Abstract
The serine/threonine family of Pim kinases function as oncogenes and have been implicated in prostate cancer progression, particularly in hormone-refractory prostate disease, as a result of their anti-apoptotic function. In this study, we utilized a pharmacological inhibitor targeting the Pim family members, SGI-1776, to determine whether modulation of Pim kinase activity could alter prostate cancer cell survival and modulate chemotherapy resistance. Extensive biochemical characterization of SGI-1776 confirmed its specificity for the three isoforms of the Pim family. Treatment of prostate cancer cells with SGI-1776 resulted in a dose-dependent reduction in phosphorylation of known Pim kinase substrates that are involved in cell cycle progression and apoptosis (p21Cip1/WAF1 and Bad). Consequently, SGI-1776 compromised overall cell viability by inducing G1 cell cycle arrest and triggering apoptosis. Overexpression of recombinant Pim-1 markedly increased sensitivity of SGI-1776-mediated prostate cancer cell apoptosis and p21Cip1/WAF1 phosphorylation inhibition, reinforcing the specificity of SGI-1776. An additional cytotoxic effect was observed when SGI-1776 was combined with taxane-based chemotherapy agents. SGI-1776 was able to reduce cell viability in a multidrug resistance 1 (MDR1) protein based taxane-refractory prostate cancer cell line. In addition, SGI-1776 treatment was able to resensitize chemoresistant cells to taxane-based therapies by inhibiting MDR1 activity and inducing apoptosis. These findings support the idea that inhibiting Pim kinases, in combination with a chemotherapeutic agent, could play an important role in prostate cancer treatment by targeting the clinical problem of chemoresistance.
Keywords: Pim kinases, prostate cancer, SGI-1776, chemoresistance, pro-apoptotic
Introduction
Pim kinases are a family of serine/threonine kinases that regulate cell survival [1]. This family of kinases is composed of three different isoforms (Pim 1, Pim 2, and Pim 3) that are highly homologous at the amino acid level, yet differ partially in their tissue distribution [2,3]. Although the cellular localization of Pim kinases is mainly cytoplasmic, some evidence suggests that they can also be found in the nucleus and more recently on the cell surface [4,5]. The first family member identified, pim-1, was initially discovered as a preferential integration site for the moloney murine leukemia virus (MuLV) and has subsequently been associated with cell cycle progression, apoptosis, and tumorigenesis [6,7].
Unlike other serine/threonine kinases, the Pim family members are tightly regulated at the level of transcription and translation [8]. Their expression is mediated by the JAK/STAT signaling pathway, which is activated by various cytokines and hormones [9]. Pim kinases are known to suppress apoptosis by directly phosphorylating and inhibiting the pro-apoptotic Bcl-2 family member, Bad [10-12]. Additionally, Pim-1 kinase can regulate cell cycle progression at the G1/S and G2/M transition phases by its ability to phosphorylate Cdc25A [13], p21Cip1/WAF1 [14], and p27Kip1 [15] as well as Cdc25C [16], respectively.
The Pim kinase family members are considered oncogenes and have been implicated in tumorigenesis either alone or functioning synergistically with c-Myc [17-19]. Initially, elevated levels of Pim kinases were discovered in leukemia and lymphoma tumors [3,7,20]; however, more recently, they were found to be overexpressed in solid tumors, including pancreatic cancer and prostate cancer [11,21]. Several independent studies have demonstrated that Pim-1 is upregulated in human prostate cancer clinical samples and in various animal models [18,21,22]. Additionally, IL-6, a cytokine known to be elevated in sera from patients with advanced prostate cancer, has been shown to induce Pim-1 kinase through activation of the JAK/STAT signaling pathway in prostate cancer systems [23,24]. Recent studies have also correlated Pim-1 kinase with chemoresistance in prostate cancer cells, which is a common occurrence in more aggressive, hormone-refractory prostate cancers [25,26].
It is believed that the oncogenic and pro-survival potential of the Pim kinases contributes to tumorigenesis and promotes drug resistance in prostate cancer. Therefore, recent efforts have been placed on the identification of Pim kinase inhibitors as potential therapeutic targets of cancer [1,27-31]. The purpose of this study was to characterize a novel small molecule inhibitor of Pim kinases, SGI-1776, in prostate cancer model systems to determine whether targeting Pim kinase activity alone or in combination with a taxane-based chemotherapeutic regimen could have a significant impact on the treatment of prostate cancer. We demonstrate that SGI-1776 is a fairly selective inhibitor of the Pim kinases and can cause a reduction in prostate cancer cell viability and alter overall cytotoxic responses to taxanes. Specifically, we reveal that SGI-1776 can disrupt cell cycle progression, induce apoptosis, promote taxane sensitivity, and overcome acquired chemoresistance by inhibiting MDR1 activity in specific prostate cancer models. These findings suggest that Pim kinase inhibition may prove to be a beneficial strategy for treating prostate cancer and in particular those that are non-responsive to taxane-based chemotherapy.
Materials and methods
In vitro kinase assay
Kinase inhibition was measured by radiometric assays using the KinaseProfiler™ service at Millipore (http://www.millipore.com/drugdiscovery/dd3/KinaseProfiler, Billerica, MA). IC50 determination of SGI-1776 against the Pim kinases was performed using IC50Profiler Express™ at Millipore. For kinase inhibition, Pim-1 (h)/Pim-2 (h)/Pim-3 (h) (5-10mU) is incubated with 8mM MOPS pH 7.0, 0.2mM EDTA, 100μM KKRNRTLTV, 10mM Mg Acetate and [γ-33P-ATP] (specific activity approx. 500cpm/pmol, concentration as required) in a final reaction volume of 25μl. The reaction is initiated by the addition of the MgATP mix. After incubation for 40 min at room temperature, the reaction is stopped by the addition of 5μl of a 3% phosphoric acid solution. 10μl of the reaction is then spotted onto a P30 filtermat and washed three times for 5 min in 75mM phosphoric acid and once in methanol prior to drying and scintillation counting.
Cell culture
The LNCaP, PC3, DU145, and 22Rv1 prostate cancer cell lines were acquired from ATCC (Manassas, VA) and cultured in RPMI 1640 medium supplemented with 10% FBS. The tumorigenic RWPE2-W99 cell line (ATCC) was maintained in Keratinocyte Serum Free Medium (GIBCO Invitrogen, #17005-042) supplemented with bovine pituitary extract (BPE) and human recombinant epidermal growth factor (EGF). The LAPC-4 and C4-2B cell lines were acquired through an MTA from UCLA (Los Angeles, CA) and ViroMed Laboratories (Minnetonka, MN), respectively [32]. The LAPC-4 cell line was maintained in Iscove's modified medium and 5% FBS, while the C4-2B cell line was cultured in RPMI 1640 medium and 10% FBS.
Generation of 22Rv1-Pim1 and 22Rv1-T cell lines
The pBK/CMV-Pim-1 plasmid [33] utilized in these studies was a generous gift from Dr. Nancy Magnuson (Washington State University). The stable 22Rv1 cell line overexpressing Pim-1 cDNA (22Rv1-Pim1) was generated by Lipofectamine 2000 transfection of 22Rv1 cells with the pBK/CMV-Pim-1 plasmid followed by selection in 400μg/ml G418.
The paclitaxel-resistant 22Rv1 cell line (22Rv1-T) was generated in vitro by serially passaging the parental 22Rv1 line in the presence of increasing concentrations of paclitaxel (0-400ng/ml). After a period of approximately 4 months, the paclitaxel-insensitive derivative of 22Rv1 emerged and is currently being maintained in the presence of 5ng/ml of paclitaxel.
