Abstract
Context:
Research suggests that appropriate medical care for interscholastic athletes is frequently lacking. However, few investigators have examined factors related to care.
Objective:
To examine medical care provided by interscholastic athletics programs and to identify factors associated with variations in provision of care.
Design:
Cross-sectional study.
Setting:
Mailed and e-mailed survey.
Patients or Other Participants:
One hundred sixty-six South Carolina high schools.
Intervention(s):
The 132-item Appropriate Medical Care Assessment Tool (AMCAT) was developed and pilot tested. It included 119 items assessing medical care based on the Appropriate Medical Care for Secondary School-Age Athletes (AMCSSAA) Consensus Statement and Monograph (test-retest reliability: r = 0.89). Also included were items assessing potential influences on medical care. Presence, source, and number of athletic trainers; school size; distance to nearest medical center; public or private status; sports medicine supply budget; and varsity football regional championships served as explanatory variables, whereas the school setting, region of state, and rate of free or reduced lunch qualifiers served as control variables.
Main Outcome Measure(s):
The Appropriate Care Index (ACI) score from the AMCAT provided a quantitative measure of medical care and served as the response variable. The ACI score was determined based on a school's response to items relating to AMCSSAA guidelines.
Results:
Regression analysis revealed associations with ACI score for athletic training services and sports medicine supply budget (both P < .001) when controlling for the setting, region, and rate of free or reduced lunch qualifiers. These 2 variables accounted for 30% of the variance in ACI score (R2 = 0.302). Post hoc analysis showed differences between ACI score based on the source of the athletic trainer and the size of the sports medicine supply budget.
Conclusions:
The AMCAT offers an evaluation of medical care provided by interscholastic athletics programs. In South Carolina schools, athletic training services and the sports medicine supply budget were associated with higher levels of medical care. These results offer guidance for improving the medical care provided for interscholastic athletes.
Keywords: high schools, administration, interscholastic athletes
Key Points.
Athletic training services and the medical care provided by South Carolina high schools were significantly associated.
The size of the South Carolina high school's annual sports medicine supply budget predicted the medical care provided to its athletes.
Injuries sustained by high school athletes are a well-established public health problem, with numerous authors1–9 reporting that injuries occur in all sports, at all competition levels, in both sexes, and during both games and practices. Most recent estimates indicate that more than 1.4 million high school injuries occur each year in the United States.10 Despite widespread acknowledgment of this problem, questions regarding the availability of appropriate medical care for high school athletics have persisted for many years. Beginning in the 1970s, concern about the quality and availability of the medical care afforded high school athletes began to receive attention.11–13 Over the past 30 years, more than 20 research studies have examined some aspect of medical care provided to high school athletes in 15 states, including South Carolina,14,15 North Carolina,16 California,17 Michigan,18,19 New York,20 Illinois,21–23 Wisconsin,24 Maryland,25 Alabama,26–28 Louisiana,29 Conneticut,30 Iowa,31 Virginia,32 Hawaii,5,33 and Indiana.34 However, these studies offer only a limited understanding of medical care for high school athletes, because the authors focused on medical coverage, primarily for varsity football games, with no assessment of the comprehensive health care provided for an entire athletics program during both practices and competitions.
As early as 1985, Cartland30 suggested the need for established, standardized guidelines to identify minimal standards for the prevention and care of athletic injuries. Finally, in 2002, the “Appropriate Medical Care for Secondary School-Age Athletes (AMCSSAA) Consensus Statement”35 was created to provide standardized guidelines for appropriate medical care for high school athletics. The AMCSSAA consensus statement was developed by an interassociation task force with representatives from 17 professional organizations related to health care, athletics, and secondary school administration, including the National Athletic Trainers' Association, the American Academy of Orthopaedic Surgeons, the National Association of Secondary School Principals, and the National Federation of State High School Associations. The document established recommendations for the prevention, care, and appropriate management of injuries and illnesses specific to the secondary school–aged athlete. It recognized that appropriate care encompasses ongoing daily heath care, not merely emergency care during games. The consensus statement called for the establishment of an athletic health care team for every American high school athletics program consisting of a variety of health care providers with a designated health care provider who is trained to35
Participate in the development and implementation of a comprehensive athletic health care administrative system.
Determine an individual's readiness to participate.
Promote safe and appropriate practice, competition, and treatment facilities.
Advise on the selection, fit, function, and maintenance of athletic equipment.
Develop and implement a comprehensive emergency action plan.
Establish protocols regarding adverse environmental conditions.
Provide for on-site recognition, evaluation, and immediate treatment of injury and illness, with appropriate referrals.
Facilitate rehabilitation and reconditioning.
Provide for psychosocial consultation and referral.
Provide scientifically sound nutritional counseling and education.
Develop injury and illness prevention strategies.
In 2004, the AMCSSAA Task Force supplemented the AMCSSAA consensus statement35 with the AMCSSAA monograph.36 In the monograph, each recommendation of the consensus statement was justified with the supporting, current literature; components of each recommendation were identified; and strategies for implementation were provided. Together, the AMCSSAA consensus statement and monograph provide a comprehensive description of the requirements for a high school athletics program to properly care for its athletes. In 2008, these documents were summarized and published in an article titled “Summary Statement: Appropriate Medical Care for the Secondary School-Aged Athlete.”37
Thus, the recommendations found in the AMCSSAA consensus statement and monograph offer a standardized framework that allows the medical care provided by a high school to be assessed and the factors associated with schools that provide high levels of medical care to be identified. Such relationships could prove useful to schools implementing the AMCSSAA recommendations and improving medical care for high school athletes. Although high schools have been encouraged to hire certified athletic trainers (ATs) to improve medical care,* no authors have examined whether a relationship between athletic training services and improved medical care actually exists in the high school setting. Additionally, evidence suggests that other factors, such as school size,15,18,19,24–27 a school's proximity to a medical center,24,26 a school's public or private status,5,15,21,23 a school's sports medicine supply budget,15,17,33 a school's setting,21,23 and the socioeconomic status of the students in a school,5,21,23 may play a role in the medical care and coverage variations among high schools. Anecdotally, other factors, such as the success of a school's football program and the region of the state in which a school is located, have been linked to differences in the care given, although no evidence exists in the literature to support this claim. The purpose of our research was to examine the comprehensive medical care, as defined by the recommendations of the AMCSSAA consensus statement35 and monograph,36 provided by South Carolina high schools for all athletes in their athletics program and to identify factors associated with schools that provide high levels of care. The following question guided our research: Which factors are associated with the level of medical care if a school's setting, region of the state, and rate of free and reduced lunch qualifiers are controlled?
