Abstract
Purpose
Pharmacological concentrations of ascorbate may be effective in cancer therapeutics. We hypothesized that ascorbate concentrations achievable with intravenous dosing would be cytotoxic in pancreatic cancer where the five-year survival is < 3%.
Experimental Design
Pancreatic cancer cell lines were treated with ascorbate (0, 5, and 10 mM) for one hour, then viability and clonogenic survival were determined. Pancreatic tumor cells were delivered subcutaneously into the flank region of nude mice and allowed to grow at which time they were randomized to receive either ascorbate (4 g/kg) or osmotically equivalent saline (1 M) i.p. for two weeks.
Results
There was a time and dose-dependent increase in measured H2O2 production with increased concentrations of ascorbate. Ascorbate decreased viability in all pancreatic cancer cell lines, but had no effect on an immortalized pancreatic ductal epithelial cell line. Ascorbate decreased clonogenic survival of the pancreatic cancer cell lines, which was reversed by treatment of cells with scavengers of H2O2. Treatment with ascorbate induced a caspase-independent cell death that was associated with autophagy. In vivo, treatment with ascorbate inhibited tumor growth and prolonged survival.
Conclusions
These results demonstrate that pharmacological doses of ascorbate, easily achievable in humans, may have potential for therapy in pancreatic cancer.
Keywords: Pancreatic cancer, hydrogen peroxide, antioxidants
INTRODUCTION
Pancreatic cancer is the 4th most common cause of cancer death in the United States with 33,000 fatal cases annually in the United States alone (1). Surgical resection of the primary tumor remains the only potentially curative treatment for pancreatic cancer. However, in population-based studies the number of patients undergoing resection with curative intent can be less than 3% (2). Even after resection, median survival is only 12–18 months and less than 20% of resected patients survive 5 years. The majority of patients die of metastatic cancer recurrence (3). Other adjuvant treatments such as radiation therapy and chemotherapy have not significantly improved long-term survival. The rate of chemotherapeutic response is less than 20% (4), while less than 10% of patients benefit from radiation therapy (3). Because of the lack of therapeutic responsiveness of pancreatic cancer to surgery, chemotherapy, and radiation therapy, survival beyond five years is rare with median survival less than six months. Thus, novel and effective therapies directed against pancreatic cancer are needed to control progression and metastatic disease.
Pharmacologic ascorbate concentrations have been shown to selectively kill some cancer cell types (5). Cell death was independent of metal chelators and dependent on H2O2 formation. H2O2 generation was dependent on ascorbate concentration, incubation time, and displayed a linear relationship with ascorbate radical formation, ascorbate being the electron-donor (6). Thus, pharmacologic ascorbate concentrations producing extracellular H2O2 diffuses into cells causing cell death.
Chen and colleagues have hypothesized that pharmacological ascorbate may deplete ATP three mechanisms which would lead to cell death in tumors (6). First, DNA damage induced by H2O2 can activate PARP. The activated PARP catabolizes NAD+, thereby depleting substrate for NADH formation and subsequent ATP synthesis (7,8). Secondly, H2O2 can be catabolized by concurrent oxidation of glutathione (GSH) to glutathione disulfide (GSSG). In reducing GSSG back to GSH, glutathione reductase utilizes NADPH, which is provided by the pentose shunt from glucose. Glucose used to reduce NADP+ to NADPH cannot be used for glycolysis or NADH-production so that ATP generation is decreased (9,10). Finally, H2O2 could directly damage mitochondria, especially ATP synthase, so that ATP production decreases (11,12,13).
Recent studies have also suggested that ascorbate may lead to death through a unique caspase-independent autophagy pathway (14). Autophagy is characterized by the activation of a conserved biochemical pathway that results in the formation of double membrane organelles that initially engulf cellular proteins and cytoplasmic organelles and subsequently fuse with lysosomes to facilitate the degradation of these components. Activation of this pathway is characterized by the biochemical processing of Light Chain 3 (LC3), which results in altered size of the protein and a redistribution of the protein. Activation of this pathway can either inhibit or promote cell death, depending on the cellular context. Anticancer drugs may induce both apoptosis and autophagy separately or simultaneously (15,16,17). In a recent study by Ohtani et al., ascorbate in conjunction with the tumor suppressor gene 101F6 initiated autophagy, as determined by induction of acidic vesicular organelles and LC3 formation (14).
The goal of our study was to determine whether ascorbate is cytotoxic to pancreatic cancer cells and if so, to characterize the mechanism of ascorbate-induced cytotoxicity. Our results demonstrate that ascorbate decreased clonogenic survival and cell viability. Although ascorbate decreased ATP levels in pancreatic cancer cell lines in a dose-dependent manner, this depletion may not play a role in ascorbate-induced cytotoxicity. Overexpression of extracellular and intracellular catalase reversed ascorbate-induced cytotoxicity. Treatment with ascorbate did not induce PARP cleavage and caspase inhibition did not reverse ascorbate-induced cell death. Ascorbate did induce the processing and activation of LC3, a hallmark of autophagy. In mice with pre-established pancreatic tumors, systemic treatment with pharmacological ascorbate treatment inhibited tumor growth and prolonged survival.
MATERIALS AND METHODS
Cell culture
MIA PaCa-2, AsPC-1, and BxPC-3 human pancreatic adenocarcinoma cells were obtained from American Type Culture Collection (Manassas, VA). MIA PaCa-2 was maintained in Dulbecco modified Eagle medium supplemented with 10% fetal bovine serum and 2.5% horse serum. AsPC-1 was maintained in RPMI 1640 with 20% bovine serum and 1% sodium pyruvate. BxPC-3 was maintained in RPMI 1640 with 10% fetal bovine serum. In addition, we used an immortalized cell line derived from normal pancreatic ductal epithelial with near normal genotype and phenotype of pancreatic duct epithelial cells HPV16-E6E7 (H6c7), and the isogenic cell line that expresses K-rasG12V H6c7eR-Kras+ (18). These cell lines were maintained in keratinocyte serum free media and supplemented with epidermal growth factor and bovine pituitary extract as previously described (19). To determine the role of mitochondrial oxidative phosphorylation in ascorbate-induced cytotoxicity MIA PaCa-2 rho° cells, depleted of mitochondria DNA (mtDNA), were generated by incubating wild type cells (rho+) for 6–8 weeks with 100 ng/mL ethidium bromide. The medium was supplemented with 4.5 mg/mL glucose, 50 μg/mL uridine, and 100 μg/mL pyruvate to compensate for the respiratory metabolism deficit as described (20). After selection, the MIA PaCa-2 rho° cells were cultured in the above specified medium without ethidium bromide. To verify the mtDNA depletion, PCR demonstrated absence of mtDNA in rho° cells as described (19). All media was obtained from Invitrogen (Carlsbad, CA) and all cell lines were maintained at 37°C in 5% CO2. All cells were routinely tested for mycoplasma and only utilized when found to be negative.
Clonogenic cell survival experiments
At the beginning of each experiment, cells were rinsed with phosphate-buffered saline (PBS) and placed in media. Cells were treated with ascorbate (0–20 mM) from a stock solution of 1.0 M ascorbate, (pH 7.0) which was made under argon and stored in a volumetric flask with a tight-fitting stopper at 4 °C. Ascorbate concentration was checked at 265 nm, ε = 14,500 M−1cm−1. The solution can be kept for several weeks without significant loss of ascorbate due to the lack of oxygen (21). Cells were treated with ascorbate for 1 h at 37° C. Cells were then trypsinized, counted, diluted and plated for clonogenic cell survival assay as previously described (22). Surviving colonies were fixed and stained after 10–14 days and counted under a dissecting microscope.
Cell viability
As an indicator of cell metabolic viability, the MTT assay was used. Cells were seeded at 1 × 104 in a 96-well plate in full media. After 48 h, cells were treated with ascorbate for one h. For the cell viability experiments, all cell lines were treated in DMEM media for consistency. Then the cells were washed with PBS and incubated with fresh media for an additional 24 h. MTT (3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide) (Sigma, St. Louis, MO) 1 mg/mL was added to the wells and incubated at 37°C for 3 h. At the end of incubation, media was removed and 100 μL of DMSO was added to each well for cell lysis. The plate was read at 590 nm on a Tecan SpectraFluor Plus plate reader (Tecan, Research Triangle Park, NC).
