Abstract
We compared the clinical efficacy of a short-term intervention of 308-nm excimer laser with that of narrow-band UVB (NBUVB) phototherapy for vitiligo patients to see the early response. Twenty-three symmetrically patterned patches of vitiligo on 8 patients were selected. Vitiligo patches on one side of the body were treated 2 times per week for a maximum of 20 treatments with the excimer laser, and NBUVB phototherapy was used on patches on the other side. Improvement (repigmentation) was assessed on a visual scale via serial photographs taken every five treatments and scored as follows: 0, ≤1% improvement; 1, ≤25% improvement; 2, 26-50% improvement; 3, 51-75% improvement; and 4, ≥75% improvement. At five treatments, the excimer laser-treated patches had an average score of 0.26, compared with 0.04 for patches treated with NBUVB phototherapy. A slightly higher repigmentation (p>0.05) in the excimer treated area was thus observed. At 10, 15, or 20 treatments, the differences between the average scores were significant: 0.83, 1.17, and 1.39 for the excimer-treated patches, and 0.17, 0.30, and 0.74 for the NBUVB phototherapy-treated areas (p<0.05). In conclusion, the 308-nm excimer laser appears to be more effective than NBUVB phototherapy, as it produces more rapid and profound repigmentation.
Keywords: Vitiligo; 308-nm Excimer Laser; Laser Therapy, Low-Level; Narrow Band UVB; Phototherapy; Ultraviolet Therapy
INTRODUCTION
Vitiligo is a common idiopathic, acquired depigmentation disorder caused by the selective destruction of melanocytes. It affects 1-2% of the population with no predilection for age, sex, or racial background. The disease is characterized by circumscribed white spots on the skin that tend to enlarge centrifugally over time or, less frequently, to recover spontaneously (1).
Traditional therapies include topical or systemic corticosteroids, PUVA (topical or oral psoralen followed by UVA irradiation), and narrow-band 311-nm UVB (NBUVB) phototherapy (2). NBUVB is now used frequently with satisfactory results, although lesions in hard-to-reach areas like skin folds often do not receive adequate exposure. Additionally, the ability to deliver high doses is often limited by phototoxicity to both lesional and nonlesional skin.
The 308-nm excimer laser emits wavelengths adjacent to those of NBUVB and is presumed to have similar biological and clinical effects. This laser has been found to be effective in the treatment of localized psoriasis, where it may offer advantages over NBUVB by sparing normal adjacent skin (3). By allowing effective and selective targeting, this device also reduces cumulative cutaneous UV burdens and reduces the total number of treatments needed for clearing psoriasis. Spencer et al. (4) recently reported that the 308-nm excimer laser may also represent a new therapeutic option for the management of vitiligo, resulting in repigmentation of vitiligo patches in less time than that required with current modalities.
Previous studies have expounded on the safety and efficacy of treatment with the 308 nm excimer laser, possibly even more so than NBUVB phototherapy. However, these reports involved comparisons of groups of patients, not direct comparisons within the same patient. The present study demonstrates the greater efficacy of the 308-nm excimer laser treatment over NBUVB phototherapy through comparisons of the treatment effects on comparable patches within the same patient.
MATERIALS AND METHODS
Study population
Patients with generalized vitiligo (acrofacial or vulgaris type) were included in this study and were assessed for Fitzpatrick skin phototypes, overall disease duration, and history of previous therapy. Exclusion criteria included a history of photosensitive disorder, skin cancer, and psychological disorders. Eight patients (3 males, 5 females) were selected, and all gave informed consent. Patient ages ranged from 29 to 58 yr (mean, 41.3 yr). Lesions on the genitalia or in the gluteal crease were not treated. The treatment of subjects who had undergone previous treatment was started after a wash-out period of 2 weeks for topical steroids, 4 weeks for any form of phototherapy, and 8 weeks for PUVA or immunomodulating agents.
Selection of treatment sites
Twenty-three pairs of vitiligo patches which were symmetrically distributed on the 8 patients were selected for testing. Vitiligo patches on the left side of the body were treated with the 308-nm excimer laser, and patches on the right side were treated with NBUVB phototherapy.