ATP viability assay
Approximately 1,000 cells/well were plated in ScreenMates 384 well tissue culture treated microplates (Thermo Fisher Scientific, #4334) in 1% serum (except for RWPE2-W99 cells, which were plated in complete Keratinocyte serum free media conditions). The following day, increasing concentrations of SGI-1776 and/or paclitaxel were added to the respective wells. After a specified period of time, cell viability was assessed by adding 25μl of ATPlite reagent (Perkin Elmer, #6016739) to each well. Luminescence was determined by reading the 384 well plates on the VICTOR Light Luminescence Counter machine (Perkin Elmer). The results are based on an average of five wells per experimental sample.
Cell cycle analysis
C4-2B and 22Rv1 cells were cultured in 1% serum overnight and then treated with SGI-1776 for 24 hours. Cells were harvested and fixed in cold methanol, followed by the addition of propidium iodide (50μg/ml) and RNase for 30 minutes in order to determine the percentage of cells in each phase of the cell cycle using a flow cytometer.
Quantitative real-time RT-PCR
RNA was extracted from human prostate cancer cell lines using the Qiagen RNeasy Kit (QIAGEN). Individual Taqman primer and probe sets were purchased from Applied Biosystems (Carlsbad, CA) at a 20x concentration (see table below). 100ng of RNA per reaction per well was combined with a mastermix of Amplitaq Gold PCR Master Mix, the target primer set, ROX, Mulitscribe RNase, and RNase inhibitor (Applied Biosystems). Reactions were run at 50°C for 15 minutes, 95°C for 10 minutes, and then cycled 40 times at 95°C for 15 seconds and 60°C for 1 minute. The data was then analyzed as the ΔΔCt method on the SDS RQ manager software (Applied Biosystems). All data was normalized to 18S and displayed as relative expression.
| Primer Set Name | Human Code |
|---|---|
| PIM1 | Hs01065498_m1 |
| PIM2 | Hs00179139_m1 |
| PIM3 | Hs00420511_g1 |
| MDR1 | Hs00184500_m1 |
| 18S | Hs4310893E |
Western blot analysis
Cells were lysed using RIPA buffer (1mM Na3VO4, 1mM PMSF, 1mM NaF, and protease inhibitor cocktail (Sigma, #P8340)). Proteins (70μg) were separated and transferred on to a PVDF membrane, which were then probed with the following primary antibodies: anti-phospho p21 (Thr145) at 1:200 (Santa Cruz Biotechnology, Inc., #sc-20220-R), anti-p21 at 1:200 (Santa Cruz Biotechnology, Inc., #sc-397), anti-phospho BAD (Ser112) at 1:2,000 (Cell Signaling, #9296), anti-BAD at 1:1,000 (Cell Signaling, #9292), Mdr-1 (D-11) at 1:200 (Santa Cruz Biotechnology, Inc., #sc-55510), anti-PARP at 1:1,000 (Cell Signaling, #9542), anti-Pim-1 at 1:200 (Santa Cruz Biotechnology, Inc., #sc-13513), and anti-β-actin at 1:10,000 (Sigma, #A5441).
Analysis of apoptosis
Cells were cultured in 1% serum overnight and then incubated with SGI-1776 for 24 hours. Apoptosis was determined by measuring caspase-3 activity using the Caspase-3 Fluorometric Protease Assay (Invitrogen, #KHZ0012). Data was normalized to untreated samples and displayed as relative caspase-3 activity.
Multidrug Resistance Assay
Assay was performed according to manufacturer's instructions using a calcein AM fluorescence based assay (Vybrant Multidrug Resistance Assay Kit, Molecular Probes, #V-13180). Approximately 2.5×105 22Rv1-T cells were used per reaction and increasing concentrations of SGI-1776 and/or paclitaxel were tested in triplicate. Data are presented as a percentage of calcein retention in treated versus untreated MDR (22Rv1-T) cells. This assay was also performed on the parental (22Rv1) cells as a comparison (data not shown).
Statistical Analysis
Primarily, an unpaired student's t-test was performed to determine statistical significance in the presented studies. However, when determining whether the cytotoxic effects of two agents were additive or synergistic, a two-way ANOVA analysis was applied. For all analyses, p<0.05 was considered statistically significant and displayed as p<0.05*, p≤0.001**, p≤0.0001***.
Results
Identification and Characterization of Pim kinase inhibitor, SGI-1776
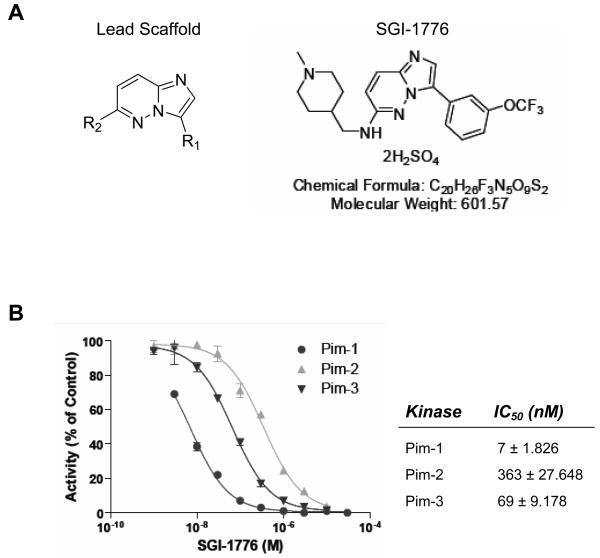
The small molecule inhibitor targeting Pim kinases known as SGI-1776 was provided by SuperGen Inc., Dublin, CA. SGI-1776, a member of the imidazo[1,2-b]pyridazine chemical class, was selected for its ability to exploit an extended ATP-binding and solvent pocket, thereby making it a selective Pim family kinase inhibitor (Fig. 1a).
Figure 1. Structure and biochemical analysis of SGI-1776.
(A) Structures of the lead scaffold and SGI-1776 compound, a member of the imidazo[1,2-b]pyridazine class. (B) In vitro kinase assays of Pim-1, -2, and -3 with varying concentrations of SGI-1776.
SGI-1776 was identified by in silico screening of 1.5 million compounds from focused and/or diverse libraries using Pim-1 kinase crystal structure in complex with AMP-PNP as a template. This discovery process identified a promising lead scaffold, imidazo[1,2-b]pyridazine, which was then used to optimize the potency and selectivity of compounds against the Pim-1 target through specific modifications at R1 and R2 groups predicted by our proprietary CLIMB based approach. A novel synthetic route was developed starting from 1,4-dibromo-trans-2-butene. We prepared the 3-bromo-6-chloro-imiadazo[1,2-b]pyridazine scaffold in three steps (Fig. 1a). Suzuki coupling with various substituted aryl boronic acids, followed by introduction of aliphatic amines led to the synthesis of more than 30 novel chemical entities as Pim-1 kinase inhibitors. Initial SAR studies revealed that the introduction of a hydrophobic moiety at R1 and small ring substituent groups with 1 or 2-CH2 spacers at the 6-amine position were vital for Pim-1 kinase inhibition.
The lead compound SGI-1776 demonstrated potent activity against Pim-1 kinase and exhibited promising selectivity against a panel of kinases [34]. Figure 1b illustrates a dose-dependent decrease in Pim-1, Pim-2, and Pim-3 activity with increasing doses of SGI-1776. The IC50 of SGI-1776 for the three isoforms of the Pim kinase family: Pim-1, Pim-2, and Pim-3, were in the low nanomolar range (7nM ± 1.826, 363nM ± 27.648, and 69nM ± 9.178, respectively) (Fig. 1b). The specificity of SGI-1776 was further confirmed by screening SGI-1776 against a panel of more than 300 kinases (KINOMEscan™, Ambit Biosciences). In addition to the three Pim kinases, SGI-1776 exhibited inhibitory activity against two other kinases: Flt-3 (IC50 44nM) and Haspin (IC50 34nM).
