Abstract
Background
Smoking accounts for a large proportion of cancer-related mortality, creating a need for better smoking cessation efforts. We investigated whether gain-framed messages (ie, presenting benefits of quitting) will be a more persuasive method to encourage smoking cessation than standard-care messages (ie, presenting both costs of smoking [loss-framed] and benefits of quitting).
Methods
Twenty-eight specialists working at the New York State Smokers’ Quitline (a free telephone-based smoking cessation service) were randomly assigned to provide gain-framed or standard-care counseling and print materials. Smokers (n = 2032) who called the New York State Smokers’ Quitline between March 10, 2008, and June 13, 2008, were exposed to either gain-framed (n = 810) or standard-care (n = 1222) messages, and all medically eligible callers received nicotine replacement therapy. A subset of 400 call recordings was coded to assess treatment fidelity. All treated smokers were contacted for 2-week and 3-month follow-up interviews. All statistical tests were two-sided.
Results
Specialists providing gain-framed counseling used gain-framed statements statistically significantly more frequently than those providing standard-care counseling as assessed with frequency ratings for the two types of gain-framed statements, achieving benefits and avoiding negative consequences (for achieving benefits, gain-framed mean frequency rating = 3.9 vs standard-care mean frequency rating = 1.4; mean difference = −2.5; 95% confidence interval [CI] = −2.8 to −2.3; P < .001; for avoiding negative consequences, gain-framed mean frequency rating = 1.5 vs standard-card mean frequency rating = 1.0; mean difference = −0.5; 95% CI = −0.6 to −0.3; P < .001). Gain-framed counseling was associated with a statistically significantly higher rate of abstinence at the 2-week follow-up (ie, 99 [23.3%] of the 424 in the gain-framed group vs 76 [12.6%] of the 603 in the standard-care group, P < .001) but not at the 3-month follow-up (ie, 148 [28.4%] of the 522 in the gain-framed group vs 202 [26.6%] of the 760 in the standard-care group, P = .48).
Conclusions
Quitline specialists can be trained to provide gain-framed counseling with good fidelity. Also, gain-framed messages appear to be somewhat more persuasive than standard-care messages in promoting early success in smoking cessation.
CONTEXT AND CAVEATS
Prior knowledge
Smoking accounts for a large proportion of cancer-related mortality, creating a need for better smoking cessation efforts. An average of 1% of all smokers (ie, 500 000 people) use quitline services per year, and 100% of the US population has access to such services.
Study design
Twenty-eight quitline specialists were randomly assigned to provide 2032 smokers with gain-framed or standard-care counseling, print materials, and nicotine replacement therapy to all medically eligible callers. Treatment fidelity was assessed in a subset of calls. All treated smokers were contacted for 2-week and 3-month follow-up interviews.
Contribution
Quitline specialists can be trained to provide gain-framed counseling with good fidelity. Gain-framed messages were more persuasive than standard-care messages in promoting early cessation of smoking (ie, at the 2-week follow-up) but not at 3 months.
Implications
Quitlines should be encouraged to test novel counseling strategies for their ability to increase smoking cessation rates. Because long-term cessation is necessary to prevent cancer-related mortality and other tobacco-induced diseases, future research should focus on how to extend the short-term rates of smoking cessation to increased long-term rates.
Limitations
Characteristics of callers who enrolled and of those who declined were different. Gain-framed interventions were longer than standard-care interventions. Follow-up rates were low. Dichotomous primary smoking outcomes (yes or no) were used. There were different levels of supervision between the counseling groups. No adjustment was made for multiple comparisons.
From the Editors
Smoking-related diseases remain the world's most preventable cause of death (1). Smoking accounts for at least 30% of all cancer deaths and 87% of lung cancer deaths (2). It is associated with an increased risk for at least 15 types of cancers and is responsible for nearly one in five deaths in the United States (3). Although the risks of smoking and benefits of quitting are well publicized and documented (4), an estimated 45 million Americans currently smoke cigarettes, and the percentage of American smokers (ie, 21%) has remained stagnant for several years (5,6). To combat cancer effectively, these smoking statistics must decrease and the effectiveness of current smoking cessation efforts should be improved.
Telephone quitlines are a cost-efficient method to deliver smoking cessation treatment that can reach and benefit many smokers. An average of 1% of all smokers (ie, 500 000 people) use quitline services per year (7), and 100% of the US population has access to such services (8). Quitlines generally offer at least one free counseling session for smokers who state that they are ready to quit (and often follow-up sessions depending on insurance status of the smoker). About one-third of state quitlines offer free medications by mail (7). Quitlines are also used by the uninsured (9) who may otherwise have limited access to treatment, young adults (10), and smokers of every race, educational level, and sex (8). Thus, quitline specialists manage large numbers of calls from a diverse population of smokers, and the heterogeneity of characteristics for these callers may explain why investigators have not attempted to train quitline specialists to consistently deliver novel counseling messages. Failure to develop improved training methods is unfortunate because no other smoking cessation method has as diverse or extensive reach as quitlines and because quit rates resulting from quitline services could be enhanced (11,12). Indeed, considering the broad reach of telephone quitlines, any efficacious change could have a substantive impact on national quit rates and could result in statistically significant reductions in the incidence of and mortality from smoking-related cancers.
Although several studies have assessed ways to improve quitline effectiveness [eg, offering free nicotine replacement therapy and comparing briefer single telephone counseling sessions to multiple longer telephone counseling sessions (12)] and most quitlines use motivational interviewing and cognitive behavioral counseling techniques (11–15), to our knowledge, a systematic evaluation of the impact of delivering novel evidence-based counseling messages or rigorously monitored fidelity to a new counseling approach has not been conducted. Gain-framed messaging is a novel counseling approach that could easily be incorporated into quitline services. The principles underlining the use of gain-framed messages in a health context derive from the framing postulate of prospect theory—that is, when gains are made prominent in a decision situation, then people are averse to risk; and when losses are made salient, individuals seek risk (16). This prediction originates from the proposal that the function relating objective outcomes to their subjective value is nonlinear. Although the messages may be equivalent factually, the framing of the message in gain vs loss terms influences an individual's willingness to incur risk to encourage a desirable outcome or to avoid an unwanted outcome (17). Accordingly, information can elicit differential responses depending on whether it is either framed to emphasize the benefits (ie, a gain-framed message) or the costs (ie, a loss-framed message) incurred by that response (16). Several investigations (17–20) have studied the effect of framing health information on people's willingness to engage in or change health-related behaviors such as HIV screening, sunscreen use, and exercise.
In their review of literature on message framing, Rothman and Salovey (21) suggest that gain- and loss-framed messages are differentially persuasive, depending on the type of health behavior addressed. For example, loss-framed messages effectively promote detection behaviors, such as receiving a mammogram (22,23), because the outcome of doing so is uncertain (ie, the patient may or may not have breast cancer), thus making the decision to obtain a mammogram involves taking a psychological risk. Gain-framed messages most effectively motivate prevention health behaviors, such as sunscreen use, because these behaviors produce relatively certain outcomes (ie, preventing skin damage), which involve little risk (24). Because smoking cessation prevents cancer and other health problems, several studies (25–28) have examined the effect of gain-framed messaging on various smoking behaviors, and all have obtained encouraging results. Toll et al. (25) showed that participants who completed a 7-week course of open-label bupropion SR (a smoking cessation pharmacotherapy) and received gain-framed messages, compared with loss-framed messages, achieved statistically significantly higher rates of continuous abstinence from smoking. Given these promising findings, we examined the feasibility and impact of incorporating gain-framed messages into a real-world smoking cessation quitline.
