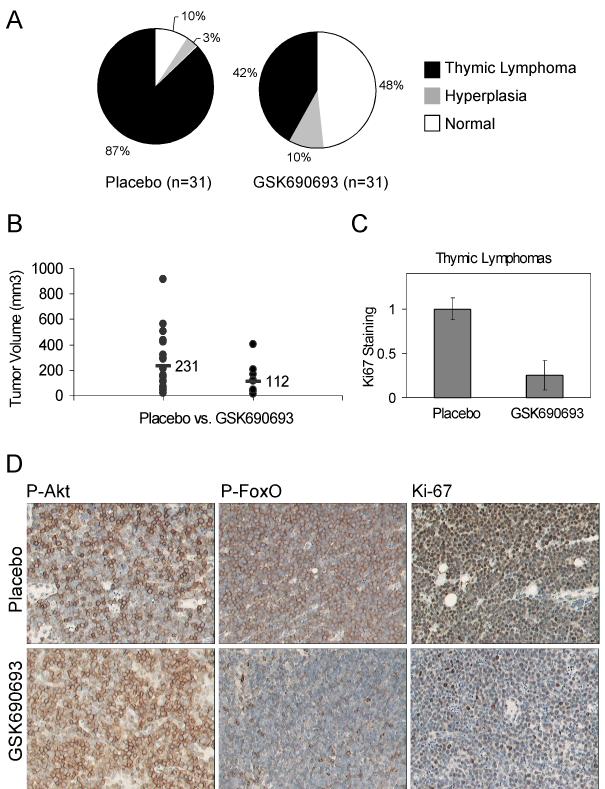
Overall, GSK690693 delayed tumor development and reduced the size of tumors in Lck-MyrAkt2 transgenic mice. Nearly 50% of the 31 GSK690693-treated mice had normal thymic histology, whereas 90% of the 31 placebo-treated mice developed thymic lymphomas or hyperplasia (Fig. 1A). Analysis of the resulting tumors from each group revealed that the average size of the 22 thymic lymphomas from the placebo-treated group was ~2-fold larger than the 11 thymic lymphomas found in the treated group (Fig. 1B). Thus, GSK690693 was efficacious in delaying tumor development in a mouse model genetically engineered to express constitutively active Akt. Moreover, immunohistochemical analysis of the thymic lymphomas derived from GSK690693-treated Lck-MyrAkt2 mice showed decreased staining for Ki-67, a marker of cell proliferation (Fig. 1C). Tumors also exhibited altered expression of phospho-proteins in the Akt signaling pathway in response to GSK690693 treatment (Fig. 1D). Specifically, as demonstrated previously (3), diminished cytoplasmic P-FoxO1/3 and/or presence of nuclear P-FoxO1/3 was indicative of GSK690693 efficacy.
Fig. 1. GSK690693 delays thymic tumor development in Lck-MyrAkt2 mice.
A, Pie charts depicting the percentage of mice that retained normal health (10% in placebo vs. 48% in treated group) or that developed hyperplasia or thymic lymphoma (90% in placebo vs. 52% in the treated group). B, Tumors that developed in GSK690693-treated mice were diminished in size (112 mm3) compared to those that developed in the placebo group (231 mm3). Student T test, p=0.026. C, Bar graph representing a significant difference between Ki-67 staining in placebo and GSK690693 mice (T-test, p=0.001) The number of positively staining tumor cells from 5 fields of 5 placebo- and 5 GSK690693-treated mice were scored using a 40x objective (0.075 mm2 field), and values were normalized relative to staining in placebo mice. Error bars represent standard error. D, Immunohistochemical staining of thymic lymphomas arising in Lck-MyrAkt2 transgenic mice. Pictures were taken with a 20x objective. P-Akt staining was strongly localized to the cytoplasm and plasma membrane (indicative of MyrAkt2 expression) in tumors from placebo-treated mice. P-Akt staining was relatively unchanged in GSK690693-treated mice. P-FoxO1/3 generally exhibited cytoplasmic staining of ++ to + in placebo treated mice and + to +/− in GSK690693-treated mice, with staining in the latter sometimes nuclear.
