Abstract
This study examined if individuals who are at increased risk for drowsy-driving because of obstructive sleep apnea syndrome (OSAS), have impairments in driving performance in the moments during microsleep episodes as opposed to during periods of wakefulness. Twenty-four licensed drivers diagnosed with OSAS based on standard clinical and polysomnographic criteria, participated in an hour-long drive in a high-fidelity driving simulator with synchronous electroencephalographic (EEG) recordings for identification of microsleeps. The drivers showed significant deterioration in vehicle control during the microsleep episodes compared to driving performance in the absence of microsleeps on equivalent segments of roadway. The degree of performance decrement correlated with microsleep duration, particularly on curved roads. Results indicate that driving performance deteriorates during microsleep episodes. Detecting microsleeps in real-time and identifying how these episodes of transition between wakefulness and sleep impair driver performance is relevant to the design and implementation of countermeasures such as drowsy driver detection and alerting systems that use EEG technology.
Keywords: Obstructive Sleep Apnea Syndrome, Microsleep, Driving Performance, EEG, Driving simulators
1. Introduction
Driver sleepiness is a major cause of motor vehicle crashes and is responsible for approximately 40,000 injuries and 1,500 deaths each year in the US alone (Horne & Reyner, 1995; Knipling & Wang, 1995; Laube et al., 1998; Lyznicki et al., 1998). Royal (2003) estimated that 1.35 million drivers were involved in a drowsy driving related crash in the five years prior to a 2002 US Gallup poll. A US DOT - NHTSA study revealed that there are six million crashes annually resulting in an economic impact of over $230 billion (Blincoe et al., 2002). Thus, over one-sixth of these costs are probably attributed to sleepiness and even this estimate may be relatively low. In a separate study conducted by McCartt et al (1996), approximately 55% of 1000 drivers surveyed indicated that they had driven while drowsy and 23% had fallen asleep at the wheel. This confirms other findings that sleepiness may play a role in crashes that are erroneously attributed to other causes (Connor et al., 2001).
A subgroup of drowsy drivers has Obstructive Sleep Apnea Syndrome (OSAS), a common sleep disorder that affects 2–4% of middle-aged adults (Young et al, 1993). Drivers with OSAS have an increased crash risk that is in the neighborhood of 2–4 times that of the general population (Findley et al., 1995; George et al., 1987; Teran-Santos et al., 1999; Wu & Yan-Go, 1996). Affected individuals typically have fragmented sleep periods associated with snoring and intermittent airway obstruction. This fragmentation of sleep leads to chronic sleep deprivation and excessive daytime sleepiness, and is a likely cause of the cognitive dysfunction that has been found in this population (Bedard et al., 1993; Feuerstein et al., 1997; Kim et al., 1997). However, there are data suggesting that the cumulative effects of chronic repeated episodes of nocturnal hypoxia may also cause irreversible cognitive deficits (Nowak et al, 2006). Regardless of the mechanism by which these deficits occur, improperly treated OSAS has been estimated to cause over $11 billion in motor vehicle crash costs (Sassani et al., 2004). An additional problem is that some individuals with OSAS are unaware of the degree of their sleepiness and cognitive impairment (Engleman et al., 1997; Horstmann et al. 2000). This is clearly a problem that society cannot afford to ignore.
Methods for quantifying driving performance errors associated with sleep onset are of key importance for reducing the number of sleep related crashes. Microsleep episodes are one such potentially useful indicator of sleep onset. They are identified by changes in the electroencephalogram. (EEG), and are associated with brief episodes of loss of attention and blank stares (Thorpy & Yager, 1991). Microsleeps are commonly seen in individuals with excessive daytime sleepiness, and their presence may be a more sensitive indicator of sleepiness than the multiple sleep latency test (Tirunahari et al, 2003). During microsleep episodes, attention lapses can impair the ability to detect and respond to crucial stimuli and events (Dinges & Kribbs, 1991). Moreover, microsleeps have been associated with poor simulated driving performance (Risser et al., 2000; Paul et al, 2005), and have previously been included as part of a multi-parametric alertness monitoring system (Heitmann et al, 2001). Thus, the detection of microsleep episodes might be useful as a means of alerting and warning drowsy drivers.
The goal of this study was to determine if drowsy drivers have deterioration in driving performance during EEG verified microsleep episodes compared to performance during wakefulness. To address this goal we tested the hypotheses that (1) drivers have worse driving performance during microsleeps compared to matched non-microsleep segments and (2) longer microsleeps produce greater declines in driving performance. We tested these hypotheses in a sample of drowsy drivers with OSAS, as outlined in the Methods.
2. Method
2.1. Participants
Twenty-four drivers with OSAS participated in this study (12 women and 12 men). Two of the participants did not complete the entire experiment and were deleted from subsequent analyses. Potential participants were recruited from the Sleep Disorders Clinic in the Department of Neurology at the University of Iowa and compensated $50 (US dollars) for their participation in this study. Participants were excluded if they were no longer driving, acutely ill, or had active, confounding medical conditions (i.e., dementia, major psychiatric and vestibular diseases, alcoholism or other forms of drug addiction, or used the following medications; stimulants, antihistamines, antidepressants, narcotics, anxiolytics, anticonvulsants and other major psychoactive medications). Potential subjects were also excluded if they had irregular sleep-wake cycles, consumed seven or more cups of coffee (or an equivalent amount of other caffeinated beverages) daily, or currently smoked cigarettes (Ohayon et al., 1997; Soldatos et al., 1980; Wetter & Young, 1994). Individuals with diseases of the optic nerve, retina, or ocular media were excluded only if they had a corrected visual acuity of less than 20/50.