Measurement of H2O2 with oxygen electrode
Ascorbate interferes with many of the standard methods to measure H2O2 especially peroxidase-based methods (23). H2O2 was measured using an oxygen electrode (Oxygen monitor system, Yellow Springs, OH). The oxygen electrode was stabilized for 15 min with 3.00 mL of air-saturated DMEM-10% FBS in the chamber. The medium was replaced by 3 mL of medium containing various concentrations of ascorbate and the recorder pen adjusted to a position 50% of full-scale deflection. Catalase solution (1000 units/mL) was injected through the cap and H2O2 concentration calculated from the “spike” of O2 evolution.
Measurement of intracellular ATP levels
Cells were grown in 60-mm tissue culture dishes for 48 h before ascorbate treatment. Intracellular ATP was measured with a luciferase-based somatic ATP assay kit (Sigma, St. Louis, MO). Briefly, cells were twice washed with PBS after exposure to ascorbate, and 400 μL of somatic cell ATP-releasing agent were added directly to the dishes. After incubating for 5 min, samples were transferred to microcentrifuge tubes and cleared by centrifugation. Supernatant (100 μL) was added to a 96-well tissue culture plate with equal volumes of ATP assay mix working solution added immediately before measuring luminescence. Luminescence was measured with Tecan Spectra Fluor Plus plate reader (Tecan, Research Triangle Park, NC). ATP levels were expressed as a percentage of control values. In addition to measurement of ATP levels, NADP+/NADPH concentrations in MIA PaCa-2 cells were determined by using EnzyChrom NADP+/NADPH assay kit (BioAssay Systems, Hayward, CA). The kit is based on a glucose dehydrogenase cycling reaction, in which a tetrazolium dye (MTT) is reduced by NADPH in the presence of phenazine methosulfate. The intensity of the reduced product color is proportionate to the NADP+/NADPH concentration in the sample.
Treatment of cells with catalase
To determine whether H2O2 was responsible for the cytotoxic effects of ascorbate, cells were treated with various catalase preparations including bovine catalase in the media (100 μg/mL) or catalase-polyethylene glycol (PEG-CAT) (200 units/mL). Catalase and PEG-catalase were purchased from Sigma (St. Louis, MO). Pancreatic cancer cells were also infected with adenovirus constructs containing the catalase enzymes. The adenovirus constructs used were replication-defective, E1- and partial E3 deleted recombinant adenovirus (20). Inserted into the E1 region of the adenovirus genome are the human catalase genes (CAT, mitCAT) both of which are driven by a cytomegalovirus promoter. The AdCAT construct was originally prepared by John Engelhardt, University of Iowa (24). The AdmitCAT construct was originally prepared by Dr. Andres Melendez with the full-length catalase cDNA combined with the MnSOD mitochondrial leader sequence added to the construct (25). Approximately 106 MIA PaCa-2 cells were plated in 10 mL of complete media in a 100-mm2 plastic dish and allowed to attach for 24 h. Cells were then washed three times in serum- and antibiotic-free media. The adenovirus construct(s) (100 MOI), suspended in 3% sucrose, was then applied to cells suspended in 4 mL of serum-and antibiotic-free media. Control cells are treated with the adenovirus-empty construct. Cells were incubated with the adenovirus constructs for 24 h. Media was then replaced with 4 mL of complete media for an additional 24 h before cells were harvested.
Cell homogenization
Cells were washed three times in PBS (pH 7.0), scraped from the dishes using a rubber policeman, and then collected in phosphate buffer (pH 7.8). This was followed by sonic disruption on ice for 30 s in 10-s bursts using a VibraCell sonicator (Sonics and Materials Inc., Danbury, CT) at 100% power. Protein concentration was determined using the Bio-Rad Bradford dye binding protein assay kit (Hercules, CA) according to the manufacturer’s instructions.
Western Blot analysis
Immunoreactive protein corresponding to catalase was identified and quantified from total cell protein by the specific reaction of the immobilized protein with its antibody. Protein (10 to 40 μg) was electrophoresed in a 4~20 % Bio-Rad ready gel. The proteins were then electotransferred to Immobilon Transfer Membranes (Millipore, Bedford, MA). After blocking in 5% nonfat milk for 1 h, the membranes were treated with anti-catalase antibody (1:5000 dilution, Santa Cruz Biotechnology, Santa Cruz, CA), anti-PARP antibody (1:1000, Cell Signaling Technology, Danvers, MA), polyclonal rabbit anti-PAR antibody (1:3000 dilution, BD Biosciences, San Jose, CA), or anti-LC3 antibody (1:1000, MBL International, Woburn, MA). Horseradish peroxidase-conjugated goat anti-rabbit (1:50,000 dilution) secondary antibody was from Chemicon International (Temecula, CA). The washed blots were then treated with SuperSignal West Pico Chemiluminescent Substrate (Thermo Scientific, Rockford, IL) and exposed to Classic Blue Autoradiography Film (MIDSCI, St. Louis, MO). All western blots were performed in duplicate.
Cell death measurements
Phosphatidylserine translocation to the outer leaflet of the plasma membrane was assessed by reaction with Annexin V-FITC apoptosis detection kit (BioVision, Mountain View, CA) and detected by a FACScan flow cytometer. MIA PaCa-2 cells (1 × 106 cells) were treated with varying doses of ascorbate and after 48 h, cells were harvested, washed with PBS, and resuspended in 500 μL of binding buffer (10 mM HEPES, pH 7.4, 140 mM NaCl, 2.5 mM CaCl2). Cells were then incubated with 5 μL of Annexin V conjugated with FITC plus 5 μg/mL propidium iodide and incubated for 5 min at room temperature in the dark. Samples were then analyzed by flow cytometry to identify apoptotic and necrotic cells.
LC3-GFP MIA PaCa-2 cells
The pTZV3 Hygro-LC3-GFP plasmid was generated by cloning the LC3-GFP cDNA (obtained from Ana Marie Cuervo, Albert Einstein College of Medicine) into the pTZV3 vector (kind gift of Dr. Andrei Gudgov, Cleveland Clinic) in which the neomycin cassette was replaced with hygromycin. MIA PaCa-2 LC3-GFP cells were then generated using a HIV based lentiviral system with the pTZV3 LC3-GFP plasmid. HEK 293T cells were cultured in RPMI 1640 supplemented with 10% FBS, 2 mM L-glutamine, 100 units/mL penicillin, 100 μg/mL streptomycin, and 57 μM 2-mercaptoethanol at 37 °C with 5% CO2. These cells were transfected with both a 5 plasmid packaging mix (pTRE-GAG-PRO-PRE-polyA, pCMV-VpR-RT-IN-polyA, pCMV-VSV-G-polyA, pCMV-TEToff-polyA, and pCMV-TAT-REV) and the target plasmid pTZV3 Hygro-LC3-GFP as previously described (26). For each 75 cm2 flask used 3.75 μg of lentiviral packaging plasmids and 1.5 μg of target plasmid were resuspended in 300 μL of EC buffer and 42 μL of Enhancer, vortexed for 1 s, and incubated for 5 min at room temperature. Next, 100 μL of Effectene was added to the plasmid mix, vortexed for 20 s, and incubated at room temperature for 20 min. EC buffer, Enhancer, and Effectene were purchased from Qiagen, Valencia, CA. This transfection mix was used to transfect HEK 293T cells in fresh media. At 18 h post transfection virus particles were harvested from the HEK 293T cells by collecting the media and filtering with a 0.22 μm syringe filter (Millipore, Billerica, MA). This collected media was then used to infect the MIA PaCa-2 cells by direct addition to these cells. The transduction procedure was then repeated 5 times over the next 3 days. Cells expressing LC3-GFP were then selected with 400 μg/mL hygromycin (Invitrogen, Carlsbad, CA) for 10 days in culture.