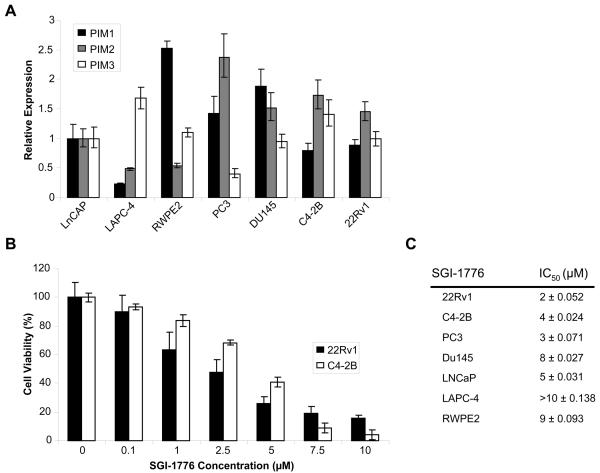
Effect of SGI-1776 on prostate cancer cell lines
Initially, we chose to evaluate SGI-1776 for activity in prostate cancer by determining its response in a collection of prostate cancer cell lines. Prior to assessing the cytotoxic effects of this inhibitor, we first confirmed Pim-1, Pim-2, and Pim-3 expression by quantitative real-time RT-PCR (Fig. 2a). Differential expression of the Pim family members was seen across the various prostate cancer model systems as also reported by other groups [25,27]. After verifying the presence of the target, we utilized the ATP viability assay and determined that SGI-1776 reduces cell viability in the examined prostate cancer cell lines in a dose dependent manner (Fig. 2b). The androgen-independent (AI) cell lines, 22Rv1, PC3, and C4-2B demonstrated the highest sensitivity to SGI-1776, with approximate IC50s of 2μM ± 0.052, 3μM ± 0.071, and 4μM ± 0.024, respectively. The LNCaP cell line showed the next greatest response (5μM ± 0.031), followed by the DU145 (8μM ± 0.027) and RWPE2-W99 (9μM ± 0.093) cell lines, while LAPC-4 (>10μM ± 0.138) cells exhibited a minimal response (Fig. 2c).
Figure 2. Effect of SGI-1776 on cell viability in prostate cancer cell lines.
(A) Quantitative real-time RT-PCR analysis of Pim-1, Pim-2, and Pim-3 expression in a panel of prostate cancer cell lines. The data was normalized to 18S and the fold change in Pim kinase expression for each cell line was determined relative to the LNCaP cell line, which was given a value of 1. (B) 22Rv1 and C4-2B cells were exposed to increasing concentrations of SGI-1776 for 72 hours and cell viability was assessed by an ATP viability assay. Each condition was the average of six individual wells. (C) Similar conditions as described in (B) were carried out on the following cell lines: PC3, DU145, LNCaP, LAPC-4, and RWPE2. The approximate IC50 for each cell line was determined after treatment with SGI-1776 for 72 hours.
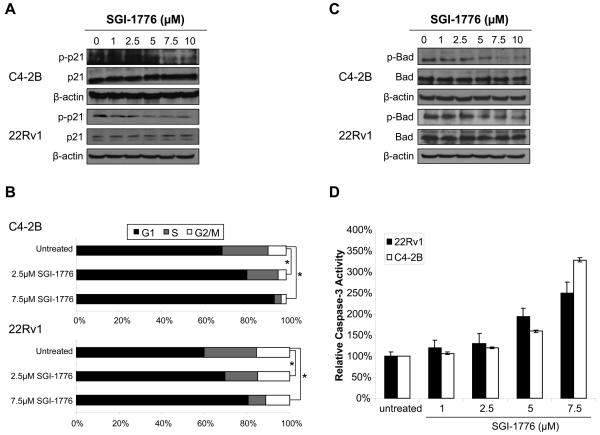
SGI-1776 causes cell cycle arrest and caspase-dependent apoptosis in prostate cancer cells
We next wanted to investigate whether SGI-1776 was capable of altering specific substrates of Pim kinase (i.e. p21 and Bad) in prostate cancer cells, which may ultimately contribute to prostate cancer growth inhibition. We focused our subsequent studies on the 22Rv1 and C4-2B cells, which demonstrate the maximal response in presence of SGI-1776. Additionally, both lines are hormone-refractory and express the androgen-receptor (AR) making them clinically relevant model systems for studying prostate cancer.
Pim-1 kinase supports cell cycle progression by phosphorylating the cell cycle inhibitor, p21Cip1/WAF1 at the Thr145 residue [14]. Increasing concentrations of SGI-1776 reduced phospho-p21 Thr145 protein levels while total p21 remained constant (Fig. 3a). Maximal inhibition of phospho-p21Thr145 was observed at 5μM and 7.5μM in 22Rv1 and C4-2B cells, respectively. In addition, treatment with SGI-1776 for 24 hours caused a G1 arrest in a dose-dependent manner, inhibiting the natural progression to S phase (Fig. 3b). For C4-2B, the percentage of cells in the G1 phase went from 72% ± 3.28 in the untreated group, to 81% ± 1.24 with the addition of 2.5μM SGI-1776, and 95% ± 0.16 with 7.5μM SGI-1776 (p<0.05). The 22Rv1 line had approximately 60% ± 0.03 of untreated cells in the G1 phase and then following treatment with 2.5μM and 7.5μM SGI-1776, the percentage of cells in G1 increased to 70% ± 2.00 and 81% ± 1.17, respectively (p<0.05).
Figure 3. SGI-1776 treatment causes cell cycle arrest and apoptosis in prostate cancer cells.
(A) Western blot analysis of phospho-p21Thr145 and total p21 was performed on C4-2B and 22Rv1 cells after a 5 hour treatment with SGI-1776. β-actin was used as a lane loading control. (B) Flow cytometry analysis of C4-2B and 22Rv1 treated with SGI-1776 for 24 hours was performed. Results from three different experiments were averaged and displayed in this figure. (C) Western blot analysis probing for phospho-BadSer112 and total Bad was performed on C4-2B and 22Rv1 cells treated with increasing doses of SGI-776 for 5 hours. β-actin was used as a lane loading control. (D) Caspase-3 activity was measured using a fluorometric protease assay after treatment with increasing doses of SGI-1776 for 24 hours. The assay was run in duplicate and the results were normalized to the untreated samples.
Besides the ability of Pim-1 to help regulate the cell cycle through the G1/S transition, this serine/threonine kinase has also been shown to have anti-apoptotic potential through its phosphorylation of Bad at serine residue 112 [10]. Western blot analysis performed on C4-2B and 22Rv1 cells treated with increasing doses of SGI-1776 revealed a clear dose-dependent decrease in phosphorylated BadSer112 protein levels, while total Bad levels remained unchanged (Fig. 3c). A reduction in phosphorylation of Bad ultimately leads to the release of cytochrome c from the mitochondria into the cytosol, which triggers the activation of caspase-9 and caspase-3 resulting in cell death [10,35]. To confirm this mechanism of action, cells were exposed to increasing doses of SGI-1776 for 24 hours and apoptosis was determined by measuring the induction of caspase-3 activity compared to the untreated samples. As evident in Fig. 3d, inhibition of Pim kinase activity with increasing concentrations of SGI-1776 caused a dose-dependent increase in caspase-3 activity levels in both C4-2B and 22Rv1 cells, signifying the induction of apoptosis. There was a concomitant increase in levels of cleaved Poly(ADP-ribose) polymerase-1 (PARP), a substrate of caspase-3, further indicating apoptosis induction with SGI-1776 treatment (Supplementary Fig. 1).