The clinical criteria for the diagnosis of OSAS were 1) a complaint of excessive daytime sleepiness or insomnia, 2) witnessed or self-reported episodes of obstructed breathing during sleep, and 3) at least one of the following; snoring, morning headaches, or dry mouth upon awakening (AASM, 2005). Potential subjects were referred to the Sleep Disorders Clinic with a clinical suspicion of OSAS and were not yet treated with continuous positive airway pressure (CPAP). Recruitment occurred at the time of their clinic visit, which occurred between 8 a.m. and noon. The Epworth Sleepiness Scale (ESS) (Johns, 1991), which was completed during their visit, was used to assess subjective sleepiness. All subjects meeting clinical criteria for OSAS underwent the simulated drive at 2 pm, with polysomnography (PSG) completed that night. All subjects had an apnea-hypopnea index of 5 or greater on PSG. Both apneas and hypopneas had a duration of at least 10 seconds. Hypopneas were defined as having a 30% or greater reduction in airflow or effort associated with either a 3–4% or greater drop in oxygen saturation or EEG arousal (Butkov, 1996).
2.2. Apparatus
The driving scenarios were implemented on the Simulator for Interdisciplinary Research in Ergonomics and Neuroscience (SIREN). This driving simulator has a four-channel, 150-degree forward view, and 50-degree rear view (Rizzo et al., 2000). All street signs and road scenarios conform to the requirements of AASHTO (American Association of State Highway and Transportation Officials) and MUTCD (Manual for Uniform Traffic Control Devices). External devices such as EEG and video collection were integrated into and synchronized with the simulator.
EEG was recorded in all drivers for identification of microsleep episodes and was performed using a Neurofax EEG-2100 (Nihon Khoden Corp, Tokyo) with 16-bit A/D conversion and sampling frequency of 200Hz. Electrodes were placed according to the international 10–20 system (Klem et al., 1993) with C3/4-A1/2 and O1/2-A1/2 used as the primary scoring channels, with bipolar derivations (e.g., C3/4-T3/4 and O1/2-T5/6) used when tracings were ambiguous or obscured by artifact. The electro-oculogram (EOG) was recorded to monitor eye movement artifacts. Electrodes were placed lateral and above the left outer canthus, and lateral and below the right outer canthus, with both referenced to A1 (Rechtschaffen & Kales, 1968).
2.3. Experimental Design
The independent variables in the analysis were road type (curve, straight), and occurrence (yes, no) and duration (short, medium, long) of microsleep episodes. Microsleep episodes were identified by visual inspection of the EEG, and were defined as 3 to 14 second artifact-free episodes during which 4–7 Hz (theta) activity replaced the waking 8–13 Hz (alpha) background rhythm (Harrison & Horne, 1996). A neurologist certified by the American Board of Sleep Medicine (author Tippin) interpreted the EEG and was blinded to the subjects’ driving performance. It was not uncommon to have small fragments of alpha activity (< 0.5 seconds in duration) intermixed with theta during microsleeps. Similarly, alpha often slowed in frequency at the beginning of a microsleep episode. These fragments and adjacent portions of persisting alpha activity were included in the microsleep if the frequency of alpha had declined from baseline by more the 1 Hz. The inclusion of this alpha activity is reasonable as alpha slowing of this degree has been shown to accompany vigilance errors (Valley & Broughton, 1983). Portions of EEG wherein changes in alpha were ambiguous or explained by the physiological blocking response (Niedermeyer, 2005), or those in which EEG was obscured by artifact were excluded from analysis. The goal of the study was centered on examining whether or not driving performance declines during well-defined microsleeps and for that reason, no attempt was made to calculate an artifact rate. As noted previously, EOG was used to monitor eye movement artifacts. This activity never interfered with the identification of alpha, especially in the occipital areas (both central and occipital channels were used to identify alpha).
Dependent measures of driver performance were speed, lane keeping, and steering control. The mean vehicle speed assessed how well drivers maintained speed control during microsleep episodes as in previous studies of OSAS in a driving simulator (Risser et al., 2000). Lane keeping behavior was assessed by the standard deviation in lane position (SDLP) and was calculated as the distance between the vehicle midline and lane centerline. SDLP is a frequently used metric (George, 2004; Risser et al., 2000; Summala et al., 1996) that indexes road tracking error or “weaving”. This increases as a driver loses control over the vehicle’s lateral position (de Waard & Brookhuis, 1991; Lenne et al., 1998; Ramaekers, 2003). The standard deviation of steering wheel angle (SDSWA) was also measured. High SDSWA is strongly correlated with poor steering control due to drowsiness or increased workload (Furukawa et al., 1990). The minimum time to lane crossing (TLC) provided another safety index, as in previous studies of drowsy drivers (van Winsum et al., 2000). The TLC is the time that it takes the vehicle to reach one of the lane boundaries (i.e., road shoulder or oncoming traffic lane) assuming the driver maintains the same steering wheel angle (Lin & Ulsoy, 1995). Greater TLCs are considered safer (Godthelp, 1986; Kwon et al., 1999; Lin & Ulsoy, 1995).
As a secondary goal, the results of SDLP, SDSWA, and min TLC measures are compared to another measure known as steering entropy (SE), a measure of randomness of steering control (Nakayama et al., 1999) to determine whether these measures would yield similar or complementary results (Paul et al., 2005a). SE is based on a Taylor series expansion of steering over time, has been used to evaluate workload changes due to alcohol (Rakauskas and Ward, 2005) and driver distraction (Donmez et al, 2006), and may provide additional evidence on changes in driver workload and vigilance across changing driving environments.
2.4. Procedure
Each participant completed a simulated drive scenario lasting approximately 60 minutes. Prior to beginning the experiment, a research assistant conducted a “warm-up and training” session lasting 5 to 10 minutes to familiarize the drivers with the vehicle controls in previous work using this simulator (McGehee et al., 2004). The familiarization session was conducted on a segment of a simulated 2-lane highway that was similar to what the drivers would be immersed in during data collection. Afterward, drivers completed a brief checklist of vehicle knowledge and operations to assure a level of proficiency sufficient to proceed with the experiment.