Autophagy measurements
MIA PaCa-2 wild type or MIA PaCa-2 LC3-GFP cells were seeded at least two days prior to the ascorbate autophagy induction experiments to insure approximately 400,000 cells per well of a 6-well plate. Ascorbate (1, 2, or 5 mM) or H2O2 (0.2 mM) was added directly to each respective well and cells were then incubated for 1 h at 37°C in 5% CO2. Following treatment, media was removed, cells were washed with Hyclone DPBS, fresh media was then added and the cells were incubated for an additional 24 h at 37°C in 5% CO2. Following this incubation the media from each well was collected and each well was washed once with DPBS. The DPBS wash fraction was also collected and added to each respective media sample. Next, cells were harvested and centrifuged at ~1000 g for 5 min to concentrate the samples. Cells were resuspended and propidium iodide (PI) (1 μg/mL) was added prior to running on a flow cytometer to discriminate live cells. In general 5,000–10,000 events were collected to examine for both the percentage of GFP positive cells and the MFI of the GFP positive cells.
Confocal microscopy
Cells were grown on a coverslip that had been autoclaved and then coated with 0.001% poly-L-lysine. Cells were treated with ascorbate or H2O2 as described above. After washing, the cells were fixed with 4% fresh paraformaldehyde in DPBS at room temperature for approximately 25 min. The cells were washed two times with DPBS and then incubated with 75 μL of freshly diluted TO-PRO-3 (1:2000 in DPBS) for 5 min in the dark. The TO-PRO-3 was then removed by wicking away with a paper towel and the coverslips were then mounted onto a slide with 30 μL VECTASHIELD Mounting Medium with DAPI (Vector laboratories, Burlingame, CA). Excess mounting medium were removed and then sealed with finger nail polish. The samples were imaged with a confocal microscope equipped with a Kr/Ar laser. The LC3-GFP fluorescence was excited using the 488 nm laser line while the TOPRO-3 was excited with the 647 nm laser. Images were acquired at 1024 × 1024 pixels with a 60× 1.4NA oil immersion objective lens. Final images were prepared using Image J Software. All images utilized identical settings for acquisition and analysis.
Animal experiments
Thirty-day-old athymic nude mice were obtained from Harlan Sprague-Dawley (Indianapolis, IN). The nude mice protocol was reviewed and approved by the Animal Care and Use Committee of The University of Iowa. The animals were housed four to a cage and fed a sterile commercial stock diet and tap water, ad libitum. Animals were allowed to acclimate in the unit for one week before any manipulations were performed. Each experimental group consisted of 13 to 15 mice. MIA PaCa-2 tumor cells (2 × 106) were delivered subcutaneously into the flank region of nude mice with a 1-mL tuberculin syringe equipped with a 25-gauge needle. The tumors were allowed to grow until they reached between 3 mm and 4 mm in greatest dimension (from 10 days to 2 weeks), at which time treatment was initiated.
Mice were divided into two treatment groups that received 1 M NaCl i.p. (controls) b.i.d. for 14 days, or ascorbate 4 g/kg i.p b.i.d. for 14 days. This was defined as day 1 of the experiment. Tumor size was measured every two to three days by means of a vernier caliper, and tumor volume was estimated according to the following formula: tumor volume = π/6 × L x W2, where L is the greatest dimension of the tumor, and W is the dimension of the tumor in the perpendicular direction (22). Animals were killed by CO2 asphyxiation when the tumors reached a predetermined size of 1000 mm3 and this was considered the time to sacrifice.
Statistical Analysis
Statistical analysis was performed by means of Systat (Systat Inc., Evanston Ill). A single factor ANOVA, followed by post-hoc Tukey test, was used to determine statistical differences between means. All means were calculated from three experiments, and error bars represent standard error of mean (SEM). All western blots were repeated at least twice. All data are expressed as means ± SEM. For the in vivo studies, the statistical analyses focused on the effects of different treatments on cancer progression. The primary outcomes of interest were time to death and tumor growth over time. Once tumors were visible, the mice were then randomly assigned to a treatment group and followed until death or until the experiment was terminated. The log-rank test was used to compare the survival times between treatment groups. Kaplan-Meier survival plots were constructed to estimate survival. Tumor sizes (mm3) were measured throughout the experiments, resulting in repeated measurements across time for each mouse. Linear mixed effects regression models were used to estimate and compare the group-specific tumor growth curves. All tests were two-sided and carried out at the 5% level of significance. Analyses were performed with the SAS and R statistical software package.
RESULTS
Ascorbate induces cytotoxicity in pancreatic cancer cells
Previous studies have demonstrated that ascorbate decreases cell viability in many, but not all, cancer cell lines (5). The effect of pharmacological ascorbate on pancreatic cancer cell lines is unknown. We hypothesized that ascorbate would lead to cytotoxicity and cell death in pancreatic cancer. Figure 1A demonstrates the differential susceptibility of the immortalized pancreatic ductal epithelial cell line, H6c7 and its derivative, H6c7er-Kras+ (H6c7 cells expressing K-ras oncogene), and pancreatic cancer cells (MIA PaCa-2, AsPC-1, BxPC-3) to the effects of pharmacologic ascorbate concentrations. All cells were treated with ascorbate (0, 5, 10 mM) for one hour in DMEM media. These doses have been shown to be readily achievable with little toxicity when administered to humans (27,28). Using the MTT assay there were significant decreases in cell viability in the pancreatic cancer cell lines treated with ascorbate 5 or 10 mM compared to no treatment. In contrast the immortalized H6c7 cell line had little change in viability with the same doses of ascorbate while its derivative, the Kras+ cell line, had significant decreases in cell viability with ascorbate, 5 and 10 mM. In addition to measuring short-term cell viability, clonogenic cell survival assays were performed to measure long-term effects of ascorbate on cancer cell growth (Figure 1B,C). In the human pancreatic cancer cell lines MIA PaCa-2 and AsPC-1, pharmacologic doses of ascorbate (5, 10, 20 mM for 1 h) markedly decreased clonogenic survival in a dose-dependent manner (Figure 1B,C). The clonogenic cell survival assay demonstrated that ascorbate treatment at higher doses resulted in no colony formation from 400 cells plated and treated with ascorbate (20 mM) in the MIA PaCa-2 cell line (Figure 1B). These results support the hypothesis that numerous pancreatic cancer cell lines are susceptible to ascorbate-induced cytotoxicity.
Figure 1.
A. Effects of pharmacologic ascorbic acid concentrations on pancreatic cancer and pancreatic ductal epithelial cells. All cells were treated with ascorbate (0, 5, 10 mM) for one hour. Cell viability determined by MTT assay. MIA PaCa-2, AsPC-1, BxPC-3 are pancreatic cancer cell lines. Immortalized pancreatic ductal epithelial cell line, H6c7 and its derivatives, and H6c7er-Kras (H6c7 cells expressing K-ras oncogene), also received ascorbate (0, 5, 10 mM) for one hour. Ascorbate decreased cell viability in all pancreatic cancer cell lines and in the H6c7 cell lines that express K-ras.
B. MIA PaCa-2 pancreatic cancer cells were treated with ascorbate (0–20 mM) for one hour and clonogenic survival determined. Ascorbate caused a dose-dependent decrease in clonogenic survival. Arrow indicates that no colonies were formed when 20 mM ascorbate was given for one hour.
C. AsPC-1 pancreatic cancer cells were treated with ascorbate (0–20 mM) for one hour and clonogenic survival determined. Ascorbate again caused a dose-dependent decrease in clonogenic survival.
Ascorbate-induced cytotoxicity is due to H2O2
Previous studies have suggested that ascorbate-induced cell death is dependent on generation of H2O2 via ascorbate radical; ascorbate serves as the electron donor to O2 to form H2O2 (5). We have previously observed a positive linear correlation for [H2O2] vs. [AscH− ] and a quadratic correlation with ascorbate radical, i.e. [H2O2] = function of ([Asc•−]2). When ascorbate is infused intravenously the resulting pharmacologic concentration will distribute rapidly into the extracellular water space (6). Thus, pharmacologic ascorbate concentrations in media, as a surrogate for extracellular fluid, should generate ascorbate radical and H2O2. Because AscH− interferes with most peroxidase-based detection methods, we measured formation of H2O2 upon addition of AscH− using a Clark-type oxygen electrode (21). Oxygen evolution was measured upon introduction by catalase: 2H2O2 → 2H2O + O2. Ascorbate-mediated generation of H2O2 in cell culture medium was both time- and dose- dependent (Supplemental data, Figure S1A,B). In Supplemental Figure S1A, ascorbate in the media for one hour increases H2O2 concentration in a dose-dependent manner. In addition, ascorbate 1 mM results in a steady increase in the concentration of H2O2 for up to 60 min after ascorbate is added to the media (Figure S1B).
