Abstract
Aims
To replicate the finding that there is a single dimension trait in alcohol use disorders and to test whether usual 5+ drinks for men and/4+ drinks for women and other measures of alcohol consumption help to improve alcohol use disorder criteria in a series of diverse patients from Emergency Departments (EDs) in four countries.
Design
Cross-sectional surveys of patient 18 and older that reflected consecutive arrival at the ED. The Composite International Diagnostic Interview Core was used to obtain a diagnosis of DSM-IV alcohol dependence and alcohol abuse. Quantity and frequency of drinking and drunkenness as well as usual number of drinks consumed during the last year.
Setting
Participants were 5,195 injured and non-injured patients attending 7 EDs in 4 countries, Argentina, Mexico, Poland the U.S., (between 1995-2001).
Findings
Using exploratory factor analyses alcohol use disorders can be described as a single, unidimensional continuum without any clear cut distinction between the criterions for dependence and abuse in all sites. Results from item response theory analyses showed that the current DSM-IV criterions tap people in the middle-upper end of the alcohol use disorder continuum. Alcohol consumption (amount and frequency of use) can be used in all EDs with the current DSM-IV diagnostic criterions to help tap the middle-lower part of this continuum. Even though some specific diagnostic criterions and some alcohol consumption variables showed differential item function across sites, test response curves were invariant for ED sites and their inclusion would not impact the final (total) performance of the diagnostic system.
Conclusions
DSM-IV abuse and dependence form a unidimensional continuum in ED patients regardless of country of survey. Alcohol consumption variables, if added, would help to tap patients with more moderate severity. DSM diagnostic system for alcohol use disorders showed invariance and performed extremely well in these samples.
Introduction
Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)[1;2] and from the Australian National Survey of Mental Health and Wellbeing [3] suggested that there is evidence of a single dimension trait for alcohol abuse and dependence in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition [4;5], but the current symptom items do not tap well into the less severe range of the alcohol disorder continuum. A good candidate to cover this part of the spectrum could be measures of alcohol consumption. Using data from the NESARC, Saha [6] concluded that “DSM-IV alcohol abuse and dependence criteria formed a continuum of alcohol use disorder severity along with drinking 5+/4+ at least once a week in the past year criterion”. That is, five or more drinks per occasion for males and four or more for females (5+/4+) at least once a week in the past year when introduced with others symptoms of the current DSM-IV criteria for alcohol abuse and dependence in an Item Response Theory analysis (IRT) tapped into the mildest range of the alcohol use disorder continuum (i.e., lower levels of severity) that was not captured by any other abuse or dependence criteria. Following the report of Saha [6], Helzer [7] discussed the evidence for the unidimensionality of substance use disorders and suggested that, for alcohol use disorders, the 5+/4+ criterion could be added to the categorical definition to strengthen the “mild to moderate range of dimensional definition”. While each dimension of the DSM diagnostic scheme is intended to describe maladaptive patterns of consumption[8], a level of consumption considered ‘maladaptive’ has not been included in the diagnostic nosology due, in part, to cross-cultural variation in normative drinking levels[9].
The introduction of measures of alcohol consumption together with a clinical approach of categorical diagnosis is promising but two limitations exist based on prior analysis in the general population. First, these results need to be replicated using different datasets, especially those across various types of clinical practice in which patients under consultation tend to have more symptoms and more severe symptoms than general population samples, such as NESARC. Secondly, it is not clear what the impact may be, across countries and cultures, of introducing consumption into the DSM-IV alcohol use disorder diagnostic criteria. In 2004 NIAAA published guidelines for at-risk drinking (that which increases the risk of developing alcohol use disorders, morbidity and mortality), defined as 5 or more drinks per occasion for males and 4 or more for females (5+/4+)[10]. While drinking 5+/4+ at least once a week in the past year is, indeed, a marker of heavy episodic drinking, this measure has a large variation in prevalence across cultures, and the variation is not necessarily in the same direction as variation in alcohol abuse and dependence. For example, Mexico has been shown to have a low-medium per-capita consumption rate when compared to countries with similar development [11], and a high abstention rate, but low levels of alcohol use disorders[12] and high levels of episodic and intoxicating drinking (such as the 5+/4+)[13]. According to a WHO report, Mexico exhibits one of the most “detrimental consumption patterns” (a value of 4) of any country, based on a large number of heavy drinking occasions, drinking outside of meals, a high level of fiesta drinking, and drinking in public places, etc., as opposed to a country exhibiting the least detrimental consumption pattern (a value of 1), based on few heavy drinking occasions, drinking with meals, no fiesta drinking, and little drinking in public places[13]. By contrast, in this same region and with a similar level of development, Argentina has a higher per capita consumption than Mexico (almost double), a low abstention rate, a much higher prevalence of alcohol dependence compared to Mexico, especially among women, but low rates of heavy drinking (almost half of the Mexican rate; and a detrimental drinking pattern value of 2)[13].
Here we build from prior work to test the unidimensionality of alcohol use disorders and the use of measures of heavy alcohol consumption in a sample of 7 emergency department (ED) sites in 4 countries, compiled as part of the Emergency Room Collaborative Alcohol Analysis Project[14]. We used exploratory factor analysis (EFA) and item response theory (IRT) to study the latent construct of alcohol use disorder in samples from ED patients from different countries in an effort to replicate the finding that there is a unique factor solution for alcohol use disorders[15]. Secondly, if unidimensionality exists, we will test whether 5+/4+ and other measures of alcohol consumption help to improve alcohol use disorder criteria by adding a criterion in the low-medium spectrum of the disorder, applicable to all four countries included here.
Methods
Samples and Data Sets
The dataset used for this analyses include 5,195 ED patients from five sites in four countries, Santa Clara, California (U.S., 1995-1996 (n=1,429)), Pachuca, Mexico (during 1996-1997 (n=1,417)), Warsaw and Sosnowiec, Poland (2002-2003 (n=1,317)) and Mar del Plata, Argentina (during 2001 (n= 978)). Details about these samples have been published elsewhere[16]. The response rates were: Santa Clara 73%, Pachuca 93%, Warsaw 67%, Sosnowiec 65% and Mar del Plata 92%. Both injured and non-injured patients were interviewed regarding quantity and frequency of usual drinking and frequency of high maximum occasions during the last year, frequency of drunkenness, alcohol dependence and abuse/harmful drinking questions, and demographic characteristics (age, gender, percentage injury, and education). Data were collected using a similar methodology and instrumentation developed by Cherpitel[17]. All studies used a probability sampling design in which each shift was equally represented for each day of the week during the period data were collected in each ED facility. Across all studies, patient samples of those 18 and older were selected from ED admission forms, which included walk-in patients as well as those arriving by ambulance, and reflected consecutive arrival at the ED. The particular sampling frame in a study depended on the number of patients admitted to the ED facility covered in each study. Once selected for the study, and as soon as possible after ED admission, patients were approached with an informed consent to participate, and were then breathalyzed and administered a questionnaire of about 25 minutes in length by trained interviewers while the patient was in the waiting room or treatment area and/or following treatment. Patients who were too severely injured or ill to be interviewed in the ED and who were subsequently hospitalized were interviewed later after their condition had stabilized. Both injured and non-injured patients were interviewed regarding quantity and frequency of usual drinking and frequency of high maximum occasions during the last year, frequency of drunkenness, alcohol dependence and abuse questions, and demographic characteristics.
Measures
Quantity-Frequency (Q-F) of Drinking and Drunkenness
Patients were asked an abbreviated version of the Graduated Frequency series of questions [18], which obtains data, for the last year, on the frequency of drinking any alcoholic beverage, and the frequency, separately of consuming 12 or more drinks in a day, and 5 or more but less than 12 in a day. Patients were also asked their usual number of drinks and the frequency of drunkenness during the last year. The frequency of 12 or more drinks, 5 or more drinks and drunkenness ranged from every day, nearly every day, 3 or 4 times a week, once or twice a week, 2-3 times a month, about once a month, 6-11 times a year, 1-5 times a year and to never during the last 12 months. Different cut-points for these frequency options were used for males and females. Heavy drinking measures to be considered as candidate measures in each of the analyses include usual quantity of at least 5+/4+ drinks per occasion for men/women, 12+ drinks monthly/any for men/women, 5+ drinks weekly/monthly for men/women, drunkenness weekly/monthly for men/women.
