Abstract
Though the pathogenic significance and the reservoir of Ewingella americana have not been clarified, this organism has caused several pathogenic infections, especially in immunocompromised patients. We report a pneumonia in a patient with chronic renal failure, who had chronic rejection of transplanted kidney. E. americana was identified to be the pathogen of pneumonia with clinical symptoms and signs and radiological examination. As soon as he was treated with ceftriaxone and isepamicin, clinical improvement was followed with no further growth of E. americana or other pathogenic isolates from sputum culture. This suggests to be the case of pneumonia caused by E. americana for the first time in the Korean literature.
Keywords: Ewingella americana; Kidney Failure, Chronic; Sputum; Pneumonia; Cefatriaxone; Isepamicin
INTRODUCTION
Ewingella americana is the only species of the genus of Ewingella in the family Enterobacteriaceae, first described from clinical specimens in 1983 (1). The pathogenic significance and niches of the reservoir have not been clarified. This organism rarely causes human infections and has been identified from various clinical specimens including wound, sputum, urine, stool, blood (1, 2), conjunctiva (3) and peritoneal dialysate (4). We present a chronic renal failure patient with fever and haziness in right lung field on chest radiography. Since the blood and urine cultures showed no other bacterial growth, pneumonia caused by E. americana suspected to be the origin of fever. Ceftriaxone and isepamicin (Yoohan, Seoul, Korea) were administered and the clinical and radiological findings were improved. As far as we know, this is the first report of a pneumonia caused by E. americana.
CASE REPORT
35-yr-old male who had undergone renal transplantation was admitted to the University Hospital of Keimyung for chronic rejection of the transplanted kidney on 1 May 2003. He had chronic renal failure for 7 yr. On the day of admission, peritoneal dialysis was initiated. After three days, he developed fever with right pleuritic chest pain. Physical examination revealed 38.2℃ of fever and pale conjunctiva with pitting edema on both legs. Blood, urine and sputum samples were obtained for culture. Laboratory findings were as follows: white blood cells 9,770/µL (neutrophils 91%), hemoglobin 8.2 g/dL, hematocrit 24.3%, platelets 133,000/µL, blood urea nitrogen 74 mg/dL, creatinine 7.3 mg/dL, fibrinogen/fibrin degradation product (FDP) positive, fibrinogen 617 mg/dL (reference range 200-400 mg/dL). The simple chest radiography was performed and revealed haziness in right upper and middle lung field.
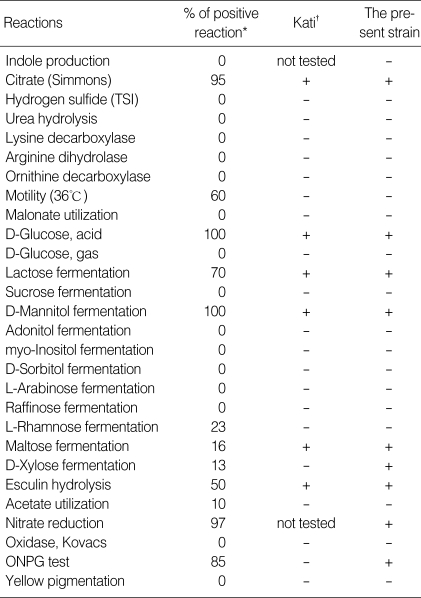
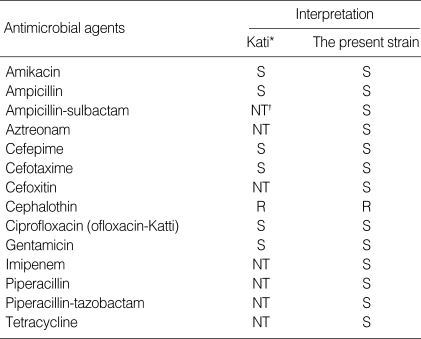
He was empirically treated with ceftriaxone starting from the very next day before the results of culture. Two days later, isepamicin was added to the treatment regimen because of persistent fever. Blood and urine culture did not show the growth of any bacteria after 5 and 2 days, respectively. Gram stain of sputum showed group 5 according to Washington-Murray Grading as determining the quality of specimen (5). Sputum culture revealed moderate growth of two-type colonies, which were alpha-hemolytic streptococci and large grayish colonies suspecting Gram-negative bacilli, on blood agar plate after overnight incubation at 36℃. Lactose fermenting Gram-negative bacilli were moderately grown on MacConkey agar plate. Triple sugar iron agar showed A/K reaction for this strain. The biochemical characteristics identified by the VITEK GNI+ card (bioMerieux Vitek, Inc., Hazelwood, MO, U.S.A.) are listed in Table 1. The antimicrobial susceptibility test carried out by disk diffusion method showed susceptibilities against amikacin, ampicillin, ampicillin-sulbactam, aztreonam, cefepime, cefoperazone-sulbactam, cefotaxime, cefoxitin, ceftazidime, ciprofloxacin, gentamicin, imipenem, piperacillin, piperacillin-tazobactam, and tetracycline, but only resistant to cephalothin (Table 2).