The effect of catalase overexpression on ascorbate-induced cytotoxicity
To determine if H2O2 mediated ascorbate-induced cytotoxicity, MIA PaCa-2 cells were pretreated with various forms of catalase. In the first set of experiments we pretreated cells with catalase 100 μg/mL or PEG-catalase 200 U/mL and then gave ascorbate 2 mM for one hour and performed a clonogenic survival assay. Western blots determined that catalase in the media and PEG catalase increased catalase protein in the media (data not shown) but did not increase intracellular catalase protein (Figure 2A). To determine if overexpression of intracellular catalase could protect from ascorbate-induced cytototoxicity, MIA PaCa-2 pancreatic cancer cells were infected with adenoviral vectors including AdEmpty (empty vector, 100 MOI), an adenovirus containing human catalase cDNA (AdCAT 100 MOI), and an adenovirus containing human catalase cDNA with an 80-bp MnSOD mitochondrial leader sequence (AdmitCAT 100 MOI). Figure 2A demonstrates the expression of catalase in MIA PaCa-2 cells infected with the AdEmpty, AdCAT, AdmitCAT, PEG-catalase or catalase. Infection with the AdCAT or the AdmitCAT increased intracellular catalase immunoreactivity.
Figure 2.
Overexpression of extracellular and cytosolic catalase reverses ascorbate induced cytotoxicity.
A. Catalase is overexpressed in MIA PaCa-2 cells transfected with adenoviruses containing human catalase cDNA. Transfection with AdCAT (100 MOI) targeted catalase expression to the cytosol while AdmitCAT (100 MOI) directed catalase to the mitochondria via an 80-bp MnSOD leader sequence. Western blotting confirmed the overexpression of intracellular catalase in cells transfected with AdCAT and AdmitCAT. MnSOD was used as a loading control.
B. Catalase pretreatment reverses ascorbate-induced decreases in clonogenic survival. Ascorbate (2 mM) for one hour decreased clonogenic survival in MIA PaCa-2 human pancreatic cancer cells. Catalase (100 μg/mL) and PEG-catalase (200 u/mL) alone had little effect on clonogenic survival. Pretreatment of cells with catalase or PEG-catalase followed by ascorbate (2 mM) reversed ascorbate-induced cytotoxicity. *P < 0.05 vs control, means ± SEM, n = 3.
C. Cytosolic-directed catalase, but not mitochondrial-directed catalase blocked ascorbate-induced cytotoxicity. MIA PaCa-2 cells were treated with either AdEmpty (100 MOI), AdCAT (100 MOI) or AdmitCAT (100 MOI) and treated with ascorbate (2 mM) for one hour. Ascorbate (2 mM) decreases clonogenic survival in cells infected with the AdEmpty and AdmitCAT vectors, but has no effect on cells infected with AdCAT. *P < 0.05 vs. - abscorbate, means ± SEM, n = 3.
Pretreatment of MIA PaCa-2 cells with catalase or PEG-catalase in the media prevented ascorbate-induced cytotoxicity (Figure 2B). Ascorbate decreased clonogenic survival to 10 ± 4% of control values; pretreatment with catalase or PEG-catalase maintained clonogenic survival at control values. Catalase alone or PEG-catalase alone had no effect on clonogenic survival. To determine if intracellular catalase would prevent ascorbate-induced cytotoxicity, MIA PaCa-2 cells were infected with the adenoviral vectors and clonogenic survival assays were performed. The clonogenic survival of cells infected with the AdCAT vector maintained clonogenic survival at control when treated with ascorbate 2 mM for one hour (Figure 2C). However, cells infected with the AdmitCAT vector had a significant decrease in clonogenic survival when treated with ascorbate. Ascorbate 2 mM resulted in a 4-fold decrease in clonogenic survival in cells infected with the AdmitCAT vector. These results indicate that ascorbate-induced cytotoxicity is due to extracellular generation of H2O2 that diffuses intracellularly into the cytosolic compartment.
Ascorbate decreases intracellular ATP levels
Chen and colleagues have hypothesized that ascorbate depletes ATP leading to cell death (6). To examine this possibility, MIA PaCa-2 cells were treated with ascorbate (0, 1, 2, and 5 mM) for one hour, with and without catalase (100 μg/mL) pretreatment and ATP levels were determined (Figure 3A). ATP levels demonstrated a dose-dependent decline with ascorbate treatment, while pretreatment of catalase prevented the decrease in ATP seen with ascorbate 2 mM or 5 mM. To determine if intracellular overexpression of catalase would reverse ascorbate-induced decreases in ATP levels, cells were infected with the adenoviral vectors AdEmpty, AdCAT, and AdmitCAT (100 MOI). Control cells and cells infected with the AdEmpty vector had significant decreases in ATP levels after ascorbate (5 mM for 1 h). Parallel to clonogenic survival, ascorbate induced decreases in ATP were prevented in cells treated with the AdCAT vector. However, in contrast to clonogenic survival (Figure 2C), the AdmitCAT blocked depletion of ATP (Figure 3B) suggesting that loss of ATP may not have a role in ascorbate-induced cytotoxicity. In addition measurement of NADP+/NADPH levels revealed only a very minor change (6 ± 1% at six hours) after ascorbate (2 mM) treatment. Also, the ratio of NADP+/NADPH was 1.0 ± 0.1 prior to ascorbate and remained unchanged at 1.0 ± 0.1 six hours after ascorbate treatment.
Figure 3.
Ascorbate decreases intracellular ATP levels. A. Catalase pretreatment blocks the ascorbate-induced dose-dependent decrease in ATP. ATP levels were significantly lower in MIA PaCa-2 cells treated with ascorbate (2 and 5 mM) when compared to the same cells pretreated with catalase (100 μg/mL). A luciferase-based somatic ATP assay kit was utilized in the measurement of intracellular ATP. *P < 0.05 vs. + catalase, means ± SEM, n = 3.
B. MIA PaCa-2 cells transfected with AdCAT or AdmitCAT restores ATP following treatment with ascorbate (5mM for one hour) relative to their controls. Ascorbate (5 mM) decreases ATP levels in control and AdEmpty treated pancreatic cancer cells. However, the decreased ATP levels are reversed in MIA PaCa-2 cells with infection of the adenoviral vectors containing human catalase cDNA (AdCAT and AdmitCAT). Although AdCAT had reversed ascorbate-induced cytotoxicity, AdmitCAT did not, suggesting that mitochondrial depletion of ATP may not play a role in ascorbate-induced cytotoxicity. *P < 0.05 vs. ascorbate 0 mM, means ± SEM, n = 3.
C. Ascorbate (0–5 mM) demonstrated significant decreases in clonogenic survival in both MIA PaCa-2 rho+ and rho° cells without pyruvate. However, ascorbate-induced cytotoxicity was reversed when pyruvate is added to the media of rho° cells to compensate for the respiratory metabolism deficit induced by the generation of mitochondrial deficient cells.
To further investigate the role of mitochondrial ATP generation in ascorbate-induced cytotoxicity, human pancreatic cancer cells deficient in oxidative phosphorylation due to the absence of mitochondrial DNA were utilized (20,29). Figure 3C shows clonogenic survival in mitochondria deficient rho° cells and the parental rho+ cells following ascorbate treatment (0, 1, 2, or 5 mM for 1 h). In the parental cell line, there is a significant decrease in clonogenic survival with doses of ascorbate of 2 or 5 mM, while in the rho° cells there is no significant decrease in clonogenic survival. However, the rho° medium was supplemented with 100 μg/mL pyruvate, a known scavenger of peroxide, to compensate for the respiratory metabolism deficit as described (20,29). When pyruvate was removed from the rho° media, clonogenic survival decreased following ascorbate treatment (Figure 3C). This result suggests that the direct scavenging of H2O2 by pyruvate may explain the resistance of the rho° cells to ascorbate. Consistent with this idea, addition of pyruvate to the rho+ cells enhanced clonogenic survival and protected the cells from ATP depletion following ascorbate treatment (data not shown). Thus, ascorbate-induced cytotoxicity and ATP depletion were similar in cells deficient in functional mitochondria when compared to cells with functional mitochondria. This suggests that ascorbate-induced cytotoxicity is not due to inhibition of mitochondria oxidative phosphorylation and subsequent ATP generation.