This study had two purposes: to assess whether quitline specialists could be trained to consistently deliver gain-framed messages to smokers and to evaluate smoking cessation outcomes of clients exposed to telephone specialists trained and supervised to deliver gain-framed messages (ie, benefits of quitting) as compared with those who were trained and supervised to provide standard-care messages (ie, both costs of smoking and benefits of quitting). Our previous research (29) has shown that New York State Smokers’ Quitline (NYSSQL) standard-care calls have low levels of gain-framed (approximately 10% of statements emphasize benefits of quitting) and loss-framed (less than 2% of statements emphasize costs of smoking) messages. Therefore, we expected to observe more gain-framed messages delivered by specialists in the gain-framed counseling group and fewer gain- and loss-framed messages delivered by specialists in the standard-care counseling group.
Participants and Methods
Study Design, Participants, and Intervention
This study design was a two-group randomized controlled study conducted with telephone specialists and their smoking clients who had contacted the NYSSQL for assistance in stopping smoking from March 10, 2008, through June 13, 2008. All 43 telephone specialists working at the NYSSQL were eligible to participate (ie, there were no exclusion criteria). Of the 43 specialists, 15 indicated that they were not interested in participating. Consequently, 28 specialists consented and were randomly assigned to either the gain-framed (n = 14) or standard-care (n = 14) training conditions from January 21, 2008, through January 22, 2008. One of the authors (R. Wu) created the allocation sequence before the start of study enrollment. After all participants consented, they were assigned numbers that were based on the order in which their consent was obtained by an outside staff member in the Department of Psychiatry at the Yale University School of Medicine. The outside staff did not know the NYSSQL staff.
On January 26, 2008, specialists delivering gain-framed messages received 4 hours of classroom training on how to provide gain-framed statements from two of the authors (B. A. Toll and A. Latimer). This training included review of gain-framed principles, role playing to develop skills, and discussion of how to implement the protocol in the NYSSQL setting. On January 27, 2008, specialists delivering standard-care messages received 4 hours of training on NYSSQL motivational interviewing principles. Specialists in both groups were paid $200 for the training, which was conducted after their usual work hours. Under the guidance of doctoral-level supervisors, all specialists in the gain-framed counseling group were required to counsel a minimum of three pilot callers to demonstrate competency with the gain-framed messaging protocol. All pilot calls were audiotaped so that supervisors could rate the tapes and certify specialists as adhering to the protocol (ie, ratings of at least a “5,” meaning “quite a bit,” on either gain-framed fidelity item during three telephone calls; possible scores were 1 = “not at all”; 2 = “a little”; 3 = “infrequent”; 4 = “somewhat”; 5 = “quite a bit”; 6 = “considerably”; and 7 = “extensively”) before being allowed to enroll smokers in the study. All 14 specialists in the gain-framed condition were able to meet this threshold and were certified to receive study callers.
After completion of their training, 28 specialists provided counseling for 2032 smokers who called the NYSSQL by using the approach they had been trained to administer. To be eligible to enroll in the study, callers had to meet the following eligibility criteria: 1) a New York State resident of at least 18 years of age; 2) English speaker; 3) a current smoker seeking quitting assistance for themselves; 4) not enrolled in the NYSSQL extended callback program, which was intended for Medicaid beneficiaries or the uninsured; and 5) not enrolled in any other special cessation programs through another source (eg, their insurance company, hospital, or county health department). The exclusion of Medicaid and uninsured clients and those receiving extra cessation services through a different provider agency was intended to limit the study to those receiving the same standard of cessation assistance.
To ensure translatability, this study conformed as much as possible to the standard practices of the NYSSQL. Consistent with these practices, all callers received an initial intake telephone call that included medical screening for a 2-week starter pack of nicotine replacement therapy containing patches, gum, or lozenges and a free mailing that included the NYSSQL's Break Loose! stop smoking booklet and smoking cessation tip sheets. This telephone call included a secure web-based structured interview and counseling session; at the time the study was conducted, this call averaged approximately 12 minutes. All callers also received a 2-week follow-up telephone call that included counseling and assessed smoking status and receipt of medication (for those who were medically eligible). We did not attempt to control for the time of each of the specialists’ calls. Because of the high call demand of this busy service (last year, the NYSSQL received more than 279 000 incoming calls), all quitline specialists, including those participating in the study, were under a great deal of pressure to keep all calls brief. Thus, we believed that the structure of the quitline service created a natural control for call length.
The primary outcomes were fidelity to treatment condition, quitting for at least 24 hours (which was measured as part of a standard 2-week follow-up call to clients), and point prevalence abstinence (ie, quitting over a specified time period) in the last 7 days (which was measured at 3 months after the intake call). The 3-month follow-up interview was conducted by an independent survey group that was blinded to subject assignment to gain-framed or standard-care counseling groups. We hypothesized that specialists in the gain-framed counseling group would provide a statistically significantly higher level of gain-framed messages and that smokers who received counseling from such specialists would have higher rates of abstinence from cigarette smoking.
Specialists provided written permission for study involvement. Callers provided verbal informed consent to participate in all three telephone-based interviews (ie, intake, 2-week follow-up, and 3-month follow-up interviews). The Institutional Review Boards of the Roswell Park Cancer Institute and the Yale University School of Medicine approved this study.
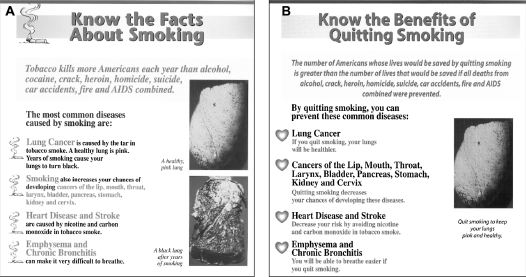
Enrolled callers received additional assessment questions included in their interviews (described below). Callers randomly assigned to the gain-framed group were exposed to gain-framed counseling statements and received newly developed, exclusively gain-framed NYSSQL printed materials by mail. Sample pages from the original and exclusively gain-framed Break Loose! booklets are presented in Figure 1. The booklet and all other printed materials were replications of original NYSSQL materials, except for the reframed text and images. We used the NYSSQL graphic designer and printer to ensure fidelity of replication of printed materials.
Figure 1.
Sample pages. A) Page from the New York State Smokers’ Quitline (NYSSQL) Break Loose! original guide. B) Page from the exclusively gain-framed NYSSQL Break Loose! guide. All loss-framed messages were either reframed to be gain-framed messages (eg, “The most common diseases caused by smoking are” became “By quitting smoking you can prevent these common diseases”) or deleted (eg, the black lung was removed).
Each intake call with gain-framed counseling statements began with the initial question, “What benefits do you expect to get from quitting smoking?” Specialists would personalize the gain-framed statements made by the caller. For instance, if the caller stated that he or she expected to live longer and save money, the specialist would reflect this response back immediately and refer to it at later points in the conversation as well. Additional examples of typical gain-framed counseling statements include “The benefits of quitting smoking begin immediately, and by quitting smoking now, you are greatly reducing your risk of health problems”; “Studies show that smokers who take nicotine replacement medication are more successful in quitting than smokers trying to quit without medication”; “People who successfully quit smoking often report becoming more confident in trying to achieve other important goals in their lives that they may have been delaying because of their smoking (eg, starting to exercise)”; and “Calling us is a step toward achieving the benefits of a smoke-free lifestyle.” These and other gain-framed statements were programmed into the web-based structured interview as pop-up bubbles that appeared when specialists in gain-framed counseling moved their cursor over items in the interview. Examples of gain-framed print statements, including the corresponding loss-framed statements that were altered, are presented in Table 1.