METHODS
Procedures
We used a 1-survey-per-school sampling approach to survey all South Carolina high schools (N = 263) fielding a varsity-level athletics program belonging to the South Carolina High School League (SCHSL) or the South Carolina Independent School Association (SCISA). Our unit of analysis was each South Carolina high school athletics program, and, as is common with researchers attempting to measure an organization's policies, procedures, and practices,40 we wanted our survey completed by the individual at the high school most knowledgeable about the school's policies, procedures, and practices related to medical care for the athletics program. Although a school's athletics director was designated as the primary survey respondent by name on the envelope and cover letter, instructions in the cover letter asked the athletics director to either complete the survey or designate another individual at the school (such as an AT, coach, physician, principal, or school nurse) to complete the survey in the event the athletics director felt that person was better qualified. All individuals completing the survey were asked to identify their positions in the school.
To maximize response rate, we used a systematic, persistent modified Dillman approach.41 A postcard was sent to each athletics director informing him or her of the survey and requesting completion when it arrived. Five days later, a cover letter describing the purpose of the survey, the survey, and a letter of endorsement from the South Carolina Athletic Coaches Association were mailed to each athletics director. Four weeks after the survey was mailed the first time, a second survey was mailed to all athletics directors who had failed to respond. Two weeks after the second mailing, we sent nonrespondent athletics directors e-mails encouraging them to complete the attached survey and return it via mail or e-mail. One week later, all nonrespondent athletics directors were sent another encouraging e-mail with the attached survey. A week after that, all nonrespondent athletics directors were sent a third encouraging e-mail with the attached survey.
Several additional methods to increase response rate were employed, including follow-up phone calls, e-mail reminders, announcements on the South Carolina Athletic Coaches Association listserve, and radio announcements on a popular, statewide sports radio program. We also were able to address all SCHSL athletics directors at the state's athletic administrators' conference, and we approached SCISA school officials attending the state basketball championships.
Respondents
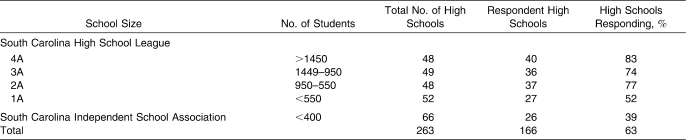
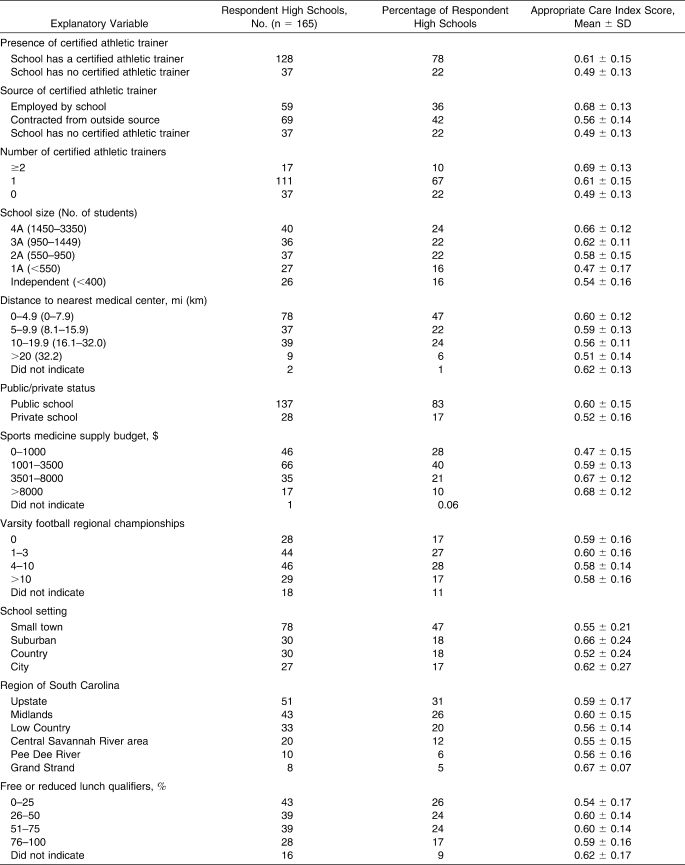
Of the 263 South Carolina high schools, 166 (63%) responded to our survey. We discarded 1 survey because it was incomplete. Surveys were most often completed by athletics directors (54%, n = 90), ATs (38%, n = 63), coaches (4%, n = 7), and other individuals (4%, n = 7). Response rates were higher from public schools than private schools (72% [n = 138] and 40% [n = 28], respectively) and larger schools (SCHSL 4A, 3A, and 2A) than smaller schools (SCHSL 1A and SCISA); however, all types of schools were represented in the sample (Table 1).
Table 1.
Appropriate Medical Care Assessment Tool Response Rate of South Carolina High Schools by School Size
All regions of South Carolina were represented in the sample, with nearly half of respondent schools being located in small towns. Most schools reported being located near a medical center. With regard to the percentage of students qualifying for the free or reduced lunch program, the sample consisted of approximately equal numbers of schools. More than three-quarters of schools (128/165) reported having an AT; few schools reported having more than 1 AT. The ATs were more frequently contracted from an outside source than employed directly by the school or school district. Most schools reported an annual sports medicine supply budget ranging from $1001 to $3500. Just over a quarter of schools had budgets of $1000 or less, whereas less than one-quarter of schools reported a budget between $3501 and $8000. Few schools reported having a budget of more than $8000. Most schools reported winning at least 1 varsity football region championship, but few had won more than 10 championships.