Mechanism of ascorbate-induced cell death
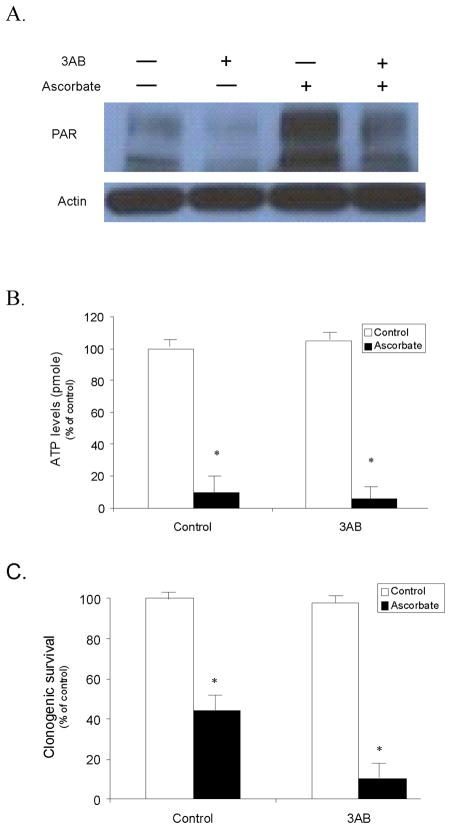
DNA damage induced by H2O2 can activate PARP (7,8). Activated PARP catabolizes NAD+, thereby depleting substrate for NADH formation and subsequent ATP synthesis. To determine if PARP is activated, MIA PaCa-2 cells were treated with ascorbate 5 mM for one hour and then cell homogenates were assayed for PARP cleavage. Supplemental Figure S2A demonstrates minimal PARP cleavage at 6 and 24 h after ascorbate treatment. In addition, the mechanism of ascorbate-induced cell death was studied by flow cytometry using annexin/propidium iodide staining. Treatment of MIA PaCa-2 cells with ascorbate (5 mM) resulted in an initial peak in percentage of apoptotic cells one hour after ascorbate treatment and a steadily increasing percentage of necrotic cells that was time dependent (Supplemental data, Figure S2B). In addition, treatment of MIA PaCa-2 cells with ascorbate (1, 2, 5, and 10 mM) resulted in significant dose-dependent increases in the percentage of necrotic cells with only minor increases in the apoptotic fraction (data not shown). Moreover, treatment of cells with QVD, a known inhibitor of caspase-mediated cell death, did not reverse the percentage of necrotic or apoptotic cells with ascorbate (5 mM). Likewise, treatment of MIA PaCa-2 cells with H2O2 (80–220 μM) also increased the percentage of necrotic cells with little change in the apoptotic fraction and QVD did not reverse the percentage of necrotic cell death (data not shown). These findings suggest that ascorbate induces caspase-independent necrotic cell death. Poly(ADP-ribose) polymerase-1 is readily activated in response to DNA damage and associated with necrotic cell death (30). As shown if Figure 4A, there was an increase in the formation of poly(ADP-ribose) (PAR) polymer, a direct result of PARP-1 activation within one hour of ascorbate (5 mM) treatment. As seen above, intracellular ATP levels were also decreased after ascorbate treatment. Ascorbate (5 mM for one hour) significantly decreased ATP levels six hours after treatment (Figure 4B). To verify whether PARP-1 activation contributes to the cell death induced by ascorbate, cells were treated with ascorbate (5 mM for 1 h), with and without 3-amino benzamide (3AB, 10 mM), a specific PARP-1 inhibitor. Pretreatment with 3AB inhibited ascorbate-induced PAR formation (Figure 4A) but did not reverse the decrease in intracellular ATP depletion (Figure 4B) and did not reverse ascorbate-induced decrease in clonogenic survival (Figure 4C). Together, these results suggest that PARP-1 activation and ATP depletion may not contribute to ascorbate-induced cell death.
Figure 4.
Poly(ADP-ribose) polymerase-1 (PARP-1) activation is not associated with ascorbate-induced cell death. Effect of 3AB (10 mM) on ascorbate-induced PARP activation, intracellular ATP depletion, and cell death. MIA PaCa-2 cells were treated with 5 mM ascorbate for 30 min with or without 1 h pretreatment of 10 mM 3 AB (Tocris Bioscience, Ellisville, MO), an inhibitor of PARP.
A. Cells were collected and subjected to Western blot analysis. Cell lysate (40 μg) was probed with polyclonal rabbit anti-PAR antibody (BD Biosciences, San Jose, CA) at dilution of 1:3000. Polymerize ADP-ribose (PAR) are identified at 116–200 kDa. Ascorbate (5 mM) induces PAR formation which is reversed with 3AB.
B. ATP levels were measured as described. ATP decreases with ascorbate treatment, which is not reversed with 3AB pretreatment. There was a significant decrease in ATP levels with ascorbate (5 mM) treatment. 3AB alone had little effect on ATP while 3AB did not reverse the ascorbate-induced ATP depletion. Means ± SEM, n = 3, *p < 0.05 vs. controls.
C. Clonogenic survival was measured after ascorbate (5 mM for 1 h) with and without 3AB (10 mM). The ascorbate-induced decrease in clonogenic survival is not reversed with 3AB. Means ± SEM, n = 3, *p < 0.05 vs. control.
Ascorbate may lead to death through a unique caspase-independent autophagy pathway (14) and is characterized by accumulation of autophagosomes that fuse with lysosomes to form auto-phagolysosomes. Activation of this pathway can be detected by the processing of LC3 to the lipidated form referred to LC3-II (14). To determine if ascorbate induced autophagy, MIA PaCa-2 cells were treated with ascorbate (5 mM for 1 h) then Western blotting of the cells for LC3 was performed. Figure 5A demonstrates an increase in LC3-II from 4 and 6 h after ascorbate treatment. To determine if the increase in LC3-II was mediated by H2O2, cells were pretreated with catalase 100 μg/mL and AdCAT (100 MOI) prior to treatment with ascorbate (5 mM). Figure 5A demonstrates a decrease in LC3-II protein at 6 h following ascorbate treatment in cells treated with catalase in the media. To confirm this finding, cells were infected with the AdCAT vector and then treated with ascorbate (5 mM). Once again, the increase in LC3-II protein induced by ascorbate at 6 h was reversed with overexpression of the catalase gene targeted to the cytosol. Also, high levels of LC3-II are present upon pretreatment with catalase. Preliminary studies in our laboratory have demonstrated that pancreatic cancer cells that express the K-ras oncogene have increased levels of reactive oxygen species (31). Perhaps the increase in LC3-II with catalase pretreatment may be due to the activity of catalase scavenging these high levels of endogenous H2O2.
Figure 5.
Ascorbate induces autophagy in MIA PaCa-2 cells. A. MIA PaCa-2 cells were treated with ascorbate (5 mM), harvested at various time points and western analysis was performed. Fortyμg of protein per well was loaded onto a 4 – 20 % Tris-HCl gel. Polyclonal rabbit anti-LC3 primary antibody (1:1000 dilution) was followed by horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG (1: 50000 dilution). The increase in LC3-I and LC3-II proteins observed 6 h following ascorbate treatment is inhibited by pretreatment with catalase.