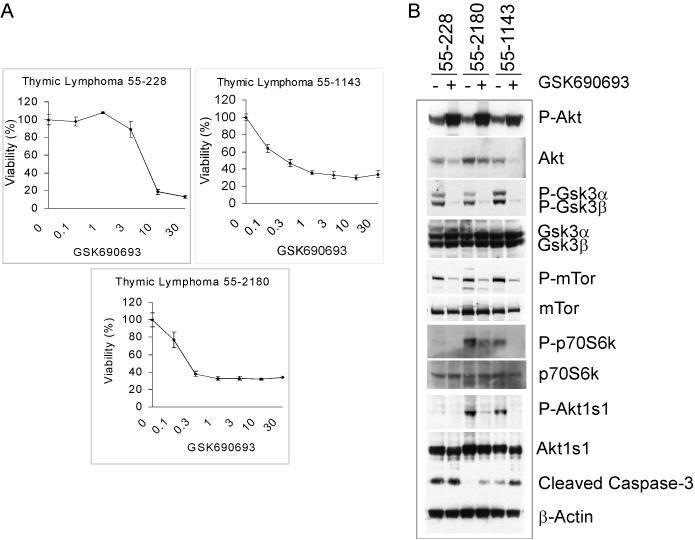
Since various human tumor cell lines have been previously tested for response to GSK690693 (3), we tested tumor cell cultures derived from the preclinical models for in vitro response to GSK690693. Dissociated thymic tumor cells were prepared from Lck-MyrAkt2 mice and were shown by MTT assays to be highly sensitive to GSK690693 treatment (Fig. 2A). Primary tumor cells from 55–1143 and 55–2180 were found to have a lower IC50 (IC50 ~0.3 μM) compared to 55–228 (IC50 ~5 μM) after 72 hrs of treatment. We then analyzed primary tumor cells for the effects of GSK690693 on the phosphorylation of Akt and downstream targets by immunoblotting with various phospho-specific antibodies (Fig. 2B). Thymic lymphoma cells exhibited down regulation of P-Gsk-3α/β, P-mTor, P-p70S6k and P-Akts1, and up regulation of P-Akt following an 8 hr treatment with 10 μM GSK690693. The up regulation of Akt phosphorylation is indicative of a feedback loop to Akt (3). However, the collective decreased phosphorylation of downstream effectors of Akt, decreased Ki-67 staining (Fig. 1C) and increased cleavage of caspase-3 are consistent with in vivo activity of GSK690693 seen in Lck-MyrAkt2 mice.
Fig. 2. GSK690693 inhibits cell viability and Akt signaling in primary tumor cells from Lck-MyrAkt2 mice.
A, Lymphoma cells from individual mice (55–228, 55–1143 and 55–2180) were treated with various concentrations of GSK690693 for 72 hrs and assessed by MTT cell viability assays. Graphs represent percent viability of GSK690693-treated cells compared to corresponding untreated cells. Error bars depict total standard deviation among replicate samples. B, Western blot analysis of thymic lymphoma cells treated with 10 μM GSK690693 for 8 hrs. Cell lysates were screened with antibodies against components of the Akt signaling cascade to detect diminished phosphorylation of downstream targets.
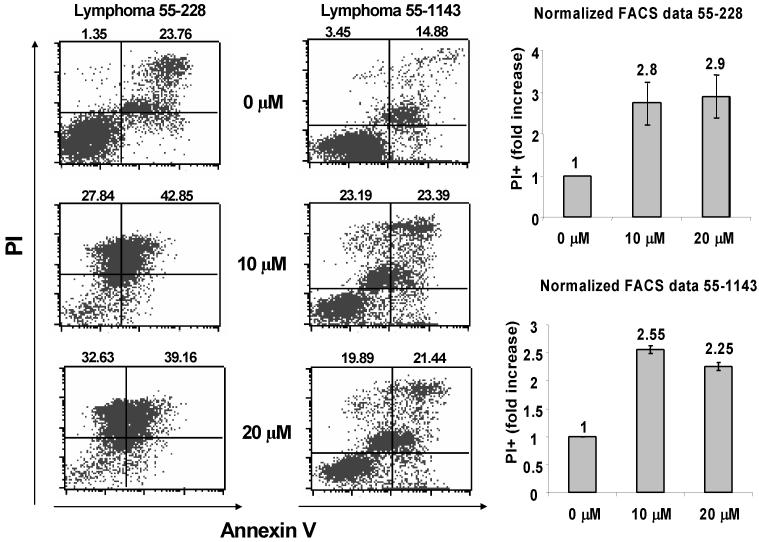
Moreover, the effectiveness of GSK690693 in inducing apoptosis also was assessed by flow cytometry analysis of tumor cells stained with propidium iodide and annexin V (Fig. 3). Thymic lymphoma cells from Lck-MyrAkt2 mice responded rapidly to treatment with GSK690693, with a 2–3 fold increase in apoptotic cells observed within 24 hrs (Fig. 3).
Fig. 3. Thymic lymphoma cells from Lck-MyrAkt2 mice are sensitive to GSK690693-induced apoptosis.
Tumor cells from two different mice were treated for 24 hrs with 0, 10 or 20 μM GSK690693 and then double labeled with propidium iodide (PI) and annexin V for flow cytometry analysis. Representative panels of the FACS analysis of lymphoma cells from mice 55–228 and 55–1143 are shown to the left. Bar graphs to the right illustrate 2–3 fold increase in PI-positive cells (dead tumor cells; upper quadrants of scatter plots) in each of the primary cultures in response to GSK690693. Error bars depict total standard deviation between replicate experiments.
To further investigate the efficacy of GSK690693 in another preclinical model, we utilized heterozygous Pten knockout mice in a pure 129/Sv strain (12). In this model, all Pten+/− female mice develop multiple hyperplastic lesions in the endometrium starting at 3 mo of age. Complete loss of Pten expression is common in small early lesions, with consequent activation of Akt. At 5 to 9 mo of age, lesions progress from extensive atypical hyperplasia to in situ carcinomas. Locally invasive carcinomas, defined by clear myometrial/serosal invasion, occur in ~30% of the mice, and most animals succumb by 10 mo of age. Overall, characteristics of the tumors closely mimic the natural progression and the pathologic features of the endometrioid subtype of endometrial cancer in humans.