Diagnostic Criteria for Alcohol Dependence and Abuse
An adaptation of the Alcohol Section of the Composite International Diagnostic Interview (CIDI) Core[19] was used to obtain a diagnosis of DSM-IV alcohol dependence and alcohol abuse. The CIDI diagnostic interview was developed as a joint project by the World Health Organization and the U.S. Alcohol, Drug Abuse and Mental Health Administration, and has been tested in several countries. The alcohol section of the CIDI has been found to perform well, is easy to use, and is acceptable to subjects in almost all cultures[20]. The DSM-IV criteria for 12 month dependence consist of three positive responses across seven domains (tolerance, withdrawal, drinking more than intended, unsuccessful efforts to control, giving up pleasures or interests to drink, spending a great deal of time in drinking activities, continued alcohol use despite problems). Also obtained was a diagnosis for DSM-IV alcohol abuse as lifetime presence among 12-month drinkers based on any one of four items: role, physical, legal or social consequences of drinking.
Data Analysis
Analysis followed closely the strategy used in Saha [6]. Dimensionality of the set of DSM-IV measures was first explored using standard factor analytic methods. This is referred to as the base model. In addition, individual heavy drinking measures were included, one at a time, in separate models along with DSM-IV items to investigate the performance of these items in the context of the larger set of DSM-IV items.
Standard psychometric methods were used, including examining marginal and bivariate distributions of variables before dimension reduction techniques were applied. To estimate the underlying factor structure on dichotomous items, non-linear link functions were utilized using Mplus[21]. A number of solutions were examined, including 1, 2, and 3 dimensional solutions and their fit was assessed using standard measures, such as the CFI (Comparative Fit Index), RMSEA (Root Mean Squared Error of Approximation), and SRMR (Standardized Root Mean Square Residual). Properties of the resulting scale(s) were examined using the Kuder-Richardson formula for examining internal scale reliability of a set of dichotomous items.
After the factor structure of the set of DSM-IV items was investigated, Item Response Theory (IRT) models were used to study the latent alcohol use disorder construct separately in probability samples of ED patients from four different countries in an effort to replicate the finding that there is an underlying common structure[15] and, if so, whether individual heavy drinking measures help to improve alcohol use disorder criteria by adding a criterion in the low-medium spectrum of the disorder, applicable to all four countries. IRT analysis implemented in Mplus[21] was used to derive two main parameters, the threshold and the discrimination parameters. The first refers to the “severity” of a criterion (threshold), with high severity being those less frequently endorsed by respondents. The second parameter measures the ability of a criterion to discriminate respondents from low to high levels of the disorder continuum (slope). Graphical aids and plots of both parameters were used. Finally, differential item functioning (DIF) was performed in the PARSCALE[22] to test whether the probabilities of responding in different categories of consumption differed by population for the same underlying level of the attribute (the latent trait measuring severity). Items were evaluated for DIF by contrasting the IRT difficulty or location (bi) and slope (ai) parameters between the groups. Finally, test response curve (TRC) were plotted using the expected raw scores by the severity of the alcohol use disorder continuum for each study site. If the TRCs for sites do not substantially differ it can conclude that the significant item-level DIFs (if found) cancel out when the total scale is used [6].
Results
In Santa Clara, a low percentage of patients were admitted to the ED with an injury (22.5%) while in Poland, the majority of ED admissions were for injury (63.7%) (see Table 1). Patients from these EDs also differed on gender (a larger proportion of males in Pachuca and Poland), age (older in Poland and Santa Clara) and educational background (a high level of education in Santa Clara and Poland). Baseline differences are also evident on measures of lifetime alcohol consumption (a larger proportion of abstention in Pachuca followed by Santa Clara), 12 month drinking (a lower proportion of in Pachuca and Santa Clara) and drinking prior to the injury (a lower proportion in Pachuca and Poland). Heavy drinking (5+/4+), nevertheless, was more common in Poland and Pachuca. All DSM-IV disorders were more common in Santa Clara, followed by Argentina, Poland and Mexico. Overall, as expected, a large variation in alcohol involvement was found across these four samples. Comparatively across sites, the Mexican sample tended to show lower overall consumption, higher episodic use and lower levels of disorders. In contrast, the sample from Argentina showed higher overall consumption, lower levels of heavy drinking and percentages of alcohol disorders midway between the other sites.
TABLE 1. Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) sites with DSM-IV alcohol data characteristics of study population N=5,195.
| Site | Santa Clara, CA | Pachuca, Mexico | Mar del Plata, Argentina | Warsaw & Sosnowiec, Poland | TOTAL | |
|---|---|---|---|---|---|---|
| (year) n |
(1995-1996) 1429 |
(1996-1997) 1417 |
(2001) 867 |
(2002-2003) 1482 |
5195 | |
| Injury | % | 22.5 | 47.4 | 45.8 | 63.7 | 44.9 |
| Male | % | 49.1 | 52.0 | 44.3 | 58.2 | 51.7 |
| <=30 years | % | 36.1 | 44.7 | 41.2 | 29.5 | 37.4 |
| Education Some college and above | % | 36.1 | 14.9 | 10.4 | 21.1 | 21.8 |
| Lifetime Alcohol use | % | 85.1 | 66.8 | 91.6 | 93.2 | 83.5 |
| Alcohol use last 12 months | % | 62.0 | 38.6 | 77.7 | 74.1 | 61.6 |
| Alcohol use six hours prior | % | 11.3 | 9.2 | 16.7 | 9.7 | 11.1 |
| Last 12 months 5+/4+ DRINKS* | % | 18.6 | 25.1 | 20.7 | 37.5 | 26.2 |
| Last 12 months alcohol abuse | % | 7.0 | 3.3 | 6.7 | 5.9 | 5.6 |
| Last 12 months alcohol dependence | % | 12.3 | 4.9 | 6.7 | 4.3 | 7.0 |
| Last 12 months alcohol abuse or dependence | % | 19.2 | 8.2 | 13.4 | 10.2 | 12.7 |
NOTE: Santa Clara data is weighted
Usual consumption of 5 or more drinks per occasion for males and 4 or more drinks for females per drinking occasion
As seen from the prior data, large variation was found in lifetime and 12 month (current) drinking prevalence rates. A different picture emerged when current drinkers only were examined (Table 2). The most striking difference was the high level of abuse and dependence among current drinkers in the Pachuca sample which ranked second, only behind the US. Among current drinkers, Poland had the lowest rates of abuse and dependence. Overall, 20% of these EDs patients had a current DSM-IV alcohol use disorder which demonstrates, as expected, the large role of alcohol among these patients. Overall, the criterion with the largest prevalence was larger/longer and the criterion with the lowest prevalence was legal problems. As expected, the four measures of heavy drinking were found to have high variation in prevalence and large differences across sites. Usual 5+/4+ was highest in Pachuca and drunkenness was highest in Santa Clara. The consumption variable with the smallest variation in prevalence across sites was 5+ weekly for men or monthly for women.