Table 1.
Typical gain-framed messages in the print interventions and corresponding loss-framed messages in standard NYSSQL print materials*
| Gain-framed message | Loss-framed message |
| If you quit smoking you will be more likely to resist colds and flu … | Smokers are more likely to get colds and flu … |
| Children not exposed to secondhand smoke are less likely to get … pneumonia, bronchitis, ear infections, severe asthma … | Children exposed to secondhand smoke are more likely to get … pneumonia, bronchitis, ear infections, severe asthma … |
| Stopping smoking can be like riding a roller coaster—but with many more ups than downs. | Stopping smoking can be like riding a roller coaster—there will be some ups and downs. |
| Nicotine does NOT cause cancer. Cigarette smoke does. By quitting, you stop inhaling harmful tobacco smoke. | Nicotine does NOT cause cancer. Cigarettes cause cancer because you inhale the dirty tobacco smoke. |
Gain-framed messages can focus on attaining a desirable outcome or not attaining (avoiding) an undesirable outcome, both beneficial. Loss-framed messages can emphasize attaining an undesirable outcome or not attaining (avoiding) a desirable outcome, both costs.
During the 4-month treatment phase of the study, specialists in both counseling groups (gain-framed and standard-care) received weekly supervision by telephone from a doctoral-level supervisor at Yale University. For specialists in the standard-care counseling group, this call was conducted in a group format; and for specialists in the gain-framed counseling group, this call was conducted on a one-on-one basis. Specialists in the standard-care counseling group discussed general topics that were related to standard-care issues (eg, helping pregnant smokers to quit). For specialists in the gain-framed counseling group, these supervision sessions were intended to help ensure a high level of adherence to the gain-framed protocol, and they included written and verbal feedback regarding one audiotape rating worksheet per week. These worksheets included adherence ratings of gain-framed items (achieving benefits and avoiding negative consequences), standard quitline items (assessing current smoking, assessing quit attempts, assessing medication use, and assessing intentions to quit smoking), and gain-framed inconsistent items (incurring costs and avoiding positive consequences), all of which were rated on a seven-point scale: 1 = “not at all”; 2 = “a little”; 3 = “infrequent”; 4 = “somewhat”; 5 = “quite a bit”; 6 = “considerably”; and 7 = “extensively.” All specialists in this study were paid $25 per supervision telephone call.
Assessments: Demographic Characteristics, Manipulation Checks, Fidelity Assessment, and Specialist Satisfaction
Demographic characteristics were collected during the initial telephone call. In this telephone call, enrolled callers completed a standard NYSSQL questionnaire by providing demographics and their personal smoking history.
Manipulation checks were conducted at the end of the intake telephone call, in which all callers were asked to answer two questions that evaluated the content of the telephone call. First, callers rated whether the telephone call focused on the benefits or the costs of smoking cessation on a scale of 1–5 (where 1 = “It focused heavily on the benefits of quitting smoking”; 2 = “It focused somewhat on the benefits of quitting smoking”; 3 = “It neither focused on the benefits of quitting or the costs of smoking”; 4 = “It focused somewhat on the costs of continuing to smoke”; and 5 = “It focused heavily on the costs of continuing to smoke”). Second, the overall tone of the telephone call was rated on a scale of 1–5 (where 1 = “extremely negative”; 2 = “somewhat negative”; 3 = “neither positive or negative”; 4 = “somewhat positive”; and 5 = “extremely positive”). Previous framing studies have used these measures and shown empirically that they are sensitive to differences in message framing (25). We also hypothesized that there would be no difference between the two groups at the 2-week follow-up on satisfaction with their initial contact with the quitline or their duration of engagement with the written materials. Satisfaction with their initial contact with the quitline was measured on a scale of 1–4 (where 1 = “very satisfied”; 2 = “mostly satisfied”; 3 = “somewhat satisfied”; and 4 = “not at all satisfied”). Duration of engagement with the written materials was measured on a scale of 0–3 (where 0 = “0 minutes”; 1 = “1 to 10 minutes”; 2 = “10 to 20 minutes”; and 3 = “more than 20 minutes”).
Fidelity of counseling delivery was tested through ratings of the audiotapes made of the interviews. Eight independent tape raters, who were blind to the study hypotheses, rated a random sample of approximately 20% of all tapes (400 tapes divided into 50 tapes per rater that were posted onto a secure password-protected web site). The raters used a validated adherence system that evaluated discriminability (ie, the capacity to discriminate) between the two types of counseling in the use of two gain-framed statement items (ie, achieving benefits and avoiding negative consequences) and four standard quitline interview items (ie, assessing current smoking, assessing quit attempts, assessing medication use, and assessing intentions to quit) (30). Raters assessed these items by use of a seven-point scale regarding adherence (where 1 = “not at all”; 2 = “a little”; 3 = “infrequent”; 4 = “somewhat”; 5 = “quite a bit”; 6 = “considerably”; and 7 = “extensively”). A reliability sample of 10 tapes revealed a high level of interrater reliability by use of the model for random effects by Shrout and Fleiss (31) (range of mean intraclass correlation coefficient estimates for all six items = .87–.99).
Finally, we hypothesized that the training would not decrease specialists’ satisfaction with their job. To test this hypothesis, at baseline and after the final smoker was enrolled in the smoking cessation study, we asked specialists: “How satisfied are you with the current coaching services that you have been providing?” This item was rated on a scale of 1–4 (where 1 = “Not at all satisfied”; 2 = “somewhat satisfied”; 3 = “mostly satisfied”; and 4 = “very satisfied”).
Outcome Measures
We analyzed treatment fidelity and smoking cessation as primary outcomes. The treatment fidelity outcome examined was the difference in ratings of frequency of gain-framed statements between the two types of counseling. Two primary smoking cessation outcomes were examined: 1) quitting for 24 hours at the 2-week follow-up and 2) point prevalence abstinence (ie, quitting over a specified time period) over the last 7 days at the 3-month follow-up. Abstinence from smoking was defined as self-reported abstinence (no smoking, not even a puff) during the specified treatment period after quitting. For all intention-to-treat analyses, in accordance with the conservative standard in the field and other large-scale smoking cessation studies (32–35), enrolled callers who dropped out were considered to be smoking.
The secondary outcomes included quit attempts, medication adherence, and positive health expectancies. At the 2-week follow-up, all callers were asked to answer whether they attempted to quit smoking in “yes” or “no” format (36). For the intention-to-treat analysis of this variable, we considered those who we were unable to reach for a follow-up call to have not made a quit attempt. Enrolled callers were asked how much medication (number of patches, pieces of gum, or number of lozenges) they had used so that medication adherence could be assessed (37). A single item was used to measure positive health expectancies at the time of the baseline call and the 3-month follow-up. All callers were asked to rate how likely they thought the statement, “I will be healthier,” would be if they stopped smoking on a scale of 1–7 (38) (where 1 = “no chance”; 2 = “very unlikely”; 3 = “unlikely”; 4 = “moderate chance”; 5 = “likely”; 6 = “very likely”; and 7 = “certain to happen”).