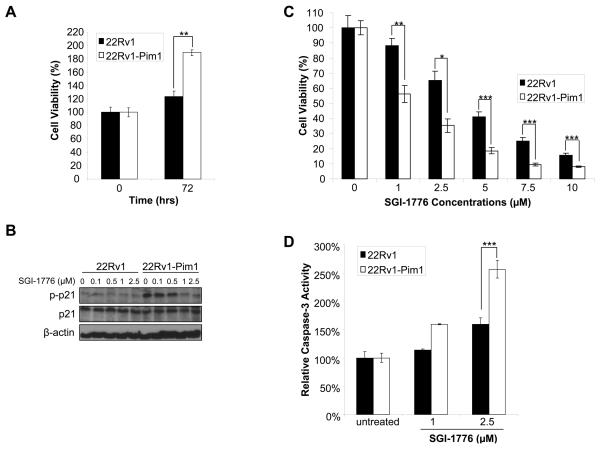
Overexpression of recombinant Pim-1 kinase increases SGI-1776 sensitivity
In order to further validate that SGI-1776 can specifically target Pim kinases, which trigger the observed cytotoxic effects seen in prostate cancer cell lines, we stably overexpressed recombinant Pim-1 in the 22Rv1 cell line and compared the overall SGI-1776 treatment responses to that of the parental line. Initial characterization of the 22Rv1-Pim1 cell line confirmed Pim-1 overexpression at the protein level (Supplementary Fig. 2) as well as demonstrated increased cell growth compared to the 22Rv1 line (Fig. 4a).
Figure 4. Effect of SGI-1776 on inhibiting Pim kinase activity in prostate cancer cells stably overexpressing recombinant Pim-1.
(A) Cell growth over a period of 72 hours was established in the 22Rv1 and 22Rv1-Pim1 cell lines using the ATP viability assay. The results are displayed as an average of four individual wells at each time point. (B) Phospho-p21Thr145 and total p21 protein levels were examined in 22Rv1 and 22Rv1-Pim1 cells after treatment with increasing doses of SGI-1776 for 2 hours. (C) Cell viability was compared between 22Rv1 and 22Rv1-Pim1 cells treated with increasing concentrations of SGI-1776 after 72 hours. The results are displayed as an average of four individual wells. (D) Caspase-3 activity was determined using a fluorometric protease assay after treatment with increasing doses of SGI-1776 for 72 hours. The samples were run in triplicate and the results were normalized to untreated samples.
To address the specificity of SGI-1776 as a Pim kinase inhibitor, we examined the effects of SGI-1776 treatment on p-p21Thr145 inhibition, which is a direct substrate of Pim-1. Treatment of the 22Rv1-Pim1 cells with increasing doses of SGI-1776 revealed a dramatic inhibition in p-p21Thr145 abundance at 1μM SGI-1776 compared to a minimal, if any, effect in the 22Rv1 line at this dose (Fig. 4b). It is worth noting that a significant decrease in p-p21Thr145 in the parental 22Rv1 cells was first observed between 2.5-5μM of SGI-1776 (Fig. 3a) under similar experimental conditions. It is also important to mention that Pim-1 overexpression considerably increased levels of p-p21Thr145 in the 22Rv1-Pim1 cell line as is expected with an enhanced Pim kinase activity.
A side by side comparison of cell viability after 72 hours of treatment with increasing concentrations of SGI-1776 demonstrated an approximate 3-fold reduction in IC50 in the 22Rv1-Pim1 line compared to the 22Rv1 line, suggesting that overexpression of the Pim-1 target increases SGI-1776 sensitivity and resulting cytotoxicity (Fig. 4c). Similarly, treatment of 22Rv1-Pim1 cells with SGI-1776 also led to a greater fold induction of apoptosis compared to 22Rv1 cells (1.6 fold at 2.5μM SGI-1776; p<0.0001) as measured by a caspase-3 fluorometric protease assay (Fig. 4d).
Taken together, these data demonstrate that SGI-1776 inhibits Pim-1 kinase in androgen-independent 22Rv1 prostate cancer cells, which results in G1 cell cycle arrest followed by an apoptotic induction.
SGI-1776 marginally sensitizes prostate cancer cells to taxane-based therapeutics
Previously, it has been shown that Pim-1 acts as a survival factor in the presence of chemotherapeutic agents [25]. In addition to the evidence presented above, which illustrates the inhibitory effects of SGI-1776 as a single agent, we were interested in determining whether SGI-1776 is capable of sensitizing prostate cancer cells to chemotherapy treatment. We treated 22Rv1 cells with increasing doses of paclitaxel in the presence or absence of SGI-1776 for 48 hours followed by an assessment of cell viability. We established sensitivity to paclitaxel and SGI-1776 as single agents as evidenced by a dose-dependent reduction in viability (Fig. 5a). We observed an additional cytotoxic effect when SGI-1776 was combined with paclitaxel treatment at specific doses. For example, 2.5μM SGI-1776 and 2.5nM paclitaxel resulted in 63% and 62.6% viability, respectively, as single agents. Yet, when the same concentrations of each compound were added together, the cell viability decreased to 42.2%, signifying a marginal benefit with combination therapy (p<0.0001) (Fig. 5a). Similar results were observed in presence of docetaxel and SGI-1776 (data not shown). Although Pim kinase inhibition with SGI-1776 did result in a minor enhancement of taxane-sensitization, a two-way ANOVA analysis revealed that this therapeutic combination was neither additive nor synergistic in prostate cancer cells.
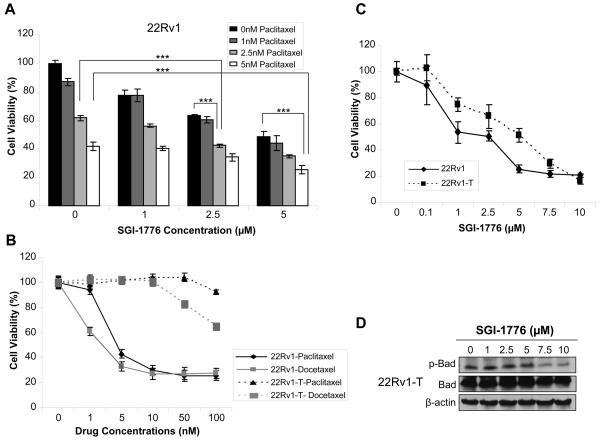
Figure 5. Alterations in cell viability using SGI-1776 combination therapy with taxane-based chemotherapy and characterization of a taxane-resistant prostate cancer cell line.
(A) Cell viability was determined for 22Rv1 cells treated with SGI-1776 or paclitaxel as single agents or in combination for 48 hours. The results were displayed as percent viability compared to the untreated samples. Each condition was the average of six individual wells. (B) Cell viability was determined for 22Rv1 and 22Rv1-T cells in the presence of increasing doses of paclitaxel and docetaxel after 72 hours. (C) Cell viability was assessed in the 22Rv1 and 22Rv1-T cell lines after 72 hours of being in the presence of increasing concentrations of SGI-1776. (D) Western blot analysis for phospho-BadSer112 and total Bad in the 22Rv1-T cell line after treatment with SGI-1776 for 5 hours. β-actin was used as a lane loading control.
Generation and characterization of a taxane-resistant prostate cancer line
With the 22Rv1 cell line being the most sensitive to SGI-1776 treatment, we generated a taxane-resistant form of this line (22Rv1-T) to examine the effects of Pim kinase inhibition on acquired resistance to paclitaxel. As seen in Fig. 5b, the 22Rv1-T cell line is clearly resistant even at high doses (100nM) of paclitaxel with little decline in cell viability observed. This result is compared to the 22Rv1 parental cell line, which is sensitive to paclitaxel as evidenced by a reduction in cell viability in a dose dependent manner. We confirmed that the 22Rv1-T line was also resistant to increasing doses of docetaxel, which is a current standard treatment for advanced hormone-refractory prostate cancer [36]; however, a slight decline in viability was observed at the higher doses (i.e. starting around 50nM) of the compound (Fig. 5b). The approximate IC50s for the 22Rv1 cell line treated with paclitaxel and docetaxel were 4.5nM ± 0.035 and 2.5nM ± 0.034, respectively. On the other hand, the 22Rv1-T cell line had IC50s >100nM when treated with either taxane.