TABLE 2. DSM-IV alcohol use disorders and criterion list by Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) sites.
| Santa Clara | Pachuca | Mar del Plata | Warsaw & Sosnowiec | TOTAL | |
|---|---|---|---|---|---|
| Among 12m drinkers (n) | 884 | 547 | 662 | 1098 | 3191 |
| 12m Prevalence of DSM-IV alcohol abuse (%) | 11.3 | 8.6 | 8.6 | 8.0 | 9.1 |
| 12m Prevalence of DSM-IV alcohol dependence (%) | 19.8 | 12.6 | 8.8 | 5.7 | 11.4 |
| 12m Prevalence of DSM-IV abuse-or-dependence (%) | 31.0 | 21.2 | 17.4 | 13.8 | 20.6 |
| DSM-IV Criterion | |||||
| D1 Tolerance (%) | 16.5 | 6.0 | 7.9 | 4.4 | 8.7 |
| D2 Withdrawal (%) | 21.6 | 18.1 | 9.1 | 11.6 | 14.9 |
| D3 Larger/Longer (%) | 25.0 | 14.5 | 13.6 | 10.7 | 16.0 |
| D4 Quit/Control (%) | 17.1 | 12.8 | 7.9 | 3.5 | 9.8 |
| D5 Time Spent (%) | 17.2 | 8.6 | 10.7 | 2.9 | 9.5 |
| D6 Activities Given Up (%) | 13.1 | 6.6 | 5.1 | 2.4 | 6.6 |
| D7 Physical/Psychological Problems (%) | 23.8 | 13.0 | 11.9 | 10.1 | 14.8 |
| A1 Neglect Roles (%) | 16.0 | 15.7 | 9.2 | 6.9 | 11.4 |
| A2 Hazardous Use (%) | 11.2 | 4.8 | 7.6 | 4.8 | 7.1 |
| A3 Legal Problems (%) | 9.5 | 1.8 | 1.8 | 2.1 | 4.1 |
| A4 Social/Interpersonal Problems (%) | 19.9 | 7.7 | 7.1 | 7.1 | 10.7 |
| Alcohol Consumption | |||||
| DRINKS DO YOU USUALLY TAKE (5+/4+) FOR MEN/WOMEN (%) | 29.2 | 64.4 | 24.8 | 50.3 | 41.6 |
| 12+ MONTHLY/ANY FOR MEN/WOMEN (%) | 23.9 | 25.4 | 24.0 | 16.3 | 21.6 |
| 5+ WEEKLY/MONTHLY FOR MEN/WOMEN (%) | 25.0 | 15.7 | 27.5 | 21.6 | 22.7 |
| DRUNKENNESS WEEKLY/MONTHLY FOR MEN/WOMEN (%) | 16.0 | 7.9 | 10.0 | 3.4 | 9.0 |
DSM-IV Criterion Description
Alcohol dependence (D)
TOLERANCE. Tolerance to the effects of alcohol; need more to get desired effect
WITHDRAWAL. Withdrawal syndrome, or alcohol or similar substance taken to avoid or relieve withdrawal symptoms
LARGER/LONGER. Alcohol is taken in larger amounts or for longer periods than required
QUIT/CONTROL. Persistent desire, or unsuccessful efforts to cut down
TIME SPENT. A great deal of time spent obtaining, using or recovering from the effects of alcohol
ACTIVITIES GIVEN UP. Reduction in important social, occupational or recreational activities because of alcohol use
PHYSICAL/PSYCHOLOGICAL PROBLEMS. Continued use despite awareness of alcohol use causing physical or psychological problems
Alcohol abuse (A)
NEGLECT ROLES. Failure to fulfill obligations, important activities at work, school or home because of alcohol use
HAZARDOUS USE. Recurrent use in physically dangerous situations e.g. driving, operating machinery, injured after drinking
LEGAL. Recurrent alcohol-related legal problems
SOCIAL/INTERPERSONAL PROBLEMS. Recurrent use despite awareness of alcohol use causing social or interpersonal problems
Alcohol consumption description
DRINKS DO YOU USUALLY TAKE (5+/4+) FOR MEN/WOMEN. 5 or more drinks per occasion for males and 4 or more for females per drinking occasion
12+ MONTHLY/ANY FOR MEN/WOMEN. Any 12 or more drinks per day for females and 12 or more drinks per day at least monthly for males
5+ WEEKLY/MONTHLY FOR MEN/WOMEN. 5 or more drinks per day at least monthly for females and 5 or more drinks per day at least weekly for males
DRUNKENNESS WEEKLY/MONTHLY FOR MEN/WOMEN. Drunkenness episodes at least monthly for females and at least weekly for males
Exploratory factor analyses was used for testing the unidimensionality of alcohol use disorders both in the merged ED sample as well as separately by site (Table 3). In the merged sample, all 11 criterions loaded significantly on a single dimension. A two factor solution produced one factor with all dependence items and one abuse item. The second factor had only two of the four abuse items. Both factors had a strong correlation (0.854) and the first eigenvalue was much larger than the second, all of which suggest that a single factor solution is a reasonable description of the data and that the 11 criterions formed a single, unidimensional trait in the merged ED patients. Inspection of the four samples did not show divergent conclusions. Among the U.S. and Mexican samples, a large correlation between the two factors and a small second eigenvalue suggest that unidimensionality is a reasonable and more parsimonious explanation for these data. The two factors solution for Santa Clara produced a first factor composed of all dependence items and one abuse item (hazardous use) while the second factor included the other three abuse items. For Pachuca, the two factor solution produced one factor with only 4 dependence items and a second factor with three abuse items (neglect roles, legal problems and social/interpersonal problems) and one dependence item (quit/control) that was not easily interpretable. The factor correlation is very high for the 1st and 2nd dimensions of the solution for both factors (.87 in Santa Clara and .89 in Pachuca) indicating little difference between the two in terms of additional information. The CFAs are also extremely high for both sites for the 1 dimensional solution (.998 in Santa Clara and 1.0 in Pachuca), where above .95 is considered very good. Additionally, the RMSEA is considered to be very low and indicates very good fit for both sites (RMSEA = .05 is considered good fit and RMSEA = .04 in Santa Clara and .01 in Pachuca). Finally, the 2nd eigenvalues were much smaller than the first for both sites (0.518 for Santa Clara and 0.716 for Pachuca) which strongly supports a 1 dimensional solution. On the other hand, for Argentina and Poland, there was clearly only one factor. A second factor in both datasets produced small and non-significant loadings, with small eigenvalues. Most importantly, this second factor had loadings that were almost identical to the loadings of the one factor solution, supporting again a 1 dimensional solution. The lower part of Table 3 shows the factor loadings of the four consumption candidates, assuming a single dimension solution. That is, assuming that the 11 items are considered to be a single factor in the merged sample, the addition of 5+/4+ would produce a factor loading of 0.470. In all sites the alcohol consumption variables loaded in the unidimensional alcohol use disorder trait, ranging from a low of 0.470 to a high of 0.865. The variables 5+/4+ and drunkenness produced the most variable loadings across sites, while 12+ drinks and 5+ drinks produced more homogenous loadings across sites.
TABLE 3. Exploratory factor Analyses of alcohol use disorder by Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) sites.
