Abstract
Primary hemangiopericytoma of the rib is extremely rare and only a few cases have been reported. A 62-yr-old man presented with an aching chest pain and dyspnea. Thoracic computed tomography revealed a homogenous mass expanding the right seventh rib. A diagnosis of hemangiopericytoma was established by percutaneous needle biopsy. Preoperative embolization of the feeding vessels of the tumor was performed in order to prevent perioperative bleeding. There was no significant bleeding during the surgery, where complete resection of the tumor with 7th to 9th ribs with a surgical margin of 5 cm was performed. Postoperative course was uneventful and there has been no recurrence for thirteen months. To our knowledge, there has been no report to apply a preoperative embolization of a primary hemangiopericytoma of the rib.
Keywords: Hemangiopericytoma; Rib; Embolization, Therapeutic; Tomography, X-ray Computed
INTRODUCTION
Hemangiopericytoma is a mesenchymal tumor that occurs most commonly in the soft tissues of the upper and lower extremities, pelvis, and retroperitoneal space and seldom in visceral organs (1). Due to its vascular origin, it can be found anywhere in the body. However, it rarely originates from the ribs (2). Transarterial embolization is a procedure which can be performed prior to surgery of highly vascular tumors in order to avoid perioperative bleeding. Although there are a few reports (3, 4) of preoperative embolization of hemangiopericytomas, to our knowledge, there has been no report to apply a preoperative embolization of a primary hemangiopericytoma of the rib.
CASE REPORT
A 62-yr-old man was admitted to our department with the complaints of progressive dyspnea, an aching chest pain on the right side, malaise and anorexia with weight loss on 4 December 2001. He denied fever, sputum production, or hemoptysis. His medical history was noteworthy for diabetes mellitus type II, a 10-pack year history of smoking, and a moderate history of alcohol.
On physical examination, the patient complained of chest pain on deep inspiration but appeared well. Respiration rate was 22 per minute. The lungs had percussion dullness in the right base with decreased tactile fremitus. There was mild to moderate tenderness over the right 7th rib. The remainder of the examination findings were within normal limits.
A chest roentgenogram on admission demonstrated a large, indistinct opacity on the peripheral region of the right lower zone associated with blunting of the right lateral costophrenic sulcus.
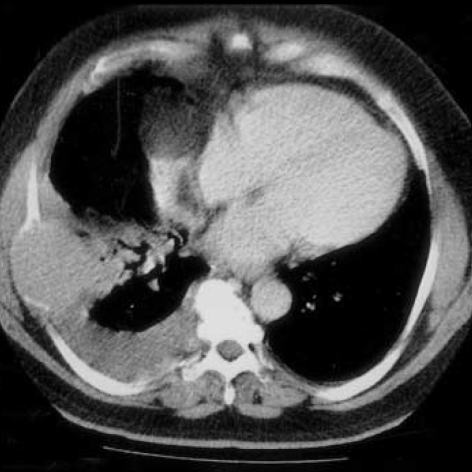
Computed tomographic (CT) scans of thorax revealed a homogeneous mass expanding the right seventh rib and invading into the adjacent lung, and a right sided pleural effusion (Fig. 1).
Fig. 1.
Computed tomographic (CT) scan of thorax demonstrates a homogeneous mass expanding the right seventh rib and invading into the adjacent lung, and also a right sided pleural effusion.
Fiberoptic bronchoscopy showed no abnormality. Thoracentesis revealed an exudative serous effusion. Cytology was reported as showing class II cells. Histopathologic examination of the pleural biopsy specimens were reported as chronic pleuritis. To clearly identify the mass, a CT-guided, core needle biopsy was performed. Histopathologic examination of the biopsy was reported as hemangiopericytoma. The staging procedures were done to determine whether the tumor was primary or metastatic. The ultrasonography and CT of the abdominopelvic region, magnetic resonance imaging of both upper and lower extremities and CT of the cranium were reported as normal. Bone scintigraphy showed increased radioactive uptake of right 7th rib.