After confirmation of resistance, we further characterized the paclitaxel-resistant line to elucidate the mechanism of chemoresistance. Several reports have alluded to multidrug resistance (MDR) mechanisms as the cause for resistance to chemotherapy agents in prostate cancer [37,38]. Therefore, we investigated whether multidrug resistance in the 22Rv1-T line was mediated by ATP-binding cassette (ABC) transporters such as multidrug resistance 1 (MDR1), breast cancer resistance protein (BCRP), or multidrug resistance protein 1 (MRP1). Both real-time RT-PCR and western blot analysis demonstrated overexpression of MDR1 mRNA and protein levels in the 22Rv1-T cell line compared to the parental 22Rv1 line (Supplementary Fig. 3a). BCRP and MRP1 were not overexpressed in the taxane-resistant prostate cancer cell line (data not shown).
Taxane-resistant prostate cancer cells are sensitive to SGI-1776
Following the characterization of the 22Rv1-T cell line, we investigated the effects of Pim kinase inhibition on cell viability in this prostate cancer model of acquired taxane-resistance. 22Rv1 and 22Rv1-T cells were treated with increasing concentrations of SGI-1776 for 72 hours. Assessment of viability in these two lines revealed that both are sensitive to SGI-1776, with the 22Rv1 parental line displaying a better overall response to treatment with the inhibitor than 22Rv1-T. The approximate IC50s for the 22Rv1 and 22Rv1-T cell lines treated with SGI-1776 were 2.5μM and 5μM, respectively (Fig. 5c).
We further verified that SGI-1776 was indeed modulating the downstream targets of Pim kinases in the 22Rv1-T cell line. Phosphorylation levels of the anti-apoptotic factor Bad were determined using identical conditions as depicted with the parental 22Rv1 cell line (Fig. 3c). Analogous to 22Rv1, there was a dose-dependent decrease in phosphorylated Bad Ser112 protein levels with SGI-1776 treatment with maximal inhibition occurring between 5-7.5μM, while total Bad levels remained unchanged (Fig. 5d).
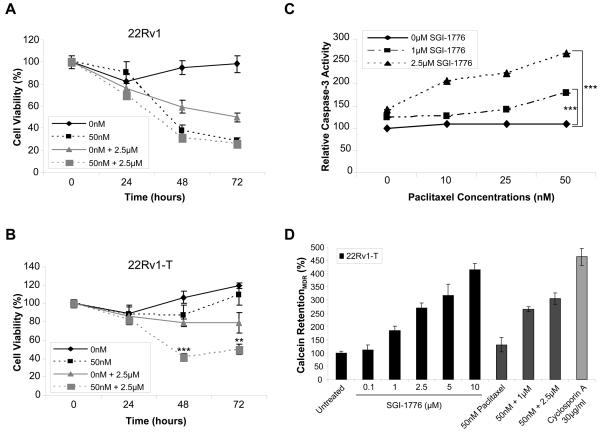
SGI-1776 resensitizes taxane-resistant prostate cancer cells to paclitaxel by inhibition of MDR1 activity
Recently, it has been suggested that targeting Pim-1 activity is capable of resensitizing drug resistant tumor cells to chemotherapeutic agents [38]. Accordingly, we predicted that SGI-1776 mediated Pim kinase inhibition would be able to overcome acquired taxane resistance in the 22Rv1-T model. A comparative time course analysis (0, 24, 48, and 72 hours after drug treatment) in 22Rv1 and 22Rv1-T cells in the presence and absence of SGI-1776 and paclitaxel as single agents or in combination was performed. As illustrated in Fig. 6b, the 22Rv1-T cell line demonstrated resistance to 50nM of paclitaxel over time compared to the 22Rv1 line, which exhibited a clear sensitivity to an equivalent dose of paclitaxel (Fig. 6a). Most striking, is the evidence that presence of SGI-1776 resensitizes the 22Rv1-T cells to 50nM paclitaxel equivalent to similar levels observed in the 22Rv1 paclitaxel-sensitive line. Specifically, the 22Rv1-T cell line does not respond to 50nM of paclitaxel alone and shows a minimal response to 2.5μM SGI-1776; however, when these two agents are combined, the cell viability decreases by as much as 40% in a time course experiment (p<0.0001) (Fig. 6b). In addition, SGI-1776 was able to re-sensitize the taxane-resistant cells to docetaxel at similar concentrations (data not shown).
Figure 6. The ability of SGI-1776 to resensitize a multidrug resistant cell line to taxanes through Pim inhibition.
(A) Cell viability was determined after treatment of 22Rv1 cells with SGI-1776 and paclitaxel either alone or in combination over a period of 72 hours. (B) Cell viability was assessed in 22Rv1-T cells after treatment with SGI-1776 and paclitaxel as single agents or in combination over a period of 72 hours. Each condition is represented as the average of six individual wells. (C) Quantitation of cell death in the 22Rv1-T cell line when treated with paclitaxel and SGI-1776 for 24 hours by determining the caspase-3 activity. The samples were run in triplicate and the results were normalized to the untreated samples. (D) MDR1 inhibition was determined using a calcein fluorescence-based assay. 22Rv1-T cells were treated with increasing doses of SGI-1776 and/or paclitaxel for 15 minutes and the quantity of fluorescent calcein retention was measured. This assay was run in triplicate and the results were normalized to the untreated samples.
Next, we demonstrated that SGI-1776 was capable of inducing apoptosis in the acquired taxane-resistant model system. A DNA specific dye, Hoechst 33342, was used to visualize the nuclear morphology in the 22Rv1-T cells after 24 hours of drug treatment. Supplementary Figure 4 depicts condensed chromatin, a characteristic of apoptotic nuclei, in 22Rv1-T cells in the presence of 2.5μM SGI-1776 alone, which is dramatically enhanced when 2.5μM SGI-1776 is combined with 50nM of paclitaxel. In addition, a more extensive quantitative analysis of apoptosis was performed by examining caspase-3 activity levels in 22Rv1-T cells treated with two different doses of SGI-1776 in the presence of increasing concentrations of paclitaxel. Again, we confirm that the 22Rv1-T cells are resistant to increasing doses of paclitaxel as evidenced by a lack of change in caspase-3 levels across the various treatments. More importantly, a gradual increase in caspase-3 activity is detected as SGI-1776 is combined with increasing doses of paclitaxel (Fig. 6c). For example, addition of 2.5μM SGI-1776 (142% ± 3) increases caspase-3 activity by 1.42 fold compared to the untreated cells (100% ± 2). However, when 2.5μM SGI-1776 is combined with 50nM paclitaxel, the caspase-3 activity level is increased by 2.7 fold (269% ± 8) (p<0.0001).