Table 1.
Biochemical characteristics of E. americana strains
Table 2.
Antimicrobial susceptibility results of E. americana
*Results from Kati et al. (4), †NT, not tested.
On 12 May 2003, subsequent sputum culture failed to grow either E. americana or any pathogenic bacteria. Chest radiography findings were improved as the clinical signs and symptoms disappeared. Ceftriaxone and isepamicin were administered for an additional week. And he was discharged with peroral medication of the antibiotics after the 15th day of admission.
DISCUSSION
Clinical infections due to E. americana, a rare Gram-negative bacilli with low pathogenic potential, have usually been involved in immunocompromised patients and caused peritonitis (4) and bacteremia (6, 7). Colonization in sputum (1), wound (8), and pseudobacteremia (9, 10) were reported in patients without clinical infections and in previously healthy patients. Sputum was reported to be the most common source of isolation (1, 2). Grimont reported that pneumonia or influenza has been developed only in 2 cases out of 5 strains (1), and Farmer et al. listed 14 sputum isolates without clinical reviews (2). Therefore, the clinical significance of the isolate has not been clear due to no further case studies. Bacteremia was the most common infections of E. americana (6, 7, 11, 12). Very recently, Tsokos reported a patient who died of Waterhouse-Friderichen syndrome had growth of E. americana in heart and spleen blood samples of postmortem bacteriologic cultures and stated that the pathogenic potentiality of this strain (13).
Though several cases were published in the literature, little is known about the natural habitat of organism. However, McNeil proposed that the citrate solutions prepared in the hospital for coagulations study may have constituted an inanimated environmental reservoir and resulted in recurrent pseudobacteremia caused by E. americana (10). Also, the sources of infection considered to be the domestic water in peritonitis of a patient undergone peritoneal dialysis (4) and the contamination of ice bath as a probable cause of bacteremia (12). On the other hand, Maertens et al. speculated on the contamination of catheter or inadequate hand hygiene as the source of infection (11). E. americana can survive in water and grow preferentially at 4℃ (10) and this isolate is not known to be the normal flora of respiratory tract. Since this study did not include evaluations dealing with water or other environmental sources throughout the admission, we could only presumed that the general hygiene or water contamination might have played a role in this infection.
According to the overall considerations of symptoms and signs, laboratory findings and the clinical course following antibiotics administration, we conclude that E. americana isolated in sputum could be the pathogen of pneumonia in this patient. Therefore we present the first case, to our knowledge, of E. americana pneumonia in a chronic renal failure patient. We have neither identified E. americana before in our laboratory nor isolated since then from the specimens of other patients. Regarding to the host and pathogenic potentiality, E. americana could become a rare but opportunistic pathogen of clinical infections, especially in a immunocompromised person. Even the etiology and route of infection have not been clearly stated, this organism, E. americana, has finally resulted in pneumonia and treated well with immediate usage of antibiotics in this patient. However, more cases and informations are needed to clarify and postulate the ecology and pathogenicity of E. americana in the hospital settings.