During the experiment, participants drove on a simulated 2-lane highway comprising three identical drive segments. Each drive segment included two straight road types and two gradual curves (radii= 600 meters). There were approximately 24,800 meters of straight road and 5,600 meters of curved sections for each segment. The participants were instructed to drive at the posted speeds of 55 mph (~89 km/h). The drive scenario contained minimal traffic or distractions and was representative of drives that may induce drowsiness. The simulator drive was performed at a fixed time in the afternoon (2 p.m.), in order to maximize driver sleepiness, increase the likelihood of recording microsleeps, and minimize confounding effects of the circadian fluctuation in alertness (Van Dongen & Dinges, 2005).
2.5. Statistical analysis
A case-crossover analysis compared case (microsleep) to control (non-microsleep) episodes. In this analysis, each participant served as his or her own control, eliminating confounding effects of age, gender, training, driving record, and other fixed characteristics (Maclure, 1991). The experimental drive comprised three repeating segments of identical roadway terrain. This allowed a 2:1 matched approach in which the driving performance on a segment where a microsleep occurred was matched with the performance at the corresponding location in the other two segments (when a microsleep did not occur).
The analysis of the dependent measures was conducted using a mixed linear model (i.e., PROC MIXED statement in SAS version 9.1). In the case-crossover design, a drive segment containing a microsleep is compared to the other two segments where a microsleep episode did not occur. However, the specific segment is not known and is therefore accounted for as a covariate in our model. Randomness associated with each microsleep event was also accounted for in the model. Dependent variables were appropriately transformed in order to support the normality assumption of an ANOVA model.
A preliminary analysis demonstrated a strong correlation between SDLP and SDSWA (ρ =0.88, p<0.0001), followed by SDLP and SE (ρ =0.34, p=0.044). However, there was no significant correlation between SDSWA and SE (ρ =0.25, p=0.146). Because the dependent steering measures are correlated, MANOVA is performed on these variables to control for overinflation of the Type I error. Significant findings are followed-up with univariate ANOVAs to assess the magnitude of the effect that each dependent variable has on the independent variables.
3. Results
The mean ages of the drivers were 46.9 (sd=11.5) years for men and 52.1 (sd= 6.8) years for women. The mean ESS score was 11.0 (sd= 5.0). A score greater than 10 is generally accepted as an indicator of excessive subjective sleepiness (Johns, 1991). There were over 150 microsleep episodes identified among the OSAS drivers used for the subsequent analysis.
3.1. Microsleep Occurrence and Performance Measures
Differences in performance between segments with and without microsleep episodes were evaluated based on mean speed, SDLP, SDSWA, and steering entropy. The averages for each performance measure stratified by microsleep episodes (yes or no) and road type are provided in Table 1.
Table 1.
The effects of microsleeps (and comparison non-microsleeps) on driving performance measures by roadway type
| Dependent Variables | Roadway | Episodes* | N | Mean | Std Dev |
|---|---|---|---|---|---|
| Mean Speed (km/hr) | Straight | Microsleep | 117 | 26.363 | 3.263 |
| Non Microsleep | 231 | 26.576 | 2.669 | ||
| Curve | Microsleep | 34 | 26.354 | 3.132 | |
| Non Microsleep | 68 | 26.633 | 2.129 | ||
| SDLP (meters) | Straight | Microsleep | 117 | 0.160 | 0.122 |
| Non Microsleep | 231 | 0.142 | 0.104 | ||
| Curve | Microsleep | 34 | 0.209 | 0.127 | |
| Non Microsleep | 68 | 0.169 | 0.101 | ||
| SDSWA | Straight | Microsleep | 117 | 1.967 | 1.763 |
| Non Microsleep | 231 | 1.782 | 1.735 | ||
| Curve | Microsleep | 34 | 2.946 | 1.840 | |
| Non Microsleep | 68 | 2.882 | 1.862 | ||
| Steering Entropy | Straight | Microsleep | 117 | 0.564 | 0.049 |
| Non Microsleep | 231 | 0.551 | 0.060 | ||
| Curve | Microsleep | 68 | 0.557 | 0.062 | |
| Non Microsleep | 34 | 0.567 | 0.397 | ||
| Minimum TLC | Straight | Microsleep | 117 | 3.828 | 3.062 |
| Non Microsleep | 231 | 3.082 | 2.215 | ||
| Curve | Microsleep | 68 | 0.766 | 0.530 | |
| Non Microsleep | 34 | 0.997 | 0.837 |
Note: Driving performance on a drive segment where a microsleep occurred are matched with the performance at the corresponding location in the other two segments
3.1.1. Speed Control
Significant differences in mean speeds were observed with higher speeds observed during non-microsleep episodes (F(1, 418)=4.57, p<0.05). Differences were also observed among the three drive segments (F(2, 417)=16.57, p<0.05) with mean speed increasing with each subsequent segment, but no interaction effects were observed between drive segments and microsleeps (p>0.05). There were also no differences observed in the mean speed between roadway types (p>0.05).
3.1.2. Lateral Control
The MANOVA results indicated that differences existed between straight and curved roads (Wilks’ Lambda F(3, 414)=8.34, p<0.0001), which were attributable to the differences observed in SDSWA (univariate F(1,416)=22.51, p<0.0001) and SDLP (F(1,416)=14.56, p=0.0002), but not in steering entropy (F(1,416)=0.28, p=0.596). Thus, as expected, greater variation was observed in vehicle position and steering control on curves. Differences in lateral performance was also observed between the microsleep and non-microsleep episodes (Wilks’ Lamda F(3,414) = 2.65, p=0.049). Univariate ANOVAs showed that this difference was due to SDLP (F(1, 416)=4.75, p=0.030) and steering entropy (F(1, 416)=4.02, p=0.0457). However, no significant differences were observed in SDSWA (F(1,416)=0.71, p=0.400). There was also a significant difference in drive segments (Wilks’ Lambda F(6,828)=3.67, p=0.0013) but this was attributed solely to differences observed in SE (univariate F(2,416)=11.08, p<0.0001). More specifically, SE significantly increased in the last drive segment (M=0.568) when compared to the first segment (M=0.548). No other differences (in main effects or interactions) were observed among these performance measures.