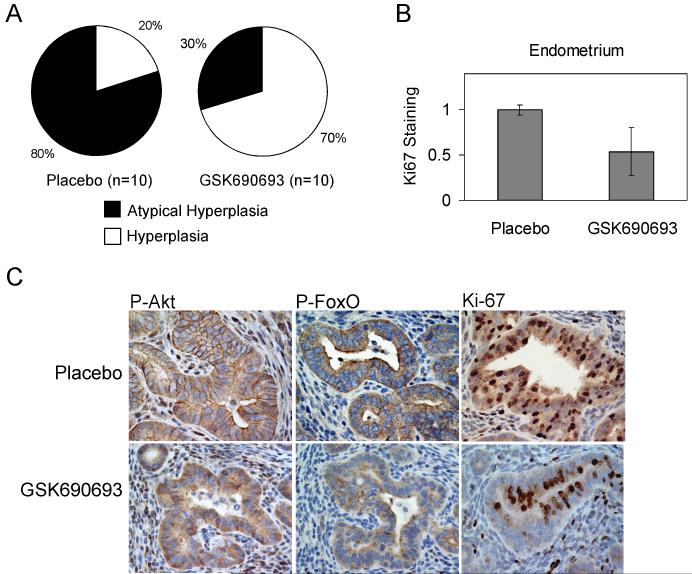
As summarized in Figure 4A, 80% of placebo-treated mice progressed to atypical endometrial hyperplasia, as compared to 30% of the GSK690693-treated mice. The group of atypical hyperplasias also contained more advanced cases that were classified as complex atypical hyperplasias. Further histopathologic assessment revealed that four mice in the placebo-treated group had possible carcinomas, in contrast to no mice in the treated group. Thus, as in Lck-MyrAkt2 mice, GSK690693 was found to be efficacious in a second mouse model genetically engineered to express activated Akt. Since no primary cell cultures were available from the Pten+/− mouse model, immunohistochemical staining was used to confirm reduced Ki-67 staining indicative of diminished cell proliferation (Fig. 4B) and down regulation of signaling downstream of Akt (Fig. 4C).
Fig. 4. GSK690693 delays endometrial tumor progression in Pten+/− knockout mice.
A, Pie charts depicting the percentage of mice that exhibited hyperplasia (20% in placebo vs. 70% in GSK690693-treated group) or that developed atypical hyperplasia (80% in placebo vs. 30% in GSK690693 group). Chi-Square test, p=0.03. B, Bar graph representing a significant difference between Ki-67 staining in placebo and GSK690693 mice (T-test, p=0.003) Stained and unstained cells from glandular endometrium from 5 fields of each of 5 placebo- and 5-GSK690693-treated mice were scored under a 40x objective (0.075 mm2 field), and percent positivity was normalized relative to staining in placebo mice. Error bars represent standard error. C, Immunohistochemical staining of endometrial neoplasms arising in Pten+/− knockout mice. Photographs were taken at 40x magnification. Like tumors from Lck-MyrAkt2 mice, P-Akt staining strongly localized to the cytoplasm and plasma membrane in placebo-treated mice, and was generally unchanged in treated mice. P-FoxO1/3 staining was cytoplasmic in placebo-treated mice (++ to +) and diminished (+ to +/−) in GSK690693-treated mice, and was sometimes nuclear.
Additionally, we employed a transgenic mouse model of spontaneous epithelial ovarian cancer, in which tumors are initiated by expression of the early region of Simian virus 40 (SV40) under transcriptional control of the 5′ upstream regulatory region of the Müllerian inhibiting substance type II receptor gene (MISIIR). Female TgMISIIR-TAg-DR26 transgenic mice develop bilateral ovarian tumors with variable latency and survive an average of 22 wks, and the tumors recapitulate the phenotype of human ovarian serous cystadenocarcinoma (13). At 9 to 14 wks of age, some tumors are still confined within the ovary, and strong immunoreactivity for Tag, P-Akt, P-mTor, and P-p70S6K are detected both in early ovarian lesions and more advanced tumors, consistent with activation of the Akt pathway (14).