After demonstrating the ability of SGI-1776 to resensitize multidrug resistant prostate cancer cells to taxanes, it was important to gain insight on the mechanism by which this Pim kinase inhibitor is able to reverse the resistance process. SGI-1776 treatments did not alter MDR1 mRNA expression levels in 22Rv1-T cells (Supplementary Fig. 3b); however, it did inhibit MDR1 activity, which is the likely mechanism for reversing taxane-resistance. Specifically, we utilized an assay that is based on the fluorogenic dye calcein acetoxymethyl ester (calcein AM) as a substrate for the efflux activity of MDR1 and measures the intensely fluorescent calcein which accumulates in the cytoplasm. In 22Rv1-T cells, the overexpression of MDR1 prevents a majority of calcein AM to cross the cell membrane and be hydrolyzed, thus reducing the amount of fluorescent calcein retained inside the cell in comparison to the non-MDR1 parental 22Rv1 line. Yet, when 22Rv1-T cells were treated for 15 minutes with varying concentrations of SGI-1776, a dose-dependent increase in fluorescent calcein retention was observed (Fig. 6d). On the contrary, paclitaxel treated cells were no different from the untreated cells with respect to calcein accumulation. Combination of paclitaxel with SGI-1776 did not further enhance calcein accumulation. Cyclosporin A, a known competitive inhibitor of MDR1-drug binding, was used as a positive control and showed a similar percentage of calcein retention to that obtained with 10μM of SGI-1776. These data indicate that SGI-1776, in addition to serving as a Pim kinase inhibitor, can overcome acquired taxane-resistance by inhibiting MDR1 activity and triggering apoptosis.
Discussion
Pim kinases are intimately involved in tumor progression and several inhibitors targeting these kinases have recently been identified [27,28,30,31,39]. A majority of the Pim kinase inhibitors described to date are specific for the Pim-1 isoform and have mainly been analyzed in leukemia systems and to a lesser degree in prostate cancer [40]. A large proportion of the prostate cancer literature concerning Pim kinases concentrates mainly on Pim-1 expression, although a few studies do report involvement of the other Pim kinase family members [22,31,41]. Despite the fact that the current Pim-1 kinase inhibitors exhibit potential anticancer effects, targeting all three members of the Pim family may be necessary to realize an improved therapeutic response. For this reason, we have identified a selective small molecule inhibitor, an imidazo[1,2-b]pyridazine derivative, against the entire Pim kinase family and present its specific cytotoxic capabilities within several in vitro prostate cancer systems in this study.
SGI-1776 was determined to have low nanomolar affinity for all three Pim family members. It also showed cross-reactivity with two other kinases (FLT3 and Haspin) present in the 300 kinase panel screened. It cannot be ruled out that the observed cytotoxic effects may, in part, be due to FLT3 inhibition; however, our data indicate that SGI-1776 is quite specific for Pim kinases. Furthermore, it is also known that Pim-1 acts downstream of FLT3 [42]. With the use of this potent inhibitor, we demonstrated that inhibition of Pim kinase activity in prostate cancer cells compromised cell viability by inducing cell cycle arrest and apoptosis. SGI-1776 treatment caused molecular alterations consistent with Pim kinase inhibition such as targeting Pim kinase substrates at very specific phosphorylation sites, as seen with Bad at Ser112 and p21 at Thr145. A few other kinases are believed to phosphorylate these exact residues (i.e. RSK1 and protein kinase A), but none of them emerged as SGI-1776 targets in the broad-scale kinase screening assay. Additionally, SGI-1776 was capable of severely inhibiting the enhanced pro-survival signals induced by recombinant Pim-1 overexpression further supporting the specificity of SGI-1776 for Pim kinases. Another important point that emerged from our analysis is that SGI-1776 selectivity is determined by the activity of the Pim kinases rather than the actual expression levels, which is unlike other Pim-1 kinase inhibitors that suggest a correlation between Pim expression levels and efficacy of the compound [4,27].
Interestingly, a correlation was noted in that androgen-independent prostate cancer cell lines appear to be more sensitive to the cytotoxic effects of SGI-1776 compared with the androgen-dependent cell lines. It has been shown that Pim-1 kinase can indirectly modulate AR transcriptional activity in prostate cancer [43]. Given that modifications in AR activity have been associated with the transition to an AI phenotype in prostate cancer progression, it may be valuable to use SGI-1776 to address the role of AR in influencing the anti-apoptotic effects of Pim kinases in AD versus AI systems in future studies.
A current standard treatment for patients with advanced or hormone-refractory prostate cancer is taxane-based chemotherapy [44]. However, the exposure of prostate cancer cells to such cytotoxic agents activates a number of survival pathways that can limit the efficacy of such treatments [45]. Recently, it has been suggested that one of the potential pro-survival signals being activated during this stress response is the Pim-1 kinase family member [26]. Not only does the treatment of prostate cancer cells with docetaxel induce Pim-1 expression, it has also been shown that overexpression of Pim-1 protects prostate cancer cells from the apoptotic effects of these cytotoxic drugs [25,26,38]. This brings up the question of whether modulation of Pim kinase activity by a small molecule inhibitor could sensitize prostate cancer cells to taxane-based therapies. As evident by our studies in the 22Rv1 prostate cancer cell line, we suggest that targeting Pim kinases through SGI-1776 treatment in combination with taxanes can generate an additional effect with respect to cell viability. Consistent with our data, Xie et al. demonstrated a similar result when the Pim-1 isoform was inhibited through siRNA techniques and combined with chemotherapy drugs [25,38]. Our ability to achieve greater clinical benefit, in the model systems studied, with a combination therapy that utilizes lower overall doses of a pharmacological agent against Pim kinases and paclitaxel than required as single agents suggests additional avenues for treatment of this disease.
Although chemotherapy as a first line treatment may initially be successful at inducing apoptosis, eventually the cancer cells become resistant to its effects. Understanding the mechanism for chemo-resistance in prostate cancer cells and targeting candidate markers in order to sensitize these cells to a chemotherapy regimen is important for effectively treating prostate cancer patients. To investigate this issue, we utilized the acquired taxane-resistant 22Rv1-T cell line to ascertain the role of Pim kinases in governing the chemotherapeutic response of prostate cancer cells. Indeed, inhibiting Pim kinase activity with SGI-1776 was able to overcome paclitaxel-resistance by resensitizing the 22Rv1-T prostate cancer cells to taxane treatment. A previous study also demonstrated that knockdown of Pim-1 by siRNA was able to overcome resistance to chemotherapeutic agents in drug resistant prostate cancer cell lines [38]. The authors suggest that the potential for Pim-1 to confer resistance is in part due to its ability to phosphorylate the half ABC transporter, BCRP/ABCG2. Incidences of BCRP overexpression have also been noted in other multidrug resistant cell lines [46]. However, BCRP expression was not found to be induced in our 22Rv1-T cell line, rather another member of the ABC transporter family, MDR1, was demonstrated to be overexpressed. Therefore, the ability to overcome drug resistance mediated by MDR1 through pharmacological inhibition of Pim kinases is a novel finding. Several prostate cancer studies have demonstrated the involvement of MDR1 in the development of drug resistance, including one study that found overexpression of MDR1 in two established paclitaxel-resistant prostate cancer cell lines [47]. Drug resistance is a complex process that involves several multi-drug resistant proteins and varies between systems. Through further investigation into the process leading to reversal of chemoresistance, we discovered that SGI-1776 is an inhibitor of MDR1 efflux activity. The proapoptotic effects of this Pim kinase inhibitor in combination with its ability to block MDR1 activity provide strong mechanistic evidence for the ability of SGI-1776 to resensitize chemoresistant cells to taxanes. Further exploration into the manner in which SGI-1776 interferes with MDR1 activity is still needed as well as determining whether this phenomenon is applicable to other drug resistant phenotypes (i.e. MRP1 and BCRP) in prostate cancer.
The study presented here is a comprehensive examination of a Pim family small-molecule inhibitor displaying anticancer activity in prostate cancer cell lines that are sensitive and resistant to chemotherapy. Given the complexity of prostate cancer development, targeting a single kinase may not be sufficient to generate an effective clinical response, suggesting combination therapy inhibiting multiple signaling cascades may be a more beneficial strategy. In this report, we provide evidence that Pim kinase inhibition using SGI-1776 in combination with chemotherapy treatment can promote taxane sensitivity in prostate cancers and may overcome acquired taxane-resistance by inhibiting MDR1 activity. Preliminary studies in leukemia have shown in vivo efficacy with SGI-1776 treatment. Studies are ongoing in prostate cancer xenografts to demonstrate anti-tumor activity and modulation of chemoresistance by SGI-1776 in vivo. Currently, this compound is being investigated in human clinical trials for hormone- and docetaxel-refractory prostate cancer as well as relapsed or refractory lymphoma.