Light source
We used a 308-nm excimer laser with a self-contained gas system of Xe-Cl (Photomedex®, Carlsbad, CA, U.S.A.). Output is initiated by a foot switch and consists of a train of short pulses with a pulse-width of 30 nanoseconds, delivered through a fiber optic hand piece. It is operated at 3 mJ per pulse with pulse repetition of up to 200 Hz. The laser allows fixed fluences to be delivered, from 100 mJ/cm2 to a maximum dose of 2,100 mJ/cm2, in 50 mJ/cm2 increments. Additional fluences can be delivered by pressing the foot switch. The NBUVB phototherapy unit (Waldmann Co., Germany) contains a bank of 48 fluorescent tubes (TL-100W/01, Phillips, Eindhoven, The Netherlands) with peak emission at 311 to 312 nm.
Interventions
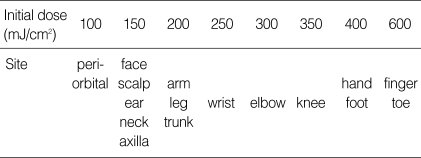
Therapy was administered twice per week on non-consecutive days, for a maximum of 20 treatments. In each session, vitiligo patches on the left side were first with the 308-nm excimer laser. The fluence administered was based on the Friedman XTRAC-excimer protocol for the treatment of vitiligo, in which the initial dose is determined by the site of the lesion (Table 1), and the subsequent dose is determined as follows: 100 mJ/cm2 increment if there is no erythema after the initial treatment, 50 mJ/cm2 increment if there is erythema lasting for less than 24 hr, and no increment if there is erythema lasting for 24 hr or more. If symptomatic erythema (burning, pain) or blistering developed, treatment was withheld until resolution, and then the dose was decreased by 50 mJ/cm2.
Table 1.
Friedman's protocol for the treatment of vitiligo showing the initial dose according to the site of the lesion
After each laser treatment, vitiligo patches on the right side were treated with NBUVB phototherapy. Patches on the left side of the body were shielded with gauze prior to treatment, to avoid NBUVB exposure. The initial irradiation dose for each patient was 250 mJ/cm2, and the dose was increased by 15% for each subsequent treatment. If the patient reported mild erythema or pruritus, the irradiation dose was held constant for the subsequent treatment, or until resolution of symptoms. If symptomatic erythema or blistering developed, the dose was decreased by 15%.
Evaluation
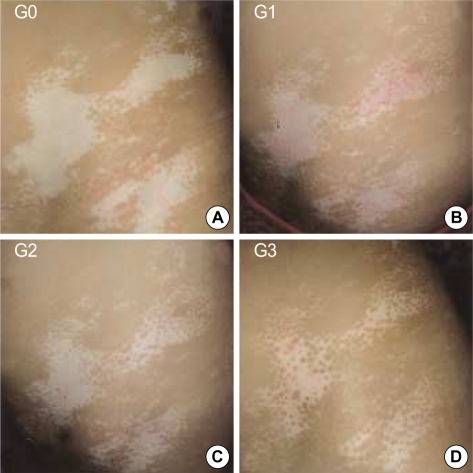
Selected patches of vitiligo were photographed using standardized 35-mm color film before the first treatment, then at five-treatment intervals until the completion of the study. Improvement (repigmentation) relative to baseline was measured quantitatively on a visual scale by two independent investigators and graded as follows: grade 0, ≤1% improvement; grade 1, ≤25% improvement; grade 2, 26-50% improvement; grade 3, 51-75% improvement; and grade 4, ≥75% improvement.
Statistical analysis
Student's paired t-test was used to evaluate the difference in repigmentation between the excimer-treated and NBUVB phototherapy-treated areas. Statistical significance was defined by a p value of less than 0.05.
RESULTS
Profile of patients
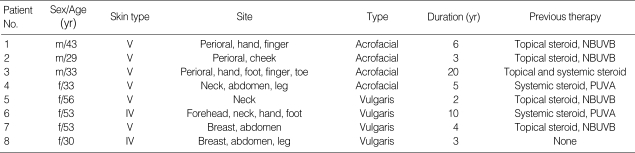
As shown in Table 2, the age range of the 8 patients was 29 to 58 yr, with a mean of 41.3 yr. Two of the eight patients had skin phototype IV, and the rest had skin phototype V. Disease duration ranged from 3 to 20 yr. Based on patient histories, all previous therapies, which included topical and systemic corticosteroids (n=7), PUVA (n=2), and NBUVB (n=4), had failed in 6 of the 7 patients. In the present study, all patients completed 20 treatments. None experienced any adverse effects from the therapy that warranted discontinuation of the treatment.