The minimum TLC was significantly different between road types (F(1,473)=102.69, p<0.05) with mean times significantly lower (overall mean=0.41) on curves compared to straight roads (overall mean = 2.22). There were no other statistically significant differences observed at p<0.05.
3.2. Performance measures and microsleep duration
The duration of microsleep episodes were segmented into three categories: short duration (3 ≤ t < 4.74 seconds), medium duration (4.74 ≤ t < 7.00 seconds), and long durations (t ≥ 7.00 seconds). The values used were based upon the calculated median microsleep duration (4.74) and the calculated 75th percentile (Q3) of all microsleep durations (7.00). The numbers of episodes of short, medium and long duration used are shown in Table 2. There were no differences observed in mean speed regardless of the microsleep duration (F (2,138) = 0.71, p=0.49).
Table 2.
Number of microsleep episodes for each microsleep duration and road type
| Road type | Microsleep Durations |
Total | ||
|---|---|---|---|---|
| Short | Medium | Long | ||
| Straight | 57 | 34 | 26 | 117 |
| Curved | 17 | 7 | 10 | 34 |
| Total | 74 | 41 | 36 | 151 |
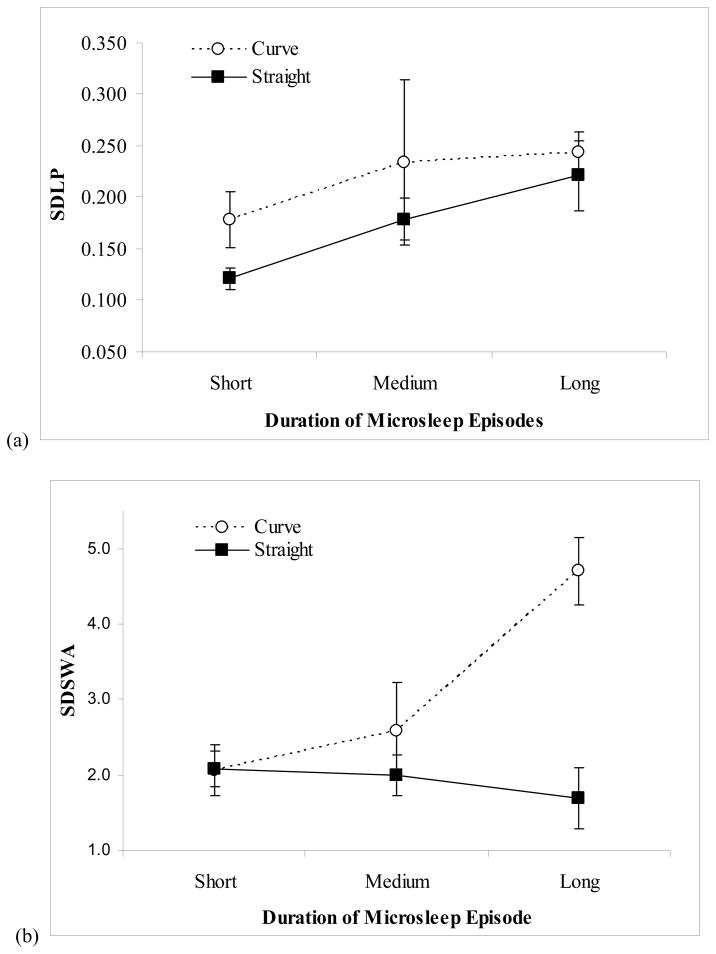
As was done previously, the steering measures were evaluated using MANOVA. The findings showed that significant differences did exist on road type (Wilks’ Lamda F(3,143)=4.59, p=0.0042), for microsleep durations (F(6,286)=3.92, p=0.0009), and the interaction between road type and microsleep durations (F(6,286)=4.47, p=0.0002). In terms of the contribution of each steering measure, univariate ANOVA showed that SDLP was significantly different for road type (F(1,145)=3.95, p=0.0486) and for microsleep durations (F(2,145)=6.61, p=0.0018). As shown in Figure 1a, SDLP was significantly higher on curves (mean SDLP = 0.20) than on straight segments (mean = 0.16) and also increased with longer microsleep durations.
Figure 1.
The effect of microsleep duration on lateral controls: (a) SDLP and (b) SDSWA.
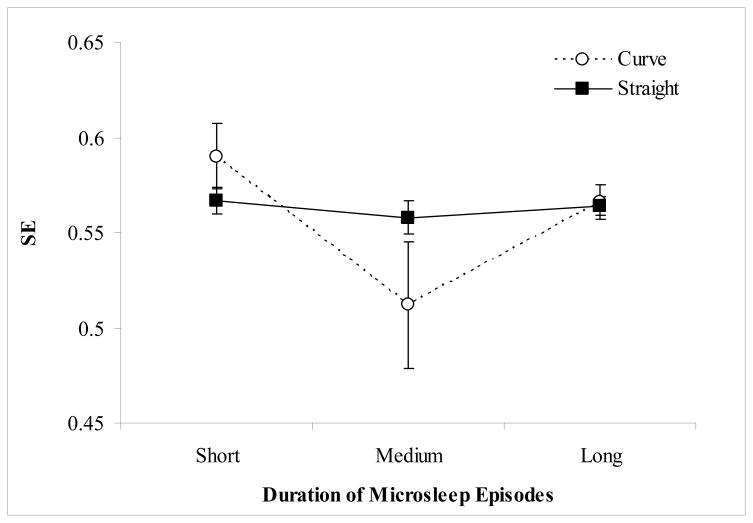
With respect to SDSWA, significant differences were observed for road type (F(1,145)=13.94, p=0.0003) and the interaction of road type with microsleep durations (F(2,145)=7.06, p=0.0012). More specifically, SDSWA increased sharply on curved road segments when the microsleep durations increased from medium (mean =2.33) to long (mean = 4.61) (Figure 1b). SE significantly decreased on curves during microsleep durations of medium length (F(2, 145)=3.33, p=0.039) and this can also be observed in Figure 2.
