Abstract
The purpose of this prospective study was to determine whether using magnetic resonance imaging (MRI) for early screening for brain metastases (BM) can improve quality of life, survival in patients with non-small cell lung cancer (NSCLC). The study group comprised 183 patients newly diagnosed with NSCLC. All patients underwent limited brain MRI and routine workups. The control group comprised 131 patients with NSCLC who underwent limited brain MRI only if they had neurologic symptoms. The incidence of BM was 20.8% (38/183) in the study group and 4.6% (6/131) in the control group. The rate of upstaging based on the MRI data was 13.5% (15/111) overall and 15.9% (11/69) in patients that had been considered initially to be resectable surgically. There was no significant difference in survival outcome between the groups. Patients who had BM alone had a greater overall survival time (49 weeks) than those who had multiple systemic metastases (27 weeks; p=0.0307). In conclusions, limited brain MRI appears to be a useful, cost-effective method to screen for BM at the time of initial staging. And it may facilitate timely treatment of patients with NSCLC and improve their survival and quality of life.
Keywords: Carcinoma, Non-Small-Cell Lung; Neoplasm Staging; Neoplasm Metastasis; Magnetic Resonance Imaging; Diagnosis; Radiography
INTRODUCTION
Lung cancer is the leading cause of cancer death in most countries. Although much effort has been made over the last few decades to improve the survival of lung cancer patients, overall five-year survival rates remain unsatisfactorily low (14% in the U.S.A.) (1).
Brain metastasis (BM) is a major cause of the low survival rate and poor quality of life of cancer patients. The prognosis for patients with BM who go untreated is extremely poor (about one month following diagnosis) (2), whereas patients with non-small cell lung cancer (NSCLC) who are treated with radiation therapy survive for about 8 months (3). The incidence of BM in patients with locally advanced NSCLC is 12-28% over the entire course of the disease. In most cases of NSCLC, BM are diagnosed only after the development of symptoms, which is partly responsible for the poor prognosis of patients with NSCLC. In patients with small cell lung cancer (SCLC), the incidence of detectable BM at the time of initial diagnosis is 10-14%; the cumulative incidence at three years for patients that are in complete remission and that have few signs of disease is 59% (4). For patients with NSCLC, the incidence of BM at the time of initial diagnosis is about 6% according to a prospective study in which computerized axial tomography (CT) was used (5). The prognoses of patients with symptomatic BM are substantially worse than those in which the metastases are asymptomatic (6-8). Clearly, improvements in systemic and local therapies can improve the long-term survival of cancer patients, which means that early and accurate diagnosis of BM has become crucial to improving the quality of life and poor survival rates of cancer patients.
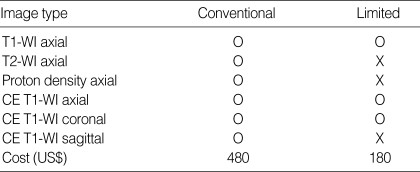
The use of imaging to detect extrathoracic metastasis, particularly BM, at the time of initial staging in asymptomatic patients is the subject of debate (8-10). Imaging is usually recommended in patients who form part of a population in which the overall incidence of BM is particularly high, such as in cases with adenocarcinomas (6, 11-13). Of the different imaging methods, MRI is more sensitive than CT and is the method of choice with which to screen for intracranial metastasis (12, 14-17). However, a major drawback to the routine use of brain MRI is its high cost. Therefore, we carried out the modified standard MRI or limited MRI procedure to detect BM at lower cost and without loss of sensitivity (18). In our pilot study limited MRI showed no difference with conventional MRI for detecting BM (sensitivity 97.67%, specificity 100%) (18). The cost of the modified MRI was US$ 180, which is substantially lower than the cost of conventional brain MRI (US$ 480). Based on these results, we conducted the present study to screen for BM at the time of initial staging and validated the clinical significance of the early detection of BM using limited brain MRI. The results have implications for the quality of life and survival of patients with NSCLC.