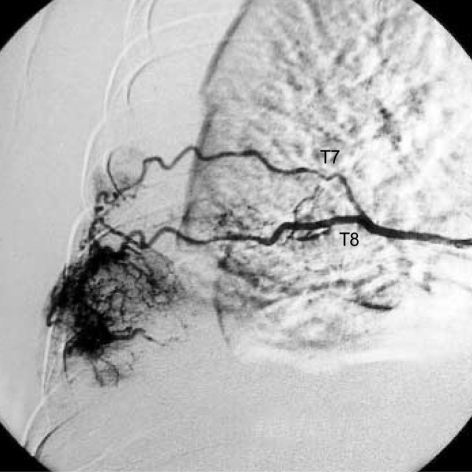
Preoperative angiography showed hypervascularization of the tumor from the right 7th and 8th (Fig. 2), and also from 9th intercostal arteries. We performed embolization with polyvinyl alcohol (PVA) particles. Firstly, we embolized arterioles within the tumor for which we used PVA, 250 µm in size. Then, embolization of the feeding arteries of the tumor was done with PVA, 750-1,000 m in size. Immediate postembolization arteriogram demonstrated complete occlusion of the arteries.
Fig. 2.
Preoperative angiography shows hypervascularization of the tumor from the right 7th and 8th intercostal arteries.
A right thoracotomy was performed on 14 January 2001. It was seen that the tumor was originating from the right seventh rib. Complete resection of the mass with 7th, 8th, and 9th rib with a surgical margin of 5 cm and a wedge resection of the adjacent lung was done. There was no any significant bleeding during the operation.
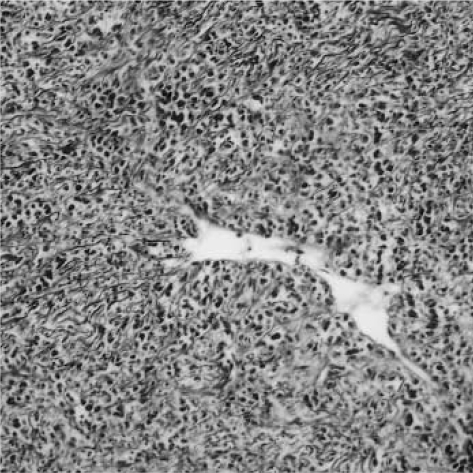
Macroscopic evaluation of the resected tumor revealed an encapsulated and lobulated mass located posteriorly to the 6th to 9th ribs. The sectioned surface had a grayish-white colour. Microscopic evaluation of the tumor revealed a solid mesenchymal mass composed of indistinct fusiform to rounded cells arranged around slit-like and branching thin-walled vessels (Fig. 3). No pleomorphism or atypia was detectable. The mitotic count was very low. A reticulin stain showed delicate reticulin network around each tumoral cell. Immunohistochemically tumor cells stained positively for vimentin and focally for CD-34, and negatively for cytokeratin, smooth muscle actin, S-100 and CD-31. Surgical borders were tumor free except the pleural infiltration on the wedge resection material. Postoperative course was uneventful. There has been no recurrence for thirteen months.
Fig. 3.
Microscopic evaluation of the tumor reveals a solid mesencymal mass composed of indistinct fusiform to rounded cells arranged around slit-like and branching thin-walled vessels (Hematoxylin-Eosin, ×120).
DISCUSSION
Hemangiopericytomas, that are believed to be derived from the vascular pericyte, rarely originate from ribs, although they can be found in any region which contains pericytes (5). Clinical manifestations are varied. Usually chest pain, dry cough and dyspnea are the presenting symptoms. But, it may be asymptomatic and may be detected as an abnormal shadow on a chest radiography film (3). There is a predilection for the right side (5). The radiographic appearance is that of a mass on the lateral chest wall (6). Rarely, it may reach a huge size occupying two thirds of one hemithorax (7). In our case, thorax CT revealed that a large indistinct opacity on the peripheral region of the right lower zone on chest radiography was a homogeneous mass expanding the right seventh rib.