B. MIA PaCa-2 cells transduced with LC3-GFP were treated with the indicated doses of ascorbate or H2O2 for 1 h and allowed to recover in fresh media for 24 h. Cells were harvested, stained with propidium iodide (1 μg/mL) to discriminate live cells and then run on a BD Calibur flow cytometer. The top row shows the gating strategy for the live cells (PI negative). The percentage of live cells is shown in each plot with decreasing viability shown for both treatments (Tx). The bottom row shows the GFP fluorescence of the live cells. The GFP negative cells (WT) were used to adjust the gate for the LC3-GFP positive cells. The percentage of LC3-GFP positive cells is indicated within each plot and the GFP mean florescence intensity (MFI) of this population is indicated above each plot. Both ascorbate and H2O2 increase the percentage of positive cells as well as the MFI.
C. The relative increase in the percentage of LC3-GFP cells (No Tx = 1.0) is shown for three independent experiments (mean +/− standard deviation). A One-way ANOVA with Tukey’s post-hoc test shows that all 4 treatment groups were significantly different than the control (*p < 0.05).
D. Ascorbate and H2O2 induced punctated distribution of LC3-GFP and autophagosome maturation detected by selective increase in GFP fluorescence in cells expressing the LC3-GFP fusion protein. Cells were fixed, stained, and digitized images were analyzed by confocal microscopy and representative cells were selected and photographed. The percentage of LC3-GFP cells as evaluated by digital image analysis was increased in pancreatic cancer cells treated with ascorbate (1 and 2 mM) and H2O2 (200 μM) compared to no treatment. Cells were fixed, stained, and the digitized images were analyzed
E. Pretreatment of MIA PaCa-2 LC3-GFP cells with catalase 100 μg/mL reverses the increase in mean fluorescence intensity (MFI) induced by ascorbate. Means ± SEM, n = 3, *p < 0.05.
To confirm whether ascorbate induces functional autophagy, we generated cells (MIA PaCa-2 LC3-GFP) expressing a fusion product of LC3 and GFP that is used to detect the induction of autophagy (32). Cells were treated with ascorbate (0, 1, 2, and 5 mM) and H2O2 (200 μM as a positive control). Both ascorbate and H2O2 significantly increased the GFP mean fluorescence intensity (MFI) in these cells (Figure 5B). In addition, both ascorbate and H2O2 significantly increased the percentage of LC3-GFP cells (*P < 0.05 vs. no treatment, Means ± SEM, n = 3) (Figure 5C). To further confirm these findings, the MIA PaCa-2 LC3-GFP cells were examined under confocal microscopy. As shown in Figure 5D, both ascorbate and H2O2 markedly increased the punctate GFP fluorescence in these cells. The percentage of punctated cells increased from 25% with no treatment, to 56% and 59% in cells treated with ascorbate, 1 mM and 2 mM, respectively. The percentage of punctated cells increased to 67% in cells treated with H2O2 (200 μM). In addition, there was a significant increase in the MFI of LC3-GFP positive cells with ascorbate (5 mM), and this increase was blocked by catalase pretreatment (Figure 5E).
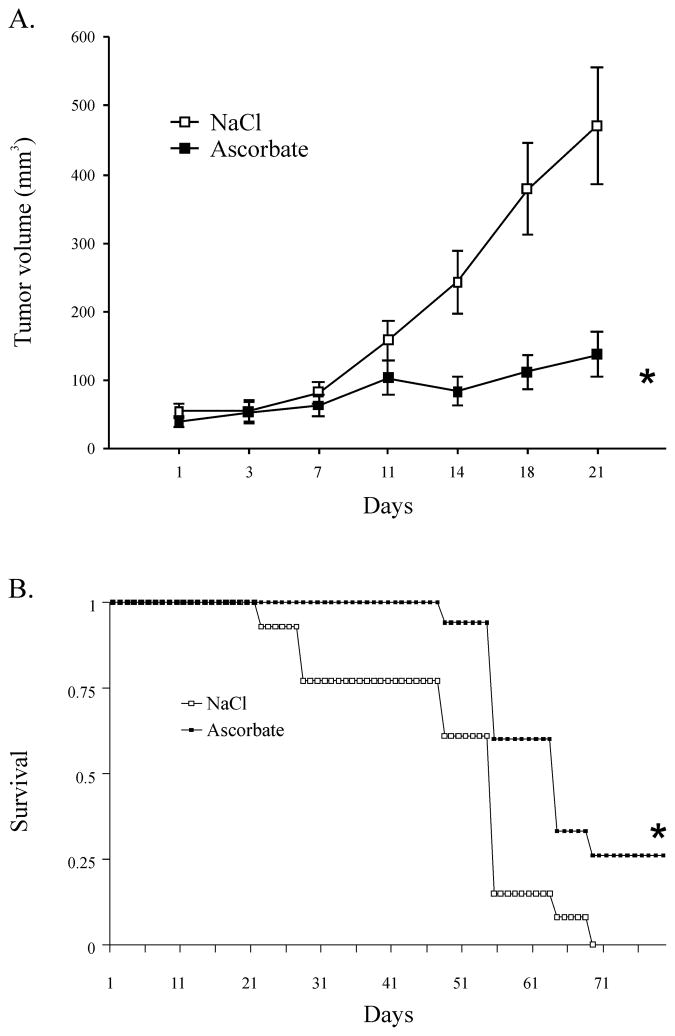
Ascorbate inhibited tumor growth and increased survival
To test the hypothesis that pharmacological ascorbate could reduce tumor growth in vivo, we injected 2 × 106 MIA PaCa-2 cells subcutaneously into the flank region of nude mice and allowed tumors to reach 4 mm × 5 mm in greatest dimension. Mice were then treated with ascorbate 4 g/kg i.p b.i.d. for 14 days or 1 M NaCl i.p. b.i.d. for 14 days. For the controls, 1 M NaCl was used at an equivalent osmolarity to the dose of ascorbate needed to give 4 g/kg. Tumor volume was followed over time until they reached 1000 mm3 at which the mice were sacrificed. Both controls and ascorbate-treated mice had slight but not significant decreases in weight during the treatment period. All of the mice completed the treatment period and there were no deaths during the treatment. None of the animals during the study had to be sacrificed for continued weight loss or cachexia. In animals treated with ascorbate a slower rate of growth in tumor was observed in comparison to the group of animals that received NaCl (Figure 6A). On day 21 of the experiment, the control group had a mean tumor volume of 472 mm3, while the ascorbate group had a mean tumor volume of 138 mm3. The mixed linear regression analysis of the tumor growth curves demonstrated that their rate of growth differed significantly between the groups (p < 0.01). Estimated tumor growth curves are displayed in Figure 6A. The estimated survival curves for each treatment group are given in the Kaplan-Meier plots of Figure 6B. The log-rank analyses of survival demonstrated that the animals that received ascorbate had increased survival compared to controls (68 days vs. 78 days). The global test of equality indicates that there is a significant difference in the survival times (p < 0.0001) between groups.
Figure 6.
A. Ascorbate treatment decreased MIA PaCa-2 tumor growth in nude mice. Animals that received ascorbate (4 g/kg, i.p., b.i.d. for 14 days) had significantly slower tumor growth when compared to animals that received saline (1 M, i.p., b.i.d., for 14 days) (Means ± SEM, p < 0.001, n = 13 control animals and 15 ascorbate-treated animals). On day 21 there was greater than a 3-fold decrease in tumor growth in animals receiving ascorbate when compared to treatment with saline.
B. Kaplan-Meier plots of estimated survival in nude mice. There was a significant difference in survival between saline and ascorbate treated groups of mice (p < 0.001).
DISCUSSION
Ascorbate is one of the early unorthodox therapies for cancer (33–35). This approach was subsequently promoted by Cameron and Pauling (36,37). Cameron and Campbell initially published case reports of 50 patients, some of whom seemed to have benefited from high dose ascorbate treatment (38). Cameron and Pauling then published results of 100 patients with terminal cancer, in whom conventional therapy was no longer considered useful and were given intravenous ascorbate (39). The ascorbate-treated patients were compared to 1000 retrospective controls with similar disease but had not received ascorbate; the comparison demonstrated that patients who received ascorbate survived 300 days longer than controls (39).