Table 2.
Profile of patients
Treatment outcome
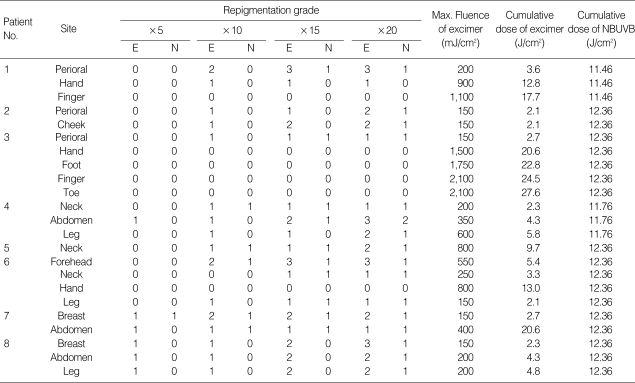
The outcomes are presented in Table 3. In the excimer laser treatment, the mean cumulative doses were 3.96 J/cm2 for treating the face, 6.84 for the trunk, 4.07 for the extremities, 17.3 for the hands/feet, and 23.3 for the digits. In NBUVB phototherapy, the mean cumulative dose was 12.17±0.34 J/cm2.
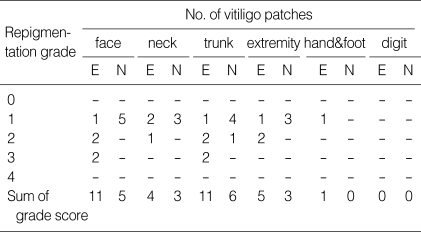
Table 3.
Summary of results: repigmentation grade after X number of treatments
*E, excimer laser; N, NBUVB phototherapy.
In this comparative study, the authors noted that the 308-nm excimer laser produces more rapid and more profound repigmentation, compared with NBUVB phototherapy (Fig. 1-3). In addition, in patients that did not respond to prior treatment with conventional phototherapy including NBUVB, repigmentation appeared (Fig. 4).
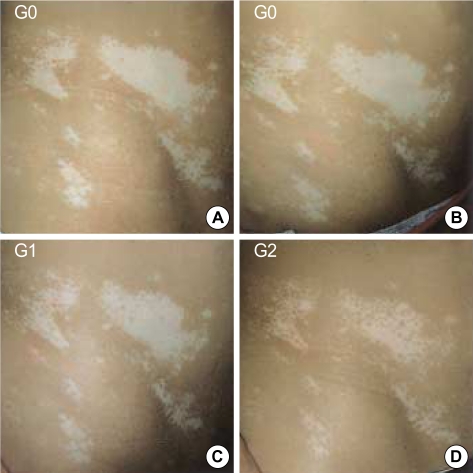
Fig. 1.
Vitiligo patches on the left side of the trunk (A) prior to the 308-nm excimer laser treatment, (B) at 5 treatments, (C) at 15 treatments, and (D) at 20 treatments (G: repigmentation grade).
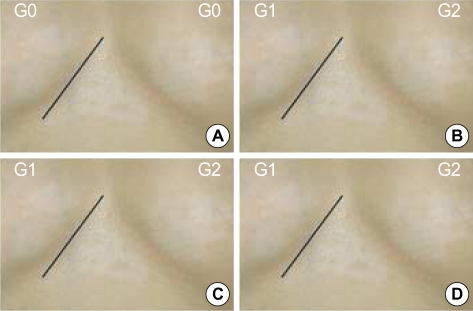
Fig. 3.
Vitiligo patches on the breast region (right side of line: NBUVB phototherapy-treated area, left side of line: excimer laser-treated area) (A) prior to NBUVB phototherapy, (B) at 5 treatments, (C) at 15 treatments, and (D) at 20 treatments (G: repigmentation grade).
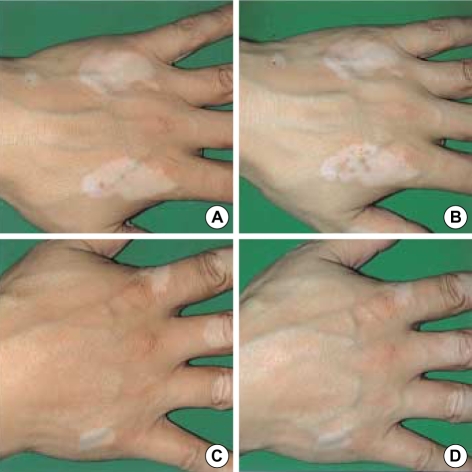
Fig. 4.