Microscopically the tumor consists of numerous vascular spaces of variable size and shape separated by aggegates of tightly packed oval to spindle-shaped cells with bland nuclei. Mitotic figures and nuclear atypia are variable in number and degree (6). In our case, microscopic evaluation of the tumor revealed a solid mesencymal mass composed of indistinct fusiform to rounded cells arranged around slit-like and branching thin-walled vessels. No pleomorphism or atypia was detectable. The mitotic count was very low. Gomori silver impregnation method revealed a dense reticulin meshwork confirming the perivascular distribution of tumoral cells. The results of immunohistochemical studies were consistent with the diagnosis (8). Because hemangiopericytomas are highly vascular tumours, because the choice of treatment for primary ones is surgery, and because some authors (3, 5) reported massive bleeding during the operation of hemangiopericytomas, we performed transarterial embolization preoperatively in order to prevent or decrease perioperative bleeding (3). And then, the patient underwent a right thoracotomy during which there was no any significant bleeding. Because the recurrence rate was reported as 50% (7, 9), long-term follow-up is necessary for the patient. In our case, there has been no recurrence for thirteen months.
Finally, our case report has two important features: 1) primary hemangiopericytoma of the rib is an extremely rare tumor; 2) preoperative embolization of a primary hemangiopericytoma of the rib have not been reported heretofore.
References
- 1.Enzinger FM, Smith BH. Hemangiopericytoma. An analysis of 106 cases. Hum Pathol. 1976;7:61–82. doi: 10.1016/s0046-8177(76)80006-8. [DOI] [PubMed] [Google Scholar]
- 2.Collet P, Loire R, Guerin JC, Brune J. Hemangiopericytomes thoraciques apparemment primitifs. Rev Pneumol Clin. 1985;41:151–154. [PubMed] [Google Scholar]
- 3.Craven JP, Quigley TM, Bolen JW, Raker EJ. Current management and clinical outcome of hemangiopericytomas. Am J Surg. 1992;163:490–493. doi: 10.1016/0002-9610(92)90394-7. [DOI] [PubMed] [Google Scholar]
- 4.Morandi U, Stefani A, De Santis M, Paci M, Lodi R. Preoperative embolization in surgical treatment of mediastinal hemangiopericytoma. Ann Thorac Surg. 2000;69:937–939. doi: 10.1016/s0003-4975(99)01361-2. [DOI] [PubMed] [Google Scholar]
- 5.Yanagihara K, Ueno Y, Isobe J, Yoshimi N, Itoh M. Hemangiopericytoma of the chest wall. Ann Thorac Surg. 1997;63:537–539. doi: 10.1016/s0003-4975(96)00935-6. [DOI] [PubMed] [Google Scholar]
- 6.Fraser RS, Müller NL, Colman N, Pare PD. Diagnosis of Diseases of the Chest. 4th ed. Philadelphia: W.B. Saunders Company; 1999. [Google Scholar]
- 7.Biagi G, Gotti G, Bisceglie M, Lorenzini L, Toscano M, Sforza V. Uncommon intrathoracic extrapulmonary tumor: primary hemangiopericytoma. Ann Thorac Surg. 1990;49:998–999. doi: 10.1016/0003-4975(90)90888-d. [DOI] [PubMed] [Google Scholar]
- 8.Wick MR, Swanson PE, Manivel JC. Immunohistochemical analysis of soft tissue sarcomas. Comparisons with electron microscopy. Appl Pathol. 1988;6:169–196. [PubMed] [Google Scholar]
- 9.Feldman F, Seaman WB. Primary thoracic hemangiopericytoma. Radiology. 1964;182:998–1009. doi: 10.1148/82.6.998. [DOI] [PubMed] [Google Scholar]