Statistical Analysis
The χ2 tests and independent sample t tests, respectively, were used to analyze 1) manipulation check items and 2) differences in adherence between specialists in the gain-framed counseling group and those in the standard-care counseling group. Paired samples t tests were used to assess differences in specialists’ satisfaction. Because of the small sample sizes for analyses regarding specialists’ satisfaction, Cohen d estimates (39) were also calculated. The distribution of the variables measuring specialists’ adherence and satisfaction, both of which were measured on an ordinal scale, was checked and tested for normality, and any item with a skew index of greater than 3.0 or a kurtosis index of greater than 8.0 (40) was analyzed with a nonparametric test (Mann–Whitney test for adherence and Wilcoxon signed-rank test for satisfaction). Baseline characteristics of the specialists and callers in the smoking cessation study were analyzed by use of χ2 tests for categorical variables and a general linear model for continuous variables. Consistent with the standard in the field (32–35,41,42), no adjustments were made for multiple comparisons of multiple endpoints. To examine treatment effects, differences between groups in the smoking cessation outcomes (ie, quitting for 24 hours at the 2-week follow-up and 7-day point prevalence abstinence at the 3-month follow-up) were analyzed by use of logistic regression, with gain-framed counseling compared with standard-care counseling in single regression models. Analyses were conducted with both survey respondents and an intention-to-treat population. All callers who were enrolled at the initial intake telephone call were included in the intention-to-treat population. For secondary outcomes (ie, quit attempts at the 2-week follow-up, medication adherence at the 3-month follow-up, and change in positive health expectancies from baseline to the 3-month follow-up), we analyzed categorical outcomes by use of logistic regression and continuous outcomes by use of a general linear model. We used SPSS version 16.0 for Windows (SPSS, Inc, Chicago, IL) and SAS version 9.1 for Windows (SAS Institute, Inc, Cary, NC) to conduct all analyses. All statistical tests were two-sided.
Results
Specialist and Caller Characteristics
Twenty-eight NYSSQL specialists consented and were enrolled in the study. Because we had a larger sample of enrolled callers who received standard-care counseling than gain-framed counseling (ie, 1222 callers in the standard-care group and 810 in the gain-framed group), we examined our recruitment and call-length data. We discerned that the recruitment rates (defined as the number who consented divided by number of eligible callers during the study time period) were similar in the standard-care group (mean = 41.4% and median = 41%) and in the gain-framed group (mean = 31.8% and median = 31%; mean difference = 9.7%, 95% confidence interval [CI] = −2.7% to 22.1%; P = .12). We analyzed the length of calls in a random sample of 400 calls (this sample of calls was also used for the fidelity analyses below) and found that the time spent per call was statistically significantly longer in the gain-framed group (n = 200; mean = 14 minutes and 37 seconds) than in the standard-care group [n = 200; mean = 12 minutes and 8 seconds; t(df = 398) = 3.5; mean difference = −2 minutes and 29 seconds, 95% CI = −3 minutes and 53 seconds to −1 minute and 5 seconds; P = .001]. Thus, the time available for specialists in the gain-framed counseling group to take calls was reduced by about 2.5 minutes per call compared with specialists in the standard-care counseling group. However, the randomization procedure appeared to be effective in that the specialists in the two groups were similar in age, sex, ethnicity, and education level (Table 2).
Table 2.
Baseline specialist demographic variables
| Variables | Gain-framed group (n = 14) | Standard-care group (n = 14) | P* |
| Age, y (±SD) | 30.1 (±8.1) | 34.9 (±11.8) | .23 |
| % women | 78.6 | 57.1 | .23 |
| % white | 71.4 | 85.7 | .36 |
| % with bachelor's degree | 50 | 50 | .68 |
Variables were analyzed with χ2 tests for categorical variables and a general linear model for continuous variables. All statistical tests were two-sided.
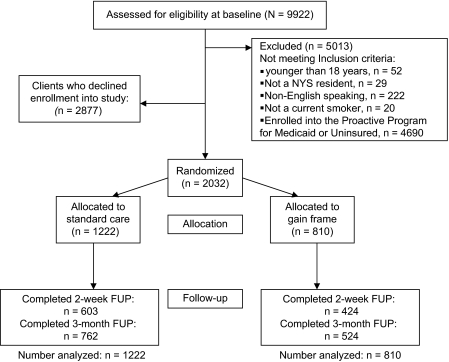
The flow of callers enrolled for smoking cessation treatment from initial screening to study completion is presented in Figure 2. Although we based our initial power estimates on a sample size of 2500 callers (1250 callers per counseling group), which we anticipated being able to recruit in 3 months, recruitment was slower than anticipated, and we needed to end the study before accruing our entire sample so that other scheduled studies could be conducted at the NYSSQL. Of the 9922 callers screened, 5013 were excluded because they did not meet inclusion criteria, 2877 declined enrollment, and 2032 were enrolled in the study. As presented in Table 3, callers who declined enrollment were different from those who were enrolled on racial background, sex, caller education, number of cigarettes smoked per day, and years smoked. Age was similar between these groups.
Figure 2.
Flow of callers for smoking cessation treatment study. FUP = Follow-up; NYS = New York State.
Table 3.
Baseline characteristics by caller enrollment
| Variables | Enrolled (n = 2032) | Declined (n = 2877) | P* |
| % white | 76.7 | 73.1 | <.001 |
| % women | 56.7 | 52.9 | <.001 |
| % with some college education | 25.2 | 23.4 | <.001 |
| No. of cigarettes smoked per day (±SD) | 20.1 (±11.1) | 18.3 (±14.5) | <.001 |
| No. of years smoking cigarettes (±SD) | 26.0 (±14.3) | 23.1 (±14.8) | <.001 |
| Age, y (±SD) | 46.7 (±13.7) | 46.2 (±14.4) | .29 |
Variables were analyzed with χ2 tests for categorical variables and a general linear model for continuous variables. All statistical tests were two-sided.
Therefore, the intention-to-treat sample was composed of 2032 callers who consented to and were enrolled at the initial treatment telephone call and were randomly assigned to either the gain-framed or standard-care counseling group. In this sample, there were no differences on demographic and smoking history variables between the treatment conditions (Table 4). Follow-up data were obtained for 1027 (50.5%) of the 2032 enrolled callers at 2 weeks and 1286 (63.3%) at 3 months. There were no differences in follow-up rates by counseling group for either the 2-week or the 3-month follow-up (Table 4).
Table 4.
Baseline variables and study follow-up rates of callers enrolled and counseled
| Variables | Gain-framed group (n = 810) | Standard-care group (n = 1222) | P* |
| % white | 79.6 | 75.8 | .19 |
| % women | 59.1 | 55.2 | .08 |
| % graduated from high school | 32.8 | 33.4 | .09 |
| Age, y (±SD) | 47.2 (±13.4) | 46.4 (±13.9) | .20 |
| No. of cigarettes smoked per day (±SD) | 20.1 (±11.2) | 20.1 (±11.0) | .98 |
| No. of years of smoking cigarettes (±SD) | 26.7 (±13.8) | 25.5 (±14.6) | .07 |
| Follow-up data obtained | |||
| 2-wk follow-up, % (No.) | 52.3 (424) | 49.3 (603) | .19 |
| 3-mo follow-up, % (No.) | 64.7 (524) | 62.4 (762) | .29 |
Variables were analyzed with χ2 tests for categorical variables and a general linear model for continuous variables. All statistical tests were two-sided.