MATERIALS AND METHODS
Between May, 2001 and April, 2002, 183 patients were newly diagnosed with primary NSCLC at Chungnam National University Hospital. All patients underwent the following initial staging procedures: clinical examination; routine blood tests; chest radiography; chest CT (including liver and adrenal glands); whole-body bone scan; and limited brain MRI. The limited brain MRI was modified from conventional MRI by omitting T2-weighted axial, proton density axial, and contrast- enhanced T1-weighted images (Table 1) to decrease the cost from US$ 480 to US$ 180 without any decrease in sensitivity (18). As a control group, we used 131 patients who were newly diagnosed with NSCLC between May, 2000 and April, 2001. Control patients underwent the initial staging procedures described above, except that a brain MRI was carried out only in cases that exhibited neurologic symptoms related to BM (e.g. headaches, seizures, or unexplained weakness) at the time of initial diagnosis. The incidence of BM in the initial staging of patients with primary NSCLC and the incidence of metastases to other systemic sites were compared. We compared the clinically relevant characteristics of both groups (age, sex, cell type, performance status, clinical stage, and incidence of brain metastasis). Patients were followed up until the 30th of April, 2003 (i.e., a minimum period of one year) and we analyzed the clinical significance of early detection of BM and the relationships among the various prognostic factors. The statistical analysis was done using SPSS (version 11.0). Differences between the two groups were evaluated for statistical significance using a chi-squared test. Survival data were calculated using the Kaplan-Meier method and statistical differences were confirmed by means of the log-rank test.
Table 1.
Differences between conventional and limited brain magnetic resonance imaging (MRI)
WI, weighted image; CE, contrast-enhanced.
RESULTS
There were no statistically significant differences between the groups with respect to gender, age, performance status, tumor subtype, or clinical stage (excluding brain metastasis) (Table 2).
Table 2.
Patients' characteristics
Sq, squamous cell carcinoma; Ad, adenocarcinomas; La, large cell carcinoma; Un, undifferentiated; NS, not significant.
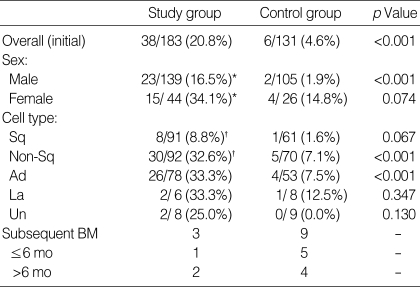
BM was detected in 38 of 183 (20.8%) and 6 of 131 (4.6%) patients in the study and control groups, respectively (p<0.001). Twenty-three of 139 (16.5%) males and 15 of 44 (34.1%) females had BM. Patients with non-squamous-type cells (32.6%) had a higher frequency of BM than those with squamous-type cells (8.8%). During the follow-up period, subsequent BM developed in 3 of study group, and 9 of control group. In these patients, 1 of study group and 5 of control group had synchronous BM (within 6 months after initial diagnosis) (Table 3).
Table 3.
Incidence of brain metastasis according to the patients' characteristics
Sq, squamous cell carcinoma; Ad, adenocarcinomas; La, large cell carcinoma; Un, undifferentiated. *male vs. female: p=0.0124, †squamous vs. nonsquamous: p<0.0001. BM; brain metastasis.
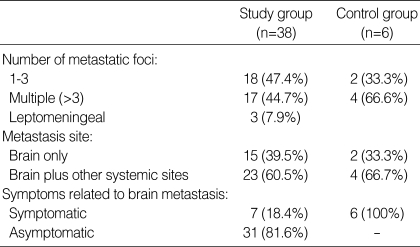
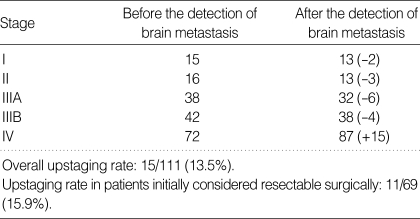
Eighteen patients (47.4%) had a single focus of metastasis within the brain, 17 patients (44.7%) had multiple intracranial foci, and 3 patients (7.9%) had a leptomeningeal pattern of metastasis (Table 4). Only 7 of 38 patients (18.4%) in which BM was observed using limited MRI also exhibited clinical symptoms related to BM (Table 4). In 15 of 38 patients (39.5%) in which BM was observed using limited MRI, the brain was the only site of systemic metastasis, and these 15 patients were upstaged to stage IV based solely on the diagnosis of BM. This number included 11 of 68 patients (15.9%) that were considered initially to be resectable surgically in the absence of BM. Two stage I, three stage II, six stage IIIA, and four stage IIIB patients were upstaged to stage IV (Table 5).
Table 4.
Characteristics of brain metastasis
Table 5.