Figure 2.
The effects of microsleep duration on steering entropy by road type.
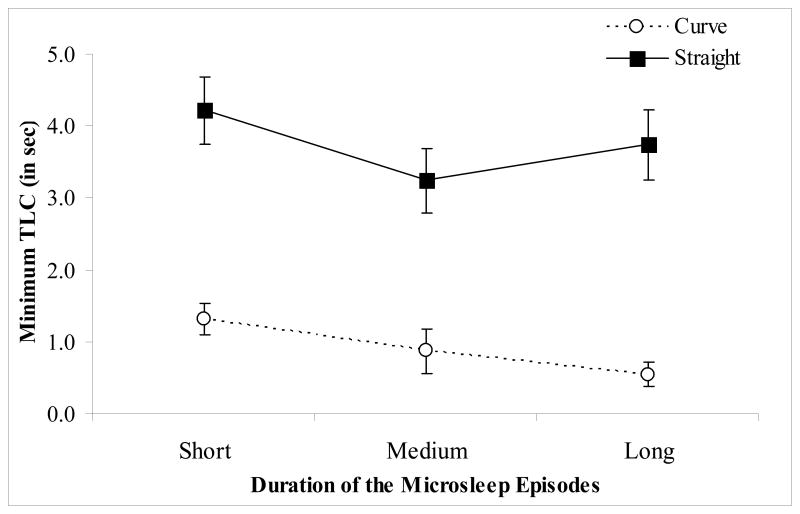
The minimum TLC did not significantly differ among the microsleep durations (F(2, 143)=1.84, p>0.05). There was, however, a significant difference between road types (F (1, 141)=33.85, p<0.0001) with an overall mean TLC being 2.85 sec on straight segments and 0.59 on curves (Figure 3). No interaction effect was observed between microsleep duration and road types (F(2,143)=0.30, p>0.05).
Figure 3.
The effects of microsleep duration on minimum TLC by road type.
4. Discussion
This study examined the momentary effects of microsleeps on the driving performance in drivers who are at particular risk for drowsy driving because of OSAS. We tested the hypothesis that drowsy drivers would show measurable changes in driving performance during microsleep compared to matched non-microsleep segments. The results of this study showed significant differences in driver control that were related to both the occurrence and duration of microsleeps. Drivers showed lower speeds during microsleep episodes, indicating that drowsy drivers exert less control over the accelerator pedal during microsleeps by failing to continue to depress it as needed to maintain the recommended speed. Changes such as momentary vehicle slowing are not likely to have much effect on a vacant rural road, but might produce interactions that alter the traffic flow in highly congested areas, when sleepy drivers are returning home during peak traffic periods. Risser et al (2000) found greater speed variability in drowsy drivers with OSAS compared to controls over an entire simulator drive, but did not assess momentary changes related to microsleeps. They also noted that lane position variability correlated with the frequency and duration of EEG-defined “attention lapses”.
Although there was no effect for SDSWA due to microsleeps, drivers with OSAS showed greater variability in maintaining lane position during microsleep episodes compared to non-microsleep episodes. SE increased during microsleep episodes and with successive drive segments, a finding not observed with the other lateral measures. Unlike the other steering measures, SE is related to moment to moment predictability and will increase as drivers make more error corrective maneuvers.
The finding that entropy increased with each drive segment indicates that sleepy drivers with microsleep episodes showed worse vehicle control the longer they drove. The finding of lower minimum TLC on curves, calculated using the method of van Winsum and Godthelp (1996), suggests that changes in road geometry may lead to a greater crash risk. Minimum TLCs were longer on straight segments, probably due to invariant road geometry and lack of external challenges. These findings suggest that drivers can maintain a relatively high TLC on straight segments during microsleep episodes of differing durations even if they may not be controlling the vehicle as actively.
Use of a fixed-base driving simulator in this study allowed us to make safe observations of sleepy driver behavior with a high degree of experimental control. A drawback of this approach is that feedback to the driver in any simulator differs from that in a moving vehicle. Drivers in actual road conditions get more tactile and vibratory feedback from the steering wheel, seat and vehicle frame, as well as vestibular feedback, all of which provide potential cues for drivers to exert control over the vehicle.
There are also challenges in using EEG to study sleepy driving. Because movement and muscle artifacts may hinder the EEG interpretation, this study analyzed only artifact-free EEG data. Microsleeps occurring during these segments would be missed. Although we used expert visual inspection of the EEG to identify microsleeps according to generally accepted criteria, this technique is inherently subjective. Several studies have used “quantitative” EEG methods to identify driver sleepiness (de Waard & Brookhuis, 1991; Eoh et al., 2005; Kecklund & Akerstedt, 1993; Horne & Reyner, 1996; Lal & Craig, 2002). Alpha and theta power (usually expressed as the relative power of alpha + theta/beta), and the frequency of alpha and theta bursts typically increase during prolonged driving, and are associated with poor driving performance. As these techniques typically average EEG activity over several seconds (up to one minute), detection of brief microsleep episodes, as studied here, would not be possible. Eoh et al (2005) showed that the numbers of short (1 second) alpha bursts and driving incidents increased with driving duration. However, instead of finding bursts occurring at the time of an incident, they noted a drop in alpha + theta/beta power in the seconds after incidents compared to the preceding 10 seconds. Although the current study did not include spectral analysis of EEG data, decline in alpha + theta/beta power probably reflects post-event alerting, while microsleep episodes reflect both pre- and post-event EEG changes. Risser et al (2000) found that “attention lapses”, comprising EEG episodes of increased alpha or theta activity lasting more than 3 seconds (which differs from the conventional definition of microsleeps) correlated with lane position variability and crash frequency. The best techniques for identifying impending driver sleepiness by EEG are targets for future research.