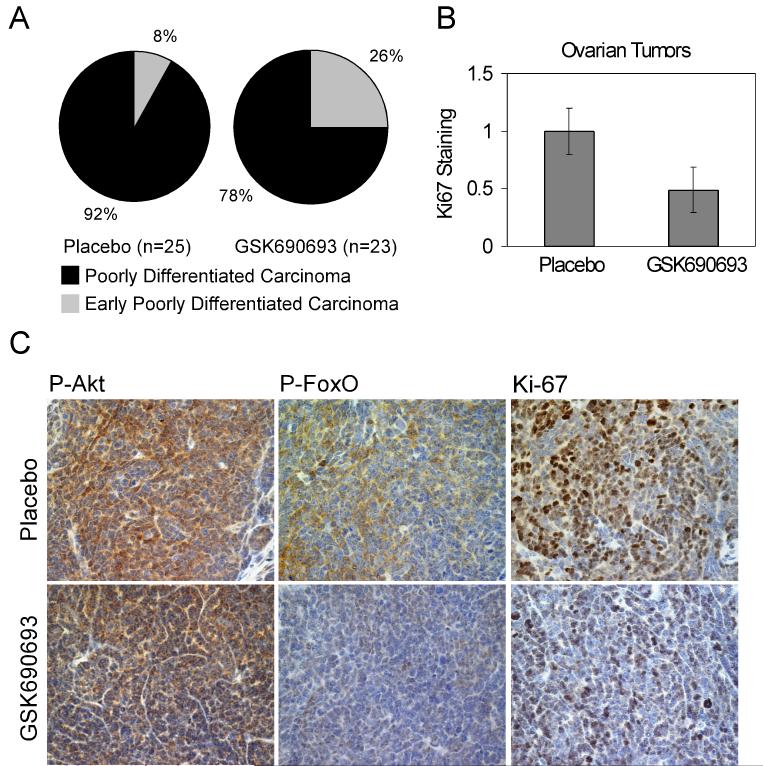
Overall, there was a tendency for GSK690693 to delay ovarian tumor progression in TgMISIIR-TAg-DR26 mice (Fig. 5A). All mice developed poorly differentiated ovarian carcinomas, although only 2 of 25 (8%) placebo-treated mice were interpreted to have early disease, whereas, 6 of 23 (26%) GSK690693-treated mice had early or very early disease. Although all mice exhibited histological evidence of bilateral disease, significantly more GSK690693-treated mice needed microscopic evaluation for detection of the tumors (16 of 46 ovarian tumors, 35%) compared to the placebo-treated mice (4 of 50 ovarian tumors, 8%) (Supplemental Table 1, Chi-Square test, p=0.003). Immunohistochemical staining showed diminished staining for Ki-67 and downstream P-FoxO1/3 (Fig. 5B, C).
Fig. 5. GSK690693 delays ovarian tumor progression in TgMISIIR-TAg-DR26 mice.
A, Pie charts depicting the percentage of mice that developed poorly differentiated carcinomas and the percent of mice with early disease, based on histopathological assessment. B, Bar graph representing a significant difference between Ki-67 staining in placebo and GSK690693 mice (T-test, p=0.029) Tumor cells from 5 fields of each of 5 placebo- and 5 GSK690693-treated mice were scored for positivity using a 20x objective (0.15 mm2 field), and values were normalized relative to staining in placebo mice. Error bars represent standard error. C, Immunohistochemical staining of ovarian tumors arising in TgMISIIR-TAg-DR26 transgenic mice. Photographs were taken at 40x magnification. Cytoplasmic staining of P-Akt was relatively unchanged in GSK690693-treated mice vs. placebo-treated mice. P-FoxO1/3 staining was modestly decreased (from ++/+ to + or +/−) in the cytoplasm of tumors from GSK690693-treated mice and was sometimes nuclear.
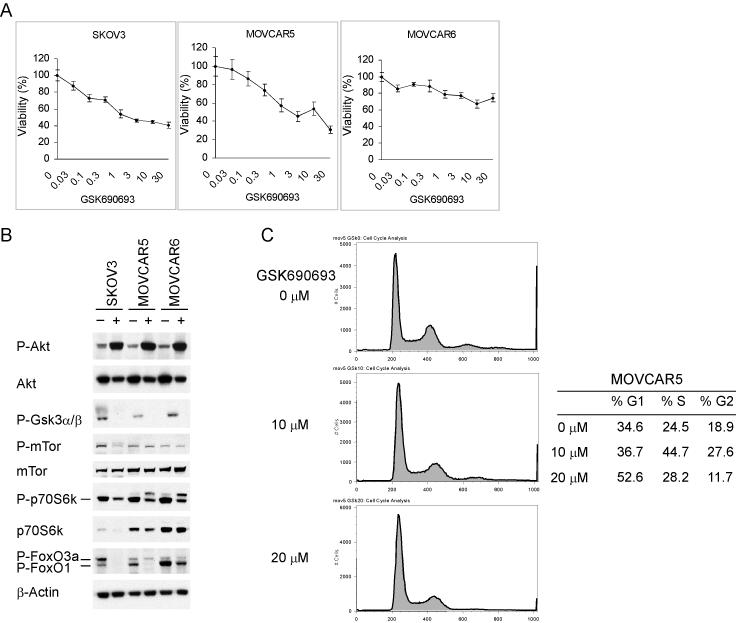
Thus, GSK690693 had a modest effect in delaying tumor development in the TgMISIIR-TAg-DR26 mice, perhaps due to the fact that tumor progression in this mouse model is compounded by deregulation of p53 and Rb due to the expression of large T antigen, in addition to activation of Akt via deregulation of the phosphatase PP2A by small t antigen (reviewed in 15). Moreover, compared to control human SKOV3 ovarian carcinoma cells (which are characterized by constitutive activation of AKT), one isolate of mouse ovarian carcinoma (MOVCAR5) cells was sensitive to GSK690693 and another isolate (MOVCAR6) was only marginally responsive to GSK690693 treatment as assessed by MTT assay (Fig. 6A). Even after 72 hrs of treatment, MOVCAR5 and MOVCAR6 cells did not exhibit a significant amount of apoptosis, although MOVCAR5 cells did exhibit ~50% increase in cell cycle arrest in G1 phase (Fig. 6C). These findings, along with the diminished Ki-67 staining in the GSK690693-treated tumors, suggest that response to the drug in ovarian tumor cells from TgMISIIR-TAg mice occurs via inhibition of cell cycle progression. Immunoblotting of ovarian tumor cells with phospho-specific antibodies following overnight treatment of tumor cells with 10 μM GSK690693 showed that MOVCAR cells and control SKOV3 cells exhibited decreased expression of P-Gsk3, P-FoxO1 and P-p70S6k with a lesser effect on P-FoxO3a and P-mTor (Fig. 6B).