| ALL EDS | US-Santa Clara | Mexico-Pachuca | Mar del Plata-Argentina | Warsaw & Sosnowiec, Poland | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Base model | Base model | Base model | Base model | Base model | |||||||||||
| One factor (N=3,191) |
Two factors (N=3,191) |
One factor (N=884) |
Two factors (N=884) |
One factor (N=547) |
Two factors (N=547) |
One factor (N=662) |
Two factors (N=662) |
One factor (N=1098) |
Two factors (N=1098) |
||||||
| Tolerance (D) | 0.860 | 0.880 | -0.015 | 0.888 | 0.971 | -0.084 | 0.888 | 0.743 | 0.163 | 0.808 | 0.809 | 0.009 | 0.746 | 0.821 | -0.219 |
| Withdrawal (D) | 0.844 | 0.733 | 0.129 | 0.911 | 0.911 | 0.005 | 0.788 | 0.850 | -0.049 | 0.778 | 0.783 | 0.243 | 0.824 | 0.840 | -0.026 |
| Larger/Longer (D) | 0.892 | 0.951 | -0.057 | 0.906 | 0.932 | -0.024 | 0.963 | 0.987 | -0.004 | 0.879 | 0.872 | -0.169 | 0.788 | 0.902 | -0.304 |
| Quit/Control (D) | 0.896 | 0.851 | 0.056 | 0.953 | 0.942 | 0.016 | 0.790 | 0.023 | 0.797 | 0.842 | 0.846 | 0.018 | 0.847 | 0.850 | 0.010 |
| Time spent (D) | 0.947 | 0.957 | -0.004 | 0.967 | 0.942 | 0.032 | 0.924 | 0.562 | 0.387 | 0.943 | 0.937 | -0.274 | 0.913 | 0.917 | 0.017 |
| Activities given up (D) | 0.942 | 0.944 | 0.006 | 0.958 | 0.966 | -0.005 | 0.877 | 0.452 | 0.451 | 0.978 | 0.975 | -0.060 | 0.868 | 0.907 | -0.089 |
| Phys/psych problems (D) | 0.886 | 0.658 | 0.257 | 0.890 | 0.634 | 0.286 | 0.873 | 0.833 | 0.056 | 0.921 | 0.926 | 0.089 | 0.830 | 0.790 | 0.133 |
| Neglect roles (A) | 0.819 | 0.443 | 0.416 | 0.810 | 0.189 | 0.676 | 0.901 | 0.174 | 0.763 | 0.821 | 0.815 | -0.180 | 0.791 | 0.768 | 0.086 |
| Hazardous use (A) | 0.782 | 0.558 | 0.251 | 0.795 | 0.589 | 0.231 | 0.726 | 0.386 | 0.360 | 0.818 | 0.820 | 0.086 | 0.755 | 0.763 | -0.003 |
| Legal problems (A) | 0.894 | -0.001 | 0.968 | 0.881 | -0.006 | 0.958 | 0.796 | 0.002 | 0.820 | 0.931 | 0.931 | -0.035 | 0.953 | 0.659 | 0.678 |
| Social/Interpersonal problems (A) | 0.895 | 0.228 | 0.730 | 0.885 | 0.216 | 0.730 | 0.857 | -0.062 | 0.953 | 0.881 | 0.888 | 0.217 | 0.944 | 0.816 | 0.286 |
| Factor correlation | -- | 0.854 | -- | 0.867 | -- | 0.892 | -- | -0.006 | -- | 0.293 | |||||
| Eigenvalue | 8.659 | 9.112 | 8.955 | 9.473 | 8.189 | 8.905 | 8.563 | 9.134 | 7.910 | 8.632 | |||||
| Comparative Fit Index (CFI) | 0.998 | 1.000 | 0.998 | 1.000 | 1.000 | 1.000 | 0.999 | 1.000 | 0.995 | 0.999 | |||||
| Tucker Lewis Index (TLI) | 0.997 | 1.000 | 0.998 | 1.000 | 1.000 | 1.000 | 0.999 | 1.000 | 0.993 | 0.998 | |||||
| Root mean squared error of approximation RMSEA | 0.030 | 0.011 | 0.039 | 0.000 | 0.010 | 0.000 | 0.021 | 0.011 | 0.031 | 0.015 | |||||
| Factor loadings when Add one Alcohol Consumption Variable | |||||||||||||||
| “Usual 5+/4+” for Men/Women | 0.470 | -- | -- | 0.611 | -- | -- | 0.503 | -- | -- | 0.608 | -- | -- | 0.537 | -- | -- |
| “12+ drinks” (Monthly/Any) | 0.726 | -- | -- | 0.741 | -- | -- | 0.706 | -- | -- | 0.782 | -- | -- | 0.754 | -- | -- |
| “5+ drinks” (Weekly/Monthly) | 0.730 | -- | -- | 0.775 | -- | -- | 0.733 | -- | -- | 0.773 | -- | -- | 0.764 | -- | -- |
| “Got drunk” (Weekly/Monthly) | 0.792 | -- | -- | 0.771 | -- | -- | 0.741 | -- | -- | 0.788 | -- | -- | 0.865 | -- | -- |
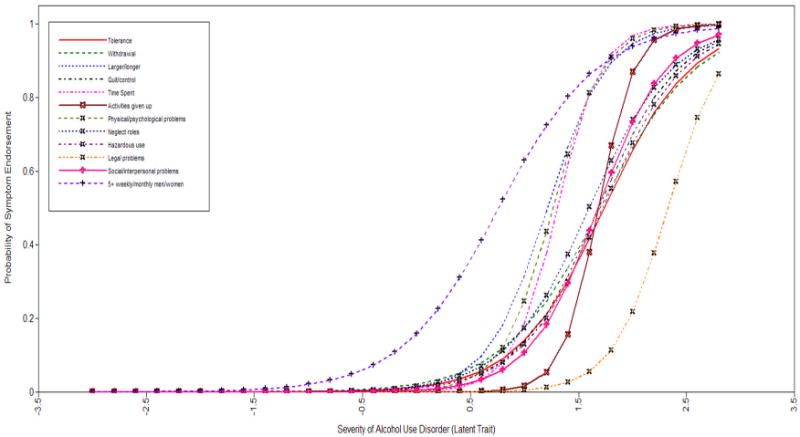
IRT results for the merged sample and by site are presented in Table 4. In the merged sample, the largest discrimination score was found for the item “time spent” and the lowest for the item “hazardous use”. The largest severity score was found for the item “legal problems” and the lowest for the item “larger/longer” (see Figure 1)
TABLE 4. Item Response Theory analyses of alcohol use disorder by Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) sites.
| ALL ERS | US-Santa Clara | Mexico-Pachuca | Mar del Plata-Argentina | Warsaw & Sosnowiec, Poland | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Base model | Base model | Base model | Base model | Base model | ||||||
| Discrimination (S.E.) |
Severity (S.E.) |
Discrimination (S.E.) |
Severity (S.E.) |
Discrimination (S.E.) |
Severity (S.E.) |
Discrimination (S.E.) |
Severity (S.E.) |
Discrimination (S.E.) |
Severity (S.E.) |
|
| Tolerance (D) | 1.79 (0.1) | 1.57 (0.05) | 1.97 (0.2) | 1.10 (0.07) | 2.32 (0.4) | 1.69 (0.11) | 1.43 (0.2) | 1.74 (0.14) | 1.33 (0.2) | 2.18 (0.14) |
| Withdrawal (D) | 1.62 (0.1) | 1.23 (0.04) | 2.15 (0.2) | 0.86 (0.06) | 1.38 (0.2) | 1.14 (0.10) | 1.26 (0.2) | 1.72 (0.14) | 1.58 (0.2) | 1.44 (0.08) |
| Larger/Longer (D) | 2.04 (0.1) | 1.11 (0.04) | 2.19 (0.3) | 0.73 (0.06) | 3.41 (0.6) | 1.11 (0.07) | 1.99 (0.3) | 1.23 (0.09) | 1.28 (0.1) | 1.61 (0.10) |
| Quit/Control (D) | 2.02 (0.1) | 1.45 (0.05) | 2.99 (0.4) | 1.00 (0.06) | 1.33 (0.2) | 1.44 (0.12) | 1.60 (0.2) | 1.68 (0.13) | 1.78 (0.3) | 2.11 (0.13) |
| Time spent (D) | 2.94 (0.2) | 1.39 (0.04) | 3.52 (0.5) | 0.98 (0.06) | 2.88 (0.5) | 1.46 (0.09) | 2.88 (0.5) | 1.30 (0.08) | 2.76 (0.5) | 2.02 (0.10) |