Supplementary Material
Acknowledgments
The authors would like to thank Sabrina Lei for her assistance with data review and analysis, Rajashree Joshi for her advice on drug formulations, Doug Evans for the generation of the taxane-resistant cell line, and Jim Mirocha for the ANOVA statistical analysis.
Grant support:
This work was supported by the Sumner Redstone Prostate Cancer Research Program (D.B.A. and A.J.), the National Cancer Institute U54 CCNE Award (CA119367; D.B.A. and A.J.), and the Jerry and Joyce Monkarsh Young Investigator Award from the Prostate Cancer Foundation (A.J.)
Abbreviations
- ABC
ATP binding cassette
- MDR1
multidrug resistance 1
- MRP1
multidrug resistance protein 1
- BCRP
breast cancer resistance protein
- AR
androgen-receptor
- AD
androgen-dependent
- AI
androgen-independent
References
- 1.Amaravadi R, Thompson CB. The survival kinases Akt and Pim as potential pharmacological targets. J Clin Invest. 2005;115:2618–24. doi: 10.1172/JCI26273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eichmann A, Yuan L, Breant C, Alitalo K, Koskinen PJ. Developmental expression of pim kinases suggests functions also outside of the hematopoietic system. Oncogene. 2000;19:1215–24. doi: 10.1038/sj.onc.1203355. [DOI] [PubMed] [Google Scholar]
- 3.Allen JD, Verhoeven E, Domen J, van der Valk M, Berns A. Pim-2 transgene induces lymphoid tumors, exhibiting potent synergy with c-myc. Oncogene. 1997;15:1133–41. doi: 10.1038/sj.onc.1201288. [DOI] [PubMed] [Google Scholar]
- 4.Hu XF, Li J, Vandervalk S, Wang Z, Magnuson NS, Xing PX. PIM-1-specific mAb suppresses human and mouse tumor growth by decreasing PIM-1 levels, reducing Akt phosphorylation, and activating apoptosis. J Clin Invest. 2009 doi: 10.1172/JCI33216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Z, Bhattacharya N, Weaver M, et al. Pim-1: a serine/threonine kinase with a role in cell survival, proliferation, differentiation and tumorigenesis. J Vet Sci. 2001;2:167–79. [PubMed] [Google Scholar]
- 6.Cuypers HT, Selten G, Quint W, et al. Murine leukemia virus-induced T-cell lymphomagenesis: integration of proviruses in a distinct chromosomal region. Cell. 1984;37:141–50. doi: 10.1016/0092-8674(84)90309-x. [DOI] [PubMed] [Google Scholar]
- 7.Selten G, Cuypers HT, Berns A. Proviral activation of the putative oncogene Pim-1 in MuLV induced T-cell lymphomas. Embo J. 1985;4:1793–8. doi: 10.1002/j.1460-2075.1985.tb03852.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yip-Schneider MT, Horie M, Broxmeyer HE. Transcriptional induction of pim-1 protein kinase gene expression by interferon gamma and posttranscriptional effects on costimulation with steel factor. Blood. 1995;85:3494–502. [PubMed] [Google Scholar]
- 9.Bachmann M, Moroy T. The serine/threonine kinase Pim-1. Int J Biochem Cell Biol. 2005;37:726–30. doi: 10.1016/j.biocel.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Aho TL, Sandholm J, Peltola KJ, Mankonen HP, Lilly M, Koskinen PJ. Pim-1 kinase promotes inactivation of the pro-apoptotic Bad protein by phosphorylating it on the Ser112 gatekeeper site. FEBS Lett. 2004;571:43–9. doi: 10.1016/j.febslet.2004.06.050. [DOI] [PubMed] [Google Scholar]
- 11.Li YY, Popivanova BK, Nagai Y, Ishikura H, Fujii C, Mukaida N. Pim-3, a protooncogene with serine/threonine kinase activity, is aberrantly expressed in human pancreatic cancer and phosphorylates bad to block bad-mediated apoptosis in human pancreatic cancer cell lines. Cancer Res. 2006;66:6741–7. doi: 10.1158/0008-5472.CAN-05-4272. [DOI] [PubMed] [Google Scholar]
- 12.Yan B, Zemskova M, Holder S, et al. The PIM-2 kinase phosphorylates BAD on serine 112 and reverses BAD-induced cell death. J Biol Chem. 2003;278:45358–67. doi: 10.1074/jbc.M307933200. [DOI] [PubMed] [Google Scholar]
- 13.Mochizuki T, Kitanaka C, Noguchi K, Muramatsu T, Asai A, Kuchino Y. Physical and functional interactions between Pim-1 kinase and Cdc25A phosphatase. Implications for the Pim-1-mediated activation of the c-Myc signaling pathway. J Biol Chem. 1999;274:18659–66. doi: 10.1074/jbc.274.26.18659. [DOI] [PubMed] [Google Scholar]
- 14.Wang Z, Bhattacharya N, Mixter PF, Wei W, Sedivy J, Magnuson NS. Phosphorylation of the cell cycle inhibitor p21Cip1/WAF1 by Pim-1 kinase. Biochim Biophys Acta. 2002;1593:45–55. doi: 10.1016/s0167-4889(02)00347-6. [DOI] [PubMed] [Google Scholar]
- 15.Morishita D, Katayama R, Sekimizu K, Tsuruo T, Fujita N. Pim kinases promote cell cycle progression by phosphorylating and down-regulating p27Kip1 at the transcriptional and posttranscriptional levels. Cancer Res. 2008;68:5076–85. doi: 10.1158/0008-5472.CAN-08-0634. [DOI] [PubMed] [Google Scholar]
- 16.Bachmann M, Kosan C, Xing PX, Montenarh M, Hoffmann I, Moroy T. The oncogenic serine/threonine kinase Pim-1 directly phosphorylates and activates the G2/M specific phosphatase Cdc25C. Int J Biochem Cell Biol. 2006;38:430–43. doi: 10.1016/j.biocel.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Wang Z, Li X, Magnuson NS. Pim kinase-dependent inhibition of c-Myc degradation. Oncogene. 2008 doi: 10.1038/onc.2008.123. [DOI] [PubMed] [Google Scholar]
- 18.Ellwood-Yen K, Graeber TG, Wongvipat J, et al. Myc-driven murine prostate cancer shares molecular features with human prostate tumors. Cancer Cell. 2003;4:223–38. doi: 10.1016/s1535-6108(03)00197-1. [DOI] [PubMed] [Google Scholar]
- 19.Moroy T, Verbeek S, Ma A, Achacoso P, Berns A, Alt F. E mu N- and E mu L-myc cooperate with E mu pim-1 to generate lymphoid tumors at high frequency in double-transgenic mice. Oncogene. 1991;6:1941–8. [PubMed] [Google Scholar]
- 20.Cohen AM, Grinblat B, Bessler H, et al. Increased expression of the hPim-2 gene in human chronic lymphocytic leukemia and non-Hodgkin lymphoma. Leuk Lymphoma. 2004;45:951–5. doi: 10.1080/10428190310001641251. [DOI] [PubMed] [Google Scholar]
- 21.Dhanasekaran SM, Barrette TR, Ghosh D, et al. Delineation of prognostic biomarkers in prostate cancer. Nature. 2001;412:822–6. doi: 10.1038/35090585. [DOI] [PubMed] [Google Scholar]
- 22.Chen WW, Chan DC, Donald C, Lilly MB, Kraft AS. Pim family kinases enhance tumor growth of prostate cancer cells. Mol Cancer Res. 2005;3:443–51. doi: 10.1158/1541-7786.MCR-05-0007. [DOI] [PubMed] [Google Scholar]