To test whether ascorbate was effective, Moertel conducted two randomized placebo controlled studies using ascorbate given orally; neither study showed any benefit (40,41). However, oral and intravenous ascorbate have strikingly different pharmacokinetic properties (27). Cameron gave patients ascorbate intravenously as well as orally, while Moertel’s patients received only oral ascorbate. Our study suggests that the role of ascorbate in pancreatic cancer treatment should be further examined.
Clinical data show that when ascorbate is given orally, fasting plasma concentrations are tightly controlled at < 100 μM (42). As doses exceed 200 mg, absorption decreases, urine excretion increases and ascorbate bioavailability is reduced (42,43). In contrast, when 1.25 grams of ascorbate are administered intravenously, plasma concentrations as high as 1 mM are achieved. Some clinicians have infused more than 10 grams of ascorbate in cancer patients and achieved plasma concentration of 1 to 5 mM (27,28). Both intravenous and intraperitoneal administration of ascorbate achieved serum ascorbate concentrations up to 20 mM (44). Thus, it is clear that intravenous administration of ascorbate can yield very high plasma levels, while oral treatment does not. Our study demonstrates that ascorbate induces cytotoxicity in pancreatic cancer cells at levels achievable with intravenous infusions. Additionally, systemic administration of ascorbate inhibited pancreatic tumor growth in mice.
Our study suggests oxidative stress, mediated by hydrogen peroxide, as a mechanism of ascorbate-induced cytotoxicity since catalase either extracellularly or overexpressed in the cytoplasmic compartment, reversed the decrease in clonogenic survival induced by ascorbate. In addition, an autophagic mechanism may also be involved as an increase in LC3 protein was observed in cells treated with ascorbate. The role of autophagy in cellular responses to oxidative stress is as yet unclear. ROS can induce autophagy, which contributes to caspase-independent cell death in a variety of cell types (45). In contrast, a number of studies demonstrate a protective role of autophagy against ROS-mediated necrosis (46). Additional studies have demonstrated a role of PARP-1 in regulation of autophagy, which enhances cell survival in cells under oxidative stress (31). Both the peroxide-mediated mechanism and autophagic-mediated mechanism could potentially be enhanced to induce more cancer cell killing with peroxide.
In summary, ascorbate, in doses achievable in humans, decreased viability in all pancreatic cancer cell lines via a H2O2–mediated mechanism. Treatment with pharmacological ascorbate induced a noncaspase-mediated cell death consistent with autophagy. In mice with pre-established pancreatic tumors, treatment with ascorbate inhibited tumor growth and prolonged survival. Pharmacological doses of ascorbate, achievable in humans may have potential for therapy in pancreatic cancer.
Supplementary Material
Acknowledgments
Supported by NIH grants CA115785, the Medical Research Service, Department of Veterans Affairs, and the Susan L. Bader Foundation of Hope and the Intramural Research Program, NIH.
We would like to thank Dr. Ming-Sound Tsao from the Department of Pathology and Division of Cellular Molecular Biology and the Ontario Cancer Institute/Princess Margaret Hospital Toronto, and University of Toronto, Ontario, Canada for providing the HPV16-E6E7 and H6c7eR-Kras+ cell lines.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer Statistics, 2008. CA Cancer J Clin. 2008 Mar-Apr;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Bramhall SR, Allum WH, Jones AG, et al. Treatment and survival in 13,560 patients with pancreatic cancer, and incidence of the disease, in the epidemiological study. Br J Surg. 1995;82:111–5. doi: 10.1002/bjs.1800820137. [DOI] [PubMed] [Google Scholar]
- 3.Yeo CJ, Cameron JL. Pancreatic cancer. Curr Probl Surg. 1999;36:59–152. [PubMed] [Google Scholar]
- 4.White R, Lee C, Anscher M, et al. Preoperative chemoradiation for patients with locally advanced Adenocarcinoma of the pancreas. Ann Surg Oncol. 1999;6:38–45. doi: 10.1007/s10434-999-0038-z. [DOI] [PubMed] [Google Scholar]
- 5.Chen Q, Espey MG, Krishna MC, et al. Pharmacologic ascorbic acid concentrations selectively kill cancer cells: Action as a pro-drug to deliver hydrogen peroxide to tissues. Proc Natl Acad Sci U S A. 2005;102:13604–9. doi: 10.1073/pnas.0506390102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Q, Espey MG, Sun Y, et al. Ascorbate in pharmacologic concentrations selectively generates ascorbate radical and hydrogen peroxide in extracellular fluid in vivo. Proc Natl Acad Sci U S A. 2007;104:8749–54. doi: 10.1073/pnas.0702854104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee YJ, Schacter EJ. Oxidative stress inhibits apoptosis in human lymphoma cells. J Biol Chem. 1999;274:19792–8. doi: 10.1074/jbc.274.28.19792. [DOI] [PubMed] [Google Scholar]
- 8.Shraufshtatter IU, Hinshaw DB, Hyslop PA, Spragg RG, Cochrane CG. Glutathione cycle activity and pyridine nucleotide levels in oxidant-induced injury of cells. J Clin Invest. 1985;76:1131–9. doi: 10.1172/JCI112068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee YJ, Galoforo SS, Berns CM, et al. Glucose deprivation-induced cytotoxicity and alterations in mitogen-activated protein kinase activation are mediated by oxidative stress in multidrug-resistant human breast carcinoma cells. J Biol Chem. 1998;273:5294–9. doi: 10.1074/jbc.273.9.5294. [DOI] [PubMed] [Google Scholar]
- 10.Hyslop PA, Hinshaw DB, Halsey WA, et al. Mechanisms of oxidant-mediated cell injury. The glycolytic and mitochondrial pathways of ADP phosphorylation are major intracellular targets inactivated by hydrogen peroxide. J Biol Chem. 1988;263:1665–75. [PubMed] [Google Scholar]
- 11.Comelli M, Di Pancrazio F, Mavelli I. Apoptosis is induced by decline of mitochondrial ATP synthesis in erythroleukemia cells. Free Rad Biol Med. 2003;34:1190–9. doi: 10.1016/s0891-5849(03)00107-2. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad IM, Aykin-Burns N, Sim JE, et al. Mitochondrial production of O2•- and H2O2 mediates glucose deprivation-induced cytotoxicity and oxidative stress in human cancer cells. J Biol Chem. 2005;280:4254–63. doi: 10.1074/jbc.M411662200. [DOI] [PubMed] [Google Scholar]
- 13.Nath KA, Ngo EO, Hebbel RP, Croatt AJ, Zhau B, Nutter LM. α-ketoacids scavenge H2O2 in vitro and in vivo and reduce menadione-induced DNA injury and cytotoxicity. Am J Physiol. 1995;268:C227–36. doi: 10.1152/ajpcell.1995.268.1.C227. [DOI] [PubMed] [Google Scholar]
- 14.Ohtani S, Iwamaru A, Deng W, et al. Tumor suppressor 101F6 and ascorbate synergistically and selectively inhibit non-small cell lung cancer growth by caspase-independent apoptosis and autophagy. Cancer Res. 2007;67:6293–303. doi: 10.1158/0008-5472.CAN-06-3884. [DOI] [PubMed] [Google Scholar]
- 15.Daido S, Yamamoto A, Fujiwara K, et al. Inhibition of the DNA-dependent protein kinase catalytic subunit radiosensitizes malignant glioma cells by inducing autophagy. Cancer Res. 2005;65:4368–75. doi: 10.1158/0008-5472.CAN-04-4202. [DOI] [PubMed] [Google Scholar]
- 16.Takeuchi H, Kondo Y, Fujiwara K, et al. Synergistic augmentation of rapamycin-induced autophagy in malignant glioma cells by phosphatidylionistol 3-kinase/protein kinase B inhibition. Cancer Res. 2005;65:3336–46. doi: 10.1158/0008-5472.CAN-04-3640. [DOI] [PubMed] [Google Scholar]