Instrument
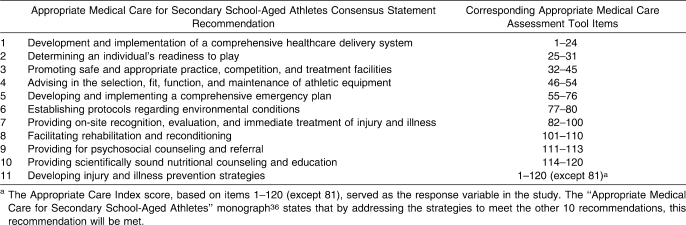
For this study, we created the 132-item Appropriate Medical Care Assessment Tool (AMCAT) to examine the comprehensive medical care provided by a high school for athletes in all sports in its athletic program. The AMCAT items were based on the recommendations of the AMCSSAA consensus statement35 and supporting information cited in the AMCSSAA monograph36 (Table 2). Monograph recommendations for each point of the AMCSSAA consensus statement were identified, summarized, rephrased as policies or practices, and included as items 1–121 on the AMCAT. (Note that the authors of the monograph made no recommendations for consensus statement point 11, “Developing prevention strategies for injury and illness,” because they stated that by meeting the recommendations for the other 10 AMCSSAA consensus statement points, point 11 would also be met.) Use of the consensus statement and monograph recommendations in this manner is consistent with the intention of the AMCSSAA Task Force. In fact, the authors of the AMCSSAA monograph summarized the purpose of the monograph as follows:
Table 2.
Appropriate Medical Care for Secondary School-Aged Athletes Consensus Statement35 Recommendationsa and Corresponding Appropriate Medical Care Assessment Tool Items
This communication will help organizations sponsoring athletic programs for this age group justify the importance of providing appropriate medical care and establishing an athletic health care team to identify the resources they should make available to adolescents participating in organized athletic programs. This article can be also used as an evaluation tool to assess current athletic care delivery programs.36(p5)
Response options for items involving policies were fully in place, partially in place, in planning stages, and does not exist; these responses were assigned the scores 3, 2, 1, or 0, respectively. Response options for items involving practices were always, most of the time, some of the time, and never; these were also assigned the scores 3, 2, 1, or 0, respectively. Items that assessed the existence of equipment were rated on a 2-point scale: yes (1 point) or no (0 points). For all items, higher scores were considered more favorable indicators of provision of medical care.
The points accrued from responses on AMCAT items 1–80 and items 82–120 were used to determine the Appropriate Care Index (ACI) score, ranging from 0 (lowest) to 1 (highest). Thus, the higher the ACI score, the higher the quality of overall medical care provided by a school. Because the AMCAT is a newly developed tool, no normative data exist to determine a “good” ACI score, although higher scores are considered more desirable. We calculated scores for each school in the following manner to ensure that each recommendation of the consensus statement was weighted equally in the overall score, regardless of the number of points possible for assessment of each recommendation category. Points in each of the 10 recommendation categories were summed and then divided by the number of items in that category, yielding 10 scores. As the AMCSSAA consensus statement and monograph did not prioritize 1 recommendation as more important than another, we weighted all 10 recommendation category scores equally and averaged them to create the ACI score. The ACI score served as the response variable and provided an overall score for the medical care provided by a high school.
For example, on the AMCAT were 11 items related to AMCSSAA recommendation category 7, which involves a school's provision of on-site recognition, evaluation, and immediate treatment of injuries and illness. Responses for each item were assigned a score of 3, 2, 1, or 0, as previously described. Thus, for this recommendation category, 33 points were possible. If a respondent accumulated 22 points of the possible 33 points based on responses, we would then divide 22 by 33 to yield a score of 0.67. These steps were repeated for each of the 10 recommendation categories. Finally, all 10 recommendation category scores were averaged to calculate an ACI score ranging between 0 and 1.0.
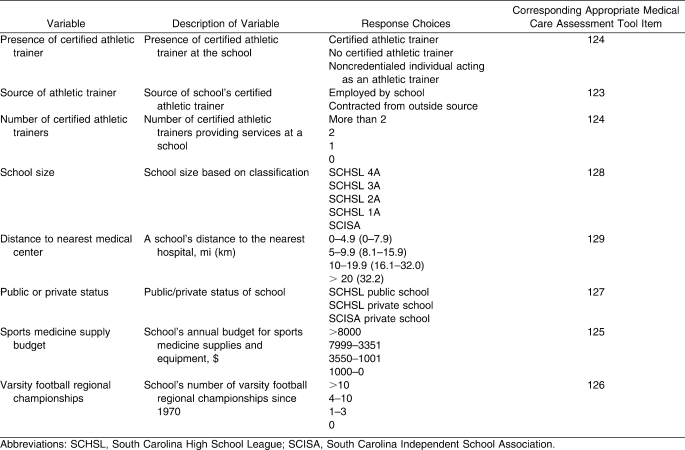
Items 123–129 on the AMCAT assessed factors thought to be associated with the provision of medical care for high school sports, including the presence of an AT, the source of the AT, the number of ATs, school size, distance to the nearest medical center, public or private status, sports medicine supply budget, and the number of varsity football regional championships (Table 3). Many of these factors had been suggested by previous researchers as being associated with medical care in high school sports. In our study, these factors served as explanatory variables, each of which had relevant response choices. For example, for a school's annual sports medicine supply budget, the choices were $0–$1000, $1001–$3500, $3501–$8000, or more than $8000. These ranges were based on our professional experiences in South Carolina high school athletics in an effort to represent different levels of budgeting in the target population.
Table 3.
Explanatory Variables, Descriptions of Variables, Corresponding Appropriate Medical Care Assessment Tool Item, and Supporting Literature
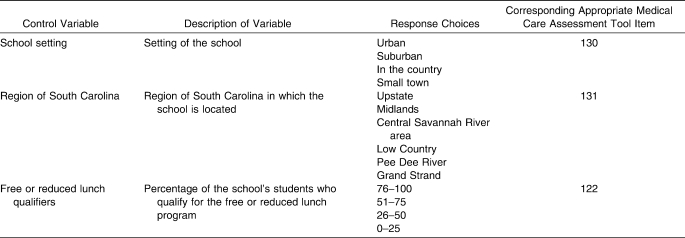
Several school-level factors that could influence the provision of medical care were included on the AMCAT as control variables: items 122, 130, and 131 (Table 4). The factors consisted of the setting of the school, the region of South Carolina in which the school was located, and a school's rate of free and reduced lunch qualifiers.