Impact of limited brain MRI screening on stage determination
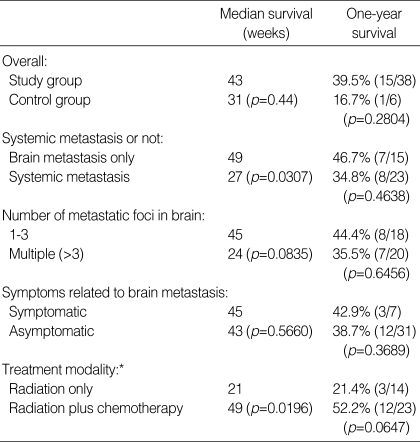
For the survival analysis, 10 of 183 patients in the study group were excluded due to insufficient follow-up data. The survival analysis was carried out on 173 patients. The overall median survival time and one-year survival rate of patients with BM were 43 weeks and 39.5% and 31 weeks and 16.7% for the study and control groups, respectively. The number of patients in the control group was too small to determine whether there were any statistically significant differences between the two groups. The one-year survival rate and median survival time of patients who had BM (46.7% and 49 weeks, respectively) was greater only than patients who had multiple systemic metastases that included the brain (34.8% and 27 weeks, respectively). Eighteen patients had between one and three metastatic nodules in the brain that could be accessed for stereotactic radiosurgery and 20 patients (including three with leptomeningeal involvement) had multiple (>3 nodules) foci within the brain. The one-year survival rate and median survival time for the former and latter type of patient was 44.4% and 45 weeks and 35.0% and 24 weeks, respectively. Of the 38 patients who had BM and were strongly recommended to receive radiation therapy to the brain with systemic chemotherapy, 14 were treated with whole brain irradiation only and 23 were treated with both radiation and chemotherapy. One patient refused any further treatment. The one-year survival rate and median survival time of irradiation- treated patients was 21.4% and 21 weeks, respectively, and the one-year survival rate and median survival time of those treated with both radiation and chemotherapy was 52.2% and 49 weeks, respectively. The one-year survival rate and median survival time for symptomatic vs. asymptomatic patients was 42.9% and 45 weeks and 38.7% and 43 weeks, respectively (Table 6).
Table 6.
Median survival period and one-year survival rate of patients with brain metastasis detected by limited brain MRI screening
*No treatment: 1 case.
The one-year survival rate and median survival time overall for stage IV patients were 36.1% and 37 weeks, respectively. The median survival of 12 patients in whom BM was diagnosed during the follow-up treatment period was 8 weeks.
DISCUSSION
Even though locoregional control rates of 50% and higher have been achieved after neoadjuvant chemoradiotherapy and definitive resection (multimodal therapy) in patients with locally advanced NSCLC, the brain is the most frequent site of initial treatment failure and is the site of approximately one third of all relapses that occur (11, 13, 19, 20). Therefore, treatment strategies that reduce the risk of BM are needed to optimize the efficacy of multimodal therapy and to improve survival.
Between 25 and 30% of all patients with lung cancer develop BM at some stage, and this incidence is likely to increase if survival is prolonged by means of aggressive multi-modal treatment. The increasing frequency of treatment failure, the development of new imaging techniques and treatments, as well as the reports of prolonged survival of patients that have received aggressive treatment, suggest that approaches to treating patients who have BM should be reassessed. Specifically, novel treatment paradigms should be developed to ensure that such patients receive optimal therapeutic intervention. To this end, prophylactic cranial irradiation in NSCLC and SCLC patients has been introduced and has led to several reports of positive outcomes, although a large-scale study is needed to confirm this (11, 13, 21). An alternative means to the same end is the introduction of brain imaging when the initial workup is carried out. This approach would facilitate the early detection of BM and promote the timely application of appropriate treatments, which would improve the survival rates of cancer patients. However, such early imaging should be considered only if it is practicable and available at a reasonable cost. Considering each of the aforementioned factors, we designed the present study to assess the clinical effectiveness of using limited brain imaging at the time of initial screening of lung cancer patients.
The rate of BM in patients with locally advanced NSCLC has been estimated previously to be between 17 and 32% (median: 22%) with a median time-to-brain recurrence of 7.5-9.3 months (8, 11, 13). It has been shown previously that most recurrences of metastases within the central nervous system occur within 2 yr of the initial diagnosis (13). Furthermore, BM is a direct cause of death in between one third and one half of affected patients (12).