A variety of physiological measures have been proposed for identifying and alerting drowsy drivers. One of the most investigated is PERCLOS (or PERcent CLOSure), a measure of drowsiness associated with slow eye closures (Grace et al., 1998; Hayami et al., 2002; Pilutti & Ulsoy, 1997). However, PERCLOS does not identify drivers with “blank stares”, whose eyes remain open while they are drowsy. EEG changes, including microsleep episodes, may provide complementary evidence of impending sleep in these drowsy drivers. Paul et al (2005b) showed that drivers had greater variation in steering and lane position during microsleep episodes when compared to the periods before and after a microsleep. Lal and Craig (2002) identified early signs of sleepiness in a driving simulator task using EEG that was later proposed for fatigue-detection countermeasure systems (Lal et al., 2003).
Combining EEG and PERCLOS data may permit the design of an onboard system that could alert sleepy drivers to unsafe situations before lid closure occurs. While the current study did not directly study this issue, EOG recordings (made to exclude potential artifacts during EEG recordings) showed that eye blinks often continued during microsleeps, indicating that the eyes were at least partially open. In fact, eye closure characteristically leads to an increase in alpha (Niedermeyer, 2005), rather than the decrease that was used as the primary criterion for determining the presence of a microsleep. Further studies are needed to establish the extent to which EEG and eye closure information provide complementary information.
This study used a within subject design and was specifically aimed at evaluating driver performance related to microsleeps in an enriched population of drowsy drivers. It did not address the relationship between overall performance and EEG changes, or correlate findings with subjective measures of sleepiness such as the ESS. The costs and benefits of EEG monitoring of drivers, and how the findings discriminate between groups of safe and unsafe drivers with varying degrees of sleepiness or sleep disorders are topics for future studies.
In conclusion, drowsy drivers with OSAS show deterioration in simulated driving performance during EEG-verified microsleeps. The degree of deterioration correlated with microsleep duration and was worse when microsleeps occurred on curved road segments. Identifying how microsleep episodes influence driving behavior may prove to be relevant to the design and implementation of countermeasures, such as drowsy driver detection and alerting systems.
Acknowledgments
The funding for this study was made possible by grants from the Center for Disease Control (CDC R49 CCR 721682) and the National Institute of Aging (NIA R01 AG017177). The authors would also like to thank Malcolm Yeh, MD for his assistance in screening the participants used in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Academy of Sleep Medicine (AASM) International classification of sleep disorders, 2nd edition: Diagnostic and coding manual. Westchester, Illinois: American Academy of Sleep Medicine; 2005. pp. 51–55. [Google Scholar]
- Bedard M, Montplaisir J, Malo J, Richer F, Rouleau I. Persistent neuropsychological deficits and vigilance impairment in sleep apnea syndrome after treatment with continuous positive airways pressure (CPAP) Journal of Clinical & Experimental Neuropsychology. 1993;15:330–341. doi: 10.1080/01688639308402567. [DOI] [PubMed] [Google Scholar]
- Blincoe LJ, Seay A, Zaloshnja E, Miller TR, Romano E, Luchter S, et al. The economic impact of motor vehicle crashes, 2000. Washington, DC: National Highway Traffic Safety Administration; 2002. [Google Scholar]
- Butkov N. Atlas of Clinical Polysomnography. Vol. 1. Ashland, Oregon: Synapse Media; 1996. pp. 184–189. [Google Scholar]
- Connor J, Whitlock G, Norton R, Jackson R. The role of driver sleepiness in car crashes; a systematic review of epidemiological studies. Accident Analysis and Prevention. 2001;33:31–41. doi: 10.1016/s0001-4575(00)00013-0. [DOI] [PubMed] [Google Scholar]
- de Waard D, Brookhuis KA. Assessing driver status: a demonstration experiment on the road. Accid Anal Prev. 1991;23(4):297–307. doi: 10.1016/0001-4575(91)90007-r. [DOI] [PubMed] [Google Scholar]
- Dinges DF, Kribbs NB. Performing while sleeping: effects of experimentally induced sleepiness. In: Monk TH, editor. Sleep, sleepiness, and performance. Chichester, UK: Wiley & Sons; 1991. pp. 97–128. [Google Scholar]
- Donmez B, Boyle L, Lee J. The impact of driver distraction mitigation strategies on driving performance. Journal of Human Factors and Ergonomics Society. 2006;48(4):785–804. doi: 10.1518/001872006779166415. [DOI] [PubMed] [Google Scholar]
- Engleman HM, Hirst W, Douglas NJ. Under reporting of sleepiness and driving impairment in patients with sleep apnoea/hypopnoea syndrome. J Sleep Res. 1997;6:272–275. doi: 10.1111/j.1365-2869.1997.00272.x. [DOI] [PubMed] [Google Scholar]
- Eoh HJ, Chung MK, Kim SH. Electroencephalographic study of drowsiness in simulated driving with sleep deprivation. Int J Industrial Ergonomics. 2005;35:307–320. [Google Scholar]
- Findley L, Unverzagt M, Guchu R, Fabrizio M, Buckner J, Suratt P. Vigilance and automobile accidents in patients with sleep apnea or narcolepsy. Chest. 1995;108(3):619–624. doi: 10.1378/chest.108.3.619. [DOI] [PubMed] [Google Scholar]
- Feuerstein C, Naegele B, Pepin J, Levy P. Frontal lobe-related cognitive functions in patients with sleep apnea syndrome before and after treatment. Acta Neurologica Belgica. 1997;140:529–530. [PubMed] [Google Scholar]