| Activities given up (D) | 2.80 (0.3) | 1.61 (0.05) | 3.03 (0.5) | 1.19 (0.07) | 2.14 (0.4) | 1.67 (0.11) | 3.45 (0.9) | 1.69 (0.11) | 2.13 (0.3) | 2.21 (0.12) |
| Physical/psychological problems (D) | 1.95 (0.1) | 1.18 (0.04) | 1.89 (0.2) | 0.80 (0.06) | 1.88 (0.3) | 1.30 (0.09) | 2.57 (0.4) | 1.25 (0.08) | 1.58 (0.2) | 1.54 (0.09) |
| Neglect roles (A) | 1.54 (0.1) | 1.45 (0.05) | 1.38 (0.1) | 1.24 (0.09) | 2.13 (0.3) | 1.13 (0.08) | 1.57 (0.2) | 1.58 (0.12) | 1.48 (0.2) | 1.82 (0.11) |
| Hazardous use (A) | 1.37 (0.1) | 1.84 (0.07) | 1.39 (0.2) | 1.52 (0.11) | 1.23 (0.2) | 2.18 (0.23) | 1.49 (0.2) | 1.74 (0.14) | 1.34 (0.2) | 2.12 (0.14) |
| Legal problems (A) | 1.98 (0.2) | 1.98 (0.07) | 1.79 (0.2) | 1.52 (0.09) | 1.76 (0.4) | 2.39 (0.25) | 2.35 (0.7) | 2.32 (0.19) | 2.38 (0.4) | 2.22 (0.13) |
| Social/Interpersonal problems (A) | 1.92 (0.1) | 1.41 (0.05) | 1.73 (0.2) | 0.98 (0.07) | 1.91 (0.3) | 1.62 (0.11) | 1.87 (0.3) | 1.67 (0.12) | 2.44 (0.4) | 1.61 (0.08) |
| Bayesian Information Criterion (BIC) | 15280.343 | 5602.446 | 2680.439 | 2907.884 | 4054.591 | |||||
| Sample-Size Adjusted BIC | 15210.439 | 5532.578 | 2610.602 | 2838.033 | 3984.713 | |||||
| Akaike (AIC) | 15146.845 | 5497.188 | 2585.741 | 2808.988 | 3944.563 | |||||
| Usual 5+/4+ for Men/Women | 0.54 (0.04) | 0.44 (0.05) | 0.77 (0.1) | 0.89 (0.10) | 0.54 (0.1) | (-0.76) (0.15) | 0.85 (0.1) | 1.05 (0.11) | 0.69 (0.1) | (-0.01) (0.07) |
| Bayesian Information Criterion (BIC) | 19318.55 | 6518.006 | 3362.339 | 3548.913 | 5470.552 | |||||
| Sample-Size Adjusted BIC | 19242.292 | 6441.787 | 3286.153 | 3472.712 | 5394.322 | |||||
| Akaike (AIC) | 19172.916 | 6403.179 | 3259.032 | 3441.026 | 5350.522 | |||||
| 12+ Monthly/Any for Men/Women | 1.08 (0.1) | 1.08 (0.05) | 1.09 (0.1) | 0.97 (0.09) | 0.87 (0.1) | 1.01 (0.12) | 1.38 (0.2) | 0.88 (0.08) | 1.23 (0.1) | 1.29 (0.08) |
| Bayesian Information Criterion (BIC) | 17877.09 | 6342.244 | 3214.044 | 3453.668 | 4813.899 | |||||
| Sample-Size Adjusted BIC | 17800.831 | 6266.025 | 3137.858 | 3377.467 | 4737.669 | |||||
| Akaike (AIC) | 17731.455 | 6227.417 | 3110.737 | 3345.782 | 4693.869 | |||||
| 5+ Weekly/Monthly for Men/Women | 1.08 (0.1) | 1.03 (0.05) | 1.23 (0.1) | 0.87 (0.08) | 0.97 (0.1) | 1.46 (0.15) | 1.29 (0.2) | 0.76 (0.08) | 1.22 (0.1) | 1.03 (0.07) |
| Bayesian Information Criterion (BIC) | 17956.534 | 6321.914 | 3076.866 | 3510.967 | 4964.491 | |||||
| Sample-Size Adjusted BIC | 17880.276 | 6245.695 | 3000.68 | 3434.766 | 4888.261 | |||||
| Akaike (AIC) | 17810.9 | 6207.087 | 2973.559 | 3403.08 | 4844.461 | |||||
| Drunk Monthly/Any for Men/Women | 1.34 (0.1) | 1.69 (0.05) | 1.18 (0.1) | 1.31 (0.10) | 1.14 (0.2) | 1.91 (0.19) | 1.30 (0.2) | 1.63 (0.13) | 1.92 (0.3) | 2.09 (0.13) |
| Bayesian Information Criterion (BIC) | 16608.255 | 6168.202 | 2919.738 | 3223.419 | 4253.866 | |||||
| Sample-Size Adjusted BIC | 16531.997 | 6091.983 | 2843.552 | 3147.218 | 4177.636 | |||||
| Akaike (AIC) | 16462.621 | 6053.375 | 2816.431 | 3115.533 | 4133.836 | |||||
Graph 1. Criterion response curves for DSM-IV abuse and dependence criteria in the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP)-All Emergency Departments combined.
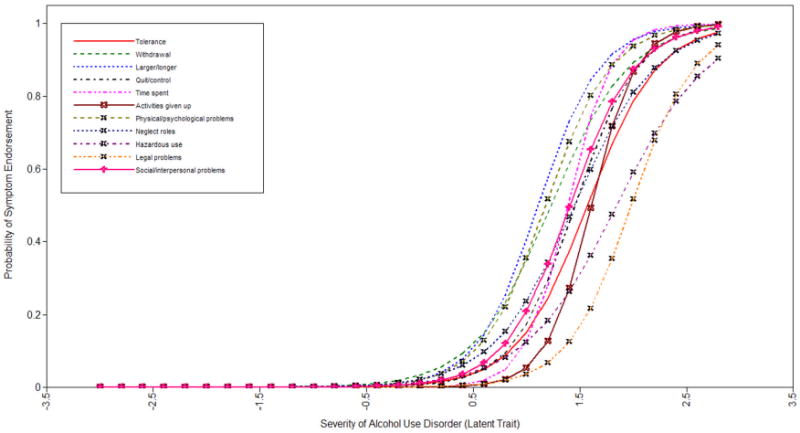
It is apparent from the comparison across sites that there are several differences in both the discrimination and severity estimates for different criterion. The bottom of Table 4 shows the values of discrimination and severity for the consumption variables. In general the inclusion of a consumption measure item along with other DSM items appears to have accomplished the stated goal of including an additional item that is consistent with other items of alcohol use disorders and that also taps the mildest range of the alcohol use disorder continuum. Nevertheless, the usual 5+/4+ is too low in discrimination and severity (also with very high Bayesian Information Criterion [BIC] values) and while slightly lower BICs were found in the model using the drunkenness variable, the BIC value was still too high, possibly a result of multidimensionality introduced by including the item. These conclusions apply for all sites. The two best candidates to tap the lower level of severity of the continuum while keeping acceptable BICs scores were 12+ drinks monthly/any for men/women, and 5+ drinks weekly/monthly for men/women. The variable 5+ drinks weekly/monthly for men/women performed slightly better for Santa Clara and Pachuca, while the 12+ drinks monthly/any for men/women variable performed slightly better for Argentina and Poland, accordingly to their BICs values. For illustrative purposes we present the graphs of the criterion response curves for DSM-IV abuse and dependence criteria and 5+ drinks weekly/monthly for men/women in each study site.