The incidence of BM in the initial screening of patients with primary lung cancer has been reported to be between 12 and 18% (22, 23). In the present study, the incidence was 18.9%. We suspect that this slightly higher incidence was the result of using the limited brain MRI procedure, which is more sensitive than brain CT (5, 17). There are several risk factors that are related to BM, including non-squamous histological characteristics (particularly adenocarcinomas), bulky lymph nodes in the mediastinum, younger age, stage IIIB, etc. (5, 6, 11-13, 24, 25). Our data supported the same trend and, in addition, suggested that the incidence of such risk factors is greater in females than in males. Specifically, in the present study, the incidence of BM and non-squamous tumors in females was 30.6 and 26.2%, respectively, which was statistically higher than in males (15.5 and 8.8%, respectively). The incidence of BM in all patients with adenocarcinomas was 33.3%, whereas the incidence in females with adenocarcinomas was 50%. In clinical stage IV patients, the brain was the second most common site of metastasis (38/87 patients or 43.7%), following bone (39/87, 44.8%), and was a more common site of metastasis than lung, liver, and the adrenal glands.
Most patients with BM were asymptomatic, even those with multiple foci. Symptomatic metastasis was observed in only 7 of 38 patients (18.4%). Although neurological symptoms have been reported to be associated with a poor prognosis (7, 8, 14), the survival rates in the present study were unrelated to the presence of clinical symptoms. We found that patients who had a single focus of BM, and isolated BM, and who were treated with chemotherapy had better survival, as reported by others. The survival rate of patients who had BM was equivalent to those who did not have any clinical symptoms of BM; this was due to early treatment using whole brain radiotherapy, stereotactic radiosurgery, and chemotherapy. Fujita et al. reported that the use of chemotherapy to control not only BM but also extracranial lesions prolonged the survival of patients with BM due to NSCLC (26). In the present study, the survival rates of patients who had BM and who received both chemotherapy and radiotherapy were similar to those of patients in stage IIIB (data not shown), which would appear to support our hypothesis that early detection of BM and subsequent application of appropriate treatment may improve overall survival.
In the present study, 15 patients (15/111, 13.5%) were upstaged from clinical stage I (n=2), II (n=3), IIIA (n=6), or IIIB (n=4) to stage IV, because of the presence of BM, including 11 patients (11/68, 15.9%) who had been considered initially to be suitable for surgical resection in the absence of evidence for the presence of BM. All of the aforementioned patients were treated with either radiotherapy alone (n=7) or both radiotherapy and chemotherapy (n=8). The median survival time and one-year survival rate of the former and latter patients was 43 weeks and 28.6% and 72 weeks and 66.7%, respectively. That was greater than the survival rate of all patients with BM (median survival time and one-year survival rate for radiotherapy only and radiotherapy plus chemotherapy for all patients with BM were 21 weeks and 21.4%, and 49 weeks and 52.2%, respectively) (Table 6). During a follow up period of at least one year, 12 patients (3 of study group and 5 of control group) subsequently developed BM. All of these patients (except one) were treated with chemotherapy after the diagnosis of BM. Initially, these patients responded to chemotherapy such that four exhibited partial responses, five exhibited a stable disease state, and three exhibited progression of the disease. The median time to relapse in treated patients (n=11) was 38 weeks, which is similar to the time reported by Ceresoli et al. (9 months) (13). These 11 patients were treated with radiation only without any further chemotherapy; their median survival time after the diagnosis of BM was 8 weeks, which was shorter than that of patients in whom metastasis was detected during the initial screening and who were treated with radiation therapy alone (21 weeks). Their overall median survival time and one-year survival rate (after the diagnosis of lung cancer) was 38 weeks and 27.3%, respectively, worse than the study group that had BM at the time of the initial screening (43 weeks and 39.5%) and worse than patients who received whole-brain radiation and chemotherapy (49 weeks and 52.2%) following the initial screening. Nevertheless, these outcomes were slightly better than those of the control patients, who were diagnosed and treated for brain metastasis only upon the development of symptoms (31 weeks and 16.7%).
In conclusion, limited brain MRI appears to be a useful and cost-effective means by which to detect BM at the time of initial staging of lung cancer patients. Such early detection of BM enabled patients to be treated immediately with radiotherapy and chemotherapy and led to improved rates of survival. Consequently, we recommend that limited brain MRI should be used as an initial screening procedure for the early detection of BM. This will allow lung cancer patients to receive the appropriate treatment in a timely manner, which should improve both the survival and quality of life of such patients.