Table 4.
Control Variables, Descriptions of Variables, and Corresponding Appropriate Medical Care Assessment Tool Items
As is common in survey-based research,41 AMCAT items 81 and 121 (pertaining to having showers and working water fountains) were sham (or “throwaway”) items intended to reduce potential socially desirable responses on other items by allowing participants to “save face” because these are commonly available.
Pilot Study
We conducted a pilot study as a trial to ensure the clarity of the items and to determine the amount of time necessary to complete the AMCAT. The AMCAT was pilot tested on 3 former athletics directors at 3 South Carolina high schools and 4 ATs and 1 former AT at 5 high schools. The former athletics directors answered the AMCAT based on the medical care provided by their former school during the time in which each served as the program's athletics director. The ATs consisted of 2 groups. One group included 4 graduate assistant ATs from a large public university who were serving 1-year commitments as the ATs at area high schools. Also included was an AT who had formerly worked at a high school in another state. None of the individuals who took part in the pilot testing participated in the study.
All respondents were asked to complete the survey describing the medical care provided at their schools, to identify any items that seemed unclear, and to state how long it took them to complete the survey. For the 8 participants in the pilot study, the survey took approximately 10 to 15 minutes to complete. We modified the language of several items as a result of participants' feedback.
Instrument Reliability
In order to examine instrument reliability, we asked 20 schools to complete the AMCAT a second time and then compared those ACI scores with their original scores. The Pearson product moment correlation showed the test-retest reliability for ACI scores from the AMCAT to be high (r = 0.89).
Data Analysis
We used the statistical software package SPSS (version 12.0; SPSS Inc, Chicago, IL) for data analysis. Descriptive statistics (frequencies, percentages, means, and SDs) were calculated to describe the ACI scores for respondent schools in terms of presence of an AT, source of the AT, number of ATs, school size, distance to the nearest medical center, public or private status, annual sports medicine supply budget, and varsity football regional championships.
In order to determine which explanatory variables should be included in the linear regression analyses, we performed a series of 1-way analyses of variance (ANOVAs) to examine the association between categorical explanatory variables (presence of an AT, source of the AT, number of ATs, school size, distance to the nearest medical center, public or private status, sports medicine supply budget, and regional championships in football) and the continuous response variable (ACI score). Explanatory variables that had an association with the ACI score were later included in the initial regression analyses. Before performing the regression analyses, we calculated Spearman correlations among explanatory and control variables to avoid including 2 highly correlated variables in the regression analysis at the same time. Linear regression analyses were conducted to determine which explanatory variables were associated with the level of medical care as assessed by AMCAT when controlling for the school setting, region of the state, and rate of free or reduced lunch qualifiers. For variables identified as significant in the regression, a Tukey post hoc analysis was conducted. The level of significance was set at an α level of .05.
RESULTS
Descriptive Statistics
The mean ACI score for South Carolina high schools was 0.58, ranging from a low of 0.15 to a high of 0.94. Descriptive statistics (frequencies, means, and SDs) for explanatory and control variables are presented in Table 5.
Table 5.
Appropriate Medical Care Assessment Tool Respondents and Descriptive Statistics by Explanatory Variables
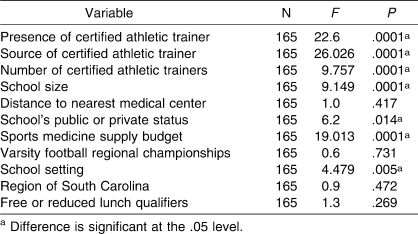
Narrowing Explanatory Variables
In order to determine the best explanatory variables to include in the regression analyses, we conducted a series of 1-way ANOVAs to identify associations between explanatory variables and ACI score. The presence of an AT, source of an AT, number of ATs, school size, school's public or private status, school's sports medicine supply budget, and school setting were associated with mean ACI score, whereas the distance to the nearest medical center, number of varsity football regional championships won, region of the state, and percentage of free and reduced lunch qualifiers were not associated with mean ACI score (Table 6).
Table 6.
One-Way Analysis of Variance for Explanatory Variables
Excluding Redundant Variables
A Spearman correlation was conducted to examine associations between all explanatory and control variables in order to exclude any variables that were closely associated and to prevent redundant variables from being included in the regression analysis. Three variables related to athletic training services (presence of an AT, source of the AT, and number of ATs) were found to be highly correlated: presence of an AT and number of ATs (r = 0.874), presence of an AT and source of the AT (r = 0.775), and source of the AT and number of ATs (r = 0.751). Given this high level of association between variables related to athletic training services, these variables were treated as essentially the same variable. Thus, only 1 variable (source of the AT) was selected for inclusion in the regression. Because of its close relationship with other variables related to athletic training services, it was renamed athletic training services. Although no other strong associations were identified between variables, it should be noted that budget was also moderately correlated with the variables involving athletic training services: source of the AT and budget (r = 0.576), number of ATs and budget (r = 0.519), and presence of an AT and budget (r = 0.441).
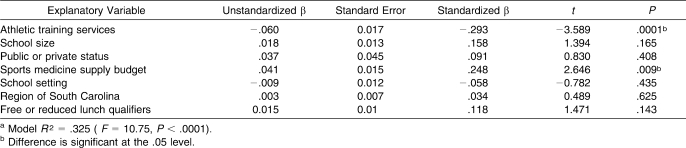
Regression Analyses
We conducted a series of linear regression analyses to identify factors associated with the level of medical care as assessed by AMCAT when controlling for the school setting, region of South Carolina, and percentage of free and reduced lunch qualifiers (Table 7). The following factors were regressed on the ACI score: athletic training services, school size, public or private status, sports medicine supply budget, school setting, region of South Carolina, and percentage of free and reduced lunch qualifiers. Excluded from this analysis were distance to the nearest medical center and varsity football regional championships, because they were not associated with ACI score on the 1-way ANOVAs. Even though the region of South Carolina and the percentage of free and reduced lunch qualifiers were not associated with ACI score in the preliminary analyses, they were included in the regression because they are commonly used as control variables. The resulting model was significant (F = 10.75, P < .0001) and accounted for almost one-third of the variance in the ACI scores (R2 = 0.325).