Manipulation Checks
In accordance with the objective of this study, differences emerged on specific manipulation check items. A higher proportion of callers who received gain-framed counseling rated the telephone call as focusing heavily on the benefits of quitting smoking (89.4%) than callers who received standard-care counseling (81.7%) [χ2(df = 4) = 23.1, P < .001]. This difference is similar in magnitude to our other message-framing studies (25,26) that have shown statistically significant effects on smoking behavior. The overall tone of the telephone call was rated as extremely positive by a higher proportion of callers in the gain-framed counseling group (70.5%) than in the standard-care counseling group (52.2%) [χ2(df = 4) = 68.9, P < .001]. Consistent with our expectations, there were no differences between the groups on satisfaction with their initial contact with the quitline (for the gain-framed group, 92.4% = very satisfied; for the standard-care group, 91.4% = very satisfied; P = .32) or level of engagement with the written materials (for the gain-framed group, 37.8% read materials more than 20 minutes; for the standard-care group, 34.6% read materials more than 20 minutes; P = .55).
Fidelity Outcomes
As presented in Table 5 and consistent with the hypotheses of this study, there were statistically significant differences between the two experimental counseling groups on the two gain-framed statement items and no differences between the two counseling groups on the four standard quitline interview items. Specialists providing gain-framed counseling used gain-framed statements statistically significantly more frequently than those providing standard-care counseling as assessed with frequency ratings for the two types of gain-framed statements, achieving benefits and avoiding negative consequences (for achieving benefits, gain-framed mean frequency rating = 3.9 vs standard-care mean frequency rating = 1.4; mean difference = −2.5; 95% CI = −2.8 to −2.3; P < .001; for avoiding negative consequences, gain-framed mean frequency rating = 1.5 vs standard-card mean frequency rating = 1.0; mean difference = −0.5; 95% CI = −0.6 to −0.3; P < .001). The gain-framed item, “avoiding negative consequences,” was the only item with positive skew and kurtosis (mean = 1.3; 95% CI = 1.2 to 1.4; skew = 3.0 [ie, most of the scores were below the mean]; kurtosis = 10.8 [ie, the distribution had a higher peak and heavier tails]). This item remained statistically significantly different between groups when tested with a Mann–Whitney test (gain-framed mean rank statistic = 229.8, standard-care mean rank statistic = 171.3, and Mann–Whitney U statistic = 14 150; P < .001).
Table 5.
Mean adherence ratings of specialists in gain-framed and standard-care counseling groups*
| Type of message and items | Mean score |
Mean difference | 95% CI of mean difference | Statistics† |
||
| Gain-framed group | Standard-care group | t | P | |||
| Gain-framed | ||||||
| Achieve benefits | 3.9 | 1.4 | −2.5 | −2.8 to −2.3 | 20.1 | <.001 |
| Avoid negative consequences | 1.5 | 1.0 | −0.5 | −0.6 to −0.3 | 7.1 | <.001 |
| Standard-care | ||||||
| Assess current smoking | 4.5 | 4.4 | 0.1 | −0.5 to 0.3 | 0.5 | .62 |
| Assess quit attempts | 2.9 | 2.9 | 0 | −0.1 to 0.2 | 0.5 | .62 |
| Assess medication use | 2.9 | 2.9 | 0 | −0.3 to 0.2 | 0.1 | .94 |
| Intentions to quit smoking | 3.8 | 3.8 | 0 | −0.3 to 0.2 | 0.2 | .82 |
All ratings were made on a seven-point Likert scale (1 = “not at all”; 2 = “a little”; 3 = “infrequent”; 4 = “somewhat”; 5 = “quite a bit”; 6 = “considerably”; and 7 = “extensively”), with higher values indicating higher levels of adherence. There were 400 specialists in this analysis (200 per group). The gain-framed messages focused on attaining a desirable outcome (eg, living longer) or not attaining (or avoiding) an undesirable outcome (eg, reduced risk of health problems), both benefits of quitting smoking. CI = confidence interval.
All independent samples t tests had 398 df. All statistical tests were two-sided.
Specialist Satisfaction
Satisfaction was rated as higher than baseline for specialists in both the gain-framed counseling group [at baseline, mean satisfaction rating = 2.7; at end of enrollment, mean = 3.2; mean difference = −0.5; 95% CI = −0.9 to 0.0; t(df = 10) = 2.2; P = .05; d = 0.8] and the standard-care counseling group [at baseline, mean satisfaction rating = 3.2; at end of enrollment, mean = 3.5; mean difference = −0.3; 95% CI = −0.6 to 0.0; t(df = 11) = 2.3; P = .04; d = 0.7]. Analysis of the distribution of the data for these variables showed that neither was nonnormal (ie, neither skew nor kurtosis was above our prespecified cutoff values [which were skew greater than 3.0 and kurtosis greater than 8.0]).
Smoking Outcomes
As presented in Table 6, a statistically significant effect favoring the gain-framed group as compared with the standard-care group was found for 24-hour abstinence in the 2-week follow-up survey (P < .001; Wald statistic = 19.8; df = 1; n = 1027; 99 [23.3%] of the 424 in the gain-framed group vs 76 [12.6%] of the 603 in the standard-care group; odds ratio [OR] = 2.1; 95% CI = 1.5 to 2.9). The difference at the 3-month survey follow-up for 7-day point prevalence abstinence was not statistically significant (P = .48; 148 [28.4%] of the 522 in the gain-framed group vs 202 [26.6%] of the 760 in the standard-care group). Outcomes that were based on an intention-to-treat analysis revealed generally lower quit rates but paralleled survey respondent outcomes (24-hour abstinence at the 2-week follow-up: P < .001; Wald statistic = 21.5; df = 1; n = 2032; 99 [12.2%] of the 810 in the gain-framed group vs 76 [6.2%] of the 1222 in the standard-care group; OR = 2.1; 95% CI = 1.5 to 2.9; and 7-day point prevalence abstinence at the 3-month follow-up: P = .31, 148 [18.3%] of the 810 in the gain-framed group vs 202 [16.5%] of the 1222 in the standard-care group).
Table 6.
Quit attempts and smoking cessation for gain-framed and standard-care counseling groups*
| Outcome | Sample size, No. | % gain-framed group (No. quit attempt or abstinent/No. responded to follow-up survey) | % standard-care group (No. quit attempt or abstinent/No. responded to follow-up survey) | OR (95% CI) |
| Quit attempt | 1027 | 31.1 (132/424) | 16.7 (101/603) | 2.2† (1.7 to 3.0) |
| 24-h abstinence at 2-wk follow-up | 1027 | 23.3 (99/424) | 12.6 (76/603) | 2.1† (1.5 to 2.9) |
| 7-d abstinence at 3-mo follow-up | 1282 | 28.4 (148/522) | 26.6 (202/760) | 1.1 (0.9 to 1.4) |
Callers in the gain-framed counseling group received counseling and printed materials with statements and messages regarding the benefits of quitting. Callers in the standard-care counseling group received counseling and printed materials with statements and messages regarding both the costs of smoking and the benefits of quitting. CI = confidence interval; OR = odds ratio; both from logistic regressions.
P < .001. All statistical tests were two-sided.