Vitiligo patches on the left side of the hand (A) prior to the 308-nm excimer laser treatment and (B) at 20 treatments. Vitiligo patches on the right side of the hand (C) prior to NBUVB phototherapy and (D) at 20 treatments.
At the end of the study period the results were the following. At five treatments, 6/23 (26%) vitiligo patches that received the excimer laser treatment were evaluated as showing grade 1 improvement; for NBUVB phototherapy, 1/23 (4%) patches were classed as grade 1. At ten treatments, 13/23 (57%) patches were grade 1, and 3/23 (13%) patches were grade 2 in the excimer laser-treated areas, while 5/23 (22%) patches showed only grade 1 improvement in NBUVB phototherapy-treated areas. At 15 excimer laser treatments, 9/23 (39%) patches were grade 1, 6/23 (23%) were grade 2, and 2/23 (9%) were grade 3. In NBUVB phototherapy-treated areas, 10/23 patches showed grade 1 improvement. At 20 excimer laser treatments, 6/23 (26%) patches were grade 1, 7/23 (30%) were grade 2, and 4/23 (17%) were grade 3; of the NBUVB phototherapy-treated patches, 15/23 (65%) were grade 1, and 1/23 (4%) were grade 2.
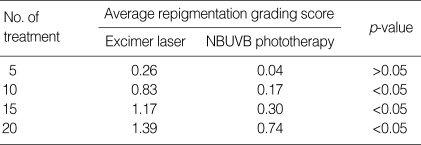
We compared the average repigmentation scores of vitiligo patches that received the excimer laser treatment with those of NBUVB-treated patches at intervals of five treatments. Improvement was seen with both modalities, but, starting after ten treatments, significantly greater improvement was apparent with excimer laser treatment (p<0.05) (Table 4).
Table 4.
Repigmentation with excimer laser treatment or NBUVB phototherapy
The response rates of vitiligo lesions at various sites are given in Table 5. For both treatment methods, the best response was achieved with lesions located on the face and trunk. Lesions located on the neck and extremities also responded with some repigmentation, and one of the lesions located on a hand, foot, or digit showed a response.
Table 5.
Repigmentation by treatment area (after 20 treatments)
*E, excimer laser; N, NBUVB phototherapy.
DISCUSSION
The recent report by Spencer et al. (4) has demonstrated some advantages of targeted phototherapy with the 308-nm excimer laser, namely, the rapidity of onset of repigmentation and the lower number of treatments needed to achieve satisfactory repigmentation, compared with conventional NBUVB. However, the benefits of the excimer laser over conventional NBUVB have not been confirmed by a comparative trial in individual patients.
In this comparative study, with the 308 nm excimer laser, the authors noted an early appearance of repigmentation in the majority of patients (17 of 23 vitiligo patches) compared with NBUVB phototherapy (5 of 23) between treatment 5 and 10 (Table 3, Fig. 1-3). In addition, in patients that did not respond to prior treatment with conventional phototherapy including NBUVB, repigmentation appeared at 20 laser treatments (Fig. 4). Table 4 shows that the average grade of repigmentation in the excimer laser-treated patches was higher than that in NBUVB-treated patches. It is not yet clear whether excimer laser treatment is more effective than NBUVB phototherapy beyond 20 times laser or UVB irradiation. Because in conventional NBUVB it is not uncommon to see a patient responding to treatment after more than 20 treatments, when hardly any pigmentation was seen after 20 treatments. The results of this study suggest that excimer laser treatment may allow repigmentation within a shorter period of time than does NBUVB phototherapy, while limiting exposure to only selected areas. Also, the rapid onset of repigmentation may play an important role in supporting patient motivation and compliance.