Table 7.
First Regression Analysis With Explanatory Variables Identified as Significantly Associated With Appropriate Care Index Score From 1-Way Analyses of Variancea
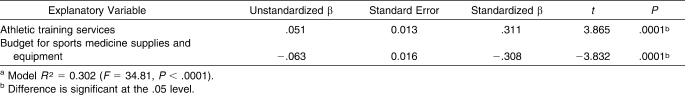
Of the variables included in the first regression, school size, public or private status, school setting, region of South Carolina, and percentage of free and reduced lunch qualifiers were found not to be predictors of ACI score and were, therefore, excluded from the final regression. When the regression analysis was run again, including only the 2 variables that were associated with ACI score in the preliminary analyses (athletic training services and sports medicine supply budget), the model remained significant (F = 34.81, P < .0001) and accounted for almost as much variance in ACI score (R2 = 0.302) as the first model (Table 8). Thus, athletic training services and a school's sports medicine supply budget were associated with variance in ACI score, suggesting that these variables were related to schools that provided higher levels of medical care for high school athletics in South Carolina.
Table 8.
Second Regression Analysis With Explanatory Variables Identified as Significantly Associated With Appropriate Care Index Score From First Regression Analysisa
Tukey Post Hoc Analysis
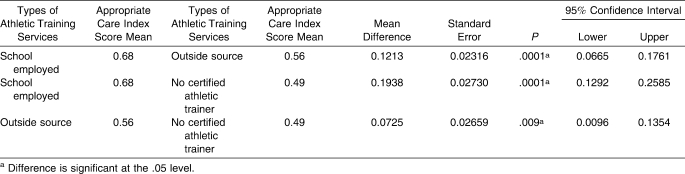
Post hoc analysis for athletic training services showed differences among ACI scores in schools at various levels. Differences were identified among schools with a school-employed AT, schools with an AT contracted from an outside source (mean difference = 0.1213 ± 0.023, P < .0001), and schools with no AT (mean difference = 0.1938 ± 0.027, P < .0001; Table 9). Differences in ACI scores between schools with an AT contracted from an outside source and those without an AT were also identified (mean difference = 0.0725 ± 0.027, P < .009).
Table 9.
Significant Associations From Post Hoc Analysis for Budget for Athletic Training Services
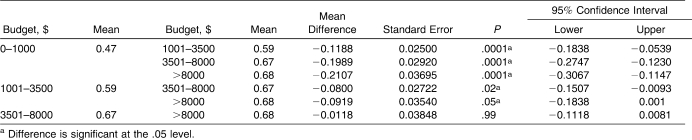
The post hoc analysis for sports medicine supply budget showed differences among ACI scores from schools at several levels. Differences were identified between schools with the lowest budgets and schools with budgets from $1001 to $3500 (mean difference = −0.12 ± 0.025, P < .0001), budgets of $3501 to $8000 (mean difference = −0.20 ± 0.029, P < .0001), and those schools with budgets greater than $8000 (mean difference = 0.21 ± 0.037, P < .0001; Table 10). Differences were also noted between schools with budgets of $1001 to $3500 and schools with budgets of $3501 to $8000 (mean difference = −0.08 ± 0.027, P < 0.02).
Table 10.
Significant Associations From Post Hoc Analysis for Budget for Sports Medicine Supplies and Equipment
DISCUSSION
Despite more than 30 years of recommendations for improvement,† medical care for high school athletes often remains lacking, with a group16 reporting in 2006 that half of high schools admitted to providing inadequate medical care for their athletes. No researchers have examined the medical care provided from a comprehensive framework or attempted to conduct a scientific analysis to determine factors related to schools that provide high-quality health care to their athletes. We used an instrument (AMCAT) based on such a framework (AMCSSAA consensus statement35 and monograph36) and conducted such an analysis. Unchangeable factors such as school size, distance to the nearest medical center, public or private status, varsity football regional championships, school setting, region of South Carolina, and percentage of free and reduced lunch qualifiers. We did find that in South Carolina, the existence of athletic training services and the size of a school's annual sports medicine supply budget were associated with the level of medical care provided by a high school for its athletes. Fortunately, both factors are changeable and under the control of a school or school district's decision makers. Our findings have great potential in assisting schools to improve the medical care provided to their athletes by allowing them to focus their resources on 2 factors that have been shown to make a difference: athletic training services and the sports medicine supply budget.
Athletic Training Services Associated With Medical Care Provided in a Secondary School Setting
In 1998, the American Medical Association (AMA) resolution H-470.995 recommended that all high schools provide athletic training services for their athletes.39 Many high schools have been slow to adopt this recommendation, with the National Athletic Trainers' Association estimating that only 42% of American high schools provide athletic training services for their athletes.42 Additionally, the AMA resolution called for a scientific assessment of the effect of ATs on the medical care provided in the high school setting. Our study, based on the recommendations of the AMCSSAA consensus statement35 and monograph,36 provides such an assessment, and our results offer support for the AMA recommendation of an AT in every high school.
Athletic training services were associated with the medical care provided by a high school, and differences in the medical care provided by schools are not related to school size, proximity to a medical center, public or private status, success of the school's varsity football program, school setting, region of South Carolina, or socioeconomic status of a school's students. This finding is encouraging, as it suggests that a school can improve the medical care provided for its athletes by hiring an AT, regardless of a variety of factors beyond the control of the school. When we consider the frequent recommendations to hire an AT to improve medical care for high school athletes from both the literature‡ and professional organizations,38,39,44 a significant difference in the medical care provided by a high school based on access to athletic training services is not surprising. However, until recently, the relationship between athletic training services and medical care has been assumed and anecdotal, with few researchers actually assessing the relationship in the high school setting. Although several groups45–48 provided some evidence that ATs improve certain aspects of medical care, we used the AMCAT, which was based on the AMCSSAA consensus statement35 and monograph,36 to scientifically assess the relationship between comprehensive medical care and athletic training services as requested by the AMA resolution. Our findings provide evidence to support the recommendation that high schools should hire ATs to coordinate comprehensive health care delivery systems for high school athletics programs.