Quit Attempts, Medication Adherence, and Expectancies
A survey respondent analysis showed that statistically significantly more callers in the gain-framed group than in the standard-care group made an attempt to quit smoking, as determined by self-report at the 2-week follow-up survey (P < .001; Wald statistic = 28.6; df = 1; n = 1027; 132 [31.1%] of the 424 in the gain-framed group vs 101 [16.7%] of the 603 in the standard-care group; OR = 2.2; 95% CI = 1.7 to 3.0) (Table 6). Consistent with the smoking outcomes, intention-to-treat analysis of quit attempts showed a lower rate of attempts but paralleled the survey respondent outcome (P < .001). When surveyed at the 3-month follow-up, callers in both groups reported use of a similar number of nicotine replacement therapy products (ie, the numerical value representing the number of patches, pieces of gum, or number of lozenges) (n = 1231; in the gain-framed group, mean = 26.9 patches, gum, or lozenges; and in the standard-care group, mean = 30.6 patches, gum, or lozenges; mean difference = 3.7; 95% CI = −2.6 to 9.9; P = .25), indicating no differences in medication adherence between the counseling groups. When examining change in scores from baseline to the 3-month follow-up, callers in the gain-framed group had statistically significantly higher expectancies that they would be healthier (n = 500 in the gain-framed group; mean rating of likelihood of being healthier = 0.2) than those in the standard-care group [n = 702 in the standard-care group; mean rating of likelihood of being healthier = 0.1; mean difference = −0.1; 95% CI = −0.3 to 0.0; F(df = 1) = 5.3; P = .02].
Discussion
The fidelity outcomes from this study suggest that quitlines can train their staff to deliver gain-framed counseling in a consistent fashion. Smokers who spoke with a specialist who received the gained-framed training and ongoing supervision had slightly better smoking cessation outcomes than those who spoke with a specialist who received standard-care training and ongoing supervision. Moreover, there were no differences in callers’ ratings of satisfaction with NYSSQL services between the study groups, and specialists’ ratings of satisfaction were not negatively affected as well. Although the findings from this study need to be replicated and validated by the NYSSQL and other quitlines, they support the hypothesis that quitlines can improve their services by implementing relatively straightforward training programs for telephone staff. Future studies should explore the application of different counseling techniques that might boost cessation outcomes by using rigorous procedures to monitor treatment fidelity (30,43–45). For instance, although virtually all quitlines use some type of motivational interviewing or cognitive behavioral counseling strategies (11–15), the effectiveness of these techniques in a quitline setting has not been tested empirically.
In this study, consistent with previous findings (25) from our smoking cessation clinical trial testing message framing to augment bupropion SR, we observed an initial statistically significant increase in quit rates at 2 weeks but this difference was no longer statistically significant at the 3-month follow-up. In accordance with our hypotheses, we found a statistically significant increase in positive health expectancies over time for callers in the gain-framed group, indicating that the gain-framed intervention did, in fact, affect smokers’ expectations about quitting in the intended manner.
The fact that the difference in quit rates at 3 months was no longer statistically significant might be explained by the low intensity of the gain-framed intervention. To ensure that the study was truly translational, the gain-framed counseling intervention conformed to the brief nature of the NYSSQL standard-care interventions, but this brevity might have attenuated our results. Multiple messages may be necessary for longer-term impact (46). Our use of the dichotomous primary smoking cessation outcomes (ie, yes or no at 2 weeks and 3 months) should also be considered as a possible measurement constraint. Several of our previous studies (25,26,28) that showed a benefit of gain-framed messages used continuous variables as primary or secondary endpoints. For instance, Schneider et al. (26) found a decrease in number of cigarettes smoked among participants who were exposed to gain-framed messages, and Steward et al. (28) found higher intentions to quit among participants who received gain-framed messages. Toll et al. (25) found that time to first cigarette was more sensitive to message-framing effects than the primary cessation outcomes, both of which were categorical. Indeed, we found that our continuous secondary outcome of expectancy ratings showed statistically significant differences favoring the gain-framed counseling. Given the brevity of quitline calls and the pressure to have very brief assessments, we did not include a more comprehensive continuous outcome, such as time to first cigarette. Consequently, future quitline studies should consider including brief measures of time to first cigarette. Although it may not be possible to use a time-intensive calendar method, such as the timeline follow back in which every day of smoking is documented (47), callers could be asked the date of their first cigarette, so that time to first cigarette could be calculated.
The initial advantage that we found for gain-framed smoking cessation messages might be prolonged in a real-world setting with additional electronic interventions implemented at multiple time points (eg, biweekly or monthly follow-up text messaging or telephone calls). This type of intervention would allow for further research on more intensive gain-framed messaging without disrupting the actual operations of the NYSSQL or other quitlines. Additionally, by standardizing message delivery, the intervention could provide more consistent, and perhaps higher quality, counseling than is available in some settings (48). Recent research conducted on automated delivery of smoking cessation services appears to be promising. For instance, it has been found that text messaging (49,50), interactive voice response (51), and some combination of these services (52) improve rates of quitting. Thus, we suggest that future studies should attempt to improve on the short-term advantage found in this study by adding some type of automated system that delivers gain-framed smoking cessation messages. This addition may prove to be a cost-effective alternative to hiring additional staff.
A recent review (53) suggests that for nicotine replacement therapy to have the greatest impact on tobacco control and public health, increases in quit attempts and nicotine replacement therapy adherence are needed. Thus, it is encouraging that callers who received the gain-framed intervention were more likely to make a quit attempt. However, consistent with our previous message framing and bupropion study (25), in which targeted gain-framed statements aimed at medication use did not improve adherence with bupropion, we found that gain-framed statements that specifically targeted nicotine replacement therapy use did not result in improved nicotine replacement therapy adherence for those in the gain-framed counseling group. Thus, now there are two studies [(25) and this study] showing no relationship between message framing and adherence to smoking cessation medication.
The specialists in the gain-framed group provided 2.5 minutes of additional counseling on average compared with those in the standard-care group. Previous research on number of minutes of smoking cessation counseling has been mixed, with one meta-analysis reporting a benefit for longer interactions (54) and another reporting no effect (55). Whether or not the increases in quit rates that we found in this study are attributable to an increase in counseling minutes or to gain-framed messaging, researchers and policy makers need to weigh whether the additional time required for gain-framed counseling is worth the small increases in quit rates observed in this study. Although the 10% advantage in quit rates found at 2 weeks had diminished to a little less than 2% at 3 months, some have argued that even a 2% advantage would be clinically meaningful (56), especially in the context of a large-scale cessation program. Of course, the goal of interventions should be to achieve the highest quit rates possible for the most meaningful health gains (eg, additional years of life).
The study has several strengths. These include random assignment of specialists to gain-framed or standard-care counseling groups; robust attention controls for counseling intervention; and specialist supervision across counseling groups, large sample size, and translatability of findings.
The study has several potential limitations. The limitations include in addition to the low intensity of the gain-framed intervention and use of dichotomous primary smoking outcomes, different levels of supervision (ie, individual supervision for the gain-framed counseling group and group supervision for the standard-care counseling group) and low follow-up rates. However, the follow-up rates that we observed are consistent with many large-scale rigorous quitline studies conducted by our group (36,57,58) and others (11,12). The callers who enrolled in this study, compared with those who declined, were more likely to be female, higher educated, and white and to have smoked more cigarettes for a longer time period. Hence, generalizability is limited to callers who have similar characteristics. The fact that gain-framed counseling specialists spent approximately 2.5 minutes longer per call than standard-care counseling specialists, a statistically significant difference, might account for the differences in smoking cessation effects between the two groups. However, as described above, results for minutes per session from meta-analyses have been mixed (54,55). Finally, consistent with the standard in the field of smoking cessation research, no adjustments were made because of multiple comparisons (32–35,42,59).