Fig. 6. GSK690693 inhibits cell viability, in part through cell cycle arrest, and down regulates Akt signaling in ovarian tumor cells from a subset of TgMISIIR-TAg-DR26 mice.
A, Murine ovarian carcinoma cells (MOVCAR5 and MOVCAR6) and control human SKOV3 ovarian tumors cells were treated with various concentrations of GSK690693 for 72 hrs and analyzed for cell viability by MTT assays. The IC50 was ~3 μM GSK690693 for MOVCAR5 and SKOV3 cells, whereas, MOVCAR6 cells did not reach an IC50 with the drug concentrations used in this experiment. Error bars depict total standard deviation among replicate samples. B, Western blot analysis of MOVCAR5, MOVCAR6 and SKOV3 cells treated overnight with 10 μM GSK690693. Representative panels were screened with antibodies against components of the Akt signaling cascade to detect diminished phosphorylation of downstream targets. C, MOVCAR5 cells, but not the more resistant MOVCAR6 cells (not shown), exhibited cell cycle arrest in response to GSK690693. Cells were treated with 0, 10 and 20 μM GSK690693 for 72 hrs, and representative FACS profile and percentage of cells in G1, S and G2/M are shown.
Discussion
Akt was first identified as an oncogene transduced by a murine retrovirus that induced thymic lymphomas (17), and AKT kinases are frequently hyperactivated in human solid tumors and hematologic malignancies (reviewed in 18). Our data demonstrate that AKT inhibition with GSK690693 delays tumorigenesis in several preclinical models of spontaneously arising tumors in genetically defined mice. Although GSK690693 treatment did not reduce tumor incidence, it did result in fewer mice with advanced disease.
Importantly, we did not use the same treatment regimen across all of the genetically defined mouse models, because each was known to develop spontaneous tumors with different latencies. For example, Lck-MyrAkt2 mice from founder line 55 develop aggressive thymic lymphomas with a median latency of 16 wks of age (10). Consequently, we initiated treatments at 8 wks of age and continued for 4 wks duration, when a significant subset of untreated mice started exhibiting difficulty in breathing due to the presence of large thymic lymphomas that could constrict the heart and lungs. Interestingly, GSK690693 was most effective in delaying tumor progression in this mouse model, even though the thymic lymphocytes expressed a membrane-bound, constitutively active form of Akt2 that is not dependent on upstream signaling by PI3K or Pten functionality. Previously, we have proposed that thymic lymphomas arising in these mice have a strong dependence on Akt2 for survival of the tumor cells (10). Treatment with GSK690693 delayed tumor progression, as evidenced by a dramatic change in histopathology from the presence of thymic lymphomas in ~90% of the placebo-treated mice to a prevalence for hyperplasia or normal health in ~60% of the GSK690693-treated mice. Caliper measurements of thymic lymphomas arising in the remaining ~40% of the GSK690693-treated mice revealed that tumor volume was decreased by more than 2-fold compared to thymic lymphomas arising in placebo-treated mice.
A 30 mg/kg dose was used for all three models, although the schedule varied. We have previously reported the pharmacokinetic/pharmacodynamic (PK/PD) relationship of GSK690693 in mice bearing subcutaneous xenograft models (3). As reported, the maximum concentration (Cmax) was ~1 hr or earlier with a very short half-life in mice, and almost all the drug is gone from circulation ~8 hrs after the intra-peritoneal administration. No accumulation of drug was observed after repeat daily administration and as such, the PK/PD relationship shown after a single dose is a fair reflection of events after repeat dosing. As reported before, >3 μM concentration of GSK690693 in vivo was associated with sustained decrease in GSK3-β phosphorylation in vivo for up to 8 hrs (3).
Pten+/− mice required the longest duration of treatment with GSK690693 relative to other preclinical models tested here. Because the hyperplastic lesions in the endometrium could be observed starting at 3 mo of age, with progression to atypical hyperplasia and in situ carcinomas at 5 to 9 mo of age (12), treatment of Pten+/− knockout mice with GSK690693 was started at 5 mo of age and consisted of 3 cycles of 3 wks of i.p. injections, followed by 1 wk rest. Like the Lck-MyrAkt2 mouse model, immunohistochemical evidence supports the fact that Akt is strongly activated in this knockout model, as demonstrated by the strong staining for P-Akt in the cytosol and plasma membrane. This preclinical model also exhibited a strong response to GSK690693 in that there was a shift in histology from the atypical hyperplasias that were observed in 80% of the placebo-treated mice to an earlier hyperplastic phenotype in the tumor progression cascade that was detected in 70% of the GSK690693-treated mice. Although increased apoptosis was not observed in tumors from GSK690693-treated Pten+/− mice, Ki-67 staining was significantly diminished, indicating that inhibition of cell proliferation is a primary response to GSK690693 in this mouse model.