Additionally, results of our post hoc analysis demonstrated that schools with ATs, whether employed by the school or contracted from an outside source, provided higher levels of medical care than schools without athletic training services. Furthermore, schools with school-employed ATs had higher ACI scores and could be said to provide higher levels of medical care than schools with ATs contracted from outside sources. Nass49 concluded that schools with school-employed ATs provided better medical care to high school athletes than schools with ATs contracted from an outside source. He attributed this difference in medical care to the limited amount of time the contracted AT was available to the athletes and encouraged further investigation. Our results support his conclusion that a difference in the level of medical care exists among schools based on the source of athletic training services. Awareness of this difference may help schools attempting to improve medical care for their athletics program by hiring school-employed ATs.
Sports Medicine Supply Budget Associated With Medical Care Provided in a Secondary School Setting
Although an association between the amount of money allocated to purchase sports medicine supplies and equipment and the medical care provided by high schools has been suggested,15,17,33,48 we are the first to identify a significant association between the size of the sports medicine supply budget and the level of medical care provided by a high school. We found the sports medicine supply budget to be associated with the ACI score when controlling for factors such as school size, distance to the nearest medical center, public or private status, varsity football regional championships, school setting, region of South Carolina, and percentage of free and reduced lunch program qualifiers. Thus, special consideration should be given to providing funds specifically designated for sports medicine supplies and equipment, because our findings suggest that the medical care provided by schools varies with budget size, regardless of many uncontrollable factors.
Further analysis of a school's annual sports medicine supply budget provided insight into the amount of funding. In our study, schools with sports medicine supply budgets greater than $8000 reported an ACI score mean of 0.68, schools with budgets of $3501 to $8000 reported a mean of 0.67, schools with budgets of $1001 to $3500 reported a mean of 0.59, and schools with sports medicine budgets of $0 to $1000 reported a mean of 0.47. Post hoc analysis suggested differences among some budget levels. Schools with the lowest budgets ($0–$1000) provided the lowest levels of medical care compared with schools in all other budget categories. A difference in medical care also existed between schools with budgets of $1001 to $3500 and schools with budgets of $3501 to $8000. No difference was identified between schools with budgets of $3501 to $8000 and schools with budgets of more than $8000. Thus, our data suggest that medical care in South Carolina high schools varied with 3 levels of budgets: $0–$1000, $1001–$3500, and more than $3500. This trend indicates that medical care improved with increased budgets, at least to a point. In short, our findings support Nass's49 conclusion that the level of medical care was commensurate with the amount of money a school was willing to invest, although there may be a point at which no additional improvement in medical care occurs after certain supplies and equipment are acquired. Our findings could be helpful for a school in determining an appropriate budget for its sports medicine program.
Implications: Evidence-Based Support for ATs in High Schools
In recent years, programs and policies adopted and implemented by school administrators have been the result of evidence-based research based on significant findings. The results of our study provide decision makers, such as school administrators and state legislators, with empirically based evidence for providing appropriate medical care to high school athletes that supports years of recommendations. Such data could finally be the impetus for decision makers to commit the funds needed to improve medical care for high school athletes by improving access to athletic training services for all athletes and providing reasonable sports medicine supply budgets.
Perhaps the results could even be used to lobby state legislators to provide the necessary funding to place ATs in all public high schools, as in Hawaii.5 In Hawaii, before the mid-1990s, public schools lacked the athletic training services that private schools offered to their athletes. Recognizing that a standard of care had been set by the state's private schools, the Hawaiian state legislature elected to provide funding for an AT for each public school. Our results quantify this difference for South Carolina high schools and show a difference in the medical care provided by high schools with access to athletic training services compared with schools lacking such access. These results provide support for the long-held recommendation that ATs should be hired to coordinate medical care for high school athletics programs. Decision makers (school administrators and state legislators) and those who influence decision makers (parents) should consider these data to help improve medical care for their high school athletes by committing to the hiring of ATs.
Limitations
Of course, certain limitations of our research must be acknowledged. First, we examined schools from only 1 state. Additionally, in our sample, schools with ATs responded at rates considerably higher than schools without ATs, public schools responded at rates considerably higher than private schools, and large schools responded at rates considerably higher than small schools. Several factors might have played a role in the failure of some schools to return the AMCAT. These schools may have chosen not to participate for fear of bringing attention to a deficiency in their athletics program. Athletics directors with heavy teaching or coaching loads might have had a limited amount of time to devote to their athletics director duties and insufficient time to complete the AMCAT. This explanation may account for the difference in response rates between large and small schools. It also likely explains the difference in response rates for public and private schools, because South Carolina private schools are small schools.
As with any survey-based research, social desirability could have influenced our respondents' answers. Additionally, the perspective of the respondent was likely colored by his or her past experiences. For example, a respondent who was previously employed at another institution, which provided what the respondent perceived as a higher or lower level of medical care, might have skewed his or her responses accordingly. Also, variability was evident in the background of the respondents, not uncommon in surveys examining the policies and practices of an organization or institution.40 Some respondents were athletics directors, some were ATs, and a few were other individuals, such as coaches or nurses. Although these differences in job responsibilities could have skewed the results, it should be noted that the AMCAT directions stated, “It should be filled out by the individual at your school who is most knowledgeable about the policies and practices regarding healthcare and safety issues in your athletics program.” Thus, the individual best suited to complete the survey would be expected to vary, based on the athletic department personnel employed by the school. Finally, it must be emphasized that cross-sectional studies, such as this one, can only identify associations, not establish causation.
Areas for Future Research
Many questions remain. Considering that our regression model only accounted for about one-third of the variance in medical care for high school athletes, other factors have important implications for improving care. We suspect that other factors related to athletic training services that were not examined in this study (such as the AT's years of experience, years employed at the school, teaching load, job description, compensation package, and athletic training facilities) may account for some of the remaining variance not explained in this study's model.
This study was limited to examining associations between the overall medical care provided by a high school and possibly related factors, but examining the significant factors pertinent to each recommendation of the consensus statement35 might also be insightful for improvements in care. Such an analysis might reveal different factors to be associated with different recommendations. Identifying such associations could have implications for even further improvements in the medical care provided by a high school's athletics program.