The fidelity outcomes from this study should encourage quitlines to test novel counseling strategies for their ability to increase smoking cessation rates and, thus, prevent cancer. Furthermore, gain-framed statements appear to be somewhat beneficial in enhancing short-term smoking cessation and other secondary outcomes, such as quit attempts and positive health expectancies. A higher rate of long-term smoking cessation was not obtained for callers who received the gain-framed intervention compared with the standard-care intervention. Given that long-term cessation is necessary to prevent cancer-related mortality and other tobacco-induced diseases, future translational research should investigate how to extend the short-term effects that we observed in this study to long-term increases in smoking cessation rates.
Funding
National Institutes of Health grants (R21-CA127818 to B.A.T., K12-DA000167 to B.A.T., P50-AA15632 to S.O., K05-AA014715 to S.O., R01-CA068427 to P.S.) from the National Cancer Institute, National Institute on Drug Abuse, and the National Institute on Alcohol Abuse and Alcoholism, by a contract from the New York State Department of Health and by the State of Connecticut, Department of Mental Health and Addictions Services.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the National Institute on Drug Abuse, the National Institute on Alcohol Abuse and Alcoholism, or the National Institutes of Health. The corresponding author had full access to all data in this study and had final responsibility for the decision to submit the paper for publication.
Dr S. O’Malley received honoraria as a member of workgroup on medications development for alcoholism sponsored by the American College of Neuropsychopharmacology and received travel reimbursement for talks at the Controlled Release Society, the Drug Information Association, and the Association for Medical Education and Research in Substance Abuse. She has consulted to the University of Chicago on studies of naltrexone for smoking cessation. She is a partner in Applied Behavioral Research, and she is a Scientific Panel Member, Butler Center for Research at Hazelden.
We would like to thank Srinivasa Seshadri for his assistance with implementing the project, Elaine LaVelle for assistance with the randomization procedures and data management, and Nicole Katulak and Kristina Schmid for assistance with creating the gain-framed intervention. Portions of this article were presented at the National Conference on Tobacco or Health in Phoenix, AZ, in June 2009. The study is publicly registered at www.clinicaltrials.gov (Identifier: NCT00589277).
References
- 1.US Department of Health and Human Services. Cancer Facts & Figures 2008. Atlanta, GA: American Cancer Society; 2008. [Google Scholar]
- 2.US Department of Health and Human Services. Reducing the Health Consequences of Smoking: 25 Years of Progress: A Report of the Surgeon General: 1989 Executive Summary. Rockville, MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1989. [Google Scholar]
- 3.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services. The Health Benefits of Smoking Cessation. Rockville, MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. [Google Scholar]
- 5.National Center for Health Statistics. Health, United States, 2006, With Chartbook With Trends in the Health of Americans. Hyattsville, MD: Public Health Service; 2006. [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2004. Morb Mortal Wkly Rep. 2005;54(44):1121–1124. [PubMed] [Google Scholar]
- 7.Cummins S, Bailey L, Campbell S, Koon-Kirby C, Zhu S-H. Tobacco cessation quitlines in North America: a descriptive study. Tob Control. 2007;16(suppl I):i9–i15. doi: 10.1136/tc.2007.020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control. Best Practices for Comprehensive Tobacco Control Programs. Atlanta, GA: USDHHS; 2007. [Google Scholar]
- 9.Swartz SS, Cowan TM, Klayman JE, Welton M, Leonard BA. Use and effectiveness of tobacco telephone counseling and nicotine therapy in Maine. Am J Prev Med. 2005;29(4):288–294. doi: 10.1016/j.amepre.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 10.Cummins H, Anderson KK, Mills C, Zhu J. Reaching young adult smokers through quitlines. Am J Public Health. 2007;97(8):1402–1405. doi: 10.2105/AJPH.2006.101741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.An L, Schillo B, Kavanaugh A, et al. Increased reach and effectiveness of a statewide tobacco quitline after the addition of access to free nicotine replacement therapy. Tob Control. 2006;15(4):286–293. doi: 10.1136/tc.2005.014555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hollis J, McAfee T, Fellows J, Zbikowski S, Stark M, Riedlinger K. The effectiveness and cost effectiveness of telephone counseling and the nicotine patch in a state tobacco quitline. Tob Control. 2007;16(Suppl 1):i53–i59. doi: 10.1136/tc.2006.019794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu S-H, Anderson C, Tedeschi G, et al. Evidence of real-world effectiveness of a telephone quitline for smokers. N Engl J Med. 2002;347(14):1087–1093. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- 14.Borland R, Segan C, Livingston P, Owen N. The effectiveness of callback counseling for smoking cessation: a randomized trial. Addiction. 2001;96(6):881–889. doi: 10.1046/j.1360-0443.2001.9668819.x. [DOI] [PubMed] [Google Scholar]
- 15.Gilbert H, Sutton S. Evaluating the effectiveness of proactive telephone counseling for smoking cessation in a randomized controlled trial. Addiction. 2006;101(4):590–598. doi: 10.1111/j.1360-0443.2006.01398.x. [DOI] [PubMed] [Google Scholar]
- 16.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–458. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- 17.Rothman AJ, Bartels RD, Wlaschin J, Salovey P. The strategic use of gain- and loss-framed messages to promote healthy behavior: how theory can inform practice. J Commun. 2006;56(Suppl 1):S202–S220. [Google Scholar]
- 18.Rothman AJ, Salovey P, Antone C, Keough K, Martin CD. The influence of message framing on intentions to perform health behaviors. J Exp Soc Psychol. 1993;29(5):408–433. [Google Scholar]
- 19.Apanovitch AM, McCarthy D, Salovey D. Using message framing to motivate HIV testing among low income, ethnic minority women. Health Psychol. 2003;22(1):60–67. doi: 10.1037//0278-6133.22.1.60. [DOI] [PubMed] [Google Scholar]
- 20.Mann T, Sherman D, Updegraff J. Dispositional motivations and message framing: a test of the congruency hypothesis in college students. Health Psychol. 2004;23(3):330–334. doi: 10.1037/0278-6133.23.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behavior: the role of message framing. Psychol Bull. 1997;121(1):3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- 22.Banks SM, Salovey P, Greener S, et al. The effects of message framing on mammography utilization. Health Psychol. 1995;14(2):178–184. doi: 10.1037//0278-6133.14.2.178. [DOI] [PubMed] [Google Scholar]
- 23.Schneider TR, Salovey P, Apanovitch AM, et al. The effects of message framing and ethnic targeting on mammography use among low-income women. Health Psychol. 2001;20(4):256–266. doi: 10.1037//0278-6133.20.4.256. [DOI] [PubMed] [Google Scholar]
- 24.Detweiler JB, Bedell BT, Salovey P, Pronin E, Rothman AJ. Message framing and sunscreen use: gain-framed messages motivate beach goers. Health Psychol. 1999;18(2):189–196. doi: 10.1037//0278-6133.18.2.189. [DOI] [PubMed] [Google Scholar]