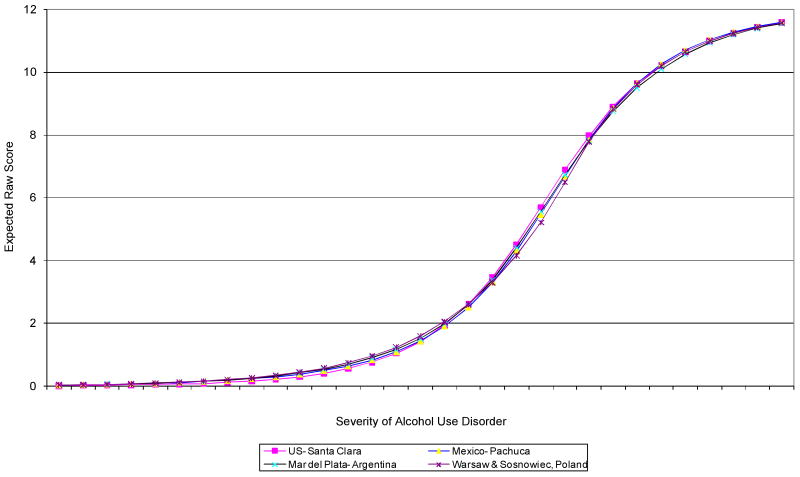
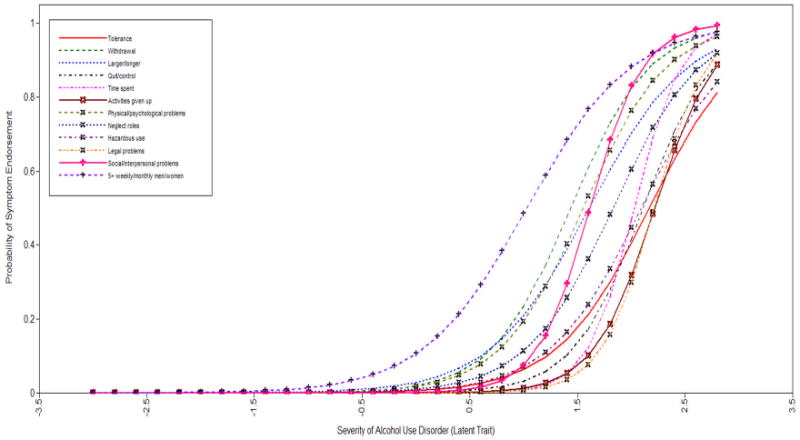
DIF analyses was performed for each of the 11 alcohol use disorder criteria contrasting at the same time severity (thresholds) and discrimination (slopes) parameters (Table 5). Four dependence items (withdrawal, time spent, larger/longer and quit/control) showed heterogeneity across study site (p < 0.05), while three abuse items and three consumption variables showed heterogeneity in threshold estimates. DIF was also found in discrimination (slopes) for two dependence criterions (time spent and phys/psych problems), one abuse criterion (social/interpersonal) and three consumption variables, suggesting heterogeneity of discrimination estimates across EDs sites. Next, the test response curves were plotted to examine whether these item specific differences canceled out in the total alcohol use disorder continuum. The results were very similar for most alcohol consumption variables (with the exception of usual 5+/4+) and suggested that there was no evidence of DIF between study site at the total score level. As an example, Figure 6 shows the DIF results that incorporated the variable 5+ drinks weekly/monthly for men/women. The DIF curves for all sites were virtually identical, suggesting that even if consumption variables had different severities and discriminations across sites, as expected, in the aggregate level their inclusion would not impact the final (total) performance of the diagnostic scheme.
TABLE 5. Differential Item Function analyses for Thresholds (severity) & Slopes (discrimination) of alcohol use disorder by Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) sites Results from PARSCALE: Adjusted thresholds and slopes across four sites.
| Thresholds Estimates | US-Santa Clara | Mexico-Pachuca | Mar del Plata-Argentina | Warsaw & Sosnowiec, Poland | χ2(3df) | p |
|---|---|---|---|---|---|---|
| Tolerance (D) | 1.10 | 1.28 | 1.19 | 1.28 | 2.96 | 0.400 |
| Withdrawal (D) | 0.86 | 0.49 | 0.99 | 0.34 | 38.92 | <0.001 |
| Larger/Longer (D) | 0.73 | 0.53 | 0.64 | 0.45 | 12.05 | 0.007 |
| Quit/Control (D) | 1.00 | 0.96 | 1.25 | 1.50 | 13.51 | 0.004 |
| Time spent (D) | 0.98 | 1.00 | 0.70 | 1.27 | 11.17 | 0.011 |
| Activities given up (D) | 1.19 | 1.28 | 1.25 | 1.39 | 2.47 | 0.483 |
| Phys/psych problems (D) | 0.80 | 0.73 | 0.75 | 0.55 | 4.70 | 0.193 |
| Neglect roles (A) | 1.24 | 0.64 | 0.86 | 1.27 | 21.96 | <0.001 |
| Hazardous use (A) | 1.52 | 1.67 | 1.11 | 1.45 | 5.13 | 0.161 |
| Legal problems (A) | 1.52 | 2.12 | 2.01 | 1.71 | 13.65 | 0.004 |
| Social/Interpersonal problems (A) | 0.98 | 1.23 | 1.19 | 0.73 | 9.43 | 0.024 |
| Usual 5+/4+ for Men/Women | 0.89 | -1.72 | 0.74 | -1.78 | 320.16 | <0.001 |
| 12+ Monthly/Any for Men/Women | 0.97 | 0.70 | 0.38 | 0.65 | 31.47 | <0.001 |
| 5+ Weekly/Monthly for Men/Women | 0.88 | 0.88 | 0.43 | 0.71 | 18.88 | <0.001 |
| Drunk Monthly/Any for Men/Women | 1.32 | 1.45 | 1.23 | 1.36 | 0.80 | 0.851 |
| Slopes Estimates | US-Santa Clara | Mexico-Pachuca | Mar del Plata-Argentina | Warsaw & Sosnowiec, Poland | χ2(3df) | p |
| Tolerance (D) | 1.97 | 2.33 | 1.51 | 3.85 | 18.97 | <0.001 |
| Withdrawal (D) | 2.15 | 1.31 | 1.66 | 1.54 | 20.57 | <0.001 |
| Larger/Longer (D) | 2.19 | 4.11 | 1.84 | 1.40 | 19.76 | <0.001 |
| Quit/Control (D) | 3.00 | 1.19 | 2.26 | 2.72 | 37.13 | <0.001 |
| Time spent (D) | 3.53 | 2.52 | 3.11 | 5.40 | 6.10 | 0.105 |
| Activities given up (D) | 3.04 | 1.91 | 2.90 | 0.56 | 21.49 | <0.001 |
| Phys/psych problems (D) | 1.89 | 2.09 | 2.44 | 1.64 | 2.89 | 0.410 |
| Neglect roles (A) | 1.37 | 3.31 | 1.52 | 0.82 | 30.68 | <0.001 |
| Hazardous use (A) | 1.39 | 1.67 | 1.81 | 2.31 | 9.15 | 0.027 |
| Legal problems (A) | 1.79 | 2.25 | 2.82 | 7.30 | 17.93 | 0.001 |
| Social/Interpersonal problems (A) | 1.73 | 1.77 | 1.88 | 2.16 | 1.35 | 0.722 |
| Usual 5+/4+ for Men/Women | 0.77 | 0.75 | 0.64 | 0.60 | 4.00 | 0.260 |
| 12+ Monthly/Any for Men/Women | 1.08 | 0.84 | 1.22 | 1.13 | 2.75 | 0.433 |
| 5+ Weekly/Monthly for Men/Women | 1.22 | 0.97 | 1.10 | 1.14 | 2.08 | 0.560 |
| Drunk Monthly/Any for Men/Women | 1.17 | 1.49 | 1.32 | 2.64 | 12.06 | 0.007 |
Graph 6. Test response curves (TRCs) for DSM-IV abuse and dependence criteria, and 5+Weekly/Monthly for Men/Women by each study site.
Discussion
Two main conclusions can be drawn from these analyses based on clinical samples of EDs patients from four different countries with very heterogeneous per-capita alcohol consumption and drinking cultures. First, exploratory factor analyses indicated that alcohol use disorders can be described as a single, unidimensional continuum without any clear cut distinctions between the criteria for dependence and abuse in all sites. This finding is in concordance with other reports from general population samples in Australia[3], the U.S.[2;23], samples of U.S. adolescents from clinical[24] and adjudicated, clinical, and community samples[25] and samples of treatment-seeking addicts[26] and psychiatric outpatients[27]. In these studies, as in the one reported here, even when some abuse items loaded on a second factor, a single unidimensional trait emerges as a much more parsimonious solution. Samples here of patients undergoing medical or injury treatment also strengthen the generalizability of the unidimensional finding for alcohol use disorders beyond community samples. These samples included patients that have been characterized as heavy chronic and acute drinkers[28;29]and, indeed, have a much higher prevalence of both alcohol use disorders and endorsement of alcohol use disorders symptoms than that reported in community samples, but lower than that reported in a clinical sample of adolescents in alcohol treatment[25] and under clinical treatment[26;27]. The cross-national nature of our sample widens the applicability of this conclusion and supports a unitary diagnosis of DSM alcohol use disorders that goes beyond a U.S. or English speaking milieu.