- 23.Hobisch A, Ramoner R, Fuchs D, et al. Prostate cancer cells (LNCaP) generated after long-term interleukin 6 (IL-6) treatment express IL-6 and acquire an IL-6 partially resistant phenotype. Clin Cancer Res. 2001;7:2941–8. [PubMed] [Google Scholar]
- 24.Ueda T, Bruchovsky N, Sadar MD. Activation of the androgen receptor N-terminal domain by interleukin-6 via MAPK and STAT3 signal transduction pathways. J Biol Chem. 2002;277:7076–85. doi: 10.1074/jbc.M108255200. [DOI] [PubMed] [Google Scholar]
- 25.Xie Y, Xu K, Dai B, et al. The 44 kDa Pim-1 kinase directly interacts with tyrosine kinase Etk/BMX and protects human prostate cancer cells from apoptosis induced by chemotherapeutic drugs. Oncogene. 2006;25:70–8. doi: 10.1038/sj.onc.1209058. [DOI] [PubMed] [Google Scholar]
- 26.Zemskova M, Sahakian E, Bashkirova S, Lilly M. The PIM1 Kinase Is a Critical Component of a Survival Pathway Activated by Docetaxel and Promotes Survival of Docetaxel-treated Prostate Cancer Cells. J Biol Chem. 2008;283:20635–44. doi: 10.1074/jbc.M709479200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holder S, Zemskova M, Zhang C, et al. Characterization of a potent and selective small-molecule inhibitor of the PIM1 kinase. Mol Cancer Ther. 2007;6:163–72. doi: 10.1158/1535-7163.MCT-06-0397. [DOI] [PubMed] [Google Scholar]
- 28.Pogacic V, Bullock AN, Fedorov O, et al. Structural analysis identifies imidazo[1,2-b]pyridazines as PIM kinase inhibitors with in vitro antileukemic activity. Cancer Res. 2007;67:6916–24. doi: 10.1158/0008-5472.CAN-07-0320. [DOI] [PubMed] [Google Scholar]
- 29.Pierce AC, Jacobs M, Stuver-Moody C. Docking study yields four novel inhibitors of the protooncogene Pim-1 kinase. J Med Chem. 2008;51:1972–5. doi: 10.1021/jm701248t. [DOI] [PubMed] [Google Scholar]
- 30.Xia Z, Knaak C, Ma J, et al. Synthesis and evaluation of novel inhibitors of Pim-1 and Pim-2 protein kinases. J Med Chem. 2009;52:74–86. doi: 10.1021/jm800937p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beharry Z, Zemskova M, Mahajan S, et al. Novel benzylidene-thiazolidine-2,4-diones inhibit Pim protein kinase activity and induce cell cycle arrest in leukemia and prostate cancer cells. Mol Cancer Ther. 2009;8:1473–83. doi: 10.1158/1535-7163.MCT-08-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Craft N, Chhor C, Tran C, et al. Evidence for clonal outgrowth of androgen-independent prostate cancer cells from androgen-dependent tumors through a two-step process. Cancer Res. 1999;59:5030–6. [PubMed] [Google Scholar]
- 33.Zhang Y, Wang Z, Magnuson NS. Pim-1 kinase-dependent phosphorylation of p21Cip1/WAF1 regulates its stability and cellular localization in H1299 cells. Mol Cancer Res. 2007;5:909–22. doi: 10.1158/1541-7786.MCR-06-0388. [DOI] [PubMed] [Google Scholar]
- 34.Bearss D. In vivo activity of SGI-1776, an orally active Pim kinase inhibitor. Abs #332. Eur. J. Cancer. 2008:6. [Google Scholar]
- 35.Datta SR, Ranger AM, Lin MZ, et al. Survival factor-mediated BAD phosphorylation raises the mitochondrial threshold for apoptosis. Dev Cell. 2002;3:631–43. doi: 10.1016/s1534-5807(02)00326-x. [DOI] [PubMed] [Google Scholar]
- 36.De Dosso S, Berthold DR. Docetaxel in the management of prostate cancer: current standard of care and future directions. Expert Opin Pharmacother. 2008;9:1969–79. doi: 10.1517/14656566.9.11.1969. [DOI] [PubMed] [Google Scholar]
- 37.van Brussel JP, Mickisch GH. Multidrug resistance in prostate cancer. Onkologie. 2003;26:175–81. doi: 10.1159/000071510. [DOI] [PubMed] [Google Scholar]
- 38.Xie Y, Xu K, Linn DE, et al. The 44-kDa Pim-1 kinase phosphorylates BCRP/ABCG2 and thereby promotes its multimerization and drug-resistant activity in human prostate cancer cells. J Biol Chem. 2008;283:3349–56. doi: 10.1074/jbc.M707773200. [DOI] [PubMed] [Google Scholar]
- 39.Cheney IW, Yan S, Appleby T, et al. Identification and structure-activity relationships of substituted pyridones as inhibitors of Pim-1 kinase. Bioorg Med Chem Lett. 2007;17:1679–83. doi: 10.1016/j.bmcl.2006.12.086. [DOI] [PubMed] [Google Scholar]
- 40.Shah N, Pang B, Yeoh KG, et al. Potential roles for the PIM1 kinase in human cancer - a molecular and therapeutic appraisal. Eur J Cancer. 2008;44:2144–51. doi: 10.1016/j.ejca.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 41.Dai H, Li R, Wheeler T, et al. Pim-2 upregulation: biological implications associated with disease progression and perinueral invasion in prostate cancer. Prostate. 2005;65:276–86. doi: 10.1002/pros.20294. [DOI] [PubMed] [Google Scholar]
- 42.Kim KT, Baird K, Ahn JY, et al. Pim-1 is up-regulated by constitutively activated FLT3 and plays a role in FLT3-mediated cell survival. Blood. 2005;105:1759–67. doi: 10.1182/blood-2004-05-2006. [DOI] [PubMed] [Google Scholar]
- 43.Thompson J, Peltola KJ, Koskinen PJ, Janne OA, Palvimo JJ. Attenuation of androgen receptor-dependent transcription by the serine/threonine kinase Pim-1. Lab Invest. 2003;83:1301–9. doi: 10.1097/01.lab.0000087585.03162.a3. [DOI] [PubMed] [Google Scholar]
- 44.Roth BJ, Yeap BY, Wilding G, Kasimis B, McLeod D, Loehrer PJ. Taxol in advanced, hormone-refractory carcinoma of the prostate. A phase II trial of the Eastern Cooperative Oncology Group. Cancer. 1993;72:2457–60. doi: 10.1002/1097-0142(19931015)72:8<2457::aid-cncr2820720825>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 45.Burchert A, Wang Y, Cai D, et al. Compensatory PI3-kinase/Akt/mTor activation regulates imatinib resistance development. Leukemia. 2005;19:1774–82. doi: 10.1038/sj.leu.2403898. [DOI] [PubMed] [Google Scholar]
- 46.Doyle LA, Ross DD. Multidrug resistance mediated by the breast cancer resistance protein BCRP (ABCG2) Oncogene. 2003;22:7340–58. doi: 10.1038/sj.onc.1206938. [DOI] [PubMed] [Google Scholar]
- 47.Takeda M, Mizokami A, Mamiya K, et al. The establishment of two paclitaxel-resistant prostate cancer cell lines and the mechanisms of paclitaxel resistance with two cell lines. Prostate. 2007;67:955–67. doi: 10.1002/pros.20581. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.