Perhaps the greatest potential for further study lies in other researchers making use of the assessment tool, the AMCAT. With the creation of the AMCAT, a survey based on a widely accepted set of recommendations (the AMCSSAA consensus statement35 and monograph36) has been developed to evaluate the medical care provided by a high school athletics program. Although we used the AMCAT to assess care in South Carolina, the survey could easily be applied to assess care provided by high school athletics programs in other states.
CONCLUSIONS
Our results, based on the recommendations of the AMCSSAA consensus statement35 and monograph,36 provide an answer to the AMA request50 for empirical data assessing the effect of ATs on the level of medical care in the high school setting, with associations noted between athletic training services and the medical care provided by high school athletics programs in South Carolina. Additionally, the size of the annual sports medicine supply budget also appears to be a critical predictor for the medical care provided to South Carolina high school athletes. This study's results provide guidance for improving the medical care provided for high school athletes and support the association between athletic training services and medical care in the high school setting.
Acknowledgments
We thank the athletics directors, coaches, and athletic trainers of South Carolina for their participation in this project.
Footnotes
*: References 1, 4, 5, 11, 17, 18, 20, 22, 25, 28, 30, 33, 38, 39.
†: References 1, 4, 5, 11, 17, 18, 20, 22, 25, 28, 30, 33, 38, 39.
‡: References 4, 5, 11, 14–17, 18–20, 22–25, 27, 30, 31, 33, 34, 43, 44.
REFERENCES
- 1.Garrick J. G., Requa R. K. Injuries in high school sports. Pediatrics. 1978;61(3):465–469. doi: 10.1542/peds.61.3.465. [DOI] [PubMed] [Google Scholar]
- 2.Culpepper M. I., Niemann K. M. A comparison of game and practice injuries in high school football. Physician Sportsmed. 1983;11(10):117–122. doi: 10.1080/00913847.1983.11708662. [DOI] [PubMed] [Google Scholar]
- 3.Powell J. 636,000 injuries annually in high school football. Athl Train J Natl Athl Train Assoc. 1987;22(1):19–22. [Google Scholar]
- 4.Whieldon T. J., Cerny F. J. Incidence and severity of high school athletic injuries. Athl Train J Natl Athl Train Assoc. 1990;25(4):344–349. [Google Scholar]
- 5.Buxton B. P., Okasaki E. M., McCarthy M. R., Ho K. W. Legislative funding of athletic training positions in public secondary schools. J Athl Train. 1995;30(2):115–120. [PMC free article] [PubMed] [Google Scholar]
- 6.Gomez E., DeLee J. C., Farney W. C. Incidence of injury in Texas girls' high school basketball. Am J Sports Med. 1996;24(5):684–687. doi: 10.1177/036354659602400521. [DOI] [PubMed] [Google Scholar]
- 7.Beachy G., Akau C. K., Martinson M., Olderr T. F. High school sports injuries: a longitudinal study at Punahou School. 1988 to 1996. Am J Sports Med. 1997;25(5):675–681. doi: 10.1177/036354659702500515. [DOI] [PubMed] [Google Scholar]
- 8.Powell J. W., Barber-Foss K. D. Injury patterns in selected high school sports: a review of the 1995–1997 seasons. J Athl Train. 1999;34(3):277–284. [PMC free article] [PubMed] [Google Scholar]
- 9.Powell J. W., Barber-Foss K. D. Sex-related injury patterns among selected high school sports. Am J Sports Med. 2000;28(3):385–391. doi: 10.1177/03635465000280031801. [DOI] [PubMed] [Google Scholar]
- 10.Rechel J. A., Yard E. E., Comstock R. D. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204. doi: 10.4085/1062-6050-43.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Redfearn R. W. Are athletes getting good health care? Physician Sportsmed. 1975;3(8):34–39. doi: 10.1080/00913847.1975.11948239. [DOI] [PubMed] [Google Scholar]
- 12.Bowers K. D., Jr Young athletes enduring alarming treatment delays. Physician Sportsmed. 1976;4(10):57–59. [Google Scholar]
- 13.Kegerreis S. Health care for student athletes. J Phys Educ Rec. 1979;50(6):78–79. [Google Scholar]
- 14.Lackland D. T., Akers P., Hirata I., Jr High school football injuries in South Carolina: a computerized survey. J S C Med Assoc. 1982;78(2):75–78. [PubMed] [Google Scholar]
- 15.Carek P. J., Dunn J., Hawkins A. Health care coverage of high school athletics in South Carolina: does school size make a difference? J S C Med Assoc. 1999;95(11):420–425. [PubMed] [Google Scholar]
- 16.Aukerman DF, Aukerman M. M., Browning D. Medical coverage of high school athletics in North Carolina. South Med J. 2006;99(2):132–136. doi: 10.1097/01.smj.0000199749.22741.5e. [DOI] [PubMed] [Google Scholar]
- 17.Vangsness C. T., Jr, Hunt T., Uram M., Kerlan R. K. Survey of health care coverage of high school football in Southern California. Am J Sports Med. 1994;22(5):719–722. doi: 10.1177/036354659402200524. [DOI] [PubMed] [Google Scholar]
- 18.Lindaman L. M. Physician care for interscholastic athletes in Michigan. Am J Sports Med. 1991;19(1):82–87. doi: 10.1177/036354659101900114. [DOI] [PubMed] [Google Scholar]
- 19.Lindaman L. M. Athletic trainer availability in interscholastic athletics in Michigan. J Athl Train. 1992;27(1):9–16. [PMC free article] [PubMed] [Google Scholar]
- 20.Tucker J. B., O'Bryan J. J., Brodowski B. K., Fromm B. S. Medical coverage of high school football in New York State. Physician Sportsmed. 1988;16(9):120–130. doi: 10.1080/00913847.1988.11709601. [DOI] [PubMed] [Google Scholar]
- 21.Porter M., Noble H. B., Bachman D. C., Hoover R. L. Sportsmedicine care in Chicago-area high schools. Physician Sportsmed. 1980;8(2):95–99. doi: 10.1080/00913847.1980.11948564. [DOI] [PubMed] [Google Scholar]