- 17.Shao Y, Gao Z, Marks PA, et al. Apoptotic and autophagic cell death induced by histone deacetylase inhibition. Proc Natl Acad Sci U S A. 2004;52:18030–65. doi: 10.1073/pnas.0408345102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qian J, Niu J, Li M, Chiao PJ, Tsao MS. In vitro modeling of human pancreatic duct epithelial cell transformation defines gene expression changes induced by K-ras oncogenic activation in pancreatic carcinogenesis. Cancer Res. 2005:5045–53. doi: 10.1158/0008-5472.CAN-04-3208. [DOI] [PubMed] [Google Scholar]
- 19.Lewis A, Ough M, Du J, Tsao MS, Oberley LW, Cullen JJ. Targeting NAD(P)H:quinone oxidoreductase (NQO1) in pancreatic cancer. Molecular Carcinogenesis. 2005;43:215–24. doi: 10.1002/mc.20107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du J, Daniels DH, Asbury CA, et al. Mitochondrial production of reactive oxygen species mediate dicumarol-induced cytotoxicity in cancer cells. J Biol Chem. 2006;281:37416–26. doi: 10.1074/jbc.M605063200. [DOI] [PubMed] [Google Scholar]
- 21.Buettner GR. In the absence of catalytic metals, ascorbate does not autoxidize at pH 7: Ascorbate as a test for catalytic metals. J Biochem Biophys Methods. 1988;16:27–40. doi: 10.1016/0165-022x(88)90100-5. [DOI] [PubMed] [Google Scholar]
- 22.Coleman MC, Asbury C, Daniels DH, et al. Inhibition of glucose metabolism in pancreatic cancer induces cytotoxicity via metabolic oxidative stress. Free Rad Biol Med. 2008;44:322–32. doi: 10.1016/j.freeradbiomed.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 23.Clement MV, Ramalingam R, Long LH, Halliwell B. The in vitro cytotoxicity of ascorbate depends on the culture medium used to perform the assay and involves hydrogen peroxide. Antioxid Redox Signal. 2001;3:157–63. doi: 10.1089/152308601750100687. [DOI] [PubMed] [Google Scholar]
- 24.Zwacka RM, Dudus L, Epperly MW, Greenburger JS, Engelhardt JF. Redox gene therapy protects human IB-3 lung epithelial cells against ionizing radiation-induced apoptosis. Hum Gene Ther. 1998;9:1381–6. doi: 10.1089/hum.1998.9.9-1381. [DOI] [PubMed] [Google Scholar]
- 25.Bai J, Rodriguez AM, Melendez JA, Cederbaum AI. Overexpression of catalase in cytosolic or mitochondrial compartment protects HepG2 cells against oxidative injury. J Biol Chem. 1999;274:26217–24. doi: 10.1074/jbc.274.37.26217. [DOI] [PubMed] [Google Scholar]
- 26.Budanov AV, Sablina AA, Feinstein E, Koonin EV, Chumakov PM. Regeneration of peroxiredoxins by p53-regulated sestrins, homologs of bacterial AhpD. Science. 2004 Apr 23;304(5670):596–600. doi: 10.1126/science.1095569. [DOI] [PubMed] [Google Scholar]
- 27.Padayatty SJ, Sun H, Wang Y, et al. Vitamin C pharmacokinetics: implications for oral and intravenous use. Ann Intern Med. 2004;140:533–7. doi: 10.7326/0003-4819-140-7-200404060-00010. [DOI] [PubMed] [Google Scholar]
- 28.Hoffer LJ, Levine M, Assouline S, et al. Phase 1 clinical trial of i.v. ascorbic acid in advanced malignancy. Ann Oncol. 2008;19:1969–74. doi: 10.1093/annonc/mdn377. [DOI] [PubMed] [Google Scholar]
- 29.Cloos C, Daniels DH, Kalen A, et al. Mitochondrial DNA depletion induces radioresistance by suppressing G2-checkpoint activation in human pancreatic cancer cells. Radiat Res. 2009;171:581–7. doi: 10.1667/RR1395.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jagtap P, Szabo C. Poly(ADP-ribose) polymerase and the therapeutic effects of it inhibitors. Nat Rev Drug Discov. 2005;4:421–40. doi: 10.1038/nrd1718. [DOI] [PubMed] [Google Scholar]
- 31.Du J, Tsao MS, Oberley LW, Cullen JJ. K-ras oncogene increases reactive oxygen species (ROS): Mechanisms involved in regulating pancreatic cancer cell growth. Free Radical Biology and Medicine. 2007;43:S53. [Google Scholar]
- 32.Huang Q, Wu YT, Tan HL, Ong CN, Shen HM. A novel function of poly(ADP-ribose) polymerase-1 in modulation of autophagy and necrosis under oxidative stress. Cell Death Differ. 2008;16:264–77. doi: 10.1038/cdd.2008.151. [DOI] [PubMed] [Google Scholar]
- 33.McCormick WJ. Cancer: the preconditioning factor in pathogenesis. Arch Pediatr. 1954;71:313–22. [PubMed] [Google Scholar]
- 34.McCormick WJ. Cancer: a collagen disease, secondary to a nutritional deficiency? Arch Pediatr. 1959;76:166–71. [PubMed] [Google Scholar]
- 35.Cameron E, Rotman D. Ascorbic acid, cell proliferation, and cancer. Lancet. 1972;299:542. doi: 10.1016/s0140-6736(72)90215-2. [DOI] [PubMed] [Google Scholar]
- 36.Cameron E, Pauling L. Ascorbic acid and the glycosaminoglycans. An orthomolecular approach to cancer and other diseases. Oncology. 1973;27:181–92. doi: 10.1159/000224733. [DOI] [PubMed] [Google Scholar]
- 37.Cameron E, Pauling L. Supplemental ascorbate in the supportive treatment of cancer: Prolongation of survival times in terminal human cancer. Proc Natl Acad Sci U S A. 1976;73:3685–9. doi: 10.1073/pnas.73.10.3685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cameron E, Campbell A. The orthomolecular treatment of cancer. II Clinical trial of high-does ascorbic acid supplements in advanced human cancer. Chem Biol Interact. 1974;9:285–315. doi: 10.1016/0009-2797(74)90019-2. [DOI] [PubMed] [Google Scholar]
- 39.Cameron E, Pauling L. Supplemental ascorbate in the supportive treatment of cancer: reevaluation of prolongation of survival times in terminal human cancer. Proc Natl Acad Sci U S A. 1978;75:4538–42. doi: 10.1073/pnas.75.9.4538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Creagan ET, Moertel CG, O’Fallon JR, Schutt AJ, O’Connell MJ, Rubin J, Frytak S. Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial. N Engl J Med. 1979;301:687–90. doi: 10.1056/NEJM197909273011303. [DOI] [PubMed] [Google Scholar]
- 41.Moertel CG, Flemin TR, Creagan ET, Rubin J, O’Connell MJ, Ames MM. High-dose vitamin C versus placebo in the treatment of patients with advanced cancer who have had no prior chemotherapy. A randomized double-blind comparison. N Engl J Med. 1985;312:137–41. doi: 10.1056/NEJM198501173120301. [DOI] [PubMed] [Google Scholar]
- 42.Levine M, Conry-Cantilena C, Wang Y, et al. Vitamin C Pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance. Proc Natl Acad Sci U S A. 1996;93:3704–9. doi: 10.1073/pnas.93.8.3704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Graumlich JF, Ludden TM, Conry-Cantilena C, Cantilena LR, Jr, Wang Y, Levine M. Phamacokinetic model for ascorbic acid in healthy male volunteers during depletion and repletion. Pharm Res. 1997;14:1133–9. doi: 10.1023/a:1012186203165. [DOI] [PubMed] [Google Scholar]
- 44.Verrax J, Calderon PB. Pharmacologic concentrations of ascorbate are achieved by parenteral administration and exhibit antitumoral effects. Free Rad Biol Med. 2009;47:32–40. doi: 10.1016/j.freeradbiomed.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 45.Chen Y, McMillan-Ward E, Kong J, Israels SJ, Gibson SB. Oxidative stress induces autophagic cell death independent of apoptosis in transformed and cancer cells. Cell Death Differ. 2008;15:171–82. doi: 10.1038/sj.cdd.4402233. [DOI] [PubMed] [Google Scholar]
- 46.Wu YT, Tan HL, Huang Q, et al. Autophagy plays a protective role during zVAD-induced necrotic cell death. Autophagy. 2008;4:457–66. doi: 10.4161/auto.5662. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.