- Furukawa Y, Takei A, Kobayashi M, Kawai T. Effects of active steering control on closed-loop control performance. Paper presented at the Eighteenth Fisita Congress - The Promise of New Technology in the Automotive Industry; May 7–11 1990; Torino, Italy.. 1990. [Google Scholar]
- George CF. Sleep center dot 5: Driving and automobile crashes in patients with obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004;59(9):804–807. doi: 10.1136/thx.2003.007187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CFP, Nickerson PW, Hanly PJ, Millar TW, Kryger MH. Sleep apnea patients have more automobile accidents. The Lancet. 1987:447. doi: 10.1016/s0140-6736(87)90974-3. [DOI] [PubMed] [Google Scholar]
- Godthelp H. Vehicle Control During Curve Driving. Human Factors. 1986;28(2):211–221. doi: 10.1177/001872088602800209. [DOI] [PubMed] [Google Scholar]
- Grace R, Byrne VE, Bierman DM, Legrand JM, Gricourt D, Davis BK, et al. A drowsy driver detection system for heavy vehicles; Paper presented at the Proceedings of 17th Digital Avionics Systems Conference; Bellevue, WA, USA. 1998. [Google Scholar]
- Harrison Y, Horne JA. Occurrence of “microsleeps’ during daytime sleep onset in normal subjects. Electroencephalogr Clin Neurophysiol. 1996;98(5):411–416. doi: 10.1016/0013-4694(96)95612-6. [DOI] [PubMed] [Google Scholar]
- Hayami T, Matsunaga K, Shidoji K, Matsuki Y. Detecting drowsiness while driving with eye movement - a pilot study. Proceedings of IEEE ITSC; 2002. pp. 156–161. [Google Scholar]
- Heitmann A, Guttkuhn R, Aquirre A, Trutschel U, Moore-Ede M. Technologies for the monitoring and prevention of driver fatigue. Proceeding of the 1st International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design; Iowa City, IA: Public Policy Center, University of Iowa; 2001. pp. 81–86. [Google Scholar]
- Horne JA, Reyner LA. Sleep related vehicle accidents. British Medical Journal. 1995;310(6979):565–567. doi: 10.1136/bmj.310.6979.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne JA, Reyner LA. Counteracting driver sleepiness: effects of napping, caffeine, and placebo. Psychophysiology. 1996;33(3):306–309. doi: 10.1111/j.1469-8986.1996.tb00428.x. [DOI] [PubMed] [Google Scholar]
- Horstmann S, Hess CW, Bassetti C, Gugger M, Mathis J. Sleepiness-related accidents in sleep apnea patients. Sleep. 2000;23:383–389. [PubMed] [Google Scholar]
- Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- Kecklund G, Akerstedt T. Sleepiness in long distance driving: an ambulatory EEG study of night driving. Ergonomics. 1993;36(9):1007–1017. doi: 10.1080/00140139308967973. [DOI] [PubMed] [Google Scholar]
- Kim H, Young T, Matthews C, Weber S, Woodward A, Palta M. Sleep-disordered breathing and neuropsychological deficits. A population-based study. American Journal of Respiratory & Critical Care Medicine. 1997;156:1813–1819. doi: 10.1164/ajrccm.156.6.9610026. [DOI] [PubMed] [Google Scholar]
- Klem G, Luders H, Jasper H, Elger C. The ten-twenty electrode system of the International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol Suppl. 1993;52:3–6. [PubMed] [Google Scholar]
- Knipling RR, Wang J-S. Revised estimates of the US drowsy driver crash problem size based on general estimates system and case reviews. Paper presented at the Annual Meeting of the Association for the Advancement of Automotive Medicine; Chicago, Ill. 1995. Oct 18, [Google Scholar]
- Kwon W, Lee JW, Shin D, Roh K, Kim DY, Lee S. Experiments on decision making strategies for a lane departure warning system. Proceedings of the 1999 IEEE International Conference on Robotics and Automation, ICRA99; May 10-May 15 1999; 1999. pp. 2596–2601. [Google Scholar]
- Lal SKL, Craig A. Driver fatigue: Electroencephalography and psychological assessment. Psychophysiology. 2002;39:1–9. doi: 10.1017/s0048577201393095. [DOI] [PubMed] [Google Scholar]
- Lal SKL, Craig A, Boord P, Kirkup L, Nguyen H. Development of an algorithm for an EEG-based driver fatigue countermeasure. J Safety Res. 2003;34:321–328. doi: 10.1016/s0022-4375(03)00027-6. [DOI] [PubMed] [Google Scholar]
- Laube I, Seeger R, Russi EW, Bloch KE. Accidents related to sleepiness: review of medical causes and prevention with special reference to Switzerland. Schweiz Med Wochenschr. 1998;128(40):1487–1499. [PubMed] [Google Scholar]
- Lenne MG, Triggs TJ, Redman JR. Interactive effects of sleep deprivation, time of day, and driving experience on a driving task. Sleep. 1998;21(1):38–44. doi: 10.1093/sleep/21.1.38. [DOI] [PubMed] [Google Scholar]
- Lin C-F, Ulsoy AG. Calculation of the time to lane crossing and analysis of its frequency distribution. Paper presented at the Proceedings of the 1995 American Control Conference. Part 5 (of 6); Jun 21–23 1995; Seattle, WA, USA. 1995. [Google Scholar]
- Lyznicki JM, Doege TC, Davis RM, Williams MA. Sleepiness, driving, and motor vehicle crashes. Council on Scientific Affairs, American Medical Association. JAMA. 1998;279(23):1908–1913. doi: 10.1001/jama.279.23.1908. [DOI] [PubMed] [Google Scholar]
- Maclure M. The Case-Crossover Design - a Method for Studying Transient Effects on the Risk of Acute Events. American Journal of Epidemiology. 1991;133(2):144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- McCartt AT, Ribner SA, Pack AI, Hammer MC. The scope and nature of the drowsy driving problem in New York State. Accident Analysis Prevention. 1996;28(4):511–517. doi: 10.1016/0001-4575(96)00021-8. [DOI] [PubMed] [Google Scholar]
- McGehee DV, Lee JD, Rizzo M, Dawson J, Bateman K. Quantitative analysis of steering adaptation on a high performance fixed-base driving simulator. Transportation Research, Part F: Traffic Psychology and Behavior. 2004 May;7:3. [Google Scholar]