- 25.Toll B, O’Malley S, Katulak N, et al. Comparing gain- and loss-framed messages for smoking cessation with bupropion: a randomized controlled trial. Psychol Addict Behav. 2007;21(4):534–544. doi: 10.1037/0893-164X.21.4.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schneider TR, Salovey P, Pallonen U, Mundorf N, Smith NF, Steward WT. Visual and auditory message framing effects on tobacco smoking. J Appl Soc Psychol. 2001;31(4):667–682. [Google Scholar]
- 27.McKee S, O’Malley S, Steward W, Neveu S, Land M, Salovey P. How to word effective messages about smoking and oral health: emphasize the benefits of quitting. J Dent Educ. 2004;68(5):569–573. [PubMed] [Google Scholar]
- 28.Steward WT, Schneider TR, Pizarro J, Salovey P. Need for cognition moderates responses to framed smoking-cessation messages. J Appl Soc Psychol. 2003;33(12):2439–2464. [Google Scholar]
- 29.Latimer A, Green K, Schmid K, et al. The identification of framed messages in the New York State Smokers’ Quitline materials and coaching. Health Educ Res. 2009 doi: 10.1093/her/cyp041. doi: 10.1093/her/cyp041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carroll K, Nich C, Sifry R, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57(1):225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- 31.Shrout P, Fleiss J. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 32.Gonzales D, Rennard S, Nides M, et al. Varenicline, an alpha-4-beta-2 nicotinic acetylcholine receptor partial agonist, vs. sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. JAMA. 2006;296(1):47–55. doi: 10.1001/jama.296.1.47. [DOI] [PubMed] [Google Scholar]
- 33.Jorenby D, Hays J, Rigotti N, et al. Efficacy of varenicline, an alpha-4-beta-2 nicotinic acetylcholine receptor partial agonist, vs. placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296(11):56–63. doi: 10.1001/jama.296.1.56. [DOI] [PubMed] [Google Scholar]
- 34.Ahluwalia JS, Harris KJ, Catley D, Okuyemi KS, Mayo MS. Sustained-release bupropion for smoking cessation in African Americans: a randomized controlled trial. JAMA. 2002;288(4):468–474. doi: 10.1001/jama.288.4.468. [DOI] [PubMed] [Google Scholar]
- 35.Hurt RD, Sachs DP, Glover ED, et al. A comparison of sustained-release bupropion and placebo for smoking cessation. N Engl J Med. 1997;337(17):1195–1202. doi: 10.1056/NEJM199710233371703. [DOI] [PubMed] [Google Scholar]
- 36.Cummings K, Hyland A, Fix B, et al. Free nicotine patch giveaway program: 12 month follow-up of participants. Am J Prev Med. 2006;31(2):181–184. doi: 10.1016/j.amepre.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 37.Jolicoeur D, Ahluwalia J, Richter K, et al. The use of nicotine patches with minimal intervention. Prev Med. 2000;30(6):504–512. doi: 10.1006/pmed.2000.0670. [DOI] [PubMed] [Google Scholar]
- 38.Mckee S, O’Malley S, Salovey P, Krishnan-Sarin K, Mazure C. Perceived risks and benefits of smoking cessation: gender-specific predictors of motivation and treatment outcome. Addict Behav. 2005;30(3):423–435. doi: 10.1016/j.addbeh.2004.05.027. [DOI] [PubMed] [Google Scholar]
- 39.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 40.Kline R. Principles and Practice of Structural Equation Modeling. 2nd ed. New York, NY: The Guilford Press; 2005. [Google Scholar]
- 41.Hays J, Hurt R, Rigotti N, et al. Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation: a randomized controlled trial. Ann Intern Med. 2001;135(6):423–433. doi: 10.7326/0003-4819-135-6-200109180-00011. [DOI] [PubMed] [Google Scholar]
- 42.Swan GE, McAfee T, Curry SJ, et al. Effectiveness of bupropion sustained release for smoking cessation in a health care setting. Arch Intern Med. 2003;163(2):2337–2344. doi: 10.1001/archinte.163.19.2337. [DOI] [PubMed] [Google Scholar]
- 43.Carroll K, Ball S, Nich C, et al. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: a multisite effectiveness study. Drug Alcohol Depend. 2006;81(3):301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Martino S, Carroll K, Nich C, Rounsaville B. A randomized controlled pilot study of motivational interviewing for patients with psychotic and drug use disorders. Addiction. 2006;101(10):1479–1492. doi: 10.1111/j.1360-0443.2006.01554.x. [DOI] [PubMed] [Google Scholar]
- 45.Martino S, Ball S, Nich C, Frankforter T, Carroll K. Community program therapist adherence and competence in motivational enhancement therapy. Drug Alcohol Depend. 2008;96(1–2):37–48. doi: 10.1016/j.drugalcdep.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Latimer A, Rench T, Rivers S, et al. Promoting participation in physical activity using framed messages: an application of prospect theory. Br J Health Psychol. 2008;13(pt 4):659–681. doi: 10.1348/135910707X246186. [DOI] [PubMed] [Google Scholar]
- 47.Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Wilson VB, editors. Assessing Alcohol Problems: A Guide for Clinicians and Researchers. 2nd ed. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. pp. 75–99. [Google Scholar]
- 48.Carroll K, Ball S, Martino S, et al. Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. Am J Addict. 2008;165(5):881–888. doi: 10.1176/appi.ajp.2008.07111835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Obermayer J, Riley W, Asif O, Jean-Mary J. College smoking-cessation using cell phone text messaging. J Am Coll Health. 2004;53(2):71–78. doi: 10.3200/JACH.53.2.71-78. [DOI] [PubMed] [Google Scholar]
- 50.Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomized trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14(4):255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reid R, Pipe A, Quinlan B, Oda J. Interactive voice response telephony to promote smoking cessation in patients with heart disease: a pilot study. Patient Educ Couns. 2007;66(3):319–326. doi: 10.1016/j.pec.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 52.Brendryen H, Kraft P. Happy Ending: a randomized controlled trial of digital multi-media smoking cessation intervention. Addiction. 2008;103(3):478–484. doi: 10.1111/j.1360-0443.2007.02119.x. [DOI] [PubMed] [Google Scholar]
- 53.Amodei N, Lamb R. Over-the-counter nicotine replacement therapy: can its impact on smoking cessation be enhanced. Psychol Addict Behav. 2008;22(4):472–485. doi: 10.1037/0893-164X.22.4.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fiore M, Jaén C, Baker T, et al. Treating Tobacco Use and Dependence 2008 Update: Clinical Practice Guideline. Rockville, MD: USDHHS; 2008. [Google Scholar]
- 55.Pan W. Proactive telephone counseling as an adjunct to minimal intervention for smoking cessation: a meta-analysis. Health Educ Res. 2006;21(3):416–427. doi: 10.1093/her/cyl040. [DOI] [PubMed] [Google Scholar]
- 56.West R. The clinical significance of “small” effects of smoking cessation treatments [editorial] Addiction. 2007;102(4):506–509. doi: 10.1111/j.1360-0443.2007.01750.x. [DOI] [PubMed] [Google Scholar]
- 57.Cummings K, Fix B, Celestino P, Carlin-Menter S, O’Connor R, Hyland A. Reach, efficacy, and cost-effectiveness of free nicotine medication giveaway programs. J Public Health Manag Pract. 2006;12(1):37–43. doi: 10.1097/00124784-200601000-00009. [DOI] [PubMed] [Google Scholar]
- 58.Miller N, Frieden T, Liu S, et al. Effectiveness of a large-scale distribution programme of free nicotine patches: a prospective evaluation. Lancet. 2005;365(9474):1849–1854. doi: 10.1016/S0140-6736(05)66615-9. [DOI] [PubMed] [Google Scholar]
- 59.Hays J, Hurt R, Rigotti N, et al. Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation: a randomized controlled trial. Ann Intern Med. 2001;135(6):423–433. doi: 10.7326/0003-4819-135-6-200109180-00011. [DOI] [PubMed] [Google Scholar]