References
- 1.Grimont PA, Farmer JJ, 3rd, Grimont F, Asbury MA, Brenner DJ, Deval C. Ewingella americana gen. nov., sp. nov., a new Enterobacteriaceae isolated from clinical specimens. Ann Microbiol (Paris) 1983;134:39–52. doi: 10.1016/0769-2609(83)90102-3. [DOI] [PubMed] [Google Scholar]
- 2.Farmer JJ, 3rd, Davis BR, Hickman-Brenner FW, McWhorter A, Huntley-Carter GP, Asbury MA, Riddle C, Wathen-Grady HG, Elias C, Fanning GR, Steigerwalt AG, O'Hara CM, Morris GK, Smith PB, Brenner DJ. Biochemical identification of new species and biogroups of Enterobacteriaceae isolated from clinical specimens. J Clin Microbiol. 1985;21:46–76. doi: 10.1128/jcm.21.1.46-76.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heizmann WR, Michel R. Isolation of Ewingella americana from a patient with conjunctivitis. Eur J Clin Microbiol Infect Dis. 1991;10:957–959. doi: 10.1007/BF02005452. [DOI] [PubMed] [Google Scholar]
- 4.Kati C, Bibashi E, Kokolina E, Sofianou D. Case of peritonitis caused by Ewingella americana in a patient undergoing continuous ambulatory peritoneal dialysis. J Clin Microbiol. 1999;37:3733–3734. doi: 10.1128/jcm.37.11.3733-3734.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray PR, Washington JA. Microscopic and bacteriologic analysis of expectorated sputum. Mayo Clin Proc. 1975;50:339–344. [PubMed] [Google Scholar]
- 6.Devreese K, Claeys G, Verschraegen G. Septicemia with Ewingella americana. J Clin Microbiol. 1992;30:2746–2747. doi: 10.1128/jcm.30.10.2746-2747.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pien FD, Farmer JJ, 3rd, Weaver RE. Polymicrobial bacteremia caused by Ewingella americana (family Enterobacteriaceae) and an unusual Pseudomonas species. J Clin Microbiol. 1983;18:727–729. doi: 10.1128/jcm.18.3.727-729.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bear N, Klugman KP, Tobiansky L, Koornhof HJ. Wound colonization by Ewingella americana. J Clin Microbiol. 1986;23:650–651. doi: 10.1128/jcm.23.3.650-651.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNeil MM, Davis BJ, Anderson RL, Martone WJ, Solomon SL. Mechanism of cross-contamination of blood culture bottles in outbreaks of pseudobacteremia associated with nonsterile blood collection tubes. J Clin Microbiol. 1985;22:23–25. doi: 10.1128/jcm.22.1.23-25.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McNeil MM, Davis BJ, Solomon SL, Anderson RL, Shulman ST, Gardner S, Kabat K, Martone WJ. Ewingella americana: recurrent pseudobacteremia from a persistent environmental reservoir. J Clin Microbiol. 1987;25:498–500. doi: 10.1128/jcm.25.3.498-500.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maertens J, Delforge M, Vandenberghe P, Boogaerts M, Verhaegen J. Catheter-related bacteremia due to Ewingella americana. Clin Microbiol Infect. 2001;7:103–104. doi: 10.1046/j.1469-0691.2001.00195.x. [DOI] [PubMed] [Google Scholar]
- 12.Pien FD, Bruce AE. Nosocomial Ewingella americana bacteremia in an intensive care unit. Arch Intern Med. 1986;146:111–112. [PubMed] [Google Scholar]
- 13.Tsokos M. Fatal Waterhouse-Friderichsen syndrome due to Ewingella americana infection. Am J Forensic Med Pathol. 2003;24:41–44. doi: 10.1097/01.PAF.0000051704.91568.A6. [DOI] [PubMed] [Google Scholar]