- Nakayama O, Futami T, Nakamura T, Boer ER. Development of a steering entropy method for evaluating driver workload. Paper presented at the SAE International Congress and Exposition; Detroit, Michigan, USA. 1999. [Google Scholar]
- Niedermeyer E. The normal EEG of the waking adult. In: Niedermeyer E, da Silva FL, editors. Electroencephalography: Basic Principles, Clinical Applications, and Related Fields, 5th edition. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 167–192. [Google Scholar]
- Nowak M, Kornhuber J, Meyrer R. Daytime impairment and neurodegeneration in OSAS. Sleep. 2006;29(12):1521–1530. doi: 10.1093/sleep/29.12.1521. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Caulet M, Philip P, Guilleminault C, Priest RG. How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med. 1997;157(22):2645–2652. [PubMed] [Google Scholar]
- Paul A, Boyle L, Boer E, Tippin J, Rizzo M. Proceedings of the 3rd International Driving Symposium on Human Factors in Driving Assessment, Training, and Vehicle Design. Iowa City, IA: Public Policy Center, University of Iowa; 2005a. Steering entropy changes as a function of microsleeps; pp. 18–24. [Google Scholar]
- Paul A, Boyle L, Tippin J, Rizzo M. Variability of driving performance during microsleeps. Proceedings of the 3rd International Driving Symposium on Human Factors in Driving Assessment, Training, and Vehicle Design; Iowa City, IA: Public Policy Center, University of Iowa; 2005b. pp. 433–440. [Google Scholar]
- Pilutti T, Ulsoy AG. Identification of driver state for lane-keeping tasks: experimental results. Paper presented at the Proceedings of the American Control Conference; Albuquerque, NM, USA. 1997. [Google Scholar]
- Rakauskas ME, Ward NJ. Behavioral effects of driver distraction and alcohol impairment. Proceedings of 49th annual meeting of the Human Factors and Ergonomics Society; Orlando, Florida. September 26–30, 2005..2005. [Google Scholar]
- Ramaekers JG. Antidepressants and driver impairment: empirical evidence from a standard on-the-road test. J Clinical Psychiatry. 2003;64(1):20–29. [PubMed] [Google Scholar]
- Rechtschaffen A, Kales A. A Manual of Standardized Terminology, Techniques, and Scoring System for Sleep Stages of Human Subjects (Institute of Health Publication No. 204) Washington, DC: U.S. Government Printing Office; 1968. pp. 2–12. [Google Scholar]
- Risser MR, Ware JC, Freeman FG. Driving simulation with EEG monitoring in normal and obstructive sleep apnea patients. Sleep. 2000;23(3):393–398. [PubMed] [Google Scholar]
- Rizzo M, McGehee D, Jermeland J. Design and installation of a driving simulator in a hospital environment. In: Brookhuis K, DeWaard D, Weikert C, editors. Human System Interaction: Education, Research and Application in the 21st Century. Maastricht, The Netherlands: Shaker Publishing; 2000. pp. 69–77. [Google Scholar]
- Royal D. Findings for National survey of distracted and drowsy driving attitudes and behavior: 2002. U.S. DOT NHTSA. 2003;I Retrieved. from http://www.nhtsa.dot.gov/People/injury/drowsy_driving1/survey-distractive03/index.htm.
- Sassani A, Findley L, Kryger M, Goldlust E, George C, Davidson T. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27(3):453–458. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- Soldatos CR, Kales JD, Scharf MB, Bixler EO, Kales A. Cigarette smoking associated with sleep difficulty. Science. 1980;207(4430):551–553. doi: 10.1126/science.7352268. [DOI] [PubMed] [Google Scholar]
- Summala H, Nieminen T, Punto M. Maintaining lane position with peripheral vision during in-vehicle tasks. Human Factors. 1996;38(3):442–451. [Google Scholar]
- Teran-Santos J, Jiminez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. The New England Journal of Medicine. 1999;340(11):847–851. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- Thorpy M, Yager J. The encyclopedia of sleep and sleep disorders. New York: Facts On File; 1991. p. 129. [Google Scholar]
- Tirunahari VL, Zaidi SA, Sharma R, Skurnick J, Ashtyani H. Microsleep and sleepiness: a comparison of multiple sleep latency test and scoring of microsleep as a diagnostic test for excessive daytime sleepiness. Sleep Med. 2003;4(1):63–67. doi: 10.1016/s1389-9457(02)00250-2. [DOI] [PubMed] [Google Scholar]
- Valley V, Broughton R. The physiological (EEG) nature of drowsiness and its relation to performance deficits in narcoleptics. Electroencephaolgr Clin Neurophysiol. 1983;55:243–251. doi: 10.1016/0013-4694(83)90201-8. [DOI] [PubMed] [Google Scholar]
- Van Dongen HPA, Dinges DF. Circadian rhythms in sleepiness, alertness, and performance. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine, 4th edition. Philadelphia: Elsevier; 2005. pp. 435–443. [Google Scholar]
- van Winsum W, Brookhuis KA, De Waard D. A comparison of different ways to approximate time-to-line crossing (TLC) during car driving. Accident Analysis and Prevention. 2000;32(1):47–56. doi: 10.1016/s0001-4575(99)00048-2. [DOI] [PubMed] [Google Scholar]
- van Winsum W, Godthelp H. Speed Choice and Steering Behaviour in Curve Driving. Human Factors. 1996;38(3):434–441. [Google Scholar]
- Wetter DW, Young TB. The relation between cigarette smoking and sleep disturbance. Preventive Medicine. 1994;23(3):328–334. doi: 10.1006/pmed.1994.1046. [DOI] [PubMed] [Google Scholar]
- Wu H, Yan-Go F. Self-reported automobile accidents involving patients with obstructive sleep apnea. Neurology. 1996;46:1254–1257. doi: 10.1212/wnl.46.5.1254. [DOI] [PubMed] [Google Scholar]
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. The New England Journal of Medicine. 1993;328:1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]