Secondly, results from the IRT analyses showed that in all EDs the current DSM-IV criteria tap people in the middle-upper end of the alcohol use disorder continuum. Data on alcohol consumption (amount and frequency of use) can be used in all EDs with the current DSM-IV diagnostic criteria to help tap the middle to lower part of this continuum, as first reported by Saha [6]. Nevertheless, as expected, there is no single alcohol consumption measure that is, by itself, invariant (both on severity and discrimination values) within these diverse ED populations. Even when in all ED samples a single dimension of alcohol use disorders exists and alcohol consumption may be used to tap people at the low end of the continuum, differences in severity and discrimination was observed across samples in some of the 11 alcohol use disorder criteria and in three of the four alcohol consumption variables. Prior qualitative research in the scope of current nosological classifications [30] and quantitative analyses at the criterion level for an alcohol dependence diagnosis [31] has warned that not all criterions are similarly understood across different societies (such as impaired control and neglect of interests) and should be fine tuned for use in a cross-cultural context. While reports of cross-cultural differences in the prevalence of alcohol consumption variables, especially measures of heavy or harmful drinking, have previously been reported, this is the first report to show that differences on heavy drinking measures also abound in the context of the two parameters, severity and discrimination, on IRT analyses. Nevertheless, just a few of such DSM-IV criteria for alcohol dependence showed heterogeneity in estimates across sites. Most of the heterogeneity was found in abuse criteria and in alcohol consumption variables. These results also supported the finding from Saha [6] that even when some individual criteria show heterogeneity in severity and discrimination across subgroups (here among study sites) the total classification of the alcohol use disorder continuum is basically invariant. The addition of a consumption variable to the 11 criteria does not change the total performance of current diagnostic criteria. Two measures of consumption emerged as particularly useful for these countries, 12+ drinks monthly/any for men/women, and 5+ drinks weekly/monthly for men/women.
As a summary of our results, the inclusion of a Q-F measure performed as expected. It did improve DSM criteria by including respondents at the lower end of the dependence continuum. When a Q-F measure was included, it did not change the overall performance of the diagnostic criteria. But our analyses also found cross-country variation in the difficulty of endorsing a heavy drinking criterion such as and 5+ drinks weekly/monthly for men/women, one of the best Q-F candidate measures for these samples. Although differential item functioning was also observed among several other DSM-IV criteria, the heavy drinking measures appeared to exhibit some of the largest cross-cultural variation in the difficulty parameter seen among all DSM-IV criteria. While the four countries examined here are clearly not representative of all drinking cultures and although the ER samples are likely different from their respective general populations, findings here suggest that caution should be used in including culturally sensitive measures such as heavy drinking in the proposed DSM-V, and that additional research in this area is necessary.
Finally, in order to recommend a change in the current DSM-IV criteria we still need to consider the overall impact that this change may have in the performance of the full criteria, especially the impact in sensitivity and specificity. How the choice of a particular measure of alcohol consumption affects the total prevalence of alcohol use disorders when added to the current 11 criteria is a matter of great relevance, but goes beyond the scope of the present analyses. This change may have implications/ramifications across cultures since different cultures have very different drinking patterns. Even more, when applied to different cultures Q-F measures also need to consider other dimensions such as drinking context and duration of drinking. These issues were not discussed in this paper, as they go beyond the scope of any EFA and IRT framework and merit a separate analysis. From the differential item functioning of some measures of heavy drinking (such as any 5+/4+ for men/women or monthly drunkenness/any for men/women) it is clear that the choice of the alcohol consumption measure can have dramatic influences on the definition of the final criteria under study, as showed in the NESARC when adding a binge drinking measure to the current 11 criteria of DSM-IV.[32]
Study limitations
This study is limited to an analysis of data from patients with non-fatal injuries and medical emergencies who attended specific emergency departments. Although the study design provides a representative sample of patients from each ED facility, patients may not be representative of other ED facilities in the region or country. Additionally, reported here are data from only four countries, and while each demonstrated distinctly different drinking patterns, the inclusion of EDs from other countries may have influenced study findings. An additional limitation is that cultural factors may have influenced willingness to report the presence of specific criterion as well as the interpretation of survey items related to these criterion, such as the hazardous use criterion illustrated by drinking and driving behaviors[33]. It is important to note that even when we presented data on the inclusion of Q-F questions into current DSM-IV definition of alcohol use disorders, our definitions of Q-F were not exactly the same used by Saha et al. (2007) and replication of their findings may still be needed. Finally, results reported here are limited to the scope of the EFA and IRT analyses. Whether the addition of a consumption item (and which item) as a new criterion for alcohol use disorders would affect prevalence estimates across societies is an important topic that is beyond the scope of this report, but will be pursued in future analyses.
Graph 2. Criterion response curves for DSM-IV abuse and dependence criteria and 5+Weekly/Monthly for Men/Women in each study site. (US-Santa Clara).
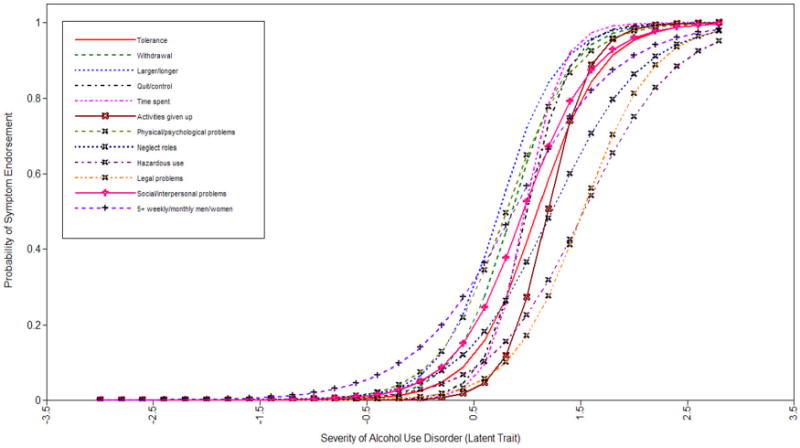
Graph 3. Criterion response curves for DSM-IV abuse and dependence criteria and 5+Weekly/Monthly for Men/Women in each study site. (Mexico-Pachuca).
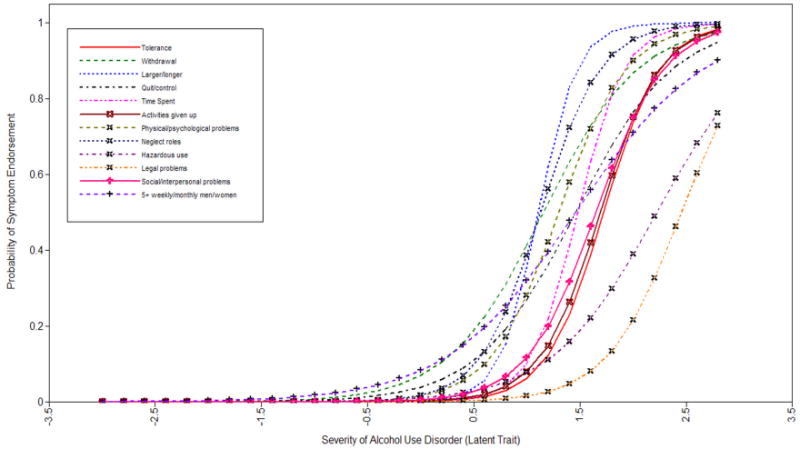
Graph 4. Criterion response curves for DSM-IV abuse and dependence criteria and 5+Weekly/Monthly for Men/Women in each study site. (Mar del Plata-Argentina).