References
- 1.Minna J. Neoplams of the lung. In: Braunbald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's principles of internal medicine. 15th ed. New York: McGraw-Hill, Inc; 2001. pp. 562–571. [Google Scholar]
- 2.Sorensen JB, Hansen HH, Hansen M, Dombernowsky P. Brain metastases in adenocarcinoma of the lung: frequency, risk groups, and prognosis. J Clin Oncol. 1988;6:1474–1480. doi: 10.1200/JCO.1988.6.9.1474. [DOI] [PubMed] [Google Scholar]
- 3.Zabel A, Milker-Zabel S, Thilmann C, Zuna I, Rhein B, Wannenmacher M, Debus J. Treatment of brain metastases in patients with non-small cell lung cancer (NSCLC) by stereotactic linac-based radiosurgery: prognostic factors. Lung Cancer. 2002;37:87–94. doi: 10.1016/s0169-5002(02)00030-2. [DOI] [PubMed] [Google Scholar]
- 4.Vines EF, Le Pechoux C, Arriagada R. Prophylactic cranial irradiation in small cell lung cancer. Semin Oncol. 2003;30:38–46. doi: 10.1053/sonc.2003.50013. [DOI] [PubMed] [Google Scholar]
- 5.Yokoi K, Kamiya N, Matsuguma H, Machida S, Hirose T, Mori K, Tominaga K. Detection of brain metastasis in potentially operable non-small cell lung cancer. A comparison of CT and MRI. Chest. 1999;115:714–719. doi: 10.1378/chest.115.3.714. [DOI] [PubMed] [Google Scholar]
- 6.Hochstenbaga MM, Twijnstra A, Hofman P, Wouters EF, ten Velde GP. MR-imaging of the brain of neurologic asymptomatic patients with large cell or adenocarcinoma of the lung. Does it influence prognosis and treatment? Lung Cancer. 2003;42:189–193. doi: 10.1016/s0169-5002(03)00291-5. [DOI] [PubMed] [Google Scholar]
- 7.Virgo KS, McKirgan LW, Caputo MC, Mahurin DM, Chao LC, Caputo NA, Naunheim KS, Flye MW, Gillespie KN, Johnson FE. Post-treatment management options for patients with lung cancer. Ann Surg. 1995;222:700–710. doi: 10.1097/00000658-199512000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yokoi K, Miyazawa N, Arai T. Brain metastasis in resected lung cancer: value of intensive follow-up with computed tomography. Ann Thorac Surg. 1996;61:546–551. doi: 10.1016/0003-4975(95)01096-3. [DOI] [PubMed] [Google Scholar]
- 9.Cole FH, Jr, Thomas JE, Wilcox AB, Halford HH., 3rd Cerebral imaging in the asymptomatic preoperative bronchogenic carcinoma patient: is it worthwhile? Ann Thorac Surg. 1994;57:838–840. doi: 10.1016/0003-4975(94)90185-6. [DOI] [PubMed] [Google Scholar]
- 10.Silvestri GA, Littenberg B, Colice GL. The clinical evaluation for detecting metastatic lung cancer. A meta-analysis. Am J Respir Crit Care Med. 1995;152:225–230. doi: 10.1164/ajrccm.152.1.7599828. [DOI] [PubMed] [Google Scholar]
- 11.Andre F, Grunenwald D, Pujol JL, Girard P, Dujon A, Brouchet L, Brichon PY, Westeel V, Le Chevalier T. Patterns of relapse of N2 non-small cell lung cancer patients treated with preoperative chemotherapy. Should prophylactic cranial irradiation be reconsidered? Cancer. 2001;91:2394–2400. [PubMed] [Google Scholar]
- 12.Gasper L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R. Recursive partitioning analysis (RPA) of prognostic factors in three radiation therapy oncology group (RTOG) brain metastatses trials. Int J Radiat Oncol Biol Phys. 1997;37:745–751. doi: 10.1016/s0360-3016(96)00619-0. [DOI] [PubMed] [Google Scholar]
- 13.Ceresoli GL, Reni M, Chiesa G, Carretta A, Schipani S, Passoni P, Bolognesi A, Zannini P, Villa E. Brain metastases in locally advanced nonsmall cell lung carcinoma after multimodality treatment; risk factors analysis. Cancer. 2002;95:605–612. doi: 10.1002/cncr.10687. [DOI] [PubMed] [Google Scholar]