In TgMISIIR-TAg-DR26 mice, 50% of females show ovarian tumors by 6–13 wks of age (13), and in the present study, we wanted to determine the efficacy of GSK690693 as a therapeutic agent. Thus, treatment of TgMISIIR-TAg-DR26 mice with GSK690693 was initiated at 14 wks and continued for 4 wks duration. In contrast, in our previous chemoprevention strategy with RAD001, treatment of TgMISIIR-TAg-DR26 mice was initiated at 5 wks of age and continued for 20 wks (14). Tumor delay in our previous chemoprevention study was quite striking using this preclinical model. However, a therapeutic strategy is more relevant to the current situation in the clinic, because a chemoprevention approach has yet to be established for ovarian cancer. Overall, all placebo- and GSK690693-treated mice developed bilateral poorly differentiated ovarian carcinomas, although more early tumors were observed in the GSK690693-treated mice. In fact, unlike the situation in placebo-treated mice, a significant subset of tumors in GSK690693-treated mice required microscopic evaluation in order to be detected. This is consistent with our findings of decreased Ki-67 staining in tumors from GSK690693-treated mice and the induction of G1 arrest in MOVCAR5 cells treated in vitro with GSK690693. Thus, as in the other mouse models tested, decreased cell cycle progression appears to be the predominant effect of GSK690693 in TgMISIIR-TAg mice.
Measurement of downstream substrate phosphorylation represents an important means of assessing drug response on AKT activity. Our findings that P-FoxO1/3 cytoplasmic staining is reduced and that nuclear staining is sometimes observed in GSK690693-treated tumors from all three mouse models is consistent with previous reports demonstrating that treatment of U2OS cells led to nuclear accumulation of FoxO (3). Moreover, we observed nuclear translocation of P-FoxO1/3 signal in normal ovarian tissue in response to GSK690693 in mice. Similarly, the effect of GSK690693 on GSK3-beta phosphorylation, another downstream readout of AKT activity, in normal liver was described in an earlier publication (6).
In fact, GSK690693 caused a dose-dependent reduction in the phosphorylation state of multiple proteins downstream of Akt such as P-Gsk3α/β, P-mTor and P-p70S6k in tumor cells, in accordance with previous reports (3). However, GSK690693 treatment also resulted in a dose-dependent increase in the phosphorylation of Akt (3). An increase in AKT phosphorylation at both Ser-473 and Thr-308 sites was observed with GSK690693, consistent with the feedback mechanism observed previously with this and other AKT kinase inhibitors (3, 19). Up regulation of P-Akt levels is not unique to GSK690693, in that rapamycin and related mTORC1 inhibitors (20), as well as another AKT inhibitor, A-443654 (19), have been shown to enhance the activation of Akt via a feedback mechanism. It has been suggested that S6K-induced IRS-1 phosphorylation and mTORC2 are involved in this feedback mechanism. The up regulation of P-Akt by GSK690693 was not sufficient to rescue the downstream substrate phosphorylation.
As previously reported, GSK690693 treatment in cell culture results in some increase in apoptosis in LNCaP and BT474 cells at 24–48 hrs (3, 4). GSK690693 treatment also inhibited proliferation of a subset of tumor cell lines in vitro and inhibited growth of tumor xenografts in mice (3). Further analysis of the molecular mechanisms of GSK690693 action in cells is being investigated using phospho-proteomics and transcriptomics. Preliminary results show a predominant activation of cell cycle arrest genes with weak evidence for up regulation of proapoptotic pathways. These studies are being extended to multiple cell lines and xenografts to better understand the heterogeneity of responses (21). Collectively, our data with tumor-prone genetically engineered mice and derived tumor cells confirm previous studies that suggest that inhibition of AKT kinases regulates both cell proliferation and apoptotic pathways, although the primary effect appears to be anti-proliferative in the cell lines and xenografts evaluated thus far.
The testing of GSK690693 in various models is important to address its overall potential utility in different tumors and tumor cell contexts. One cautionary note is that, in addition to the potent inhibition of Akt kinases, GSK690693 at higher concentrations can inhibit novel PKCs, PKCβ1, PAK-4,5,6, PKA, PKG1β and PrkX, which can potentially contribute to the overall anti-tumor effect through inhibition of cell proliferation and transformation (3).
Overall, GSK690693 exhibited its greatest efficacy in tumors and tumor-derived cell lines in which there was specific, targeted deregulation of the Akt kinase, i.e., those expressing myristylated, constitutively active Akt or loss of the Pten tumor suppressor protein. It is postulated that tumor cells that have an addiction for strong constitutive activation of Akt may be more sensitive to inhibition of the pathway. For example, early evidence from our laboratory suggests that thymic lymphoma cells derived from Lck-MyrAkt2 mice also are sensitive to downstream mTOR inhibition by rapamycin, as demonstrated by strong down regulation of P-p70S6k and P-4EBP1. As with GSK690693, rapamycin and its derivatives may be able to induce apoptosis under certain conditions, but the primary mechanism is to induce cell cycle arrest. Side-by-side preclinical comparisons between an AKT inhibitor such as GSK690693 and an mTOR inhibitor such as RAD001 are needed to address whether these inhibitors exhibit equivalent efficacy.