Graph 5. Criterion response curves for DSM-IV abuse and dependence criteria and 5+Weekly/Monthly for Men/Women in each study site. (Warsaw & Sosnowiec, Poland).
Acknowledgments
Funding was provided by a contractual agreement with the American Psychiatric Association to Guilherme Borges and Cheryl Cherpitel and a grant from NIAAA (2 RO1 AA013750-04) (Cheryl Cherpitel P.I.).
Footnotes
No conflict of interest
Reference List
- 1.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and Co-occurrence of Substance Use Disorders and Independent Mood and Anxiety Disorders Results From the National Epidemiologic Survey on Alcohol and Related Conditions. Am Med Assoc. 2004:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 2.Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:931–941. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- 3.Proudfoot H, Baillie AJ, Teesson M. The structure of alcohol dependence in the community. Drug and alcohol dependence. 2006;81:21–26. doi: 10.1016/j.drugalcdep.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV-TR) American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 5.American Psychiatric Association. DSM-IV. Washington, D.C.: American Psychiatric Association; 1994. [Google Scholar]
- 6.Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug and alcohol dependence. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helzer JE, Bucholz KK, Gossop M. A dimensional option for the diagnosis of substance dependence in DSM-IV. International Journal of Methods in Psychiatric Research. 2007;16:S24–S33. doi: 10.1002/mpr.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. British Medical Journal. 1976;1:1058. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenfield TK, Kerr WC. Alcohol measurement methodology in epidemiology: recent advances and opportunities. Addiction. 2008;103:1082. doi: 10.1111/j.1360-0443.2008.02197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NIAAA. Helping Patients Who Drink Too Much. A clinician's guide. Rockville, MD: National Institutes of Health; 2005. [Google Scholar]
- 11.Medina-Mora ME, Borges G, Villatoro J. The measurement of drinking patterns and consequences in Mexico. Journal of Substance Abuse. 2000;12:183–196. doi: 10.1016/s0899-3289(00)00048-1. [DOI] [PubMed] [Google Scholar]
- 12.Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, Bijl R, Borges G, Caraveo-Anduaga JJ, Dewit DJ. Comorbidity of substance use disorders with mood and anxiety disorders Results of the international consortium in psychiatric epidemiology. Addictive Behaviors. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- 13.WHO 2004. Comparative Quantification of Health Risks Chapter 12, Alcohol, in Global Status Report on Alcohol 2004. WHO; Geneva, Switzerland: 2004. p. 94. ed. [Google Scholar]
- 14.Cherpitel CJ, Bond J, Ye Y, Borges G, Macdonald S, Giesbrecht N. A cross-national meta-analysis of alcohol and injury: data from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP) Addiction. 2003;98:1277. doi: 10.1046/j.1360-0443.2003.00459.x. [DOI] [PubMed] [Google Scholar]
- 15.Kraemer HC, Shrout PE, Rubio-Stipec M. Developing the diagnostic and statistical manual V: what will ôstatisticalö mean in DSM-V? Social Psychiatry and Psychiatric Epidemiology. 2007;42:259–267. doi: 10.1007/s00127-007-0163-6. [DOI] [PubMed] [Google Scholar]
- 16.Borges G, Cherpitel CJ, Orozco R, Bond J, Ye Y, Macdonald S, Giesbrecht N, Stockwell T, Cremonte M, Moskalewicz J. Acute alcohol use and the risk of non-fatal injury in sixteen countries. Addiction. 2006;101:993. doi: 10.1111/j.1360-0443.2006.01462.x. [DOI] [PubMed] [Google Scholar]
- 17.Cherpitel CJ. A study of alcohol use and injuries among emergency room patients. Drinking and casualties: accidents, poisonings and violence in an international perspective. 1989:288–299. [Google Scholar]
- 18.Greenfield TK. Ways of measuring drinking patterns and the difference they make: experience with graduated frequencies. Journal of Substance Abuse. 2000;12:33–49. doi: 10.1016/s0899-3289(00)00039-0. [DOI] [PubMed] [Google Scholar]
- 19.WHO (1990a) Composite International Diagnostic Interview: Autorized Core Version 1.0. WHO; Geneva: 2009. ed. [Google Scholar]
- 20.Wittchen HU, Robins LN, Cottler LB, Sartorius N, Burke JD, Regier D. Cross-cultural feasibility, reliability and sources of variance of the Composite International Diagnostic Interview (CIDI). The Multicentre WHO/ADAMHA Field Trials. The British journal of psychiatry: the journal of mental science. 1991;159:645. doi: 10.1192/bjp.159.5.645. [DOI] [PubMed] [Google Scholar]
- 21.Muthén LK, Muthén B. Mplus version 5.1. Muthé LK, Muthén B; 2008. [Google Scholar]
- 22.SSI 2. Item Response Theory (IRT) from SSI. Scientific Software International; Lincolnwood, IL: 2009. Du Toit, M. [Google Scholar]
- 23.Krueger RF, Nichol PE, Hicks BM, Markon KE, Patrick CJ, Iacono WG, McGue M. Using latent trait modeling to conceptualize an alcohol problems continuum. Psychological Assessment. 2004;16:107–118. doi: 10.1037/1040-3590.16.2.107. [DOI] [PubMed] [Google Scholar]
- 24.Martin CS, Chung T, Kirisci L, Langenbucher JW. Item response theory analysis of diagnostic criteria for alcohol and cannabis use disorders in adolescents: implications for DSM-V. Journal of Abnormal Psychology. 2006;115:807. doi: 10.1037/0021-843X.115.4.807. [DOI] [PubMed] [Google Scholar]
- 25.Gelhorn H, Hartman C, Sakai J, Stallings M, Young S, Rhee SH, Corley R, Hewitt J, Hopfer C, Crowley T. Toward DSM-V: an item response theory analysis of the diagnostic process for DSM-IV alcohol abuse and dependence in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:1329. doi: 10.1097/CHI.0b013e318184ff2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Langenbucher JW, Labouvie E, Martin CS, Sanjuan PM, Bavly L, Kirisci L, Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. Journal of Abnormal Psychology. 2004;113:72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- 27.Ray LA, Kahler CW, Young D, Chelminski I, Zimmerman M. The factor structure and severity of DSM-IV alcohol abuse and dependence symptoms in psychiatric outpatients. Journal of studies on alcohol and drugs. 2008;69:496. doi: 10.15288/jsad.2008.69.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borges G, Cherpitel CJ, Median-Morea ME, Mondraon L, Casanova L. Alcohol consumption in emergency room patients and the general population: a population-based study. Alcoholism: Clinical and Experimental Research. 1998;22:1986–1991. [PubMed] [Google Scholar]
- 29.Cherpitel CJ. Alcohol and injuries: a review of international emergency room studies. Addiction. 1993;88:923–937. doi: 10.1111/j.1360-0443.1993.tb02110.x. [DOI] [PubMed] [Google Scholar]
- 30.Room R, Janca A, Bennett LA, Schmidt L, Sartorius N. WHO cross-cultural applicability research on diagnosis and assessment of substance use disorders: an overview of methods and selected results. Addiction. 1996;91:199–220. doi: 10.1046/j.1360-0443.1996.9121993.x. [DOI] [PubMed] [Google Scholar]
- 31.Ustün B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Göğüş A, Mavreas V, Peters L. WHO study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug and alcohol dependence. 1997;47:161–169. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- 32.Hasin DS, Beseler CL. Dimensionality of lifetime alcohol abuse, dependence and binge drinking. Drug and alcohol dependence. 2009 doi: 10.1016/j.drugalcdep.2008.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keyes KM, Geier T, Grant BF, Hasin DS. Influence of a Drinking Quantity and Frequency Measure on the Prevalence and Demographic Correlates of DSM-IV Alcohol Dependence. Research Society on Alcoholism. 2008 doi: 10.1111/j.1530-0277.2009.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]