- 14.Walsh GL, O'Connor M, Willis KM, Milas M, Wong RS, Nesbitt JC, Putnam JB, Jr, Lee JJ, Roth JA. Is follow-up of lung cancer patients after resection medically indicated and cost-effective? Ann Thorac Surg. 1995;60:1563–1572. doi: 10.1016/0003-4975(95)00893-4. [DOI] [PubMed] [Google Scholar]
- 15.Sze G, Milano E, Johnson C, Heier L. Detecton of brain metastases: comparison of contrast-enhanced MR with unenhanced MR and enhanced CT. Am J Neuroradiol. 1990;11:785–791. [PMC free article] [PubMed] [Google Scholar]
- 16.Davis PC, Hudgins PA, Peterman SB, Hoffman JC., Jr Diagnosis of cerebral metastases: Double-dose delayed CT vs contrast-enhanced MR imaging. Am J Neuroradiol. 1991;12:293–300. [PMC free article] [PubMed] [Google Scholar]
- 17.Haberkorn U, Schoenberg SO. Imaging of lung cancer with CT, MRI and PET. Lung Cancer. 2001;34(Suppl 3):13–23. doi: 10.1016/s0169-5002(01)00369-5. [DOI] [PubMed] [Google Scholar]
- 18.Kwon SJ, Lee YS, Ahn JY, Jung SS, Kim JO, Kim SY. Detection of brain metastases using limited brain magnetic resonance imaging. Tuberculosis and Respiratory Diseases. 2003;55:499–505. [Google Scholar]
- 19.Choi NC, Carey RW, Daly W, Mathisen D, Wain J, Wright C, Lynch T, Grossbard M, Grillo H. Potential impact on survival of improved tumor downstaging and resection rate by preoperative twice-daily radiation and concurrent chemotherapy in stage IIIA non-small cell lung cancer. J Clin Oncol. 1997;15:712–722. doi: 10.1200/JCO.1997.15.2.712. [DOI] [PubMed] [Google Scholar]
- 20.Eberhardt W, Wilke H, Stamatis G, Stuschke M, Harstrick A, Menker H, Krause B, Mueller MR, Stahl M, Flasshove M, Budach V, Greschuchna D, Konietzko N, Sack H, Seeber S. Preoperative chemotherapy followed by concurrent chemoradiation therapy based on hyperfractionated accelerated radiotherapy and definitive surgery in locally advanced non-small cell lung cancer: Mature results of phase II trial. J Clin Oncol. 1998;16:622–634. doi: 10.1200/JCO.1998.16.2.622. [DOI] [PubMed] [Google Scholar]
- 21.Stuschke M, Eberhardt W, Pottgen C, Stamatis G, Wilke H, Stuben G, Stoblen F, Wilhelm HH, Menker H, Teschler H, Muller RD, Budach V, Seeber S, Sack H. Prophylactic cranial irradiation in locally advanced non-small cell lung cancer after multimodality treatment: long-term follow-up and investigations of late neuropsychologic effects. J Clin Oncol. 1999;17:2700–2709. doi: 10.1200/JCO.1999.17.9.2700. [DOI] [PubMed] [Google Scholar]
- 22.Mintz BJ, Tuhrim S, Alexander S, Alexander S, Yang WC, Shanzer S. Intracranial metastases in the initial staging of bronchogenic carcinoma. Chest. 1984;86:850–853. doi: 10.1378/chest.86.6.850. [DOI] [PubMed] [Google Scholar]
- 23.Hooper RG, Tenholder MF, Underwood GH, Beechler CR, Spratling L. Computed tomographic scanning of the brain in initial staging of bronchogenic carcinoma. Chest. 1984;85:774–776. doi: 10.1378/chest.85.6.774. [DOI] [PubMed] [Google Scholar]
- 24.Gregor A. Prevention and management of brain metastases. Lung Cancer. 2003;41(Suppl 3):42. [Google Scholar]
- 25.Robnett TJ, Machtay M, Stevenson JP, Algazy KM, Hanh SM. Factors affecting the risk of brain metastases after definitive chemoradiation for locally advanced non-small cell lung cancer. J Clin Oncol. 2001;19:1344–1349. doi: 10.1200/JCO.2001.19.5.1344. [DOI] [PubMed] [Google Scholar]
- 26.Fujita A, Fukuoka S, Takabatake H, Tagaki S, Sekine K. Combination chemotherapy of cisplatin, ifosfamide, and irinotecan with rhG-CSF support in patients with brain metastases from non-small cell lung cancer. Oncology. 2000;59:291–295. doi: 10.1159/000012185. [DOI] [PubMed] [Google Scholar]