In vitro studies of primary tumor cell cultures were consistent with the in vivo findings in the corresponding mouse models, and may help to explain the responsiveness of one model versus another. For example, in thymic lymphoma cell cultures from Lck-MyrAkt2 mice, treatment with GSK690693 was efficacious, and it is noteworthy that tumor cell cultures from multiple Lck-MyrAkt2 founder 55 mice have identical karyotypic findings, i.e., a specific recurrent chromosomal translocation (10). On the other hand, variable responses to GSK690693 were observed in MOVCAR cell lines from TgMISIIR-TAg mice, perhaps complicated by the fact that we have found that these cell cultures have variable cytogenetic findings, most likely attributed to the potential genetic instability that would be expected as a result of perturbation of the p53 and pRb pathways due to the expression of SV40 large T antigen (reviewed in 22). Variable responses to drug treatments in independent tumor cell lines derived from the same animal model, either Lck-MyrAkt2 or TgMISIIR-TAg. Thus, the predisposing genetic modification in these tumor-prone mouse models may be accompanied by additional variable genetic and expression changes that influence tumor cell growth and chemosensitivity.
Of importance to this study, we have shown the utility of different genetically tumor-prone mouse models for the preclinical evaluation of a small molecule inhibitor that targets the Akt signaling. A side-by-side comparison of GSK690693 in three different mouse models and in independently derived tumor cells derived from these mice showed that this class of inhibitor may have efficacy in delaying tumor growth and/or progression. Through preclinical testing of thymic lymphomas, endometrial and ovarian tumor models, our results provide rationale for the potential usefulness of GSK690693 in therapeutic trials.
Supplementary Material
Acknowledgements
Special thanks to Dr. Denise Connolly at Fox Chase Cancer Center for the gift of TgMISIIR-TAg mice and for suggestions concerning manuscript preparation. The following Fox Chase Cancer Center/Ovarian SPORE shared facilities were used in the course of this work: Laboratory Animal Facility, Biomarker and Genotyping, Histopathology, Cell Culture, and Flow Cytometry and Cell Sorting Core Facilities.
Grant Support: Grant support provided by National Cancer Institute Grants CA77429 (J.R. Testa), CA83638 (SPORE in Ovarian Cancer), CA06927 (core grant), and CA97097 (A. Di Cristofano); a research contract from GlaxoSmithKline; and an appropriation from the Commonwealth of Pennsylvania. D.A. Altomare was supported by the Liz Tilberis Scholar Program, funded by the Ovarian Cancer Research Fund, Inc.
Abbreviations
- Akt1s1
Akt1 substrate 1 (proline-rich), human synonym PRAS40 for proline-rich Akt substrate 40 kDa
- GSK3
glycogen synthase kinase 3
- MISIIR
Mullerian inhibiting substance type II receptor
- MOVCAR
mouse ovarian carcinoma
- mTOR
mammalian target of rapamycin
- p70S6k
p70 S6 kinase
- PI3K
phosphatidylinositol 3-kinase
- PP2A
protein phosphatase 2A
- PD
pharmacodynamic
- PK
pharmacokinetic
- SV40
simian virus 40
- Tag
SV40 large T-antigen
- tag
SV40 small t-antigen
Footnotes
Statement of Translational Relevance
We hypothesized that targeted inhibition of AKT, an important mediator of cell signaling pathways considered to be hallmarks of cancer, can impede tumor growth and progression. Three different genetically-defined mouse models that develop spontaneous thymic lymphoma, endometrial carcinoma or ovarian cancer showing hyperactivation of Akt were used to test a novel pharmaceutical agent, GSK690693, which directly targets Akt activity. GSK690693 was found to have efficacy in each of these preclinical models. Moreover, immunohistochemical analysis of tumor specimens and experiments on tumor-derived cell cultures demonstrated that phosphorylation of downstream effectors of Akt were inhibited in vivo and in vitro, respectively, in response to GSK690693. These results are translational because they indicate that GSK690693 or other inhibitors of this class of drug might have therapeutic efficacy in human cancers with hyperactivated AKT and/or a dependence on AKT signaling for tumor progression.