Photobiologically, the wavelengths of the excimer laser (308 nm) and NBUVB (311 nm) are very close to one another, and the therapeutic effects may well be similar. Recently, the mechanism of the excimer laser's high efficacy in psoriasis treatment has been investigated. Psoriasis vulgaris is mediated by activated T-lymphocytes infiltrating the epidermis and the dermo-epidermal interface (5). The major mechanism of action of UVB light in the treatment of inflammatory dermatosis is the cytotoxic effect on infiltrating T cells, where the mechanism of cell death is most probably apoptosis. The capacity of a UVB light source to induce T cell apoptosis is paralleled by its clinical efficacy (6, 7). Novak et al. (8) demonstrated that the irradiation of T cells with the excimer laser in vitro induced a higher number of apoptotic cells than did irradiation with NBUVB light at the same dosage. The more effective induction of T cell apoptosis by the excimer laser may be responsible for its greater clinical efficacy. The biological effects of coherent laser light may differ from those of incoherent light of the same wavelength. Conventional UVB sources emit polychromatic, continuous, incoherent light, whereas the excimer laser emits coherent, monochromatic, UVB light in short pulses. This permits the variation of some important phototherapeutic parameters, such as impulse frequency and intensity. It has been suggested that these optical properties of the excimer laser should make it more effective than NBUVB in the treatment of vitiligo (9).
The results of this study strongly support targeted phototherapy with the xenon-chloride 308-nm excimer laser as more effective than NBUVB phototherapy in the treatment of vitiligo. Long-term studies are needed to confirm and extend these findings.
Fig. 2.
Vitiligo patches on the right side of the trunk (A) prior to NBUVB phototherapy, (B) at 5 treatments, (C) at 15 treatments, and (D) at 20 treatments (G: repigmentation grade).
References
- 1.Le Poole IC, Das PK, Van den Wijngaard RM, Bos JD, Westerhof W. Review of the etiopathomechanism of vitiligo: a convergence theory. Exp Dermatol. 1993;2:145–153. doi: 10.1111/j.1600-0625.1993.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 2.Scherschun L, Kim JJ, Lim HW. Narrow-band ultraviolet B is a useful and well-tolerated treatment for vitiligo. J Am Acad Dermatol. 2001;44:999–1003. doi: 10.1067/mjd.2001.114752. [DOI] [PubMed] [Google Scholar]
- 3.Asawanonda P, Anderson RR, Chang Y, Taylor CR. 308-nm excimer laser for the treatment of psoriasis: a dose-response study. Arch Dermatol. 2000;136:619–624. doi: 10.1001/archderm.136.5.619. [DOI] [PubMed] [Google Scholar]
- 4.Spencer JM, Nossa R, Ajmeri J. Treatment of vitiligo with the 308-nm excimer laser: A pilot study. J Am Acad Dermatol. 2002;46:727–731. doi: 10.1067/mjd.2002.121357. [DOI] [PubMed] [Google Scholar]
- 5.Trehan M, Taylor CR. High-dose 308-nm excimer laser for the treatment of psoriasis. J Am Acad Dermatol. 2002;46:732–737. doi: 10.1067/mjd.2002.120538. [DOI] [PubMed] [Google Scholar]
- 6.Ozawa M, Ferenczi K, Kikuchi T, Cardinale I, Austin LM, Coven TR, Burack LH, Krueger JG. 312-nanometer ultraviolet B light (narrow-band UVB) induces apoptosis of T cells within psoriatic lesions. J Exp Med. 1999;189:711–718. doi: 10.1084/jem.189.4.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bianchi B, Campolmi P, Mavilla L, Danesi A, Rossi R, Cappugi P. Monochromatic excimer light (308 nm): an immunohistochemical study of cutaneous T cells and apoptosis-related molecules in psoriasis. J Eur Acad Dermatol Venereol. 2003;17:408–413. doi: 10.1046/j.1468-3083.2003.00758.x. [DOI] [PubMed] [Google Scholar]
- 8.Novak Z, Bonis B, Baltas E, Ocsovszki I, Ignacz F, Dobozy A, Kemeny L. Xenon chloride ultraviolet B laser is more effective in treating psoriasis and in inducing T cell apoptosis than narrow-band ultraviolet B. J Photochem Photobiol B. 2002;67:32–38. doi: 10.1016/s1011-1344(02)00280-4. [DOI] [PubMed] [Google Scholar]
- 9.Baltas E, Csoma Z, Iynacz F, Dobozy A, Kemeny L. Treatment of vitiligo with the 308-nm xenon chloride excimer laser. Arch Dermatol. 2002;138:1619–1620. [PubMed] [Google Scholar]