- 22.Bell G. W., Cardinal R. A., Dooley J. N. Athletic trainer manpower survey of selected Illinois high schools. Athl Train J Natl Athl Train Assoc. 1984;19(1):23–24. [Google Scholar]
- 23.Tonino P. M., Bollier M. J. Medical supervision of high school football in Chicago: does inadequate staffing compromise healthcare? Physician Sportsmed. 2004;32(2):37–40. doi: 10.3810/psm.2004.02.123. [DOI] [PubMed] [Google Scholar]
- 24.Rutherford D. S., Niedfeldt M. W., Young C. C. Medical coverage of high school football in Wisconsin in 1997. Clin J Sport Med. 1999;9(4):209–215. doi: 10.1097/00042752-199910000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Wrenn J. P., Ambrose D. An investigation of health care practices for high school athletes in Maryland. Athl Train J Natl Athl Train Assoc. 1980;15(2):85–92. [Google Scholar]
- 26.Culpepper M. I. The availability and delivery of health care to high school athletes in Alabama. Physician Sportsmed. 1986;14(1):131–137. doi: 10.1080/00913847.1986.11708971. [DOI] [PubMed] [Google Scholar]
- 27.Culpepper M. I., Niemann K. M. Professional personnel in health care among secondary school athletics in Alabama. South Med J. 1987;80(3):336–338. doi: 10.1097/00007611-198703000-00015. [DOI] [PubMed] [Google Scholar]
- 28.deShazo W. F., III High school athletic injuries: a coaches' and physicians' dilemma. Ala Med. 1983;53(2):21–22. [PubMed] [Google Scholar]
- 29.Brunet M. E., Giardina D. Sports medicine in Louisiana: a survey of 242 high schools. J La State Med Soc. 1984;136(8):25–27. [PubMed] [Google Scholar]
- 30.Cartland J. E., Jr Medical care of high school athletes in Connecticut. Conn Med. 1985;49(10):645–646. [PubMed] [Google Scholar]
- 31.Fick D. Medical supervision of student athletes. Iowa Med. 1995;85(9):362. [PubMed] [Google Scholar]
- 32.Mathews E., Esterson P. Sports medicine in Northern Virginia high schools. Athl Train J Natl Athl Train Assoc. 1983;18(2):181–182. [Google Scholar]
- 33.McCarthy M. R., Hiller W. D., Yates-McCarthy J. L. Sports medicine in Hawaii: care of the high school athlete in Oahu's public schools. Hawaii Med J. 1991;50(11):395–396. [PubMed] [Google Scholar]
- 34.Schrader J. W. An analysis of athletic health care management in Indiana's secondary schools. Indiana Med. 1985;78(12):1104–1106. [PubMed] [Google Scholar]
- 35.Appropriate medical care for secondary school-age athletes consensus statement. National Athletic Trainers' Association Web site. http://www.nata.org/statements/consensus/Consensus%20Statement_Final%20Version_Sept02.pdf. Accessed July 8, 2008.
- 36.Appropriate medical care for the secondary school-age athlete monograph. National Athletic Trainers' Association Web site. http://www.nata.org/statements/support/secondary_school_medcarecommunication.pdf. Accessed July 8, 2008.
- 37.Almquist J., Valovich McLeod T. C., Cavanna A., et al. Summary statement: appropriate medical care for the secondary school-aged athlete. J Athl Train. 2008;43(4):416–427. doi: 10.4085/1062-6050-43.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Athletic trainers for high school athletes. American Academy of Family Physicians Web site. http://www.aafp.org/online/en/home/policy/policies/s/athletictrainhsathletes.html. Accessed July 8, 2008.
- 39.Certified athletic trainers in secondary schools. American Medical Association Council on Scientific Affairs Web site. http://www.ama-assn.org/ama1/pub/upload/mm/443/csaa-98.pdf. Accessed July 8, 2008. [PMC free article] [PubMed]
- 40.DeVellis R. F. Scale and Development: Theory and Applications. Thousand Oaks, CA: Sage; 2003. 2nd ed. [Google Scholar]
- 41.Dillman D. A. Mail and Internet Surveys: The Tailored Design Method. New York, NY: Wiley and Sons; 2000. [Google Scholar]
- 42.Robinson B. Value of athletic trainers in secondary school. National Federation of State High School Associations Web site. http://www.nfhs.org/web/2009/01/value_of_athletic_trainers_in_th.aspx. Accessed March 17, 2009.
- 43.Lackland D. T., Testor J. M., Akers P. C., Hirata I. H. Jr, Knight R. M., Mason J. L. The utilization of athletic trainer/team physician services and high school football injuries. Athl Train J Natl Athl Train Assoc. 1985;20(1):20–23. [Google Scholar]
- 44.Chambers C. L. President's column: when developing policies on school safety, don't neglect the safety of student athletes. Sch Board News. August 2000. http://www.nsba.org/HPC/Features/AboutSBN/SbnArchive.aspx. Published August 8, 2000. Accessed November 4, 2005.
- 45.Legwold G. Injury rate lowered by high school trainers. Physician Sportsmed. 1983;11(11):35–36. [Google Scholar]
- 46.Albohm M. J., Wilkerson G. B. An outcome assessment of care provided by certified athletic trainers. J Rehabil Outcomes Meas. 1999;3(3):51–56. http://www.nata.org/employers/occ-ind/outcomes.pdf. Accessed July 8, 2008. [Google Scholar]
- 47.Value model of the certified athletic trainer in the occupational setting. National Athletic Trainers' Association Web site. http://www.nata.org/employers/occ-ind/value_model.pdf. Accessed July 8, 2008.
- 48.Certified athletic trainers deliver ROI in occupational work settings. National Athletic Trainers' Association Web site. http://www.nata.org/employers/hosp-clinic/deliver_ROI.htm. Accessed July 8, 2008.
- 49.Nass S. J. A survey of athletic medicine outreach programs in Wisconsin. J Athl Train. 1992;27(2):180–183. [PMC free article] [PubMed] [Google Scholar]
- 50.Lyznicki J. M., Riggs J. A., Champion H. C. Certified athletic trainers in secondary schools: report of the Council on Scientific Affairs, American Medical Association. J Athl Train. 1999;34(3):272–276. [PMC free article] [PubMed] [Google Scholar]