References
- 1.Altomare DA, Testa JR. Perturbations of the AKT signaling pathway in human cancer. Oncogene. 2005;24:7455–64. doi: 10.1038/sj.onc.1209085. [DOI] [PubMed] [Google Scholar]
- 2.Heerding DA, Rhodes N, Leber JD, et al. Identification of 4-(2-(4-amino-1,2,5-oxadiazol-3-yl)-1-ethyl-7-{[(3S)-3-piperidinylmethyl]oxy}-1H-imidazo[4,5-c]pyridin-4-yl)-2-methyl-3-butyn-2-ol (GSK690693), a novel inhibitor of AKT kinase. J Med Chem. 2008;51:5663–79. doi: 10.1021/jm8004527. [DOI] [PubMed] [Google Scholar]
- 3.Rhodes N, Heerding DA, Duckett DR, et al. Characterization of an Akt kinase inhibitor with potent pharmacodynamic and antitumor activity. Cancer Res. 2008;68:2366–74. doi: 10.1158/0008-5472.CAN-07-5783. [DOI] [PubMed] [Google Scholar]
- 4.Levy DS, Kahana JA, Kumar R. AKT inhibitor, GSK690693, induces growth inhibition and apoptosis in acute lymphoblastic leukemia cell lines. Blood. 2009;113:1723–9. doi: 10.1182/blood-2008-02-137737. [DOI] [PubMed] [Google Scholar]
- 5.Lo Russo PM, Hurwitz HI, Chiorean EG, et al. AKT inhibitor GSK690693: Preliminary results from the first time in human study; Proc 99th Annu Meet AACR; San Diego, CA. 2008; Abstract LB-68. [Google Scholar]
- 6.Crouthamel MC, Kahana JA, Korenchuk S, et al. Mechanism and management of AKT inhibitor-induced hyperglycemia. Clin Cancer Res. 2009;15:217–25. doi: 10.1158/1078-0432.CCR-08-1253. [DOI] [PubMed] [Google Scholar]
- 7.Malstrom S, Tili E, Kappes D, Ceci JD, Tsichlis PN. Tumor induction by an Lck-MyrAkt transgene is delayed by mechanisms controlling the size of the thymus. Proc Natl Acad Sci USA. 2001;98:14967–72. doi: 10.1073/pnas.231467698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rathmell JC, Elstrom RL, Cinalli RM, Thompson CB. Activated Akt promotes increased resting T cell size, CD28-independent T cell growth, and development of autoimmunity and lymphoma. Eur J Immunol. 2003;33:2223–32. doi: 10.1002/eji.200324048. [DOI] [PubMed] [Google Scholar]
- 9.Tan Y, Timakhov RA, Rao M, et al. A novel recurrent chromosomal inversion implicates the homeobox gene Dlx5 in T-cell lymphomas from Lck-Akt2 transgenic mice. Cancer Res. 2008;68:1296–302. doi: 10.1158/0008-5472.CAN-07-3218. [DOI] [PubMed] [Google Scholar]
- 10.Timakhov RA, Tan Y, Rao M, et al. Recurrent Chromosomal Rearrangements Implicate Oncogenes that Contributing to T-Cell Lymphomagenesis in Lck-MyrAkt2 Transgenic Mice. Genes Chromosomes Cancer. 2009;48:786–94. doi: 10.1002/gcc.20683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu J, Testa JR. DLX5 (distal-less homeobox 5) promotes tumor cell proliferation by transcriptionally regulating MYC. J Biol Chem. 2009;284:20593–601. doi: 10.1074/jbc.M109.021477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vilgelm A, Lian Z, Wang H, et al. Akt-mediated phosphorylation and activation of estrogen receptor alpha is required for endometrial neoplastic transformation in Pten+/- mice. Cancer Res. 2006;66:3375–80. doi: 10.1158/0008-5472.CAN-05-4019. [DOI] [PubMed] [Google Scholar]
- 13.Connolly DC, Bao R, Nikitin AY, et al. Female mice chimeric for expression of the simian virus 40 TAg under control of the MISIIR promoter develop epithelial ovarian cancer. Cancer Res. 2003;63:1389–97. [PubMed] [Google Scholar]
- 14.Mabuchi S, Altomare DA, Connolly DC, et al. RAD001 (Everolimus) delays tumor onset and progression in a transgenic mouse model of ovarian cancer. Cancer Res. 2007;67:2408–13. doi: 10.1158/0008-5472.CAN-06-4490. [DOI] [PubMed] [Google Scholar]
- 15.Arroyo JD, Hahn WC. Involvement of PP2A in viral and cellular transformation. Oncogene. 2005;24:7746–55. doi: 10.1038/sj.onc.1209038. [DOI] [PubMed] [Google Scholar]
- 16.Gallion HH, Pieretti M, DePriest PD, van Nagell JRJ. The molecular basis of ovarian cancer. Cancer. 1995;76:1992–7. doi: 10.1002/1097-0142(19951115)76:10+<1992::aid-cncr2820761315>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 17.Staal SP, Hartley JW, Rowe WP. Isolation of transforming murine leukemia viruses from mice with a high incidence of spontaneous lymphoma. Proc Natl Acad Sci USA. 1977;74:3065–7. doi: 10.1073/pnas.74.7.3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bellacosa A, Kuman CC, Di Cristofano A, Testa JR. Activation of AKT kinases in cancer: implications for therapeutic targeting. Adv Cancer Res. 2005;94:29–86. doi: 10.1016/S0065-230X(05)94002-5. [DOI] [PubMed] [Google Scholar]
- 19.Han EK, Leverson JD, McGonigal T, et al. Akt inhibitor A-443654 induces rapid Akt Ser-473 phosphorylation independent of mTORC1 inhibition. Oncogene. 2007;26:5655–61. doi: 10.1038/sj.onc.1210343. [DOI] [PubMed] [Google Scholar]
- 20.O’Reilly KE, Rojo F, She QB, et al. mTOR inhibition induces upstream receptor tyrosine kinase signaling and activates Akt. Cancer Res. 2006;66:1500–8. doi: 10.1158/0008-5472.CAN-05-2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar R, Blakemore SJ, Ellis CE, et al. Causal reasoning identifies mechanisms of sensitivity for a novel AKT kinase inhibitor, GSK690693; Proc 100th Annu Meet AACR; Denver, CO. 2009; Abstract 4389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barbanti-Brodano G, Sabbioni S, Martini F, Negrini M, Corallini A, Tognon M. Simian virus 40 infection in humans and association with human diseases: results and hypotheses. Virology. 2004;318:1–9. doi: 10.1016/j.virol.2003.09.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.